Introduction
Meniere's disease (MD) is a complex inner ear
disease that clinically manifests as recurrent rotatory vertigo,
sensorineural hearing loss, tinnitus and sensation of ear fullness
(1). Previous epidemiological
studies found that there were 17-513 patients with MD per 100,000
individuals in Asia, where prevalence is markedly higher compared
with that for systemic lupus erythematosus and multiple lupus
erythematosus (2,3). Endolymphatic hydrops is a
characteristic pathological manifestation of MD (4). Although a previous study has found
that the etiology of endolymphatic hydrops may be associated with
autoimmunity, allergy, inheritance and infection, there is no
definitive cause to this condition (5). Since the etiology and pathogenesis of
MD remain unclear, no specific diagnostic guidelines are available
that can be used in clinical settings (6,7). In
addition, empirical symptomatic or surgical treatments and drug
therapy for treating the mechanism of action of MD are also
unavailable (6,7). Therefore, it is important and of
scientific significance to investigate the pathogenesis, potential
auxiliary diagnostic marker(s) and therapeutic agents for MD.
Immunological factors are important in the
development of MD in some patients (8). A previous study demonstrated that the
endolymphatic sac is important in immune responses, where they can
mediate the development of endolymphatic hydrops (9). MD may be an immune-mediated disease or
even an autoimmune disease (10).
In a previous study investigating the immunological mechanism of
MD, Harada et al (11) used
stria vascularis tissues from rabbits as antigens to immunize
guinea pigs to construct an endolymphatic hydrops model.
Immunoglobulin G antibody and complement components were detected
in the endolymph fluid of the experimental guinea pigs, leading to
the hypothesis that circulating immune complex (CIC) deposited in
the stria vascularis of the inner ear damages the secretion and
absorptive function of the endolymph fluid, resulting in
endolymphatic hydrops (11).
Numerous studies have also demonstrated that the CIC level was
significantly higher in most patients with MD (12-14).
Therefore, the role of the immune complex during the onset of MD
has become an interesting topic of research. However, there remains
to be a lack of investigations into the association between CIC
levels in patients with MD and the severity, clinical stages and
prognosis assessment of endolymphatic hydrops.
MD remains to be a disease that is difficult to
diagnose, particularly in the early stages due to the absence of
significant symptoms. Therefore, for complex inner ear diseases,
such as MD, the therapeutic goals should not be limited to only
controlling the symptoms. Instead, it is important to also develop
tools for the effective diagnosis and treatment of inner ear
diseases. Of note, there is a trend to specifically select a
treatment to block the generation of endolymphatic hydrops by
analyzing the causes of endolymphatic hydrops (15). Immunotherapy have been widely used
for the treatment of tumors (16,17)
and have been documented to be beneficial in controlling the
symptoms in patients with MD (18,19).
However, to the best of our knowledge, no previous study exist that
clearly addressed the mechanism of action and efficacy of
immunosuppressants in MD. Cyclophosphamide (CTX) is a nitrogen
mustard derivative that is hydrolyzed by phosphoamidase or
phosphatase activities in the liver or tumors to become the
phosphoramide nitrogen mustard (20). CTX is toxic to rapidly proliferating
cells and mediate their effects primarily by weakening DNA
synthesis, rendering it to be a commonly used immunosuppressant
(21). In addition, CTX has been
widely used for numerous different diseases, such as acute
leukemia, lymphoma, solid tumors and several autoimmune diseases,
including severe rheumatoid arthritis, systemic lupus
erythematosus, nephrotic syndrome in children and multiple
granuloma (22,23). However, studies investigating the
efficacy of CTX for the treatment of MD remain insufficient.
Therefore, the present study aimed to explore the
diagnostic value of serum CIC in MD patients, in addition to
investigating the therapeutic potential of CTX for the treatment of
MD. Data on patients with MD in a clinical setting was collected in
the present study, following which CIC expression levels in
different clinical stages of MD were statistically analyzed.
Additionally, the potential value of using CIC for the diagnosis
and treatment of patients with MD was also investigated. In another
branch of the present study, an autoimmune MD guinea pig model was
constructed to compare the association between CIC change prior to
and following CTX treatment and the degree of endolymphatic hydrops
and clinical symptom improvement to investigate the therapeutic
potential in MD.
Materials and methods
Clinical sample collection
A total of 48 unilateral patients with MD (20 males
and 28 females; mean age, 43.79±1.35 years) who were diagnosed
between July 2017 and May 2019 were collected and screened based on
the Diagnosis and Treatment Guidelines of Meniere's Disease (2017)
(24) from The Affiliated Hospital
of Inner Mongolia Medical University (Hohhot, China). Patients with
nephritis, systemic lupus erythematosus, allergic diseases and
other immune system diseases and those who received hormone or
immunosuppressive therapy within the last 3 months were excluded.
In addition, another 48 age-matched healthy adult individuals (18
males and 30 females; mean age, 45.27±1.22 years), who came in for
physical examination at The Affiliated Hospital of Inner Mongolia
Medical University, were recruited as the control group. All
individuals were fasted for 6 h before the collection of 10 ml
peripheral venous blood, which was subsequently stored at -20˚C for
subsequent experiments. The present study was reviewed and approved
by the Ethics Committee of The Affiliated Hospital of Inner
Mongolia Medical University and written informed consent was
provided from the patients and the healthy controls.
Clinical diagnostic criteria
The following clinical diagnostic criteria for MD
was used: i) In total, > two vertigo onsets, each lasting
between 20 min and 12 h; ii) in total, ≥ one audiological
examination confirming low to medium sensorineural hearing loss of
the affected ear during the course of the disease; and iii) the
affected ear had fluctuating hearing loss, tinnitus and/or
sensation of ear fullness. The following exclusion criteria were
used: i) Vertigo induced by other diseases, including vestibular
migraine, sudden deafness, benign paroxysmal positional vertigo,
labyrinthitis, vestibular neuronitis, paroxysmal vestibulopathy,
drug toxic vertigo, posterior circulation ischemia and intracranial
space-occupying lesion; and ii) secondary endolymphatic
hydrops.
Pure tone audiometry and disease
classification method
A pure tone audiometer (GSI 61™; Grason-Stadler,
Inc.) was used for pure tone audiometry. The average air conduction
thresholds at 0.5, 1, 2 and 4 kHz were obtained from the result of
the auditory threshold. In addition, disease was classified based
on the following classes from the result of pure tone audiometry
(25): i) Class 1, pure tone
average (PTA) <25 decibels hearing level (dBHL); ii) Class 2,
PTA=26-40 dBHL; iii) Class 3, PTA=41-70 dBHL; and iv) Class 4, PTA
>70 dBHL.
Magnetic resonance imaging (MRI)
The mix of normal saline and gadopentetate
dimeglunmine (0.5 ml/person) injection (Consun Pharmaceutical
Group, Ltd.) was used as the contrast medium for MRI and injected
following an 8-fold dilution at ratio of seven saline: One
gadopentetate dimeglunmine. An Allegra 3.0T MRI Scanner (Siemens
AG) was used for scanning, whilst an 8-channel head coil was used
for collection. The fast spin echo (T2 weighted image turbo spin
echo) was first used to obtain a conventional coronal T2-weighted
image scan through the inner hear duct plane to exclude any lesions
in the intracerebral and cerebellopontine angle areas. A
three-dimensional (3D)-FLAIR sequence was then used to produce a
high-resolution labyrinth scan and localization throughout the
inner ear.
Multiplanar image reconstruction (Picture archiving
and communication systems, PACS/RIS 3.1; Neusoft Medical Systems
Co., Ltd.) was performed to obtain horizontal images for analysis.
Following injection of the contrast reagent, the peri-lymphatic
fluid was shown as the high-intensity zone whereas the membranous
labyrinth was presented as the low-intensity zone on the 3D-FLAIR
MRI original thin-layer image.
Subsequently, 3D reconstruction (Picture archiving
and communication systems, PACS/RIS 3.1; Neusoft Medical Systems
Co., Ltd.) was performed on the image at the post-processing stage
to measure the area of endolymph space in the vestibulum and the
total area of ipsilateral vestibulum auris. The following
calculation was used to determine the ratio (R): R=low-intensity
zone/(low-intensity zone + high-intensity zone) x100%. Using the
following diagnostic criteria proposed by Nakashima et al
(26), endolymphatic hydrops was
diagnosed in cases of moderate hydrops and severe hydrops: i) Mild
hydrops, R value ≤33.3%; ii) moderate hydrops, R value >33.3 and
≤50.0%; and iii) severe hydrops, R value >50.0%.
Vestibular-evoked myogenic potential
(VEMP) test
A CHARTR Diagnostics System (model MCU-90; ICS
Medical Corporation) was used for the VEMP (ICS Chartr EP 200;
Natus Medical, Inc.) test (27).
The recording electrode was first placed onto the skin surface at
the midpoint of the sternocleidomastoid muscle, whilst the
reference electrode was placed onto the upper part of sternum. The
center of the forehead was grounded. The parameters used for the
test were the following: i) Band-pass filtering, 50-3,000 Hz; ii)
scanning time, 100 msec; iii) stacking fold, 150; iv) stimulation
rate, 5.1/sec; v) short pure tone frequency, 500 Hz; vi) envelope,
2 msec rise/decline; vii) plateau stage, 0 msec; and viii) alter
polarity, stimulation intensity, 95 decibels (dB) normal hearing
level (dBnHL). During the examination, each individual was asked to
raise the head by 30˚ to tense up the sternocleidomastoid muscle at
certain times but kept the head and neck still to record the VEMP
latency, amplitude under bilateral short sound stimulation
condition and to calculate the VEMP bilateral amplitude ratio and
symmetry. A bilateral amplitude ratio >1.61 was considered to be
abnormal.
