Introduction
Ankylosing spondylitis (AS) is an unexplained
systemic disease characterized by the chronic inflammatory response
of the central axis (1,2). The typical age of disease onset is
16-40 years old and the condition is more common in men (3). The main clinical manifestations of AS
are low back stiffness or pain and spinal lesions, which become
progressively aggravated (4), and
spinal rigidity, deformity and dysfunction that occurs in the
advanced stages of the disease and seriously affects the quality of
life of patients. Patients with advanced AS are unable to walk
upright, lie flat or look straight ahead and the condition may
additionally affect the heart, lung and digestive function
(5). Patients with AS often suffer
from mental illness due to bad physical symptoms. Spinal orthopedic
surgery is required to correct the long-term torso flexion
deformity of patients. Following orthopedic surgery, the abdominal
skin is severely stretched, often causing abdominal skin pain and
tension blisters and resulting in increased patient suffering
(6-9).
Though surgeons pay attention to whether the patient has
neurological symptoms associated with the lower limbs and whether
the patient's orthosis is satisfactory, there is often less concern
over the effects seen in the skin. Abdominal skin problems often
seriously affect the quality of life of patients during the
perioperative period. To the best of our knowledge, there are no
reported solutions related to this issue. To solve this problem,
the present study adopted new nursing measures for AS patients
undergoing orthopedic surgery in our department and a randomized
control study in comparison with traditional nursing measures was
conducted.
Materials and methods
Research objective
The present study was approved by the Ethics
Committee of the General Hospital, of the People's Liberation Army.
A total of 90 patients with AS who had kyphosis following posterior
vertebral kyphosis between January 2012 and December 2014 were
selected. Patients provided their written informed consent for
participation in the study and the use of their clinical data.
Patients were assessed based on the Assessment of SpondyloArthritis
International Society (ASAS) classification criteria (10). This study was a prospective study
and sample collection was continuous. Patients were randomized into
one of two groups, the experimental group or the control group. The
preoperative heart and lung functions of all patients were assessed
using the MAX-ii cardiopulmonary function evaluation system, where
they were deemed within the normal range, and postoperative
patients were awake and displayed normal vital signs (data not
shown). All anesthesia was performed by single-lumen endotracheal
intubation with Remifentanil. All patients were treated with an
analgesic pump of the same adjusted dose and time (Remifentanil, 1
µg/kg).
Inclusion criteria
In accordance with the assessment of
SpondyloArthritis international Society (ASAS) classification
criteria revised in the 1984 New York Conference (11) patients displayed symptoms of
cervical or cervicothoracic kyphosis; preoperative thoracic or
thoracolumbar kyphosis and posterior spinal pedicle osteotomy
orthopaedics (12).
Exclusion criteria
Patients with advanced AS have lower limb paralysis,
heart, brain and kidney and severe hematopoietic system; high
fever, tuberculosis, skin ulceration, and infectious diseases
(13). Patients who did not follow
the protocols were also excluded.
Preoperative care Skin care
Skin care was performed seven days before operation,
lasting for seven days. Patients in the control group were given
routine preoperative guidance as follows. The abdominal skin folds
were cleaned and kept dry daily and the patient was bathed in soapy
water one night before surgery. After the patients in the
experimental group were admitted to the hospital, the abdominal
skin was cleaned daily, and vaseline cream (Guangzhou Xindi
Chemical Co., Ltd.; 2 g/cm2) was evenly applied to the
abdominal skin every 3 h for 3-5 min.
Abdominal skin stretching
exercises
Abdominal skin stretching exercises were performed
seven days before the operation, lasting for seven days. The
patients in the experimental group performed daily abdominal skin
stretching exercises. They were instructed to face the wall with
both hands touching the wall and reach upwards, three times per day
for 15-20 min each time, every 10 times for a group, complete 10
groups daily. Flexion and extension of the hip joint were in the
maximum range of activity.
Psychological care
Both groups of patients were counseled
preoperatively, following a course of kyphosis for one month.
Corrective spinal surgery carries high risks, such as paralysis and
hemorrhagic shock (14). Thus, the
patients may be burdened with high psychological stress. Counseling
included discussion of post-operative abdominal skin tension pain
and possible tension blisters and worries about the surgery-related
complications.
