Introduction
Radical mastoidectomy has been performed as early as
the 16th century and its main purpose is to eradicate chronic
otitis media or cholesteatoma and create anatomical conditions to
prevent reoccurrence (1). By
anatomic (drainage) results, it is understood that removing
lesions, maintaining unobstructed drainage and reducing
complications both intra and extracranial is required to obtain a
reliable, safe and disease-free middle-ear (2,3). The
usual surgical approach is represented by canal wall-up (CWU) and
the canal wall-down (CWD) mastoidectomies. Intact canal wall
procedures, such as CWU, are known to be associated with high risk
of recurrence and residual inflammatory lesions (4), but at the same time they preserve much
of the anatomy, while radical and radical modified mastoidectomy
techniques, such as CWD, allow for good visualization of structures
and consequently proportional good chances of complete removal of
lesions (5). It is however certain
that while pursuing anatomic results (complete drainage and cavity
cleanliness), the functional results are occasionally poor (hearing
is destroyed or at least gravely impaired) as we have stated in our
previous two studies involving the same cohort of patients
(6,7). We found that recreating the continuity
of the ossicular chain (OC) is paramount both for functional and
anatomical results in middle ear surgery (8,9), but
useless without a well-performed mastoidectomy. These aspects
should not be taken lightly since hearing loss represents one of
the most serious afflictions worldwide (World Health Organization
estimates that between 65 and 330 million individuals suffer from
some form of middle ear suppuration and 50% of them suffer from
hearing impairment) (10). Other
environmental and clinical risk factors cannot be ruled out and the
clinician must always bear in mind that a situation where genetic
predisposition is augmented by environmental factors is common and
even more complicated (10).
Thus, the aim of the present study was to determine
to what extent can a completely and permanently ‘dry ear’ be
expected and identify the potential parameters that most influence
the drainage results.
Patients and methods
Patient selection
The same cohort of patients used in our previous
studies on the long-term functional results of mastoidectomy and
long-term results of ossicular replacement with biovitroceramic
prosthesis (6,7) were used in the present study. We find
it important to be able to compare functional, anatomical and
reconstructive results for the same patients, using the same
surgical techniques and communicate long-term data. This
retrospective non-controlled study took into consideration the same
random selection of 200 long-term patients with both radical CWD
and modified radical mastoidectomy (MRM), performed over a 3-year
period. The techniques for both types of surgery are well-known and
described in literature (5,11,12).
The initial cohort was comprised of 209 patients, of which nine
died (eight of causes non-related to middle-ear disease, one
directly related to middle-ear disease after otogenic brain
abscess). The basic statistical criteria for the selection were
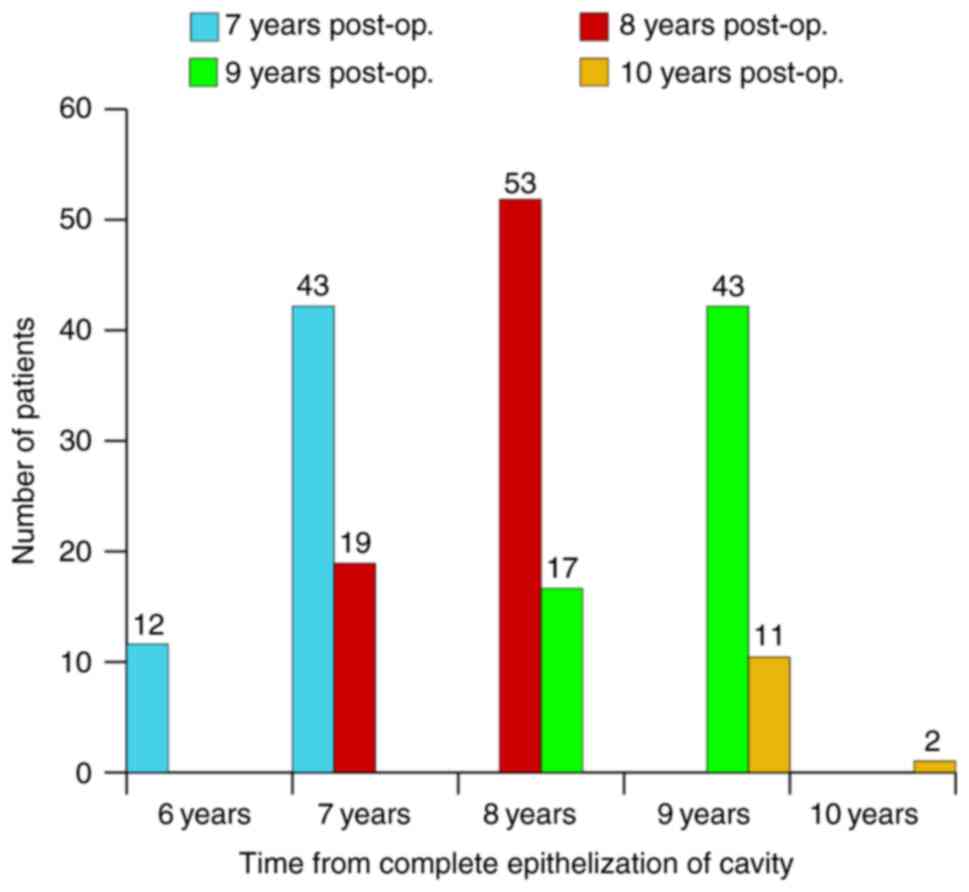
post-operative time span. Data analysis began in 2004, giving a
post-operative follow-up period of 8.12 years for the entire cohort
from the moment of surgery, and 7.86 years from the time of
complete epithelization of cavity, which allows us to consider it
as long-term evaluation. All patients were clinically evaluated
(microscope otoscopy), both before the surgery and after the
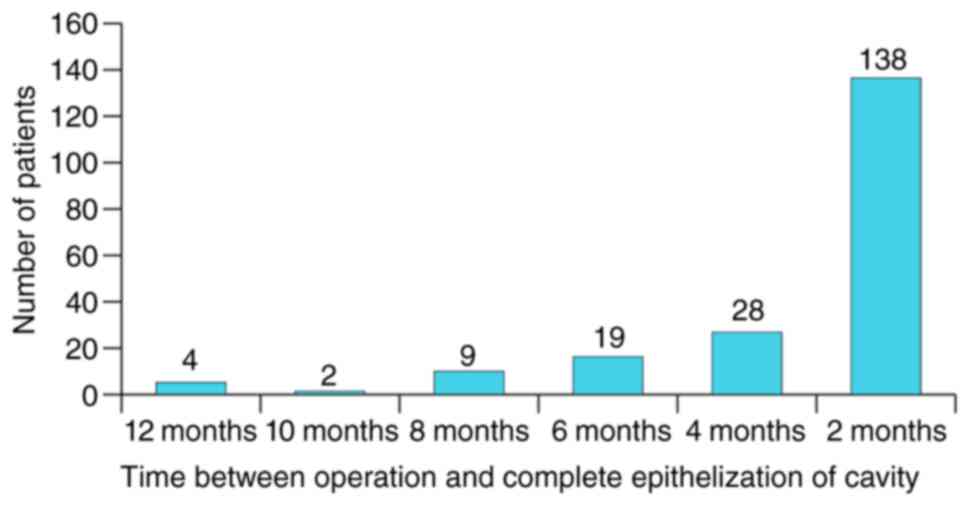
surgery as follows: i) Monthly for the first 6 months
post-operative; ii) every 2 months for the next 6 months (up to 1
year, corresponding to the moment of complete epithelization of
cavity for >80% of cases); iii) every 6 months in the 2nd year;
iv) every 8 months for the 3rd and 4th year post-op; and v) every
12-16 months for the 5th year post-op and also at any other
occurrent otorrhea episode. The follow-up of drainage results
started from the moment of complete epithelization of cavity for
each patient (Figs. 1 and 2).
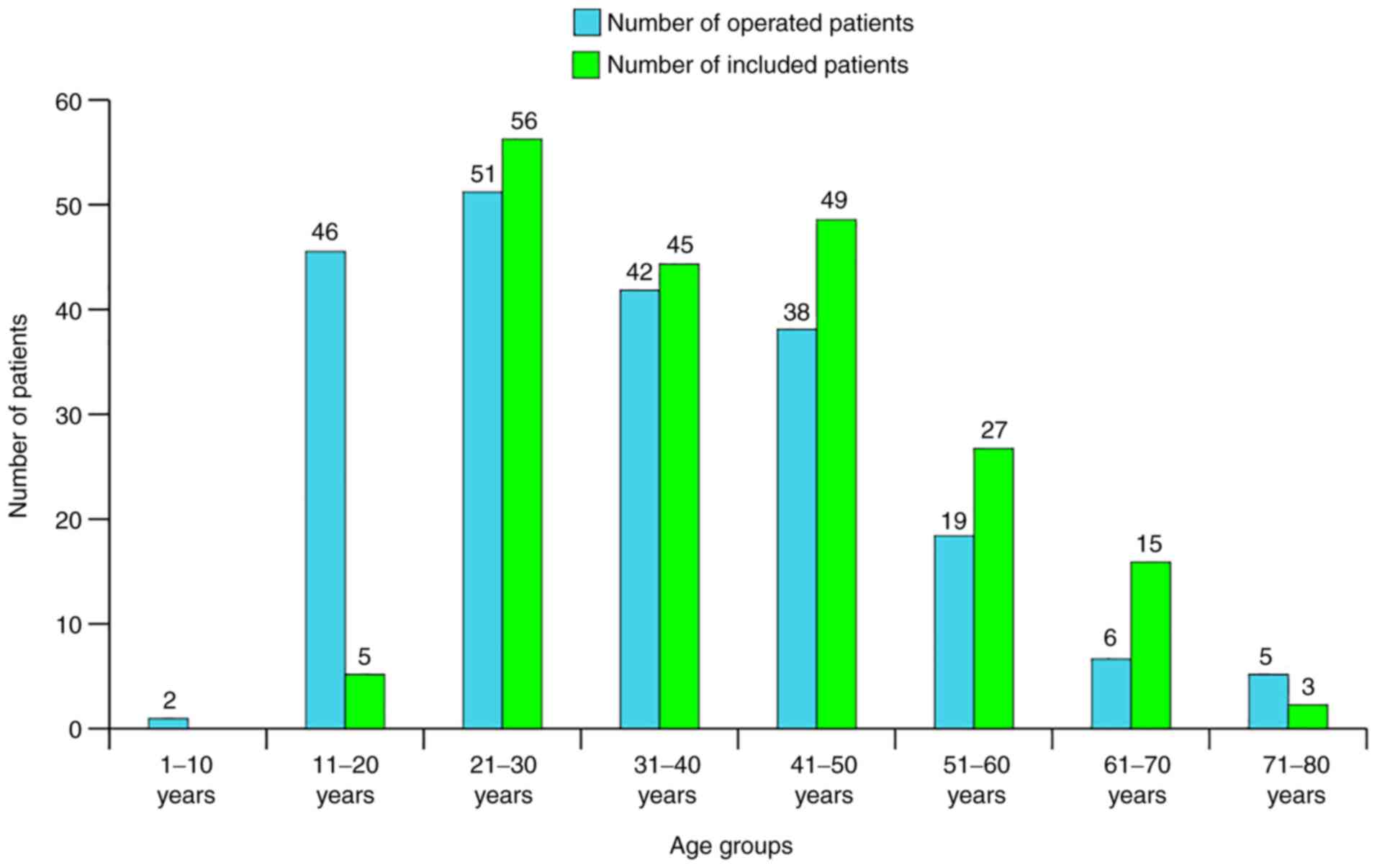
It is also noteworthy to point out the shift in the
age group distribution of patients that follows the long-term study
of a cohort (Fig. 3). Age was
defined at the time of surgery as: Physical time, duration of
evolution, aging (progressive degradation of function at different
rates), an unstoppable increase in damaged cells proportion,
increase of degree or intensity of disease, rise of hearing
thresholds-all of these being included in a formalized model
(physical-mathematical model).
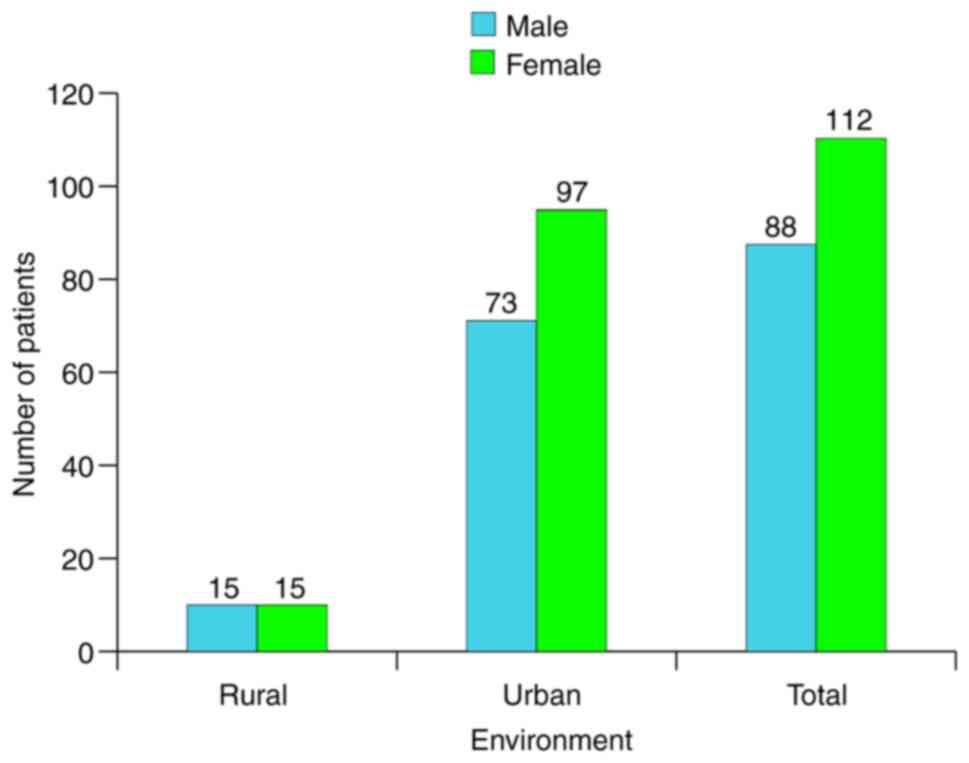
The distribution of sex and environment is presented
in absolute frequencies in Fig.
