Introduction
The number of teenagers who exhibit myopia and
myopic astigmatism is increasing each year. Numerous patients
choose soft contact lenses (SCLs) to manage the problem of
refractive error. The normal physiology of the ocular surface
(1,2), including changes in the corneal
epithelium (3,4) and endothelium (5,6), can
be affected by direct contact between the contact lens and the
cornea. Numerous previous studies have suggested that long-term SCL
wear can decrease oxygen uptake (1), induce cell death (7) and lead to corneal epithelial thinning
(8-10),
which may become more obvious with extended SCL wear. The corneal
epithelial thickness can increase following discontinuation of SCL
wear; however, the corneal epithelial thickness is unable to reach
the normal range exhibited by people without SCL wear (11). A previous study (12) demonstrated that the corneal
epithelial thickness reached stability following discontinued wear
of SCLs within 2 weeks; nevertheless, individual variation should
not be discounted.
In recent years, methods of corneal refractive
surgery have been improving. Corneal refractive surgery provided
another option for the correction of visual acuity, particularly in
myopic patients with the experience of SCL wear. Small incision
lenticule extraction (SMILE) is a relatively new surgical method of
corneal refractive surgery, which realizes the flapless surgical
mode, leaving the epithelium and the Bowman's layer undamaged
except for the small side cut incision to extract the lenticule
(13). After SMILE, corneal
biomechanical properties exhibit greater stability. Reinstein et
al (14) demonstrate that the
postoperative total stromal tensile strength following SMILE is
higher than both photorefractive keratecotomy (PRK) and laser in
situ keratomileusis (LASIK). Subepithelial stromal plexus
damage and the postoperative inflammatory reaction are decreased
and dry eye symptoms are less pronounced (15,16).
This surgical method has advantages in terms of safety,
effectiveness, good predictability and stability (13,17).
Numerous myopic patients with experience of wearing SCLs have
chosen corneal refractive surgery to obtain satisfactory visual
acuity. The purpose of the present study was to investigate
epithelial thickness changes after SMILE following long-term wear
of SCLs, as well as the influence of SCL wear on surgical
outcomes.
Previous studies have been performed to evaluate the
central region of the cornea (18,19).
In the present study, anterior segment optical coherence tomography
imaging was applied to determine corneal epithelial thickness in
nine zones across a 5-mm corneal diameter, which demonstrated
higher reproducibility and accuracy in both normal and
postoperative eyes.
Patients and methods
Patients
This retrospective observational study included 57
eyes of 30 patients (16 male and 14 female; mean age 25.90±5.90
years; range 16-34 years) who were scheduled for SMILE as treatment
for myopia or myopia astigmatism at The First Affiliated Hospital
