Introduction
According to the World Health Organization (WHO),
breast cancer is the most frequent cancer diagnosed among women,
and also accounts for the highest number of cancer-related deaths
among women. In 2018, approximately 15% of all cancer-related
deaths among women were attributable to breast cancer (1). Recent research progress and newly
developed therapies in the approach to breast cancer have greatly
improved the quality of life and life expectancy of many patients
(2).
According to the literature, 70-75% of breast cancer
patient tumors express hormone receptors [estrogen receptor (ER)
and/or progesterone receptor (PR) positive] (3,4). As a
milestone of hormone-dependent breast cancer therapy, strategies
include selective ER modulators (SERMs, tamoxifen), selective ER
downregulators (SERDs, fulvestrant) and estrogen biosynthesis
blockers [aromatase inhibitors (AIs)] (5). More recently, hormone
receptor-positive, HER2-negative breast cancer patients with
metastatic or advanced disease may receive therapy with CDK4/6
inhibitors palbociclib or ribociclib in addition to AIs or to the
ER downregulator fulvestrant. This additional strategy has resulted
in a longer progression-free survival (PFS) compared to the
antiestrogen alone treatment in patients with advanced hormone
receptor-positive breast cancer (6).
The cell cycle is divided into four phases: G1, S,
G2 and M phase (7,8). The transition from G1 to S phase is
regulated by cyclin-dependent kinases (CDKs). In the presence of
mitogenic signals, CDK4 and CDK6 interact with cyclin D and form
the cyclin D-CDK4/6 complex which phosphorylates the retinoblastoma
protein (RB) and lifts the suppression of E2F transcription genes
which causes progression from G1 to S phase. Activities of CDKs are
affected by naturally occurring cyclin-dependent kinase inhibitors
(CKIs) (9-11).
Several oncogenic pathways including the RAS-MAPK
and PI3K pathways can stimulate the cyclin D-CDK4/6 complex which
phosphorylates RB causing inactivation of RB leading to cell
proliferation (12).
CDK4 and CDK6 together with D-type cyclins (D1, D2
and D3) promote cell cycle entry and progression through the G1
phase by inactivating RB by inhibiting an INK4 family of CDK
inhibitors (CDKN2A/B). CDK4 induces cell cycle progression and also
plays a key role in hormone-independent cell growth (13). A common feature of breast cancer is
the aberrant activation of CDKs which leads to dysregulated cell
cycle progression from G1 to the S phase. It has been shown that
some cell cycle proteins, particularly those of the cyclin
D1-CDK4/6-RB complex may play an oncogenic role in breast cancer
and also as a potential therapeutic target (13,14).
The PALOMA-1 Study showed that the addition of palbociclib (a
small-molecule inhibitor for CDK4/6) to letrozole significantly
improved PFS in women with hormone receptor-positive, HER2-negative
advanced breast cancer who had not received systemic treatment for
advanced disease (15). Ribociclib
was the second CDK4/6 inhibitor approved as treatment for hormone
receptor-positive, HER2-negative advanced breast cancer in
combination with an aromatase inhibitor (AI) in postmenopausal
women based on the MONALESSA-2 trial (16).
Fatigue is a common side effect of palbociclib while
neutropenia is a dose-limiting adverse effect of both palbociclib
and ribociclib (17). Hematologic
adverse events are common in palbociclib therapy, although it is
associated with a higher PFS rate and lower serious complication
rate (18).
Multiple fundamental studies have shown that CDK4/6
inhibitors may become a standard of care in combination with AIs or
fulvestrant in women with hormone receptor-positive/HER2-negative
advanced or metastatic breast cancer showing a significant increase
in PFS (12,17).
Patients and methods
In our gynecologic-oncology clinic of the Clinic of
Obstetrics and Gynecology, Diakonie-Klinikum Schwäbisch Hall, we
followed and registered our first clinical experience with
palbociclib and ribociclib in the two years since palbociclib and
ribociclib were officially approved for general use in Germany.
