Neuroendocrine neoplasms (NENs) are a heterogenous
group of rare malignancies that arise from neuroendocrine cells
distributed throughout the body and produce peptide hormones and/or
biogenic amines (1). NENs can be
dichotomised into ‘functional’ (F) and ‘non-functional’ (NF) tumors
(2). The F-NENs category
represents 33% of all NENs and is mainly characterized by
well-defined clinical symptoms that are caused by the over
secretion of their circulating products (2). Examples of F tumors include NENs in
the midgut (such as the small intestine), which are classically
associated with carcinoid syndrome (CS) due to the overproduction
of serotonin (3). Symptoms of CS
have been previously reported to be associated with the
overproduction of serotonin by F NENs. By contrast, NF NENs are
more common in terms of incidence and can cause mechanical
symptoms, including ischemia or obstruction, the complications of
which from local tumor growth can ultimately result in mortality
(2).
Due to the substantial heterogeneity in these NENs
both in terms of clinical aggressiveness and response to therapy,
management of patients with such diseases is a significant
challenge (4). In total, 60-80% of
NENs have already metastasized on diagnosis (5). Prognostic and predictive markers have
been intensively investigated to explore the optimal clinical
management strategy for this category of neoplasms (6). Investigation into prognostic markers
contribute valuable information in understanding the physiology of
NENs and their natural course. They reveal beneficial mechanistic
information underlying the aggressive properties of the disease and
the risk of recurrence or death. By contrast, predictive markers
can be used to estimate the benefit of a certain therapy compared
with their corresponding condition at baseline, which can assist in
implementing the optimal treatment strategy for the most favorable
outcome (7).
At present, the most important prognostic factor for
NENs is morphological differentiation characteristics, which can be
divided into the well- or poorly-differentiated categories,
corresponding to neuroendocrine tumors (NETs) or neuroendocrine
carcinomas (NECs) (8).
Furthermore, NENs display a varying degree of proliferation known
as grade (G), which is approximated using the Ki-67 proliferation
index and mitotic count (9).
Specifically, the latest 2019 World Health Organization (WHO)
classification of gastro-entero-pancreatic (GEP)-NENs distinguishes
three grades of NENs that are classified into the low (G1),
intermediate-(G2) and high-grade (G3) categories based on the
degree of differentiation, with the mention that poorly
differentiated NECs are considered definitively G3 (10,11).
Although the WHO classification of tumors is considered to be the
gold standard tumor classification, it differs depending on their
primary site in the body. For example, the 2015 WHO Classification
of Tumors of the Lung, Pleura, Thymus and Heart does not make use
of the Ki-67 proliferation index (11). However, the current consensus is to
improve the management of NENs by adopting an uniformized
nomenclature system towards different organs (12). It is hoped that this new
classification will serve as a novel grading tool that can be
introduced into common clinical practice to reveal essential
information regarding NENs (12).
In addition to adequate classification and grading,
tumor staging also carries prognostic significance (13). European Neuroendocrine Tumors
Society (ENETS) and tumor, nodes and metastases (TNM)
classification of the American Joint Committee on Cancer (AJCC) are
currently used staging systems that present the classification
criteria but are not identical and are site specific (14,15).
A number of studies have reported comparative data between the two
systems for the classification of pancreatic neuroendocrine tumors
(Pan-NETs), suggesting a similar prognosis being found by the two
systems in ENETS and TNM of the AJCC, both regarding progression
free-survival (PFS) and overall survival (OS) (16,17).
However, further studies are needed, as the ENETS staging system
appeared to be superior in stratifying prognosis for each stage of
pancreatic NENs according to a previous report (18).
However, in terms of the formulation of concrete
guidelines for the clinical management of these tumors, numerous
issues persist due to the lack of comprehensive databases and
registries (9). In addition, an
insufficient number of lesion types have been studied despite wide
variations in tumor heterogeneity (9). The 5-year survival rate ranges
between 15 and 95%, depending on the location of the tumor primary
site, the level of metastatic spread at diagnosis, the available
treatment options and the geographical site of care (19-21).
Several methods have been reported to predict OS and
PFS, including nomograms taking into account the number of liver
metastases, tumor size and the Ki-67 index (22), the blood neutrophil-lymphocyte
ratio, Ki-67 index and the lymph node ratio (23) or phosphorylated histone H3(24). However, further research is
required.
An important obstacle in clinical practice is the
scarcity of a set of sensitive and specific tumor biomarkers
(25). The ‘perfect’ biomarker
would ideally be characterized by high sensitivity in diagnosing
NENs, good prediction of disease evolution and response to therapy
(26). Currently available NETs
biomarkers belong to the mono-analyte class and vary in the rates
of sensitivity and specificity for indicating the biological
characteristics, such as primary tumor site, or functional or
non-functional type secretion. In addition, these mono-analyte
measurements are unable to define the state of disease progression
or efficacy of therapy (27),
which frequently do not correlated well with radiological
evaluation data (28). To overcome
these shortcomings, interest in the molecular profiling of NENs is
increasing. Recent studies have demonstrated the utility of
molecular imaging as a viable option for predicting the prognosis
of NENs (29,30). Since the density of somatostatin
receptors (SSTRs) can also be quantitively assessed using
immunohistochemistry (IHC) in the surgical specimens, this can be
used to predict treatment response (31-33).
Furthermore complementary imaging modalities or early radiological
biomarkers, such as the tumor grade rate (TGR), have been proposed
to contribute valuable prognostic information (34,35).
Molecular diagnostics have previously been performed
on biopsies of solid tumor tissues (13). As one branch of this technique,
‘liquid’ biopsy is a non-invasive strategy that can provide the
opportunity to investigate the molecular genomic mechanism of tumor
cells in circulating blood (the ‘tumor circulome’) to characterize
the circulating molecular profiles, which may be useful for
subsequent diagnosis and monitoring (36,37).
Emerging biochemical and therapeutic markers have become
increasingly popular since 2004 and their relevance are expected to
increase exponentially by 2050 (13,38,39).
Identifying novel parameters is important for optimally predicting
the prognosis and treatment response for each patient. Therefore,
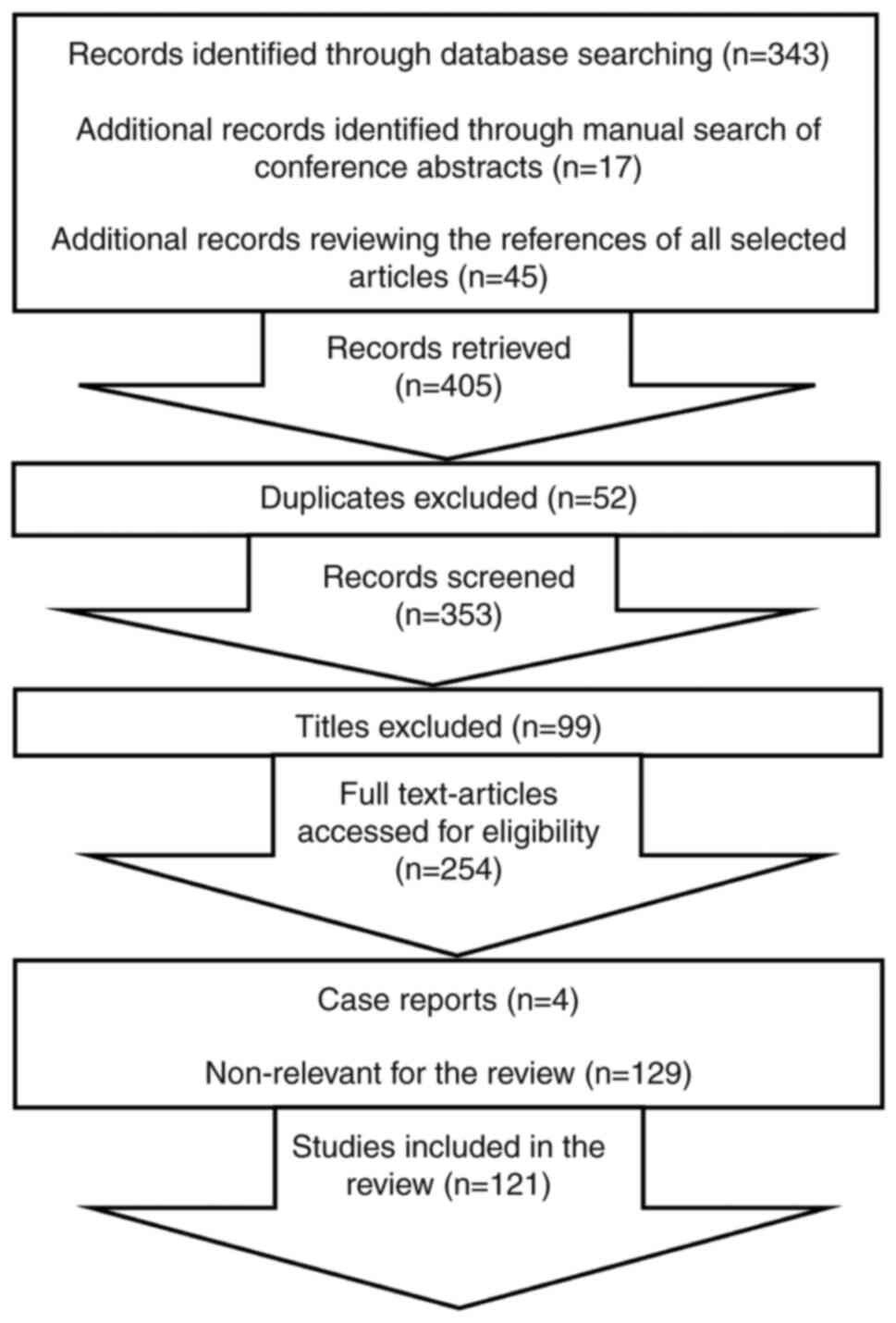
the present review summarizes some of the current and future
directions in this field of research with an emphasis on
GEP-NENs.
The aim of the present review is to summarize the
available data on the diagnostic, prognostic and predictive
biomarkers for NENs. The review is structured into the following
two parts: i) Discussion of the markers most commonly used in
clinical practice at present; and ii) potential future diagnostic,
prognostic and predictive biomarkers.
A number of biomarkers are currently applied for the
diagnosis of NENs. However, they are frequently not correlated with
diagnosis or clinical outcomes, mainly due to sensitivity and
specificity issues (Table I).
Human CgA is a glycoprotein that belongs to the
family of chromogranins and is localized in the secretory granules
alongside peptide hormones and catecholamines throughout the
neuroendocrine system (40).
Recognition of CgA as the default NET biomarker is widely applied
over the past decade due to its broad-spectrum nature, with high
levels being found in both F and NF NENs (41-43).
Yet, CgA detection and reliability are still based on different
non-standardized assays (44).
However, Cg A is highly expressed in NETs tissue, but can also be
measured in serum or plasma as a widely used circulating tumor
marker (40). High levels of CgA
are mainly observed in well-differentiated NETs and are associated
with larger tumor burden, especially in gut NETs (5,45).
By contrast, CgA suffers from low sensitivity for
poorly-differentiated tumors, where its production is less
pronounced (40,46).
As a result, enthusiasm for the application of CgA
as a marker is waning, which is compounded by the accumulating
evidence of its low utility (43,47).
The specific cut-off value (identified by the receiver operating
characteristic analysis between different assays) (44), primary location of the NEN
(48), endocrine-associated
syndrome (5), disease spread,
liver metastases (49),
false-positive elevations in CgA typically caused by proton pump
inhibitors, atrophic gastritis and kidney failure (13), can all influence the accuracy of
this test.
