Introduction
Myomas or fibroids are a type of benign uterine
smooth muscle tumors, found in women of reproductive age, with an
incidence of up to 70% (1-4).
Myomas are frequently diagnosed in 20-25% of women of reproductive
age (30-40 years) and 30-40% of women older than 40 years (5-9).
They often have a negative impact on reproduction. They can be
single, but more often multiple, causing significant morbidity and
deterioration of quality of life (5,9,10).
Most women are asymptomatic, only 30-40% of them present with
symptoms such as heavy menstrual bleeding, lower abdominal pain,
infertility, recurrent pregnancy loss, dyspareunia, abdominal
bloating or constipation, increased urinary frequency or
incontinence, anemia from heavy bleeding, fatigue, and pressure
symptoms. The severity of symptoms depends on the size, location,
and number of myomas (11-14).
Based on the relationship between the myoma and the uterine wall,
there are three types of myomas: submucous myoma, intramural myoma,
and subserous myoma (15).
For most of the women presenting with myomas, the
treatment remains, in the end, surgical removal (1,2).
Myomectomy is the gold standard treatment in women who wish to
preserve their fertility. It can also be performed in those women
who desire to preserve the uterus for social, cultural, and
psychological reasons, even if they have a complete family
(16).
The techniques used in gynecological practice
include abdominal myomectomy, transvaginal myomectomy, laparoscopic
myomectomy, laparoscopically assisted myomectomy via minilaparotomy
incision, and robot-assisted laparoscopic myomectomy (1,6-8).
Additional interventions to reduce intraoperative bleeding during
myomectomy are uterine artery embolization/ligation, pericervical
tourniquet placement, intramyometrial vasopressin/epinephrine
administration, use of uterotonics (e.g. ergometrine, oxytocin and
misoprostol), and antifibrinolytic agents (e.g. tranexamic acid,
recombinant factor VIIa) (2,17).
The data regarding the associated epidemiological
factors are either well-defined or not yet completely understood.
These factors are age, race, heritage, sex hormone imbalance,
earlier age at menarche, obesity, lifestyle factors (diet,
caffeine, alcohol, smoking, and stress), environmental factors, and
possibly many others. In the literature, the impact of these
factors remains conflicting. It may be attributed to selection
bias, given the fact that studies are based on surgical/symptomatic
cases, or on the incidental diagnosis of myomas (5,9,18-20).
The data on racial differences, other than in
Caucasian and African American women, are limited (9,18,21).
Though most women are asymptomatic, myoma symptoms
can affect the quality of a woman's life.
The incidence and prevalence of myomas remain
currently unknown (22-25).
Stating the fact that the incidence of myoma varies greatly around
the world, the aim of our study was to provide information about
the incidence and prevalence of this disease in the gynecological
patients admitted to the Iasi ‘Cuza Voda’ University Hospital of
Obstetrics and Gynecology in Northeastern Romania.
Patients and methods
This retrospective study conducted at the Iasi ‘Cuza
Voda’ University Hospital of Obstetrics and Gynecology (Romania)
included 11,538 patients, representing all patients admitted to the
Gynecology Department between January 2013 and December 2019. All
these patients had surgical interventions performed in our hospital
from which 4,035 were hysterectomies. From all the 4,035
hysterectomies performed, only 2,196 were performed for myomas.
The present study aimed at establishing the
detection rate of myoma cases, as well as the differential
diagnosis with other pelvic diseases.
During the study interval, patients with different
gynecological conditions were admitted for surgical reasons
(laparoscopy, open laparotomy, hysteroscopy). The obstetric
patients were excluded from the study. Of the 11,538 patients only
2,786 met the inclusion criteria. They had a surgery prior
diagnosis of myoma, histopathologically confirmed afterwards. From
these 2,786 patients with myomas, 590 had myomectomy performed and
2,196 had hysterectomy performed for this diagnosis.
All patients signed our hospital informed consent.
Institutional review board approval from the Ethics Committee of
‘Cuza Voda’ Iasi University Hospital of Obstetrics and Gynecology
was obtained to conduct this retrospective study (10425/2021).
