Introduction
Transient acantholytic dermatosis (TAD), also known
as Grover's disease, was named after an individual who thoroughly
characterized the disease in 1970(1). TAD is characterized by papulovesicular
eruptions on the trunk, which are typically focal acantholysis and
dyskeratosis on histological examination. Characteristic skin
lesions are erythematous to red-brown keratotic papules that are
localized on the anterior part of the chest, upper part of the back
and lower part of the rib cage with widespread scatter and no
tendency to coalesce, whereas the scalp, palms and soles are
usually not affected (2).
Acneiform, vesicular, pustular and rarely bullous lesions, as well
as unusual distributions, including unilateral or zosteriform
eruptions, have been reported as dermatological presentations of
TAD (3). Lesions may resolve with
postinflammatory pigmentation. No systemic symptoms are associated
with TAD, but oral lesions can develop as slightly painful aphthae.
Skin lesions are accompanied by pruritus, with variable degrees of
itching from mild to severe. Patients with severe pruritus
typically present with multiple, disseminated lesions affecting the
neck, shoulders, trunk, arms and legs (4,5).
The presentation of TAD can be subtle or may closely
resemble other pruritic dermatoses. TAD is a reactive skin
condition that is benign, self-limited and resolves over a period
of weeks or months, but there are also cases with long evolution
and a tendency to become persistent, which are difficult to manage
due to the recurrence of physical signs and persistent pruritus
(6). The exact etiology of TAD is
unknown.
Viral, bacterial and other pathogens have been
proposed as causative agents of TAD, but no causative role has been
established. Bullous impetigo, common impetigo, staphylococcal
scalded skin syndrome and herpes simplex virus
(HSV)/varicella-zoster virus (VZV) infection result in vesicles
that clinically present as bullae and acantholysis on
histopathological examination (7).
In these cases, for the confirmation of the diagnosis, the
clinicopathological correlations, epidemiological context and drug
intake are necessary. Herpetic infections, including human
herpesvirus (HHV)-1, HHV-2 and HHV-3 (also known as VZV), are
characterized by an intraepidermal blister, ballooning degeneration
of keratinocytes and multinucleate keratinocyte giant cells that
allow for easy diagnosis. Epithelial multinucleated giant cells are
usually associated with HSV infections, but they also can be
present in skin biopsy specimens of benign and malignant skin
tumors or in acantholytic dermatoses (8). In special cases, when a herpes simplex
infection is suspected, but the skin lesions do not have the
typical appearance (for example vesicular lesions at a distance or
disseminated vesicles) and when there is a lack of response to
antiviral therapy, laboratory tests are performed to rule out the
diagnosis of viral infection; the existence of an acantholytic
dermatosis must be considered and a skin biopsy must be performed
(8).
Heat, sweating and the obstruction of sweat ducts
have been suggested as potential causative factors for the disease;
however, it has also been reported that xerosis is a potential
cause of TAD, and that the disease is exacerbated by cold weather.
The disease seems to occur more frequently in patients with atopic
dermatitis and asteatotic dermatitis. We hypothesize that the
appearance of cutaneous lesions is closely related to
individual-specific neurovegetative reactions to cholinergic and
adrenergic stimuli, as sweat secretion is regulated by the central
nervous system and the autonomic nervous system. Both cholinergic
and adrenergic pathways seem to be involved in sweating.
Acetylcholine, a neurotransmitter released by sympathetic nerve,
acts as a potent stimulator for sweat secretion (9-11).
Dysfunction of the autonomic nervous system, in particular the
sympathetic nervous system, may cause sweating disorders, such as
hyperhidrosis or hypohidrosis (12). The role of sweat gland secretion is
to regulate the body temperature when it rises, which is controlled
by the sympathetic nervous system (12).
In this context of sweating disorders, drugs and
their adverse reactions should be considered. For example, b
blockers, which induce hyperhidrosis secondary to β-adrenoreceptor
blockade, are widely used in the treatment of common diseases, such
as hypertension and heart failure, that are often encountered in
elderly people (11).
Exposure of the normal epidermis to heat
(cholinergic stimulation), stress, intense physical exertion,
certain professional activities and emotional factors results in
increased sweat secretion. However, blocking the acrosyringial
ducts may also be a factor contributing to the disruption of sweat
secretion. Cold exposure of an intact xerotic epidermis with low
sweat secretion, based on atopic dermatitis and asteatotic
dermatitis, may be a causative agent of TAD (10,12).
