Introduction
Nasopharyngeal carcinoma (NPC) is a rare
Epstein-Barr virus (EBV)-associated malignant tumor with a specific
geographical distribution within endemic areas (Southern China,
Taiwan, the Philippines, Vietnam and Northern Africa), several
predisposing etiologic factors (such as smoking, salt-preserved
fish and other foods, and a low diet in fresh fruits and
vegetables) and a strong genetic susceptibility revealed by the
high frequency of NPC among Chinese migrant patients (10- to
30-fold higher than other populations) and among Chinese
individuals born in other countries (1,2).
Other risk factors that are already established for
type III NPC include the Cantonese ethnicity, male sex, EBV
infection, the presence of human leukocyte class I alleles (HLA-I,
more specifically HLA-A2-B46 and -B17, both present in the Chinese
and other Asian populations who are at high risk; HLA-B5, in
Caucasians: An ethnic background that suggests the risk of a
possible morphea development; HLA-A11, present in all ethnicities;
B13, present in the Chinese and Tunisian populations, and A2,
present in the non-Chinese populations) and a family history
(familial clustering) of NPC (1-5).
An important risk factor is currently being taken into
consideration, i.e., poor oral hygiene; patients with
infrequent/non-daily teeth brushing, multiple dental cavities and
possibly individuals living with the human immunodeficiency virus
(HIV) can have an increased risk of developing NPC (1,3-5).
A patient suffering from NPC can present with
several signs and symptoms, including palpable neck masses, nasal
obstruction with some discharge, epistaxis, headaches and various
non-specific findings. This malignancy has an unfortunate
prognosis, being identified late in its development, frequently
when it has already metastasized, in an advanced clinical stage
(over 70% of cases). Such rare malignant tumors (NPC,
spiradenocarcinoma, pulmonary neuroendocrine tumors) or even ones
that have high incidence rates (hepatocellular carcinoma) have
aggressive behavior that translates as rapid local invasion, high
rate of metastasis and recurrence and frequent recurrence. As in
many cases of aggressive malignant tumors, multimodal treatment
involving a multidisciplinary team seems to be an optimal approach,
involving a tandem of surgery, chemotherapy, radiotherapy, or
immunotherapy.
Nasopharyngeal examination consists initially of an
indirect nasopharyngoscopy procedure, with subsequent direct
nasopharyngoscopy with the help of a fiberoptic endoscope, and, if
a tumor mass is found, it is also biopsied. If a tumor mass is
suspected and a direct examination is not diagnostic, further
imaging studies are needed such as computer tomography (CT) scan
and/or magnetic resonance imaging (MRI) studies, a technique that
offers better contrast among structures and an improved multiplanar
capability, offering an improved view of the disease extension and
that of the tumor margins (1,3,6-8).
As far as treatment goes, NPC is a malignant tumor
that is highly sensitive to radiation therapy, even though it
registers high local recurrence and metastasis rates. Tumors that
are locally infiltrative (advanced) benefit from a combined therapy
of chemotherapy and radiotherapy, with improved survival rates and
disease-free intervals (1,2).
Case report
An 80-year-old hypertensive patient with right
auricular prosthesis and left ear cophosis, was admitted to the
otorhinolaryngology (ORL) clinic at the ‘Sfantul Apostol Andrei’
Emergency Clinical Hospital in Galati, in September 2019 suffering
from bloody otorrhea, deteriorating hypoacusis on the right side,
right hemicranias and also vertigo. The patient revealed a personal
history with a surgically treated gastric ulcer and a moderately
differentiated rectal adenocarcinoma diagnosed in 2013, which was
surgically removed, revealing invasion in the tunica muscularis
propria. Ethics approval was granted by the ‘Dunarea de Jos’
University's Ethics Committee with the decision number 331 from
15.04.2021. Written informed consent was provided by the
patient.
In September 2019, the initial clinical diagnosis
was haemorrhagic otitis media, for which the patient received a
treatment course with antibiotics, antialgics, sedatives,
anti-hypertensives (including β-blockers, which can have various
immunologic or non-immunologic side effects) (9) and specific local treatment with
aspiration, instillations and local hygienic measures. The patient
was advised to avoid aggressive endauricular maneuvers and to avoid
wearing the hearing prosthesis. The medical measures improved the
patient's overall state by stopping the hemorrhage, but they did
not relieve the hemicrania. The otomicroscopic examination revealed
a perforated tympanic membrane with granulations which were further
excised. The previous treatment was continued.