Statistical analysis
The emphasis of this study is on proportion
estimates. Therefore, the absolute and relative frequencies were
computed. For a consistent information estimation, we used the
confidence interval with standard 0.95 probability (95% CI). The
binomial proportion confidence interval using the Clopper-Pearson
(exact method) formula was applied in order to have a minimum
coverage probability of 0.95 (conservative method). Computations
were made in R version 4.0.2 (2020-06-22) using the package
DescTools (version 0.99.40, https://www.rdocumentation.org/packages/DescTools/versions/0.99.40)
(26).
Results
Of the total number of 11,538 surgeries performed in
our gynecology department during 2013-2019, 4,035 were
hysterectomies, meaning that approximatively one-third of the total
surgeries (34.97%) (95% CI: 34.10-35.84) were hysterectomies.
Table I shows the
total number of hysterectomies and hysterectomies for myomas, and
their corresponding percentage and confidence interval. During the
study interval, the number of hysterectomies (total and for myomas)
increased from 2013 to 2017.
 | Table INumber and percentage of
hysterectomies in the period 2013-2019. |
Table I
Number and percentage of
hysterectomies in the period 2013-2019.
| Year | Total
hysterectomies n (% of the total) | Hysterectomies for
myomas n (% of the total) | Percentage % (95%
CI) |
|---|
| 2013 | 468 (11.59) | 106 (4.82) | 22.64
(18.93-26.71) |
| 2014 | 527 (13.07) | 200 (9.11) | 37.95
(33.79-42.24) |
| 2015 | 535 (13.25) | 229 (10.43) | 42.80
(38.56-47.12) |
| 2016 | 543 (13.46) | 312 (14.20) | 57.45
(53.17-61.65) |
| 2017 | 652 (16.15) | 478 (21.78) | 73.31
(69.74-76.67) |
| 2018 | 664 (16.46) | 428 (19.49) | 64.45
(60.68-68.1) |
| 2019 | 646 (16.01) | 443 (21.17) | 68.57
(64.83-72.14) |
| Total | 4,035(100) | 2,196(100) | 54.42
(52.87-55.96) |
From 2013 to 2017 there was also an increase in the
percentage of hysterectomies from 22.64 to 73.31%, followed by a
decrease to 64.45% in 2018, and to 68.57% in 2019, which means that
two-thirds of the hysterectomies were performed for myomas. The
percentage for the entire period 2013-2019 was 54.42%. As a general
rule, confidence intervals are wider for small sample sizes.
In Table II, the
total gynecological surgical cases, myoma cases and the percentage
of myomas (with 95% CI) from total surgical cases from 2013-2019
are documented. All of these values increased with time, the only
exception being the year 2015.
 | Table IINumber and percentage of myomas from
the total gynecological surgeries. |
Table II
Number and percentage of myomas from
the total gynecological surgeries.
| Year | Total surgeries n
(% of the total) | Myomas n (% of the
total) | Percentage of
myomas from surgeries (95% CI) |
|---|
| 2013 | 1,468 (12.72) | 50 (8.47) | 3.40
(2.53-4.46) |
| 2014 | 1,610 (13.95) | 81 (13.72) | 5.03
(4.01-6.21) |
| 2015 | 1,531 (13.26) | 58 (9.83) | 3.78
(2.88-4.87) |
| 2016 | 1,675 (14.51) | 74 (12.54) | 4.41
(3.48-5.51) |
| 2017 | 1,741 (15.08) | 104 (17.62) | 5.97
(4.90-7.19) |
| 2018 | 1,726 (14.95) | 108 (17.30) | 6.25
(5.16-7.50) |
| 2019 | 1,787 (15.48) | 115 (19.49) | 6.43
(5.34-7.67) |
| Total | 11,538(100) | 590(100) | 5.11
(4.71-5.53) |
The percentage of myomas from the total surgeries
performed, during the study period, almost doubled from 3.40%
(2.52-4.46) in 2013 to 6.43% (5.34-7.67) in 2019.