In atopic skin, the altered composition of perspiration
(concentration of salt, water, lactic acid and urea) may serve a
role in the etiopathology of TAD, regardless of the influence of
environmental factors on the intensity of perspiration (10). Thyroid dysfunction and
neurovegetative abnormalities may also serve important roles in the
etiology of TAD.
TAD most commonly affects middle-aged white male
patients over the age of 40, but the disease has also been reported
in children. Epidemiological studies demonstrated that men are more
affected than women, with an incidence ratio of 3:1(1).
A number of studies have reported a direct
relationship between autoimmune antibodies and TAD, but whether the
autoimmune antibodies cause TAD or an increase in the number of
autoimmune antibodies is a result of TAD is not completely
understood (13,14). Therefore, further studies are
required to determine whether TAD is an immunological disorder.
The disease is associated with a number of other
skin diseases, including eczema, solar keratosis, psoriasis,
autoimmune disorders (such as bullous pemphigoid, vitiligo and
alopecia areata), immunological diseases and malignancies (13,15).
Future studies should assess the cellular and humoral immunity
disturbances in TAD, and also investigate its association with the
aforementioned skin diseases using a large patient population.
TAD has also been observed in oncology patients. TAD
was primarily observed in patients with hematologic malignancies,
including acute and chronic myelogenous leukemia and lymphoma,
solid tumors and carcinoma of the genitourinary organs (16,17).
In previous case reports, it has also been reported that the
occurrence of TAD coincided with the onset of malignancy in some
cases or with the recurrence of malignancy in three individuals
(12%). In the other 23 oncology patients, TAD was considered to be
secondary to specific antineoplastic therapy or excessive
perspiration, fever, occlusive immobility, or ionizing or UV
radiation (16-18).
Melanoma therapy with cytotoxic
T-lymphocyte-associated protein 4 inhibition has been also
associated with TAD (18). However,
there is not a sufficient number of related cases to consider the
disease as a paraneoplastic disorder.
The prevalence of TAD is not available primarily due
to the clinical and histopathological similarities with other types
of dermatitis, especially with the limited papulovesicular lesions
of the trunk. It has been proposed that the disease is under
diagnosed. Both the dermatologist and dermatopathologist must be
aware of entities that mimic classic acantholytic dermatoses and of
rare disease variants, which are characterized by acantholysis.
Positive diagnosis is obtained by clinical presentation and
histopathological examination, which typically reveals focal
acantholysis and dyskeratosis, and spongiosis is also commonly
observed. The presence of spongiosis, acantholysis and vesicle
formation in the same specimen should raise the possibility of TAD
(19).
Acantholysis, associated with dyskeratosis, may
mimic Darier disease, Hailey-Hailey disease or pemphigus, and
accurate histological examination is important for diagnosis
(6). Dermoscopic examination is
also limited, as no specific features for TAD have been reported
yet. Moreover, immunofluorescence has been proven negative in most
cases, as well as inconsistent, and has not yet been directly
correlated to the histology of the disease (20); however, this may become an area for
research into the etiology of TAD.
From a clinical and histological point of view, the
disease resembles numerous dermatoses, including Darier disease,
pemphigus foliaceus, Hailey-Hailey disease and dermatitis
herpetiformis. Therefore, an accurate diagnosis is difficult as
specific lesions occur more frequently in patients with atopic
dermatitis and asteatotic dermatitis. Positive diagnosis is based
on historical, clinical and histological examination, but is
difficult because the disease can mimic a lot of dermatoses,
especially when it is accompanied by pruritus (19,21).
Treatment success relies on the correct
identification of the disease, follow-up over time and multiple
checks to prevent recurrences, which appear frequently for
refractory cases. Current treatment strategies include topical
steroids, calcineurin inhibitors, vitamin D analogs, retinoids,
methotrexate and 5-aminolevulinic acid photodynamic therapy. In
addition, activities that cause excess heat and sweating should be
avoided. Potent topical corticosteroids are used for their
anti-inflammatory effect, as well for the control of itching. For
pruritus, menthol or pramoxine-containing lotions can also be used
(6). Liquid nitrogen therapy has
been reported as an effective strategy for patients with persistent
TAD, which involves the application of liquid nitrogen on papular
lesions for 15 sec beyond formation of the ice field, followed by a
second cycle after 3-5 min of complete thawing. At 3 months
post-liquid nitrogen therapy, no new lesions or pruritus were
observed, only a few residual hyperpigmentation macules were
identified and no recurrence within 1 year was reported (22). Vitamin A (50,000 U, 3 times/day for
2 weeks followed by a single daily dose for up to 12 weeks) and
isotretinoin (40 mg/day for 2-12 weeks) have been suggested as
effective treatment strategies for refractory cases (23). Oral corticosteroids, UV-B exposure,
psoralen plus ultraviolet A light, grenz radiation and methotrexate
have also been reported to be effective in treating severely
resistant cases. However, some cases are refractory to all forms of
therapy.