of Soochow University (Suzhou, China) between June 2017 and April
2018. A complete ophthalmic examination was performed to screen for
corneal abnormalities and determine the eligibility of the patients
for refractive surgery. The inclusion criteria were: Age >18
years; spherical equivalent refraction converted by preoperative
optometry of -2.00 to -6.00 diopters; intraocular pressure ranging
from 10-21 mmHg; no history of hard contact lens wear; and a normal
corneal topograghy examination. Patients with ocular pathological
conditions such as corneal opacity and keratoconus were excluded.
Additionally, patients with other ocular diseases and systemic
organic diseases affecting the recovery from surgery were excluded
from the study.
A previous study found that a 2-week contact
lens-free period seemed to be adequate for the cornea to stabilize
(9). The present study aimed to
elucidate the effects of long-term SCL wear on corneal epithelial
thickness; therefore, 1 year was chosen as the long-term period.
According to the duration of SCL wear, the patients were divided
into three groups. Patients who had never worn SCLs were included
into group A, while the others who had worn SCLs for <1 year
were in group B and those who had worn SCLs for >1 year were in
group C. All patients were asked to stop wearing SCLs at least 2
weeks prior to the surgery. This retrospective study was approved
by the Ethics Committee of The First Affiliated Hospital of Soochow
University, and all patients provided consent at the time of the
surgery.
Corneal epithelial thickness
measurement
The corneal epithelial thickness data were obtained
preoperatively and then at 1 week, and 1, 3 and 6 months
postoperatively using the RTVue-100 anterior segment optical
coherence tomography system (Optovue, Inc.). Each measurement was
performed by one experienced technician in a room where light
levels were reduced by half. All patients were forbidden from using
any eye drops for 2 h prior to the measurements.
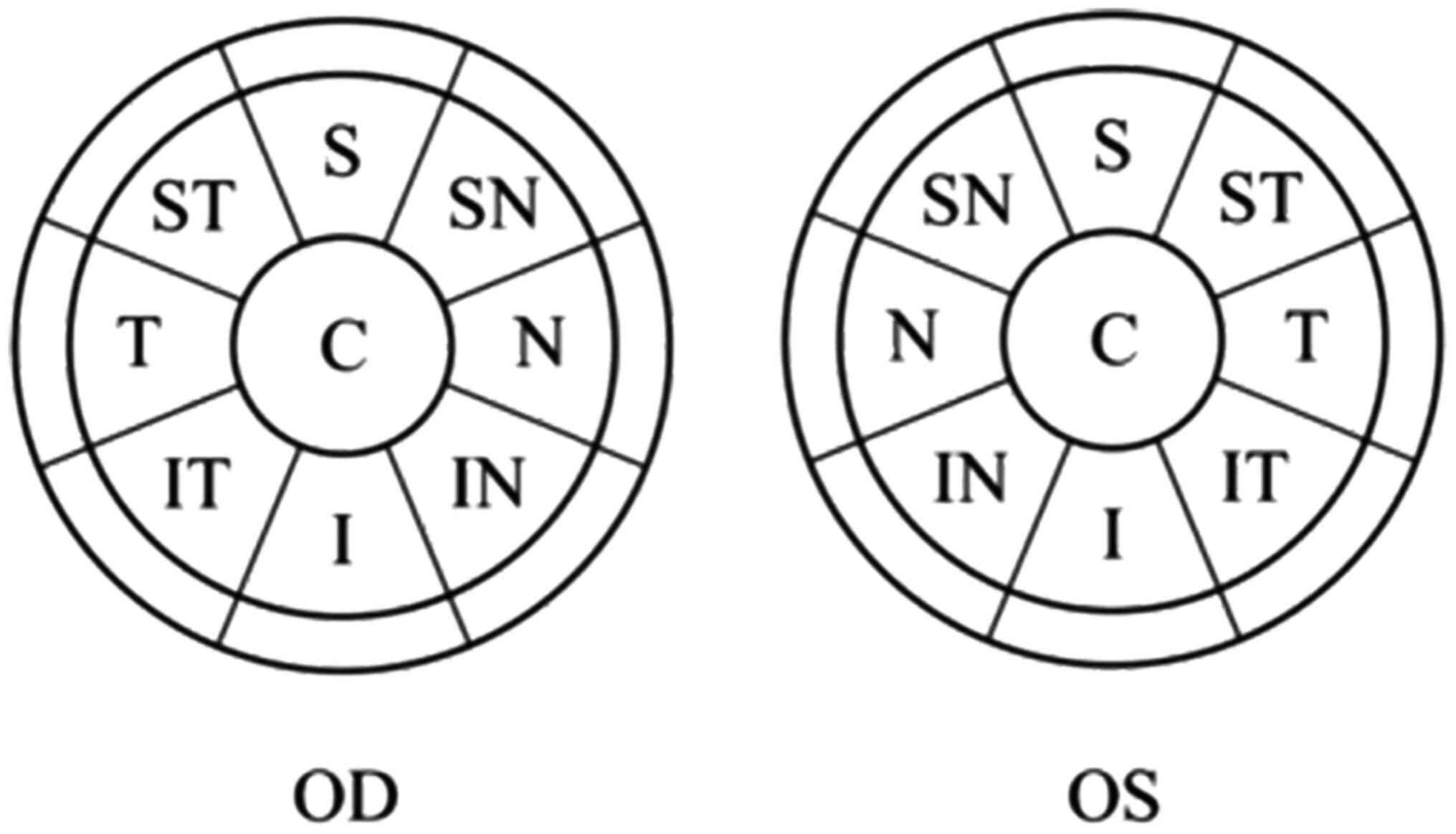
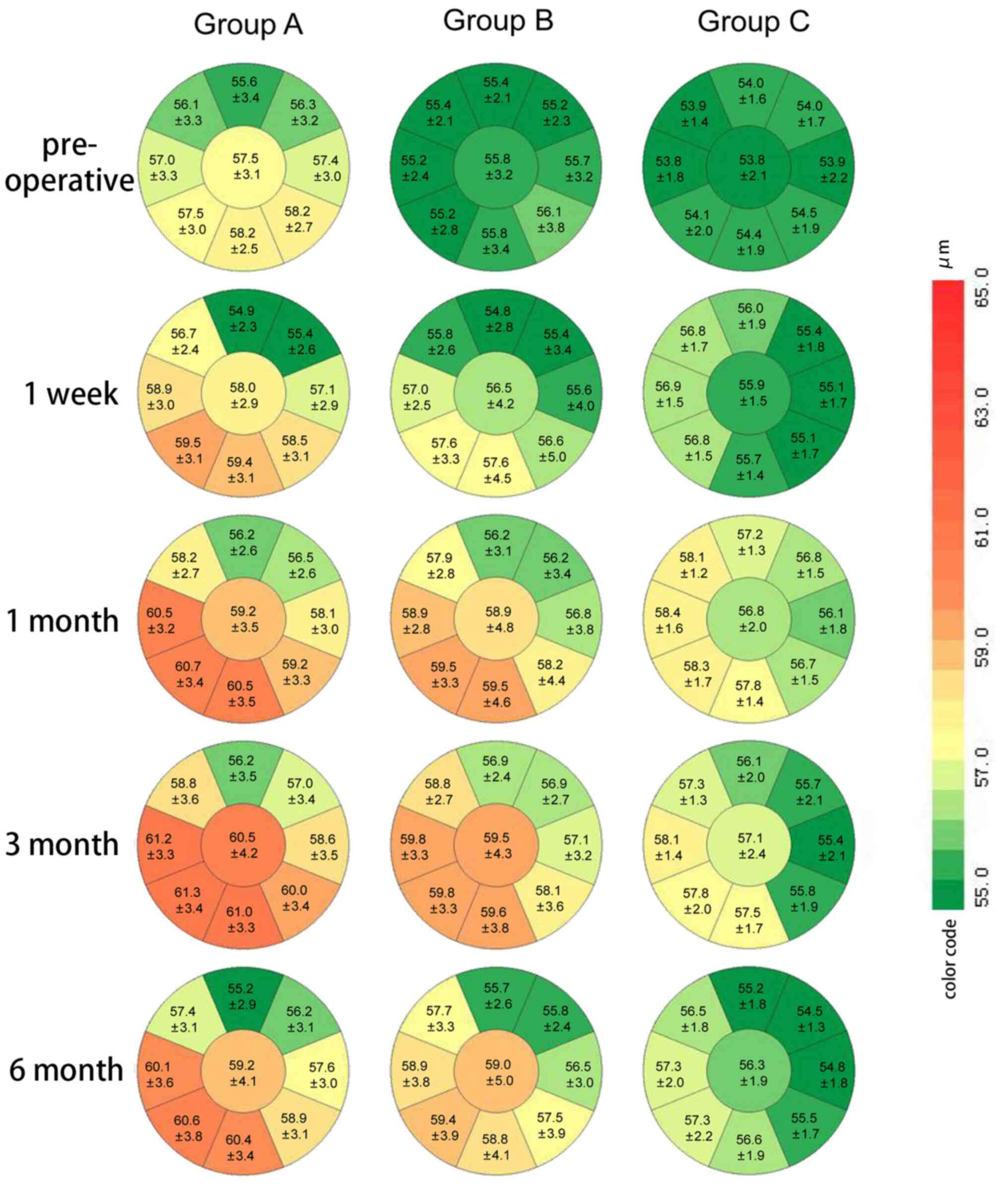
The anterior segment optical coherence tomography
obtained the epithelial thickness of a circular region over a 6-mm
diameter centered at the pupil center. The maps were divided into 3
zones by the annular rings: Central zone (2-mm diameter),
paracentral zone (2- to 5-mm diameter) and mid-peripheral zone (5-
to 6-mm diameter). The paracentral and mid-peripheral zones were
each divided into the following 8 sectors: Superior, superonasal,
nasal, inferonasal, inferior, inferotemporal, temporal and
superotemporal (Fig. 1). Finally,
epithelial maps were created and left eyes maps were mirrored
vertically so as to make them comparable with right eyes. The
present study analyzed the corneal epithelial thickness of 9
sectors over the central and paracentral zones, as well as the
maximum-minimum (max-min) and standard deviation (SD) values of
corneal epithelial thickness in the central 5-mm diameter (due to
the covering of eyelids, peripheral data were not accurate.).