Electrocochleography (EcochG)
test
A CHARTR Diagnostics System (model MCU-90; ICS
Medical Corporation) was also used for the EcochG test. A Life-Tech
ear electrode model 8501 (Life-Tech) was used as a silver bead
electrode, whilst the ICS Medical insert earphones 300 ohms (ICS
Medical Corporation) was applied as an insert earphone. This test
was conducted in a sound-proof chamber. The silver bead electrode
was placed underneath the posterior lower quadrant of the eardrum,
whilst the reference electrode was placed at the ipsilateral
earlobe. The contralateral earlobe was grounded. Test parameters
were recorded as follows: i) Short sound stimulation, cycle 100
µsec; scanning time, 10 msec; band-pass filtering, 5-3,000 Hz;
sparse wave/dense wave alter polarity, gain 50-100 k; stimulation
rate, 11.1/sec; stacking fold, 1,000; and stimulation intensity, 90
dBnHL; ii) Short tone burst, envelope 2 msec rise/decline; plateau
stage, 10 msec; scanning time, 20 msec; band-pass filtering,
5-3,000 Hz; alter polarity, gain 50-100 k; stimulation rate,
11.1/sec, stacking fold, 1,000; and stimulation intensity, 90
dBnHL. The amplitude of summating potentia (SP) and Action
potential and Compound action potential (AP) were measured with the
initial baseline set as the standard, in µV. SP/AP ≥0.4 was
considered to be abnormal.
Auditory brainstem response (ABR)
Using the Smart EP M010000 device (Intelligent
Hearing Systems), click short sound stimulation was used to record
the response threshold, wave I, III, V latency and interpeak
latency in guinea pigs. The test is carried out in the room with
sound insulation and electric shielding. The recording electrode
was then placed subcutaneously on the top of the skull before the
reference electrode was placed in the posterior region of the
ipsilateral ear in guinea pigs. The tip of the nose is grounded.
Earphone and hollow silicone tube were inserted and connected to
the external auditory canal of guinea pigs. The mean and 2X
standard deviation were used as the criterion for abnormity. Wave
I, ≥1.82 msec; wave III, ≥4.14 msec; and wave V, ≥6.02 msec were
considered as prolonged latency. The distortion product otoacoustic
emission (OAE3.75, Intelligent Hearing Systems; https://www.medicalexpo.com.cn/prod/intelligent-hearing-systems/product-79938-500100.html)
was applied to record the response amplitude and signal-to-noise
ratio.
ELISA
ELISA was used for detecting the concentrations of
CIC (cat. no. JL11776; Shanghai Jianglai industrial, Ltd.), tumor
necrosis factor-α (TNF-α; cat. no. FT-P32761R; Shanghai Fantai
Biotechnology Co., Ltd.) and heat shock protein 70 (HSP70; cat. no.
FT-P32201R; Shanghai Fantai Biotechnology Co., Ltd.; https://www.hbzhan.com/st628355/product_20565139.html)
in the serum samples of patients with MD and those from healthy
individuals according to the manufacturer's protocols. The
concentration of isologous crude inner ear antigens (ICIEAg) was
measured from ~2 ml serum of guinea pigs before euthanasia (the
guinea pigs were euthanized immediately after blood collection)
using a specially made ELISA kit (provided by Shanghai Fantai
Biotechnology Co., Ltd.) which was constructed by Shanghai Fantai
Biotechnology Co., Ltd. After the blood samples were collected,
they were kept at room temperature for 15 min and then stored at
4˚C until further use. The samples were then centrifuged at 1,200 x
g for 30 min at 4˚C before the supernatant was transferred into a
new microcentrifuge tube and stored at -20˚C for subsequent
use.
The standard was diluted serially five times,
according to the manufacturer's protocols. Standard, blank and test
sample wells were then constructed, using 50 µl of the
serially-diluted standard, no sample or enzyme-labeled reagent and
4 µl standard diluent and 10 µl test sample, respectively.
After loading the samples, the plate was sealed then
incubated at 37˚C for 30 min. The coated plate was then rinsed
after the liquid was discarded and then spin-dried following which,
50 µl enzyme-labeled reagent was added into the standard and test
sample wells and incubated at 37˚C for 30 min. Subsequently, the
plate was spin-dried for a second time, before 50 µl developer A
and B were added into each well and the plate was incubated at 37˚C
for 15 min after mixing.
Subsequently, 50 µl stop buffer was added into each
well, the blank well was zeroed and the absorbance [optical density
(OD)] of each well was measured at 450 nm using a Varioskan LUX
reader (Thermo Fisher Scientific, Inc.). The concentration of each
sample was determined using a calibration curve, which was plotted
based on the concentration and OD value of the standard
samples.
Construction and processing of the
autoimmune MD guinea pig model
The construction of the model refers to the previous
research (28). The animal
experiments were performed at the Specific Pathogen Free Animal
Laboratory at the Inner Mongolia Medical University (Hohhot,
China). A total of 45 male guinea pigs (purchased from
GemPharmatech, Co., Ltd.; age, 5 months; weight, 600-900 g) were
housed with four animals per cage at 20-25˚C with 60% humidity in a
quiet and well-ventilated environment with 12-h light/dark cycle.,
where food (containing vitamin C) and water were supplied freely.
Animal health and behavior were monitored every day and body
weights were assessed weekly over the course of the study.
ICIEAgs were obtained as follows: In total, five
guinea pigs were decapitated under anesthesia (pentobarbital sodium
40 mg/kg was injected intraperitoneally) to obtain the inner ear
tissues and to separate and place the membranous labyrinth in PBS
for grinding, pulverizing and mixing. This solution was centrifuged
using 15-cm centrifuge tubes at 200 x g at 4˚C for 10 min. The
supernatant was collected to obtain the protein content following
quantification using the bicinchoninic acid Protein Assay kit
(Beyotime Institute of Biotechnology).
ICIEAg (0.4 mg) and Freund's adjuvant (0.2 ml) were
injected in each animal for immunization, following which ICIEAg
(0.2 mg) and Freund's adjuvant (0.2 ml) were injected 10 days later
for two supplementary immunizations (fortified immunity), at an
interval of 10 days. The guinea pigs were also tested under
different Hz 1 day before immunization. At total of 10 days after
the last immunization, ICIEAg (0.05 mg) and Freund's adjuvant
(0.025 ml) were used for local lymph sac immunization (local lymph
sac immunization). The concentration of ICIEAg in immunity (ICIEAg
immunization 10 days), fortified immunity (ICIEAg and Freund's
adjuvant immunization 10 days after the immunity stage) and
lymphatic sac immunity (ICIEAg and Freund's adjuvant immunization
10 days after the fortified immunity stage) groups was measured
using ELISA. The hearing threshold of pre-immunization (before the
ICIEAg immunization) and post-immunization (2 weeks after local
lymph sac immunization) group at 4, 8 and 16 kHz was measured via
ABR. In total each animal (30 animals) were immunized four times
with three injections per immunization. In total, 10 guinea pigs
were immunized with PBS as the control group.
A total of 30 guinea pigs were used for the further
study and were randomly divided into the following three groups (10
guinea pigs per group): i) Group A, normal saline (NaCl) group; ii)
group B, dexamethasone group (intraperitoneal injection of
dexamethasone, 2 mg/d/kg); and iii) group C, CTX group
(intraperitoneal injection of CTX, 2.5 mg/d/kg). Guinea pigs were
housed in individual cages, with ad libitum access to food and
water and administered. After 2 weeks of raising, guinea pigs was
treated with dexamethasone or CTX in different groups. Guinea pigs
were anesthetized using an intraperitoneal injection of 40 mg/kg
sodium pentobarbital. Under anesthesia, all guinea pigs were
decapitated. ICIEAg concentration in the serum was also measured 2
weeks after being treated with dexamethasone or CTX in the three
groups before euthanasia. Death was confirmed by the stopping of
the heart and breathing rate, as well as the disappearance of the
foot withdrawal reflex.
The present study was approved by the Animal Ethics
Committee of Affiliated Hospital of Inner Mongolia Medical
University (approval no. IMMU2018028; Hohhot, China). All related
experiments were conducted in accordance with the ‘Code for the
Care and Use of Animals for Scientific Purposes’ statement and
under the principles of 3R (replacing, refining, and reducing)
(29).
Total inner ear protein extraction and
western blotting
Following intraperitoneal injection for anesthesia,
the guinea pigs were decapitated to rapidly obtain the inner ear
tissues and to remove the entire membranous labyrinth tissue under
sterile conditions at 4˚C. The tissue was placed into PBS
containing 40 g/l phenylmethylsulfonyl fluoride, 10 mmol/l
β-mercaptoethanol and 1% SDS, mixed at 4˚C, frozen and thawed for
four cycles (-20 to 4˚C) before being centrifuged at 12,000 x g at
4˚C for 20 min. The concentration of the protein in the supernatant
was then determined using bicinchoninic acid Protein Assay kit and
separated using 10% SDS-PAGE (40 µg protein per lane). The proteins
were then transferred onto a PVDF membrane before being blocked for
1 h with 5% skimmed milk at 25˚C. After washing, the membrane was
incubated at 4˚C overnight with the following prediluted primary
antibodies: Anti-HSP70 (1:1,000; cat. no. ab2787; Abcam) and
anti-β-actin (1:2,000; cat. no. ab8226; Abcam). The membrane was
then incubated with horseradish peroxidase (HRP)-conjugated
secondary antibody (1:1,000; cat. no. A0208; Beyotime Institute of
Biotechnology) without agitation for 60 min at 20-25˚C. Signals
were visualized using ECL reagents (EMD Millipore) and detected
using an Amersham™ Imager 680 (Cytiva).
Hematoxylin and eosin (H&E)
staining
Following cardiac puncture and blood withdrawal from
the guinea pigs under anesthesia, they were decapitated under
anesthesia to rapidly harvest their inner ear tissues and for
fixation in 4% paraformaldehyde for 24 h at 25˚C.
EDTA-Na2 (10 mM) was used for decalcification for 10-15
days at 25˚C. Tissues were paraffin-embedded at 56˚C and sliced at
the central axis (10-mm thickness), followed by deparaffinization
at 60˚C for 10 min, a 15 min immersion in xylene and rehydrated in
a descending ethanol gradient. hematoxylin (5 min) and eosin (1
min) staining at 25˚C and observed using an Olympus light
microscope at x400 magnification (Olympus Corporation).