Case report
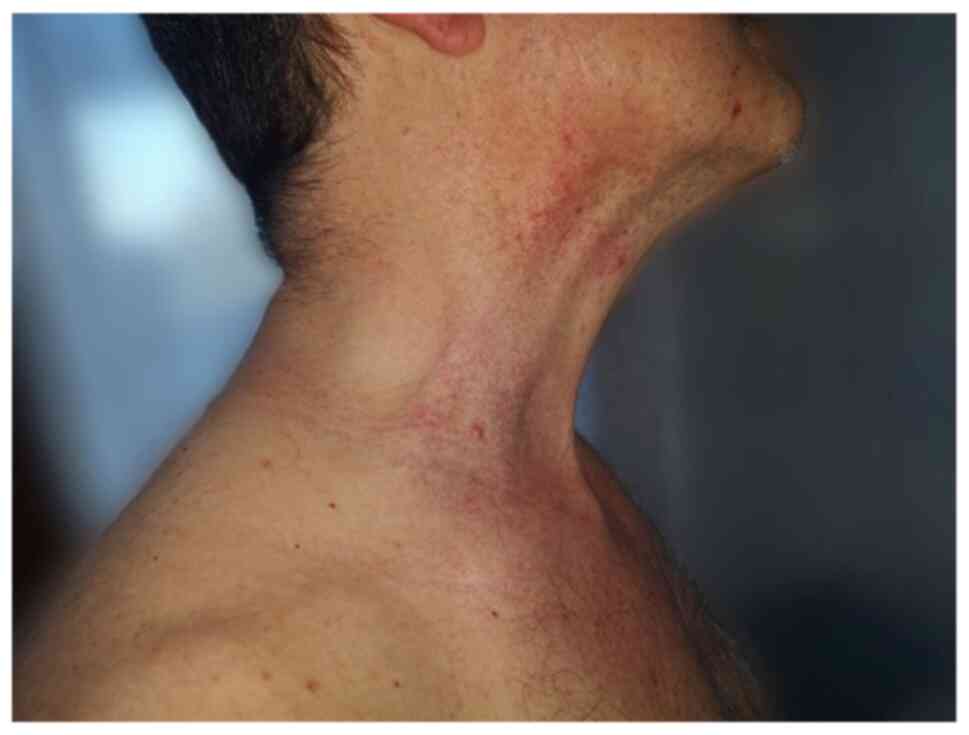
A 55 year-old Caucasian male presented in the
Dermatology Department (County Emergency Clinical Hospital Oradea,
Romania) in July 2018, for well-delimitated, axillary, bilateral
erythematous plaques and placards with geographical borders, as
well as vesicle-bullae in periphery, some of which were pustulated.
Papulovesicles were present at distance on the anterior part of the
neck (Fig. 1) and the lateral part
of the trunk, where red-brown papular lesions and non-follicular
lesions were also observed (Fig.
2). No lesions were observed on the face, scalp, extremities,
palms, soles or mucous membranes. The lesions were accompanied by
mild pruritus. History revealed no systemic disorders,
dermatological diseases or drug intake of medications associated
with disease etiology (including anastrozole, vemurafenib,
dabrafenib, cetuximab, mercury and d-penicillamine). Papular drug
eruption exhibits papules that tend to coalesce into plaques, but
do not spare the extremities. The laboratory tests reported nothing
pathological, with negative tests for VZV, HSV1 and HSV2. A skin
biopsy was performed from a papulovesicle lesion of the trunk. The
sample was fixed in 10% buffered formalin for 24 h at room
temperature. Following paraffin embedding, the tissues were cut
into 4-µm thick sections, which were then stained with H&E.
Images of the stained sections, obtained with a light microscope,
were captured using a DM1000 installed camera (Leica Microsystems,
Inc.).