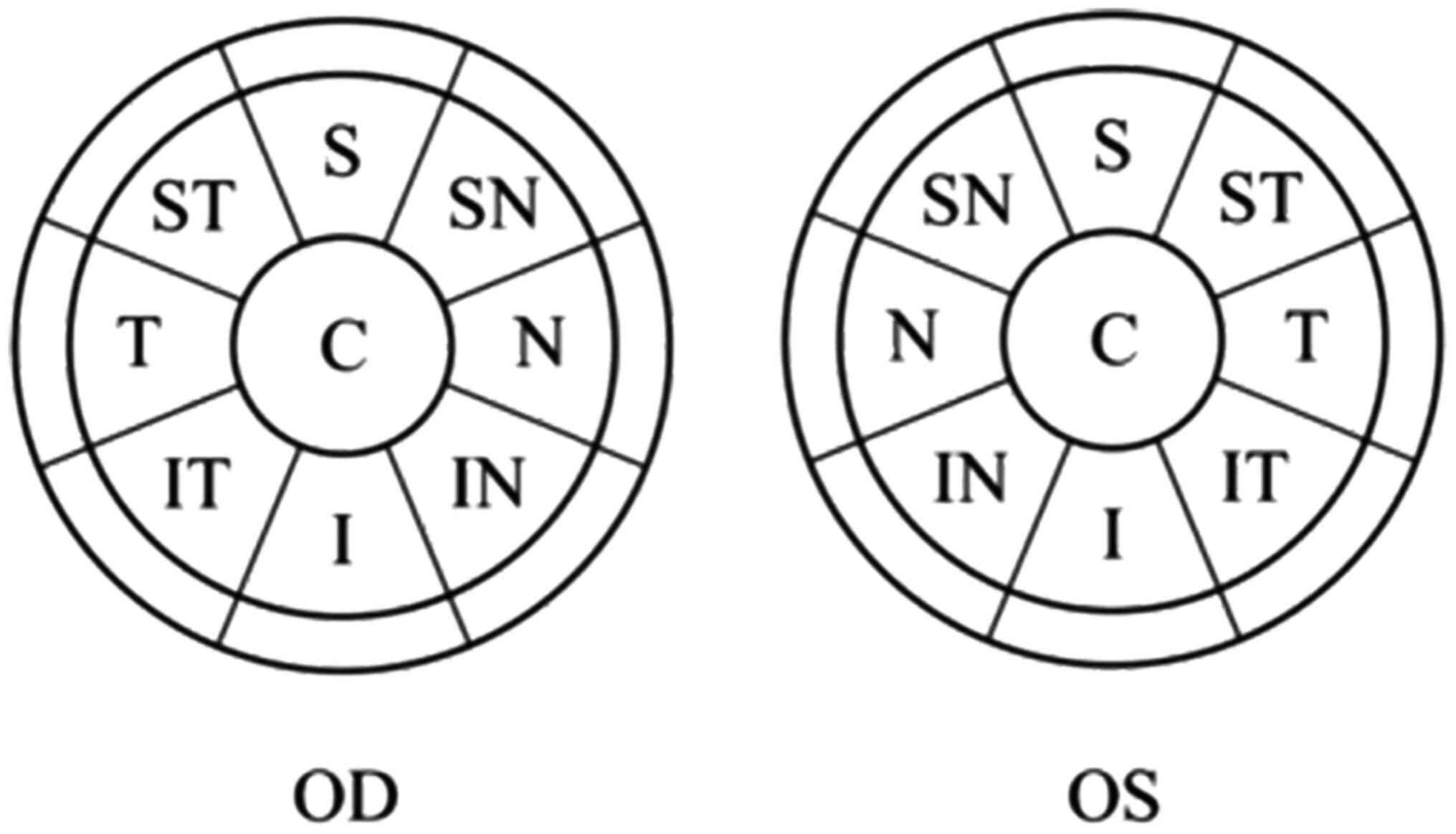 | Figure 1Zoning of corneal epithelium (diameter
of central 6 mm). C, central; S, superior; SN, superonasal; N,
nasal; IN, inferonasal; I, inferior; IT, inferotemporal; T,
temporal; ST, superotemporal; OD, oculus dexter; OS, oculus
sinister. |
Corneal topography measurement
Corneal topography measurements were acquired using
a Sirius Corneal Topographer (CSO, Inc.). Three consecutive scans
were taken and the best quality scan was selected for further
analysis. For this, the Scheimpflug image area needed to be
>90%, the centration positioning needed to be >90% and the
Placido disk needed to cover an area of >90%. The total higher
order aberrations, spherical aberrations and coma aberrations were
noted for analysis.
Surgical technique
All myopic operations were performed by one
experienced surgeon (from Department of Ophthalmology, The First
Affiliated Hospital of Soochow University). Preoperative medication
included topical 0.5% levofloxacin (Santen Pharmaceutical Co.,
Ltd.) three times for 3 days.
All SMILE procedures were performed by VisuMax
500-kHz femtosecond laser (Carl Zeiss AG). The diameter of the cap
was 7.3-7.5 mm (7.48±0.05 mm) and the intended cap thickness was
120 µm. A 3-mm incision was made at the 90˚ meridian to extract the
lenticule and the side-cut angle was 90˚. The optical zone diameter
was 6.3-6.8 mm (6.60±0.13 mm). The maximum thickness of the
lenticule was 59-135 µm (108.5±17.9 µm) and the lenticule side-cut
angle was 90˚. The data were described as mean ± SD.
Postoperative medications included topical
tobramycin dexamethason (Novartis International AG) four times for
30 min after surgery, 0.5% levofloxacin (Santen Pharmaceutical Co.,
Ltd.) four times every day for 7 days, 0.1% fluorometholone (Santen
Pharmaceutical Co., Ltd.) four times every day, which decreased one
time each week until once a day for one week. Patients were
followed up at postoperative week 1, and months 1, 3 and 6.
Uncorrected distance visual acuity (UDVA), manifest refraction and
intraocular pressure (IOP) were measured, and anterior segment
optical coherence tomography and corneal topography were performed
at every visit.
Statistical analysis
SPSS for Windows software (version 17.0; SPSS, Inc.)
was used for statistical analysis. Preoperative examinations among
groups were analyzed by one-way ANOVA followed by Bonferroni's
correction. The corneal aberrations within groups, the epithelial
thickness and the difference in epithelial thickness, the corneal
aberrations and the difference in corneal aberrations and the
max-min and SD values of corneal epithelial thickness across a 5-mm
diameter among three groups were compared with a two-way mixed
ANOVA followed by Bonferroni's correction. Kruskal-Wallis H test
was used to analyze UDVA and spherical equivalent among three
groups. P<0.05 was considered to indicate a significant
difference.
Results
Study population and
characteristics
The study cohort consisted of 30 patients with 57
eyes undergoing SMILE for myopia correction. A total of 8 eyes were
treated in group B in patients who had worn one-day disposable
hydrogel SCLs (Johnson & Johnson) and 9 eyes in patients who
had worn monthly disposable hydrogel SCLs (Johnson & Johnson or
Bausch & Lomb). A total of 8 eyes were treated in group C in
patients who had worn one-day disposable hydrogel SCLs (Johnson
& Johnson) and 10 eyes in patients who had worn monthly
disposable hydrogel SCLs (Johnson & Johnson or Bausch &
Lomb). The ratio of daily and monthly disposable lens in group B
was consistent with that in group C. The mean age, preoperative
spherical equivalent refractive power and preoperative epithelial
thickness of the central 5-mm zone were similar among the three
groups. There were no statistically significant differences in
baseline measurements among the three groups, except epithelial
thickness (P<0.05). The preoperative mean corneal epithelial
thickness was thinner in group C than in group A (P<0.05),
whereas no significant difference in preoperative epithelial
thickness was observed in group B compared with groups A and C
(P>0.05) (Table I).
 | Table IPreoperative comparative data for all
three study groupsa. |
Table I
Preoperative comparative data for all
three study groupsa.
| Parameters | Group A | Group B | Group C | F-value | P-value |
|---|
| Eyes, n | 22 | 17 | 18 | - | - |
| Age, years | 23.55±6.46 | 26.78±5.07 | 28.30±4.16 | 2.156 | 0.135 |
| Sphere, D | -4.25±1.10 | -4.43±1.12 | -4.61±1.15 | 0.511 | 0.603 |
| Cylinder, Dcyl | -0.80±0.37 | -0.75±0.40 | -0.57±0.55 | 1.407 | 0.254 |
| SE, D | -4.65±1.11 | -4.80±1.13 | -4.90±1.08 | 0.259 | 0.772 |
| ET, µm | 57.10±2.90 | 55.52±2.59 | 54.05±1.71 | 7.462 | 0.001b |
Comparison of visual acuity and
manifest refraction
Visual acuity values (in logMAR) at postoperative
week 1, and months 1, 3 and 6 were similar among the three groups.