4.
Paraclinical diagnosis
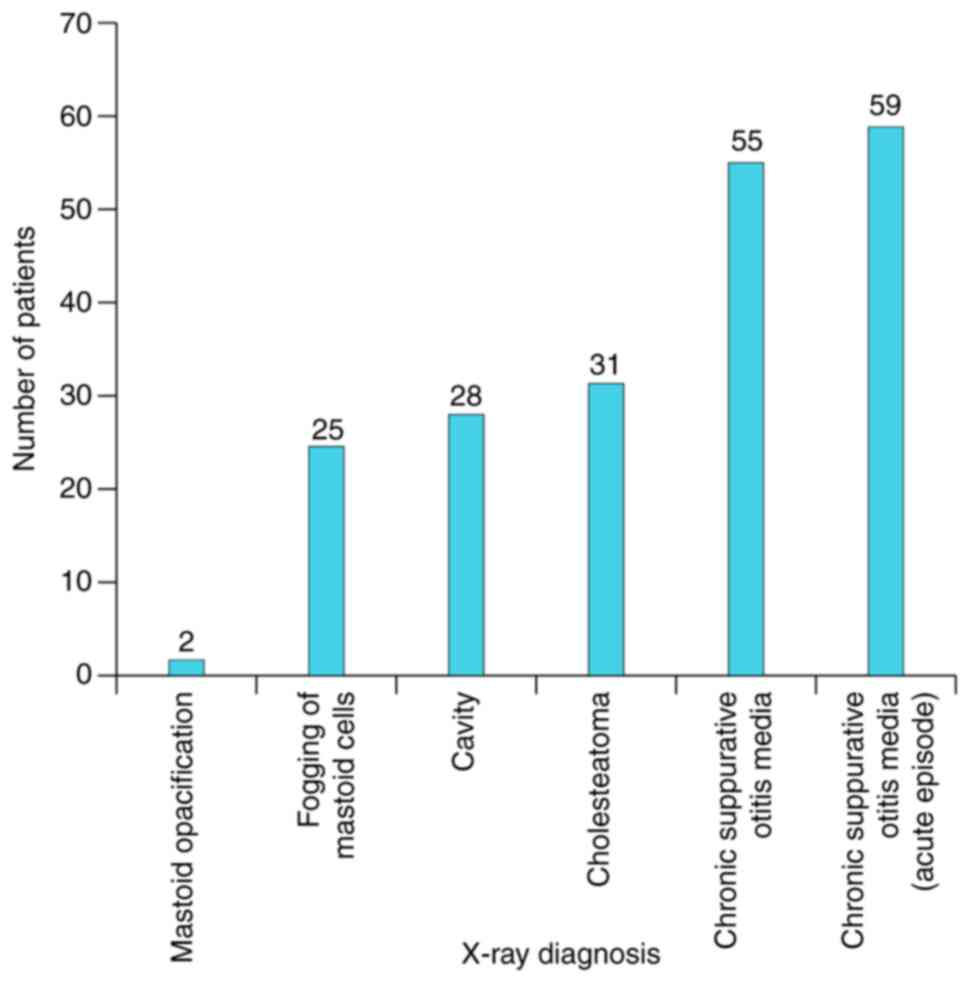
Radiological examination was also performed for all
patients (bilateral X-ray in Schuller's view) with high degree of
sensitivity and specificity for mastoid diagnosis. A total of 55%
(n=31) of the cholesteatoma cases and 61% (n=28) of previously
operated ears could be correctly diagnosed (Fig. 5).
The main goal of the present study was to define the
situations and factors that influence the drainage results of
mastoidectomy that could provide us with some type of anatomical
prognosis. Based on the selection criteria of the studied group and
by performing statistical analysis of the correlation of anatomic
results and statistically significant variables, pertinent
conclusions could be formulated regarding the drainage success rate
of mastoidectomy.
Statistical analysis
Although largely clinical, this study also included
some statistical analysis, including creating Microsoft Excel
databases and attributing codes to facilitate data analysis using
Excel (Microsoft Corporation) and SPSS v15 (SPSS, Inc.). Factors
such as age of patient, presence of cholesteatoma, stage of disease
etc., were associated with the functional results of mastoidectomy.
Data were synthesized as percentage, mean values and standard
deviation. P<0.05 was considered to indicate a statistically
significant difference. Parametric (unpaired Student's t-test) or
non-parametric (Mann-Whitney) tests were also applied.
Studied variables Pre-surgery
variables
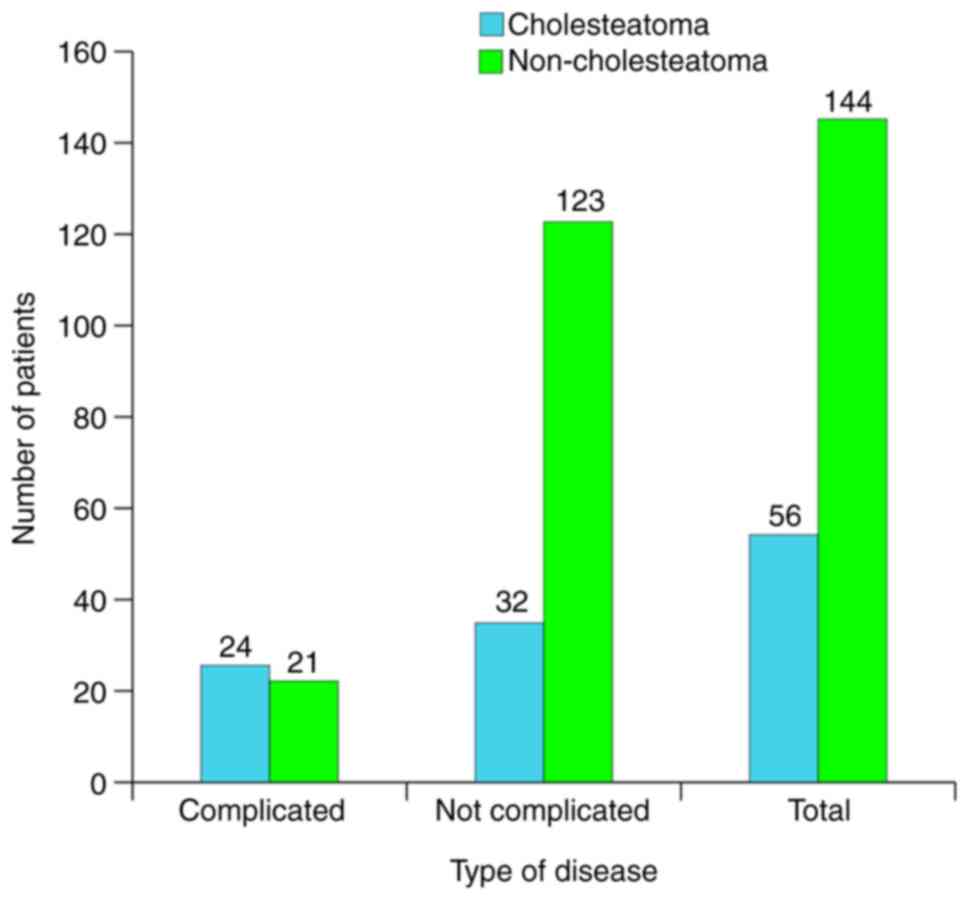
Pre-surgery variables were as follows: i) Age group,
0-10 years (n=1), 11-20 years (n=4), 21-30 years (n=56), 31-40
years (n=45), 41-50 years (n=49), 51-60 years (n=27), 61-70 years
(n=15) or 71-80 years (n=3); ii) clinical stage of disease,
complicated (n=45) or not complicated (n=155); iii) type of
disease, cholesteatoma (n=56) or non-cholesteatoma (n=144); and iv)
type of tympanic membrane perforation, marginal (n=75) or central
(n=125).
Intraoperative data
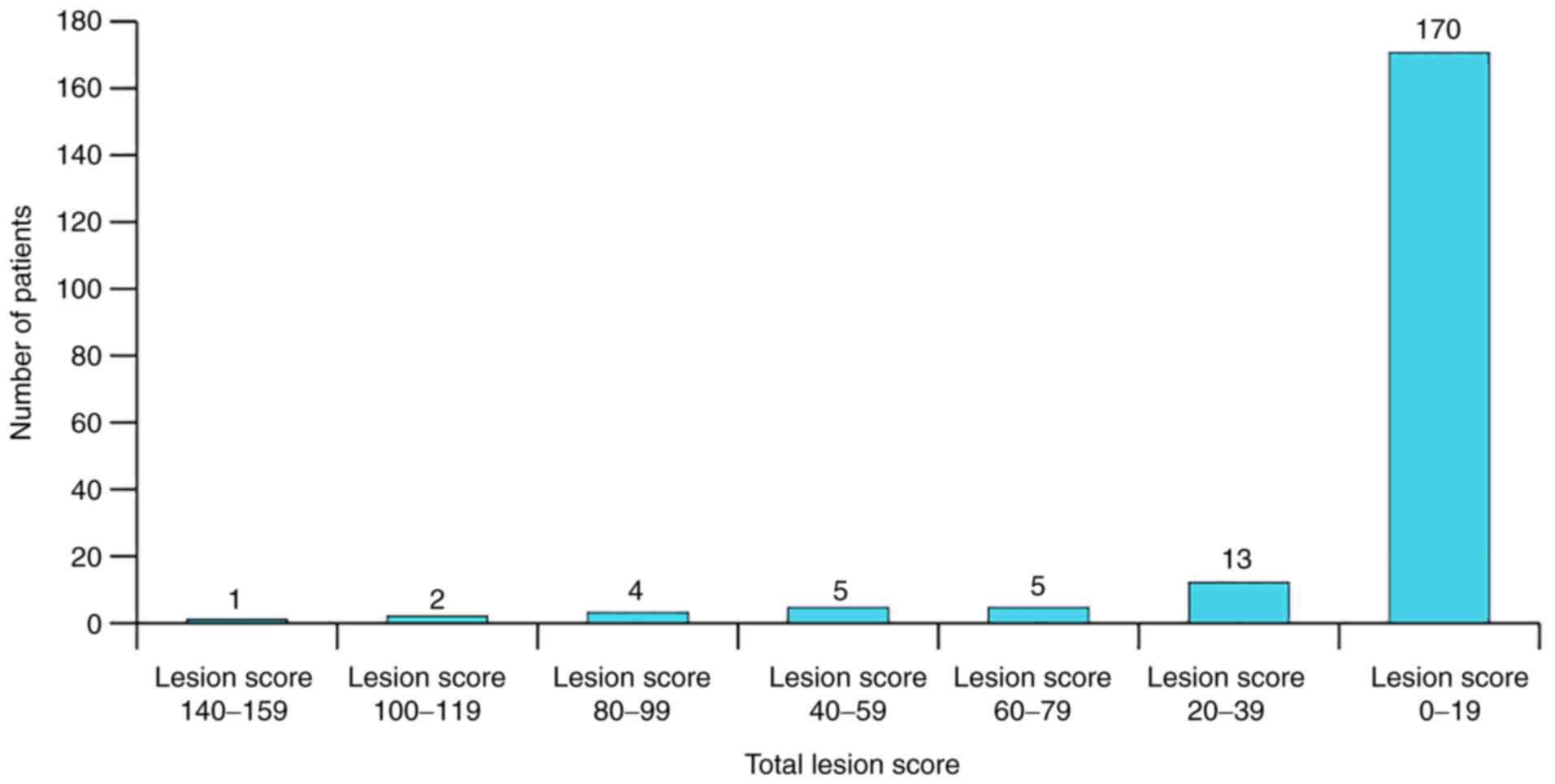
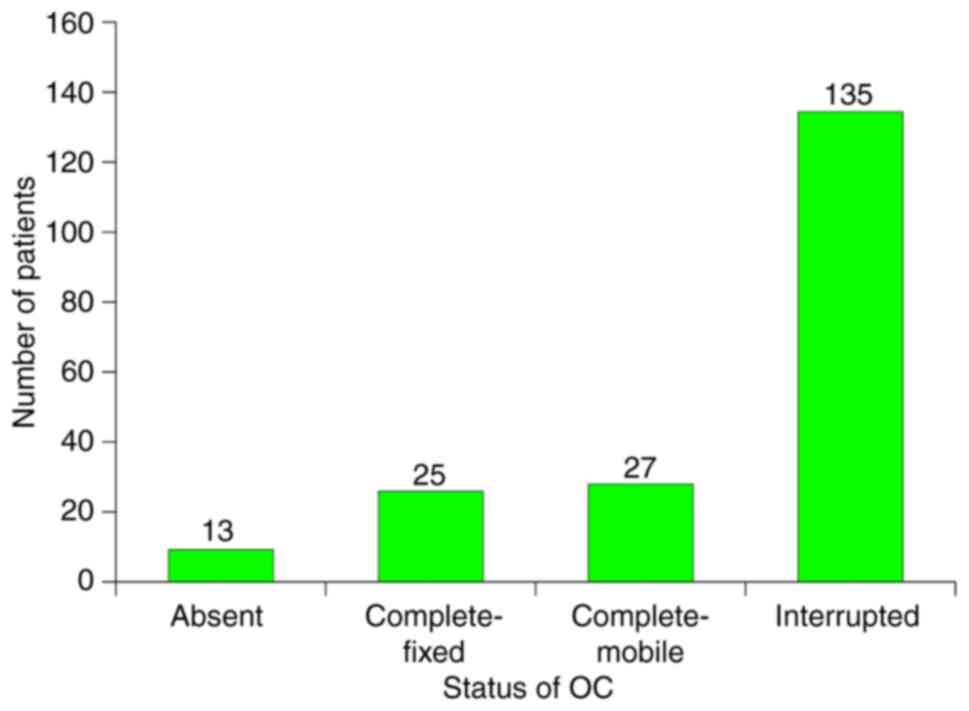
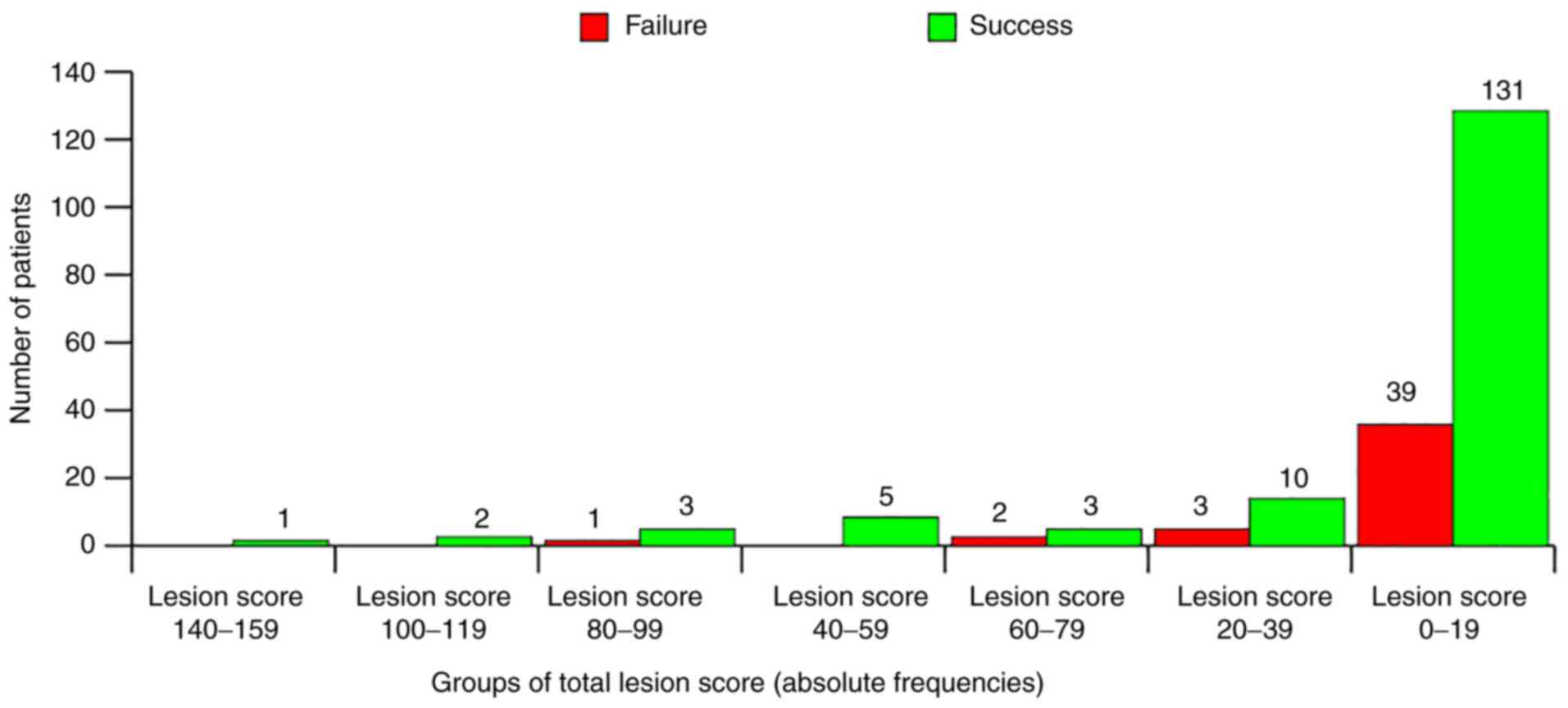
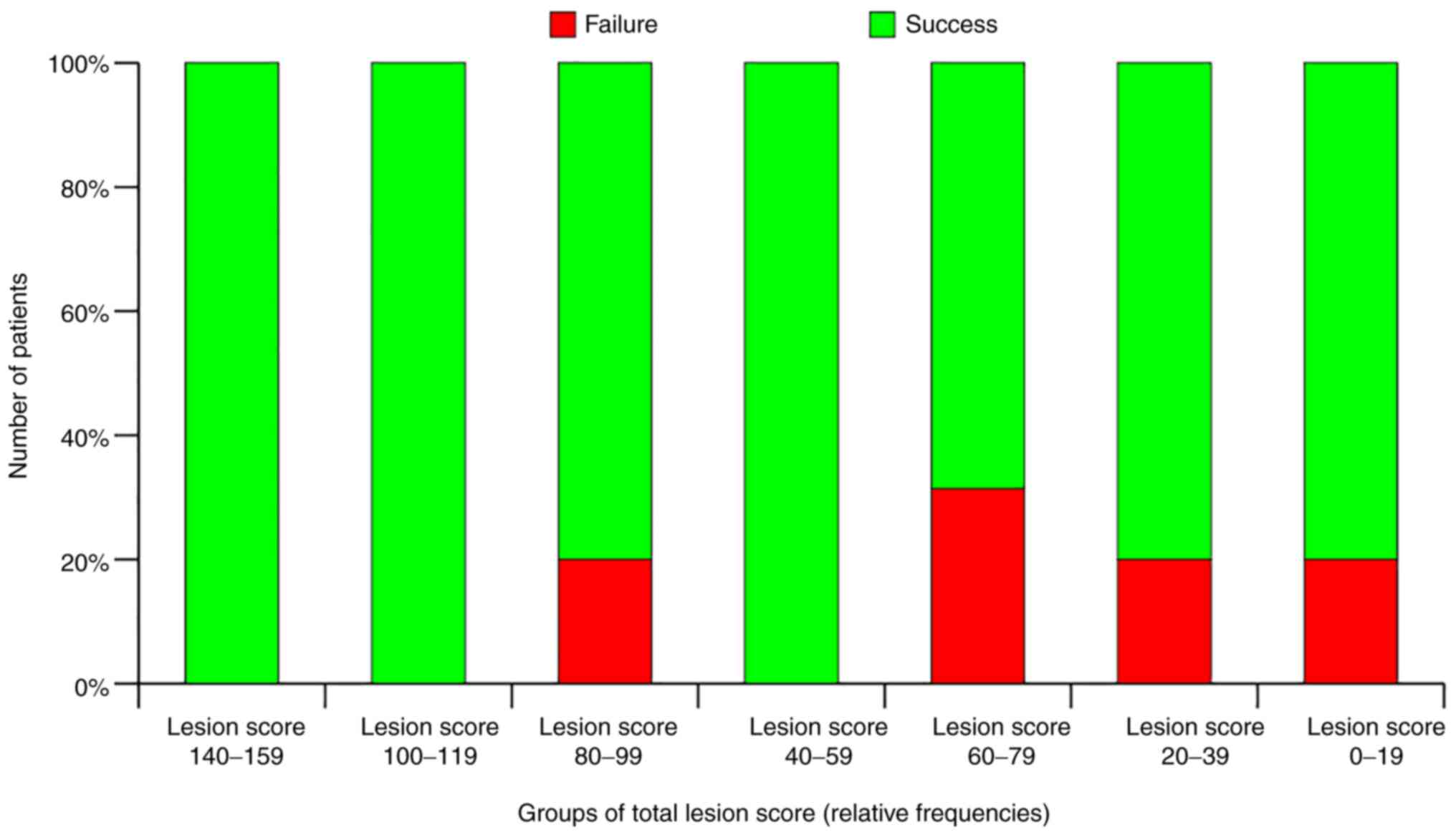
Intraoperative data variables were as follows: i)
Type of mastoidectomy, modified radical (n=125) or radical (n=75);
ii) OC status, absent (n=13), complete and mobile (n=27), complete
and fixed (n=25), or interrupted (n=135); and iii) total lesion
score, 0-19 (n=170), 20-39 (n=13), 40-59 (n=5), 60-79 (n=5), 80-99
(n=4), 100-119 (n=2) or 140-159 (n=1).
Follow-up data
Follow-up data variables were as follows: i) Period
for complete epithelization of cavity, 2 months, 1 year, 2 years,
3-4 years or 8 years; ii) cavity self-cleansing, present or absent;
and iii) mastoidectomy result (drainage effect), failure or
success.
Results and Discussion
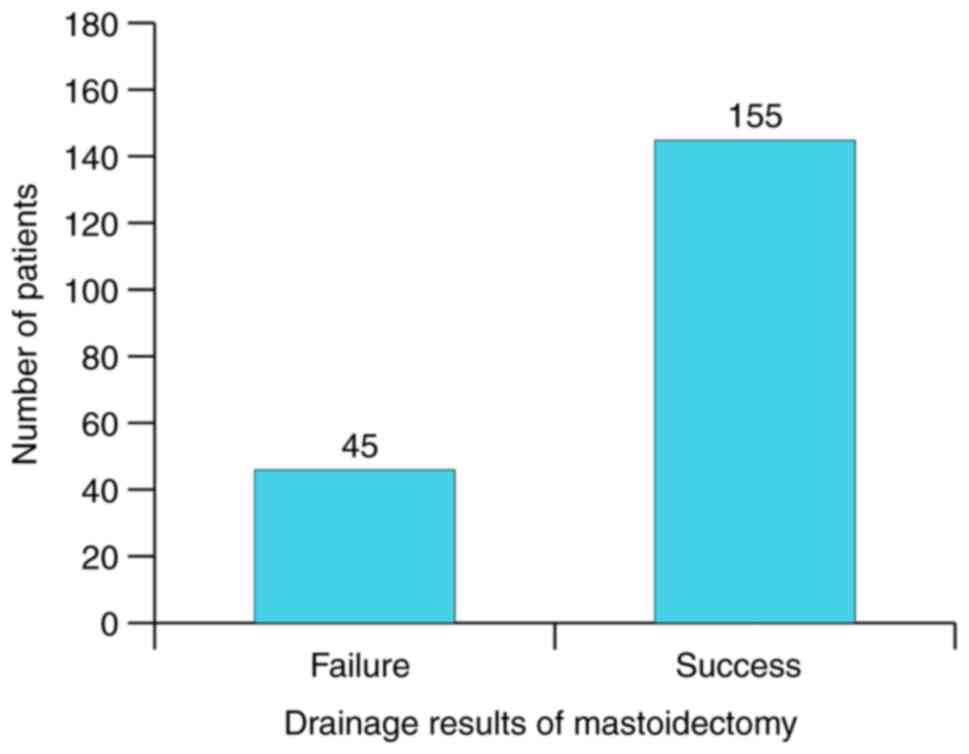
