Introduction
The piriformis is, as the name suggests, a
pear-shaped, flat muscle located in the deep gluteal region. Its
origin is usually located on the anterior surface of the lateral
processes of the second to fourth sacral segments (1), on the anterior part of the capsule of
the sacroiliac joint, on the gluteal surface of the ilium in the
vicinity of the greater sciatic notch and, occasionally, on the
sacrotuberous ligament. The insertion is located on the medial
surface of the superior aspect of the greater trochanter of the
femur, where its tendon fuses with the tendons of the superior
gemellus, obturator internus and inferior gemellus muscles to form
the conjoint tendon. The piriformis muscle passes from the
posterior pelvic region to the gluteal region through the greater
sciatic notch. Its nerve supply passes through the anterior
branches of the S2 and S3 sacral nerves arising from the sacral
plexus (2,3).
The sciatic nerve is the widest peripheral nerve of
the body and the terminal branch of the sacral plexus. It usually
runs as a single trunk through the pelvic cavity, the gluteal
region and the posterior region of the thigh, until it reaches the
superior angle of the popliteal fossa, where it divides into the
tibial and the common peroneal nerves (1).
On occasion, the close anatomical relationship
between the piriformis muscle and the sciatic nerve may lead to the
compression of the latter, described as the piriformis syndrome
(4).
There are wide variations in the relationship
between the piriformis muscle and the sciatic nerve, with six
possible anatomical associations (5-7):
i) The sciatic nerve passes below the piriformis muscle; ii) the
divided sciatic nerve passes through and below the muscle; iii) the
divided sciatic nerve passes above and below the muscle; iv) the
undivided sciatic nerve passes through the muscle; v) the divided
sciatic nerve passes above and through the muscle; and vi) presence
of a smaller accessory piriformis muscle with a separate tendon,
located below them main piriformis muscle, with the sciatic nerve
passing between the two. Among all these variants, the most common
is the sciatic nerve passing undivided below the piriformis muscle,
found in 84% of 120 cadavers dissected by Beaton and Anson
(6) and in 78% of 130 cadavers
dissected by Pećina (7), followed
by the variant with the divided sciatic nerve passing through and
below the piriformis muscle, found in 12% of the cases in the study
of Beaton and Anson (6) and in 21%
in the study of Pećina (7).
The piriformis syndrome is often misdiagnosed, being
mainly confused with discogenic compression neuropathy or with
other causes of gluteal or hip pain, including trochanteric
bursitis, sacroileitis and sciatica (3).
Sciatica is defined as referred pain felt in the
lower limb, throughout the distribution of the sciatic nerve. Low
back pain is also a frequently reported symptom (4).
The treatment for this syndrome can be either
non-surgical or surgical (8).
In 1928, Yeoman (9)
was the first to describe the relationship between the piriformis
muscle and the sciatic nerve as an etiological factor of low back
pain and sciatic pain.
In 1934, Freiburg and Vinke (10) stated that inflammatory processes
within the sacroiliac joint primarily affect the piriformis muscle
and fascia, followed by irritation of the elements of the lumbar
and sacral plexuses.
Four years later in 1938, Beaton and Anson (11) conducted a study based on cadaver
dissections, concluding that the spasm of the piriformis muscle may
be a cause of irritation of the sciatic nerve.
The term ‘piriformis syndrome’ was introduced in
1947 by Robinson (12), who used it
to define the sciatic pain related to an abnormal piriformis
muscle, usually of traumatic origin.
The piriformis syndrome has long been considered as
a clinical diagnosis and, occasionally, a diagnosis of exclusion,
for which no clear diagnostic criteria have been determined to date
(12).
A recent clinical study by Hopayian and Danielyan
(13) states that there are four
symptoms that define the syndrome: Gluteal pain, pain exacerbation
upon sitting, external tenderness near the greater sciatic notch
and limitation of straight leg raising due to pain.
The deep gluteal syndrome is a condition
characterized by a set of clinical symptoms and other semiotic data
occurring in isolation and in combination (14-16),
with the most common being posterior pain, tenderness and/or
dysesthesia in the gluteal region, hip area or posterior thigh
region. The symptoms are usually unilateral, but they can occur
bilaterally. Other symptoms reported by patients include
intolerance to sitting for >20-30 min, limping, loss of
sensitivity in the affected limb, and pain at night that improves
during the day (15-17).
The piriformis syndrome is considered as a subgroup
of the deep gluteal syndrome (15),
which occurs due to several conditions: Asymmetrical hypertrophy of
the piriformis muscle with anterior displacement of the sciatic
nerve; dynamic sciatic nerve entrapment by the piriformis muscle;
and variants in the course of the sciatic nerve related to the
piriformis muscle.
In addition to the piriformis syndrome, the deep
gluteal syndrome also includes the gemelli-obturator internus
syndrome, the ischiofemoral impingement syndrome and the proximal
hamstring syndrome (18).
The aim of the present study was to combine
cadaveric dissections and pelvic MRI examinations to establish
clear osseous landmarks that may help evaluate the anatomical
associations between the sciatic nerve and the piriformis muscle
and identify possible nerve compression points.
Materials and methods
Study intent
The controversies regarding the existence of the
piriformis syndrome, the high rate of misdiagnosed and mistreated
cases and the complex anatomy of the pelvic and gluteal regions
require further morphological studies. This led to the concept of
conducting combined anatomical and imaging studies, using
dissection of the region and comparison to the images obtained
through MRI examination, in the hope that the anatomical study
should help physicians with clinical and imaging diagnosis.