However, a recent systematic review and
meta-analysis evaluated the role of CgA in bronchopulmonary NENs
because of the scarcity of evidence in this field (43). This previous study reported the
clinical utility of CgA for the diagnosis of lung NENs, especially
in small cell lung cancer (SCLC) with a mean diagnostic specificity
of 79.5±3.1 and sensitivity of 59.9±6.8%. Still, this finding
require further validation (43).
5-HIAA is a metabolite of serotonin, which is
excessively produced by serotonin-secreting tumors and is excreted
in the urine (13). Prior to
interpretating the 5-HIAA test measurement in the urine as a
result, pharmacological and dietary artifacts must first be ruled
out, typically by avoiding the intake of tryptophan- and
serotonin-rich foods (50).
Measurement of urinary 5-HIAA excretion is more practical for
patients with primary midgut (jejunoileal, appendiceal and
ascending colon) NETs, which produces the highest levels of
serotonin (51). For carcinoid
syndrome (CS), this test has a reported sensitivity of >90% and
a specificity of 90% (52).
Additionally, a level of 5-HIAA >300 mmol/24 h and three
flushing episodes per day can be considered to be a predictive
factor of carcinoid heart disease (CHD) (53). There is also evidence that 5-HIAA
in combination with N-terminal probrain natriuretic peptide
(NT-proBNP) can be accurately used in screening for CHD (54). Nevertheless, its prognostic role
remains controversial.
NT-pro BNP is a peptide that is released by
myocardial cells as a result of an increase in heart volume and
pressure and is used especially for CHD prediction, which has been
previously correlated with patient survival (55,56).
A high sensitivity and specificity for CHD, 92 and 91%,
respectively, has been reported at the cut-off value of 260 pg/ml
(57). In addition, measurement of
the level of serum NT-proBNP has been recommended for intestinal
NENs and CS for the diagnosis and follow-up of CHD (54).
NSE is the main enolase-isoenzyme present in
neuronal and neuroendocrine tissues (58). Although mainly expressed
poorly-differentiated NET cells, measurement of serum NSE cannot be
used to distinguish among different subtypes of NENs (59). Consequently, although elevated
levels of NSE seems to have a degree of prognostic value for poor
outcome and correlate with tumor burden, NSE is now rarely used in
clinical practice since it is inferior to CgA in terms of the
information that can be extracted (59). However, NSE is currently applied as
the default tumor marker for SCLC diagnosis, prognosis and
follow-up, even though elevated levels of NSE can also be found in
non-small cell lung cancer (NSCLC) (58).
PP is serum marker produced by the neuroendocrine
cells of the colon and pancreas (60). PP is considered to be a
non-specific marker for NENs, where its levels has a modest degree
of accuracy as a diagnostic marker (13). However, it appears that an >50%
increase in the serum levels of PP in GEP-NETs patients has a
direct proportional relationship with the increase in tumor
according to RECIST 1.1 criteria on conventional imaging (CT scan ±
MRI scan) imaging (60).
CTGF is a modular secreted protein that serves an
important role in complex biological mechanisms, including
angiogenesis, tumorigenesis and wound healing (61). In addition, CTGF can regulate
various types of fibrosis formation, such as cardiac fibrosis
(62). Therefore, CTGF has a
reported sensitivity of 80% in detecting heart disease (62). For NETs, previous studies have
reported that CTGF expression measured in plasma is more likely to
be found in small-bowel ileal rather than in bronchial, pancreatic
or rectal NETs (63,64). However, a high level of CTGF was
found to be an independent predictive factor for right ventricular
dysfunction (61).
Mitotic count, Ki-67 index and necrosis are
typically used for the grading of NENs (9). While mitotic count is recommended to
be reported as mitoses per mm2 area, in clinical
practice this process could be affected by limited areas available
for counting. On the other hand, Ki 67 is determined using IHC
measured in the most mitotically active areas of the pathological
specimen, but due to the intratumoral heterogeneity this process
can be affected (9). However, this
manner of scoring can be time-consuming, which is compounded by the
lack of consensus in the optimal method for determining the
proliferative rate (9,65). In clinical practice, when there is
a discordance between these two types of measurements in assigning
the grade, higher ‘grade counts’ are normally negatively associated
with poorer prognosis (65-67).
For example, in ~33% of well-differentiated Pan-NETs, a G1 grade is
determined based on the mitotic count, whereas the G2 grade is
determined using the Ki-67 proliferation index (66). In addition, the same percentage
(33%) of G2 Pan-NETs are found for after mitotic count, but G3
according to the Ki-67 proliferation index (64). Therefore, the use of Ki-67 IHC
staining is essential for accurately grading well-differentiated
NETs (65,66)
In clinical practice, detection of multiple primary
tumors, multiple lymph node metastases and/or multiple distant
metastases are recommended for evaluating tissue blocks with the
biggest focus of tumor due to the intratumoral heterogeneity
(75). Furthermore, the Ki-67
index may present a variability during the course of the disease or
between primary tumor and metastasis (76). In a previous study, the Ki-67 index
was evaluated in 103 GEP-NETs, of which 24% presented with higher
grades in the metastasis, 10% with higher grades in the primary
tumor and 66% with same grade between the metastasis and the
primary tumor (77). The PFS and
OS were found to be identical for both G1 primaries and G2
metastasis categories, and also for G2 primaries and metastasis;
however, these are worse compared with the G1 primary tumors only
(G1 stable category). Therefore, any G2 tumors (in primary or in
metastases of NETs) influences patient survival.
The Ki-67 index also hold promising potential for
clinical application in NECs, since a Ki-67 index with a 55%
cut-off for response was found to be associated with poorer
prognosis, favorable response to platinum-based chemotherapy (CHT)
(78) and adverse reactions to
temozolomide CHT (79).
The current demand in this field is to improve the
methodology for the diagnosis, treatment and prognosis of NENs.
Therefore, novel markers have been evaluated over the past
decade.
Recent studies have benefited from advances in
sequencing technology for characterizing the complex molecular
landscape of NENs (80,81). Regarding PanNETs, the current trend
is mainly focused on determining the roles of multiple endocrine
neoplasia 1 (MEN1), death-domain associated protein
(DAXX), α-thalassemia and mental retardation syndrome
X-linked (ATRX) genes in the alternative lengthening of
telomeres (ALT) axis and components in the mTOR and DNA damage
pathways (82,83). In particular, molecular alterations
have been consistently associated with the following four events:
DNA damage repair; cell cycle regulation; PI3K/AKT/mTOR signaling;
and telomere maintenance (84).
Recent studies have revealed increasingly consistent
findings despite the lower mutation burden of PanNETs (82) as mutations in the MEN1,
ATRX and DAXX genes were frequently observed in this
type of tumors (85-87).
In total, up to 40% of well-differentiated NENs in the pancreas
exhibit somatic mutations in the DAXX and ATRX genes
(82). These two genes encode
proteins that interact and have multiple cellular functions,
including modulating telomeric chromatin. ATRX and
DAXX interact to deposit histone H3.3-containing nucleosomes
in the centromeric and telomeric regions of the genome and may
interact to suppress the ALT pathway under normal circumstances
(88,89). ATRX/DAXX mutations result in loss
of nuclear expression of their proteins, as detected by IHC, in
tumor tissue, which correlates with the suppression of ALT
(90). A negative expression of
ATRX/DAXX is typically associated with well-differentiated NENs,
and correlate with worse survival in Pan-NETs (90,91).
ALT is a telomerase-independent telomere maintenance mechanism that
has been previously studied using fluorescence in situ
hybridization (92). Altered
telomeres are a key process frequently found in PanNETs (93). As such, positive ALT status in
liver metastases of NENs was found to associate with worse survival
and increased risk of recurrence (94,95).
It has been previously shown that there is 100% concordance among
the ALT phenotype, ATRX/DAXX mutations and/or protein loss
(92), where the presence of
ALT-positive and ATRX/DAXX-negative (inactivation mutation)
in well-differentiated PanNETs is associated with a significantly
higher grade, size, grading, vascular/perineural invasion,
metastatic disease and with reduced relapse-free and tumor-specific
survival (96). Therefore, this
profile can be applied as a marker of more aggressive PanNET
phenotypes for patient stratification (97,98).
Application of fine-needle aspiration (FNA) makes it
possible to detect the loss of ATRX/DAXX and the presence of ALT as
a non-invasive method to sample tumors. As aforementioned, somatic
mutations of ATRX/DAXX genes can be detected using IHC to indicate
a loss of nuclear expression of their respective proteins (90). In addition, ALT can be assessed
using telomere-specific fluorescence in situ hybridization
(92). This procedure is becoming
increasing important in clinical practice, through which ALT or the
loss of ATRX or DAXX expression can be verified with
higher degrees of confidence during the prognostic process
(92).
Mutations in the tuberous sclerosis complex 2 (TSC2)
and PTEN genes are suppressors of the Akt/mTOR pathway, which are
present in up to 11% of sporadic PanNETs (100). Reduced expression of both
PTEN and TSC2 was found to be associated with more
aggressive phenotypes, presence of liver metastases and reduced
disease-free survival and OS in a cohort of 72 primary PanNETs
according to microarray analysis (99). However, further studies are
warranted before mutations of components in the PI3K pathway can be
considered as a biomarker of response.
The most recent 2019 WHO classification of GEP-NENs
made a clear distinction between NET G3 and NEC (10). NET G3 lacks consensus-based
recommendations is associated with longer OS (98). In certain cases, histology is not
sufficient for differentiating between highly proliferative NETs
and NECs (103), where it is
hoped that molecular profiling can amend this deficiency. Abnormal
immunolabeling of p53 and RB1 pathways are currently
being proposed for the distinction of well-differentiated NETs,
especially NETs G3 from poorly differentiated NECs during diagnosis
(103). Although p53 and RB1 are
considered to be two key drivers of NECs, but in NETs these
mutations are rarely observed (104-107).
Double inactivation of the TP53 and RB1 genes is one
of the genetic signatures of SCLC (108). The presence of these inactivated
mutations is used as a predictive marker of the response to
platinum-based CHT in lung and GEP-NECs (104,105,108). In addition, the loss of
RB1 is associated with superior responses to platinum salts
in both lung and pancreas NECs (104,109), whilst the presence of p53
staining in colorectal NECs is associated with weaker responses to
platinum-based CHT and worse prognosis (105). In GEP-NECs, p53 IHC is
currently under examination as a possible diagnostic, prognostic
and predictive method for GEP-NECs, which was reported in several
studies with frequencies of p53 immunoreactive cells ranging
from 20-100% (103), where
mutations in TP53 associates poor survival, moreover TP53
being the most prevalent mutation in NECs (105,110).
INSM1 is a zinc-finger family of transcription
factors that serves a role in neurogenesis and neuroendocrine cell
differentiation (111). INSM1
confers certain advantages in NECs as it more sensitive compared
with traditional general neuroendocrine markers, such as CgA or
synaptophysin, since the clear nuclear expression pattern of INSM1
facilitates its accurate interpretation and quantification whilst
reducing the incidence of staining artifacts (65).
The Notch/hairy and enhancer of split-1 (Hes-1)
signaling pathway serves a key role in tumor growth and
development, which has also been reported to inhibit INSM1(112). INSM1 has recently been reported
to be an important biomarker in the diagnosis of SCLC as it serves
as an important factor in ASCL1-driven pathways. ASCL1 is needed
for the protein expression of NE molecules and in the development
of lung NE cells (113,114). Furthermore, functional
interactions between ASCL1 and the Notch1-Hes1 pathway have been
reported (113). As
aforementioned, the Notch1-Hes1 pathway is involved in the
suppression of INSM1 expression (112). Moreover, the implication of INSM1
suppression is being studied as a modulator factor in PanNETs,
which could be connected to the Notch1-Hes1 signaling pathway
(112,115).