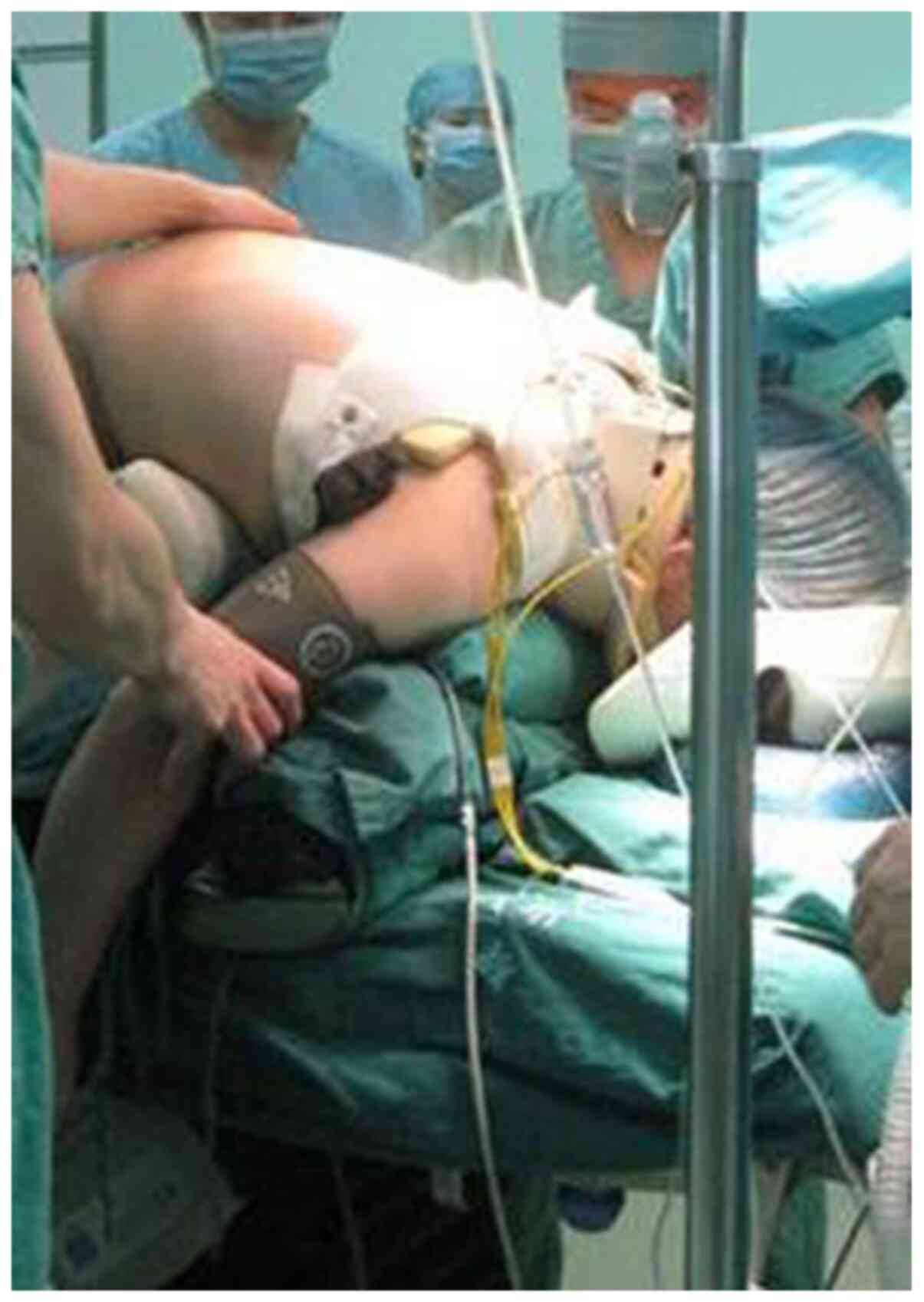
Intraoperative care
All patients with ankylosing spondylitis were placed
in the same position during surgery, as previously described
(12).
Postoperative care Skin care
The abdominal skin was kept dry in the control
group. Vaseline was smeared on the abdominal skin every 6 h for 3-5
min in the experimental group (Guangzhou Xindi Chemical Co., Ltd.;
concentration of Vaseline cream was 2 g/cm2).