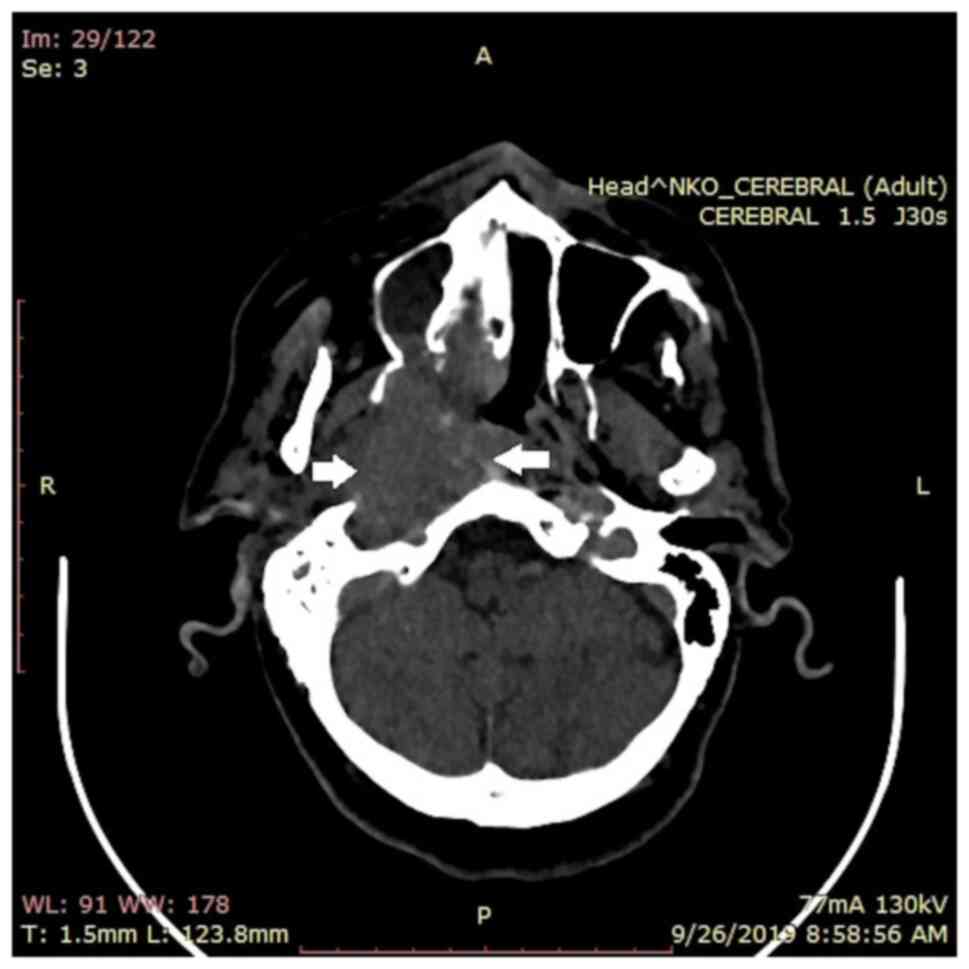
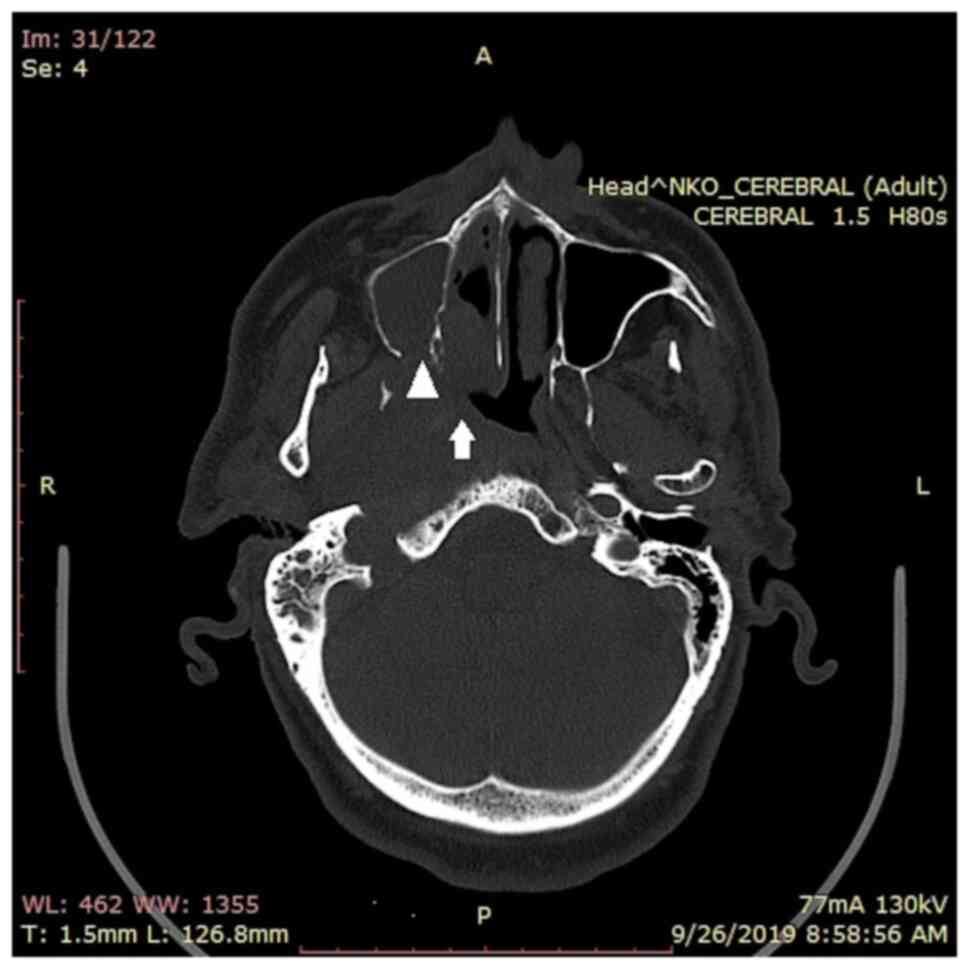
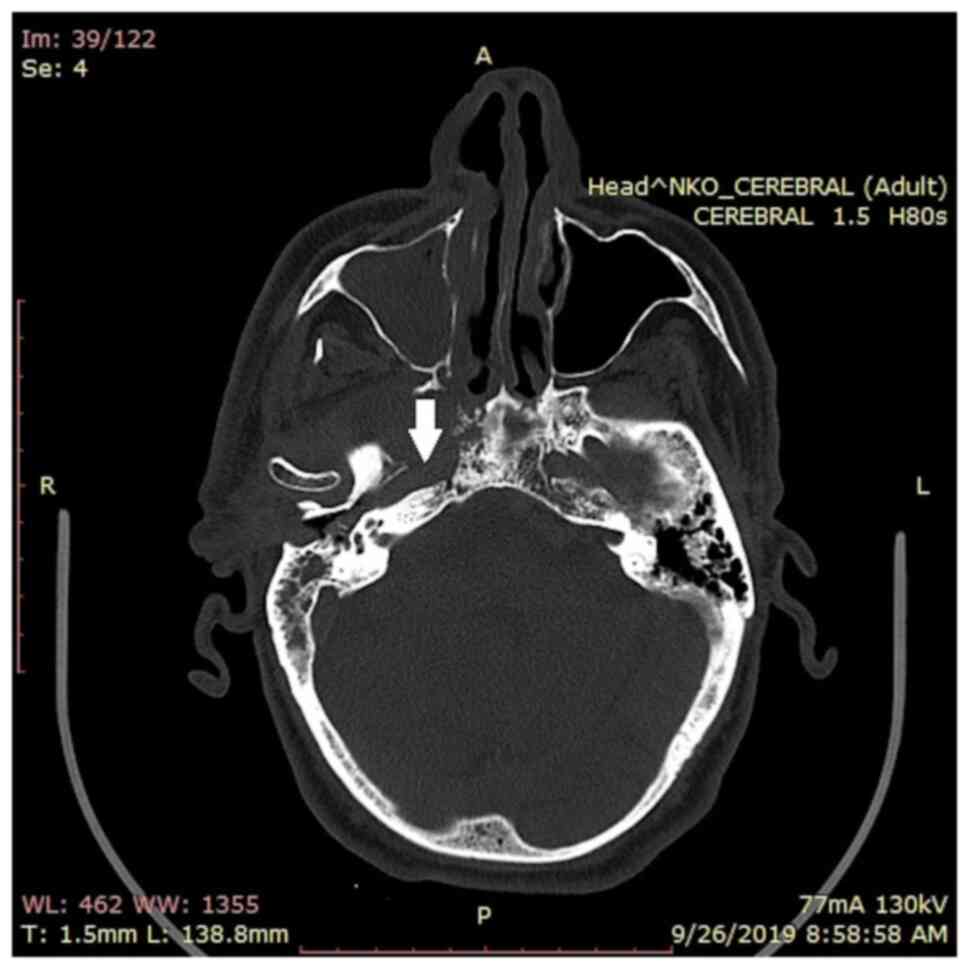
In September 2019, a CT scan was carried out
involving the middle ear, temporal bone and brain; it revealed the
presence of a 54/45 mm tumor mass located in the right
infratemporal fossa with extension in the rhinopharynx, the right
nasal fossa and maxillary sinus, and adjacent bone destruction and
inflammation, as shown in Fig. 1,
Fig. 2 and Fig. 3.
The vegetant, cauliflower-like tumor mass was
biopsied and the pathology report revealed it to be a poorly
differentiated squamous cell carcinoma (G3). As surgical treatment
was not an option, radiotherapy examination was carried out for
palliative care. The pathology report, associated with the clinical
and radiotherapy examination confirmed the diagnosis of a locally
invasive tumor mass, with distant metastases, and a poorly
differentiated squamous cell carcinoma with left cervical lymph
node metastasis, a clinical stage of IVB.
At the radiotherapist's request, an MRI examination
was performed, revealing a right cavum expansive tumor process with
skull base, maxilla-sphenoidal sinus, perineural, right carotid
wall and ipsilateral jugular vein wall involvement, and with a
right superior jugular lymph node metastasis. This led to a