Table III shows,
along with the 95% CI, the percentage of each type of surgery for
myoma. Studying the values, no general rules, such as increasing or
decreasing trend with time are noted. Consequently, we compared the
2019 percentages with the 2013 baseline. The rate of laparoscopic
surgery showed a small decrease [34% (2013) to 31.30% (2019)],
classic therapy showed a decrease by more than 10% [from 54% (2013)
to 29.56% 2019)] and the rate of hysteroscopy rate tripled (12%
(2013) to 39.14% (2019)] in 2019 compared to 2013.
 | Table IIITypes of surgery for myomas. |
Table III
Types of surgery for myomas.
| Year | Myoma cases, n (%
of the total) | Laparoscopy cases,
n (%) (95% CI) | Classic cases, n
(%) (95% CI) | Hysteroscopy cases,
n (%) (95% CI) |
|---|
| 2013 | 50 (8.47) | 17 (34.00)
(21.20-48.76) | 27 (54.00)
(39.32-68.18) | 6 (12.00)
(4.53-24.31) |
| 2014 | 81 (13.73) | 31 (38.27)
(27.68-49.74) | 41 (50.62)
(39.27-61.91) | 9 (11.11)
(5.20-20.04) |
| 2015 | 58 (9.83) | 19 (32.75)
(21.00-46.34) | 28 (48.28)
(34.95-61.78) | 11 (18.97)
(9.86-31.40) |
| 2016 | 74 (12.54) | 18 (24.32)
(15.09-35.69) | 37 (50.00)
(38.14-61.85) | 19 (25.68)
(16.22-37.15) |
| 2017 | 104 (17.63) | 27 (25.97)
(17.85-35.48) | 43 (41.34)
(31.77-51.42) | 34 (32.69)
(23.81-42.58) |
| 2018 | 108 (18.31) | 40 (37.04)
(27.94-46.86) | 33 (30.55)
(22.05-40.15) | 35 (32.41)
(23.71-42.09) |
| 2019 | 115 (19.49) | 36 (31.30)
(22.98-40.61) | 34 (29.56)
(21.42-38.79) | 45 (39.14)
(30.16-48.67) |
| Total | 590 (100%) | 188 (31.87)
(28.11-35.79) | 243 (41.19)
(37.18-45.27) | 159 (26.94)
(23.4-30.72) |
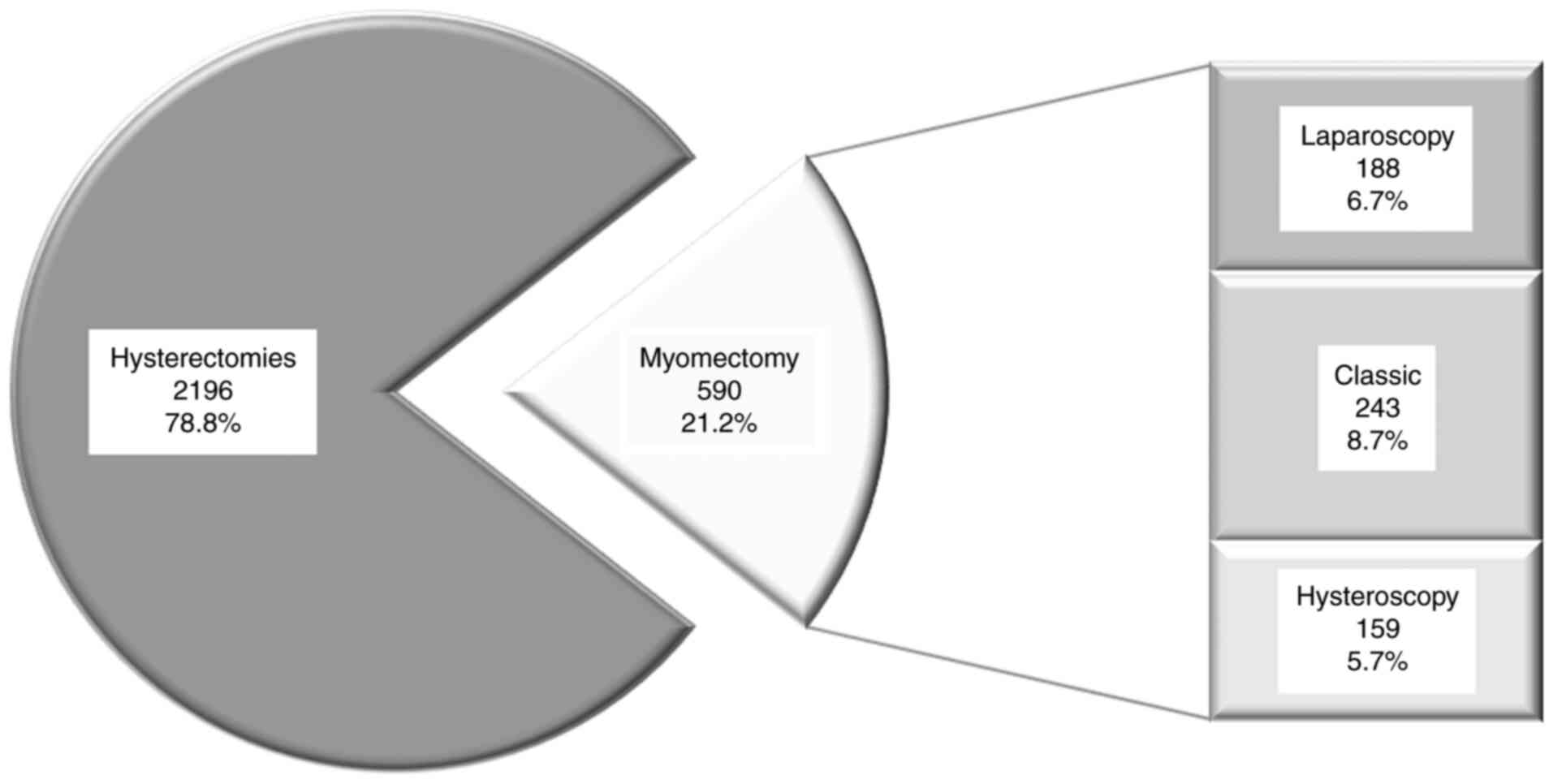
Table IV shows that