Postoperative position
In the control group, the patients were placed in a
supine position. For patients with cervical or hip ankylosis, a
soft pillow was placed under the occipital and knee joints and
dressing protection was applied to the appendix. In the
experimental group, the left or right lateral decubitus position
was alternated within 24 h after patients returned from the
operating theater to the ward. Cushions were used between the
knees, and under bilateral ankles to avoid decubitus ulcer.
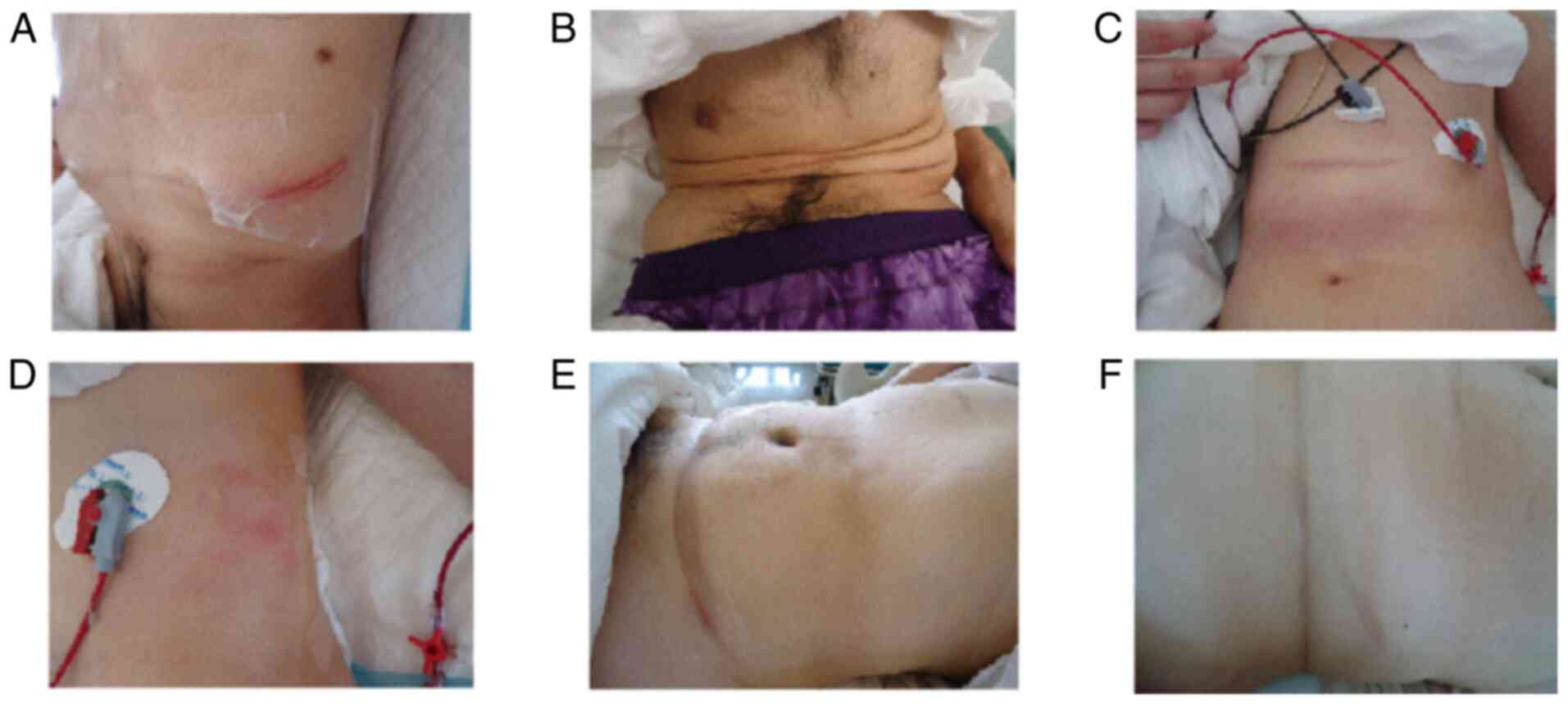
Tension blister care
In both the control and experimental groups, once
tension blisters appeared, they were carefully protected using the
3M transparent film. After 1-2 days, the swelling of the affected
limb may have been reduced and the blisters may have formed a scar.