thoracic CT examination which found no evidence of metastatic
involvement.
By taking into consideration the local and regional
extent of the tumor without proof of any distant metastatic
involvement, neoadjuvant chemotherapy treatment was recommended
with paclitaxel-carboplatin. In March 2020, after the last
evaluation due to a persistent thrombocytopenia, the patient could
not undergo radiotherapeutic treatment, and in February 2021 the
patient's overall state was stable.
Discussion
NPC is a distinct neoplasm among other types of head
and neck cancers. By gross examination this tumor can reveal many
different aspects: It can appear as a flat; smooth lesion of the
mucosa; as a small, elevated nodule with or without surface
ulceration; or even as a vegetant, cauliflower-like, frankly
infiltrative mass, or it can also not be visible at all (10).
Most NPC histopathology studies are based on the
primary tumor biopsy sample (although primary full-tumor excision
would be more beneficial in patient survival, as Koebner phenomena
manifested as in situ recurrence/field cancerization is
frequent in oral cancers) (11-13).
In many cases it is followed by cervical lymph node excision, which
is frequently positive for metastases, the tumor's aggressive
behavior being explained by apoptosis, proliferation and
neovascularization (three processes on which the tumor's growth and
metastatic capacity reside and which are promoted by interleukin-6
activity on the tumor and the immune system) (11,14,15).
By analyzing non-keratinizing carcinoma types, the more frequent
undifferentiated subtype has a tumor growth that is characterized
morphologically by a syncytial pattern of large malignant tumor
cells with inconspicuous margins and vesicular oval nuclei with
central, large nucleoli. These malignant cells are stacked together
and sometimes the nuclei seem to have larger quantities of
chromatin, with hyperchromasia, with less of a vesicular chromatin
pattern (10). Low power
non-keratinizing NPC biopsy examination reveals a proliferation of
large epithelioid cells that are separated by layers of small
lymphocytes and plasma cells, while a higher power view reveals the
epithelioid component's pleomorphic nuclei with open chromatin
pattern and conspicuous nucleoli. At this magnification the
lymphocytic and plasma cell component is also clearly visible, and
the malignant cells are positive for EBV ribonucleic acid (RNA) and
following immunohistochemistry examination they are positive for
CK5/6, with membrane staining having a brown pattern (16).