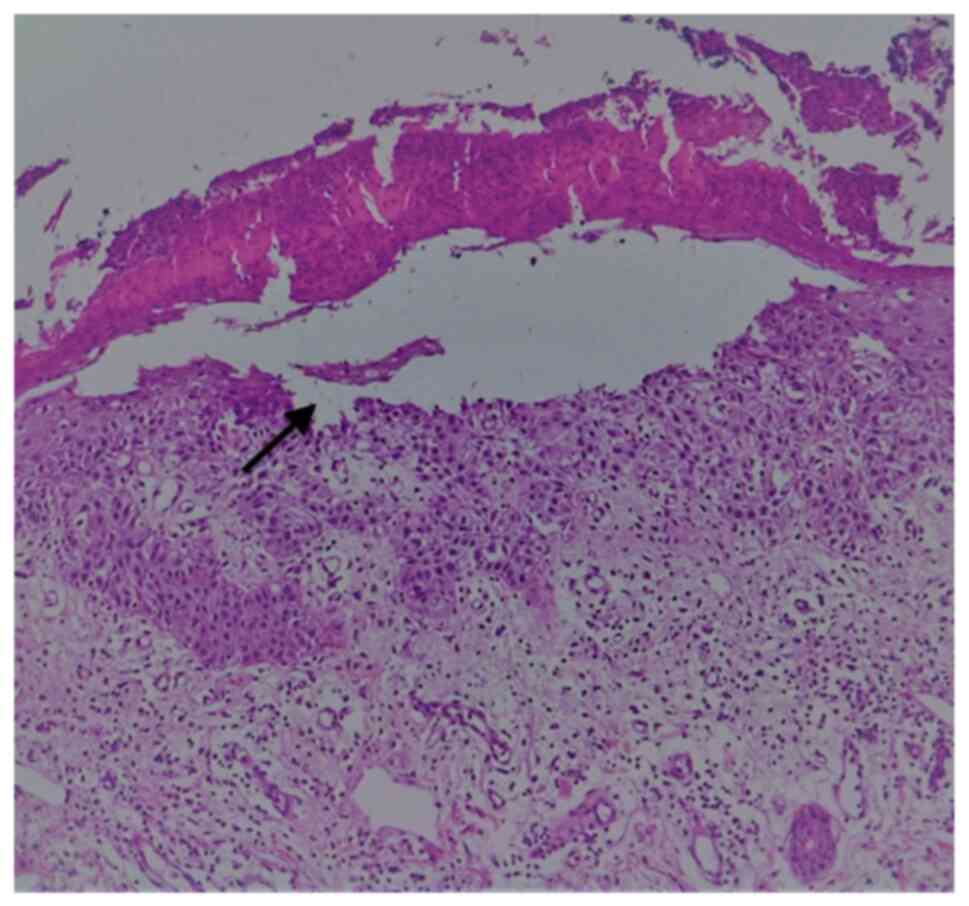
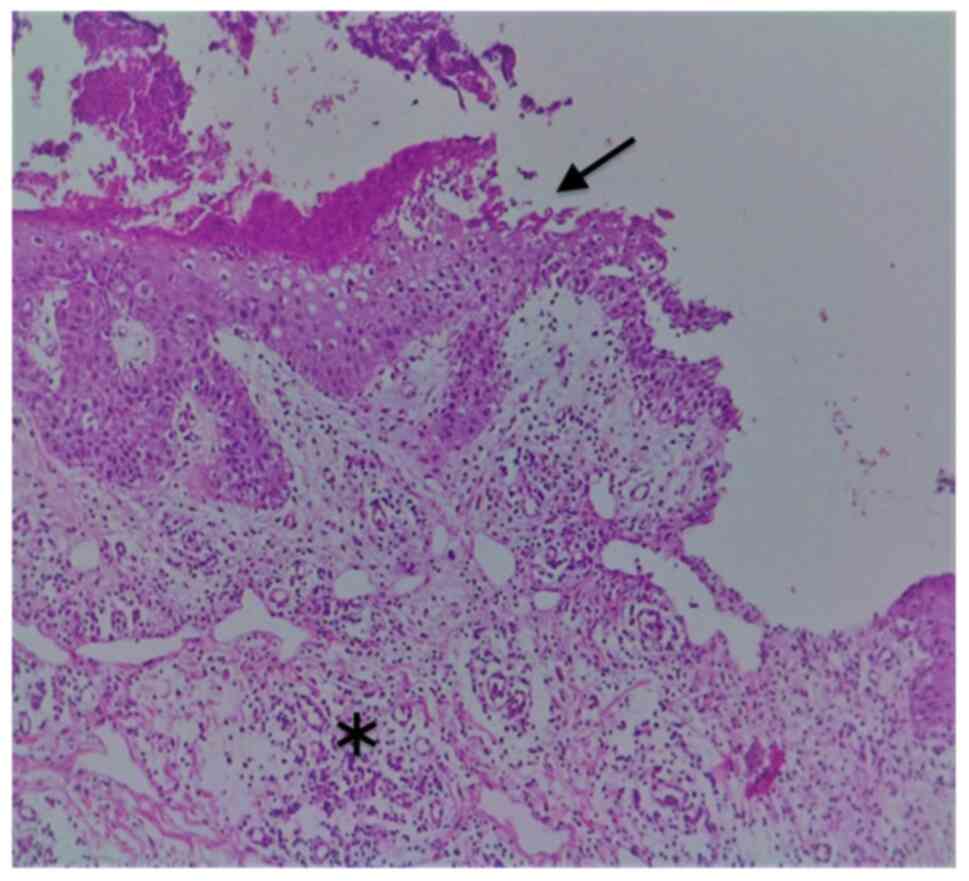
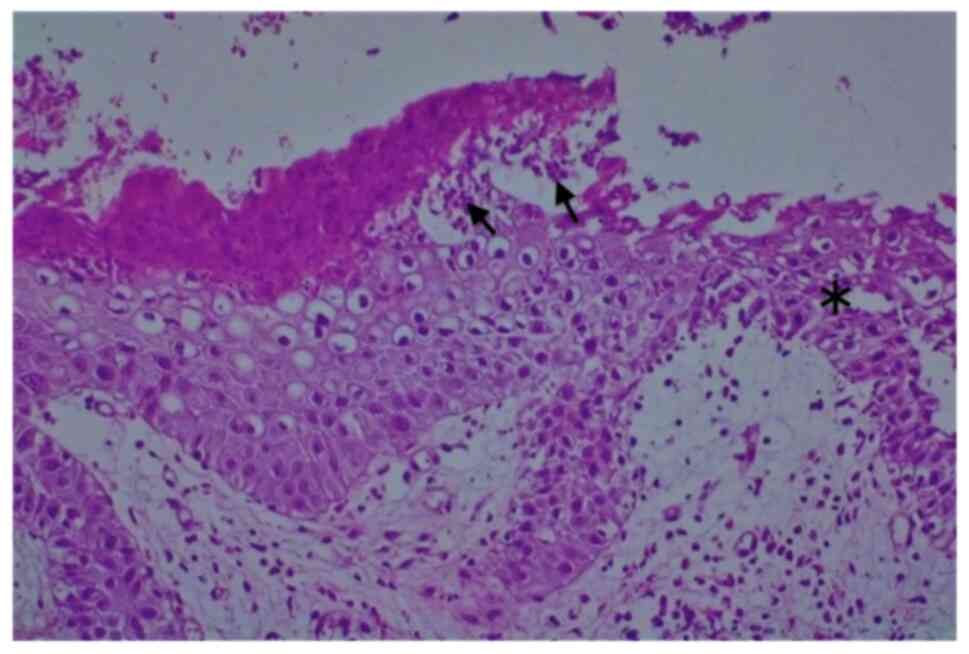
Gross examination revealed a 6/4 mm post-fixation
skin specimen with a centrally located vesicle. A polymorphous
lesion with suprabasilar and subcorneal spongiosis covered with a
thick keratin layer filled with neutrophils was observed (Figs. 3 and 4). In one area, there was an erosion of
the epidermis, potentially developed secondary to scratching. As
shown in Fig. 5, a neutrophil
microabscess adjacent to this erosion was identified. In the
papillary dermis, there was edema and mixed perivascular
inflammation (neutrophils, lymphocytes, plasma cells and
eosinophils). Detailed examination of the spongiosis revealed some
dyskeratotic round cells, with abundant granules of keratohyalin
associated with elongation of rete ridges (Darier-like patterns).
The superficial dermis that contains perivascular lymphocytes and
severe edema is shown in Fig. 5. A
total of 13 levels of the tissue sections were needed for diagnosis
of the disease via H&E staining (no immunofluorescence staining
was performed). The clue for positive diagnosis in this case was
the multiplicity of histological lesions in a single papulovesicle
of only several rete ridges wide. There were no acantholytic cells
in the lesion, which excluded the possibility of a pemphigus
vulgaris-like lesion in this patient, but suprabasilar spongiosis
can be associated with other pemphigus-like lesions. A presence of
>2 histological findings limited to small foci and specific
clinical information could mislead towards the diagnosis of Darier
disease.
Discussion
Bilateral axillaries erythematous plaques that are
well delimitated with geographical borders and pustules in the
periphery, suggested tinea corporis, but the coexistence of
polymorphous lesions as bullas, papule-vesicles, and red-brown
papular lesions on the anterior part of the neck and on the lateral
part of the trunk were considered elements for a complex diagnosis
and the decision for a skin biopsy was made in the present
case.