The study was intended to combine direct anatomical
observation and an analysis of MRI scans in order to explain the
anatomical background of the development of the piriformis
syndrome.
Cadaveric dissection
For the purposes of the present study, five female
cadavers obtained from the Anatomy Department of the ‘Carol Davila’
University of Medicine and Pharmacy (Bucharest, Romania) were
dissected in an appropriate manner so as to emphasize the
morphology and the anatomical relations of the piriformis muscle,
the sciatic nerve and the internal pudendal neurovascular
bundle.
In order to obtain a favorable approach, the pelvis
of the cadavers was separated from the rest of the body by using
transverse cross sections at the following levels: Cranially
through the L4-L5 intervertebral disc and caudally at 10 cm below
the greater trochanter. The obtained anatomical specimen was then
sagittally sectioned 1-2 cm lateral to the pubic symphysis.
The dissection was conducted in anatomical planes
all the way to the level of the levator ani muscle. This muscle was
disinserted from the fascia of the internal obturator muscle and
reflected medially in order to create good access towards the
ischiorectal fossa. The sacral origins of the piriformis muscle and
the trunks of origin of the sciatic nerve were identified and
separated through careful dissection.
In another plane, the origins and the organization
pattern of the pudendal nerve, the sacrospinous ligament, the
coccygeus muscle and the perineal course of the internal pudendal
neurovascular bundle were dissected and separated from the
surrounding anatomical elements.
The superior and inferior gluteal artery and the
internal pudendal artery, which are branches of the internal iliac
artery, were preserved and highlighted.
The internal obturator muscle was been carefully
dissected, emphasizing the orientation of its origins and the
manner in which its fascicles unite to exit the pelvis below the
ischial spine. The infrapiriform space was also dissected to
emphasize the anatomical relations of the sciatic and internal
pudendal nerves.
In order to demonstrate the perineal course of the
internal pudendal nerve, dissections of the gluteal region were