According to the drug information sheet, one cycle
of therapy with palbociclib entails 28 days consisting of 1x125
mg/day per o.s. for 21 days, followed by 7 days without therapy
(19).
The ribociclib drug information sheet recommends 600
mg ribociclib/day per o.s. for 21 days, followed by 7 days without
therapy; one therapy cycle has a length of 28 days (20).
For both drugs, it is recommended to administer the
therapy until there is progression of the tumor or unacceptable
toxicity appears.
We registered the side effects of the two drugs that
were presented by the hormone receptor-positive/HER2-negative
advanced or metastatic breast cancer patients receiving therapy
with palbociclib or ribociclib in combination with AIs or
fulvestrant. The collected data were compared with the official
drug information.
Based on the clinical experience and the official
drug information, the followed side effects included fatigue,
leukopenia, neutropenia, thrombocytopenia, mucositis, mild
alopecia, nausea, vomiting, diarrhea, elevated liver parameters
(GOT, GPT and γGT) and atrial fibrillation. We registered also the
long-term dose reduction and when during the therapy at least one
week of therapy pause was necessary because of the side effects but
subsequently it was possible to continue the therapy.
Results
In the two years of experience in our clinic, we
followed up 24 patients (41%) receiving therapy with palbociclib or
ribociclib from a total number of 59 hormone
receptor-positive/HER2-negative advanced or metastatic breast
cancer patients. The other 59% were receiving another treatment or
refused the therapy.