The second option was familial benign pemphigus
(Hailey-Hailey Disease), considering the vesicles and erythematous
plaques, erosions located on the axillary areas, bilateral, chest
and neck, but in the case assessed in the present study, there was
no family history of this disease. Hailey-Hailey Disease is a
chronic autosomal dominant disorder with incomplete penetrance.
Among those with familial benign pemphigus, ~2/3 of patients have a
family history of the disorder. Also, in cases of familial benign
pemphigus, vesicles and erythematous plaques with overlying crusts
typically occur in the genital area. Histological findings in
familial benign pemphigus are suprabasilar and widespread
acantholysis (6), not a focal one
with spongiosis as seen in the present case.
From a histological point of view, TAD presents as
focal acantholysis frequently associated with dyskeratosis that may
mimic Darier disease, Hailey-Hailey disease or pemphigus. Darier
disease (keratosis follicularis) is histologically characterized by
two primary features, acantholysis and dyskeratosis.
Hyperkeratosis, a keratin plug that overlies each lesion, is also
common. Keratosis follicularis, also known as Darier disease or
Darier-White disease, is an autosomal dominantly-inherited
genodermatosis that is characterized by greasy hyperkeratotic
papules in seborrheic regions, nail abnormalities and changes to
the mucous membrane. The majority of patients (80%) have mild
flexural involvement, with scattered papules in the groin, axillae
or sub mammary skin in women. However, in 10% of patients, flexural
disease predominates with large, warty, vegetative plaques in the
axillae, groin or perineum (5).
A lack of history of Darier Disease, no keratotic
warty lesions on seborrheic areas, no follicular involvement or
abnormalities in the nails and mucous membranes resulted in the
exclusion of the Darier disease in the present case despite
histological similarities.
TAD is an acquired acantholytic dermatosis, not an
inherited acantholytic dermatitis, such as Darier disease and
Hailey-Hailey disease. Plaques with vesicles, erosions and
erythematous papules are also seen in dermatitis herpetiformis
(24); however, the present case
did not present with clustered vesicles, herpetiform pattern
distributed over elbows, knees and/or buttocks. The diagnosis of
dermatitis herpetiformis is suspected based on the distribution of
the eruption and the genetic predisposition to the development of
gluten sensitivity, and the disease is generally accepted as a
cutaneous manifestation of celiac disease. Biopsy specimens of
lesional skin reveals neutrophils in the dermal papillae, with the
formation of microabscesses that progress to subepidermal
vacuolization and vesicle formation. Edema and eosinophils can also
be present. Granular IgA deposits observed in the dermal papillae
of perilesional skin via direct immunofluorescence is the criterion
standard of diagnosis (6,24).
In the present case, there was no history or
evidence for gluten-sensitive enteropathy. In the skin specimen
biopsy, papillary dermis edema and mixed perivascular inflammation,
containing neutrophils, lymphocytes, plasma cells and eosinophils,
were observed, but instead of a subepidermal vesicle, a
supra-epidermic, centrally located vesicle, a polymorphous lesion
with suprabasilar and subcorneal spongiosis associated with
acantholysis and dyskeratosis was identified.
Pemphigus foliaceus, which is characterized by
intraepidermal acantholysis and the loss of intercellular adhesion
of keratinocytes in the upper parts of the epidermis resulting in
the formation of superficial blisters, could be another potential
diagnosis. From a clinical point of view, typical pemphigus
foliaceus presents as small, superficial blisters or flaccid bullas
on an erythematosus base, primarily confined to seborrheic areas,
which are difficult to find because they are transient and
transform fast into crusted, scaly erosions. Pemphigus foliaceus is
an autoimmune vesiculobullous disorder that is characterized by
intraepidermal acantholysis, intercellular deposition of IgG and
complement on mucocutaneous junctions, and circulating
autoantibodies (6).
In the present case, there was no involvement of the
face and scalp, nor any itchy papules on the trunk. Only a few
erosions were identified on the trunk, not as primary elementary
lesions, but were considered secondary to scratches. Suprabasilar
acantholysis, associated with diskeratosis round cell spongiosis
with keratohyalin granules, was also highlighted.
Galli-Galli disease is a rare variant of the
genodermatosis Dowling-Degos disease, with clinical and
histological features similar to TAD (25), belonging to the spectrum of
reticulate pigment dermatoses, classified as an acantholytic
variant of Dowling-Degos disease on the basis of its characteristic
clinical and histological findings. It is a rare inherited
condition, characterized by 1-2 mm slightly keratotic red to dark
brown papules, which are confluent in a reticulate pattern, slowly
progressive and result in disfiguring reticulate hyperpigmentation
of the flexures. The histopathological characteristics consist of
suprabasal and non-dyskeratotic acantholysis.