conducted through a posterior approach and the nerve was
highlighted following removal of the gluteus maximus muscle.
MRI scans
The second part of the study included the analysis
of 10 MRI scans selected from the patients of the ‘Victor Babeş’
Diagnosis and Treatment Center, the clinic where one of the authors
works in. The selection criteria comprised the absence of any
pathological findings in the pelvic and gluteal areas and the high
quality of the images obtained during the examination. This allowed
us to perform a thorough analysis and correctly evaluate the
association with the aspects emphasized through dissection. The
landmarks useful for identifying the critical relations of the
nervous structures were identified based on data acquired through
dissection.
The MRI equipment utilized for obtaining the images
included in the present study was a Siemens Magnetom Avanto 1.5T
(Siemens Healthineers). The Body and the Flex Large coils were
used. The examination protocol included the following sequences:
Axial T2 turbo spin echo (TSE), axial T1 SE, coronal short tau
inversion recovery (STIR), coronal T1 TSE and sagittal T2 TSE.
Results
Observations during dissection
For the purposes of the first part of this study,
all the dissection specimens that were considered as the most
significant for the pelvic, extrapelvic and perineal course of the
internal pudendal neurovascular bundle were selected (Figs. 1 and 2).
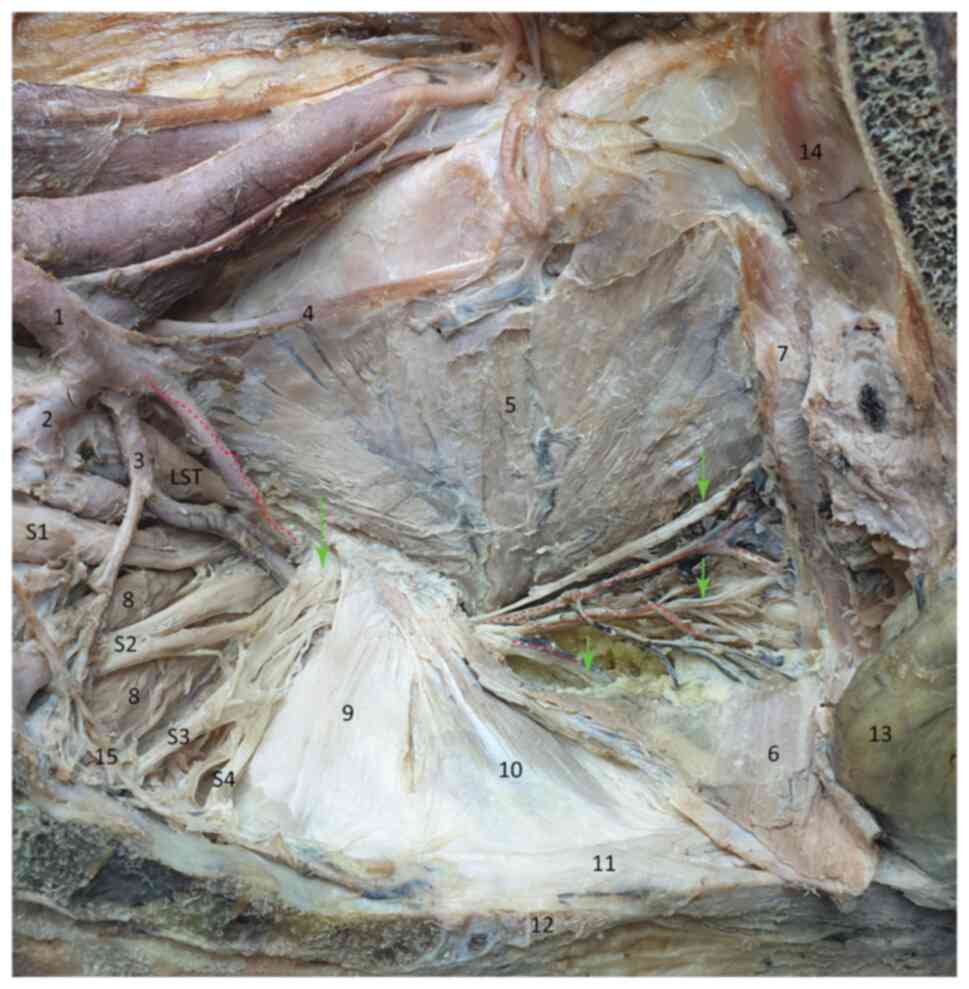
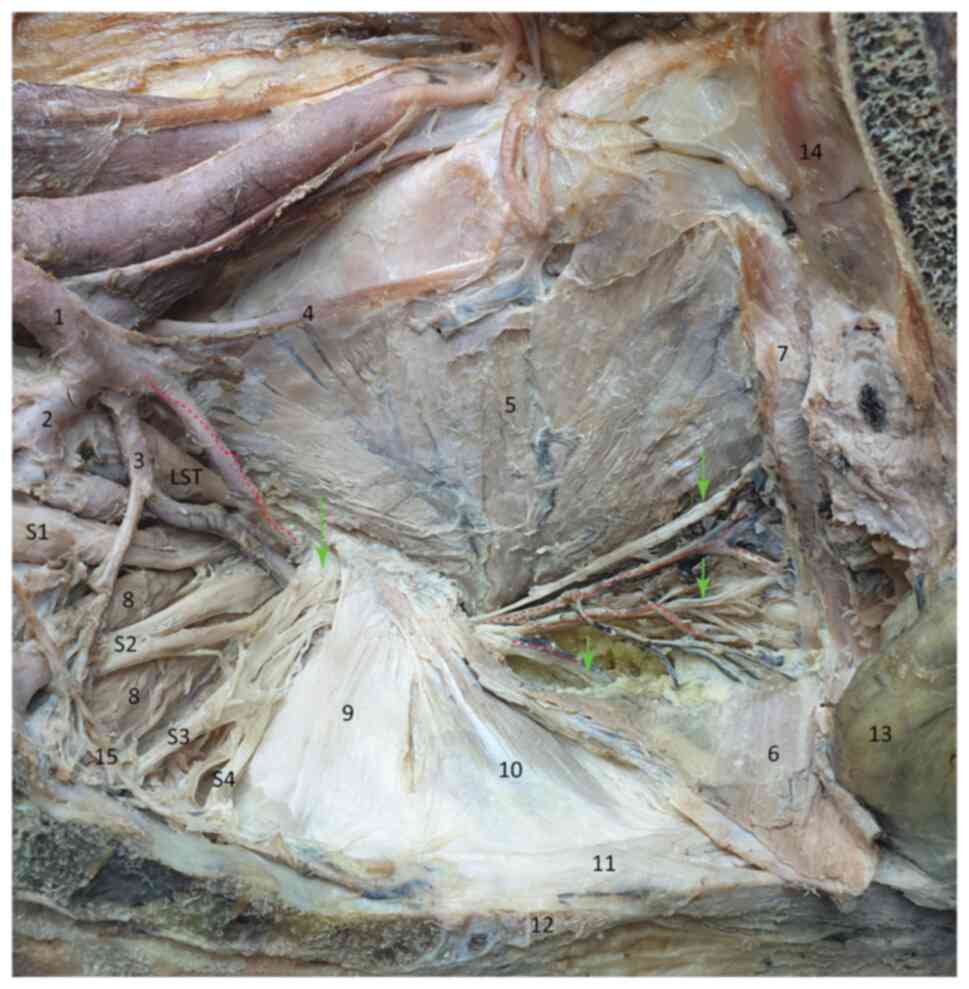 | Figure 1Internal view of the pelvic wall. The
red dotted line marks the internal pudendal artery and its
branches; the green arrows mark the internal pudendal nerve and its
branches: Dorsal nerve of clitoris, perineal, inferior rectal
nerves; S1-S4, anterior branches of the sacral plexus. 1, Internal
iliac artery; 2, superior gluteal artery; 3, inferior gluteal
artery; 4, obturator nerve; 5, internal obturator muscle; 6,
levator ani muscle (reflected); 7, levator ani muscle (cut); 8,
piriformis muscle; 9, sacrospinous ligament; 10, coccygeus muscle;
11, anococcygeal ligament; 12, coccyx bone 13, rectum. 14, pubic
bone; 15, sympathetic trunk. |