Analysis with the Kruskal-Wallis H test revealed no statistically
significant differences in UDVA among the three groups at all
postoperative time points (P>0.05; Table II).
 | Table IIComparative data of UDVA and SE among
three groupsa. |
Table II
Comparative data of UDVA and SE among
three groupsa.
| Parameters | Time | Group A (n=22) | Group B (n=17) | Group C (n=18) | U | P-value |
|---|
| UDVA, logMAR | 1 week
postoperative | -0.05±0.06 | -0.05±0.06 | -0.04±0.06 | 0.402 | 0.818 |
| | 1 month
postoperative | -0.06±0.06 | -0.05±0.06 | -0.06±0.07 | 0.475 | 0.789 |
| | 3 months
postoperative | -0.05±0.05 | -0.04±0.08 | -0.04±0.04 | 0.142 | 0.932 |
| | 6 months
postoperative | -0.09±0.07 | -0.07±0.06 | -0.04±0.07 | 4.018 | 0.134 |
| SE, D | 1 week
postoperative | 0.05±0.30 | 0.07±0.49 | -0.20±0.43 | 2.978 | 0.226 |
| | 1 month
postoperative | 0.01±0.42 | 0.10±0.39 | 0.19±0.26 | 1.696 | 0.428 |
| | 3 months
postoperative | 0.03±0.35 | 0.05±0.37 | -0.13±0.46 | 1.637 | 0.441 |
| | 6 months
postoperative | 0.02±0.28 | 0.05±0.49 | 0.02±0.28 | 0.103 | 0.950 |
Spherical equivalent was compared at postoperative
week 1, and months 1, 3 and 6 among the three groups. Analysis with
the Kruskal-Wallis H test revealed no statistically significant
differences in spherical equivalent among the three groups at each
pair of consecutive time points (P>0.05) (Table II).
Epithelial thickness analysis
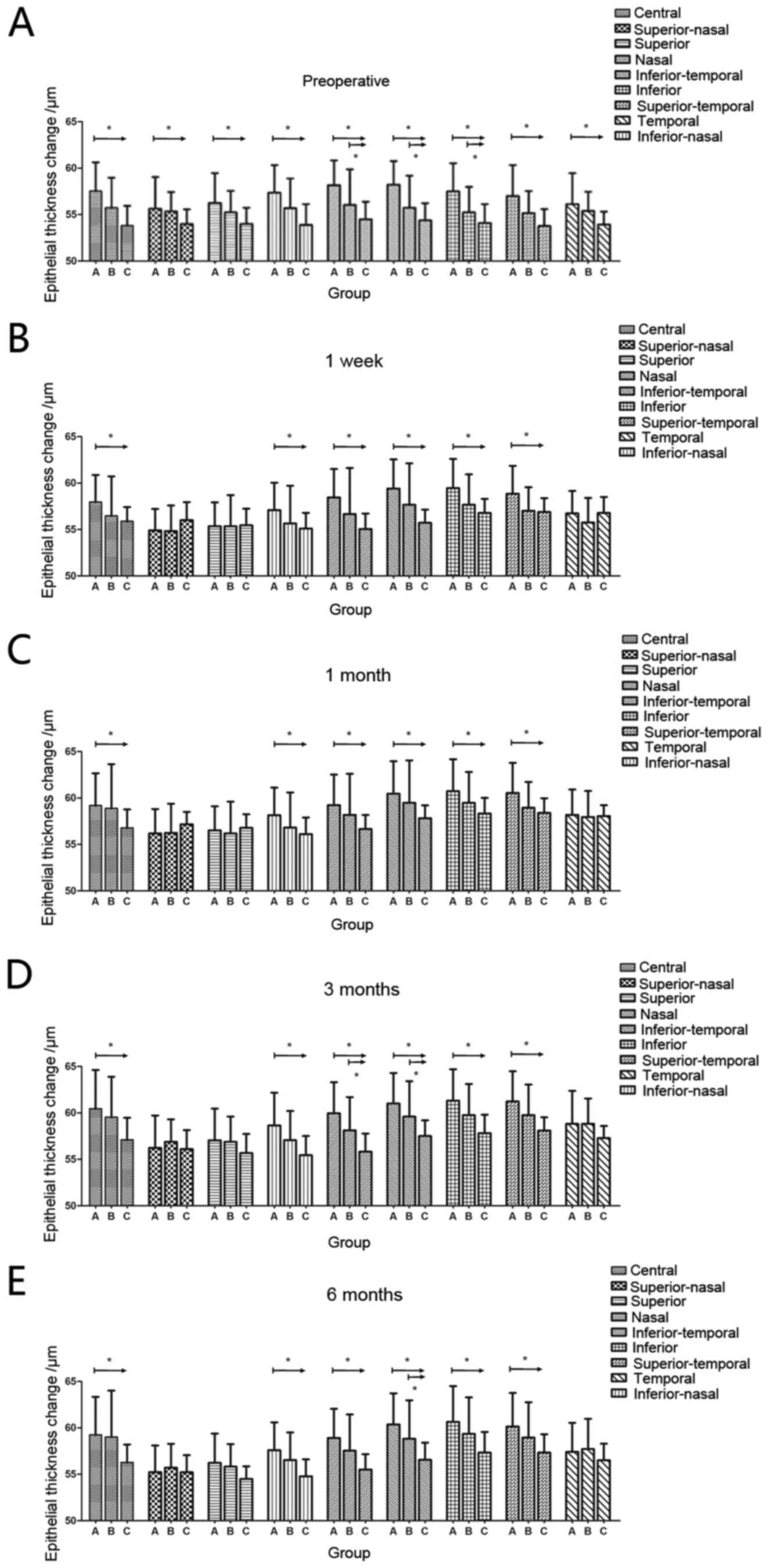
The preoperative superior epithelial thickness was
thinner than the preoperative inferior epithelial thickness of the
nine sectors in group A (FA=15.669, P<0.01;
t=-2.614, P<0.05); by contrast, there were no
statistically significant differences in epithelial thickness of
the nine sectors in groups B or C (FB=0.965,
P=0.395; FC=1.724, P=0.151). Preoperatively, the
corneal epithelial thicknesses in the inferonasal, inferior and
inferotemporal sectors were thinner in group B than in group A
(P<0.05); the epithelial thicknesses of all nine sectors were
thinner in group C than in group A (P<0.05; Fig. 2).
At postoperative week 1 and month 1, the epithelial
thicknesses in the central, nasal, inferonasal, inferior,
inferotemporal and temporal segments were thinner in group C than
in group A (P<0.05). At postoperative month 3, the epithelial
thicknesses in the central, nasal, inferonasal, inferior,
inferotemporal and temporal regions were significantly thinner in
group C than in group A (P<0.05); the inferonasal and inferior
regions were thinner in group C than in group B. At postoperative
month 6, the epithelial thicknesses in the central, nasal,
inferonasal, inferior, inferotemporal and temporal segments were
significantly thinner in group C than in group A (P<0.05); the
epithelial thicknesses in the inferior segment were thinner in
group C than in group B (Fig.
2).