The NETest uses multianalyte assays with algorithmic
analyses (MAAAs), which is a novel method including procedures that
incorporate results derived from multiple assays and can increase
both the sensitivity and specificity (117). This assay involves mRNA
isolation, cDNA synthesis followed by the subsequent
quantitative-PCR measurement of 51 circulating NET marker genes
(117). These genes were chosen
based on the analyzed microarray datasets containing the cellular
profiles of fresh frozen tumor samples and whole blood samples from
patients diagnosed with NET to characterize the expression patterns
(117). Finally, a multi-analyte
liquid biopsy representative for NETs was used to determine the
biological activity of the tumor and therefore clinical status of
the patient (118). Results are
presented as the numeric score (NET score) that include the
following three categories: i) Low, ≤21-40%; ii) intermediate,
41-79%; and iii) high (biologically aggressive), ≥80%. The PCR test
is standardized and reproductible; moreover, diet, proton pump
inhibitors medication, age, sex and ethnicity do not interfere with
the accuracy of the test (119,120). In addition, MAAA is reproducible
at multiple time points, which provides real-time NET scores
(118,120).
In a cohort of 100 patients with three different
types of tumors (GEP, lung bronchopulmonary NETs and unknown origin
tumors), the NETest test had a reported diagnostic sensitivity of
96%, which was >90% effective in combination with diagnostic
imaging for guiding treatment decisions (121). This previous study also
demonstrated that a low NET score (≤40%) was associated with
superior outcomes, where the PFS was not reached, whilst
intermediate to high NETest scores (41-100%) were associated with
significantly shorter PFS and treatment failures (121). In addition, the NETest has been
documented to be a useful tool for the detection of lung, thymic,
pancreatic and gastrointestinal tract NETs, as well as
paragangliomas and pheochromocytomas with ≥90% accuracy (39). Moreover, the NETest can predict
aggressive tumor behavior in other NENs (122,123), or the outcome following tumor
resection and efficacy of medical treatments, such as somatostatin
analogues (SSAs) or peptide receptor radionuclide therapy (PRRT)
(39).
A recent meta-analysis was conducted to assess the
eligibility of NETest as a biomarker tool in the field of oncology
(124). The results supported the
utility of this test as a diagnostic tool for GEP and
bronchopulmonary NETs, which reported an accuracy of 85% in
differentiating between stable and progressive disease whereas a
specificity of ~90% was reported (124).
ARX and PDX1 are regulatory proteins involved as
epigenetic modifiers in pancreatic development (86). The assessment of ARX/PDX1
expression has been previously studied as a potential pre-operative
risk stratification marker for PanNETs (125). Since >50% PanNETs already have
liver metastases at first presentation, novel strategies are
emerging for the other 50% with aims to reduce the risk of
metastasis (126). Although the
choice of surgery for the primary tumor can reduce the risk of
metastasis, it is also associated with increased risk of
post-surgery morbidity and mortality. Therefore, apart from tumor
size, transcription factors ARX and PDX1 alongside ATRX/DAXX
mutations and the status of ALT were studied as prognostic markers
in resected NF PanNETs (96).
Cytological specimens of PanNETs obtained by endoscopic FNA was
previously studied using the IHC staining of ARX, PDX1 and
telomere-specific fluorescence in situ hybridization to
detect ALT (125). Positive ALT
activity and ARX expression in the tumor coupled with negative PDX1
staining was documented to predict metastatic phenotype for the
stratification of patients into the low- or high-risk groups
preoperatively (125).
miRNAs are a class of RNAs that do not encode
protein and are ~22 nucleotides in length (127). They typically regulate
post-transcriptional gene expression by targeting mRNA molecules
(127). Circulating miRNAs can be
used as minimally invasive biomarkers of ovarian, cervical or
breast cancer as they are readily detectable in a wide variety of
biofluids, including plasma, serum and saliva (128).
The global microRNA expression patterns were studied
in normal pancreas, PanNETs and acinar carcinomas in order to
assess the role of microRNAs in malignant transformation and
progression (129). miR-103 and
miR-107 expression levels were found to be higher whereas the level
miR-155 expression was lower in PanNETs compared with the normal
pancreas (129). Furthermore,
miR-21 expression level appears to be higher in the plasma of
patients with PanNETs compared with that in patients with chronic
pancreatitis (129). Therefore,
it can be applied both as a diagnostic and a prognostic tool for
PanNETs, since higher levels of miR-21 expression and high Ki-67
proliferation index were associated with the presence of metastases
(129,130).
It was recently reported that in tumors without a
known primary site, miRNA expression can be used to facilitate
diagnosis (131). miRNA
expression profiles were previously analyzed in four pathological
types of GEP-NETs, including samples from pancreatic, ileal,
appendiceal and rectal NETs (131). The results were promising, as the
midgut NETs (ileum and appendix) could be discriminated from
non-midgut NETs (rectum, pancreas) according to miR-615 and miR-92b
expression (131). In addition,
ileal NETs could be discriminated from appendiceal NETs according
to miR-125b, miR-192 and miR-149 expression, whilst rectal NETs
could be distinguished from pancreatic NETs based on miR-429 and
miR-487b expression (131).
Due to their stability in the circulation and
abundance, cell-type and disease stage specificity and their
reported roles in a number of biological processes, miRNAs have
been investigated in various studies. However, due to the lack of
consistency in the reported signatures (between results that used
tissue and those that used circulating blood) for the same disease
and the lack of standardization methods with accurate techniques,
further research is required (132,133).
The role of the MGMT enzyme is to repair DNA
lesions as a result of alkylating agents usually used in NENs. Loss
of MGMT function occurs as a result of epigenetic events, such as
hypermethylation, of the MGMT gene promoter (136). This in turn leads to the loss of
MGMT protein expression, which can be detected using IHC or
detected on the gene level by methylation analysis (for example
using methyl-specific PCR or pyrosequencing). Analysis of the MGMT
status can be used to predict the prognosis and response to
alkylating agents that induce DNA damage in well-differentiated
NENs (107). Previous studies
showed that reduced MGMT expression is associated with increased
rates of treatment response to temozolomide, dacarbazine and
streptozotocin CHT in digestive and lung NENs (136,137).
The importance of tumor-specific alterations in
cell-free DNA (cfDNA) in liquid biopsies is becoming increasingly
recognized, which can either complement or replace tissue biopsies
for several types of cancer, including NSCLC with mutations in the
EGFR gene (138,139). cfDNA consists of a proportion of
circulating tumor DNA (ctDNA) in the blood plasma, which originates
from the tumor following apoptosis, necrosis and active secretion
(140,141). cfDNA can be used as a biomarker
for cancer, as patients with patients are reported to have greater
levels of plasma cfDNA compared with tumor-free controls (142); in addition, high levels of cfDNA
are also described in other diseases, such as autoimmune disorders
(143). However, further studies
in NENs are required to verify the utility of cfDNA as a profiling
tool. Boons et al (141)
first reported that the presence of ctDNA through the
identification of copy number variations and tumor specific point
mutations using shallow whole genome sequencing and droplet digital
PCR, respectively can be used to differentiate between metastatic
and localized PanNET. The results of this study demonstrated that
ctDNA is found in the plasma samples of patients with metastatic
disease. This was shown by tumor-specific variants that were
obtained through whole exome sequencing (WES) analysis of primary
tumor tissue and germline DNA, in comparison with localized PanNETs
where when genotyping variants in cfDNA, the variants could not be
detected. Therefore, cfDNA is a candidate as an alternative
biomarker to tissue biopsies for molecular profiling.
CTCs are typically released into the blood of
patients who have undergone epithelial and mesenchymal transition,
which cause metastatic disease (13,144). The presence of CTCs at the moment
of recruitment/initial evaluation in the blood samples of patients
with midgut, pancreas, bronchopulmonary and of unknown primary
metastatic NENs was previously associated with worse PFS and OS
(145). In addition, CTCs are
associated with higher tumor grades and burden, high levels of CgA
and higher Ki-67 indices in G1 and G2 midgut and pancreatic NETs
(146). Their potential
predictive role was previously studied in a cohort of 138 patients
with metastatic NENs, where 41 (29.7%) received long-term SSAs.
Changes in repeat CTC count at 3-5 weeks after initiation of
therapy were associated with both progressive disease and OS
(147). Improved survival was
recorded in patients who did not have CTCs at baseline and after
therapy in addition to those who presented with >50% CTC
reduction after treatment (147).
However, CTC lacks sensitivity and specificity as a diagnostic tool
for different types of NENs (13).
This limitation is currently under investigation in a multicenter,
exploratory CalmNET phase IV study (ClinicalTrials.gov Identifier, NCT02075606), which is
monitoring a relatively homogeneous group of patients with F G1-G2
midgut NETs treated with lanreotide autogel. This study is
attempting to evaluate the predictive power of CTC count on
clinical outcome, PFS and quality of life (148).
Expression of SSTR in the majority of NENs,
particularly subtype 2, can be imaged by labelling SSAs with a
radionuclide, which is typically 68Ga, using a chelate,
such as 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid
(DOTA) (149,150).
At present, two types of molecular imaging that can
be used to target SSTR in clinical practice:
111In-pentetreotide (OctreoScan) and
68Ga-DOTA-Phe1-Tyr3-Octreotide
(TOC), 68Ga-DOTA-NaI3-Octreotide (NOC) or
68Ga-DOTA-Tyr3-Octreotate (TATE).
68Ga-DOTA-TATE/TOC/NOC-PET/CT confers higher scanner
sensitivity, superior spatial resolution and require lower
radiation doses (151). Although
all three radiotracers (DOTA-TOC, DOTA-NOC and DOTA-TATE) have good
affinity for SSTR types 2 and 5, 68Ga-DOTA-NOC exhibits
higher affinity for SSTR type 3(152). However, 68Ga-DOTA-TATE
confers superior diagnostic precision for the nuclear imaging of
NENs and is currently used in USA, whilst
68Ga-DOTA-TOC-PET is mainly used clinically in the
European Union (153,154).
PRRT is a key second-line treatment option for G1
or G2 midgut NETs with disease progression on SSA treatment
(91). PRRT can be used to
identify radiation delivered by radionuclides, such as lutetium-177
(177Lu) or yttrium-90 (90Y), to NET cells
following internalization after binding to SSTR (151). However, the expression of SSTRs
is currently being studied as a predictive marker for treatment
response (13). In the NETTER-1
prospective randomized phase 3 clinical trial (ClinicalTrials.gov Identifier, NCT01578239),
177Lu-DOTA-TATE demonstrated its superiority compared
with high-dose octreotide in prolonging the PFS in patients with
midgut NETs (PFS at month 20, 65.3% for 177Lu-DOTATATE;
10.8% for high-dose octreotide group) (159).
Higher tumor uptake of radiolabeled somatostatin
receptor antagonists their potential role has been studied for
diagnostic and therapeutic approach in NETs (160). Previous studies reported higher
sensitivity and diagnostic accuracy with increased image contrast
for 68Ga-NODAGA-JR11 (68Ga-OPS202), a SSTR-2 antagonist,
compared with agonists 68Ga-DOTA-TATE and
68Ga-DOTA-TOC, for staging G1 and G2 GEP-NETs
(ClinicalTrials.gov identifier,
NCT02162446) (160,161). A ‘theragnostic
pair’-68Ga/177Lu-DOTA-JR11 combination was
also investigated in a single-center study (ClinicalTrials.gov identifier, NCT02609737). Although
there are indications that it binds to more cell types compared
with DOTA-TATE or DOTA-TOC in low-grade NETs, this investigation
remain in progress at present. Similarly, a peptide ligand,
68Ga-DOTA-bombesin, which can bind to the gastrin
realizing peptide receptor in prostate cancer cells (162), is another example of this
receptor system that is under evaluation for NENs. Its first
application for PET imaging in humans for prostate and breast
cancer has been previously reported (162).