Immunohistochemistry detection of CIC
expression in the inner ear
The inner ear tissues were removed under anesthesia
and the cochleae was separated. A hole was created at the cochlear
tip to open the oval and round windows. At 4˚C, the cochlea was
perfused with PBS containing 4% paraformaldehyde via the cochlear
tip. The cochleae were then fixed in the same solution for 24 h at
25˚C and rinsed with PBS before being placed into formic acid. In
sodium formate solution, 1 week of decalcification was performed at
room temperature, with the decalcifying solution replaced every
day. After rinsing using PBS, the cochleae were removed and placed
into a 30% sucrose solution overnight at 4˚C. After sedimentation,
optimal cutting compound embedding (cat. no. 4583; Sakura Finetek
Europe B.V.) was performed. The cryostat slicer moved in 10 µm
sections, in a parallel direction to the modiolus for continuous
slicing at -20˚C. After drying, CIC immunohistochemistry was
performed.
The tissue sections were deparaffinized by a 15 min
immersion in xylene. The sections were then rehydrated via
sequential incubation in 100, 90 and 70% ethanol. Samples were
rinsed with PBS followed by distilled water and incubated for 30
min in 3% H2O2 at 25˚C. Antigen retrieval
(cat. no. P0085; Beyotime Institute of Biotechnology) was performed
via microwave irradiation at 95˚C for 10 min. The sections were
first permeabilized using 0.3% Triton X-100 at 25˚C for 5 min and
then blocked with 10% rabbit serum (Beijing Solarbio Science &
Technology Co., Ltd.) at 37˚C for 20 min. Afterwards, sections were
incubated with anti-C3 (1:1,000; cat. no. ab200999; Abcam) at 4˚C
overnight (an important component of CIC) (30,31).
The slides were washed four times in TBS/saponin and incubated with
horseradish peroxidase-conjugated rabbit SignalStain®
Boost IHC Detection Reagent (1:2,000, cat. no. 8114S; Cell
Signaling Technology, Inc.) for 30 min at 25˚C for 1 h. The slides
were incubated with a 0.5 mg/ml HRP substrate solution (DAB +
H2O2 prepared in distilled water) to expose
the resulting peroxidase activity. Slides were washed four times in
PBS and counterstained for 1 min with hematoxylin at 25˚C. The
slides were sealed and observed under optical light microscopy at
x40 magnification.
Statistical analysis
SPSS v19.0 (IBM Corp.) and GraphPad Prism v7
statistical software packages (Graphpad Software, Inc.) were used
for statistical analyses. The measurement data are presented as the
mean ± SD. Student's t-test was used for between-group comparisons,
whilst one-way ANOVA with Tukey's post hoc test was used for
pairwise comparisons among multiple groups. Pearson's test was
conducted to analyze the correlation between plasma and inner ear
CIC concentration. The enumeration data were analyzed using
χ2 test and linear correlation analysis. P<0.05 was
considered to indicate a statistically significant difference.
Results
Clinical information
There were a total of 48 patients with MD and 48
healthy control volunteers who were included in the present study.
There were 18 males in the control group (37.5%) and 20 males in
the MD group (41.7%). The mean weight of the patients was
67.04±1.01 and 69.1±1.08 kg in control and MD groups, respectively.
There was no significant difference in the age, sex distribution
and weight distribution between the two groups (Table I). In addition, the clinical
characteristics and stage of the patients with MD were analyzed
(Table I). Pure tone audiometry was
investigated in the patients with MD and the results found that
10.4 (n=5), 33.3 (n=16), 41.7 (n=20) and 14.6% (n=7) of patients
had stage I, II, III and IV, respectively (Table I). MRI was subsequently used to
assess the degree of endolymphatic hydrops in the patients with MD
and the results revealed that 20.8 (n=10), 56.3 (n=27) and 22.9%
(n=11) of patients had mild, moderate and severe endolymphatic
hydrops, respectively (Table I).
The VEMP test showed that normal, abnormal and negative VEMP was
observed in 41.7 (n=20), 37.5 (n=18) and 20.8% (n=10) of patients,
respectively (Table I). Finally,
the results of the ECochG test revealed that 39.6 (n=19) and 60.4%
(n=29) of patients had normal and abnormal results, respectively
(Table I).
 | Table IClinical characteristics of the
patients with MD and healthy controls. |
Table I
Clinical characteristics of the
patients with MD and healthy controls.
|
Characteristics | Control (n=48) | MD (n=48) | P-value |
|---|
| Mean age ± SD
(years) | 45.27±1.215 | 43.79±1.347 | >0.05 |
| Sex, male, n
(%) | 18 (37.5) | 20 (41.7) | >0.05 |
| Mean weight ± SD
(kg) | 67.04±1.006 | 69.1±1.082 | >0.05 |
| Pure tone
audiometry, n (%) | | | |
|
Phase I | | 5 (10.4) | |
|
Phase
II | | 16 (33.3) | |
|
Phase
III | | 20 (41.7) | |
|
Phase
IV | | 7 (14.6) | |
| Endolymphatic
hydrops, n (%) | | | |
|
Light | | 10 (20.8) | |
|
Medium | | 27 (56.3) | |
|
Severe | | 11 (22.9) | |
| VEMP, n (%) | | | |
|
Normal | | 20 (41.7) | |
|
Abnormal | | 18 (37.5) | |
|
Negative | | 10 (20.8) | |
| ECochG, n (%) | | | |
|
Normal | | 19 (39.6) | |
|
Abnormal | | 29 (60.4) | |
Concentration of immune parameters in
the serum from patients with MD
To investigate the association between MD and the
immune response, the concentration of CIC, TNF-α and HSP70 in the
serum of patients with MD was investigated. The results showed that
the concentration of CIC, TNF-α and HSP70 was significantly
increased in the serum of patients with MD compared with that in
the control group, suggesting that the occurrence and development
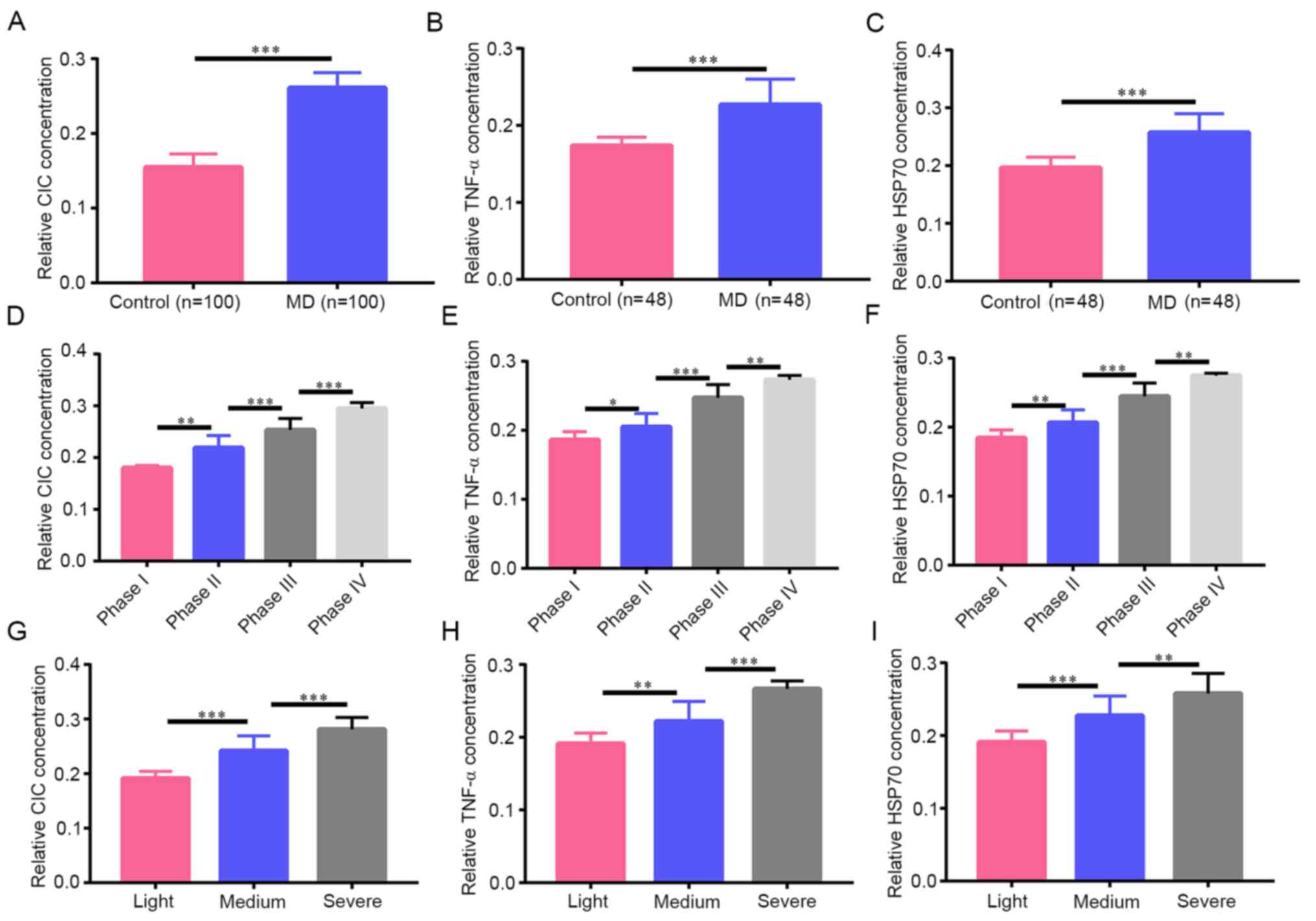
of MD was associated with the immune response (Fig. 1A-C). Subsequently, the association
between the concentration of CIC, TNF-α and HSP70 and the clinical
characteristics of patients with MD, was also analyzed. The results
indicated that the phase of pure tone audiometry was positively
associated with the concentration of CIC, TNF-α and HSP70 in the
serum of patients with MD (Fig.