The keratinizing type of NPC has an obvious
microscopic squamous differentiation, with intercellular bridges
and keratin pearls (sometimes present as an extensive tumor
component). Frequently, an in situ component is also found.
This carcinoma has a development pattern characterized by tumor
islands within an abundant desmoplastic stroma with a variable
number of lymphocytes, plasma cells, neutrophils and eosinophils
(10). Eosinophils are mainly found
in the stroma in between the malignant islands, but can also be
seen among the tumor cells as part of the aforementioned islands
(17). This moderate inflammatory
reaction to the malignant component is mostly composed of
lymphocytes and polymorphonuclear leucocytes, with a reduced number
of plasma cells (11,17).
The epithelial component is comprised of
multi-layered polygonal malignant cells having distinct cell
borders and evident intercellular bridges. The cells that are found
in the center of the islands and those that are located more
superficially frequently have a larger quantity of glassy,
eosinophilic cytoplasm, sometimes with readily identifiable
cytoplasmic tonofibrils (a marker of single-cell keratinization)
(11).
Although it is considered a rare type of malignancy,
NPC is one of the most aggressive ones, having one of the highest
metastatic rates not only in the head and neck region, but also in
the distant locations. Cutaneous metastases, although rare, can be
found locally or regionally, including at the thorax level, making
it necessary to differentiate from other tumors (18,19).
This type of carcinoma is not only capable of cell migration,
invasion and metastasis, but its specific micro-environment may
also determine various changes in other tissues, increasing the
chance of a new cancer-type development (12,20).
In the medical practice, the development of two
different cancer types that are not linked in any way, has almost
never been documented, although each time this occurs, the possible
link needs to be investigated in depth.
NPC may influence the development of colorectal
cancer (or vice-versa), especially if the host is predisposed to
gene instability. These two types of malignant tumors have a series
of common genes that can influence their progression.
Serine protease inhibitor kazal-type 6
(SPINK-6) is the main gene involved in the proliferation and
metastasis development of NPC. SPINK-6 protein is part of the
serine protease inhibitor kazal-type family, inhibiting the
activity of the kallikrein (KLK) protease; it is a serine protease
inhibitor selective for KLK. In metastatic cells, overexpression of
SPINK-6, correlated with KLK protease inhibition was identified by
Zheng et al (20). On the
other hand, it has been proven that SPINK proteins are involved in
the upregulation of colorectal cancer, promoting its growth,
angiogenesis, migration and invasion (21,22).
Bcl-2 mutation is associated both with colorectal
cancer, and NPC (23,24). The mutant Bcl-2 gene is
responsible for defective apoptosis, leading to an increased
aggressive behavior of the tumor. Ismail et al (25) estimated that 30-94% of colorectal
cancer cases present abnormal Bcl-2 expression, inhibiting cell
apoptosis and promoting tumor cell development and progression. On
the other hand, the same mutation has been found in 90-100% of NPC
cases. Bcl-2 overexpression in this type of cancer is directly
correlated to its aggressive behavior (26).
It is less likely that concomitant Bcl-2 mutation
development in the two different types of cells (colorectal and
nasopharyngeal ones) are independent of each other. The Bcl-2
mutation in the colorectal tissue determines changes in the
microenvironment, which in turn can determine Bcl-2 mutation in the
nasopharyngeal tissue (or vice versa), especially in a patient
whose genes are unstable and predisposed to mutations.
This case's particularity stems from the development
of a metachronous tumor, i.e., a rectal adenocarcinoma and NPC, two
malignant tumors that have different prognosis and progression. A
noteworthy fact concerns paraneoplastic syndromes that may take
form in head and neck carcinomas, as in the case of squamous cell
carcinoma. The syndromes may be identified as a preceding,
concurrent or subsequent manifestation of malignancy, as a result
of tumor-producing protein hormones, enzymes or fetal proteins,
tumor-induced antibody production or cytokine production.