In the present case, there was no evidence of
inherited disorders, and no clinical signs for keratotic papules or
reticulate hyperpigmentation. The patient presented with
papulovesicular lesions on an erythematous base in bilateral
axillae, and the skin specimen biopsy from a papulovesicle lesion
of the trunk showed suprabasal acantholysis with dyskeratosis and
spongiosis.
Our final diagnosis was TAD based on the clinical
and histological findings.
Oral treatment with retinoids and acitretin
(Neotigason) (20 mg/day for 9 months) was initiated. The treatment
displayed good results, and dapsone, an anti-inflammatory agent
related to inhibition of neutrophil migration and function, was
administered as a maintenance therapy to avoid recurrences. The
treatment was selected based on the existence of mixed perivascular
inflammation in papillary dermis, including neutrophils,
lymphocytes, plasma cells and eosinophils, which were identified by
histological examination.
Dapsone is an aniline derivate belonging to the
group of synthetic sulfones with antimicrobial, antiprotozoal and
anti-inflammatory effects that resemble non-steroidal
anti-inflammatory drugs. The underlying mechanism of action of
dapsone is not completely understood. Previous studies showed that
dapsone inhibits chemotaxis when certain stimuli are applied, and
displays an inhibitory effect on prostaglandin synthesis and
liberation and on eosinophil peroxidase, which provides a potential
explanation for the therapeutic efficacy of dapsone in
eosinophil-mediated diseases (26,27).
The disease-specific antiphlogistic and antichemotactic activities
and steroid-sparing effects of dapsone have resulted in its use for
the treatment of neutrophilic and/or eosinophilic dermatoses in
chronic disorders, in and outside the field of dermatology (e.g.
bronchial asthma) (26,27). The patient was monitored during
therapy for well-known adverse effects of dapsone, including
hematological effects (e.g. anemia, met-Hb formation, hemolysis and
agranulocytosis), adverse gastrointestinal effects (e.g. anorexia,
abdominal pain, nausea and vomiting), hepatic dysfunction and
neuropathy. Good results obtained with long-term dapsone treatment
resulted in selecting this treatment option for maintenance therapy
to prevent recurrences.
TAD is underdiagnosed due to its resemblance to a
number of other dermatoses, including inherited dermatoses (such as
Darier Disease, Hailey-Hailey disease and Galli-Galli disease) and
immunological-mediated dermatoses (such as pemphigus foliaceus, IgA
pemphigus and dermatitis herpetiformis). Due to the clinical
similarities with other dermatoses and variable histopathologic
findings, a high index of suspicion is necessary for the accurate
diagnosis of this disease, and a clinicopathologic correlation is
required.
The exact pathogenesis of TAD has not yet been
elucidated. Variations in sweat responses to environmental factors,
stress and emotions may be important causative factors. Therefore,
the disease could be considered as polypathogenic in nature. Future
studies are required to further investigate the etiology of this
disease.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
IB was responsible for the clinical management of
the patient, and the processing and scientific interpretation of
the data. GLF was responsible for evaluating the data and revising
the manuscript. CT was responsible for the analysis of the
specialized literature, the study of the clinical case and writing
the manuscript. OT was responsible for obtaining and processing
histopathological data. ACV was responsible for data processing and
revising the manuscript. SI was responsible for studying, data
processing and revising the manuscript. CDN was responsible for the
analysis of the specialized literature and interpreting the data.
DEB was responsible for evaluating the data and revising the
manuscript. IB, CT and GLF confirm the authenticity of all the raw
data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient.
Patient consent for publication
Written informed consent was obtained from the
patient.
Competing interests
The authors declare that they have no competing
interests.
Authors' information
Ilarie Brihan is the Head of the Dermatology Clinic
at County Emergency Clinical Hospital Oradea.
References
|
1
|
Grover RW: Transient acantholytic
dermatosis. Arch Dermatol. 101:426–434. 1970.PubMed/NCBI
|
|
2
|
Fantini F, Kovacs E and Scarabello A:
Unilateral transient acantholytic dermatosis (Grover's disease)
along Blaschko lines. J Am Acad Dermatol. 47:319–320.
2002.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Liss WA and Norins AL: Zosteriform
transient acantholytic dermatosis. J Am Acad Dermatol. 29:797–798.