1D-F). In addition, the concentrations of CIC, TNF-α and HSP70
in the serum of patients with MD were also positively associated
with the the severity of endolymphatic hydrops (Fig. 1G-I). Taken together, CIC in the
serum of patients with MD were significantly increased compared
with that in the control group, demonstrating that immune factors
can potentially be important for the development of MD. Further
analysis of the results indicated that immune indices CIC, TNF-α
and HSP70 are positively associated with the clinical stages and
severity of MD, suggesting that they can be applied as potential
diagnostic markers of MD.
CIC expression in the autoimmune MD
guinea pig model
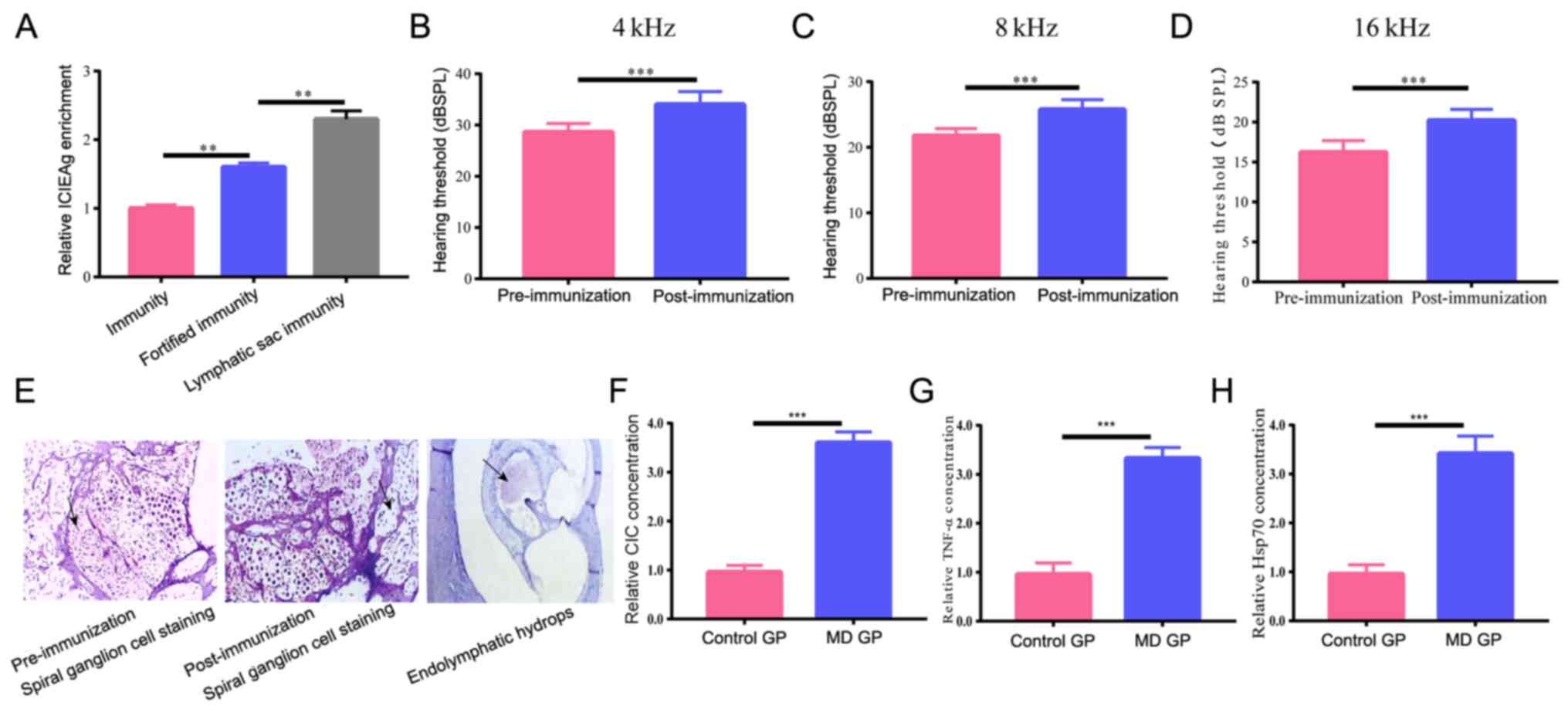
To further identify the potential value of CIC for
the diagnosis and treatment of MD, a guinea pig MD model was
established using autoimmunity via injection with ICIEAg isolated
from other guinea pigs. To determine if the model had been
successfully established, the concentration of ICIEAg in guinea
pigs during the early immunization stage, after systemic booster
immunization and local lymph sac immunization was detected. The
results of ELISA showed that after each stage of immunization,
ICIEAg concentration in guinea pigs was significantly increased
compared with that at the previous stage (Fig. 2A), suggesting effective
immunization. In total, 1 day before immunization and 2 weeks after
the final ICIEAg + freund's adjuvant, the ABR threshold at 4, 8 and
16 kHz was measured, where the results revealed that at all three
frequencies, the threshold post-immunization was significantly
higher compared with that before immunization (Fig. 2B-D). H&E staining results
indicated that at 2 weeks post-immunization, spiral ganglions were
notably fewer in number in guinea pigs with endolymphatic hydrops
clearly observed compared with that in the pre-immunization group
(Fig. 2E), suggesting successful
construction of the MD guinea pig model. Subsequently, CIC
expression level in the control and MD guinea pigs (2 weeks after
the final immunization) were determined and it was found that CIC
expression was significantly increased in the serum of MD guinea
pigs compared with that in the control group (Fig. 2F), which further implicate the
potentially important roles of CIC during the course of MD. In
addition, TNF-α and HSP70 concentrations in the MD guinea pigs were
significantly higher compared with that in the control group
(guinea pigs immunized with PBS; Fig.
2G and H).
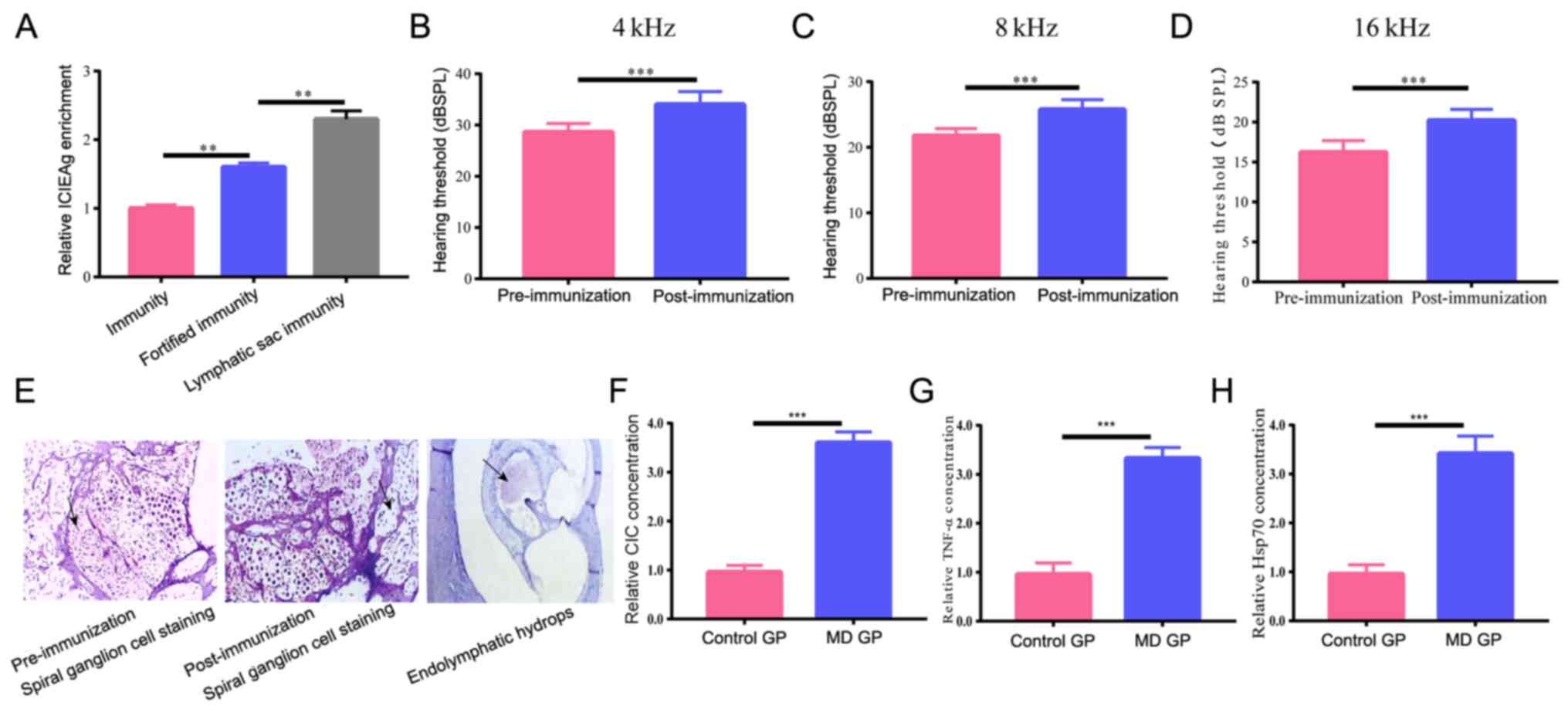 | Figure 2CIC expression level in the
autoimmune MD guinea pig model. (A) ELISA was conducted to detect
the ICIEAg concentration in guinea pigs in early immunization,
after systemic booster immunization and local lymph sac
immunization was gradually increased after each stage of
immunization. The auditory brainstem response threshold at (B) 4,
(C) 8 and (D) 16 kHz threshold was notably higher 2 weeks after
immunization compared with that before immunization through
auditory brainstem response. (E) Hematoxylin and eosin staining
results indicated that 2 weeks after immunization, spiral ganglions
were fewer in number in guinea pigs with extensive endolymphatic
hydrops. Magnification x400. (F) CIC, (G) TNF-α and (H) HSP70
concentration in serum was significantly increased in guinea pigs
with MD compared with that in the control group via ELISA.