Our palbociclib/ribociclib group had a median age of
67 years with an age range of 44-87 years. A total of 79% of our
group received palbociclib and 21% received ribociclib.
In the palbociclib group, we found that the shortest
administration period of palbociclib was 2 months and the longest
was 34 months with ongoing therapy. In the ribociclib group, the
shortest administration period was 2 months and the longest was 14
months while the patients were still receiving therapy in
combination with letrozole.
Before the therapy with palbociclib was started, 79%
of the group had bone metastasis, 26% had lung metastasis and 37%
had liver metastasis.
Before the therapy with ribociclib was started, all
patients had bone metastasis and 60% had lung metastasis. In the
ribociclib group, there was no patient with liver metastasis before
ribociclib was started.
In the palbociclib group 74% also received
fulvestrant, 16% anastrozole and 10% letrozole.
In the ribociclib group all the patients received
denosumab because of the bone metastasis and ribociclib was
combined with letrozole in those cases, while in the palbociclib
group just 79% were given denosumab in combination.
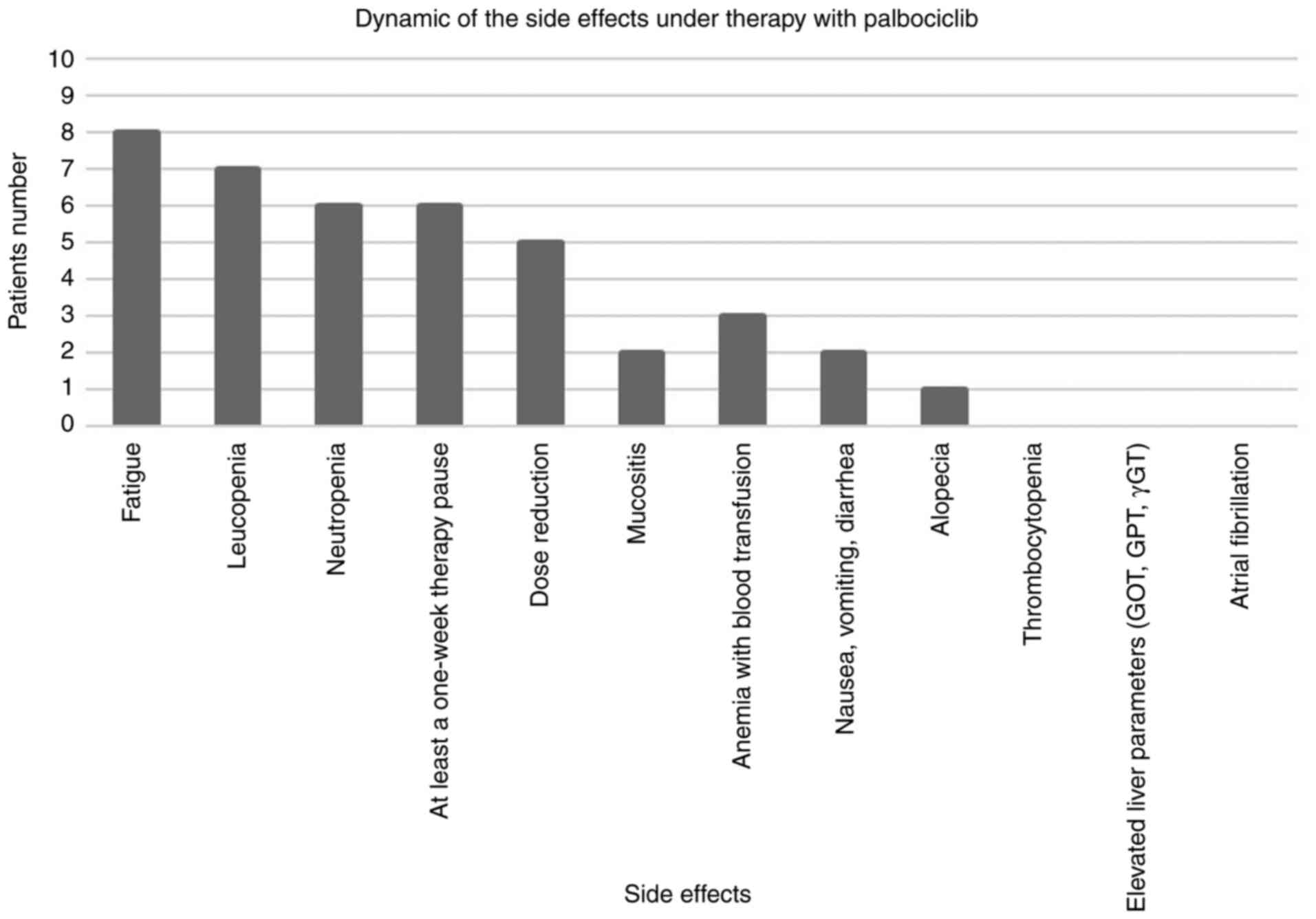
We documented the side effects under therapy with
palbociclib (Fig. 1). The main
observed and reported side effects included fatigue, leukopenia,
neutropenia, thrombocytopenia, mucositis, mild alopecia, nausea,
vomiting and diarrhea. In some of the patients, during the therapy
with palbociclib, at least one week of therapy pause was necessary
because of the side effects but subsequently it was possible to