The paraneoplastic syndromes, which can be found in
squamous cell carcinoma of the head and neck region, can be
classified as follows: i) endocrine manifestations, ectopic
antidiuretic hormone secretion [leading to the syndrome of
inappropriate antidiuretic hormone secretion (SIADH)], humoral
hypercalcemia of malignancy (HHM) with hypercalcemia complications,
ectopic adrenocorticotropic hormone (ACTH), ginecomastia; ii)
neurological and muscular manifestations in the form of subacute
cerebellar degeneration developing as tumor-producing antineural
antibodies that determine neuronal death, Eaton-Lambart myasthenic
syndrome, paraneoplastic encephalomyelitis with anti-Hu antibodies,
and limbic encephalitis; iii) ophthalmic manifestations, i.e.,
photophobia due to auto-antibodies against retinal tissue with
apoptosis; iv) rheumatologic manifestations including
polyarthritis, polymyalgia rheumatica, and hypertrophic
osteoarthropathy; v) dermatological manifestations such as itching,
alopecia, herpes zoster, acanthosis nigricans, acrokeratosis
paraneoplastica (also known as Bazex syndrome), Sweet's syndrome
(also known as, acute febrile neutrophillic dermatosis), digital
necrosis, paraneoplastic pemphigus, and vitiligo (as part of the
Cowden syndrome, but mainly develops in regards to thyroid
carcinoma, in which case the patient needs to be further
investigated for other autoimmune-type diseases); vi) hematological
manifestations including non-bacterial thrombotic endocarditis with
venous thrombosis and arterial emboli, paraneoplastic
polyvasculitis, hypereosinophilia and itching accompanying
thrombocytosis, anemia, erythrocytosis, disseminated intravascular
coagulation (DIC), and leukemoid reactions (immature white blood
cells in the bloodstream) (27-31).
It is presumed that cavum tumor development is
linked to the vicious handling of the hearing aid, lack of local
hygiene or hearing aid hygiene, and to aggressive endauricular
maneuvers. Another hypothesis is based on the existence of
multiple, chronic exudative, relapsing otitis media that were
therapeutically neglected. The risk factors that are also present
in this patient are: Age, sex, decreased immunity, other
comorbidities and a highly probable positive EBV status. A possibly
important risk factor was antihypertensive drug use; including
hydrochlorothiazide, statins are incriminated in non-melanoma skin
cancer development (such as basal and squamous cell carcinoma, 2
types of cancer in the development of which another drug class is
used, e.g., tetracyclines) (32-34).
Thus, as stated previously, it is highly probable
that the two malignant tumors (developed in the same patient, at
different time intervals and with such different locations and
morphology) may have a linking genetic component. This atypical and
highly interesting case presented clinical and imaging
characteristics which uphold the idea that this very rare type of
tumor is difficult to diagnose in its early stages, a reason for
applying treatment frequently as palliative care. In such cases,
psychological support based on physician trust and open
communication is one of the ways of tilting the scale towards
recovery and long-term survival. In Romania, individual and
(support) group psychotherapy is still not given the proper place
it needs in patient management (35).
In summary, research is still open in what concerns
the role played by Bcl-2 and SPINK6 in tumor promotion, the
therapeutic management options and the ways in which they can be
identified as early stage, taking into consideration that most
patients suffering from this malignancy are mainly from the rural
environment, with little medical education, a high number of
comorbidities, and who frequently ignore the signs and symptoms and
their eventual treatment, steps which could be of vital importance
to their survival.
Acknowledgements
Not applicable.
Funding
The present study was supported by ‘Dunarea de Jos’ University
of Galati (internal grant no. RF3668/01.10.2021).
Availability of data and materials
The information generated and analyzed during the
current study is available from the corresponding author on
reasonable request.
Authors' contributions
DJ(S), ALT, ML, EN, CO, LR, AME, CB and LA have
contributed to the acquisition, analysis and interpretation of data
and they have supervised and substantially revised this work; they
have substantial contributions to the conception and design of the
work. All authors had equal participation, equal contributions and
the same rights to this article. All authors have read and agreed
to the published version of the manuscript. DJS and EN confirm the
authenticity of the raw data.