Successful mastoidectomy was defined in the present
study as the total absence of otorrhea episodes after total
epithelization of cavity and by failure of the presence of at least
one such episode. According to this definition the global drainage
results of mastoidectomy could be appreciated in this study. What
remained to be determined was to what extent could a completely and
permanently ‘dry ear’ be expected, and to identify the potential
parameters that most influenced the outcome.
Fig. 6 shows the
distribution of patients associated with the type of disease and
presence of complications. A total of 23% of patients (n=45)
presented with complications, but it was observed that
cholesteatoma cases had a 43% rate of complications, whilst
non-cholesteatoma cases had only 16%.
Complications of disease have predictive clinical
significance, which can be hierarchized (Table I). For obtaining an exact
quantitative lesion profile (including all other lesions except
those of the middle-ear mucosa, protympanum, tympanic cavity,
aditus to mastoid antrum, mastoid bone and petrous apex), points
were assigned (directly proportional to presumed gravity) for each
type of lesion (Table II). Vertigo
for instance was 3.36 times more significant than facial paralysis
and exteriorization and 4.56 times less significant than sudden
hearing loss (Tables I and II). It was considered most surprising
that the proportion of middle cranial fossa dehiscence was the
largest, and equally surprising was the proportion of Fallopian
canal dehiscence and its ratio to clinically documented facial
paralysis. This meant that patients could be categorized by this
lesion score, as seen in Fig.
7.
 | Table IAbsolute and relative frequencies of
complications. |
Table I
Absolute and relative frequencies of
complications.
| Type of
complication | Number of
patientsa | Relative frequency,
% |
|---|
| MCF internal
cortical dehiscence | 39 | 20.0 |
|
Vertigob | 37 | 18.5 |
| Fallopian canal
dehiscence | 24 | 12.0 |
|
Deafnessb | 22 | 11.0 |
| Macroscopic
labyrinth lesion | 17 | 8.5 |
| Sigmoid cortical
dehiscence | 15 | 7.5 |
| PCF internal
cortical dehiscence | 14 | 7.0 |
| Fungal
pachymeningitis | 14 | 7.0 |
| Facial
paralysisb | 11 | 5.5 |
| Exteriorization of
suppurative processb | 11 | 5.5 |
| Lateral
semicircular canal fistula | 11 | 5.5 |
| Sudden hearing
lossb | 8 | 4.0 |
| Macroscopic facial
nerve lesion | 7 | 3.5 |
| Sigmoid sinus
phlebitis | 6 | 3.0 |
| Labyrinthine
fistula | 6 | 3.0 |
| Posterior
semicircular canal fistula | 5 | 2.5 |
| Extradural abscess
PCF | 3 | 1.5 |
| Extradural abscess
MCF | 2 | 1.0 |
| Acute
meningitis | 1 | 0.5 |
| Mandibular fossa
abscess (extra-articular) | 1 | 0.5 |
| Cerebellum
abscess | 1 | 0.5 |
 | Table IILesion scores for complications. |
Table II
Lesion scores for complications.