continue the therapy. However, for some of the patients long-term
dose reduction was necessary.
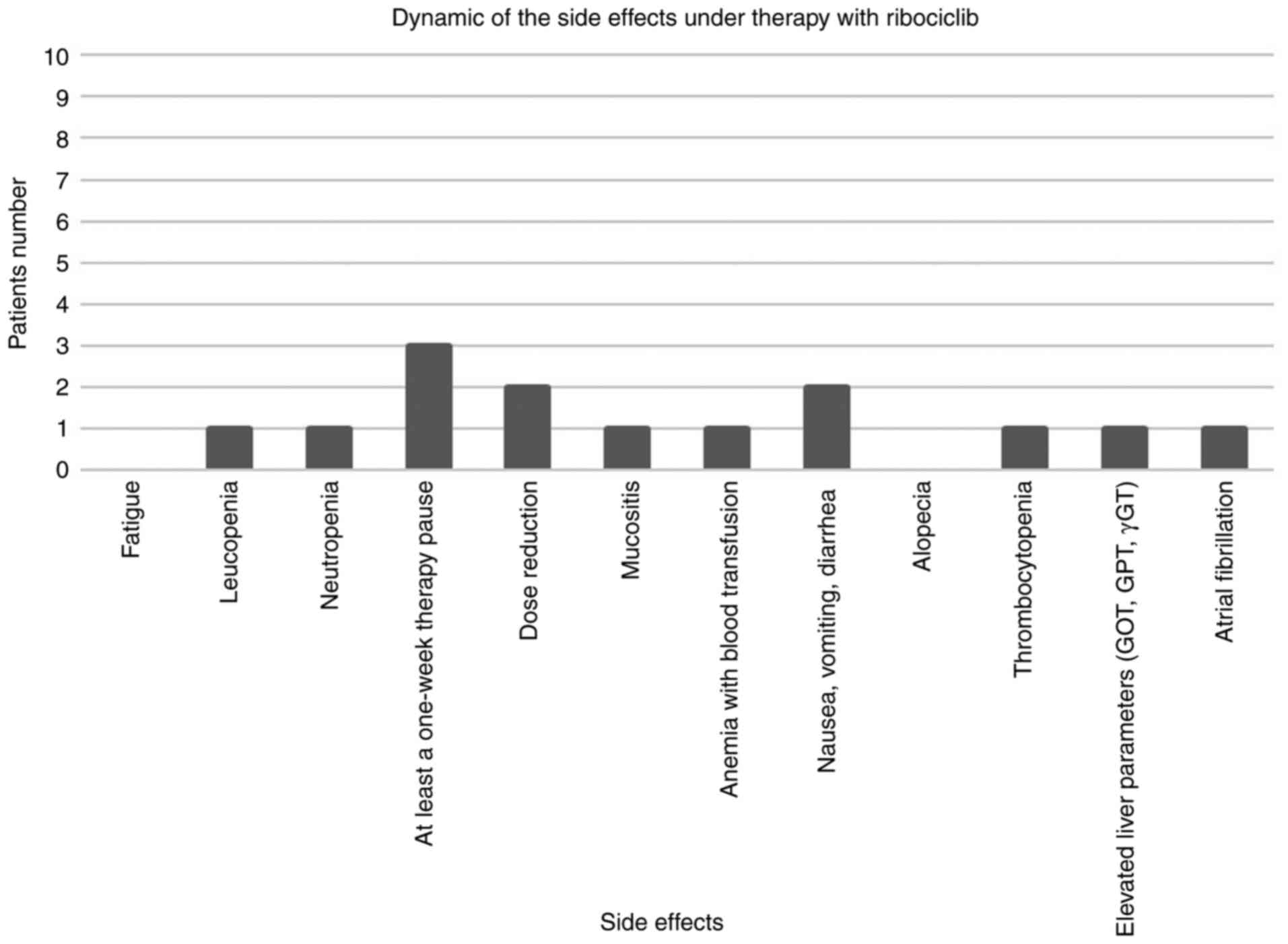
The side effects under therapy with ribociclib
(Fig. 2) consisted of leukopenia,
neutropenia, thrombocytopenia, mucositis, elevated liver parameters
(GOT, GPT and γGT), atrial fibrillation, nausea, vomiting and
diarrhea. Some patients with severe side effects or persistent
toxicity under therapy with ribociclib required at least a one-week
therapy pause. Afterwards it was possible to continue the therapy,
but in some cases long-term dose reduction was necessary.
We followed the bone metastasis under therapy with
palbociclib and we noted no tumor progression in the patients where
a re-staging could be done; 16% had stable disease, 47% had tumor
regression and in 37% the situation was unknown because the therapy
duration was too short in order to perform a re-staging.
A total of 37% of the patients with palbociclib and
liver metastasis had stable disease, 5% had tumor regression, 21%
had tumor progression and in 37% the situation is unknown because
the therapy administration was too short for performing a
re-staging.
Among the patients with lung metastasis under
therapy with palbociclib, 47% showed stable disease, 11% had tumor
regression, 5% had tumor progression and in 37% of the cases the
situation was unknown because the therapy administration was too
short for re-staging.
A total of 20% of the group under therapy with
ribociclib showed stable bone metastasis and 20% stable lung
metastasis and in 80% the situation was unknown because the therapy
administration was too short for re-staging.