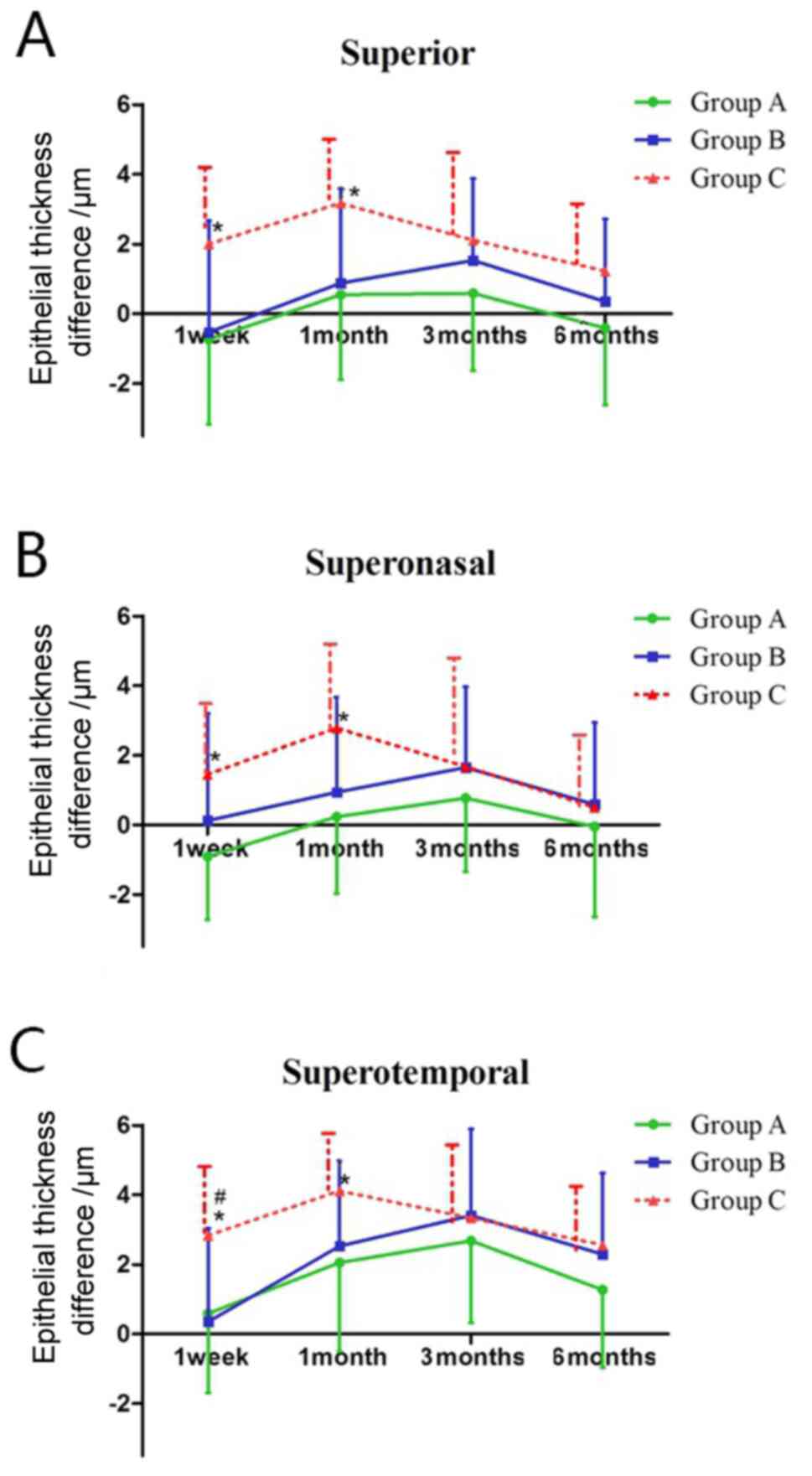
In the superior and superonasal regions of the
cornea, the change in epithelial thickness at postoperative week 1
and month 1 was greater in group C than in group A (P<0.05) In
the superotemporal region, the change in epithelial thickness was
greater in group C than in group A at postoperative week 1 and
month 1 (P<0.05); it was also greater in group C than in group B
at postoperative week 1 (P<0.05; Fig. 3).
It should be noted that at all examined time points,
the epithelial thickness in the central, nasal, inferonasal,
inferior, inferotemporal and temporal segments was less in group C
than in group A, but in the superior, superotemporal and
superonasal zones had no statistically significant difference
between group A and group C at all postoperative time points which
the epithelial thickness difference of the three zones was more in
group C than in group A at postoperative week 1 and month 1
(Fig. 2).
Uniformity of epithelial
thickness
Table III shows
the max-min values and SDs of epithelial thickness within the
central 5-mm zone for the examined time points, compared among the
three groups. Statistically significant differences were present in
the max-min values among the three groups at postoperative week 1,
month 3 and 6 (P<0.05). Differences were also observed in SD
values among the three groups at all postoperative time points
except postoperative month 1; the max-min value and SD in group C
were lower than those in group A at postoperative week 1, month 3
and 6 (P<0.05; Table III).
 | Table IIIComparative data of corneal
epithelial map within central 5-mm uniformity indices among three
groupsa. |
Table III
Comparative data of corneal
epithelial map within central 5-mm uniformity indices among three
groupsa.
| Parameters | Group A (n=22) | Group B (n=17) | Group C (n=18) |
|---|
| Preoperative | | | |
|
Max-min,
µm | 6.36±1.68 | 5.47±2.45 | 5.06±0.80 |
|
SDb | 1.51±0.45 | 1.27±0.68 |
1.10±0.22c |
| 1 week
postoperative | | | |
|
Max-min,
µmb | 9.82±2.32 | 8.82±3.13 |
7.83±1.50c |
|
SDb | 2.39±0.72 | 2.14±0.83 |
1.76±0.29c |
| 1 month
postoperative | | | |
|
Max-min,
µm | 9.77±2.99 | 9.71±3.58 | 8.33±1.81 |
|
SD | 2.42±0.71 | 2.28±0.58 | 1.90±0.37 |
| 3 months
postoperative | | | |
|
Max-min,
µmd | 10.77±2.69 | 9.53±2.72 |
8.11±1.57c |
|
SDb | 2.58±0.64 | 2.22±0.61 |
2.04±0.41c |
| 6 months
postoperative | | | |
|
Max-min,
µmb | 10.82±3.00 | 9.76±3.49 |
8.22±1.73c |
|
SDd | 2.70±0.75 | 2.31±0.79 |
1.96±0.34c |
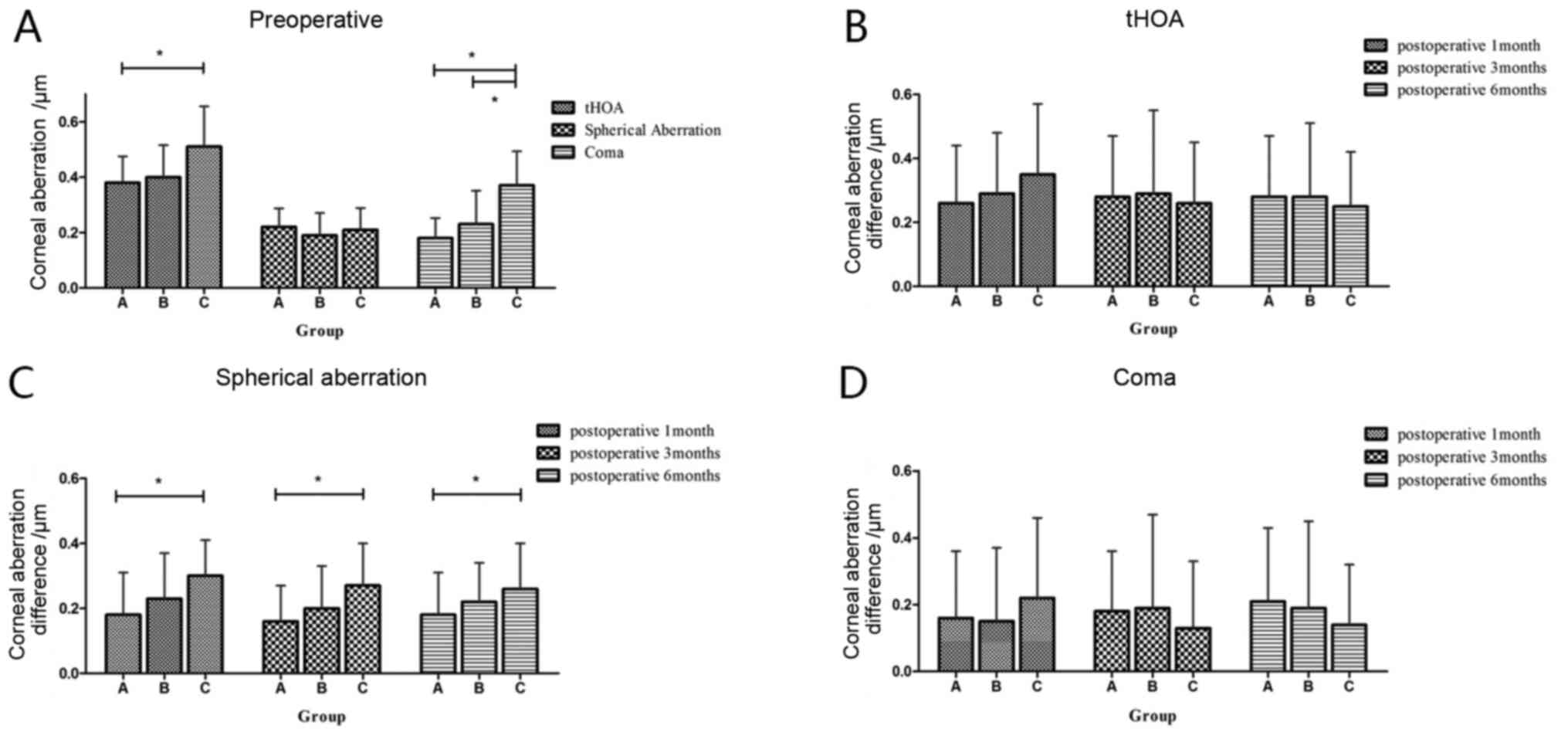
Corneal aberrations analysis
The total higher-order aberrations of the three
groups were increased postoperatively, compared with preoperatively
(P<0.05). Preoperatively and at postoperative months 1, 3 and 6,
the total higher-order aberrations were greater in group C than in
group A (P<0.05). At postoperative month 1 and 3, the total
higher-order aberrations were greater in group C than group B
(P<0.05). However, there were no statistically significant
differences in the numbers of total higher-order aberrations
difference among the three groups after surgery (P>0.05).
Postoperatively, spherical aberrations were
increased among the three groups, compared with preoperative
measurements (P<0.05; Table
IV). Preoperatively and at postoperative month 1, no
statistically significant differences were found in spherical
aberrations among the three groups (P>0.05). However, at
postoperative months 3 and 6, spherical aberrations were greater in
group C than group A (P<0.05). At postoperative 1 month, the