**P<0.01 and ***P<0.001. GP, guinea
pigs; dBSPL, Decibel Sound Pressure Level; CIC, circulating immune
complex; TNF, tumor necrosis factor; HSP70, heat shock protein 70;
MD, Meniere's disease. |
CTX suppresses MD progression by
reducing CIC generation
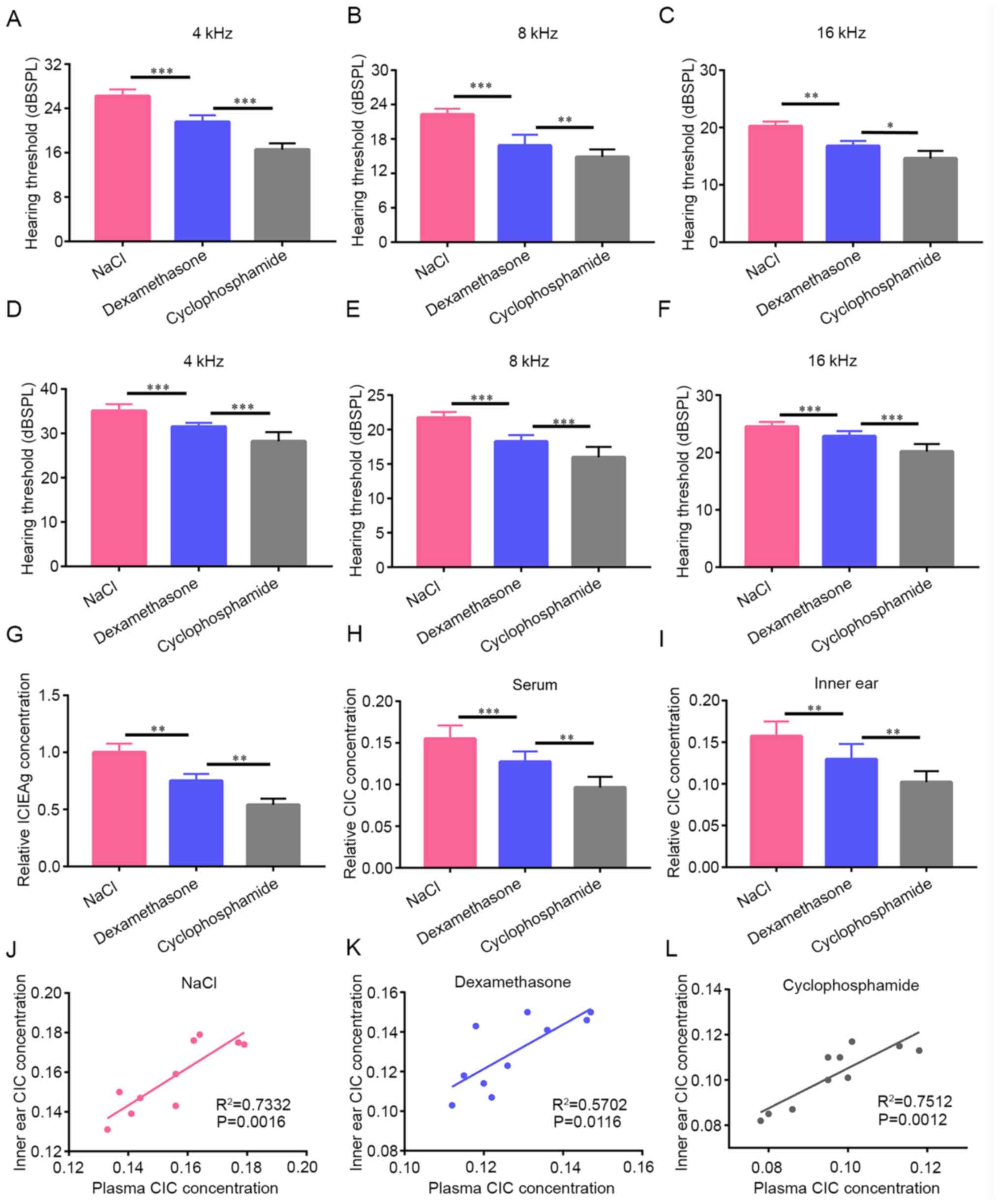
To investigate the effects of CTX treatment on MD,
MD guinea pigs were randomly divided into the NaCl, dexamethasone
and CTX groups, with 10 guinea pigs in each group, with treatment
beginning 2 weeks after the final immunization. At 1 (Fig. 3A-C) and 2 weeks (Fig. 3D-F) post-treatment, changes in the
ABR threshold were detected at 4, 8 and 16 kHz in each group. The
results revealed that the threshold was the highest in the NaCl
group, followed by the dexamethasone and CTX groups, with the
differences among the three groups significant (Fig. 1A-F), suggesting that CTX is more
effective compared with that in dexamethasone. ICIEAg concentration
in the serum was next measured 2 weeks after treatment in the three
groups and it was found that the concentration of ICIEAg in the
dexamethasone group was significantly lower compared with that in
the NaCl group, whilst the ICIEAg concentration in the CTX group
was significantly decreased compared with that in the dexamethasone
group (Fig. 3G). Subsequently, CIC
expression was detected in the serum samples of each group after 2
weeks treatment, where the highest CIC expression was found in the
NaCl group, followed by the dexamethasone and CTX groups (Fig. 3H), suggesting that CTX exerted its
roles by reducing CIC generation. Subsequently, ELISA was used to
detect the CIC deposition in the inner ear tissue of each group
after 2 weeks treatment and the results revealed that CIC
expression showed the same trend as that exhibited by CIC levels in
the serum (Fig. 3I), suggesting
that CTX also reduced CIC deposition in the inner ear tissues.
Finally, Pearson's correlation analysis was used to analyze the
correlation between CIC expression in the serum and inner ear
tissues of each group, where the results indicated that CIC
expression in the serum was positively correlated with that in the
inner ear tissue in all three treatment groups tested (Fig. 3J-L). This suggest that CIC
deposition in the inner ear tissue could be found by detecting CIC
expression in the circulation, rendering CIC expression to be
potentially useful as an index for evaluating the degree of MD. CTX
was also found to suppress MD progression more effectively than
dexamethasone by reducing CIC generation.
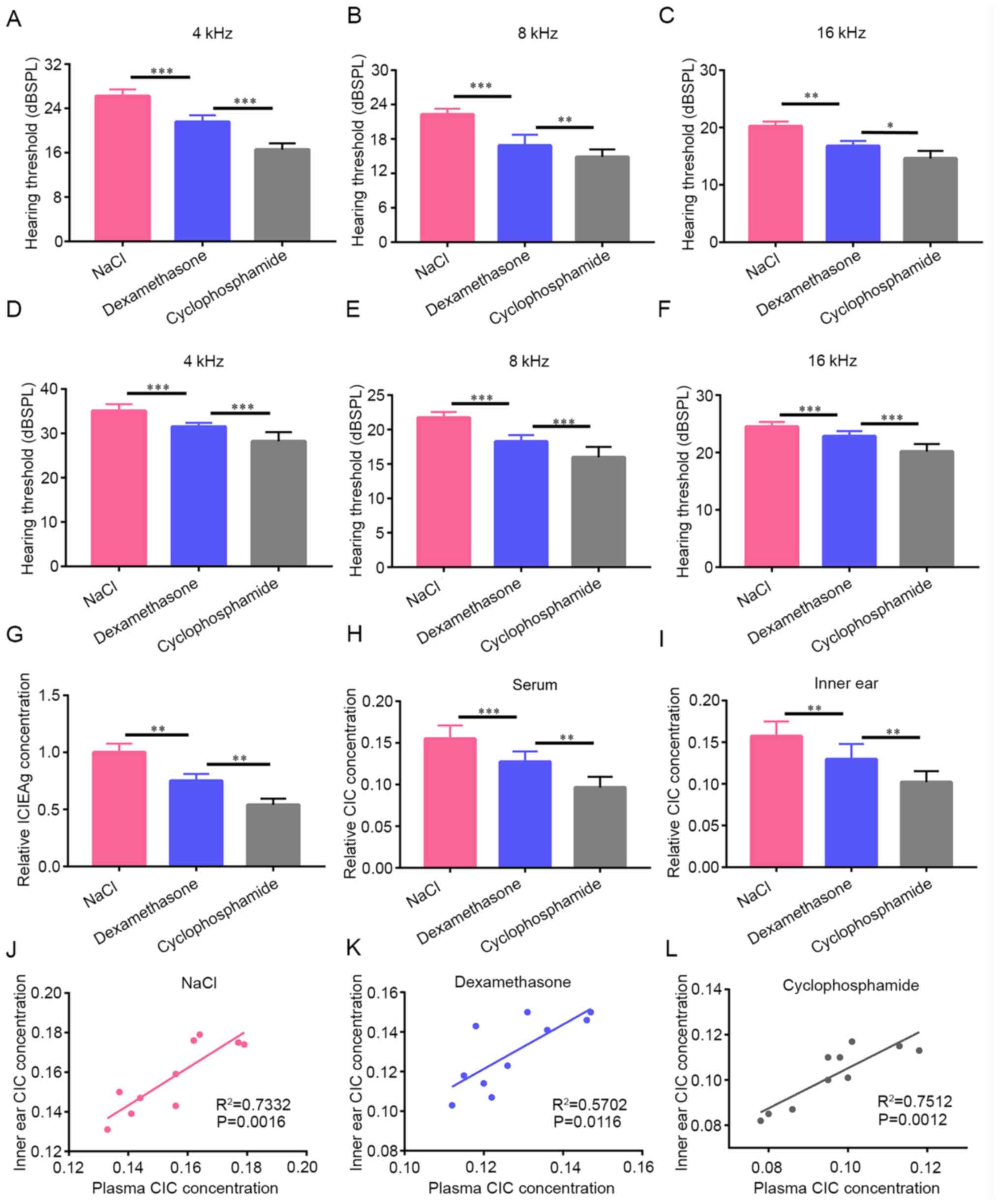 | Figure 3CTX suppresses MD progression by
reducing CIC generation. A total of 1-week post-treatment, the ABR
threshold at (A) 4, (B) 8 and (C) 16 kHz was the highest in the
NaCl group, followed by the dexamethasone group and then the CTX
group. After 2 weeks of treatment, the CTX group exhibited the
lowest ABR threshold at (D) 4, (E) 8 and (F) 16 kHz and guinea pigs
in the NaCl group had the highest ABR threshold. (G) ICIEAg
expression in the dexamethasone group was significantly lower
compared with that in the NaCl group, whilst ICIEAg expression in
the CTX group was significantly decreased compared with that in the
dexamethasone group tested by ELISA. The CIC concentration in the
(H) serum or (I) inner ear tissues was highest in the NaCl group,
followed by the dexamethasone group and then the CTX group detected
by ELISA. (J-L) Pearson's correlation analysis showed the CIC