| Intra-operative
lesion | Attributed
score | Ordinal of
scores |
|---|
| Cerebellum
abscess | 20 | 1 |
| Cerebral
abscess | 20 | 1 |
| Sigmoid sinus
thrombophlebitis | 15 | 2 |
| Extradural abscess
MCF | 10 | 3 |
| Extradural abscess
PCF | 10 | 3 |
| Acute
meningitis | 10 | 3 |
| Sigmoid sinus
periphlebitis | 10 | 3 |
| Total lysis of
stapes footplate | 9 | 4 |
| Lateral
semicircular canal fistula | 9 | 4 |
| Posterior
semicircular canal fistula | 9 | 4 |
| Labyrinthine
fistula | 9 | 4 |
| Macroscopic
labyrinth lesion | 9 | 4 |
| Fungal
pachymeningitis | 9 | 4 |
| Mandibular fossa
abscess (extra-articular) | 8 | 5 |
| MCF internal
cortical dehiscence | 8 | 5 |
| PCF internal
cortical dehiscence | 8 | 5 |
| Sigmoid cortical
dehiscence | 8 | 5 |
| Exteriorization of
suppurative processa | 8 | 5 |
| Fallopian canal
dehiscence | 7 | 6 |
| Macroscopic facial
nerve lesion | 7 | 6 |
| Facial
paralysisa | 7 | 6 |
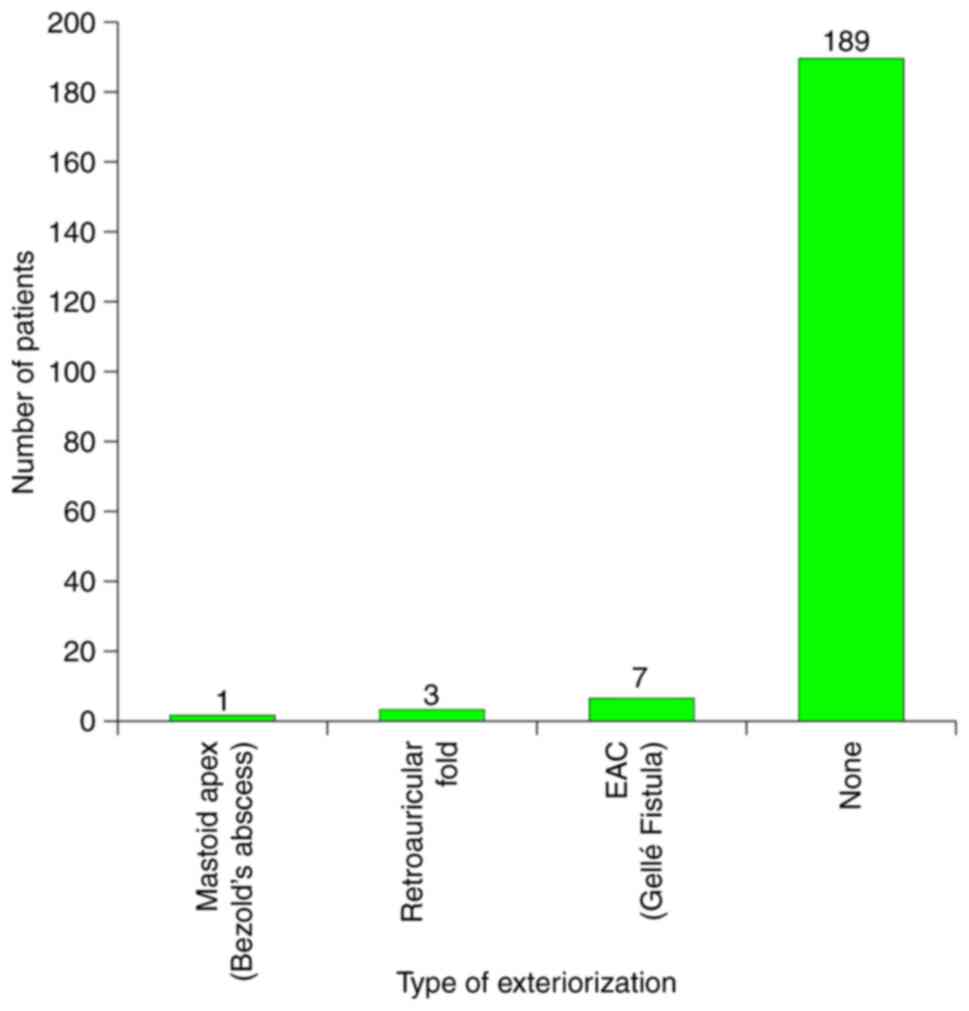
Another important parameter studied was the type of
exteriorization of the suppurative mastoid disease. The relative
frequency of these exteriorizations is presented in Fig. 8 and yielded noteworthy results.
Gellé's fistula (collapse of the posterosuperior meatal wall) had
the highest baring of 63% (n=7), followed by retroauricular fistula
27% (n=3), Bezold's abscess 9% (n=1).
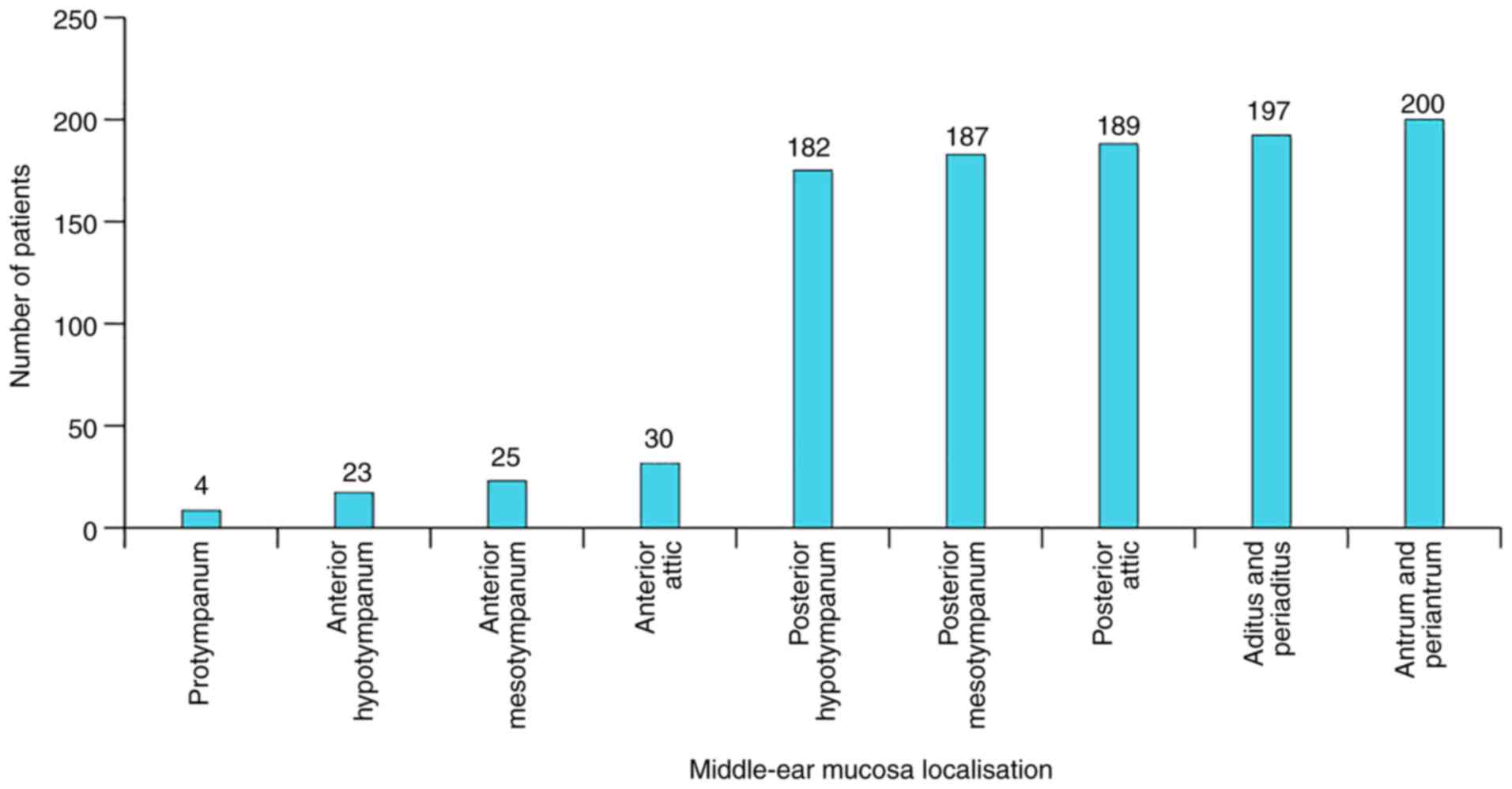
It is of note that the lesions of middle-ear mucosa
followed the frequency internal distribution law. By internal, it
is meant that the structure of the distribution is identical to the
topographic structure of middle-ear cavities. If these cavities are
considered as a co-axial suite, it could be observed that the
structure of absolute frequencies acted similarly to a non-linear
orderly series with an inflexion corresponding to the barrier
between the anterior and posterior half of the tympanic cavity
(Fig. 9).
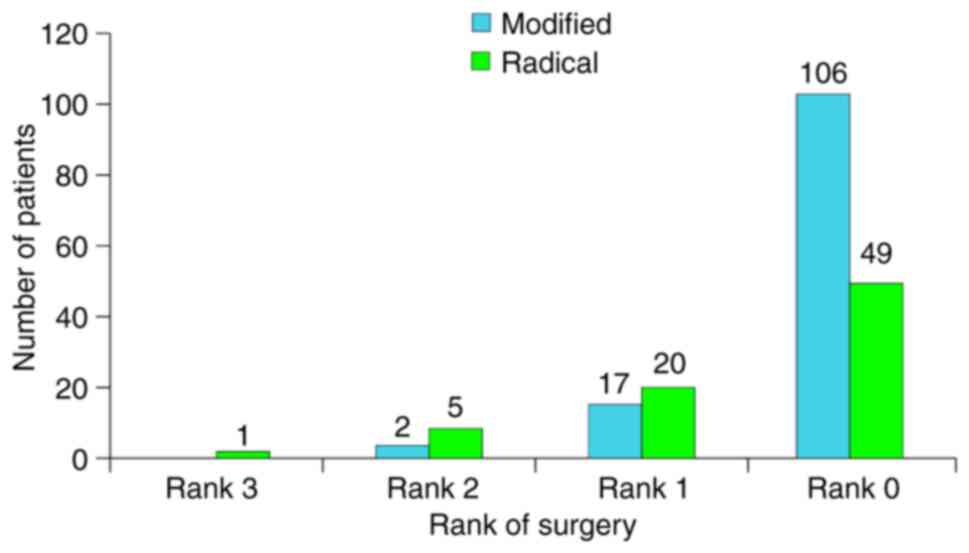
Distribution of patients according to the type and
rank of surgery is presented in Fig.
10. The rank of surgery became significant when it was
considered that the main study comparison criteria was time.
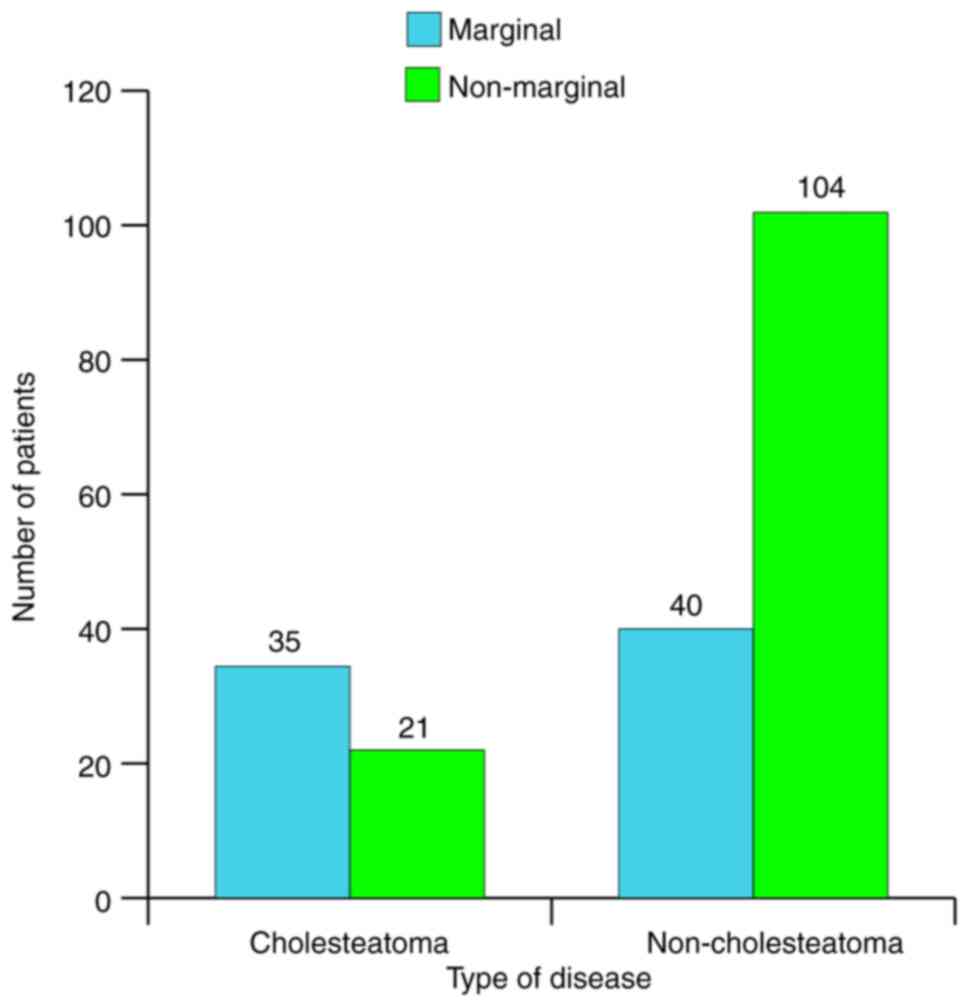
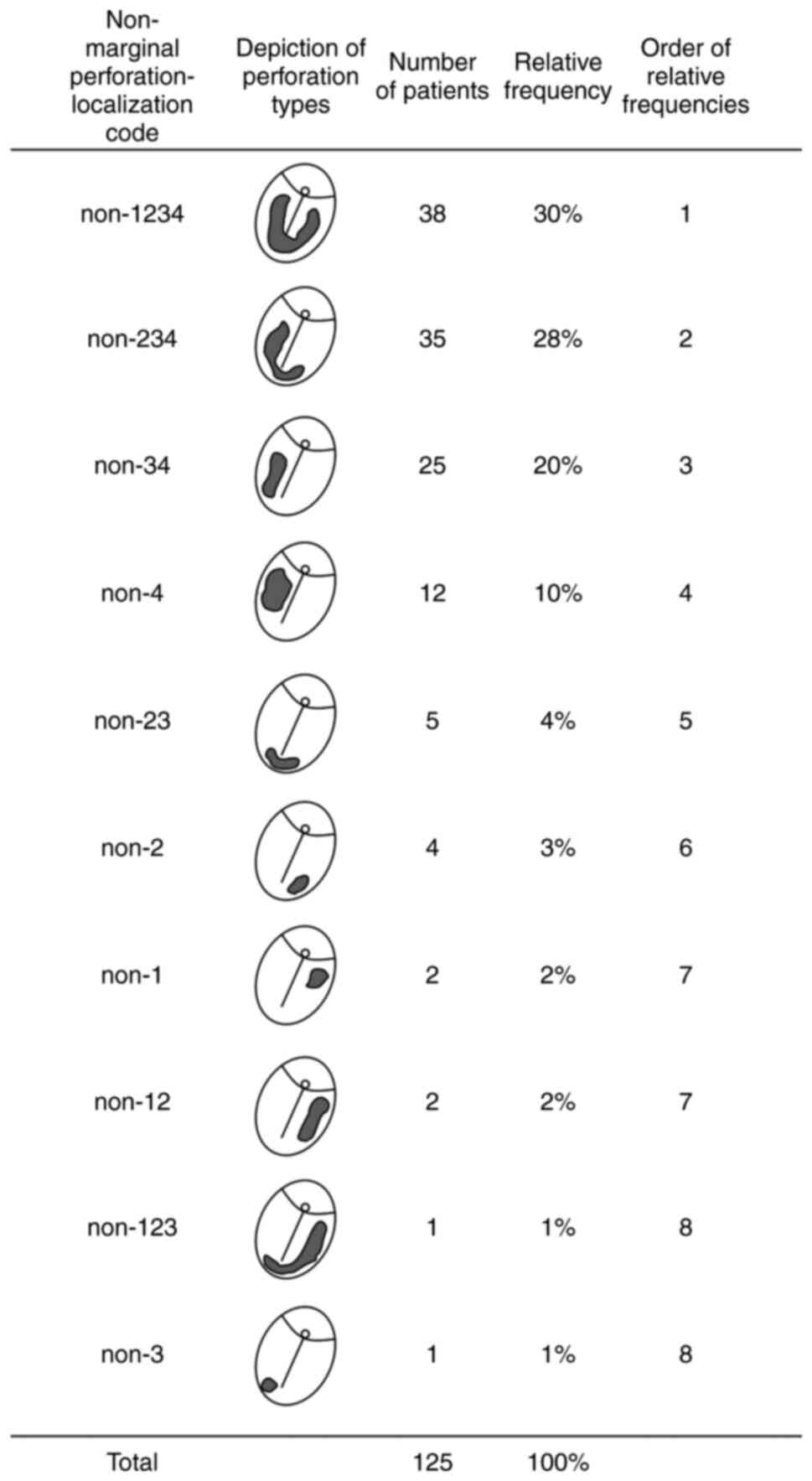
Fig. 11 presents
the distribution of patients according to type of disease and type
of tympanic membrane (TM) perforation. The relative frequency of
marginal perforation was 37.5% and that of cholesteatoma 28%.