If the blisters were large (over 2 cm in diameter) (15), after disinfection with aneriodine, a
sterile syringe was used in the lower part of the blister to draw
out the liquid and the blister wall gently pressed and draped on
the skin to prevent further damage. A 3M transparent film
protection was used until the blisters had completely disappeared
(Fig. 1).
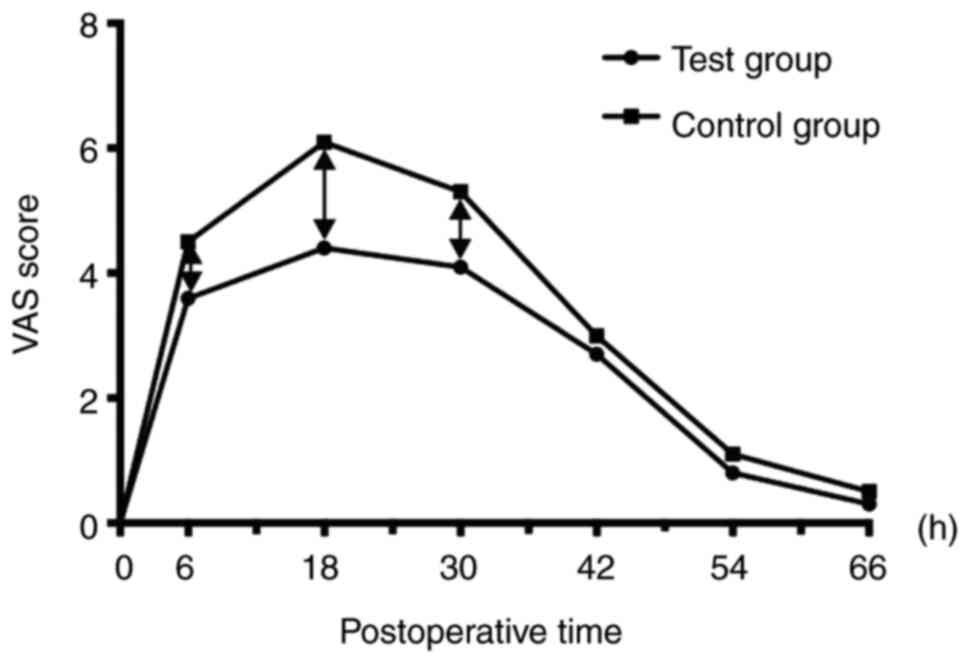
Visual analogue score (VAS)
At 1 day before surgery and 6 day after surgery, the
occurrence of tension vesicles was observed and recorded every 12
h, and the maximum diameter of the vesicles was graded. The VAS of
the abdominal skin pain was recorded. The method involves a rating
on a 10 point scale with 0 being no pain and 10 being unbearable
severe pain (16). The scoring
criteria were as follows: 0, no pain; 0<-3, slight pain that
could be endured; 4-6, the patient's pain affected sleep quality
but was tolerable; 7-10, the patient had progressively strong pain
up to a level that was unbearable, affecting appetite and sleep.
Each measurement was assessed by two experienced nurses to avoid
subjective errors.
Statistical methods
All analyses were performed using SPSS computer
software (version 13; SPSS, Inc.). An independent sample t-test was
used for the two groups of measurement data. The chi-square test
was used to compare the count data. The occurrence of tension
blisters was compared by the one-way sequence Wilcoxon rank sum
test. P<0.05 was considered to be statistically significant.