Somatostatin receptor imaging (SRI) is currently
considered the gold standard for detecting well-differentiated
NETs. However, it has a number of limitations for detecting high
grade NETs due to the possibility of false-negatives, since these
types of tumors do not express SSTRs (156). Although 18F-FDG-PET
can be used for staging G3 NECs, it is more suited for predicting
the prognosis of well-differentiated NETs, where higher levels of
uptake were associated with an increased risk of early progression
(163). By contrast, lower levels
of uptake is associated with a less aggressive phenotype of the
tumor (163). Chan et al
(165) therefore proposed a
grading system combining these two nuclear imaging techniques (SRI
and 18F-FDG-PET) as a single parameter, named ‘NET-PET’,
which was found to associate with OS. This scoring system is
designated into five risk category groups: i) Grade P0, negative
uptake for both scans; ii) grade P1, purely STTR-positive lesions
without FDG uptake above background; iii) grades P2-P4,
intermediate categories; and iv) grade P5, presence of significant
FDG-positive/STTR-negative disease (166). The NET-PET score may influence
the initial management method of patients with well-differentiated
metastatic midgut NET, since the ENETS guideline (167) recommends CHT or SSA as the
first-choice treatment option. During the initial phases of SSA
therapy, there is no consensus on the upper cut-off value of the
Ki-67 proliferation index (165).
In this case, the NET-PET score would favor SSA treatment if there
is high SRI uptake and low FDG uptake, whilst the contrary would
favor CHT (168). The same line
of reasoning can be made during patient selection for PRRT, where
high SRI uptake but low FDG uptake would suggest PRRT as a viable
treatment option, whilst higher FDG uptake and low SRI uptake would
indicate likelihood of PPRT resistance (169). Since this was a retrospective
analysis, it remains to be elucidated how the individual
intermediate classifications can influence the prognosis and
treatment decision in a prospective study.
Accumulating data suggest that the response
evaluation criteria in solid tumors (RECIST 1.1) has several
limitations in predicting the response to different types of
systemic treatments (ST) (34,170). According to RECIST 1.1, the
majority of patients with G1-2 GEP-NETs would be classified as
having ‘stable disease’ (170).
However, even non-responders can survive for a long period without
disease progression, since it is known that well-differentiated
GEP-NETs have a relatively slow growth rate (34). Therefore, is important to discover
a tumor marker that can identify patients who are at high risk of
disease progression at the early stage (171). Previous studies reported TGR to
be a dynamic marker, which analyzes images from two examinations
and the time between the examinations and can reveal beneficial
quantitative information regarding the percentage of change in the
tumor volume each month (171,172). The GREPONET I study confirmed
that the TGR measured at 3 months (TGR3m) after starting
ST or watch and wait (WW) treatment with a cut-off of 0.8%/m (m,
percentage of the change of the tumor size in one month), could be
used in clinical practice to monitor the treatment response in NETs
for the early prediction of PFS (34). In addition, an increased
TGR3m (≥0.8%/m) was found to associated with shorter
PFS, whilst a decreased TGR3m (<0.8%/m-) was found to
associate with longer PFS (34).
This finding suggests that patients with high TGR3m
should be followed up more regularly, whilst those with lower
TGR3m can receive imaging less regularly to avoid
unnecessary radiation (34).
Subsequently, the GREPONET II study explored whether beginning any
ST including WW can induce any changes in TGR, which was defined as
TGR3m-TGR0 (TGR0 was calculated by
comparing the baseline and imaging examination performed within 1
year before the baseline scan) (35). Since it was expected that TGR can
be used for monitoring treatment change with no impact on PFS,
further study is required.
Selection of the optimal treatment option for
patients with NEN is difficult due to the heterogeneity in the
tumor physiology and varying degrees of aggressiveness. There is a
demand for multidisciplinary tumor management guidelines driven by
data derived from modern radiology and molecular profiling
techniques, to inform the optimal medical decision. Overall,
further studies integrating a combination of markers based on tumor
genomics and a large spectrum of radiological techniques, such as
molecular imaging, would be better placed for shaping the future of
clinical NEN research. The present review highlights the importance
of a second opinion for improving the method of prognostic
stratification and choice of personalized treatment strategies.
Not applicable.
No funding was received.
Not applicable.
OAC wrote the literature review. SF and SM
critically reviewed the manuscript. Data authentication is not
applicable. All authors read and approved the final manuscript.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
|
1
|
Klöppel G: Neuroendocrine neoplasms:
Dichotomy, origin and classifications. Visc Med. 33:324–330.
2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Oberg K, Modlin IM, de Herder W, Pavel M,
Klimstra D, Frilling A, Metz DC, Heaney A, Kwekkeboom D, Strosberg
J, et al: Consensus on biomarkers for neuroendocrine tumour
disease. Lancet Oncol. 16:e435–e446. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Cheung VTF and Khan MS: A guide to midgut
neuroendocrine tumours (NETs) and carcinoid syndrome. Frontline
Gastroenterol. 6:264–269. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Pedraza-Arévalo S, Gahete MD, Alors-Pérez
E, Luque RM and Castaño JP: Multilayered heterogeneity as an
intrinsic hallmark of neuroendocrine tumors. Rev Endocr Metab
Disord. 19:179–192. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Modlin IM, Gustafsson BI, Moss SF, Pavel
M, Tsolakis AV and Kidd M: Chromogranin A-biological function and
clinical utility in neuro endocrine tumor disease. Ann Surg Oncol.
17:2427–2443. 2010.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zatelli MC, Grossrubatscher EM, Guadagno
E, Sciammarella C, Faggiano A and Colao A: Circulating tumor cells
and mirnas as prognostic markers in neuroendocrine neoplasms.
Endocr Relat Cancer. 24:R223–R237. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Sechidis K, Papangelou K, Metcalfe PD,
Svensson D, Weatherall J and Brown G: Distinguishing prognostic and
predictive biomarkers: An information theoretic approach.
Bioinformatics. 34:3365–3376. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lloyd RV, Osamura RY, Klöppel G and Rosai
J (eds): WHO Classification of Tumours of Endocrine Organs. 4th
edition, Volume 10. Lloyd RV, Osamura RY, IARC, 2017.
|
|
9
|
Rindi G, Klimstra DS, Abedi-Ardekani B,
Brambilla E, Asa LS, Bosman TF, Busam JK, Dietel M,
Fernandez-Cuesta L, Sasano H, et al: A common classification
framework for neuroendocrine neoplasms: An International Agency for
Research on Cancer (IARC) and World Health Organization (WHO)
expert consensus proposal. Mod Pathol. 31:1770–1786.
2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Nagtegaal ID, Odze RD, Klimstra D, Paradis
V, Rugge M, Schirmacher P, Washington KM, Carneiro F and Cree IA:
WHO Classification of Tumours Editorial Board. The 2019 WHO
classification of tumours of the digestive system. Histopathology.
76:182–188. 2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Travis WD, Brambilla E, Nicholson AG,
Yatabe Y, Austin JHM, Beasley MB, Chirieac LR, Dacic S, Duhig E,
Flieder DB, et al: The 2015 World Health Organization
classification of lung tumors: Impact of genetic, clinical and
radiologic advances since the 2004 classification. J Thorac Oncol.
10:1243–1260. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Rindi G and Inzani F: Neuroendocrine
neoplasm update: Toward universal nomenclature. Endocr Relat
Cancer. 27:R211–R218. 2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Herrera-Martínez AD, Hofland LJ, Gálvez
Moreno MA, Castaño JP, de Herder WW and Feelders RA: Neuroendocrine
neoplasms: Current and potential diagnostic, predictive and
prognostic markers. Endocr Relat Cancer. 26:R157–R179.
2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Rindi G, Klöpper G, Alhman H, Caplin M,
Couvelard A, de Herder WW, Eriksson B, Falchetti A, Falconi M,
Komminoth P, et al: TNM staging of foregut (neuro)endocrine tumors:
A consensus proposal including a grading system. Virchows Arch.
449:395–401. 2006.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Rindi G, Klöpper G, Couvelard A, Komminoth
P, Körner M, Lopes JM, McNicol AM, Nilsson O, Perren A, Scarpa A,
et al: TNM staging of midgut and hindgut (neuro) endocrine tumors:
A consensus proposal including a grading system. Virchows Arch.
451:757–762. 2007.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cho JH, Ryu JK, Song SY, Hwang JH, Lee DK,
Woo SM, Joo YE, Jeong S, Lee SO, Park BK, et al: Prognostic
validity of the American joint committee on cancer and the European
neuroendocrine tumors staging classifications for pancreatic
neuroendocrine tumors: A retrospective nationwide multicenter study
in South Korea. Pancreas. 45:941–946. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Strosberg JR, Cheema A, Weber J, Han G,
Coppola D and Kvols LK: Prognostic validity of a novel American
Joint Committee on Cancer Staging Classification for pancreatic
neuroendocrine tumors. J Clin Oncol. 29:3044–3049. 2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Rindi G, Falconi M, Klersy C, Albarello L,
Boninsegna L, Buchler WM, Capella C, Caplin M, Couvelard A,
Doglioni C, et al: TNM staging of neoplasms of the endocrine
pancreas: Results from a large international cohort study. J Natl
Cancer Inst. 104:764–777. 2012.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Gustafsson BI, Kidd M, Chan A,
Malfertheiner MV and Modlin IM: Bronchopulmonary neuroendocrine
tumors. Cancer. 113:5–21. 2008.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Yao JC, Hassan M, Phan A, Dagohoy C, Leary
C, Mares JE, Abdalla EK, Flemming JB, Vauthey IN, Rashid A and
Evans DB: One hundred years after ‘carcinoid’: Epidemiology of and
prognostic factors for neuroendocrine tumors in 35,825 cases in the
United States. J Clin Oncol. 26:3063–3072. 2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Garcia-Carbonero R, Capdevila J,
Crespo-Herrero G, Díaz Pérez JA, Martínez Del Prado MP, Alonso
Orduña V, Sevilla-García I, Villabona-Artero C, Beguiristain-Gómez
A, Llanos-Muñoz M, et al: Incidence, patterns of care and
prognostic factors for outcome of gastroenteropancreatic
neuroendocrine tumors (GEP-NETs): Results from the National cancer
registry of Spain (RGETNE). Ann Oncol. 21:1794–1803.
2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ruzzenente A, Bagante F, Bertuzzo F,
Aldrighetti L, Ercolani G, Giuliante F, Ferrero A, Torzilli G,
Grazi GL, Ratti F, et al: A novel nomogram to predict the prognosis
of patients undergoing liver resection for neuroendocrine liver
metastasis: An analysis of the Italian neuroendocrine liver
metastasis database. J Gastrointest Surg. 21:41–48. 2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Cao LL, Lu J, Lin JX, Zheng CH, Li P, Xie
JW, Wang JB, Chen QY, Lin M, Tu RH and Huang CM: A novel predictive
model based on preoperative blood neutrophilto-lymphocyte ratio for
survival prognosis in patients with gastric neuroendocrine
neoplasms. Oncotarget. 7:42045–42058. 2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Villani V, Mahadevan KK, Ligorio M,
Fernández-Del Castillo C, Ting DT, Sabbatino F, Zhang I, Vangel M,
Ferrone S, Warshaw AL, et al: Phosphorylated histone H3 (PHH3) is a
superior proliferation marker for prognosis of pancreatic
neuroendocrine tumors. Ann Surg Oncol. 23 (Suppl 5):S609–S617.
2016.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Modlin IM, Moss SF, Chung DC, Jensen RT
and Snyderwine E: Priorities for improving the management of
gastroenteropancreatic neuroendocrine tumors. J Natl Cancer Inst.