concentration in the serum was positively correlated with that in
the inner ear tissue in the (J) NaCl, (K) CTX and (L) Dexamethasone
groups. *P<0.05, **P<0.01 and
***P<0.001. CTX, cyclophosphamide; MD, Meniere's
disease; ICIEAg, isologous crude inner ear antigens; ABR, auditory
brainstem response. |
Effects of CTX on HSP70 and TNF-α
concentration
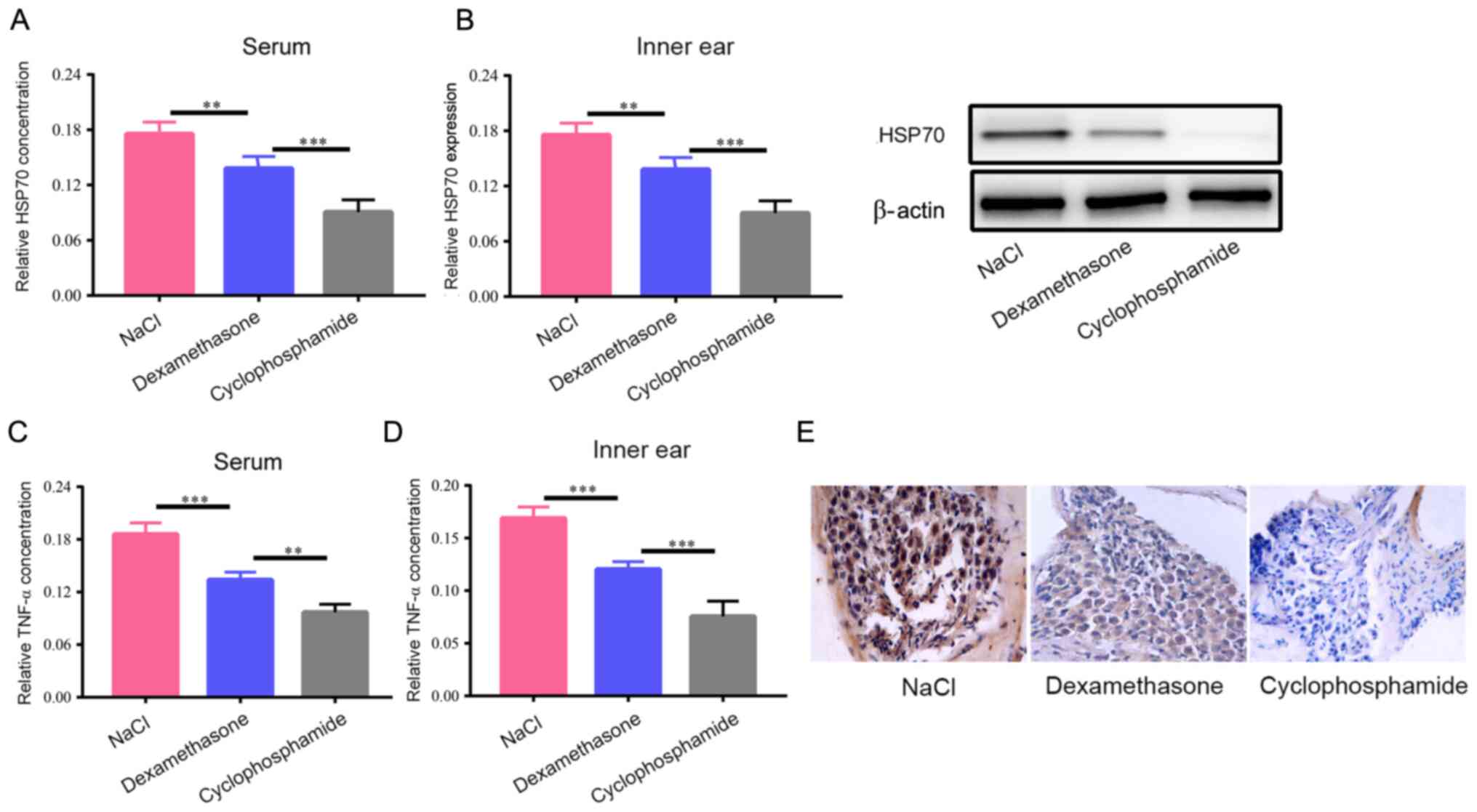
Considering that CTX may reduce the generation of
CIC, it was hypothesized whether the same role could be found with
the immune indices HSP70 and TNF-α. The results of the ELISA showed
that HSP70 concentration in the circulation of the dexamethasone
group was significantly lower compared with that in the NaCl group,
whereas HSP70 concentration in the CTX group was significantly
reduced compared with that in the dexamethasone group (Fig. 4A). After harvesting the inner ear
tissue from each group, western blot analysis was used to detect
the protein expression level of HSP70 in the inner ear tissue of
each group and the results revealed the same trend of HSP70
expression in the inner ear tissue, with HSP60 expression being the
lowest in the CTX group (Fig. 4B).
ELISA was then used to measure TNF-α concentration in the inner ear
tissue and serum samples of each group and the results revealed
that the lowest TNF-α concentrations were found in the CTX group
(Fig. 4C and D). This suggest that in addition to the
reduction of CIC generation, CTX also suppressed HSP70 and TNF-α
expression. Finally, inner ear tissues were collected from each
group for immunohistochemical staining and the results found the
most CIC deposition in the NaCl group, followed by the
dexamethasone and CTX groups (Fig.
4E). As shown by the aforementioned results, CTX exerted
specific effects on MD in manners that were more effective compared
with those exerted by dexamethasone, possibly by inhibiting the
autoimmune response.
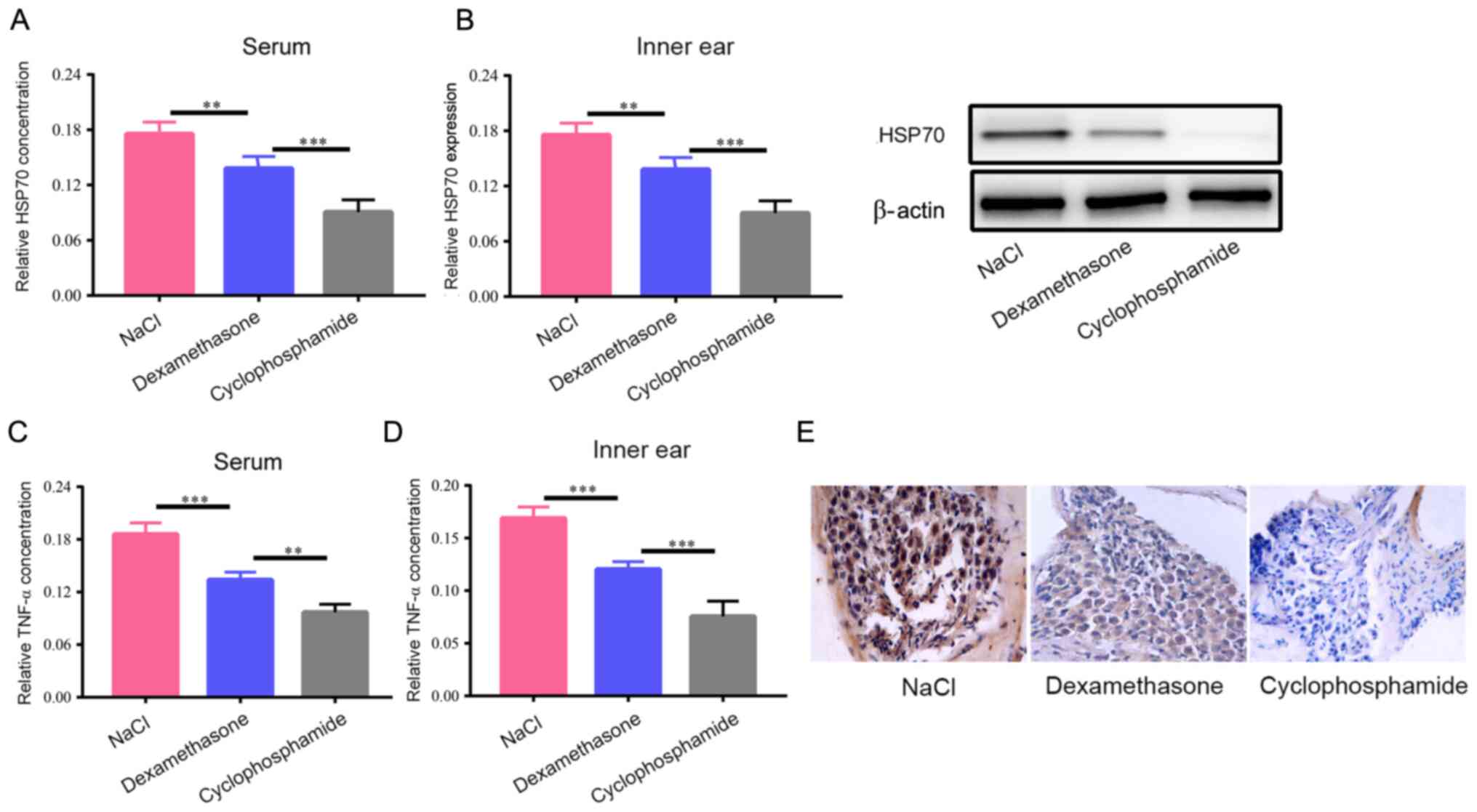 | Figure 4Effects of CTX on HSP70 and TNF-α
concentration levels. (A) ELISA revealed that HSP70 concentration
in the circulation of the dexamethasone group was significantly
lower compared with that in the NaCl group, whilst HSP70
concentration in the CTX group was significantly reduced compared
with that in the dexamethasone group. (B) Western blotting showed
that HSP70 protein expression in the inner ear of the dexamethasone
group was significantly lower compared with that in the NaCl group,
whilst HSP70 concentration in the CTX group was significantly
reduced compared with that in the dexamethasone group. ELISA showed
that the TNF-α concentration in the (C) serum or (D) the inner ear
tissues was also decreased in the NaCI, dexamethasone compared with
that in the NaCl group, whilst TNF-α concentration was lower in the
CTX group compared with that in the dexamethasone group. (E)
Immunohistochemical staining showed that the highest CIC deposition
was in the NaCl group, followed by the dexamethasone group and then
the CTX group. Magnification, x400. **P<0.01 and
***P<0.001. CIC, circulating immune complex; TNF,
tumor necrosis factor; HSP70, heat shock protein 70; CTX,
cyclophosphamide. |
Discussion
The typical histopathological manifestation of MD is
endolymphatic hydrops, which may involve the cochlea, vestibulum
and semicircular canal to damage the cochlear and vestibular
functions (32). However, the
association between the symptoms and corresponding pathological
manifestations induced by these symptoms remain unclear.