Results
Comparison of demographics between the
two groups of patients
A randomized digital table method was used to divide
the selected patients into two groups. There were 45 patients in
the experimental group, 37 males and 8 females, with a mean age of
(40.3±9.3) years (25-67 years). There were a further 45 patients in
the control group, 40 males and 5 females, with a mean age of
(38.9±9.4) years (23-70 years). There was no significant difference
in the age at surgery, sex, duration of disease, body weight or
anterior and posterior convex angle between the experimental group
and the control group (P>0.05; Table
I and Fig. 2). The average
range of spinal deformity in the experimental group before surgery
was 58.4±16.1˚, and postoperatively was -2.8±15.0˚. The average
range of spinal deformity in the control group before surgery was
56.7±18.3˚, and postoperatively was -8.3±16.6˚.
 | Table IComparison of general conditions
between the two groups of patients. |
Table I
Comparison of general conditions
between the two groups of patients.
| Variable | Test group
(n=45) | Control group
(n=45) | χ2/t | P-value |
|---|
| Age (years) | 40.3±9.3 | 38.9±9.4 | 0.710 | 0.479 |
| Sex (male) | 37 | 40 | 0.809a | 0.368 |
| Front and rear lobe
(˚) | 73.7±17.8 | 76.5±21.1 | 0.680 | 0.498 |
| Weight (kg) | 62.4±13.1 | 58.9±10.2 | 1.414 | 0.161 |
| Course of the disease
(years) | 14.2±7.6 | 11.0±8.2 | 1.920 | 0.058 |
Comparison of abdominal pain scores
between the groups
At 6, 18 and 30 h after surgery, the abdominal pain
scores of the experimental group were significantly lower than
those of the control group (P<0.05). There was no significant
difference in pain levels between the two groups after 42 h
(P>0.05), and the pain returned to the preoperative level at 66
h after surgery (Fig. 3).
Comparison of abdominal tension
vesicles in two groups
All vesicles from all patients were detected.
Tension vesicles in the abdominal skin of the experimental group
were significantly smaller in the treatment group than in the
control group, and the difference was statistically significant
(u=2.238>1.96, P<0.05; Table
II).
 | Table IIComparison of tension blister
size. |
Table II
Comparison of tension blister
size.
| Size | Total number of
blisters; Test group (n=45) | Total number of
blisters; Control group (n=45) | P-value |
|---|
| 0-0.50 cm | 22 | 15 | <0.05 |
| 0.51-1.00 cm | 12 | 10 | <0.05 |
| 1.01-1.50 cm | 8 | 7 | <0.05 |
| 1.51-2.00 cm | 2 | 8 | <0.05 |
| >2.00 cm | 1 | 5 | <0.05 |
Discussion
The development of tension blisters is often caused
by excessive swelling of the skin, excessive pressure and blood
circulation disorders. When venous return is blocked, local venous
congestion and increased permeability of the blood vessels cause
small blisters to form in the epidermis (17,18).
Patients with AS have long-term contracture deformity of the trunk
before surgery (19,20). Relaxation of the skin on the
abdominal wall is far worse than that of normal people. After
orthopedic surgery, the skin of the abdomen will be distended,
causing high tension of the skin and subcutaneous blood circulation
dysfunction, pain and tendency to develop tension blisters
(21,22). Unnecessary trouble and pain impact
postoperative prognosis and psychology (23). Therefore, reducing the occurrence of
tension blisters is of great significance for clinical nursing
work.
Patients undergoing general anesthesia for spinal
surgery are usually placed in a conventional position in which the
pillow is placed flat and the head is biased to one side, or the
lower neck and the lower occipital pillow are raised to a head
position of 10-15˚. Due to the unstable vital signs of early
patients, the bed was raised to a high angle to prevent hemodynamic
changes and fluctuations in cardiopulmonary function. The modified
semi-recumbent position can only raise the head by 10-15˚. The
purpose of the supine position is to prevent aspiration pneumonia
caused by vomiting when the patient is not awake (24). The main advantage of the improved
semi-recumbent position is that the patient's comfort can be
improved to some extent. However, patients with AS kyphosis are
different from patients with general scoliosis or other spinal
diseases in a number of ways (25):
i) Patients with AS have different degrees of inflammation or
ankylosing damage in the cervical spine before surgery, several
patients have cervical vertebrae or even full rigidity, and when
they are supine, they cannot move to lie on their side; ii) as
patients with AS kyphosis have difficulties entering the supine
position before surgery, they are used to alternating between the
left and right lateral positions in bed. If the patient is supine
after surgery, psychological and physical discomfort will occur;
iii) even after kyphotic orthopedic surgery, the sagittal balance
of patients with AS kyphosis does not necessarily reach the normal
spine-pelvic parameter standard and a kyphosis angle greater than
the normal value remains. The comfort level of the supine position
is significantly lower than that of the lateral position; iv) some
patients have hip flexion deformity before the operation. In the
supine position after spinal orthopedic surgery, the bilateral hip
and knee joints should be flexed. Even if the knee joint is placed
under the cushion, the lower limb muscle tone and hip pain of the
patient can be increased compared with the lateral position.