100:1282–1289. 2008.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Turner GB, Johnston BT, McCance DR,
McGinty A, Watson RGP, Patterson CC and Ardill JE: Circulating
markers of prognosis and response to treatment in patients with
midgut carcinoid tumours. Gut. 55:1586–1591. 2006.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Modlin IM, Oberg K, Taylor A, Drozdov I,
Bodei L and Kidd M: Neuroendocrine tumor biomarkers: Current status
and perspectives. Neuroendocrinology. 100:265–277. 2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Kulke MH, Siu LL, Tepper JE, Fisher G,
Jaffe D, Haller DG, Ellis LM, Benedetti JK, Bergsland EK, Hobday
TJ, et al: Future directions in the treatment of neuroendocrine
tumors: Consensus report of the National cancer institute
neuroendocrine tumor clinical trials planning meeting. J Clin
Oncol. 29:934–943. 2011.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Ambrosini V, Kunikowska J, Baudin E, Bodei
L, Bouvier C, Capdevila J, Cremonesi M, de Herder WW, Dromain C,
Falconi M, et al: Consensus on molecular imaging and theranostics
in neuroendocrine neoplasms. Eur J Cancer. 146:56–73.
2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Majala S, Seppänen H, Kemppainen J,
Sundström J, Shalin-Jäntti C, Gullichsen R, Schildt J, Mustonen H,
Vesterinen T, Arola J and Kauhanen S: Prediction of the
aggressiveness of non-functional pancreatic neuroendocrine tumors
based on the dual-tracer PET/CT. EJNMMI Res. 9(116)2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Bodei L, Sundin A, Kidd M, Prasad V and
Modlin IM: The status of neuroendocrine tumor imaging: From
darkness to light? Neuroendocrinology. 101:1–17. 2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Righi L, Volante M, Tavaglione V, Billè A,
Daniele L, Angusti T, Inzani F, Pelosi G, Rindi G and Pappotti M:
Somatostatin receptor tissue distribution in lung neuroendocrine
tumours: A clinicopathologic and immunohistochemical study of 218
‘clinically aggressive’ cases. Ann Oncol. 21:548–555.
2010.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Reubi JC, Waser B, Cescato R, Gloor B,
Stettler C and Christ E: Internalized somatostatin receptor subtype
2 in neuroendocrine tumors of octreotide-treated patients. J Clin
Endocrinol Metab. 95:2343–2350. 2010.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Lamarca A, Crona J, Ronot M, Opalinska M,
Lopez Lopez C, Pezzutti D, Najran P, Carvhalo L, Franca Bezerra RO,
Borg P, et al: Value of tumor growth rate (TGR) as an early
biomarker predictor of patients' outcome in neuroendocrine tumors
(NET)-The GREPONET Study. Oncologist. 24:e1082–e1090.
2019.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Lamarca A, Ronot M, Moalla S, Crona J,
Opalinska M, Lopez Lopez C, Pezzutti D, Najran P, Carvhalo L,
Bezerra ROF, et al: Tumor growth rate as a validated early
radiological biomarker able to reflect treatment-induced changes in
neuroendocrine tumors: The GREPONET-2 study. Clin Cancer Res.
25:6692–6699. 2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Hanahan D and Weinberg RA: The hallmarks
of cancer. Cell. 100:57–70. 2000.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Hanahan D and Weinberg RA: Hallmarks of
cancer: The next generation. Cell. 144:646–674. 2011.PubMed/NCBI View Article : Google Scholar
|
|
38
|
De Rubis G, Rajeev Krishnan S and Bebawy
M: Liquid biopsies in cancer diagnosis, monitoring, and prognosis.
Trends Pharmacol Sci. 40:172–186. 2019.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Malczewska A, Kos-Kudła B, Kidd M, Drozdov
I, Bodei L, Matar S, Oberg K and Modlin IM: The clinical
applications of a multigene liquid biopsy (NETest) in
neuroendocrine tumors. Adv Med Sci. 65:18–29. 2020.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Nehar D, Lombard-Bohas C, Olivieri S,
Claustrat B, Chayvialle JA, Penes MC, Sassolas G and Borson-Chazot
F: Interest of chromogranin a for diagnosis and follow-up of
endocrine tumours. Clin Endocrinol (Oxf). 60:644–652.
2004.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Baekdal J, Krogh J, Klose M, Holmager P,
Langer SW, Oturai P, Kjaer A, Federspiel B, Hilsted L, Rehfeld JF,
et al: Limited diagnostic utility of chromogranin A measurements in
workup of neuroendocrine tumors. Diagnostics (Basel).
10(881)2020.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Gkolfinopoulos S, Tsapakidis K,
Papadimitriou K, Papamichael D and Kountourakis P: Chromogranin A
as a valid marker in oncology: Clinical application or false hopes?
World J Methodol. 7:9–15. 2017.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Malczewska A, Kidd M, Matar S, Kos-Kudła
B, Bodei L, Oberg K and Modlin IM: An assessment of circulating
chromogranin a as a biomarker of bronchopulmonary neuroendocrine
Neoplasia: A systematic review and meta-analysis.
Neuroendocrinology. 110:198–216. 2020.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Zatelli MC, Torta M, Leon A, Ambrosio MR,
Gion M, Tomassetti P, De Braud F, Delle Fave G, Dogliotti L and
degli Uberti EC: Italian CromaNet Working Group. Chromogranin A as
a marker of neuroendocrine neoplasia: An Italian multicenter study.
Endocr Relat Cancer. 14:473–482. 2007.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Campana D, Nori F, Piscitelli L,
Morselli-Labate AM, Pezzilli R, Corinaldesi R and Tomassetti P:
Chromogranin A: Is it a useful marker of neuroendocrine tumors? J
Clin Oncol. 25:1967–1973. 2007.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Stridsberg M, Oberg K, Li Q, Engstrom U
and Lundqvist G: Measurements of chromogranin A, chromogranin B
(secretogranin I), chromogranin C (secretogranin II) and
pancreastatin in plasma and urine from patients with carcinoid
tumours and endocrine pancreatic tumours. J Endocrinol. 144:49–59.
1995.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Chan DL, Clarke SJ, Diakos CI, Roach PJ,
Bailey DL, Singh S and Pavlakis N: Prognostic and predictive
biomarkers in neuroendocrine tumours. Crit Rev Oncol Hematol.
113:268–282. 2017.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Baudin E, Bidart JM, Bachelot A, Ducreux
M, Elias D, Rufflé P and Schlumberger M: Impact of chromogranin A
measurement in the work-up of neuroendocrine tumors. Ann Oncol 12
Suppl. 2:S79–S82. 2001.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Nölting S, Kuttner A, Lauseker M, Vogeser
M, Haug A, Hermann KA, Hoffmann JN, Spitzweg C, Göke B and
Auernhammer CJ: Chromogranin a as serum marker for
gastroenteropancreatic neuroendocrine tumors: A single center
experience and literature review. Cancers (Basel). 4:141–155.
2012.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Mashige F, Matsushimal Y, Kanazawal H,
Sakuma I, Takai N, Besshof F and Ohkubo A: Acidic catecholamine
metabolites and 5-hydroxyindoleacetic acid in urine: The influence
of diet. Ann Clin Biochem. 33:43–49. 1996.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Feldman JM: Urinary serotonin in the
diagnosis of carcinoid tumors. Clin Chem. 32:840–844.
1986.PubMed/NCBI
|
|
52
|
Sjöblom SM: Clinical presentation and
prognosis of gastrointestinal carcinoid tumours. Scand J
Gastroenterol. 23:779–787. 1988.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Bhattacharyya S, Raja SG, Toumpanakis C,
Caplin ME, Dreyfus GD and Davar J: Outcomes, risks and
complications of cardiac surgery for carcinoid heart disease. Eur J
Cardiothorac Surg. 40:168–172. 2011.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Niederle B, Pape UF, Costa F, Gross D,
Kelestimur F, Knigge U, Öberg K, Pavel M, Perren A, Toumpanakis C,
et al: ENETS consensus guidelines update for neuroendocrine
neoplasms of the jejunum and ileum. Neuroendocrinology.
103:125–138. 2016.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Korse CM, Taal BG, de Groot CA, Bakker RH
and Bonfrer JM: Chromogranin-A and N-terminal pro-brain natriuretic
peptide: An excellent pair of biomarkers for diagnostics in
patients with neuroendocrine tumor. J Clin Oncol. 27:4293–4299.
2009.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Modlin IM, Bodei L and Kidd M:
Neuroendocrine tumor biomarkers: From monoanalytes to transcripts
and algorithms. Best Pract Res Clin Endocrinol Metab. 30:59–77.
2016.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Bhattacharyya S, Toumpanakis C, Caplin ME
and Davar J: Usefulness of N-terminal pro-brain natriuretic peptide
as a biomarker of the presence of carcinoid heart disease. Am J
Cardiol. 102:938–942. 2008.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Isgrò MA, Bottoni P and Scatena R:
Neuron-specifi c enolase as a biomarker: Biochemical and clinical
aspects. Adv Exp Med Biol. 867:125–143. 2015.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Baudin E, Gigliotti A, Ducreux M, Ropers
J, Comoy E, Sabourin JC, Bidart JM, Cailleux AF, Bonacci R, Ruffié
P and Schlumberger M: Neuron-specific enolase and chromogranin A as
markers of neuroendocrine tumours. Br J Cancer. 78:1102–1107.
1998.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Walter T, Chardon L, Chopin-Laly X,
Raverot V, Caffin AG, Chayvialle JA, Scoazec JY and Lombard-Bohas
C: Is the combination of chromogranin A and pancreatic polypeptide
serum determinations of interest in the diagnosis and follow-up of
gastro-entero-pancreatic neuroendocrine tumours? Eur J Cancer.
48:1766–1773. 2012.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Laskaratos FM, Rombouts K, Caplin M,
Toumpanakis C, Thirlwell C and Mandair D: Neuroendocrine tumors and
fibrosis: An unsolved mystery? Cancer. 123:4770–4790.
2017.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Behnes M, Brueckmann M, Lang S, Weiß C,
Ahmad-Nejad P, Neumaier M, Borggrefe M and Hoffmann U: Connective
tissue growth factor (CTGF/CCN2): Diagnostic and prognostic value
in acute heart failure. Clin Res Cardiol. 103:107–116.
2014.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Cunningham JL, Tsolakis AV, Jacobson A and
Janson ET: Connective tissue growth factor expression in endocrine
tumors is associated with high stromal expression of alpha-smooth
muscle actin. Eur J Endocrinol. 163:691–697. 2010.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Kidd M, Modlin I, Shapiro M, Camp R, Mane
S, Usinger W and Murren J: CTGF, intestinal stellate cells and
carcinoid fibrogenesis. World J Gastroenterol. 13:5208–5216.
2007.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Bellizzi AM: Immunohistochemistry in the
diagnosis and classification of neuroendocrine neoplasms: What can
brown do for you? Hum Pathol. 96:8–33. 2020.PubMed/NCBI View Article : Google Scholar
|
|
66
|
McCall CM, Shi C, Cornish TC, Klimstra DS,
Tang LH, Basturk O, Mun LJ, Ellison TA, Wolfgang CL, Choti MA, et
al: Grading of well-differentiated pancreatic neuroendocrine tumors
is improved by the inclusion of both ki67 Proliferative index and
mitotic rate. Am J Surg Pathol. 37:1671–1677. 2013.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Bellizzi AM: Pathologic considerations in
gastroenteropancreatic neuroendocrine tumors. Surg Oncol Clin N Am.
29:185–208. 2020.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Coriat R: Aggressive
gastro-entero-pancreatic neoplasms. Ann Endocrinol (Paris).