the rate of intramural and subserous myomas had a positive trend
from 23.07% in 2013 to 54.29 in 2019, while for the submucous type,
the trend was descending from 76.92% in 2013 to 45.69 in 2019. The
same positive correlation was observed in uterine myoma cases
during this period. The number of uterine myoma cases grew from
5.6% cases in 2013 to 20.03% cases in 2019. Finally, the percentage
of surgical methods used are presented in Fig. 1.
 | Table IVDistribution of the types of
myomas. |
Table IV
Distribution of the types of
myomas.
| Year | Uterine myoma
cases, n (% from total) | Submucous cases, n
(%) (95% CI) | Intramural cases, n
(%) (95% CI) | Subserous cases, n
(%) (95% CI) |
|---|
| 2013 | 156 (5.60) | 120 (76.92)
(69.51-83.28) | 22 (14.10)
(9.05-20.56) | 14 (08.97)
(4.99-14.59) |
| 2014 | 281 (10.09) | 166 (59.07)
(53.07-64.87) | 67 (23.84)
(18.98-29.26) | 48 (17.08)
(12.87-22.00) |
| 2015 | 287 (10.30) | 191 (66.55)
(60.76-71.98) | 63 (21.95)
(17.29-27.19) | 33 (11.49)
(8.04-15.76) |
| 2016 | 386 (13.85) | 247 (63.98)
(58.97-68.78) | 99 (25.64)
(21.36-30.31) | 40 (10.36)
(7.50-13.84) |
| 2017 | 582 (20.89) | 341 (58.59)
(54.46-62.620) | 149 (25.60)
(22.10-29.35) | 92 (15.80)
(12.93-19.02) |
| 2018 | 536 (19.24) | 250 (46.64)
(42.35-50.96) | 190 (35.44)
(31.39-39.66) | 96 (17.91)
(14.75-21.42) |
| 2019 | 558 (20.03) | 255 (45.69)
(41.50-49.93) | 203 (36.37)
(32.37-40.52) | 100 (17.92)
(14.82-21.36) |
| Total | 2,786(100) | 1,570 (56.35)
(54.48-58.20) | 793 (28.46)
(26.79-30.17) | 423 (15.18)
(13.86-16.57) |
Discussion
Uterine myomas are the most common indication for
hysterectomy worldwide (9,27,28).