Postoperative exercise can maintain the normal range
of motion of the thorax and the normal shape and flexibility of the
spine. In addition, postoperative exercise can maintain the motor
function of limbs, prevent or reduce limb muscle atrophy, increase
bone mineral density and prevent osteoporosis.
AS patients usually experience a reduction in pain
at the incision within 7 days after surgery (26). The results of the present study
confirmed that the abdominal wall tension pain and back incision
pain were significantly lower in the treatment group than in the
control group. One possible for reason for this may be the lateral
position of the patient in the treatment group. The patient flexes
the lower limbs when lying in a lateral position, which reduces the
sharp increase of the abdominal wall tension caused by the
kyphosis. Additionally, a lateral position reduces the pressure on
the back incision. An increase in abdominal wall tension is related
to the formation of tension vesicles in the abdominal wall of the
patient, therefore a sharp increase in the abdominal wall tension
caused by kyphosis may also reduce the formation of tension
vesicles. Patients with AS have long-term contracture deformity of
the trunk before surgery. The relaxation of the skin on the
abdominal wall is worse than that of normal people. After
orthopedic surgery, the skin of the abdomen will be pulled tight,
causing a high degree of tension in the skin, which increases pain
and causes the development of tension blisters. Flexing the torso
and the hips and knees through the lateral position can reduce the
tension of the skin to a certain extent, thereby reducing pain and
reducing the occurrence of tension blisters. In the lateral
position, reasonable care measures were taken, and there was no
significant difference in the incidence of stage I pressure ulcers
between the two groups. In addition, there was no significant
effect on the pain of the patient's back incision. Overall, the
lateral position reduced abdominal discomfort without increasing
the patient's anesthesia complications and the patient's back
incision pain. AS patients undergoing orthopedic surgery in a
lateral position had the following advantages: i) The patients bed
habits could be monitored to improve their comfort before the start
of the operation; ii) a reduction in abdominal wall tension reduced
abdominal wall pain and abdominal wall tension blisters occurrence;
iii) reduced pressure on the back incision reduced the pain of the
incision and iv) the occurrence of vomiting and aspiration in
patients was avoided. The present study showed that patients with
AS kyphosis with the experimental treatment did not experience
increased respiratory rate changes and a low incidence of
postoperative adverse events such as vomiting, dizziness and stage
I pressure sores after orthopedic surgery. On the contrary, the
experimental treatment also relieved the patient's abdominal wall
pain and back incision pain and reduced the patient's heart rate
and the incidence of abdominal wall tension blisters, which is
conducive to increasing patient comfort, reducing patient suffering
and promoting body recovery.
Vaseline is an oily substance that forms a
protective film on the skin to prevent evaporation of water,
softening of the skin (27).
Vaseline also reduces friction and shear on the skin (28). Preoperative abdominal skin
stretching training also plays a role in relaxing the skin to a
certain extent (29-31).
In addition, the left and right lateral decubitus position of the
postoperative patient put the torso, hips and knees in a slightly
flexed position, which can reduce the tension of the skin to a
certain extent, thereby reducing pain and reducing the occurrence
of tension blisters (32).
The results of the present study suggested that
patients with AS kyphosis experienced reduced pain and tension of
the abdominal skin after surgery by combined use of Vaseline cream
smear, preoperative abdominal skin stretching training and
postoperative alternative lateral decubitus positions change in
comparison with patients that received standard treatment. Also,
the occurrence of was blisters reduced. Optimal nursing is the key
to ease the pain and tension vacuole in abdominal skin.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XS and BW were responsible for conception and
design. ZW, LG and YC carried out analysis and interpretation of
data. KS, YL, CZ and CX were responsible for acquisition of data.
All authors have read and approved this final version of this
article for publication. The authenticity of all the raw data have
been assessed by XS and ZW.
Ethics approval and consent to
participate
Patients provided their written informed consent for
participation in the study and the study received ethical approval
from the Ethics Committee of the General Hospital of the People's
Liberation Army.