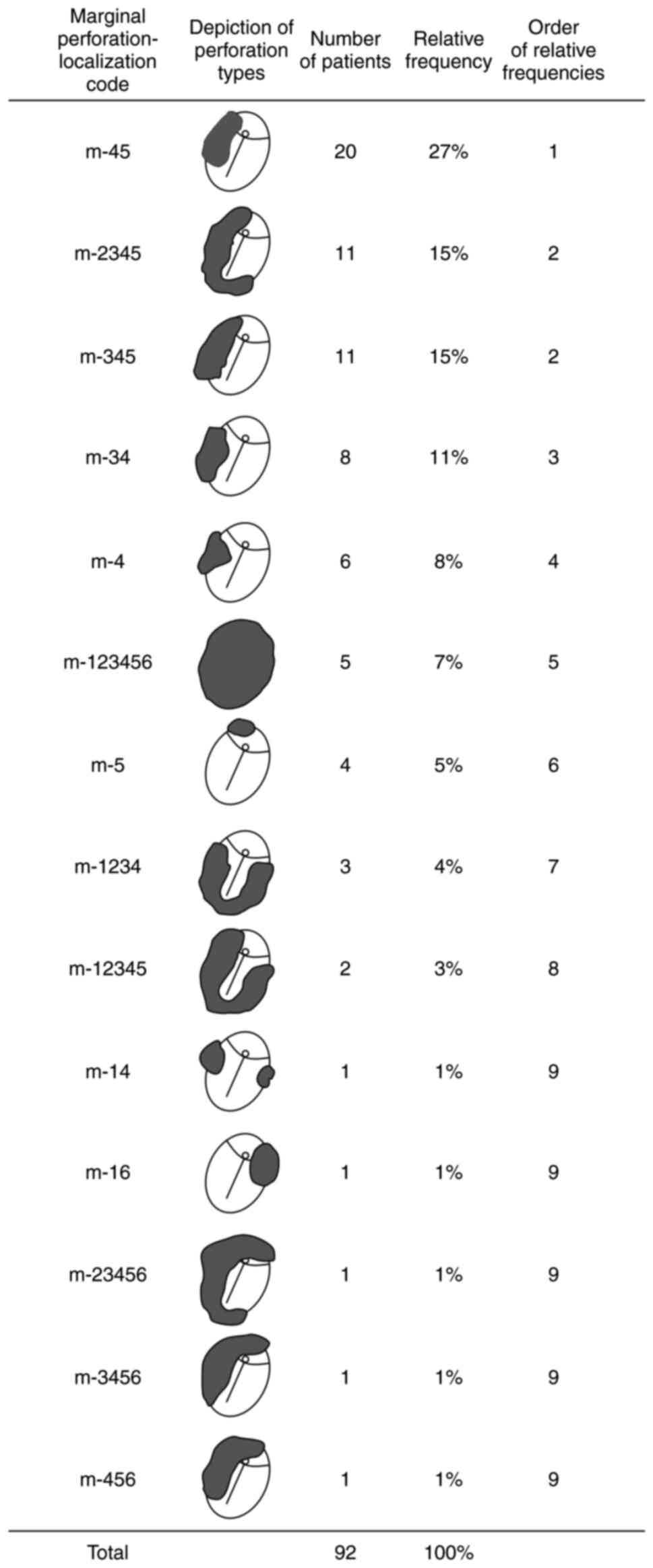
Fig. 12 shows the frequency
distribution of marginal perforations with the highest frequency
for posterosuperior quadrant and posterior part of Shrapnell's
membrane and the lowest for anterosuperior localization. Fig. 13 addresses non-marginal
perforations with the highest frequency for subtotal perforations.
The specific weights of posterior localization for both types of
perforations were as follows: 76% for marginal and 88% for
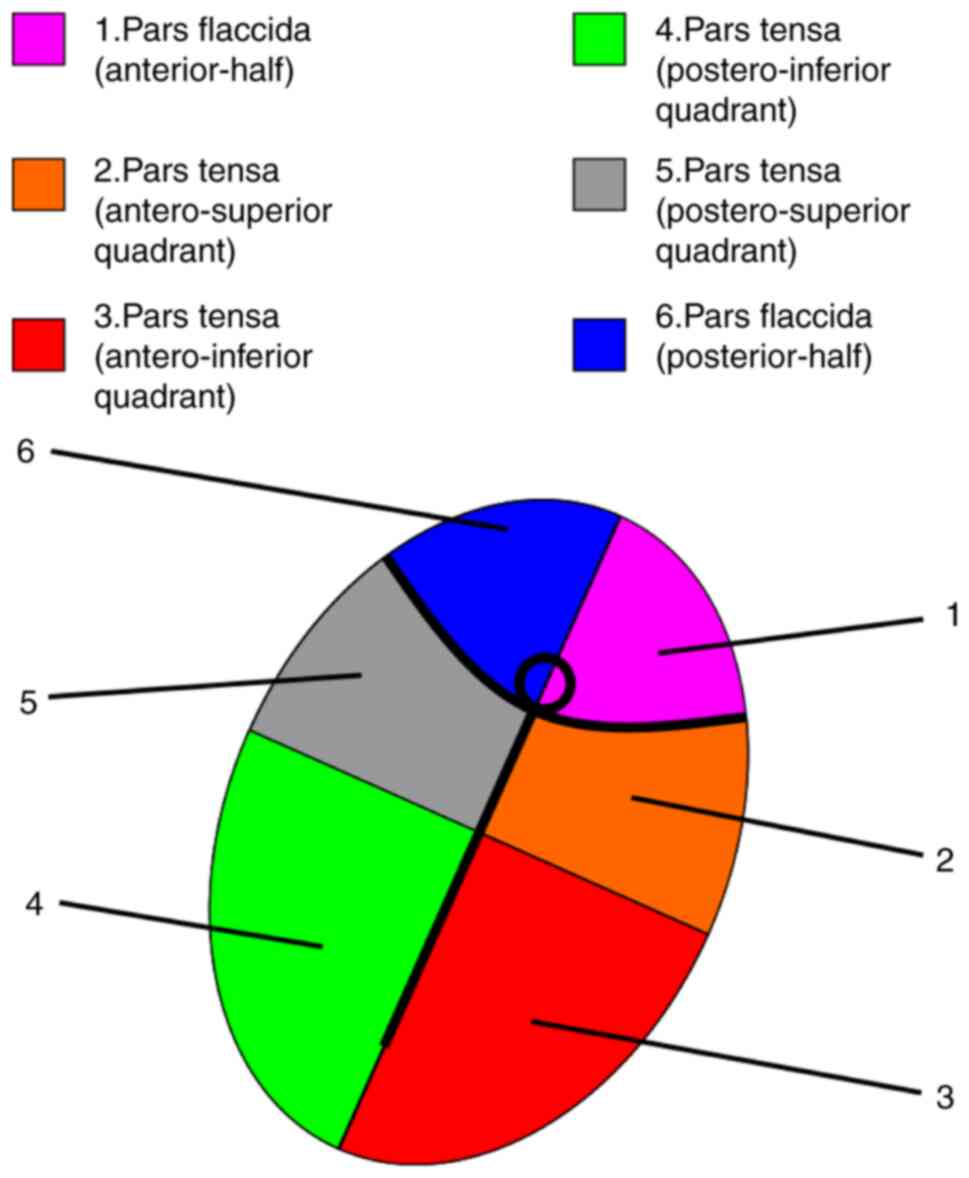
non-marginal. Fig. 14 represents
an explanation for the localization codes from Figs. 12 and 13. The letter ‘m’ stands for marginal
perforation, whilst ‘non’ stands for non-marginal. The numbers
refer to the area covered by the perforation and define the
specific quadrants of the pars tensa of the TM as well as the
halves of the pars flaccida (Shrapnell's membrane). As depicted,
some large perforations cover several neighbouring areas.
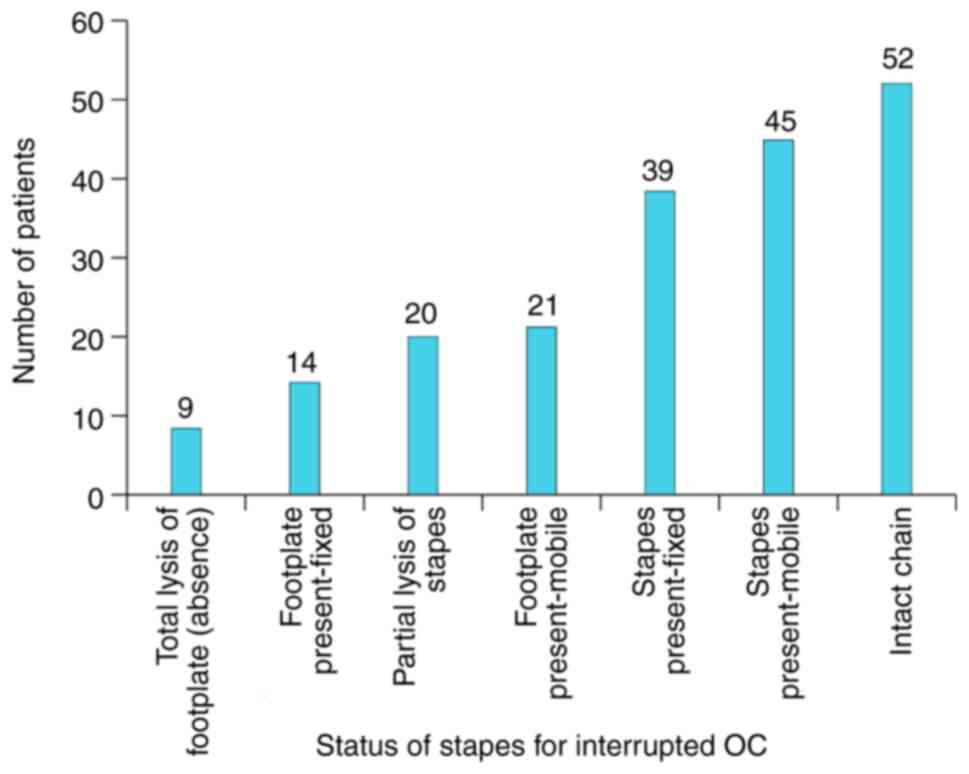
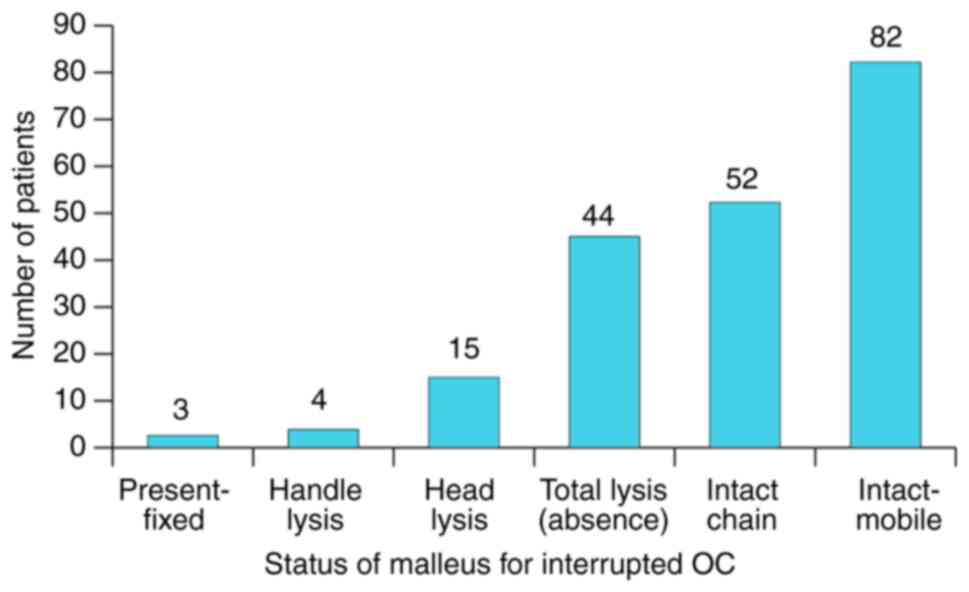
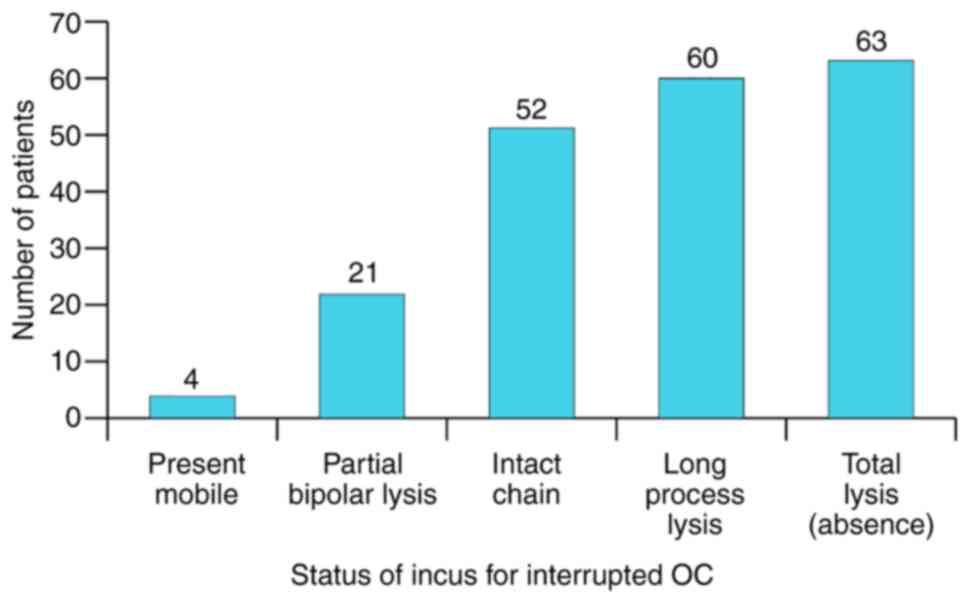
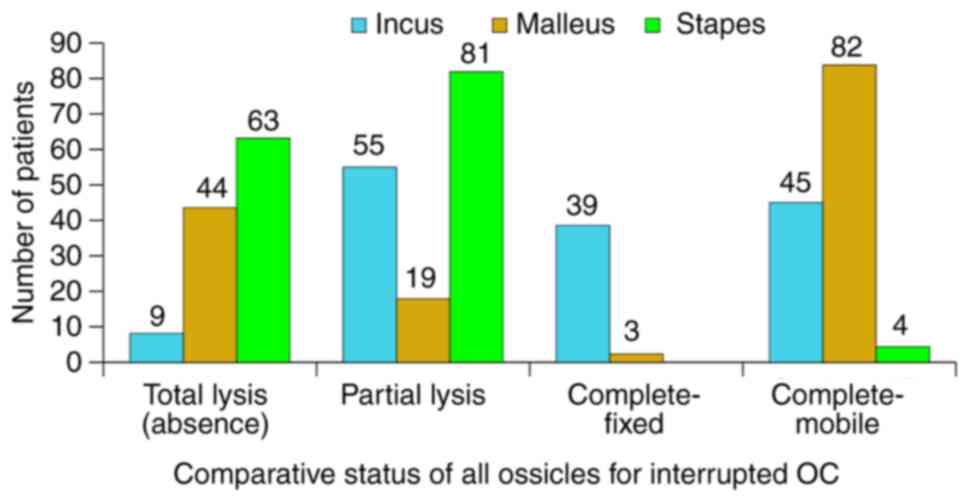
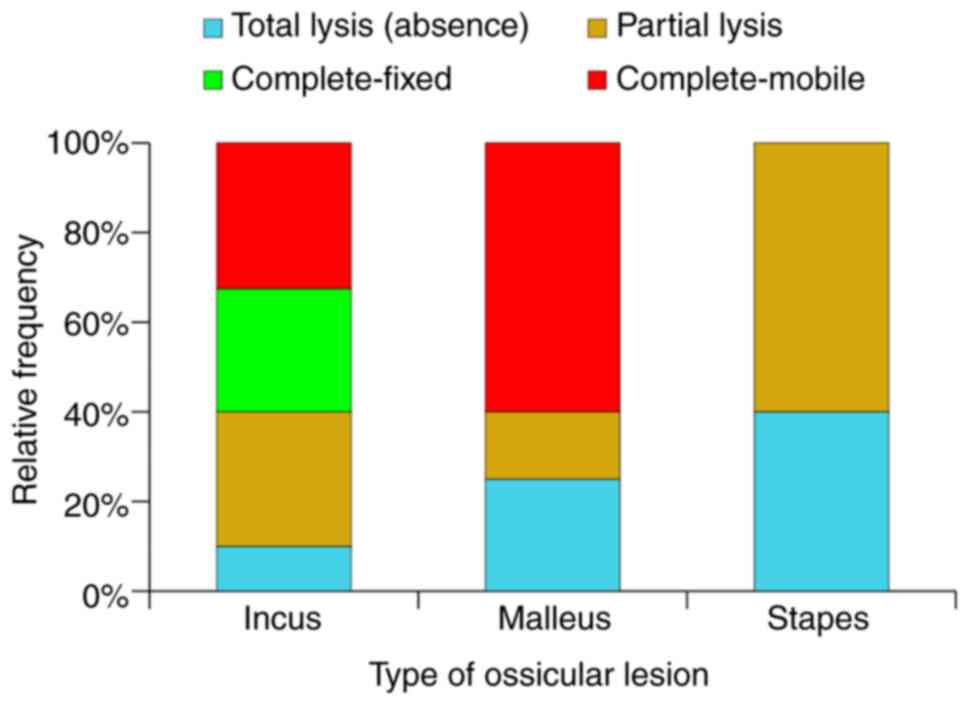
The state of the OC, as documented intra-op is
presented in Fig. 15. The specific
behaviour for each component of the OC in rapport to the
inflammatory status of the adjacent area was noted. Thus, the
stapes reacts by partial lysis and fixation to the oval window, the
malleus by total lysis, whilst the incus by osteolysis. The most
resistant towards total osteolysis was the stapes, followed by the
malleus. The incus was the most susceptible to this process. This
type of differentiated behaviour means that the total absence of
the OC (including stapes footplate) is relatively rare (7%),
fixation of a complete OC in almost double the cases (13%),
preserved complete and mobile OC in 14% and interrupted OC with the
highest frequency of 68%. This last situation represents the
characteristic response of the OC to chronic inflammatory disease
of the middle-ear (Fig. 16,
Fig. 17, Fig. 18, Fig.
19 and Fig. 20).
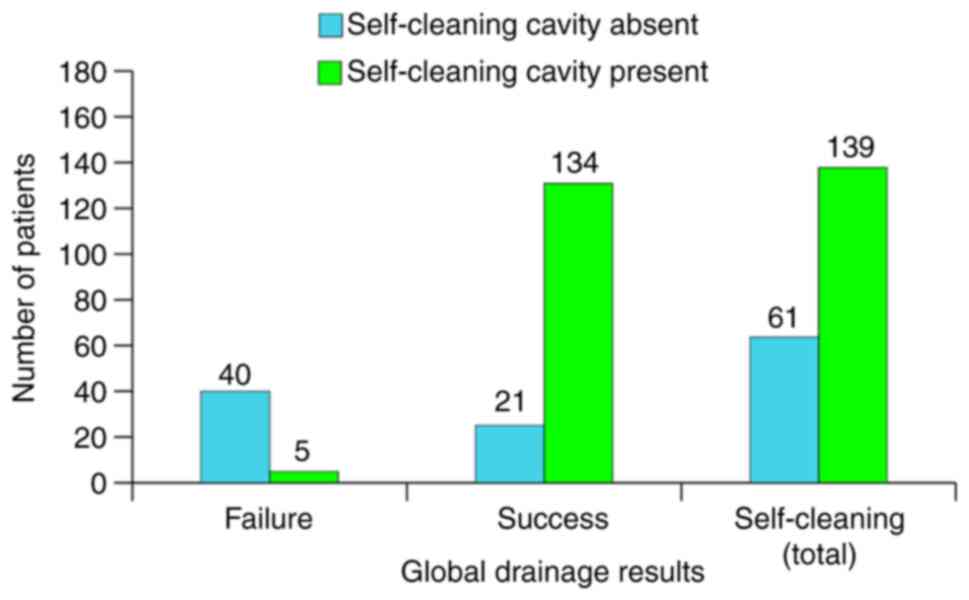
As far as success goes, the objective of the surgery
is to drain the inflammatory process and to create a new
self-cleaning external ear, a cavity with uniform walls that does
not allow cerumen deposits to form. Fig. 21 shows the global drainage results