Ultrasound studies have shown that the prevalence of myoma is much
lower in Europe than in the United States, possibly due to racial
differences. The prevalence of myoma was highly underestimated in
previous epidemiological studies, that only focused on symptomatic
patients. Epidemiological studies have become more accurate using
more advanced imaging techniques (3D-4D ultrasonography) (5,7,9,18,19,29,30).
In our study, the prevalence of hysterectomy for myomas was 54.42%.
Our results are in agreement with the data in the literature,
namely that 40-60% of all performed hysterectomies are for myomas.
The vast majority of admissions for myomas involve a surgical
procedure (94.4%), most commonly hysterectomy (79.2%) (14,31).
As in our hospital all patients were Caucasian, we
were unable to determine a race-specific prevalence. Laughlin et
al (23) determined the
following prevalence for myomas by race: 18% in Black women, 8% in
Caucasian women, 10% in Hispanic women, and 13% in an ‘Others’
group, consisting largely of Asian women (23). In regards to Caucausian women,
contrary to the above-mentioned study, in our study the prevalence
was higher.
Available data from different studies are difficult
to compare because of the differences in the study population and
screening methods (22-25).
Findings from our study are based on a small sample size, thus the
results should be considered with caution.
Different types of myoma have different impacts on
fertility. The submucosal type lowers the fertility rate,
intramural myomas may impair fertility, and the subserous type
often has no impact on the fertility rate (32,33).
The incidence of submucous myoma subtype is
particularly high. These findings are in agreement with our results
(18,25). In our study the prevalence of
submucous myoma from 2013-2019 was 56.35%; 28.46% for intramural
myoma and 15.18% for subserous myoma.
Hysteroscopic transcervical resection of myomas also
has some limitations, namely the potential conversion to laparotomy
and incomplete resection. Many studies have compared the clinical
outcomes of abdominal hysterectomy and laparoscopic or
hysteroscopic surgery without reaching any conclusions concerning
outcomes, advantages, and disadvantages of laparoscopic and
hysteroscopic surgery (15,34-36).
In our study 2,196 patients underwent hysterectomy for myoma and
590 myomectomy (243 patients with open myomectomy, 188 patients
with laparoscopic myomectomy, and 159 patients hysteroscopic
myomectomy).
It is quite difficult to assess accurately the
incidence and prevalence of uterine myoma as these increase with
aging. Myomas can seriously impact the lives of women and also are
a significant healthcare burden. It has been estimated that the
costs for uterine myomectomy/hysterectomy, in terms of care,
adverse obstetric outcomes, and workhours lost, are higher compared
to other benign gynecologic diseases (37). In the last decade, several
conservative treatments have been developed for the management of
uterine myomas (27,37-39).
The symptoms caused by myomas can affect the quality
of life and sexual function of the patients. Despite the recent
pharmacological and radiological interventions, surgery remains one
of the main treatment options for symptomatic myomas in women of
reproductive age. Postoperative quality of life and sexual function
can be used to assess surgical outcomes in association with
complication rates, blood loss, and duration of surgery (40-45).
Few studies have evaluated the patient-reported
outcomes after surgical treatment. Radosa et al conducted a
systematic literature search of PubMed. He found 29 articles but
none of them had assessed the postoperative quality of life and
sexual function in patients undergoing surgical treatment for myoma
(45).
Uterine myomas remain the most common diagnosis
among women admitted to our hospital. It is very important for the
practitioner to understand the physical and psychological needs of
these patients. Because many patients consider the uterus as a
sexual organ, as a symbol of one's fertility, the surgeon must
fathom its importance. This is the main reason why after
hysterectomy most patients suffer an emotional trauma with a
decrease in self-esteem, anxiety, and depression.
The lack of appropriate education and misconception
in which concerns the uterus as a sexual organ might complicate or
even worsen a preexisting psychiatric condition with major impact
on sexual life.
The association between myomas and infertility may
determine an increased level of stress in a couple, with a major
impact on social life and relationship with the partner.