Patient consent for publication
The patents provided their written informed consent
for the publication of their data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Thakkar SJ, Grayburn PA, Hall SA and
Roberts WC: Orthotopic heart transplantation for ankylosing
spondylitis masquerading as nonischemic cardiomyopathy. Am J
Cardiol. 123:1732–1735. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Nunes GPS, Cunha PDS, Bosco DPD and
Ribeiro SLE: Challenging management of hepatitis B infection in
ankylosing spondylitis patients in an endemic area during
immunosuppressive therapy. Rev Soc Bras Med Trop.
52(e20180386)2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Moura CS, Rahme E, Maksymowych WP,
Abrahamowicz M, Bessette L and Bernatsky S: Use of
disease-modifying anti-rheumatic or anti-tumour necrosis factor
drugs and risk of hospitalized infection in ankylosing spondylitis.
Scand J Rheumatol. 48:121–127. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Qian Q, Xu X, He H, Ji H, Zhang H, Ding Y,
Dai SM, Zou Y, Zhu Q, Yang C, et al: Clinical patterns and
characteristics of ankylosing spondylitis in China. Clin Rheumatol.
36:1561–1568. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Golder V and Schachna L: Ankylosing
spondylitis: An update. Aust Fam Physician. 42:780–784.
2013.PubMed/NCBI
|
|
6
|
Dębska J, Kotulska-Józwiak K, Pawliszak P,
Bilska M, Chmielewski D, Puzio I and Jurkiewicz E: Spinal cord
lesions in children and adolescents with multiple
sclerosis-Magnetic resonance imaging. Neurol Neurochir Pol.
51:77–81. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Braun J and Sieper J: Ankylosing
spondylitis. Lancet. 369:1379–1390. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Cozowicz C, Olson A, Poeran J, Mörwald EE,
Zubizarreta N, Girardi FP, Hughes AP, Mazumdar M and Memtsoudis SG:
Opioid prescription levels and postoperative outcomes in orthopedic
surgery. Pain. 158:2422–2430. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Memtsoudis SG, Vougioukas VI, Stundner O
and Poultsides LA: Perioperative outcomes in orthopedic surgery.
ScientificWorldJournal. 2015(648284)2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Sieper J, Rudwaleit M, Baraliakos X,
Brandt J, Braun J, Burgos-Vargas R, Dougados M, Hermann KG, Landewé
R, Maksymowych W and van der Heijde D: The assessment of
SpondyloArthritis international society (ASAS) handbook: A guide to
assess spondyloarthritis. Ann Rheum Dis. 68 (Suppl 2):ii1–ii44.
2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lilje SC, Persson UB, Tangen ST, Kåsamoen
S and Skillgate E: Costs and utilities of manual therapy and
orthopedic standard care for low-prioritized orthopedic outpatients
of working age: A cost consequence analysis. Clin J Pain.
30:730–736. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Feng J, Zhou J, Huang M, Xia P and Liu W:
Clinical and radiological outcomes of the multilevel Ponte
osteotomy with posterior selective segmental pedicle screw
constructs to treat adolescent thoracic idiopathic scoliosis. J
Orthop Surg Res. 13(305)2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Dundar U, Solak O, Toktas H, Demirdal US,
Subasi V, Kavuncu V and Evcik D: Effect of aquatic exercise on
ankylosing spondylitis: A randomized controlled trial. Rheumatol
Int. 34:1505–1511. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Passias PG, Poorman GW, Jalai CM, Line B,
Diebo B, Park P, Hart R, Burton D, Schwab F, Lafage V, et al:
Outcomes of open staged corrective surgery in the setting of adult
spinal deformity. Spine J. 17:1091–1099. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Li D, Liu Y, Qi L, Gu J, Tang Q, Wang X
and Bhushan B: Properties of blisters formed on polymer films and
differentiating them from Nanobubbles/Nanodrops. Langmuir.
35:3005–3012. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Heller GZ, Manuguerra M and Chow R: How to
analyze the visual analogue scale: Myths, truths and clinical
relevance? Scand J Pain. 13:67–75. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Song K, Zheng G, Zhang Y, Zhang X, Mao K
and Wang Y: A new method for calculating the exact angle required
for spinal osteotomy. Spine (Phila Pa 1976). 38:E616–E620.