of mastoidectomy in absolute frequencies with a success rate of
77.5%. Since completely self-cleaning ears are rather rare even in
healthy individuals, this objective was considered to be optional.
It would however instore quality of life (QoL) in the sense that
the patient could become independent from periodic visits to
clinical settings for cerumen removal. If the functional status of
the ear is also satisfactory it would bring total independence for
the patient, which is the purpose of surgery. Paradoxically,
self-cleaning was present in 11% of mastoidectomy failures
(Fig. 22) where it would be
expected to be completely absent. In the successful cases, there
was an 86% self-cleaning rate, which was lower than expected.
Overall, the global rate was 70%, which is probably the limit of
our future expectations on the subject. It can therefore be stated
that self-cleansing of a cavity is an intrinsic property of the
cavity and is governed by unclear internal laws, such as normal
keratosis and type of desquamation.
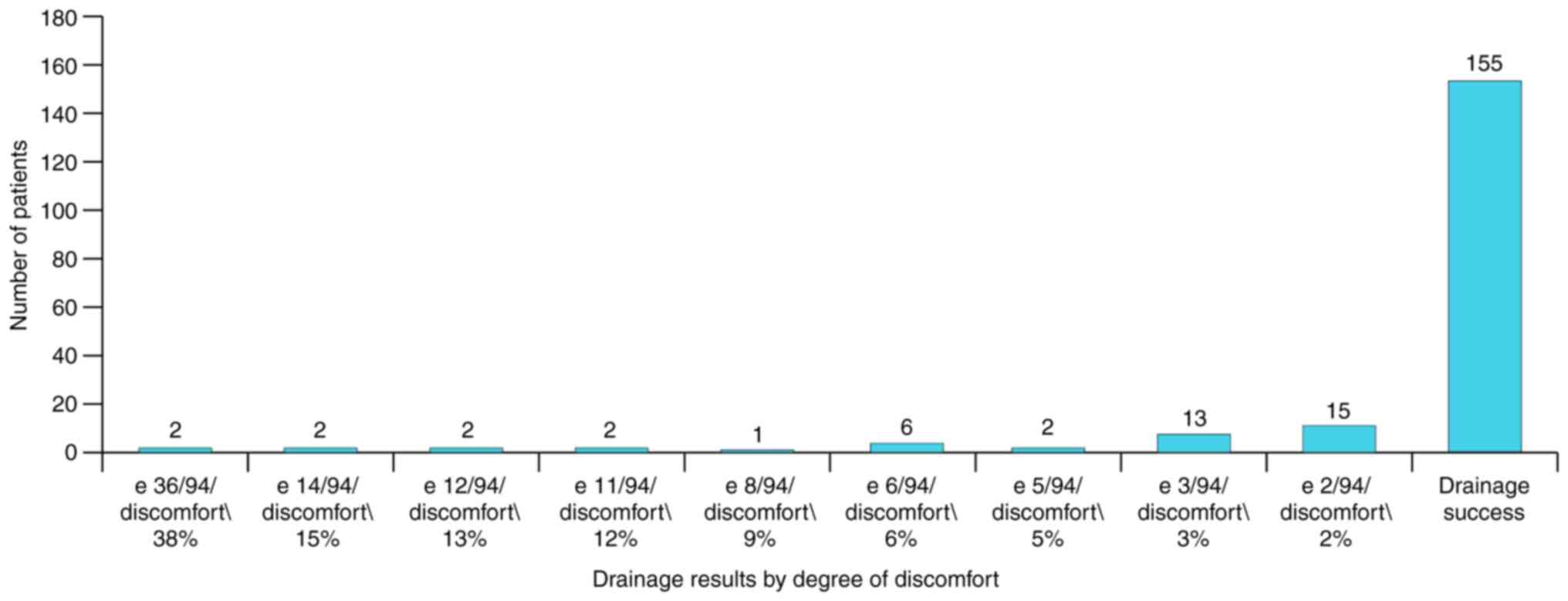
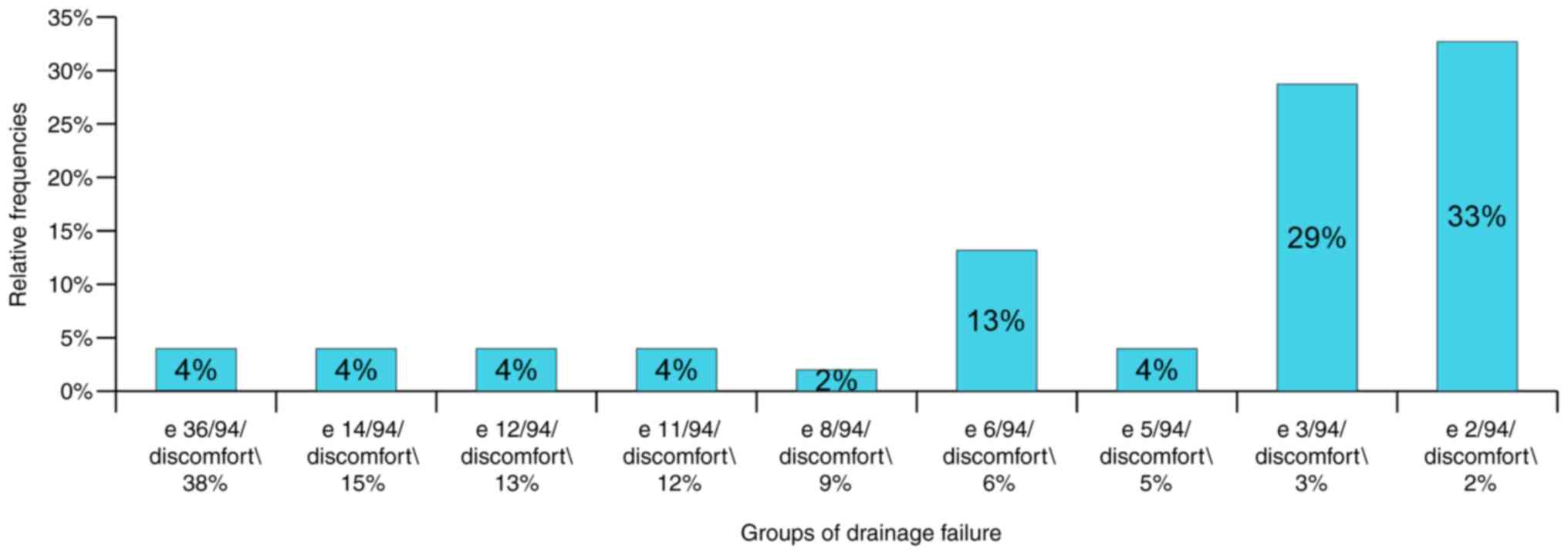
Failure of drainage requires further discussion
since it was defined by the appearance of one otorrhea episode in
7.86 years (one every 94 months), but the appearance of 36 episodes
(one every 3 months) also represented failure. In principle, both
situations are failures, but the specific situation is different
for each case, especially from the patient's point of view. This
meant that we had to find a way to differentiate failure and for
this purpose an arbitrary scale was created to quantify
comfort/discomfort of patient related to the number of otorrhea
episodes. Maximum discomfort (100% drainage failure) was considered
as monthly otorrhea episodes for the entire 7.86 years (94 months =
94 episodes). This meant that the most notable failure, 36 episodes
in 7.86 years (one episode every 3 months) corresponded to a 38%
discomfort rate and the smallest failure of two episodes in 7.86
years (one every 48 months) to a 2% discomfort rate. Fig. 23 shows the success of drainage
corresponding to each comfort/discomfort group in absolute
frequencies. Out of 45 patients with drainage failure two had the
highest discomfort score of 38% and most of them (n=15) had the
lowest score of 2%. Fig. 24
presents the same scores for failure patients; it was found that
81% of them had a discomfort score of up to 10%.