In conclusion, despite the substantial impact on
gynecologic morbidity, relatively little is known about the
etiology of myomas. Given the high frequency of asymptomatic
myomas, the most accurate estimation of their prevalence and
incidence comes from epidemiologic studies using ultrasound
evaluation. A clear insight into the epidemiology of myomas is
still not yet complete. Future research on the risk factors may
help with prevention and may provide new conservative techniques.
Considering their significant morbidity and impact on quality of
life, more research focused on determining the risk factors
associated with myoma onset and growth is needed.
Our hospital is a tertiary referral center and thus
the study was affected by the implicit statistical bias. Thus, an
overestimation of hysterectomy for uterine myomas might occur
because many of the cases treated in our department required
difficult and complex surgical interventions, often these cases
being referred to us from other gynecology services.
One major limitation of this study is that we did
not apply a questionnaire for a better exposure of symptoms. A
prospective study is needed to validate the impact of myomas on the
quality of life using a questionnaire to evaluate symptoms of
depression, infertility-related stress, and social aspects in
postoperative patients. We still miss the means to accurately
estimate these aspects. The limitation of our study is the one that
opens for us new perspectives for further research.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during this study
are available from the corresponding author on reasonable
request.
Authors' contributions
DRM, AU, LH and ID were involved in the conception
of the study, data interpretation and writing of the manuscript. BT
and VLB contributed to data collection and performed the
statistical analysis. DRM and MG revised the manuscript for
important intellectual content in regards to the literature data.
All authors read and approved the final version of the manuscript
for publication.
Ethics approval and consent to
participate
Ethical approval was obtained from the Ethics
Committee of the ‘Cuza Voda’ Obstetrics and Gynecology Clinical
Hospital, Iasi (10425/2021) and our hospital inform consent was
obtained from all participants.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Zhang R, Shi H, Ren F and Yuan Z:
Assessment of carboprost tromethamine for reducing hemorrhage in
laparoscopic intramural. Exp Ther Med. 10:1171–1174.
2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kongnyuy EJ and Wiysonge CS: Interventions
to reduce haemorrhage during myomectomy for fibroids. Cochrane
Database Syst Rev. 8(CD005355)2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Srivastava S, Mahey R, Kachhawa G, Bhatla
N, Upadhyay AD and Kriplani A: Comparison of intramyometrial
vasopressin plus rectal misoprostol with intramyometrial
vasopressin alone to decrease blood loss during laparoscopic
myomectomy: Randomized clinical trial. Eur J Obstet Gynecol Reprod
Biol. 228:279–283. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Baird DD, Dunson DB, Hill MC, Cousins D
and Schectman JM: High cumulative incidence of uterine leiomyoma in
black and white women: Ultrasound evidence. Am J Obstet Gynecol.
188:100–107. 2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Sparic R: Uterine myomas in pregnancy,
childbirth and the puerperium. Srp Arh Celok Lek. 142:118–124.
2014.PubMed/NCBI View Article : Google Scholar : (In Serbian).
|
|
6
|
Fleischer R, Weston GC, Vollenhoven BJ and
Rogers PA: Pathophysiology of fibroid disease: Angiogenesis and
regulation of smooth muscle proliferation. Best Pract Res Clin
Obstet Gynaecol. 22:603–614. 2008.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Okolo S: Incidence, aetiology and
epidemiology of uterine fibroids. Best Pract Res Clin Obstet
Gynaecol. 22:571–588. 2008.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Duhan N: Current and emerging treatments
of uterine myoma - an update. Int J Womens Health. 3:231–241.
2011.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sparic R, Mirkovic L, Malvasi A and
Tinelli A: Epidemiology of uterine myomas: A review. Int J Fertil
Steril. 9:424–435. 2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Downes E, Sikirica V, Gilabert-Estelles J,
Bolge SC, Dodd SL, Maroulis C and Subramanian D: The burden of
uterine fibroids in five European countries. Eur J Obstet Gynecol
Reprod Bio. 152:96–102. 2010.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kjerulff KH, Langenberg P, Seidman JD,
Stolley PD and Guzinski GM: Uterine leiomyomas: Racial differences
in severity, symptoms, and age at diagnosis. J Reprod Med.