change in spherical aberrations was greater in group C than in
group A (P<0.05). At all time points postoperatively, the change
in spherical aberrations was greater in group C than in groups A
(P<0.05).
 | Table IVComparative data of corneal
aberrations among three groupsa. |
Table IV
Comparative data of corneal
aberrations among three groupsa.
| Aberrations | Time | Group A (n=22) | Group B (n=17) | Group C (n=18) |
|---|
| tHOA |
Preoperativeb |
0.38±0.10c | 0.40±0.12 | 0.51±0.15 |
| | 1 month
postoperatived |
0.64±0.15c,e |
0.69±0.17c,e |
0.85±0.24e |
| | 3 months
postoperativeb |
0.65±0.15c,e |
0.69±0.22c,e |
0.78±0.20e |
| | 6 months
postoperativeb |
0.65±0.18c,e |
0.68±0.22e |
0.76±0.18e |
| Spherical
aberration | Preoperative | 0.22±0.07 | 0.19±0.08 | 0.21±0.08 |
| | 1 month
postoperative |
0.39±0.12e |
0.42±0.17e |
0.48±0.13e |
| | 3 months
postoperativeb |
0.37±0.10c,e |
0.39±0.15e |
0.48±0.12e |
| | 6 months
postoperativeb |
0.38±0.12c,e |
0.41±0.16e |
0.47±0.12e |
| Coma |
Preoperativef |
0.18±0.07c |
0.23±0.12c | 0.37±0.12 |
| | 1 month
postoperativef |
0.35±0.17c |
0.38±0.21c |
0.61±0.22e |
| | 3 months
postoperatived |
0.36±0.15c,e |
0.42±0.24c |
0.51±0.18e |
| | 6 months
postoperatived |
0.39±0.19c |
0.42±0.21c,e |
0.51±0.17e |
Coma aberrations in group A at postoperative month
3, in group B at postoperative month 6, as well as in group C at
postoperative at all time points, were greater than preoperative
values (P<0.05; Table IV). At
all examined time points, coma aberrations were greater in group C
than in groups A and B (P<0.05). Postoperative changes in coma
aberrations tended to differ among the three groups, although these
differences were not statistically significant (P>0.05; Table IV; Fig.
4).
No postoperative complications (e.g., refraction
regression, epithelial defects or diffuse lamellar keratitis) were
observed during the first 6 months postoperatively in any of the
eyes.
Discussion
Previous studies have demonstrated that contact lens
wear can lead to corneal epithelial thinning (8,11). The
results of the present study showed that corneal epithelial
thicknesses were thinner in the short-term wear group than in the
non-wearing group only in the inferonasal, inferior and
inferotemporal sectors. The epithelial thicknesses were thinner in
the long-term wear group compared with those in the non-wearing
group in all nine sectors over the 5-mm diameter area. This
indicated that longer contact lens wear was associated with a
greater number of sectors with thinner corneal epithelial
thickness.
Preoperatively, the corneal epithelial thickness is
not evenly distributed; it is characterized by a thinner epithelium
superiorly compared with that inferiorly (20), as confirmed in the present study. By
contrast, no differences were found in epithelial thicknesses in
different segments between the short- and long-term wear groups.
Corneal epithelial remodeling due to contact lens wear may have
resulted in a uniform distribution of corneal epithelial thickness.
The max-min and SD values of corneal epithelial thickness were used
to describe the uniformity of the corneal epithelial distribution,
using a previously published method (21). The present results showed that the
max-min and SD values were lower in the long-term wear group than
those in the non-wearing group, both before and after surgery;
these findings indicated uniform corneal epithelium distribution
due to corneal epithelial remodeling after contact lens wear. The
results were consistent with the observations of Lei et al
(11) and Pérez et al
(22).