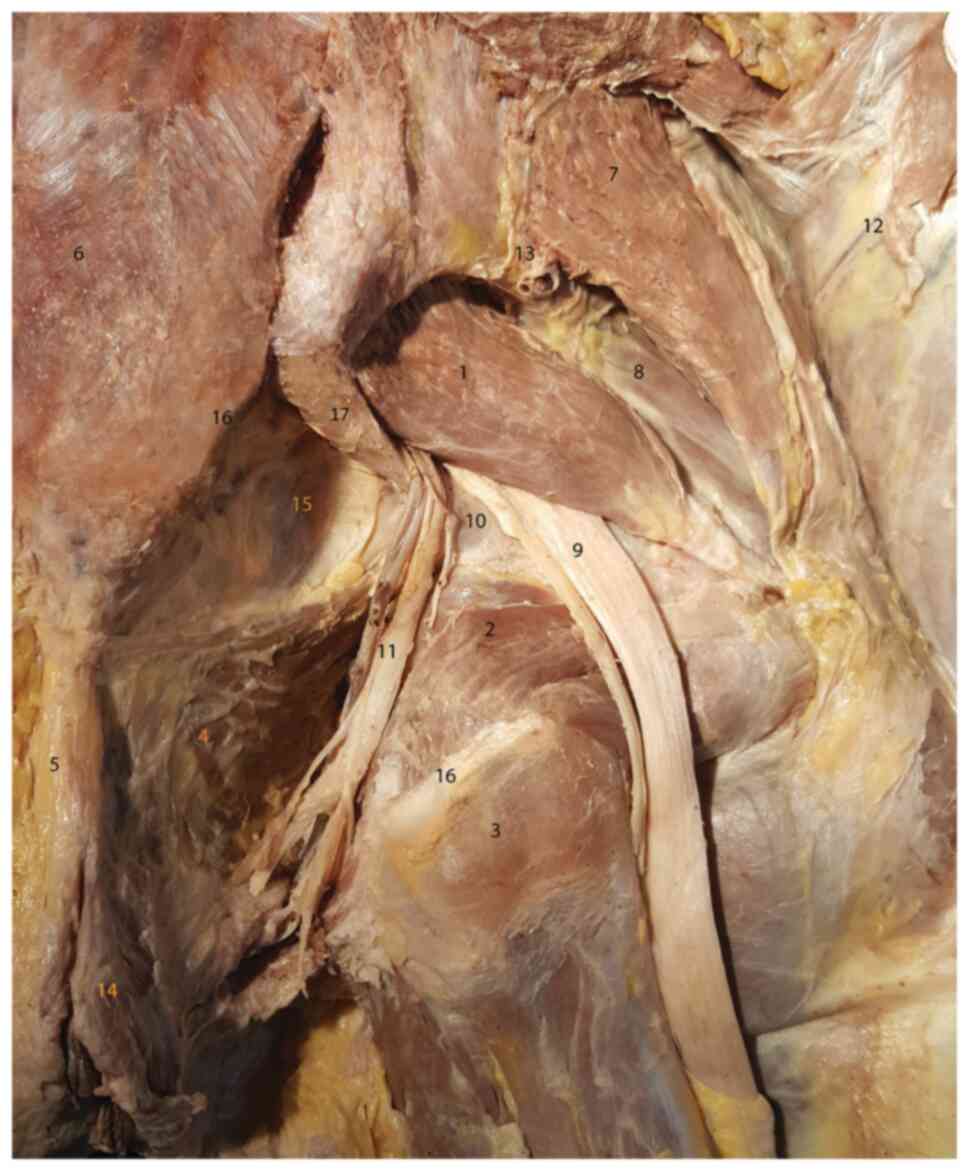
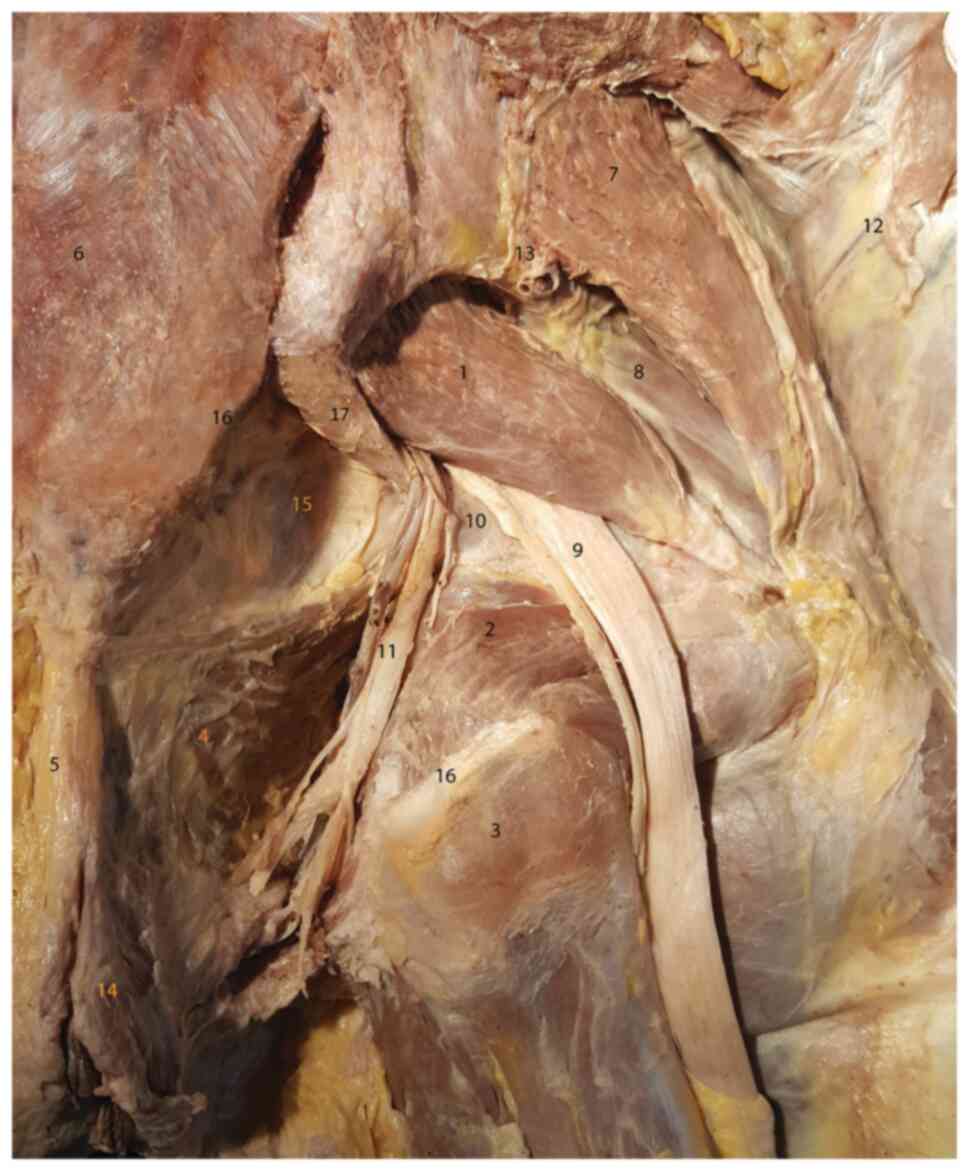 | Figure 2Dissection of the deep gluteal region
(posterior view). 1, Piriformis muscle; 2, internal obturator
muscle; 3, ischial tuberosity (posterior view); 4, levator ani
muscle (superior-medial border of the ischiorectal fossa); 5,
anococcygeal ligament; 6, sacrum; 7, gluteus medius muscle; 8,
gluteus minimus muscle; 9, sciatic nerve; 10, ischial spine; 11,
internal pudendal neurovascular bundle; 12, gluteus maximus muscle;
13, superior gluteal artery and vein; 14, external anal sphincter;
15, pelvic subperitoneal tissue visible after removing the
coccygeus muscle; 16, sacrotuberous attachment points (cut); 17,
sacrospinous ligament. |
As regards the general anatomical layout, the left
half of the pelvic floor is clearly visible. Due to its central
location, the sacrospinous ligament and the coccygeus muscle
separate the lateral pelvic wall into three zones: i) The
posterior-superior zone corresponds to the greater sciatic notch
and its content. In a deep plane, the piriformis muscle attaches to
the sacrum, with its origins slightly separated by the roots of the
sciatic nerve. The anterior divisions of the S2, S3 and S4 spinal
nerves give rise to the pudendal nerve. The dissection image
clearly shows that these roots can be compressed during the
contraction of the piriformis muscle. This nerve, together with the
internal pudendal artery, are closely associated with the rigid
superior border of the sacrospinous ligament, actually passing
between the piriformis muscle and the sacrospinous ligament and
then between the ligament and the upper border of the sciatic
spine. The elements of the internal pudendal neurovascular bundle
follow their extrapelvic course surrounding the ischial spine in
the deep gluteal region in order to reenter the pelvis through the
lesser sciatic notch. ii) The middle zone is dominated by the
attachments of the sacrospinous ligament and coccygeus muscle onto
the ischial spine, forming a rigid osteo-fibro-muscular structure.
iii) The anterior-inferior zone contains the contents of the lesser
ischial notch. In order to reach the internal pudendal
neurovascular bundle, the levator ani muscle was reflected