We noted small differences depending on whether
palbociclib or ribociclib was used in combination with letrozole,
anastrozole or fulvestrant.
Discussion
Both cyclin-dependent kinase (CDK)4/6 inhibitors
palbociclib and ribociclib have been approved for the therapy of
hormone receptor-positive/HER2-negative advanced or metastatic
breast cancer in combination with aromatase inhibitors (AIs) or
fulvestrant in patients who have already had endocrine therapy. In
premenopausal or perimenopausal women, endocrine therapy should be
combined with a luteinizing hormone-releasing hormone (LHRH)
agonist (15,19-21).
The literature reports a median age of 62 and 63
years for patients under therapy with palbociclib and ribociclib
depending on the performed study (15,19-21).
Although our group had similar characteristics to the reported
studies, we noted that our group had a median age of 67 years.
The side effects which may appear due to the
possible toxicity of the two drugs are clinically relevant. A
detailed medical check-up before therapy and also regular
monitoring under therapy is recommended, so that the side effects
are promptly identified and the patients' therapy is optimized
depending on the situation (15,19-21).
According to the literature, the most frequent side
effects (≥20%) of therapy with palbociclib are neutropenia,
infections, leukopenia, fatigue, nausea, stomatitis, anemia,
alopecia and diarrhea (19).
The side effects experienced by our patient group
under therapy with palbociclib are shown in Fig. 1. The main reported complaint was
fatigue followed by leukopenia, and neutropenia. A therapy pause of
at least one week became necessary due to the side effects but the
therapy was subsequently continued with a prolonged dose reduction
performed according to the drug information. In a small number of
patients, mucositis, nausea, vomiting, diarrhea, mild alopecia and
thrombocytopenia were presented.
The dynamic of the side effects of ribociclib in our
study (Fig. 2) revealed leukopenia,
neutropenia, thrombocytopenia, mucositis, elevated liver parameters
(GOT, GPT an γGT), atrial fibrillation, nausea, vomiting and
diarrhea. In some patients under therapy with ribociclib, a pause
of at least one week became necessary because of the side effects
but the therapy was subsequently continued with a prolonged dose
reduction.
In the palbociclib group, 79% had bone metastasis,
26% had lung metastasis and 37% had liver metastasis before
beginning the therapy, in contrast to the palbociclib drug
information which included 23.6% patients with bone metastasis at
the beginning of the therapy and 49.2% visceral metastasis
(19). We believe that this
different distribution in metastasis is because of the different
population structure. Under palbociclib-letrozole therapy a median
progression-free survival (PFS) of 24.8 months has been previously
reported (19). According to the
PALOMA studies, the combination of palbociclib and letrozole was
continued for 24 to less than 30 months, and few patients were
treated for more than 36 months. A median exposure to palbociclib +
endocrine therapy of 13.8 months (PALOMA-1), 19.8 months (PALOMA-2)
and 10.8 months (PALOMA-3) depending on the study was reported
(22). In our palbociclib group,
the shortest administration period of palbociclib was 2 months and
the longest was 34 months and the patient had ongoing therapy.
The ribociclib drug information reports a median
therapy duration of 16.5 months and 62% of the patients received
more than 12 months of therapy and a median PFS of 24.8 months for
ribociclib-letrozole therapy (20).
We noted in our ribociclib group that the shortest administration
period was 2 months and the longest was 14 months with the patient
continuing to receive the therapy in combination with
letrozole.
In previous studies, the most common (≥20%) side
effects under ribociclib therapy were infections, neutropenia,
leukopenia, headache, cough, nausea, fatigue, diarrhea, vomiting,
constipation, alopecia, erythema and abnormal liver function tests
(20,21). Before the ribociclib-letrozole
therapy was started, 21% of the patients had bone metastasis and
59% of the patients had visceral metastasis (20) while in our ribociclib-letrozole
group before the therapy was started all patients had bone
metastasis and 60% had lung metastasis. Under ribociclib-letrozole
therapy a median tumor PFS interval of 25.3 months has been
reported (20). In our study due to
the still ongoing therapy, we did not have enough data to report on
this, but the longest ribociclib-letrozole therapy administration
was 14 months.