Histopathological changes in patients with MD cannot be assessed
directly during the course of the disease in a clinical setting.
Therefore, the present study aimed to provide specific clinical
data to further elucidate the factors underlying the occurrence and
development of MD by detecting CIC concentration in the
circulation. The present study enrolled 48 patients with MD and 48
control volunteers, who were not significantly different in terms
of their age, sex or weight.
Previous studies (27,33)
showed that VEMP was weakened or could not be induced in 35-54%
patients with MD. In the present study, VEMP was weakened or could
not be induced in 58.3% of patients, which was consistent with
these previous studies aforementioned. It has been reported that
ECochG changes are one of the most typical audiological
manifestations of endolymphatic hydrops (1). ECochG manifestation in patients with
MD is represented by higher SP/AP ratios, which are associated with
higher SP or lower AP (34). This
is induced by excessive lymph fluids, resulting in the displacement
of the basilar membrane (35).
However, this examination lacks sensitivity (35). The positive rate of abnormal ECochG
was only found to be 60.4% in the present study. Nevertheless,
similar to the results in the present study, Helling et al
(36) performed ECochG in 334
patients with MD and found abnormal results in ~56.3% of patients.
This was probably due to the higher SP or lower AP caused by
multiple factors, reducing the specificity of ECochG. High
resolution MRI provides new opportunities for the diagnosis of MD
and enables a clear display of the endolymphatic hydrops (37). In the present study, MRI was used to
analyze endolymphatic hydrops in 48 patients, where more moderate
hydrops (56.3%) were found, with less mild and severe hydrops (20.8
and 22.9%, respectively).
CIC is a substance formed by the combination of
antigens and corresponding antibodies that immune complexes bind to
during the complement pathway and other immunoreactive substances
(38). They deposit onto the
vascular wall, resulting in tissue injury and vasculitis (39). If immune complexes are detected in
the circulating blood, they would be known as CICs. If CIC deposits
in the stria vascularis and endolymphatic sac, endolymphatic
hydrops may be induced accordingly (18). Savastano et al (40) previously analyzed the roles of
non-specific serological immunity tests in determining the
immunopathology of patients with MD and found that CIC was
significantly increased in serum, leading to the hypothesis that
CIC determination can be used as a prognosis index to monitor the
clinical development of MD. In the present study, ELISA was
utilized to detect CIC concentration in the patients with MD and in
the control group. The results revealed notably higher CIC levels
in patients with MD and that CIC was increased with the progression
of clinical stage and the severity of endolymphatic hydrops. This
suggest that CIC could have a certain diagnostic value for the
occurrence and development of MD, which can be used as a biomarker.
In addition, TNF-α and HSP70 concentrations showed the same trend
in patients with MD, indicating that immune factors are also
important during the course of MD.
Considering existing studies of collagen type
II-induced autoimmune ear disease, Matsuoka et al (41) found that the guinea pig
endolymphatic hydrops model could be induced by directly injecting
the collagen type II peptide monoclonal antibody into the scala
tympani, with a success rate of ~100%. This method could be used
for the study of autoimmune MD (40). To further investigate the
association between CIC and MD, in vivo experiments were
performed in the present study by constructing an autoimmune MD
guinea pig model. After local immunization using ICIEAg in
systemically sensitized guinea pigs, guinea pigs developed
significant hearing loss. The results of immunohistochemistry
revealed markedly less spiral ganglion cells in the guinea pig
model group and endolymphatic hydrops in the inner ear, suggesting
that the autoimmune MD guinea pig model was successfully
constructed. Using ELISA, CIC concentration was significantly
increased in the MD guinea pig model compared with that in the
control group. In addition, immune parameters TNF-α and HSP70 were
also notably increased, further demonstrating an association
between immune factors and MD onset.
There is currently no consensus and effective method
for the treatment of MD. A previous study has found that
betahistine may promote blood flow into the cochlea (42) that may be used to reduce the degree
and frequency of vertigo in patients with MD. However, evidence of
its effectiveness remains controversial. Bodmer et al
(43) treated patients with MD by
drip transfusion of gentamicin into the tympanum and found that
long-term vertigo was controlled effectively. However,
aminoglycosides conferred vestibulotoxicity for the treatment of MD
and therefore are not commonly used in a clinical setting (36). A previous study has found that
injecting steroid hormones into the tympanum was effective for MD
treatment (44). However, in
another study it observed that the injection of dexamethasone into
the tympanum was only a temporary alternative treatment option for
MD, where endolymphatic hydrops was temporarily reduced 1 month
after treatment but returned to the initial value 1 year later
(45). Recent studies have observed
that immunosuppressants were effective for MD (46,47). A
study previously found that CTX may notably improve hearing in
patients with autoimmune inner ear disease (48). Kilpatrick et al (49) observed that a small dose of oral
methotrexate was effective and safe for the treatment of
immune-mediated bilateral MD. However, there are only a few studies
investigating the efficacy of immunosuppressants for the treatment
of immune-mediated MD. In addition, no report exists on the
mechanism of action of CTX for immune-mediated MD. Therefore,
further investigation is required.
In the present study, MD guinea pigs were first
randomly divided into the NaCl, dexamethasone and CTX groups. At 7
and 14 days post-administration, the ABR threshold was measured in
each group. The frequency was statistically significantly different
between the dexamethasone and NaCl groups. Local dexamethasone
treatment was effective in the treatment of autoimmune MD. However,
CTX was more effective for the treatment of autoimmune MD compared
with that in dexamethasone, providing a theoretical basis for
guiding clinical medication for MD. Subsequently, the expression of
CIC and other immune parameters in the circulation and the inner
ear tissue was detected, where it was found that CTX significantly
reduced the expression of CIC, TNF-α and HSP70 compared with that
in the dexamethasone group. In addition, immunohistochemistry
results confirmed lower CIC deposition in the inner ear tissue of
the CTX group, suggesting that CTX can inhibit MD development by
reducing CIC expression.
In conclusion, the present study provided novel
strategies for the treatment of early MD, which is difficult to
diagnose using clinical screening and data. In addition, the
present study also provides evidence for the potential value of
serum CIC concentration for the diagnosis, staging and prognosis
assessment of autoimmune MD. To address the amibiguity of MD
treatment, the present study investigated the mechanism of action
and efficacy of CTX for the treatment of autoimmune MD using guinea
pig models, to demonstrate the immunological mechanism of MD and
provide an experimental foundation for the clinical promotion of
drug therapy. These data can provide a potential development
strategy for the early diagnosis and drug therapy of MD.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Natural Science
Foundation of Inner Mongolia Autonomous Region (grant no.
2019MS08123) and Inner Mongolia Medical University Youth Innovation
Fund project (grant no. YKD2017QNCX064).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
SZ designed the study. SZ and YG conducted the
guinea pig experiments. YL, BW, WG and QX conducted data analysis
and interpretation of data. SZ and YG authenticate the data in this
study. All authors read and approved the final revision of the
manuscript.
Ethics approval and consent to
participate
Animal use and care were performed in accordance
with the Guide for the Care and Use of Laboratory Animals published
by the US National Institutes of Health. This study was approved by
the Animal Ethics Committee of Affiliated Hospital of Inner
Mongolia Medical University (grant no. IMMU2018028). Written
informed consent was provided from the patients and the healthy
controls Animal experiments were performed in the SPF Animal
Laboratory at Inner Mongolia Medical University.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Anft D, Jamali Y, Scholz G and Mrowinski
D: Electrocochleography and phase audiometry in diagnosis of
Meniere disease. HNO. 49:102–108. 2001.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
2
|
Sun Y, Zhang D, Sun G, Lv Y, Li Y, Li X,
Song Y, Li J, Fan Z and Wang H: RNA-sequencing study of peripheral
blood mononuclear cells in sporadic Meniere's disease patients:
Possible contribution of immunologic dysfunction to the development
of this disorder. Clin Exp Immunol. 192:33–45. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Pai I, Mendis S, Murdin L, Touska P and
Connor S: Magnetic resonance imaging of Meniere's disease: Early
clinical experience in a UK centre. J Laryngol Otol. 134:302–310.