The underlying mechanisms of corneal epithelial
thinning after contact lens wear have been investigated in multiple
studies. Corneal oxygen uptake plays an important role in corneal
metabolism and the maintenance of corneal transparency (23). The oxygen required for corneal
metabolism is derived from the oxygen that diffuses through the
tear film, as well as oxygen supplied by the limbal vascular
circulation. Contact lens wear affects corneal oxygen uptake
(1). Patel et al (24) used confocal microscopy to study the
corneal epithelium in vivo. The study reported that
epithelial cells in long-term contact lens wearers became enlarged
and exhibited a loose arrangement; moreover, the density of
epithelial basal cells was decreased compared with that of
non-contact lens wearers. The observed decrease in epithelial cell
number and the thinning of the corneal epithelium are mainly caused
by corneal hypoxia. Based on animal experiments, Yanai et al
(4) suggested that hypoxia of the
ocular surface led to disruption of tight junctions between corneal
epithelial cells. In addition, mechanical stimulation of the ocular
surface, due to the physical presence of contact lenses, can
contribute to epithelial thinning (25). Finally, Efron (26) indicated that contact lens wear
induced pathological changes in the corneal epithelium; in this
study, mechanical stimulation was regarded as the main cause of
corneal epithelial thinning. In summary, the hypoxia of the ocular
surface and mechanical stimulation from the physical presence of
contact lenses are the important causes of corneal epithelial
thinning, which are related with the transmissibility of oxygen and
the material of the lens (9,22).
To the best of our knowledge, there have been no
studies focusing on changes in corneal epithelial thickness
following SCL wear after corneal refractive surgery. To recover the
smooth corneal anterior surface, the corneal epithelium itself
undergoes remodeling in response to corneal refractive surgery;
this remodeling is characterized by uneven thickening of the
corneal epithelium. The present results confirmed the findings of
previous studies (27,28). The corneal epithelium in Fig. 5 at all postoperative time points
were in warmer colors compared with preoperative time points which
means the corneal epithelium thickened following surgery. Previous
studies demonstrated that the epithelium was stable 3 months after
myopic surgery (29); therefore,
the present study assessed the change in the epithelial thickness
during the first 6 months after SMILE. Furthermore, the results
demonstrated that the epithelial thicknesses of the central, nasal,
inferonasal, inferior, inferotemporal and temporal sectors were
thinner in the long-term wear group than in the non-wearing group
at all postoperative time points; this was consistent with the
preoperative results. There were no differences in the epithelial
thicknesses of the superior, superonasal or superotemporal sectors
among the three groups after surgery. In addition, the changes in
epithelial thicknesses in the superior, superonasal and
superotemporal segments were greater in the long-term wear group
than in the non-wearing group. The changes in corneal epithelial
thickness among the three groups before and after surgery were
mainly due to the uneven regional thickening of the corneal
epithelium postoperatively, possibly caused by the effects of
pressure from the upper eyelid and SCL. In addition, previous
studies have suggested that the epithelial thickness gradually
recovers and reaches a stable state after a given period when
contact lenses are no longer worn (30,31);
however, it cannot match the thickness in non-wearers (11). Although all patients in the present
study had stopped contact lens wear 2 weeks preoperatively, the
epithelial thickness was thinner in the wear group than that in the
non-wearing group. The recovery of epithelial thickness after
discontinuation of contact lens wear can also explain the
difference in epithelial thicknesses before and after surgery.
No differences were found in terms of visual acuity
or manifest refraction among the three groups at all postoperative
time points after SMILE. The visual quality after SMILE did not
appear to be affected by the thinning of the corneal epithelium
induced by contact lens wear and corneal surgery. Considering that
the postoperative epithelial healing response caused by SMILE is
mild (32), changes in the corneal
epithelium appear to have minimal effects on surgical outcomes. In
a previous study, Lloyd-McKernan et al (33) reported that previous SCL wear had no
negative impact on visual outcomes following LASIK and
laser-assisted subepithelial keratecotomy (LASEK)/PRK when compared
with a non-contact lens control group, which was consistent with
the present results.
In the present study, the total higher-order and
coma aberrations of the long-term wear group were greater than
those of the non-wearing and short-term wear groups preoperatively,
which was consistent with the results after surgery. By contrast,
there were no significant differences in spherical aberrations
among the three groups, while spherical aberrations at 3 and 6
months postoperatively were greater in the long-term wear group
than in the non-wearing group. Consistent with this, the changes in
spherical aberrations at 1, 3 and 6 months postoperatively were
greater in the long-term wear group than in the non-wearing group.
Larger corneal aberrations observed in the long-term wear group may
have been related to the influence of contact lenses on the normal
physiology of the corneal epithelium (1). Long-term contact lens wear can cause a
decrease of ocular surface glycocalyx, thereby inducing eye dryness
and lowering of tear-film stability (34,35). A
decrease in tear-film stability can lead to greater corneal
aberrations (36). In the present
study, the tear-film stability and corneal epithelial integrity
were better in the non-wearing group than in the long-term wear
group, such that the corneal aberrations of the non-wearing group
were smaller than those of the contact lens wear group. The total
higher-order, spherical and coma aberrations of the three groups
after SMILE were increased by different degrees. The total
higher-order and coma aberrations of the three groups at all
postoperative time points were consistent with the results before
surgery, whereas the change in corneal aberrations was not
statistically significant. This indicates that SMILE has a
specific, but subtle influence on corneal aberrations, which may be
related to the mild change in corneal shape and minimal or moderate
changes in tear-film stability after SMILE.
The present study has a few limitations.
Investigation of corneal epithelial thickness was limited to a
region 5 mm in diameter. Furthermore, the thickness of the
peripheral corneal epithelium may have been affected by the size of
the palpebral fissure and the compression of the upper and lower
eyelids on the cornea, which led to decreased accuracy and
reliability of the measurement of peripheral corneal epithelial
thickness and may have affected the comprehensive assessment of
corneal epithelial thickness. With the possible development of more
accurate high-resolution anterior segment optical coherence
tomography technology, the epithelial thickness over the entire
cornea can be studied to fully evaluate changes in epithelial
thickness.
In summary, the present results indicate that
long-term SCL wear will lead to epithelial thinning. However,
uneven thickening of the corneal epithelium after SMILE and
discontinuation of SCL wear do not impact visual acuity or manifest
refraction after SMILE.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YX, YW and XY made substantial contributions to
acquisition of data and analysis of data. YW was involved in
drafting the manuscript. YQ, BL and XZ made substantial
contributions to conception and design, and revised the manuscript
critically for important intellectual content. XZ and YX confirm
the authenticity of all the raw data. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
Clinical trials registration reference ID: 2019-049
(The First Affiliated Hospital of Soochow University Institutional
Review Board, Suzhou, China). This retrospective study was approved
by the Ethics Committee of The First Affiliated Hospital of Soochow
University, and all patients provided consent at the time of the
surgery.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Holden BA, Sweeney DF, Vannas A, Nilsson
KT and Efron N: Effects of long-term extended contact lens wear on
the human cornea. Invest Ophthalmol Vis Sci. 26:1489–1501.
1985.PubMed/NCBI
|
|
2
|
Liesegang TJ: Physiologic changes of the
cornea with contact lens wear. CLAO J. 28:12–27. 2002.PubMed/NCBI
|
|
3
|
Zhang X, Marchetti C, Lee J, Sun Y,
Debanne S, Jiang Y, Kern J, Harrod M, Benetz BA, Pearlman E and
Szczotka-Flynn L: The impact of lens care solutions on corneal
epithelial changes during daily silicone hydrogel contact lens wear
as measured by in vivo confocal microscopy. Contact Lens Anterior
Eye. 40:33–41. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Yanai R, Ko JA, Morishige N, Chikama T,
Ichijima H and Nishida T: Disruption of zonula occludens-1
localization in the rabbit corneal epithelium by contact
lens-induced hypoxia. Invest Ophthalmol Vis Sci. 50:4605–4610.