medially, thus obtaining favorable access towards the ischiorectal
fossa. On the lateral wall of this fossa, the pudendal canal
(Alcock canal) was opened, and the fibrous remnants of the fascia
were removed in order to emphasize the neurovascular content of the
canal. In close association with the osseous plane, the fascicles
of the internal obturator muscle unite in a common body that passes
below the inferior border of the ischial spine in its course
towards the femoral attachment.
The dissection shown in Fig. 2 was realized in the gluteal region,
following the lateral reflection of the gluteus maximus muscle (no.
12).
The image is centered on the emerging sciatic nerve
(no. 9) under the inferior border of the piriformis muscle (no. 1),
in the infrapiriform space. In the medial end of this space, the
internal pudendal neurovascular bundle (no. 11) exits the pelvis,
surrounds the ischial spine and reenters the pelvis along the
lateral wall of the ischiorectal fossa, in the Alcock canal, which
was removed on dissection.
It was observed that the internal obturator and
gemellus superior muscles surrounding the lesser sciatic notch run
towards its femoral attachment.
The image lacks the sacrotuberous ligament
superficially and the coccygeus muscle in the deep plane, as the
latter was removed in order to emphasize the connective and adipose
tissue within the pelvic subperitoneal space (no. 15).
In the ischiorectal fossa, the inferior rectal
branches of the internal pudendal neurovascular bundle lying
lateral to the anococcygeal ligament (no. 5) and the external anal
sphincter (no. 14) may be clearly seen.
The internal pudendal neurovascular bundle travels
through a critical zone between the piriformis muscle and the
sacrospinous ligament, in contact with the superior margin of the
ischial spine, where compression may occur. When this bundle
reenters the pelvis, it may traverse a compression zone between the
internal obturator muscle, the gemellus superior muscle and the
inferior border of the ischial spine.
The sciatic nerve may become compressed between the
inferior margin of the piriformis muscle and the superior margin of
the ischial spine.