80:185–186. 2019.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Pape UF, Jann H, Müller-Nordhorn J,
Bockelbrink A, Berndt U, Willich SN, Koch M, Röcken C, Rindi G and
Wiedenmann B: Prognostic relevance of a novel TNM classification
system for upper gastroenteropancreatic neuroendocrine tumors.
Cancer. 113:256–265. 2008.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Strosberg J, Nasir A, Coppola D, Wick M
and Kvols L: Correlation between grade and prognosis in metastatic
gastroenteropancreatic neuroendocrine tumors. Hum Pathol.
40:1262–1268. 2009.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Lopez-Aguiar AG, Ethun CG, Postlewait LM,
Zhelnin K, Krasinskas A, El-Rayes BF, Russell MC, Sarmiento JM,
Kooby DA, Staley CA, et al: Redefining the Ki-67 index
stratification for low-grade pancreatic neuroendocrine tumors:
Improving its prognostic value for recurrence of disease. Ann Surg
Oncol. 25:290–298. 2018.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Zen Y and Heaton N: Elevated Ki-67
labeling index in ‘synchronous liver metastases’ of well
differentiated enteropancreatic neuroendocrine tumor. Pathol Int.
63:532–538. 2013.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Grillo F, Albertelli M, Brisigotti MP,
Borra T, Boschetti M, Fiocca R, Ferone D and Mastracci L: Grade
increases in gastroenteropancreatic neuroendocrine tumor metastases
compared to the primary tumor. Neuroendocrinology. 103:452–459.
2016.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Shi C, Gonzalez RS, Zhao Z, Koyama T,
Cornish TC, Hande KR, Walker R, Sandler M, Berlin J and Liu EH:
Liver metastases of small intestine neuroendocrine tumors: Ki-67
heterogeneity and World health organization grade discordance with
primary tumors. Am J Clin Pathol. 143:398–404. 2015.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Cives M and Strosberg JR:
Gastroenteropancreatic neuroendocrine tumors. CA Cancer J Clin.
68:471–487. 2018.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Singh S, Hallet J, Rowsell C and Law CH:
Variability of Ki67 labeling index in multiple neuroendocrine
tumors specimens over the course of the disease. Eur J Surg Oncol.
40:1517–1522. 2014.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Keck KJ, Choi A, Maxwell JE, Li G,
O'Dorisio TM, Breheny P, Bellizzi AM and Howe JR: Increased grade
in neuroendocrine tumor metastases negatively impacts survival. Ann
Surg Oncol. 24:2206–2212. 2017.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Sorbye H, Welin S, Langer SW, Vestermark
LW, Holt N, Osterlund P, Dueland S, Hofsli E, Guren MG, Ohrling K,
et al: Predictive and prognostic factors for treatment and survival
in 305 patients with advanced gastrointestinal neuroendocrine
carcinoma (WHO G3): The NORDIC NEC study. Ann Oncol. 24:152–160.
2013.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Welin S, Sorbye H, Sebjornsen S, Knappskog
S, Busch C and Öberg K: Clinical effect of temozolomide-based
chemotherapy in poorly differentiated endocrine carcinoma after
progression on first-line chemotherapy. Cancer. 117:4617–4622.
2011.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Jiang R, Hong X, Zhao Y and Wu W:
Application of multiomics sequencing and advances in the molecular
mechanisms of pancreatic neuroendocrine neoplasms. Cancer Lett.
499:39–48. 2021.PubMed/NCBI View Article : Google Scholar
|
|
81
|
van Riet J, van de Werken HJG, Cuppen E,
Eskens FALM, Tesselaar M, van Veenendaal LM, Klümpen HJ, Dercksen
MW, Valk GD, Lolkema MP, et al: The genomic landscape of 85
advanced neuroendocrine neoplasms reveals subtype-heterogeneity and
potential therapeutic targets. Nat Commun. 12(4612)2021.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Scarpa A, Chang DK, Nones K, Corbo V,
Patch AM, Bailey P, Lawlor RT, Johns AL, Miller DK, Mafficini A, et
al: Whole-genome landscape of pancreatic neuroendocrine tumours.
Nature. 543:65–71. 2017.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Mafficini A and Scarpa A: Genomic
landscape of pancreatic neuroendocrine tumours: The International
cancer genome consortium. J Endocrinol. 236:R161–R167.
2018.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Scarpa A: The landscape of molecular
alterations in pancreatic and small intestinal neuroendocrine
tumours. Ann Endocrinol (Paris). 80:153–158. 2019.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Pea A, Yu J, Marchionni L, Noe M, Luchini
C, Pulvirenti A, de Wilde RF, Brosens LA, Rezaee N, Javed A, et al:
Genetic analysis of small well-differentiated pancreatic
neuroendocrine tumors identifies subgroups with differing risks of
liver metastases. Ann Surg. 271:566–573. 2020.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Cejas P, Drier Y, Dreijerink KMA, Brosens
LAA, Deshpande V, Epstein CB, Conemans EB, Morsink FHM, Graham MK,
Valk GD, et al: Enhancer signatures stratify and predict outcomes
of non-functional pancreatic neuroendocrine tumors. Nat Med.
25:1260–1265. 2019.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Marinoni I: Prognostic value of DAXX/ATRX
loss of expression and ALT activation in PanNETs: Is it time for
clinical implementation? Gut gutjnl-2021-324664, 2021 (Epub ahead
of print).
|
|
88
|
Lewis PW, Elsaesser SJ, Noh KM, Stadler SC
and Allis CD: Daxx is an H3.3-specific histone chaperone and
cooperates with ATRX in replication-independent chromatin assembly
at telomeres. Proc Natl Acad Sci USA. 107:14075–14080.
2010.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Clynes D, Jelinska C, Xella B, Ayyub H,
Scott C, Mitson M, Taylor S, Higgs DR and Gibbons RJ: Suppression
of the alternative lengthening of telomere pathway by the chromatin
remodelling factor ATRX. Nat Commun. 6(7538)2015.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Singhi AD, Liu TC, Roncaioli JL, Cao D,
Zeh HJ, Zureikat AH, Tsung A, Marsh JW, Lee KK, Hogg ME, et al:
Alternative lengthening of telomeres and loss of DAXX/ATRX
expression predicts metastatic disease and poor survival in
patients with pancreatic neuroendocrine tumors. Clin Cancer Res.
23:600–609. 2017.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Pavel M, Öberg K, Falconi M, Krenning EP,
Sundin A, Perren A and Berruti A: ESMO Guidelines Committee.
Gastroenteropancreatic neuroendocrine neoplasms: ESMO clinical
practice guidelines for diagnosis, treatment and follow-up. Ann
Oncol. 31:844–860. 2020.PubMed/NCBI View Article : Google Scholar
|
|
92
|
VandenBussche CJ, Allison DB, Graham MK,
Charu V, Lennon AM, Wolfgang CL, Hruban RH and Heaphy CM:
Alternative lengthening of telomeres and ATRX/DAXX loss can be
reliably detected in FNAs of pancreatic neuroendocrine tumors.
Cancer Cytopathol. 125:544–551. 2017.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Heaphy CM, de Wilde RF, Jiao Y, Klein AP,
Edil BH, Shi C, Bettegowda C, Rodriguez FJ, Eberhart CG, Hebbar S,
et al: Altered telomeres in tumors with ATRX and DAXX mutations.
Science. 333(425)2011.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Luchini C, Lawlor RT, Bersani S, Vicentini
C, Paolino G, Mattiolo P, Pea A, Cingarlini S, Milella M and Scarpa
A: Alternative lengthening of telomeres (ALT) in pancreatic
neuroendocrine tumors: Ready for prime-time in clinical practice?
Curr Oncol Rep. 23(106)2021.PubMed/NCBI View Article : Google Scholar
|
|
95
|
Dogeas E, Karagkounis G, Heaphy CM, Hirose
K, Pawlik TM, Wolfgang CL, Meeker A, Hruban RH, Cameron JL and
Choti M: Alternative lengthening of telomeres predicts site of
origin in neuroendocrine tumor liver metastases. J Am Coll Surg.
218:628–635. 2014.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Hackeng WM, Brosens LAA, Kim JY,
O'Sullivan R, Sung YN, Liu TC, Cao D, Heayn M, Brosnan-Cashman J,
An S, et al: Non-functional pancreatic neuroendocrine tumours:
ATRX/DAXX and alternative lengthening of telomeres (ALT) are
prognostically independent from ARX/PDX1 expression and tumour
size. Gut gutjnl-2020-322595, 2021 (Epub ahead of print).
|
|
97
|
Kim JY, Brosnan-Cashman JA, An S, Kim SJ,
Song KB, Kim MS, Kim MJ, Hwang DW, Meeker AK, Yu E, et al:
Alternative lengthening of telomeres in primary pancreatic
neuroendocrine tumors is associated with aggressive clinical
behavior and poor survival. Clin Cancer Res. 23:1598–1606.
2017.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Marinoni I, Kurrer AS, Vassella E, Dettmer
M, Rudolph T, Banz V, Hunger F, Pasquinelli S, Speel EJ and Perren
A: Loss of DAXX and ATRX are associated with chromosome instability
and reduced survival of patients with pancreatic neuroendocrine
tumors. Gastroenterology. 146:453–460.e5. 2014.PubMed/NCBI View Article : Google Scholar
|
|
99
|
Missiaglia E, Dalai I, Barbi S, Beghelli
S, Falconi M, della Peruta M, Piemonti L, Capurso G, Di Florio A,
delle Fave G, et al: Pancreatic endocrine tumors: Expression
profiling evidences a role for AKT-mTOR pathway. J Clin Oncol.
28:245–255. 2010.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Stevenson M, Lines KE and Thakker RV:
Molecular genetic studies of pancreatic neuroendocrine tumors: New
therapeutic approaches. Endocrinol Metab Clin North Am. 47:525–548.
2018.PubMed/NCBI View Article : Google Scholar
|
|
101
|
Zou Z, Tao T, Li H and Zhu X: mTOR
signaling pathway and mTOR inhibitors in cancer: Progress and
challenges. Cell Biosci. 10(31)2020.PubMed/NCBI View Article : Google Scholar
|
|
102
|
Jiao Y, Shi C, Edil BH, de Wilde RF,
Klimstra DS, Maitra A, Schulick RD, Tang LH, Wolfgang CL, Choti MA,
et al: DAXX/ATRX, MEN1, and mTOR pathway genes are frequently
altered in pancreatic neuroendocrine tumors. Science.
331:1199–1203. 2011.PubMed/NCBI View Article : Google Scholar
|
|
103
|
Coriat R, Walter T, Terris B, Couvelard A
and Ruszniewski P: Gastroenteropancreatic well-differentiated grade
3 neuroendocrine tumors: Review and position statement. Oncologist.
21:1191–1199. 2016.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Hijioka S, Hosoda W, Matsuo K, Ueno M,
Furukawa M, Yoshitomi H, Kobayashi N, Ikeda M, Ito T, Nakamori S,
et al: Rb loss and KRAS mutation are predictors of the response to
platinum-based chemotherapy in pancreatic neuroendocrine neoplasm
with grade 3: A Japanese multicenter pancreatic NEN-G3 study. Clin
Cancer Res. 23:4625–4632. 2017.PubMed/NCBI View Article : Google Scholar
|
|
105
|
Ali AS, Grönberg M, Federspiel B, Scoazec
JY, Hjortland GO, Grønbæk H, Ladekarl M, Langer SW, Welin S,
Vestermark LW, et al: Expression of p53 protein in high-grade
gastroenteropancreatic neuroendocrine carcinoma. PLoS One.