41:483–490. 1996.PubMed/NCBI
|
|
12
|
Lippman SA, Warner M, Samuels S, Olive D,
Vercellini P and Eskenazi B: Uterine fibroids and gynecologic pain
symptoms in a population-based study. Fertil Steril. 80:1488–1494.
2003.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Seracchioli R, Rossi S, Govoni F, Rossi E,
Venturoli S, Bulletti C and Flamigni C: Fertility and obstetric
outcome after laparoscopic myomectomy of large myomata: A
randomized comparison with abdominal myomectomy. Hum Reprod.
15:2663–2668. 2000.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Wise LA and Laughlin-Tommaso SK:
Epidemiology of uterine fibroids-from menarche to menopause. Clin
Obstet Gynecol. 59:2–24. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zhang RC, Wu W, Zou Q and Zhao H:
Comparison of clinical outcomes and postoperative quality of life
after surgical treatment of type II submucous myoma via laparoscopy
or hysteroscopy. J Int Med Res. 47:4126–4133. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Martinez MEG and Domingo MVC: Size, type,
and location of myoma as predictors for successful laparoscopic
myomectomy: A tertiary government hospital experience. Gynecol
Minim Invasive Ther. 7:61–65. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Koh MB and Hunt BJ: The management of
perioperative bleeding. Blood Rev. 17:179–185. 2003.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Wise LA and Laughlin-Tommaso SK: Uterine
leiomyomata. In: Women and Health. Goldman MB, Troisi R and Rexrode
KM (eds). Academic Press, San Diego, pp285-306, 2013.
|
|
19
|
Wise LA, Palmer JR, Harlow BL, Spiegelman
D, Stewart EA, Adams-Campbell LL and Rosenberg L: Reproductive
factors, hormonal contraception and risk of uterine leiomyomata in
African-American women: A prospective study. Am J Epidemiol.
159:113–123. 2004.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wise LA, Ruiz-Narvaez EA, Palmer JR,
Cozier YC, Tandon A, Patterson N, Radin RG, Rosenberg L and Reich
D: African ancestry and genetic risk for uterine leiomyomata. Am J
Epidemiol. 176:1159–1168. 2012.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Jacoby VL, Fujimoto VY, Giudice LC,
Kupperman M and Washington AE: Racial and ethnic disparities in
benign gynecologic conditions and associated surgeries. Am J Obsets
Gynecol. 202:514–521. 2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Zimmermann A, Bernuit D, Gerlinger C,
Schaefers M and Geppert K: Prevalence, symptoms and management of
uterine fibroids: An international internet-based survey of 21,746
women. BMC Womens Health. 12(6)2012.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Laughlin SK, Baird DD, Savitz DA, Herring
AH and Hartmann KE: Prevalence of uterine leiomyomas in the first
trimester of pregnancy: An ultrasound screening study. Obstet
Gynecol. 113:630–635. 2019.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Marino JL, Eskenazi B, Warner M, Samuels
S, Vercellini P, Gavoni N and Olive D: Uterine leiomyoma and
menstrual cycle characteristics in a population-based cohort study.
Hum Reprod. 19:2350–2355. 2004.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Chiaffarino F, Cipriani S, Ricci E, La
Vecchia C, Chiantera V, Bulfoni A and Parazzini F: Alcohol
consumption and risk of uterine myoma: A systematic review and meta
analysis. PLoS One. 12(e0188355)2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Signorell A, Aho K, Alfons A, Anderegg N,
Aragon T, Arachchige C, Arppe A, Beddeley A, Barton K, et al: Desc
Tools: Tools for Descriptive Statistics. R package version 0.99.40.
README NEWS. 2020. https://cran.r-project.org/web/packages/DescTools/DescTools.pdf.
Accessed September 8, 2021.
|
|
27
|
Baskett TF: ‘Hysterectomy: Evolution and
trends,’. Best Pract Res Clin Obstet Gynaecol. 19:295–305.
2005.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Tinelli A, Kosmas I, Mynbaev OA, Favilli
A, Gimbrizis G, Sparic R, Pellegrino M and Malvasi A: Submucous
fibroids, fertility, and possible correlation to pseudocapsule
thickness in reproductive surgery. Biomed Res Int.