Observations on imaging
examination
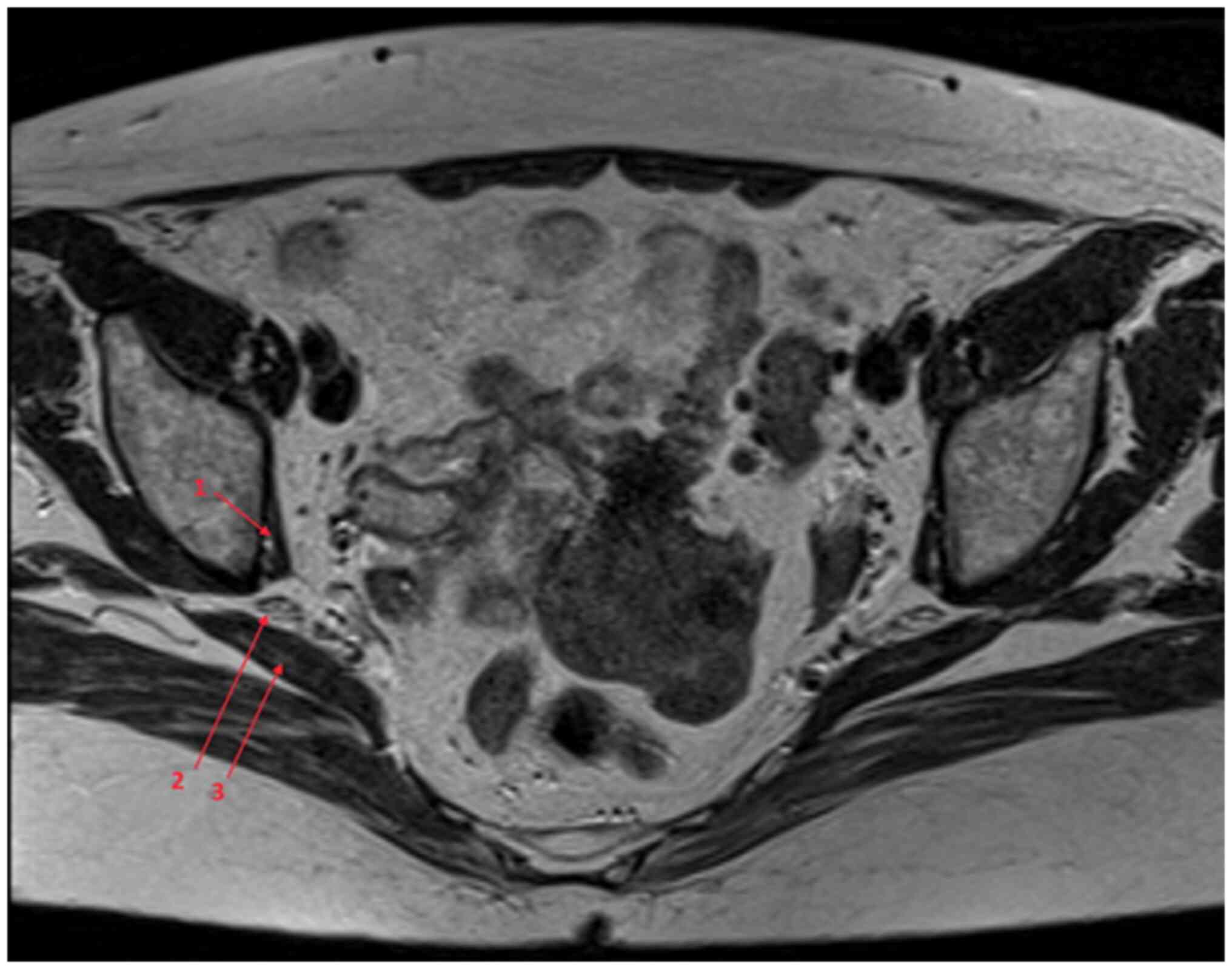
A transverse cross-section on MRI at the level of
the infrapiriform space is shown in Fig. 3. At this level, the sciatic nerve
travels through the anatomical space limited inferiorly by the
internal obturator muscle and superiorly by the piriformis
muscle.