12(e0187667)2017.PubMed/NCBI View Article : Google Scholar
|
|
106
|
Basturk O, Tang L, Hruban RH, Adsay V,
Yang Z, Krasinskas AM, Vakiani E, La Rosa S, Jang KT, Frankel WL,
et al: Poorly differentiated neuroendocrine carcinomas of the
pancreas: A clinicopathologic analysis of 44 cases. Am J Surg
Pathol. 38:437–447. 2014.PubMed/NCBI View Article : Google Scholar
|
|
107
|
Scoazec JY: Lung and digestive
neuroendocrine neoplasms. From WHO classification to biomarker
screening: Which perspectives? Ann Endocrinol (Paris). 80:163–165.
2019.PubMed/NCBI View Article : Google Scholar
|
|
108
|
George J, Lim JS, Jang SJ, Cun Y, Ozretić
L, Kong G, Leenders F, Lu X, Fernández-Cuesta L, Bosco G, et al:
Comprehensive genomic profiles of small cell lung cancer. Nature.
524:47–53. 2015.PubMed/NCBI View Article : Google Scholar
|
|
109
|
Derks JL, Leblay N, Thunnissen E, van
Suylen RJ, den Bakker M, Groen HJM, Smit EF, Damhuis R, van den
Broek EC, Chabrier A, et al: Molecular subtypes of pulmonary
large-cell neuroendocrine carcinoma predict chemotherapy treatment
outcome. Clin Cancer Res. 24:33–42. 2018.PubMed/NCBI View Article : Google Scholar
|
|
110
|
Vijayvergia N, Boland PM, Handorf E,
Gustafson KS, Gong Y, Cooper HS, Sheriff F, Astsaturov I, Cohen SJ
and Engstrom PF: Molecular profiling of neuroendocrine malignancies
to identify prognostic and therapeutic markers: A fox chase cancer
center pilot study. Br J Cancer. 115:564–570. 2016.PubMed/NCBI View Article : Google Scholar
|
|
111
|
Chen C, Notkins AL and Lan MS:
Insulinoma-associated-1: From neuroendocrine tumor marker to cancer
therapeutics. Mol Cancer Res. 17:1597–1604. 2019.PubMed/NCBI View Article : Google Scholar
|
|
112
|
Tanigawa M, Nakayama M, Taira T, Hattori
S, Mihara Y, Kondo R, Kusano H, Nakamura K, Abe Y, Ishida Y, et al:
Insulinoma-associated protein 1 (INSM1) is a useful marker for
pancreatic neuroendocrine tumor. Med Mol Morphol. 51:32–40.
2018.PubMed/NCBI View Article : Google Scholar
|
|
113
|
Fujino K, Motooka Y, Hassan WA, Ali
Abdalla MO, Sato Y, Kudoh S, Hasegawa K, Niimori-Kita K, Kobayashi
H, Kubota I, et al: Insulinoma-associated protein 1 is a crucial
regulator of neuroendocrine differentiation in lung cancer. Am J
Pathol. 185:3164–3177. 2015.PubMed/NCBI View Article : Google Scholar
|
|
114
|
Augustyn A, Borromeo M, Wang T, Fujimoto
J, Shao C, Dospoy PD, Lee V, Tan C, Sullivan JP, Larsen JE, et al:
ASCL1 is a lineage oncogene providing therapeutic targets for
high-grade neuroendocrine lung cancers. Proc Natl Acad Sci USA.
111:14788–14793. 2014.PubMed/NCBI View Article : Google Scholar
|
|
115
|
Wang H, Chen Y, Fernandez-Del Castillo C,
Yilmaz O and Deshpande V: Heterogeneity in signaling pathways of
gastroenteropancreatic neuroendocrine tumors: A critical look at
notch signaling pathway. Mod Pathol. 26:139–147. 2013.PubMed/NCBI View Article : Google Scholar
|
|
116
|
Rodriguez EF, Fite JJ, Chowsilpa S and
Maleki Z: Insulinoma-associated protein 1 immunostaining on
cytology specimens: An institutional experience. Hum Pathol.
85:128–135. 2019.PubMed/NCBI View Article : Google Scholar
|
|
117
|
Modlin IM, Drozdov I and Kidd M: The
identification of gut neuroendocrine tumor disease by multiple
synchronous transcript analysis in blood. PLoS One.
8(63364)2013.PubMed/NCBI View Article : Google Scholar
|
|
118
|
Kidd M, Drozdov I and Modlin I: Blood and
tissue neuroendocrine tumor gene cluster analysis correlate, define
hallmarks and predict disease status. Endocr Relat Cancer.
22:561–575. 2015.PubMed/NCBI View Article : Google Scholar
|
|
119
|
Genzen JR, Mohlman JS, Lynch JL, Squires
MW and Weiss RL: Laboratory-developed tests: A legislative and
regulatory review. Clin Chem. 63:1575–1584. 2017.PubMed/NCBI View Article : Google Scholar
|
|
120
|
Modlin IM, Aslanian H, Bodei L, Drozdov I
and Kidd M: A PCR blood test outperforms chromogranin A in
carcinoid detection and is unaffected by proton pump inhibitors.
Endocr Connect. 3:215–223. 2014.PubMed/NCBI View Article : Google Scholar
|
|
121
|
Liu E, Paulson S, Gulati A, Freudman J,
Grosh W, Kafer S, Wickremesinghe PC, Salem RR and Bodei L:
Assessment of NETest clinical utility in a U.S. registry-based
study. Oncologist. 24:783–790. 2019.PubMed/NCBI View Article : Google Scholar
|
|
122
|
Malczewska A, Bodei L, Kidd M and Modlin
IM: Blood mRNA measurement (NETest) for Neuroendocrine tumor
diagnosis of image-negative liver metastatic disease. J Clin
Endocrinol Metab. 104:867–872. 2019.PubMed/NCBI View Article : Google Scholar
|
|
123
|
Modlin IM, Kidd M, Malczewska A, Drozdov
I, Bodei L, Matar S and Chung KM: The NETest: The clinical utility
of multigene blood analysis in the diagnosis and management of
neuroendocrine tumors. Endocrinol Metab Clin North Am. 47:485–504.
2018.PubMed/NCBI View Article : Google Scholar
|
|
124
|
Öberg K, Califano A, Strosberg JR, Ma S,
Pape U, Bodei L, Kaltsas G, Toumpanakis C, Goldenring JR, Frilling
A and Paulson S: A meta-analysis of the accuracy of a
neuroendocrine tumor mRNA genomic biomarker (NETest) in blood. Ann
Oncol. 31:202–212. 2020.PubMed/NCBI View Article : Google Scholar
|
|
125
|
Hackeng WM, Morsink FHM, Moons LMG, Heaphy
CM, Offerhaus GJA, Dreijerink KMA and Brosens LAA: Assessment of
ARX expression, a novel biomarker for metastatic risk in pancreatic
neuroendocrine tumors, in endoscopic ultrasound fine-needle
aspiration. Diagn Cytopathol. 48:308–315. 2020.PubMed/NCBI View Article : Google Scholar
|
|
126
|
Keutgen XM, Schadde E, Pommier RF,
Halfdanarson TR, Howe JR and Kebebew E: Metastatic neuroendocrine
tumors of the gastrointestinal tract and pancreas: A surgeon's plea
to centering attention on the liver. Semin Oncol. 45:232–235.
2018.PubMed/NCBI View Article : Google Scholar
|
|
127
|
Demes M, Aszyk C, Bartsch H, Schirren J
and Fisseler-Eckhoff A: Differential miRNA-Expression as an
adjunctive diagnostic tool in neuroendocrine tumors of the lung.
Cancers (Basel). 8(38)2016.PubMed/NCBI View Article : Google Scholar
|
|
128
|
Condrat CE, Thompson DC, Barbu MG, Bugnar
OL, Boboc A, Cretoiu D, Suciu N, Cretoiu SM and Voinea SC: MiRNAs
as biomarkers in disease: Latest findings regarding their role in
diagnosis and prognosis. Cells. 9(276)2020.PubMed/NCBI View Article : Google Scholar
|
|
129
|
Roldo C, Missiaglia E, Hagan JP, Falconi
M, Capelli P, Bersani S, Calin GA, Volinia S, Liu CG, Scarpa A and
Croce CM: MicroRNA expression abnormalities in pancreatic endocrine
and acinar tumors are associated with distinctive pathologic
features and clinical behavior. J Clin Oncol. 24:4677–4684.
2006.PubMed/NCBI View Article : Google Scholar
|
|
130
|
Vicentini C, Fassan M, D'Angelo E, Corbo
V, Silvestris N, Nuovo GJ and Scarpa A: Clinical application of
microRNA testing in neuroendocrine tumors of the gastrointestinal
tract. Molecules. 19:2458–2468. 2014.PubMed/NCBI View Article : Google Scholar
|
|
131
|
Panarelli N, Tyryshkin K, Wong JJM,
Majewski A, Yang X, Scognamiglio T, Kim MK, Bogardus K, Tuschl T,
Chen YT and Renwick N: Evaluating gastroenteropancreatic
neuroendocrine tumors through microRNA sequencing. Endocr Relat
Cancer. 26:47–57. 2019.PubMed/NCBI View Article : Google Scholar
|
|
132
|
Kulke MH, Anthony LB, Bushnell DL, de
Herder WW, Goldsmith SJ, Klimstra DS, Marx SJ, Pasieka JL, Pommier
RF, Yao JC, et al: NANETS treatment guidelines: Well-differentiated
neuroendocrine tumors of the stomach and pancreas. Pancreas.
39:735–752. 2010.PubMed/NCBI View Article : Google Scholar
|
|
133
|
Reddy KB: MicroRNA (miRNA) in cancer.
Cancer Cell Int. 15(38)2015.PubMed/NCBI View Article : Google Scholar
|
|
134
|
Cives M, Simone V, Rizzo FM and Silvestris
F: NETs: organ-related epigenetic derangements and potential
clinical applications. Oncotarget. 7:57414–57429. 2016.PubMed/NCBI View Article : Google Scholar
|
|
135
|
House MG, Herman JG, Guo MZ, Hooker CM,
Schulick RD, Lillemoe KD, Cameron JL, Hruban RH, Maitra A and Yeo
CJ: Aberrant hypermethylation tumor suppressor genes in pancreatic
endocrine neoplasms. Ann Surg. 238:423–431; discussion 431-2.
2003.PubMed/NCBI View Article : Google Scholar
|
|
136
|
Campana D, Walter T, Pusceddu S, Gelsomino
F, Graillot E, Prinzi N, Spallanzani A, Fiorentino M, Barritault M,
Dall'Olio F, et al: Correlation between MGMT promoter methylation
and response to temozolomide-based therapy in neuroendocrine
neoplasms: An observational retrospective multicenter study.
Endocrine. 60:490–498. 2018.PubMed/NCBI View Article : Google Scholar
|
|
137
|
Walter T, van Brakel B, Vercherat C,
Hervieu V, Forestier J, Chayvialle JA, Molin Y, Lombard-Bohas C,
Joly MO and Scoazec JY: O6-Methylguanine-DNA methyltransferase
status in neuroendocrine tumours: Prognostic relevance and
association with response to alkylating agents. Br J Cancer.