2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Bastion ML and Mohamad MH: Study of the
factors associated with the presence of white dots in the corneas
of regular soft contact lens users from an Asian Country. Eye
Contact Lens. 32:223–227. 2006.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Edelhauser HF: The resiliency of the
corneal endothelium to refractive and intraocular surgery. Cornea.
19:263–273. 2000.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Yamamoto K, Ladage PM, Ren DH, Li L,
Petroll WM, Jester JV and Cavanagh HD: Effect of eyelid closure and
overnight contact lens wear on viability of surface epithelial
cells in rabbit cornea. Cornea. 21:85–90. 2002.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hong J, Qian T, Yang Y, Jiang C, Liu Z,
Sun X, Deng SX and Xu J: Corneal epithelial thickness map in
long-term contact lenses wearers. Optom Vis Sci. 91:1455–1461.
2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Jalbert I, Sweeney DF and Stapleton F: The
effect of long-term wear of soft lenses of low and high oxygen
transmissibility on the corneal epithelium. Eye (Lond).
23:1282–1287. 2009.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Stachura J, Mlyniuk P, Bloch W,
Jimenez-Villar A, Grulkowski I and Kaluzny BJ: Shape of the
anterior surface of the cornea after extended wear of silicone
hydrogel soft contact lenses. Ophthalmic Physiol Opt. 41:683–690.
2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lei Y, Zheng X, Hou J, Xu B and Mu G:
Effects of long-term soft contact lens wear on the corneal
thickness and corneal epithelial thickness of myopic subjects. Mol
Med Rep. 11:2020–2026. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Shehadeh-Mashor R, Mimouni M, Shapira Y,
Sela T, Munzer G and Kaiserman I: Duration of contact lens removal
before myopic refractive surgery. Eur J Ophthalmol. 31:1695–1699.
2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sekundo W, Kunert KS and Blum M: Small
incision corneal refractive surgery using the small incision
lenticule extraction (SMILE) procedure for the correction of myopia
and myopic astigmatism: Results of a 6 month prospective study. Br
J Ophthalmol. 95:335–339. 2011.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Reinstein DZ, Archer TJ and Randleman JB:
Mathematical model to compare the relative tensile strength of the
cornea after PRK, LASIK, and small incision lenticule extraction. J
Refract Surg. 29:454–460. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Denoyer A, Landman E, Trinh L, Faure JF,
Auclin F and Baudouin C: Dry eye disease after refractive surgery:
Comparative outcomes of small incision lenticule extraction versus
LASIK. Ophthalmology. 122:669–676. 2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ishii R, Shimizu K, Igarashi A, Kobashi H
and Kamiya K: Influence of femtosecond lenticule extraction and
small incision lenticule extraction on corneal nerve density and
ocular surface: A 1-year prospective, confocal, microscopic study.
J Refract Surg. 31:10–15. 2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Shah R, Shah S and Sengupta S: Results of
small incision lenticule extraction: All-in-one femtosecond laser
refractive surgery. J Cataract Refract Surg. 37:127–137.
2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Reinstein DZ, Archer TJ and Gobbe M:
Lenticule thickness readout for small incision lenticule extraction
compared to artemis three-dimensional very high-frequency digital
ultrasound stromal measurements. J Refract Surg. 30:304–309.
2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Vestergaard AH, Grauslund J, Ivarsen AR
and Hjortdal JØ: Central corneal sublayer pachymetry and
biomechanical properties after refractive femtosecond lenticule
extraction. J Refract Surg. 30:102–108. 2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Reinstein DZ, Archer TJ, Gobbe M,
Silverman RH and Coleman DJ: Epithelial thickness in the normal
cornea: Three-dimensional display with very high frequency
ultrasound. J Refract Surg. 24:571–581. 2008.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Li Y, Tan O, Brass R, Weiss JL and Huang
D: Corneal epithelial thickness mapping by Fourier-domain optical
coherence tomography in normal and keratoconic eyes. Ophthalmology.
119:2425–2433. 2012.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Pérez JG, Méijome JM, Jalbert I, Sweeney
DF and Erickson P: Corneal epithelial thinning profile induced by
long-term wear of hydrogel lenses. Cornea. 22:304–307.
2003.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Chen Y, Thompson DC, Koppaka V, Jester JV
and Vasiliou V: Ocular aldehyde dehydrogenases: Protection against
ultraviolet damage and maintenance of transparency for vision. Prog
Retin Eye Res. 33:28–39. 2013.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Patel SV, McLaren JW, Hodge DO and Bourne
WM: Confocal microscopy in vivo in corneas of long-term contact
lens wearers. Invest Ophthalmol Vis Sci. 43:995–1003.
2002.PubMed/NCBI
|
|
25
|
Markoulli M, Papas E, Cole N and Holden B:
Corneal erosions in contact lens wear. Cont Lens Anterior Eye.
35:2–8. 2012.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Efron N: Contact lens-induced changes in
the anterior eye as observed in vivo with the confocal microscope.
Prog Retin Eye Res. 26:398–436. 2007.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Luft N, Ring MH, Dirisamer M,
Mursch-Edlmayr AS, Kreutzer TC, Pretzl J, Bolz M and Priglinger SG:
Corneal epithelial remodeling induced by small incision lenticule
extraction (SMILE). Invest Ophthalmol Vis Sci. 57:OCT176–OCT183.
2016.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Ryu IH, Kim BJ, Lee JH and Kim SW:
Comparison of corneal epithelial remodeling after femtosecond
laser-assisted LASIK and small incision lenticule extraction
(SMILE). J Refract Surg. 33:250–256. 2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Reinstein DZ, Archer TJ and Gobbe M:
Change in epithelial thickness profile 24 h and longitudinally for
1 year after myopic LASIK: Three-dimensional display with artemis
very high-frequency digital ultrasound. J Refract Surg. 28:195–202.
2012.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Nourouzi H, Rajavi J and Okhovatpour MA:
Time to resolution of corneal edema after longt-term contact lens
wear. Am J Ophthalmol. 142:671–673. 2006.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Hashemi H, Firoozabadi MR, Mehravaran S
and Gorouhi F: Corneal stability after discontinued soft contact
lens wear. Cont Lens Anterior Eye. 31:122–125. 2008.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Riau AK, Angunawela RI, Chaurasia SS, Lee
WS, Tan DT and Mehta JS: Early corneal wound healing and
inflammatory responses after refractive lenticule extraction
(ReLEX). Invest Ophthalmol Vis Sci. 52:6213–6221. 2011.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Lloyd-McKernan A, Simo Mannion L and
O'Dwyer V: The effect of previous soft contact lens wear on corneal
refractive surgery outcomes. Cont Lens Anterior Eye. 40:301–310.
2017.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Fukui M, Yamada M, Akune Y, Shigeyasu C
and Tsubota K: Fluorophotometric analysis of the ocular surface
glycocalyx in soft contact lens wearers. Curr Eye Res. 41:9–14.
2016.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Guillon M and Maissa C: Dry eye
symptomatology of soft contact lens wearers and nonwearers. Optom
Vis Sci. 82:829–834. 2005.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Denoyer A, Rabut G and Baudouin C: Tear
film aberration dynamics and vision-related quality of life in
patients with dry eye disease. Ophthalmology. 119:1811–1818.
2012.PubMed/NCBI View Article : Google Scholar
|