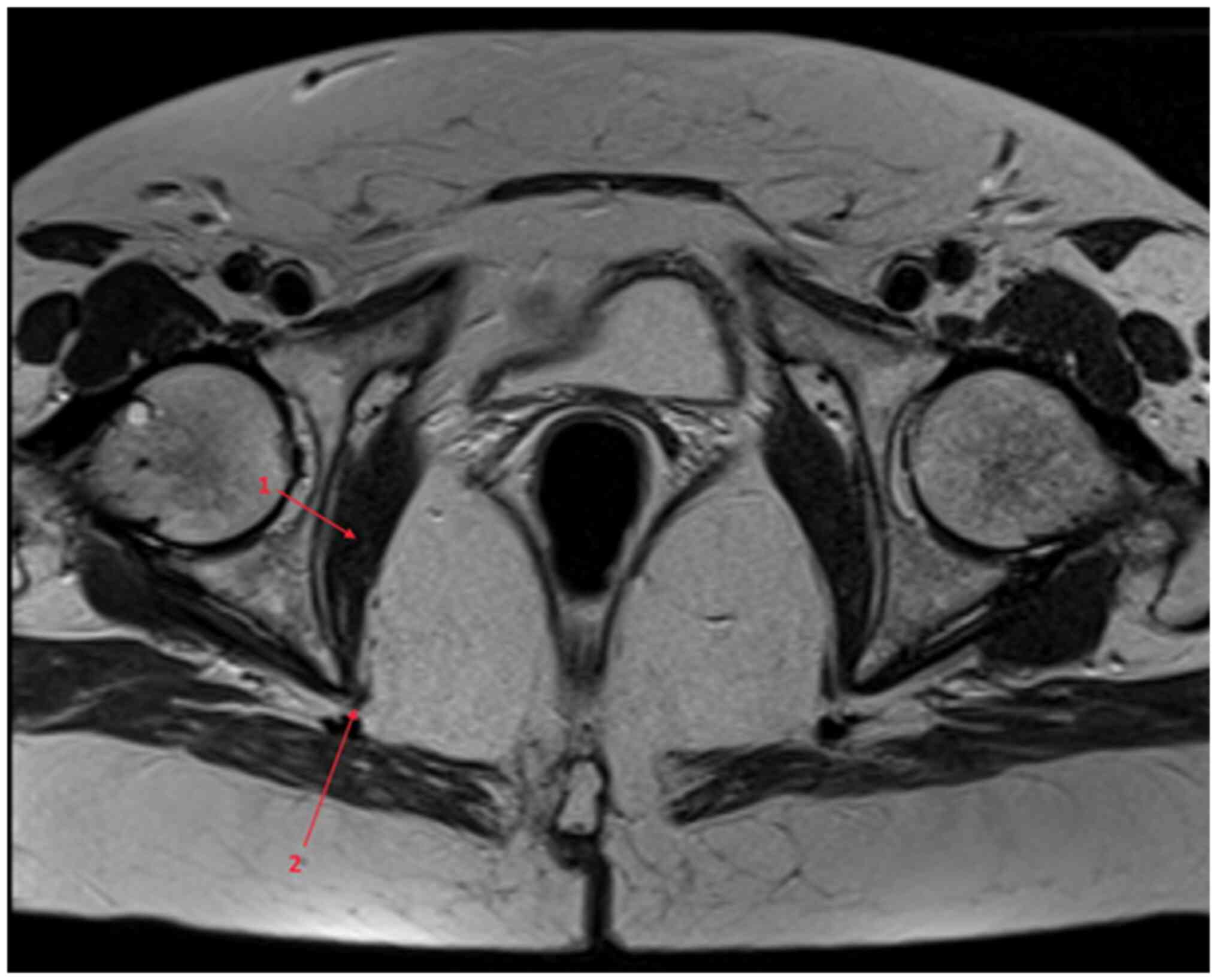
On the MRI scan shown in Fig. 4, the internal pudendal bundle can be
observed reentering the pelvis below the sciatic tuberosity,
attaching onto the medial surface of the internal obturator muscle,
on the lateral wall of the ischiorectal fossa.
Discussion
Along the course of the sciatic nerve and the
internal pudendal bundle, there are several anatomical associations
that may become involved in the compression of the nerve
structures, generating the symptoms specific to the piriformis
syndrome.
The aim of the present study was to establish clear
osseous and muscular landmarks for the MRI evaluation of such
associations.
Several aspects are important for the imaging
evaluation of the nerve tracts, such as identifying the piriformis
muscle in the greater sciatic notch, identifying the internal
obturator muscle in its course below the ischial spine, evaluation
of the upper and lower borders of the ischial spine, and sequential
evaluation of the course of the neurovascular bundles.
The difficulty of the evaluation using MRI lies with
the oblique orientation of the sacrum and the piriformis muscle,
the curving tendency of the internal obturator muscle and the
combined intra- and extrapelvic course of the internal pudendal
bundle.
The sciatic nerve can be compressed along its course
in the following locations. Its roots can be compressed
intrapelvically by the origins of the piriformis muscle; its trunk
can be compressed in the infrapiriform space between the inferior
border of the piriformis muscle and the upper border of the ischial
spine.
The internal pudendal nerve can be compressed along
its course in several locations: In its intrapelvic course, it may
be compressed in the anterior-inferior part of the piriformis
muscle and in the superior border of the sacrospinous ligament. In
this part, there are also rare cases of pudendal nerve syndrome
entrapment associated with ganglion cysts (19).
Between the piriformis muscle and the border of the
greater sciatic notch, there is a space that contains the sciatic
nerve (posterior), the internal pudendal and superior gluteal
arteries (middle) and the internal pudendal nerve, in direct
contact with the upper border of the ischial spine (anterior). At
this point, the pudendal nerve is not clearly distinguishable on
MRI scans. This is the compression region associated with the
definition of the piriformis syndrome.
In its extrapelvic course, the internal pudendal
nerve runs in the medial part of the infrapiriform space. In the
infrapiriform space, the bundle runs the following course: Upon
entering this space, the internal pudendal bundle is actually
located between the inferior border of the piriformis muscle and
the tip of the ischial spine. Next, the bundle surrounds the
lateral aspect of the sciatic spine (Fig. 2) and then reenters the pelvis
through the lesser sciatic notch, in contact with the inferior
border of the ischial spine passing between the spine, the superior
gemellus and internal obturator muscles.
In its intraperineal course, the bundle travels
along the internal aspect of the internal obturator muscle, inside
the Alcock canal. In this part, the nerve is unlikely to be
compressed by extrinsic structures.