2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hallpike CS and Cairns H: Observations on
the pathology of Meniere's syndrome: (Section of otology). Proc R
Soc Med. 31:1317–1336. 1938.PubMed/NCBI
|
|
5
|
Caulley L, Quimby A, Karsh J, Ahrari A,
Tse D and Kontorinis G: Autoimmune arthritis in Meniere's disease:
A systematic review of the literature. Semin Arthritis Rheum.
48:141–147. 2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Greco A, Gallo A, Fusconi M, Marinelli C,
Macri GF and de Vincentiis M: Meniere's disease might be an
autoimmune condition? Autoimmun Rev. 11:731–738. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Cooper MW and Kaylie DM: Is endolymphatic
sac surgery beneficial for Meniere's disease? Laryngoscope.
130:2738–2739. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Mathews J, Rao S and Kumar BN: Autoimmune
sensorineural hearing loss: Is it still a clinical diagnosis? J
Laryngol Otol. 117:212–214. 2003.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Dornhoffer JL, Waner M, Arenberg IK and
Montague D: Immunoperoxidase study of the endolymphatic sac in
Meniere's disease. Laryngoscope. 103:1027–1034. 1993.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Gazquez I, Soto-Varela A, Aran I, Santos
S, Batuecas A, Trinidad G, Perez-Garrigues H, Gonzalez-Oller C,
Acosta L and Lopez-Escamez JA: High prevalence of systemic
autoimmune diseases in patients with Meniere's disease. PLoS One.
6(e26759)2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Harada T, Matsunaga T, Hong K and Inoue K:
Endolymphatic hydrops and III type allergic reaction. Acta
Otolaryngol. 97:450–459. 1984.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lopez-Escamez JA, Saenz-Lopez P, Gazquez
I, Moreno A, Gonzalez-Oller C, Soto-Varela A, Santos S, Aran I,
Perez-Garrigues H, Ibañez A and Lopez-Nevot MA: Polymorphisms of
CD16A and CD32 Fcγ receptors and circulating immune complexes in
Meniere's disease: A case-control study. BMC Med Genet.
12(2)2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Derebery MJ, Rao VS, Siglock TJ, Linthicum
FH and Nelson RA: Meniere's disease: An immune complex-mediated
illness? Laryngoscope. 101:225–229. 1991.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hsu L, Zhu XN and Zhao YS: Immunoglobulin
E and circulating immune complexes in endolymphatic hydrops. Ann
Otol Rhinol Laryngol. 99:535–538. 1990.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kim SH, Kim JY, Lee HJ, Gi M, Kim BG and
Choi JY: Autoimmunity as a candidate for the etiopathogenesis of
Meniere's disease: Detection of autoimmune reactions and diagnostic
biomarker candidate. PLoS One. 9(e111039)2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Zheng N and Lu Y: Targeting the IL-9
pathway in cancer immunotherapy. Hum Vaccin Immunother.
16:2333–2340. 2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Oh S, Lee JH, Kwack K and Choi SW: Natural
killer cell therapy: A new treatment paradigm for solid tumors.
Cancers (Basel). 11(1534)2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Derebery MJ and Berliner KI: Allergy and
its relation to Meniere's disease. Otolaryngol Clin North Am.
43:1047–1058. 2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Di Berardino F and Zanetti D: Delayed
immunomodulatory effect of cow milk-free diet in Meniere's Disease.
J Am Coll Nutr. 37:149–153. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Kim J and Chan JJ: Cyclophosphamide in
dermatology. Australas J Dermatol. 58:5–17. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Berd D, Mastrangelo MJ, Engstrom PF, Paul
A and Maguire H: Augmentation of the human immune response by
cyclophosphamide. Cancer Res. 42:4862–4866. 1982.PubMed/NCBI
|
|
22
|
Emadi A, Jones RJ and Brodsky RA:
Cyclophosphamide and cancer: Golden anniversary. Nat Rev Clin
Oncol. 6:638–647. 2009.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Tsuchida Y, Harada M, Shoda H, Goto A,
Suzuki N, Murashima A, Osuga Y and Fujio K: Fertility preservation
in patients receiving gonadotoxic therapies for systemic autoimmune
diseases in Japan. Mod Rheumatol: Jan 18, 2021 (Epub ahead of
print). doi: 10.1080/14397595.2020.1856020.
|
|
24
|
Editorial Board of Chinese Journal of
Otorhinolaryngology Head and Neck Surgery and Society of
Otorhinolaryngology Head and Neck Surgery Chinese Medical
Association. Guideline of diagnosis and treatment of Meniere
disease (2017). Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi.
52:167–172. 2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
25
|
Kim DY, Kwon J, Kim JY, Cha HS, Kim YW,
Kim IY and Im CH: New method for pure-tone audiometry using
electrooculogram: A proof-of-concept study. Sensors (Basel).
18(3651)2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Nakashima T, Naganawa S, Pyykko I, Gibson
WP, Sone M, Nakata S and Teranishi M: Grading of endolymphatic
hydrops using magnetic resonance imaging. Acta Otolaryngol Suppl.
560:5–8. 2009.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Welgampola MS and Colebatch JG:
Characteristics and clinical applications of vestibular-evoked
myogenic potentials. Neurology. 64:1682–1688. 2005.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Lu L, Tan CQ, Cui YG, Ding GP, Ju XB, Li
YJ and Cai WJ: Analysis of the main components of inner ear
antigens inducing autoimmune Meniere's disease in guinea pigs.
Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 43:596–600.
2008.PubMed/NCBI(In Chinese).
|
|
29
|
Perry M: Revised australian code of
practice for the care and use of animals for scientific purposes.
Aust Vet J. 76(286)1998.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Kraaij T, Nilsson SC, van Kooten C, Okroj
M, Blom AM and Teng YO: Measuring plasma C4D to monitor immune
complexes in lupus nephritis. Lupus Sci Med.
6(e000326)2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Gupta S, Lau K, Harding CO, Shepherd G,
Boyer R, Atkinson JP, Knight V, Olbertz J, Larimore K, Gu Z, et al:
Association of immune response with efficacy and safety outcomes in
adults with phenylketonuria administered pegvaliase in phase 3
clinical trials. EBioMedicine. 37:366–373. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Wright T: Meniere's disease. BMJ Clin
Evid. 2015(0505)2015.PubMed/NCBI
|
|
33
|
Young YH, Wu CC and Wu CH: Augmentation of
vestibular evoked myogenic potentials: An indication for distended
saccular hydrops. Laryngoscope. 112:509–512. 2002.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Mao Z, Liu L, Peng L, Zhou L and Liu A:
Electrocochleography in the diagnosis of Meniere's disease. Lin
Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 28:964–967.
2014.PubMed/NCBI(In Chinese).
|
|
35
|
Hornibrook J: Tone burst
electrocochleography for the diagnosis of clinically certain
Meniere's disease. Front Neurosci. 11(301)2017.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Helling K, Schonfeld U and Clarke AH:
Treatment of Meniere's disease by low-dosage intratympanic
gentamicin application: Effect on otolith function. Laryngoscope.
117:2244–2250. 2007.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Gurkov R, Flatz W, Louza J, Strupp M,
Ertl-Wagner B and Krause E: In vivo visualized endolymphatic
hydrops and inner ear functions in patients with
electrocochleographically confirmed Meniere's disease. Otol
Neurotol. 33:1040–1045. 2012.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Tamai S: Physiological and pathological
aspects of circulating immune complex. Nihon Rinsho. 68 (Suppl
6):S105–S109. 2010.PubMed/NCBI(In Japanese).
|
|
39
|
Salvidio G and Andres G: Immune deposits
and immune complex disease. Clin Exp Rheumatol. 4:281–288.
1986.PubMed/NCBI
|
|
40
|
Savastano M, Giacomelli L and Marioni G:
Non-specific immunological determinations in Meniere's disease: Any
role in clinical practice? Eur Arch Otorhinolaryngol. 264:15–19.
2007.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Matsuoka H, Kwon SS, Yazawa Y, Barbieri M
and Yoo TJ: Induction of endolymphatic hydrops by directly infused
monoclonal antibody against type II collagen CB11 peptide. Ann Otol
Rhinol Laryngol. 111:587–592. 2002.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Ihler F, Bertlich M, Sharaf K, Strieth S,
Strupp M and Canis M: Betahistine exerts a dose-dependent effect on
cochlear stria vascularis blood flow in guinea pigs in vivo. PLoS
One. 7(e39086)2012.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Bodmer D, Morong S, Stewart C, Alexander
A, Chen JM and Nedzelski JM: Long-term vertigo control in patients
after intratympanic gentamicin instillation for Meniere's disease.
Otol Neurotol. 28:1140–1144. 2007.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Ren H, Yin T, Lu Y, Kong W and Ren J:
Intratympanic dexamethasone injections for refractory Meniere' s
disease. Int J Clin Exp Med. 8:6016–6023. 2015.PubMed/NCBI
|
|
45
|
Martin-Sanz E, Esteban-Sanchez J,
Rodriganez-Riesco L and Sanz-Fernandez R: Transitory effect on
endolymphatic hydrops of the intratympanic steroids for Meniere's
disease. Laryngoscope. 125:1183–1188. 2015.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Peneda JF, Lima NB, Monteiro F, Silva JV,
Gama R and Conde A: Immune-mediated inner ear disease: Diagnostic
and therapeutic approaches. Acta Otorrinolaringol Esp. 70:97–104.
2019.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Guo SY, Zhang Y and Liu B: Recent
immunology research of Meniere's disease. Zhonghua Er Bi Yan Hou
Tou Jing Wai Ke Za Zhi. 53:953–956. 2018.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
48
|
Ciorba A, Corazzi V, Bianchini C, Aimoni
C, Pelucchi S, Skarżyński PH and Hatzopoulos S: Autoimmune inner
ear disease (AIED): A diagnostic challenge. Int J Immunopathol
Pharmacol. 32(2058738418808680)2018.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Kilpatrick JK, Sismanis A, Spencer RF and
Wise CM: Low-dose oral methotrexate management of patients with
bilateral Meniere's disease. Ear Nose Throat J. 79:82–83, 86-88,
91-92. 2000.PubMed/NCBI
|