Ethics approval and consent to
participate
Ethics approval and consent to participate were
granted by the ‘Dunarea de Jos’ University's Ethics Committee with
the decision number 331 from 15.04.2021.
Patient consent for publication
Patient consent was granted and is part of the
patient's personal chart.
Competing interests
The authors declare to not have competing
interests.
References
|
1
|
Wu L, Li C and Pan L: Nasopharyngeal
carcinoma: A review of current updates. Exp Ther Med. 15:3687–3692.
2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Spano JP, Busson P, Atlan D, Bourhis J,
Pignon JP, Esteban C and Armand JP: Nasopharyngeal carcinomas: An
update. Eur J Cancer. 39:2121–2135. 2003.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Thompson LD: Update on nasopharyngeal
carcinoma. Head Neck Pathol. 1:81–86. 2007.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Tatu A, Radaschin D, Constantin V, Stana P
and Ardeleanu V: Laser therapy in superficial morphea
lesions-indications, limitations and therapeutic alternatives. J
Mind Med Sci. 7:46–51. 2020.
|
|
5
|
Draganescu M, Baroiu L, Iancu A, Dumitru
C, Radaschin D, Polea ED, Bobeica C, Tatu AL, Niculet E and Fekete
GL: Perspectives on skin disorder diagnosis among people living
with HIV in southeastern Romania. Exp Ther Med.
21(97)2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Rebegea LF, Firescu D, Dumitru M and
Patrascu A: Skin spiradenocarcinoma-case presentation. Rom J
Morphol Embryol. 57:327–330. 2016.PubMed/NCBI
|
|
7
|
Rebegea LF, Dumitru M, Serban C, Firescu
D, Ivan I, Craescu M and Romila A: Survival and toxicity after
treatment with sorafenib in unresectable hepatocellular carcinoma.
Acta Medica Mediterranea. 4:2113–2118. 2019.
|
|
8
|
Craescu M, Rebegea L, Ivan I, Dumitru M,
Serban C and Firescu D: Therapeutic challenges in a case of trachea
neuroendocrine tumor. Acta Medica Mediterranea,. 3(1493)2019.
|
|
9
|
Tatu AL, Elisei AM, Chioncel V, Miulescu M
and Nwabudike LC: Immunologic adverse reactions of β-blockers and
the skin (Review). Exp Ther Med. 18:955–959. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
EI-Naggar AK, Chan JKC, Grandis JR, Takata
T and Slootweg PJ (eds): World Health Organization Classification
of Head and Neck Tumours. IARC Press, Lyon, France, pp. 65-70,
2017.
|
|
11
|
Weiland LH: The histopathological spectrum
of nasopharyngeal carcinoma. IARC Sci Publ: 41-50, 1978.
|
|
12
|
Nwabudike LC and Tatu AL: Reply to
Gambichler T et al. Altered epigenetic pathways and cell
cycle dysregulation in healthy appearing skin of patients with
koebnerized squamous cell carcinomas following skin surgery. J Eur
Acad Dermatol Venereol. 33:e3–e4. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Nwabudike LC and Tatu AL: Reply to Happle
R et al. Koebner's sheep in Wolf's clothing: Does the
isotopic response exist as a distinct phenomenon? J Eur Acad
Dermatol Venereol. 32:e336–e337. 2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ardeleanu V, Georgescu C, Frîncu LD,
Frîncu LL and Vesa D: Angiogenesis as prospective molecular biology
technique for cancer study. Rom Biotechnol Lett. 19:9637–9648.
2014.
|
|
15
|
Niculet E, Chioncel V, Elisei AM, Miulescu
M, Buzia OD, Nwabudike LC, Craescu M, Draganescu M, Bujoreanu F,
Marinescu E, et al: Multifactorial expression of IL-6 with update
on COVID-19 and the therapeutic strategies of its blockade
(Review). Exp Ther Med. 21(263)2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Muzaffar R, Vacca F, Guo H, Mhapsekar R
and Osman M: Pediatric nasopharyngeal carcinoma as seen on 18F-FDG
PET/CT. Front Oncol. 9(110)2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Looi L: Tumor-associated tissue
eosinophilia in nasopharyngeal carcinoma. A pathologic study of 422
primary and 138 metastatic tumors. Cancer. 59:466–470.