The classical piriformis syndrome consists of the
compression of the sciatic and/or internal pudendal nerves by the
piriformis muscle. It is suggested that the compression of the
internal pudendal bundle outside the piriformis muscle may lead to
a ‘piriformis syndrome-like’ symptomatology. We herein explained
the anatomical basis for the internal pudendal nerve syndrome,
showing the compression zones that may lead to symptoms of perineal
pain.
Establishing clear anatomical landmarks and
relations in the intra- and extrapelvic course of the sciatic and
internal pudendal nerves may prove valuable for the evaluation of
the course of these nerves through MRI.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data and images used and/or analyzed during the
current study are available from the corresponding author on
reasonable request.
Authors' contributions
OCG, ME, ADT, RT, IAV AEN, DD, DI, DG, AM and FMF
designed the study, performed a literature search and selected the
included studies, and wrote the manuscript. OCG, ME, ADT, RT, IAV
AEN, DD, DI, DG, AM and FMF critically revised the manuscript for
important intellectual content. ME, FMF and ADT confirm the
authenticity of the raw data. All the authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The cadavers used in the present study were provided
by the Department of Morphological Sciences, Discipline of Anatomy
of the University of Medicine and Pharmacy (Bucharest, Romania).
The Research Ethics Committee of the University of Medicine and
Pharmacy ‘Carol Davila’ approved the use of human cadavers for the
purposes of this study (approval no. 210763/06.10.2021). The Ethics
Committee of the ‘Victor Babeş’ Diagnosis and Treatment Center
approved the use of pelvic MRI examination for the purpose of this
study (approval no. 1647/03.06.2020).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Anbumani TL, Thamarai SA and Anthony AS:
Sciatic nerve and its variations: An anatomical study. Int J Anat
Res. 3:1121–1127. 2015.
|
|
2
|
Ripani M, Continenza MA, Cacchio A, Barile
A, Parisi A and De Paulis F: The ischiatic region: Normal and MRI
anatomy. J Sports Med Phys Fitness. 46:468–475. 2006.PubMed/NCBI
|
|
3
|
Chang C, Jeno SH and Varacallo M: Anatomy,
bony pelvis and lower limb, piriformis muscle. In: StatPearls.
Treasure Island (FL): StatPearls Publishing, 2021.
|
|
4
|
Hopayian K, Song F and Sambandan RRS: The
clinical features of the piriformis syndrome: A systematic review.
Eur Spine J. 19:2095–2109. 2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Carro LP, Hernando MF, Cerezal L, Navarro
IS, Fernandez AF and Castillo AO: Deep gluteal space problems:
Piriformis syndrome, ischiofemoral impingement and sciatic nerve
release. Muscles Ligaments Tendons J. 6:384–396. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Beaton LE and Anson BJ: The relation of
the sciatic nerve and its subdivisions to the piriformis muscle.
Anat Rec. 70:1–5. 1937.
|
|
7
|
Pećina M: Contribution to the etiological
explanation of the piriformis syndrome. Acta Anat (Basel).
105:181–187. 1979.PubMed/NCBI
|
|
8
|
Vij N, Kiernan H, Bisht R, Singleton I,
Cornet EM, Kaye AD, Imani F, Varassi G, Pourbahiri M, Viswanath O
and Urits I: Surgical and non-surgical treatment options for
piriformis syndrome: A literature review. Anesth Pain Med.
11(e112825)2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yeoman W: The relation of arthritis of the
sacro-iliac joint to sciatica, with an analysis of 100 cases.
Lancet. 212:1119–1123. 1928.
|
|
10
|
Freiburg AH and Vinke TA: Sciatica and the
sacroiliac joint. J Bone Joint Surg. 16:126–36. 1934.
|
|
11
|
Beaton LE and Anson BJ: The sciatic nerve
and the piriformis muscle. Their interrelation a possible cause of
coccygodynia. J Bone Joint Surg. 20:686–688. 1938.
|
|
12
|
Robinson D: Piriformis syndrome in
relation to sciatic pain. Am J Surg. 73:356–358. 1947.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Hopayian K and Danielyan A: Four symptoms
define the piriformis syndrome: An updated systematic review of its
clinical features. Eur J Orthop Surg Traumatol. 28:155–164.
2018.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Papadopoulos EC and Khan SN: Piriformis
syndrome and low back pain: A new classification and review of the
literature. Orthop Clin North Am. 35:65–71. 2004.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hopayian K and Heathcote J: Deep gluteal
syndrome: An overlooked cause of sciatica. Br J Gen Pract.
69:485–486. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Martin HD, Kivlan BR, Palmer IJ and Martin
RL: Diagnostic accuracy of clinical tests for sciatic nerve
entrapment in the gluteal region. Knee Surg Sports Traumatol
Arthrosc. 22:882–888. 2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Martin HD, Shears SA, Johnson JC, Smathers
AM and Palmer IJ: The endoscopic treatment of sciatic nerve
entrapment/deep gluteal syndrome. Arthroscopy. 27:172–181.
2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Park JW, Lee YK, Lee YJ, Shin S, Kang Y
and Koo KH: Deep gluteal syndrome as a cause of posterior hip pain
and sciatica-like pain. Bone Joint J. 102:556–557. 2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kim YJ and Kim DH: Pudendal nerve
entrapment syndrome caused by ganglion cysts along the pudendal
nerve. Yeungnam Univ J Med. 38:148–151. 2021.PubMed/NCBI View Article : Google Scholar
|