112:523–531. 2015.PubMed/NCBI View Article : Google Scholar
|
|
138
|
Marzese DM, Hirose H and Hoon DS:
Diagnostic and prognostic value of circulating tumor-related DNA in
cancer patients. Expert Rev Mol Diagn. 13:827–844. 2013.PubMed/NCBI View Article : Google Scholar
|
|
139
|
Jänne PA, Yang JC, Kim DW, Planchard D,
Ohe Y, Ramalingam SS, Ahn MJ, Kim SW, Su WC, Horn L, et al: AZD9291
in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J
Med. 372:1689–1699. 2015.PubMed/NCBI View Article : Google Scholar
|
|
140
|
Schwarzenbach H, Hoon DS and Pantel K:
Cell-free nucleic acids as biomarkers in cancer patients. Nat Rev
Cancer. 11:426–437. 2011.PubMed/NCBI View Article : Google Scholar
|
|
141
|
Boons G, Vandamme T, Peeters M, Beyens M,
Driessen A, Janssens K, Zwaenepoel K, Roeyen G, Van Camp G and Op
de Beeck K: Cell-free DNA from metastatic pancreatic neuroendocrine
tumor patients contains tumor-specific mutations and copy number
variations. Front Oncol. 8(467)2018.PubMed/NCBI View Article : Google Scholar
|
|
142
|
Stroun M, Anker P, Maurice P, Lyautey J,
Lederrey C and Beljanski M: Neoplastic characteristics of the DNA
found in the plasma of cancer patients. Oncology. 46:318–322.
1989.PubMed/NCBI View Article : Google Scholar
|
|
143
|
Raptis L and Menard HA: Quantitation and
characterization of plasma DNA in normals and patients with
systemic lupus erythematosus. J Clin Invest. 66:1391–1399.
1980.PubMed/NCBI View Article : Google Scholar
|
|
144
|
Kalluri R and Weinberg RA: The basics of
epithelial-mesenchymal transition. J Clin Invest. 119:1420–1428.
2009.PubMed/NCBI View Article : Google Scholar
|
|
145
|
Khan MS, Tsigani T, Rashid M, Rabouhans
JS, Yu D, Luong TV, Caplin M and Meyer T: Circulating tumor cells
and EpCAM expression in neuroendocrine tumors. Clin Cancer Res.
17:337–345. 2011.PubMed/NCBI View Article : Google Scholar
|
|
146
|
Khan MS, Kirkwood A, Tsigani T,
Garcia-Hernandez J, Hartley JA, Caplin ME and Meyer T: Circulating
tumor cells as prognostic markers in neuroendocrine tumors. J Clin
Oncol. 31:365–372. 2013.PubMed/NCBI View Article : Google Scholar
|
|
147
|
Khan MS, Kirkwood AA, Tsigani T, Lowe H,
Goldstein R, Hartley JA, Caplin ME and Meyer T: Early changes in
circulating tumor cells are associated with response and survival
following treatment of metastatic neuroendocrine neoplasms. Clin
Cancer Res. 22:79–85. 2016.PubMed/NCBI View Article : Google Scholar
|
|
148
|
Childs A, Vesely C, Ensell L, Lowe H,
Luong TV, Caplin ME, Toumpanakis C, Thirlwell C, Hartley JA and
Meyer T: Expression of somatostatin receptors 2 and 5 in
circulating tumour cells from patients with neuroendocrine tumours.
Br J Cancer. 115:1540–1547. 2016.PubMed/NCBI View Article : Google Scholar
|
|
149
|
Krenning EP, Kwekkeboom DJ, Bakker WH,
Breeman WA, Kooij PP, Oei HY, van Hagen M, Postema PT, de Jong M,
Reubi JC, et al: Somatostatin receptor scintigraphy with
[111In-DTPA-d-Phe1]- and [123I-Tyr3]-octreotide: The Rotterdam
experience with more than 1000 patients. Eur J Nucl Med.
20:716–731. 1993.PubMed/NCBI View Article : Google Scholar
|
|
150
|
Bombardieri E, Ambrosini V, Aktolun C,
Baum RP, Bishof-Delaloye A, Del Vecchio S, Maffioli L, Mortelmans
L, Oyen W, Pepe G, et al: 111In-pentetreotide scintigraphy:
Procedure guidelines for tumour imaging. Eur J Nucl Med Mol
Imaging. 37:1441–1448. 2010.PubMed/NCBI View Article : Google Scholar
|
|
151
|
Hope TA, Bergsland EK, Bozkurt MF, Graham
M, Heaney AP, Herrmann K, Howe JR, Kulke MH, Kunz PL, Mailman J, et
al: Appropriate use criteria for somatostatin receptor PET imaging
in neuroendocrine tumors. J Nucl Med. 59:66–74. 2018.PubMed/NCBI View Article : Google Scholar
|
|
152
|
Eychenne R, Bouvry C, Bourgeois M, Loyer
P, Benoist E and Lepareur N: Overview of radiolabeled somatostatin
analogs for cancer imaging and therapy. Molecules.
25(4012)2020.PubMed/NCBI View Article : Google Scholar
|
|
153
|
Ivanidze J, Roytman M, Sasson A, Skafida
M, Fahey TJ III, Osborne JR and Dutruel SP: Molecular imaging and
therapy of somatostatin receptor positive tumors. Clin Imaging.
56:146–154. 2019.PubMed/NCBI View Article : Google Scholar
|
|
154
|
Graham MM, Gu X, Ginader T, Breheny P and
Sunderland JJ: 68Ga-DOTATOC imaging of neuroendocrine tumors: A
systematic review and metaanalysis. J Nucl Med. 58:1452–1458.
2017.PubMed/NCBI View Article : Google Scholar
|
|
155
|
Sadowski SM, Neychev V, Millo C, Shih J,
Nilubol N, Herscovitch P, Pacak K, Marx SJ and Kebebew E:
Prospective study of 68Ga-DOTATATE positron emission
tomography/computed tomography for detecting
gastro-entero-pancreatic neuroendocrine tumors and unknown primary
sites. J Clin Oncol. 34:588–597. 2016.PubMed/NCBI View Article : Google Scholar
|
|
156
|
Deroose CM, Hindié E, Kebebew E, Goichot
B, Pacak K, Taïeb D and Imperiale A: Molecular imaging of
gastroenteropancreatic neuroendocrine tumors: Current status and
future directions. J Nucl Med. 57:1949–1956. 2016.PubMed/NCBI View Article : Google Scholar
|
|
157
|
Miederer M, Seidl S, Buck A, Scheidhauer
K, Wester HJ, Schwaiger M and Perren A: Correlation of
immunohistopathological expression of somatostatin receptor 2 with
standardised uptake values in 68Ga-DOTATOC PET/CT. Eur J Nucl Med
Mol Imaging. 36:48–52. 2009.PubMed/NCBI View Article : Google Scholar
|
|
158
|
Kratochwil C, Stefanova M, Mavriopoulou E,
Holland-Letz T, Dimitrakopoulou-Strauss A, Afshar-Oromieh A, Mier
W, Haberkorn U and Giesel FL: SUV of [68Ga]DOTATOC-PET/CT Predicts
Response Probability of PRRT in neuroendocrine tumors. Mol Imaging
Biol. 17:313–318. 2015.PubMed/NCBI View Article : Google Scholar
|
|
159
|
Strosberg J, El-Haddad G, Wolin E,
Hendifar A, Yao J, Chasen B, Mittra E, Kunz PL, Kulke MH, Jacene H,
et al: Phase 3 trial of (177)Lu-Dotatate for Midgut Neuroendocrine
tumors. N Engl J Med. 376:125–135. 2017.PubMed/NCBI View Article : Google Scholar
|
|
160
|
Nicolas G, Mansi R, Vomstein S, Kaufmann
J, Bouterfa H, Maecke H, Wild D and Fani M: Wider safety window
with radiolabeled somatostatin receptor antagonists over agonists.
J Nucl Med. 56 (Suppl 3)(S335)2015.
|
|
161
|
Fani M, Nicolas GP and Wild D:
Somatostatin receptor antagonists for imaging and therapy. J Nucl
Med. 58 (Suppl 2):61S–66S. 2017.PubMed/NCBI View Article : Google Scholar
|
|
162
|
Nock BA, Kaloudi A, Lymperis E, Giarika A,
Kulkarni HR, Klette I, Singh A, Krenning EP, de Jong M, Maina T and
Baum RP: Theranostic perspectives in prostate cancer with the
Gastrin-Releasing peptide receptor antagonist NeoBOMB1: Preclinical
and first clinical results. J Nucl Med. 58:75–80. 2017.PubMed/NCBI View Article : Google Scholar
|
|
163
|
Garin E, Le Jeune F, Devillers A, Cuggia
M, de Lajarte-Thirouard AS, Bouriel C, Boucher E and Raoul JL:
Predictive value of 18F-FDG PET and somatostatin receptor
scintigraphy in patients with metastatic endocrine tumors. J Nucl
Med. 50:858–864. 2009.PubMed/NCBI View Article : Google Scholar
|
|
164
|
Ezziddin S, Adler L, Sabet A, Pöppel TD,
Grabellus F, Yüce A, Fischer HP, Simon B, Höller T, Biersack HJ and
Nagarajah J: Prognostic stratification of metastatic
gastroenteropancreatic neuroendocrine neoplasms by 18F-FDG PET:
Feasibility of a metabolic grading system. J Nucl Med.
55:1260–1266. 2014.PubMed/NCBI View Article : Google Scholar
|
|
165
|
Chan DL, Pavlakis N, Schembri GP, Bernard
EJ, Hsiao E, Hayes A, Barnes T, Diakos C, Khasraw M, Samra J, et
al: Dual somatostatin receptor/FDG PET/CT imaging in metastatic
neuroendocrine tumours: Proposal for a novel grading scheme with
prognostic significance. Theranostics. 7:1149–1158. 2017.PubMed/NCBI View Article : Google Scholar
|
|
166
|
Hindié E: The netpet score: Combining FDG
and somatostatin receptor imaging for optimal management of
patients with metastatic well-differentiated neuroendocrine tumors.
Theranostics. 7:1159–1163. 2017.PubMed/NCBI View Article : Google Scholar
|
|
167
|
Pavel M, O'Toole D, Costa F, Capdevila J,
Gross D, Kianmanesh R, Krenning E, Knigge U, Salazar R, Pape UF, et
al: ENETS consensus guidelines update for the management of distant
metastatic disease of intestinal, pancreatic, bronchial
neuroendocrine neoplasms (NEN) and NEN of unknown primary site.
Neuroendocrinology. 103:172–185. 2016.PubMed/NCBI View Article : Google Scholar
|
|
168
|
Panagiotidis E, Alshammari A, Michopoulou
S, Skoura E, Naik K, Maragkoudakis E, Mohmaduvesh M, Al-Harbi M,
Belda M, Caplin ME, et al: Comparison of the impact of
68Ga-DOTATATE and 18F-FDG PET/CT on clinical management in patients
with neuroendocrine tumors. J Nucl Med. 58:91–96. 2017.PubMed/NCBI View Article : Google Scholar
|
|
169
|
Nilica B, Waitz D, Stevanovic V, Uprimny
C, Kendler D, Buxbaum S, Warwitz B, Gerardo L, Henninger B,
Virgolini I and Rodrigues M: Direct comparison of (68)Ga-DOTA-TOC
and (18)F-FDG PET/CT in the follow-up of patients with
neuroendocrine tumour treated with the first full peptide receptor
radionuclide therapy cycle. Eur J Nucl Med Mol Imaging.
43:1585–1592. 2016.PubMed/NCBI View Article : Google Scholar
|
|
170
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumours:
Revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009.PubMed/NCBI View Article : Google Scholar
|
|
171
|
Ferté C, Fernandez M, Hollebecque A,
Koscielny S, Levy A, Massard C, Balheda R, Bot B, Gomez-Roca C,
Dromain C, et al: Tumor growth rate is an early indicator of
antitumor drug activity in phase I clinical trials. Clin Cancer
Res. 20:246–252. 2014.PubMed/NCBI View Article : Google Scholar
|
|
172
|
Jain RK, Lee JJ, Ng C, Hong D, Gong J,
Naing A, Wheler J and Kurzrock R: Change in tumor size by RECIST
correlates linearly with overall survival in phase I oncology
studies. J Clin Oncol. 30:2684–2690. 2012.PubMed/NCBI View Article : Google Scholar
|