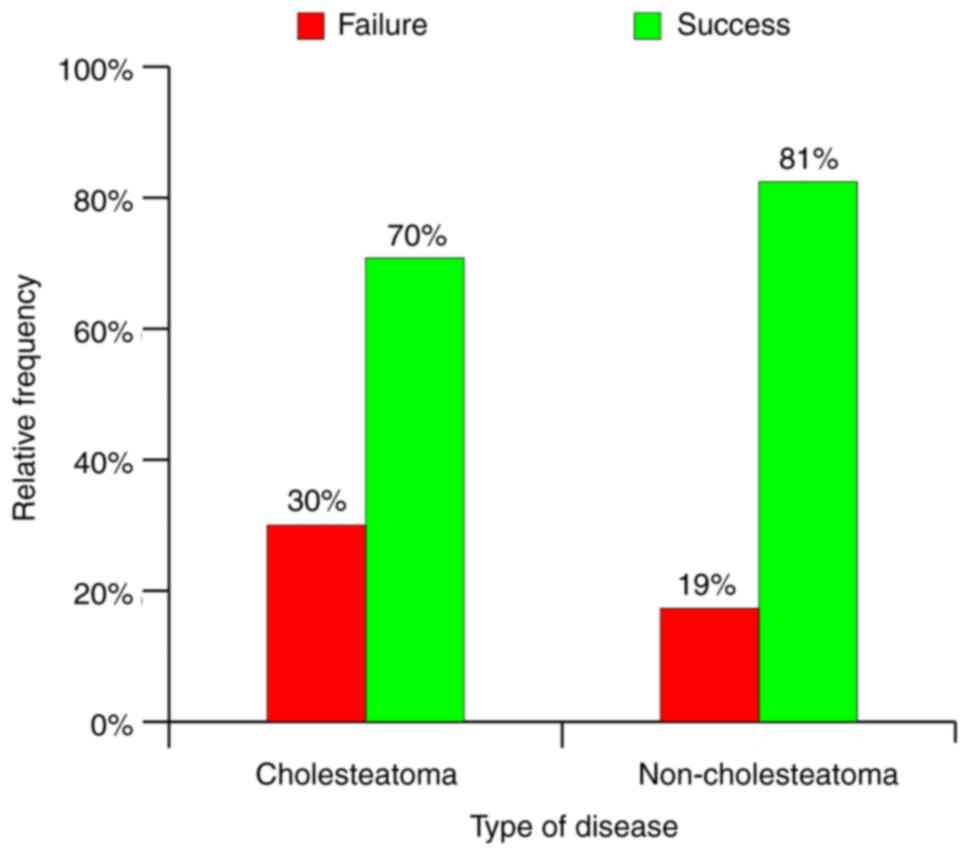
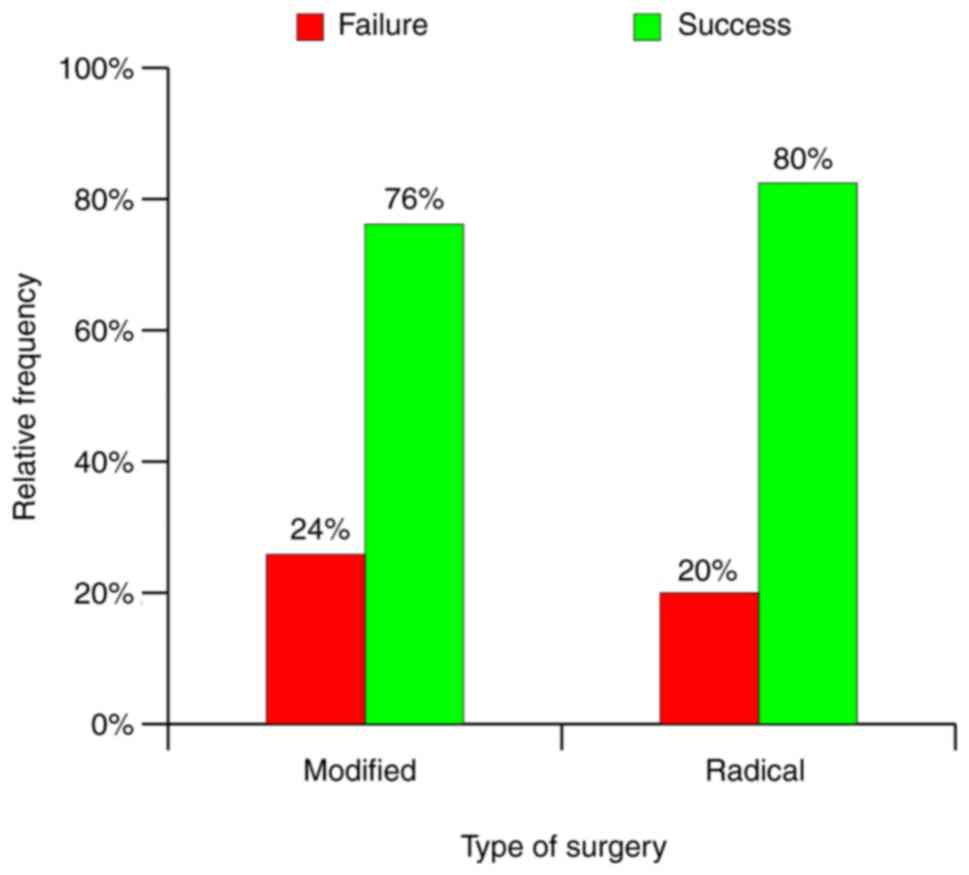
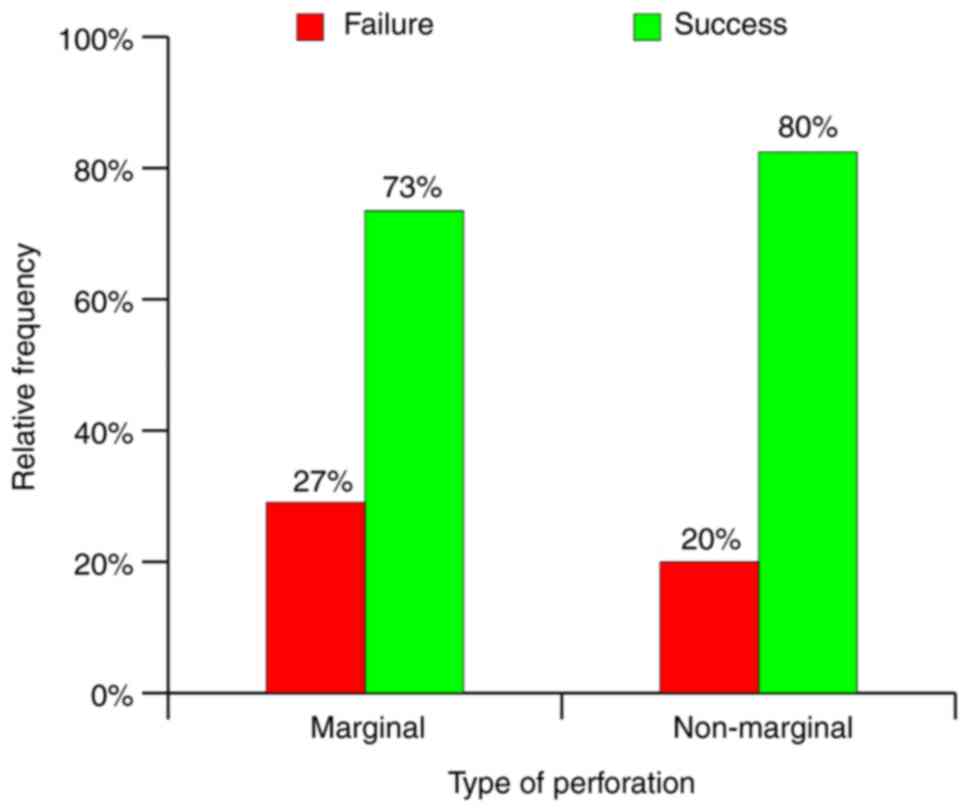
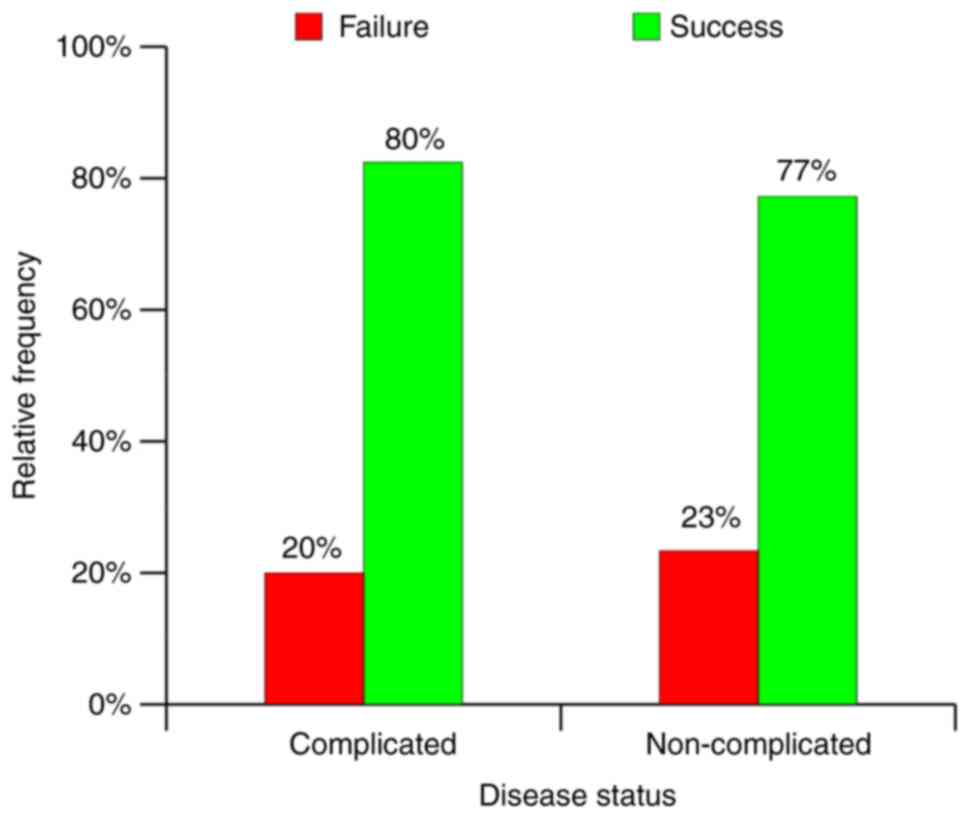
Although in our previous articles concerning
functional results of mastoidectomy for the same cohort of patients
(11,12), we encountered several factors that
influenced results, in the present study only three seemed to have
the expected influence on drainage results, including type of
disease, type of perforation and type of surgery. Presence of
cholesteatoma increased the rate of drainage success by 11%,
marginal perforation by 7% and MRM by 4% (Fig. 25, Fig.
26 and Fig. 27). By comparing
the global rates of success and/or failure to variables proven to
modify as expected the said rates, an influence of maximum 8% of
cholesteatoma presence was defined. Statistically the value was
significant, but a definitive conclusion cannot be stated in the
present study. Some of the variables, such as presence of
complications, clinical stage and total lesion score, yielded
paradoxical results and did not allow us to draw an applicable
conclusion concerning the involvement of these factors in the
evolution of long-term drainage results (Fig. 28, Fig.
29 and Fig. 30).
The most useful conclusion came from the
distribution of middle-ear mucosa lesions (Fig. 9). If the series of data are
concatenated from the chart, we obtain 10% for lesions localized
anterior and 90% posterior to a frontal conventionally drawn
geometric plan running through the middle of the tympanic cavity,
dividing the axial and coaxial spaces of the ME (by ME we
understand the sum of protympanum and the cells around it, tympanic
cavity with corresponding cells, aditus and antrum with peri-adital
cells, mastoid antrum with peri-antral cells) into two
segments-anterior and posterior to the defined geometric plan. The
concatenation involved calculating the mean value and adjusting it
to 100% of the newly obtained structure. By comparing these
empirical series to the theoretic series of endo-temporal cavity
distribution with variable geometry of the ME similar structures
were obtained: i) Peri-protympanum, 7%; ii) peri-tympanic cavity,
18%; iii) peri-aditus, 10%; and iv) peri-antrum, 65%.
Considering this series, in accordance with the
geometrical plane defined above, the following distribution was
obtained: i) Peri-protympanum, 7%; ii) peri-tympanic
cavity-anterior of plane, 9%; conventional frontal plane; iii)
peri-tympanic cavity-posterior of plane, 9%; iv) peri-aditus, 10%;
and v) peri-antrum, 65%.