2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Malone PC and Agutter PS: To what extent
might deep venous thrombosis and chronic venous insufficiency share
a common etiology? Int Angiol. 28:254–268. 2009.PubMed/NCBI
|
|
19
|
Ciciarello F, Mandolesi S, Galeandro AI,
Marceca A, Rossi M, Fedele F, Gesualdo M, Cortese F, Zito A,
Federico F, et al: Age-related vascular differences among patients
suffering from multiple sclerosis. Curr Neurovasc Res. 11:23–30.
2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Dong FH: Precise application of
Traditional Chinese medicine in minimally-invasive techniques.
Zhongguo Gu Shang. 31:493–496. 2018.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
21
|
Deslauriers N, Jacques F, Danino A, Harris
P, Martin J, Liberman M, Duranceau A and Ferraro P: Lateral
mediastinal tracheostomy in benign disease: An uncommon procedure
for a rare indication. Ann Thorac Surg. 89:979–981. 2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Sakai T, Sawada M, Sato Y, Kimura F,
Yagihashi N, Iwabuchi T, Kimura D, Tsushima T and Hatanaka R:
Tension pneumothorax developing hemothorax after chest tube
drainage. Kyobu Geka. 69:991–994. 2016.PubMed/NCBI
|
|
23
|
Rutström E, Söndergaard S, Lundborg C and
Ene K: Postoperative pain experience, pain treatment and recovery
after lumbar fusion and fixation surgery. Int J Orthop Trauma Nurs.
34:3–8. 2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Hassan EA and Baraka AAE: The effect of
reverse Trendelenburg position versus semi-recumbent position on
respiratory parameters of obese critically ill patients: A
randomized controlled trial. J Clin Nurs: Jan 12, 2021 doi:
10.1111/jocn.15645 (Epub ahead of print).
|
|
25
|
Zhang H, Zhang X, Hu F, Hu W, Wang Y and
Hao Y: Ankylosing spondylitis kyphosis surgical correction
postoperative evaluation via SRS-22 domain investigation. J Orthop
Surg Res. 13(5)2018.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Weibel S, Jelting Y, Pace NL, Helf A,
Eberhart LH, Hahnenkamp K, Hollmann MW, Poepping DM, Schnabel A and
Kranke P: Continuous intravenous perioperative lidocaine infusion
for postoperative pain and recovery in adults. Cochrane Database
Syst Rev. 6(CD009642)2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Wu Y, Xu Y, Shi J and Zhu Y: Surgical
treatment of Rüedi-Allgöwer III type Pilon Fractures. Zhongguo Xiu
Fu Chong Jian Wai Ke Za Zhi. 28:828–831. 2014.PubMed/NCBI(In Chinese).
|
|
28
|
Wolf L, Eertmans F, Wolf D, Rossel B and
Adriaens E: Efficacy and safety of a mineral Oil-based head lice
shampoo: A randomized, controlled, investigator-blinded,
comparative study. PLoS One. 11(e0156853)2016.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Tlougan BE, Mancini AJ, Mandell JA, Cohen
DE and Sanchez MR: Skin conditions in figure skaters, ice-hockey
players and speed skaters: Part I-mechanical dermatoses. Sports
Med. 41:709–719. 2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Srinivas A, Kaman L, Raj P, Gautam V,
Dahiya D, Singh G, Singh R and Medhi B: Comparison of the efficacy
of chlorhexidine gluconate versus povidone iodine as preoperative
skin preparation for the prevention of surgical site infections in
clean-contaminated upper abdominal surgeries. Surg Today.
45:1378–1384. 2015.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Ingvaldsen CA, Tønseth KA, Pripp AH and
Tindholdt TT: Microcirculatory evaluation of the abdominal skin in
breast reconstruction with deep inferior epigastric artery
perforator flap. Plast Reconstr Surg Glob Open.
4(e616)2016.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Ikegami S, Kamimura M, Uchiyama S,
Nakamura Y, Mukaiyama K and Kato H: Clinical implications of hip
flexion in the measurement of spinal bone mineral density. J Clin
Densitom. 19:270–276. 2016.PubMed/NCBI View Article : Google Scholar
|