2804830:2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Somigliana E, Vercellini P, Daguati R,
Pasin R, De Giorgi O and Crosignani PG: Fibroids and female
reproduction: A critical analysis of the evidence. Hum Reprod
Update. 13:465–476. 2007.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Cramer SF and Patel A: The frequency of
uterine leiomyomas. Am J Clin Pathol. 94:435–438. 1990.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Whiteman MK, Kuklina E, Jamieson DJ,
Hillis SD and Marchbanks PA: Inpatient hospitalization for
gynecologic disorders in the United States. Am J Obstet Gynecol.
202:541.e1–6. 2010.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Pritts EA, Parker WH and Olive DL:
Fibroids and infertility: An updated systematic review of the
evidence. Fertil Steril. 91:1215–1223. 2009.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Zhang Y and Hua KQ: Patients' age, myoma
size, myoma location, and interval between myomectomy and pregnancy
may influence the pregnancy rate and live birth rate after
myomectomy. J Laparoendosc Adv Surg Tech A. 24:95–99.
2014.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Husslein H, Frecker H, Shore EM, Lefebvre
G, Latta E, Montanari E and Satkunaratnam A: Comparing two uterine
manipulators during total laparoscopic hysterectomy: A randomized
controlled trial. J Minim Invasive Gynecol. 24:764–771.
2017.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Hosny TA: Oophoropexy for ovarian torsion:
A new easier technique. Gynecol Surg. 14:7–10. 2017.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Zeleniuk BI, Adamian LV, Obel'chak IS and
Khoroshun ND: Role of multislice spiral computed tomographic
angiography in the treatment of uterine myoma. Vestn Rentgenol
Radiol. 3:34–37. 2012.PubMed/NCBI(In Russian).
|
|
37
|
Cardozo ER, Clark AD, Banks NK, Henne MB,
Stegmann BJ and Segars JH: The estimated annual cost of uterine
leiomyomata in the United States. Am J Obstet Gynecol.
206:211.e1–9. 2012.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Mazzon I, Favilli A, Grasso M, Horvath S,
Di Renzo GC and Gerli S: Is cold loop hysteroscopic myomectomy a
safe and effective technique for the treatment of submucous myomas
with intramural development? A series of 1434 surgical procedures.
J Minim Invasive Gynecol. 22:792–798. 2015.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Tinelli A, Malvasi A, Mynbaev OA, Barbera
A, Perrone E, Guido M, Kosmas I and Stark M: The surgical outcome
of intracapsular cesarean myomectomy A match control study. J
Matern Fetal Neonatal Med. 27:66–71. 2014.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Stewart EA: Clinical practice: Uterine
fibroids. N Engl J Med. 372:1646–1655. 2015.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Ertunc D, Uzun R, Tok EC, Doruk A and
Dilek S: The effect of myoma uteri and myomectomy on sexual
function. J Sex Med. 6:1032–1038. 2009.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Dilek S, Ertunc D, Tok EC, Cimen R and
Doruk A: The effect of myomectomy on health-related quality of life
of women with myoma uteri. J Obstet Gynaecol Res. 36:364–369.
2010.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Mukhopadhaya N, De Silva C and Manyonda
IT: Conventional myomectomy. Best Pract Res Clin Obstet Gynaecol.
22:677–705. 2008.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Radosa JC, Meyberg-Solomayer G, Kastl C,
Radosa CG, Mavrova R, Graber S, Baum S and Radosa MP: Influences of
different hysterectomy techniques on patients' postoperative sexual
function and quality of life. J Sex Med. 11:2342–2350.
2014.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Radosa JC, Radosa CG, Mavrova R,
Wagenpfeil S, Hamza A, Joukhadar R, Baum S, Karsten M, Juhasz-Boess
I, Solomayer EF and Radosa MP: Postoperative quality of life and
sexual function in premenopausal women undergoing laparoscopic
myomectomy for symptomatic fibroids: A prospective observational
cohort study. PLoS One. 11(e0166659)2016.PubMed/NCBI View Article : Google Scholar
|