1993.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kanzaki T and Hashimoto K: Transient
acantholytic dermatosis with involvement of oral mucosa. J Cutan
Pathol. 5:23–30. 1978.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Brown-Joel ZO, Chung J and Stone MS:
Pityriasis rubra pilaris-like eruption in the setting of transient
acantholytic dermatosis. JAAD Case Rep. 5:733–735. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Miller JL and Hurley HJ: Diseases of the
eccrine and apocrine sweat glands. In: Dermatology. Bolognia JL,
Jorizzo JL and Rapini PR (eds). Vol. 1. Mosby Elsevier, London,
p543, 2007.
|
|
7
|
Ho J and Bhawan J: Mimickers of classic
acantholytic diseases. J Dermatol. 44:232–242. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Cohen PR, Paravar T and Lee RA: Epidermal
multinucleated giant cells are not always a histopathologic clue to
a herpes virus infection: Multinucleated epithelial giant cells in
the epidermis of lesional skin biopsies from patients with
acantholytic dermatoses can histologically mimic a herpes virus
infection. Dermatol Pract Concept. 4:21–27. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Scheinfeld N and Mones J: Seasonal
variation of transient acantholytic dyskeratosis (Grover's
disease). J Am Acad Dermatol. 55:263–268. 2006.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Hendricks AJ, Vaughn AR, Clark AK,
Yosipovitch G and Shi VY: Sweat mechanisms and dysfunctions in
atopic dermatitis. J Dermatol Sci. 89:105–111. 2018.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Tatu AL, Elisei AM, Chioncel V, Miulescu M
and Nwabudike LC: Immunologic adverse reactions of β-blockers and
the skin. Exp Ther Med. 18:955–959. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hu Y, Converse C, Lyons MC and Hsu WH:
Neural control of sweat secretion: A review. Br J Dermatol.
178:1246–1256. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Phillips C, Kalantari-Dehaghi M, Marchenko
S, Chernyavsky AI, Galitovskiy V, Gindi V, Chun S, Paslin D and
Grando SA: Is Grover's disease an autoimmune dermatosis? Exp
Dermatol. 22:781–784. 2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ellenbogen E, Geller S, Azrielant S, Zeeli
T, Goldberg I, Schmidt E, Zillikens D, Mrowietz U, Sherman S,
Mercer S, et al: Grover disease and bullous pemphigoid: A
clinicopathological study of six cases. Clin Exp Dermatol.
44:524–527. 2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Quirk CJ and Heenan PJ: Grover's disease:
34 Years on. Australas J Dermatol. 45:83–88. 2004.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Ishibashi M, Nagasaka T and Chen KR:
Remission of transient acantholytic dermatosis after the treatment
with rituximab for follicular lymphoma. Clin Exp Dermatol.
33:206–207. 2008.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Fujita Y, Sato-Matsumura KC and Ohnishi K:
Transient acantholytic dermatosis associated with B symptoms of
follicular lymphoma. Clin Exp Dermatol. 32:752–754. 2007.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Guana AL and Cohen PR: Transient
acantholytic dermatosis in oncology patients. J Clin Oncol.
12:1703–1709. 1994.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Fernández-Figueras MT, Puig L, Cannata P,
Cuatrecases M, Quer A, Ferrándiz C and Ariza A: Grover disease: A
reappraisal of histopathological diagnostic criteria in 120 cases.
Am J Dermatopathol. 32:541–549. 2010.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Millns JL, Doyle JA and Muller SA:
Positive cutaneous immunofluorescence in Grover's disease. Arch
Dermatol. 116(515)1980.PubMed/NCBI
|
|
21
|
Lacarrubba F, Boscaglia S, Nasca MR,
Caltabiano R and Micali G: Grover's disease: Dermoscopy,
reflectance confocal microscopy and histopathological correlation.
Dermatol Pract Concept. 7:51–54. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Galamgam J and Lee D: Treatment of
transient acantholytic dermatosis with liquid nitrogen. JAAD Case
Rep. 6:341–343. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Helfman RJ: Grover's disease treated with
isotretinoin. Report of four cases. J Am Acad Dermatol. 12:981–984.
1985.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Plotnikova N and Miller JL: Dermatitis
herpetiformis. Skin Therapy Lett. 18:1–3. 2013.PubMed/NCBI
|
|
25
|
Gilchrist H, Jackson S, Morse L, Nicotri T
and Nesbitt LT: Galli-Galli disease: A case report with review of
the literature. J Am Acad Dermatol. 58:299–302. 2008.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Wozel G and Blasum C: Dapsone in
dermatology and beyond. Arch Dermatol Res. 306:103–124.
2014.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Debol SM, Herron MJ and Nelson RD:
Anti-inflammatory action of dapsone: inhibition of neutrophil
adherence is associated with inhibition of chemoattractant-induced
signal transduction. J Leukoc Biol. 62:827–836. 1997.PubMed/NCBI View Article : Google Scholar
|