This in turn led to the new theoretical series: i)
Protympanum 7%; ii) peri-tympanic cavity-anterior of plane, 9=16%;
conventional frontal plane; iii) peri-tympanic cavity-posterior of
plane 9% + peri-aditus 10% + peri-antrum 65 = 84%.
The empirical series in turn (Fig. 9) became: peri-protympanum +
peri-tympanic cavity = 10%; conventional frontal plane;
peri-tympanic cavity-posterior of plane + peri-aditus + peri-antrum
= 90%.
The two series (theoretical and experimental)
obviously had similar structures. They were compared with the
drainage results of 78% success and 22% failure. To do so it was
stated that, theoretically, radical mastoidectomy completely
cleaned the peri-antrum cells (65% of total), almost all of the
peri-aditus cells (10% of total), less than half of the
peri-tympanic cavity cells (18%) and none of the peri-protympanum
cells (7%). Practically the surgery cleaned much less than the
theoretically predicted ratio: Peri-antrum=0.65x (x→1), peri-aditus
= 0.1y (y→1), peri-tympanic cavity = 0.18z (z→0.5) and
peri-protympanum = 0.07w (w→0). The maximum obtainable value for
the sum 0.65x + 0.1y + 0.18z + 0.07w was 84%. This meant that
practically and ideally, a maximum of 84% could be cleaned out of
the mastoid and petrous cells. The remaining 16% may contain
irreversible lesions. The results of almost 78% were congruent to
this theory.
From a practical point of view, no surgeon should
expect to drain the entire endo-temporal structure since this type
of exercise is rarely realized in experiments or dissections. This
means that we must admit that some of the pneumatic cavities cannot
be surgically approached, dividing the mastoid bone into surgical
cavities and non-surgical cavities. The rate of success of
mastoidectomy is entirely dependent on the chance that all lesions
will be in a surgical area and this chance is a function of the
proportion of pneumatic cells for each of the mentioned areas.
Simplifying the process, it was stated in the present study that
the proportion of surgical cavities was 75% (antrum, aditus and
adjacent cells) and non-surgical cavities was 25% (tympanic cavity,
protympanum and adjacent cells). Failure should, in turn, be
discussed as medical research can occasionally require a high
degree of abstraction (13) and
failure itself is not an unequivocal clinical fact and it requires
divisions and nuances as we have previously stated (Figs. 23 and 24). The cause of failure is obvious
whilst the cause of its division is the normal law of probability
distribution that guides the division of remnant lesions in the
non-surgical cells. In other words, the more remnant lesions in
non-surgical cells, the higher the failure rate and intensity
(higher number of otorrhea episodes, lower patient comfort).
In comparison, Mukherjee et al (2) proposed a study on 133 patients with
MRM and published long-term functional and anatomical results.
Their criteria included the notion of waterproof ears (no otorrhea
after exposure to water) and the study reported 95% (n=126) as such
(2). The anatomical status of the
stapes and the degree of ventilation within the middle-ear are also
considered proof of a successful operation, in accordance with the
conclusions of the present study and those of other authors
(5,14). Comparing results of different
studies is however complicated by case-mix variation as some
centres may have a larger number of complicated cases with higher
probability for poor post-operative results (2). These concerns can be addressed by
using scores such as the SPITE score described by Black (15) (points for various factors, such as
presence of infection and previous surgery) or our own previously
presented complication score (7)
(Tables I and II).
A smaller study by Lucidi et al (16) published the results of 31 patients
with both CWU and CWD mastoidectomies and followed the QoL over an
average of 12 months post-op. They concluded that after 12 months,
epithelization is complete, and the patient can provide reliable
self-assessment concerning QoL. However, the authors noted that
such a short follow-up may not be sufficient to consider these
results as conclusive. The recurrence rate for CWU was 20-30% and
5-9% for CWD, in accordance with the conclusions of the present
study and those of other published studies (16,17).
A more extensive study by Kos et al (1) analysed 259 cases for both functional
and anatomical results for a period of 1 to 24 years (mean period
of 7 years, very similar to the present study). Recurring
infections of the cavity were reported in 11.9% (n=31) of cases
within 6 years post-op and in 6.5% (n=17) of cases >6 years
post-op. Overall, a dry and self-cleaning cavity was obtained in
95% of cases. Complications included polyps, recurrent
cholesteatoma, TM perforation and meatal stenosis (1). These results were considered congruent
with those reported by a significant number of other researchers
(18-21).
In comparison, a study by Kuo et al (22) reported a total of 4.9% ear discharge
with residual cholesteatoma mainly affecting the attic and
retrotympanum, which was similar to other previously published
studies (22-24).
Nadol (25) defined the sigmoid
sinus and tegmen air cells as the most common recurrence site,
while Veldman and Braunius (20)
considered the facial nerve and sigmoid sinus as most frequent
(20). A previous study by Prasanna
Kumar et al (26) defined
the mastoid cells as the most common recurrence site, followed by
sinodural angle, sinus tympani and tegmen antri region.
A similar study was performed by Pareschi et
al (27) reported long-term
anatomical and functional results (10 years follow-up) for a total
of 895 patients with a total recidivism rate of 7.7% (n=69), of
which 6.7% (n=60) showed persistence of disease and 1% (n=9) showed
recurrence. Of the 60 cases, the largest rate of persistence was in
the posterior mesotympanum (n=52), followed by the anterior
mesotympanum (n=5) and hypotympanum (n=3), which validates our
previously stated conclusions on lesion distribution (7). Pareschi et al (27) and Vartiainen (28) also stated that prognostic factors
for recidivism include the status of the TM and middle-ear mucosa,
age of the patient and length of follow-up, since cholesteatoma
recurrence can develop even after 12 years, thus confirming the
conclusions of the present study.
Blanco et al (29) also reported on 45 cases of CWD
surgery with a success rate of 93.3 and 6.6% recurrence, which was
less than other similar studies such as Lin and Oghala (30). The main limitation of the previous
study by Blaco et al was the short follow-up period of only
28 months (29).
To conclude, successful mastoidectomy was defined in
the current study as the total absence of otorrhea episodes after
total epithelization of cavity and failure of the presence of at
least one such episode. A successful drainage (anatomical results)
ensured long-term stability of hearing (functional results). The
two types of results of mastoidectomy were expressions of the same
phenomenon defined as a conversion of a static population by binary
division in respect to the spatial distribution of its constituting
units. Drainage results were found to be linked by an analytical
function to factors with clinical predictive significance, such as
complications of disease, exteriorization of suppurative disease,
lesions of the ME mucosa and TM, rank of surgery, status of the OC,
age of patient and length of follow-up. The global drainage success
rate was 77.5%, and the best self-cleaning rate was 86% with a
global self-cleaning rate of 70%. From a practical point of view,
no surgeon should expect to drain the entire endo-temporal
structure since this type of exercise is rarely realized in
experiments or dissections. This means that we must admit that some
of the pneumatic cavities cannot be surgically approached, dividing
the mastoid bone into surgical cavities and non-surgical cavities.
Practically and ideally, we can clean out a maximum of 84% of the
mastoid and petrous cells. Our results of almost 78% are congruent
to this theory. The remaining 16% may contain irreversible lesions.
The rate of success of mastoidectomy is entirely dependent on the
chance that all lesions be in a surgical area and this chance is a
function of the proportion of pneumatic cells for each of the
mentioned areas. Most of the non-surgical cavities are located in
the tympanic cavity, protympanum and adjacent cells. The more
remnant lesions in non-surgical cells, the higher the failure rate
and intensity (higher number of otorrhea episodes, lower patient
comfort).
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
HM and MR contributed equally to this work and
should, therefore, both be considered first authors of this
article. HM and MR were responsible for the original idea,
conception, patient selection and care, operations, data collection
and editing structure. AIM, GC AB and MAS made substantial
contributions to acquisition, analysis and interpretation of data
and gave a final view of the article. MAS was also responsible for
the data analysis and graphical representation of the results. All
authors have read and approved the final manuscript. HM and MR
confirm the authenticity of all the raw data.
Ethics approval and consent to
participate
For this study, ethical approval was obtained from
the Research Ethics Committee of the Faculty of Medicine, Titu
Maiorescu University (approval no. 1/25.05.2021; Bucharest,
Romania). All patients provided informed written consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kos MI, Castrillon R, Montandon P and
Guyot JP: Anatomic and functional long-term results of canal
wall-down mastoidectomy. Ann Otol Rhinol Laryngol. 113:872–826.
2004.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Mukherjee P, Sauders N, Liu R and Fagan P:
Long-term outcome of modified radical mastoidectomy. J Laryngol
Otol. 118:612–616. 2004.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lv J, Li H, Wu X, Chen X and Huang Y:
Functional results of revision canal wall down mastoidectomy. J
Bio-X Res. 2:98–103. 2019.
|
|
4
|
Nyrop M and Bonding P: Extensive
cholesteatoma: Long-term results of three surgical techniques. J
Laryngol Otol. 111:521–526. 1997.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Cook J, Krishnan S and Fagan PA: Hearing
results following modified radical versus canal-up mastoidectomy.
Ann Otol Rhinol Laryngol. 105:379–383. 1996.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mocanu H, Mocanu AI, Drăgoi AM and
Rădulescu M: Long-term histological results of ossicular chain
reconstruction using bioceramic implants. Exp Ther Med.
21(260)2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Mocanu H, Mocanu AI, Bonciu A, Coadă G,
Schipor MA and Rădulescu M: Analysis of long-term functional
results of radical mastoidectomy. Exp Ther Med.
22(1216)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Neudert M, Bornitz M, Mocanu H,
Lasurashvili N, Beleites T, Offergeld C and Zahnert T: Feasibility
study of a mechanical real-time feedback system for optimizing the
sound transfer in the reconstructed middle ear. Otol Neurotol.
39:e907–e920. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mocanu H, Bornitz M, Lasurashvili N and
Zahnert T: Evaluation of Vibrant® Soundbridge™
positioning and results with laser Doppler vibrometry and the
finite element model. Exp Ther Med. 21(262)2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Neagu A, Mocanu AI, Bonciu A, Coadă G and
Mocanu H: Prevalence of GJB2 gene mutations correlated to presence
of clinical and environmental risk factors in the etiology of
congenital sensorineural hearing loss of the Romanian population.
Exp Ther Med. 21(612)2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Fagan PA: Modified radical mastoid surgery
for chronic ear disease. Ann Acad Med Singap. 20:665–673.
1991.PubMed/NCBI
|
|
12
|
Perez de Tagle JR, Fenton JE and Fagan PA:
Mastoid surgery in the only hearing ear. Laryngoscope. 106:67–70.
1996.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Alecu I, Mocanu H and Călin IE:
Intellectual mobility in higher education system. Rom J Mil Med.
120:16–21. 2017.
|
|
14
|
Fisch U and Schmid S: Radical
mastoido-epitympanectomy with tympanoplasty and partial
obliteration: A new surgical procedure? Ann Acad Med Singap.
20:614–617. 1991.PubMed/NCBI
|
|
15
|
Black B: Prevention of recurrent
cholesteatoma: Use of hydroxyapatite plates and composite grafts.
Am J Otol. 13:273–278. 1992.PubMed/NCBI
|
|
16
|
Lucidi D, de Corso E, Paludetti G and
Sergi B: Quality of life and functional results in canal wall down
vs canal wall up mastoidectomy. Acta Otorhinolaryngol Ital.
39:53–60. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kerckhoffs KG, Kommer MB, van Strien TH,
Visscher SJ, Bruijnzeel H, Smit A and Grolman W: The disease
recurrence rate after the canal wall up or canal wall down
technique in adults. Laryngoscope. 126:980–987. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Austin OF: Staging in cholesteatoma
surgery. J Laryngol Otol. 103:143–148. 1989.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Parisier SC, Hanson MB, Han JC, Cohen AJ
and Selkin BA: Pediatric cholesteatoma: An individualized,
single-stage approach. Otolaryngol Head Neck Surg. 115:107–114.
1996.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Veldman JE and Braunius WW: Revision
surgery for chronic otitis media: A learning experience. Report on
389 cases with a long-term follow-up. Ann Otol Rhinol Laryngol.
107:486–491. 1998.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Lau T and Tos M: Treatment of sinus
cholesteatoma. Long-term results and recurrence rate. Arch
Otolaryngol Head Neck Surg. 114:1428–1434. 1988.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Kuo CY, Huang BR, Chen HC, Shih CP, Chang
WK, Tsai YL, Lin YY, Tsai WC and Wang CH: Surgical results of
retrograde mastoidectomy with primary reconstruction of the ear
canal and mastoid cavity. Biomed Res Int.
2015(517035)2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Gaillardin L, Lescanne E, Moriniere S,
Cottier JP and Robier A: Residual cholesteatoma: Prevalence and
location. Follow-up strategy in adults. Eur Ann Otorhinolaryngol
Head Neck Dis. 129:136–140. 2012.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Haginomori AI, Takamaki A, Nonaka R and
Takenaka H: Residual cholesteatoma: Incidence and localization in
canal wall down tympanoplasty with soft-wall reconstruction. Arch
Otolaryngol Head Neck Surg. 134:652–657. 2008.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Nadol JB Jr: Causes of failure of
mastoidectomy for chronic otitis media. Laryngoscope. 95:410–413.
1985.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Prasanna Kumar S, Ravikumar A and Somu L:
Modified radical mastoidectomy: A relook at the surgical pitfalls.
Indian J Otolaryngol Head Neck Surg. 65 (Suppl 3):S548–S552.
2013.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Pareschi R, Lepera D and Nucci R: Canal
wall down approach for Tympano-mastoid cholesteatoma: Long-term
results and prognostic factors. Acta Otorhinolaryngol Ital.
39:122–129. 2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Vartiainen E: Ten-year results of canal
wall down mastoidectomy for acquired cholesteatoma. Auris Nasus
Larynx. 27:227–229. 2000.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Blanco P, González F, Holguín J and Guerra
C: Surgical management of middle ear cholesteatoma and
reconstruction at the same time. Colomb Med (Cali). 45:127–131.
2014.PubMed/NCBI
|
|
30
|
Lin JW and Oghalai JS: Can radiologic
imaging replace second-look procedures for cholesteatoma.
Laryngoscope. 121:4–5. 2011.PubMed/NCBI View Article : Google Scholar
|