1987.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tatu AL: Umbilicated blue black lesion on
the lateral thorax. J Cutan Med Surg. 21(252)2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Tatu AL: Black nodule on the forearm. J
Cutan Med Surg. 21(157)2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Zheng LS, Yang JP, Cao Y, Peng LX, Sun R,
Xie P, Wang MY, Meng DF, Luo DH, Zou X, et al: SPINK6 promotes
metastasis of nasopharyngeal carcinoma via binding and activation
of epithelial growth factor receptor. Cancer Res. 77:579–589.
2016.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Gouyer V, Fontaine D, Dumont P, de Wever
O, Fontayne-Devaud H, Leteurtre E, Truant S, Delacour D, Drobecq H,
Kerckaert JP, et al: Autocrine induction of invasion and metastasis
by tumor-associated trypsin inhibitor in human colon cancer cells.
Oncogene. 27:4024–4033. 2008.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Lu X, Lamontagne J, Lu F and Block TM:
Tumor-associated protein SPIK/TATI suppresses serine protease
dependent cell apoptosis. Apoptosis. 13:483–494. 2008.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Testa U, Pelosi E and Castelli G:
Colorectal Cancer: Genetic abnormalities, tumor progression, tumor
heterogeneity, clonal evolution and tumor-initiating cells. Med Sci
(Basel). 6(31)2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Dong SS, Wang N, Yang CP, Zhang GC, Liang
WH, Zhao J and Qi Y: Giant cell-rich solitary fibrous tumor in the
nasopharynx: Case report and literature review. Onco Targets Ther.
13:6819–6826. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Ismail NI, Othman I, Abas F, Lajis NH and
Naidu R: Mechanism of apoptosis induced by curcumin in colorectal
cancer. Int J Mol Sci. 20(2454)2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Geramizadeh B, Marzban M and Churg A: Role
of immunohistochemistry in the diagnosis of solitary fibrous tumor,
a review. Iran J Pathol. 11:195–203. 2016.PubMed/NCBI
|
|
27
|
Mathew DG, Rooban T, Janani V, Joshua E,
Rao U and Ranganathan K: Review of paraneoplastic syndromes
associated with oropharyngeal squamous cell carcinoma. J Oral
Maxillofac Pathol. 14:41–47. 2010.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Tatu AL and Nwabudike LC: The treatment
options of male genital lichen sclerosus et atrophicus short title
for a running head: Treatments of genital lichen sclerosus. In:
Proceedings of the 14th National Congress of Urogynecology and the
National Conference of the Romanian Association for the Study of
Pain, pp262-264, 2017.
|
|
29
|
Tatu AL and Ionescu MA: Multiple
autoimmune syndrome type III-thyroiditis, vitiligo and alopecia
areata. Acta Endocrinol (Buchar). 13:124–125. 2017.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Mihăilă B, Dinică RM, Tatu AL and Buzia
OD: New insights in vitiligo treatments using bioactive compounds
from Piper nigrum. Exp Ther Med. 17:1039–1044. 2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Alter M, Mengoni M and Gaffal E: Cutaneous
manifestations of internal malignancy. J Dtsch Dermatol Ges.
18:456–469. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Tatu AL, Ciobotaru OR, Miulescu M, Buzia
OD, Elisei AM, Mardare N, Diaconu C, Robu S and Nwabudike LC:
Hydrochlorothiazide: Chemical structure, therapeutic, phototoxic
and carcinogenetic effects in dermatology. Rev Chim. 69:2110–2124.
2018.
|
|
33
|
Nwabudike LC, Elisei A, Buzia OD, Miulescu
M and Tatu A: Statins. A review on structural perspectives, adverse
reactions and relations with non-melanoma skin cancer. Rev Chim.
69(2557)2018.
|
|
34
|
Nwabudike LC and Tatu AL: Response
to-Chronic exposure to tetracyclines and subsequent diagnosis for
non-melanoma skin cancer in a large Mid-Western US population. J
Eur Acad Dermatol Venereol. 32(e159)2018.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Rebegea L, Firescu D, Baciu G and Ciubara
A: Psycho-oncology support. Brain. 10:77–88. 2019.
|