In conclusion, CDK4/6 inhibitors have an important
and promising role in the therapy of the hormone
receptor-positive/HER2-negative advanced or metastatic breast
cancer patients. Patients age and therapy duration do not interact
with the use of palbociclib or ribociclib, although it may be
important which AI is used in combination with palbociclib. The
longest administration period was registered in combination with
letrozole.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Further information concerning the present study is
available from the corresponding author upon reasonable
request.
Authors' contributions
IMC and AR conceived and planned in detail the
present study. IMC and AEM extracted and analyzed the entire
patient data. LM performed the computations and interpreted the
patient data together with IMC and AEM. IMC took the lead in
writing the manuscript after LM and AEM wrote some parts of the
manuscript with input from AR. IMC wrote the manuscript in
consultation with AR. AR supervised this study. All authors
discussed the results and commented on the manuscript. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
This study used pre-existing, anonymized and
irreversibly de-identified data. Approval from the ethics committee
was not required.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
World Health Organisation: Breast cancer.
http://www.who.int/cancer/prevention/diagnosis-screening/breast-cancer/en/.
Accessed September 15, 2020.
|
|
2
|
Ji F, Yang CQ, Li XL, Zhang LL, Yang M, Li
JQ, Gao HF, Zhu T, Cheng MY, Li WP, et al: Risk of breast
cancer-related death in women with a prior cancer. Aging (Albany
NY). 12:5894–5906. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Nadji M, Gomez-Fernandez C, Ganjei-Azar P
and Morales AR: Immunohistochemistry of estrogen and progesterone
receptors reconsidered: Experience with 5,993 breast cancers. Am J
Clin Pathol. 123:21–27. 2005.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Cancer Genome Atlas Network. Comprehensive
molecular portraits of human breast tumours. Nature. 490:61–70.
2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Howell A, Cuzick J, Baum M, Buzdar A,
Dowsett M, Forbes JF, Hoctin-Boes G, Houghton J, Locker GY and
Tobias JS: ATAC Trialists' Group. Results of the ATAC (arimidex,
tamoxifen, alone or in combination) trial after completion of 5
years' adjuvant treatment for breast cancer. Lancet. 365:60–62.
2005.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Finn RS, Martin M, Rugo HS, Jones S, Im
SA, Gelmon K, Harbeck N, Lipatov ON, Walshe JM, Moulder S, et al:
Palbociclib and letrozole in advanced breast cancer. N Engl J Med.
375:1925–1936. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Lundberg AS and Weinberg RA: Control of
the cell cycle and apoptosis. Eur J Cancer. 35:531–539.
1999.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Caldon CE, Daly RJ, Sutherland RL and
Musgrove EA: Cell cycle control in breast cancer cells. J Cell
Biochem. 97:261–274. 2006.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sherr CJ, Beach D and Shapiro GI:
Targeting CDK4 and CDK6: From discovery to therapy. Cancer Discov.
6:353–367. 2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Shapiro GI: Cyclin-dependent kinase
pathways as targets for cancer treatment. J Clin Oncol.
24:1770–1783. 2006.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ortega S, Malumbres M and Barbacid M:
Cyclin D-dependent kinases, INK4 inhibitors and cancer. Biochim
Biophys Acta. 1602:73–87. 2002.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Gul A, Leyland-Jones B, Dey N and Pe P: A
combination of the PI3K pathway inhibitor plus cell cycle pathway
inhibitor to combat endocrine resistance in hormone
receptor-positive breast cancer: A genomic algorithm-based
treatment approach. Am J Cancer Res. 8:2359–2376. 2018.PubMed/NCBI
|
|
13
|
Miller TW, Balko JM, Fox EM, Ghazoui Z,
Dunbier A, Anderson H, Dowsett M, Jiang A, Smith RA, Maira SM, et
al: ERα-dependent E2F transcription can mediate resistance to
estrogen deprivation in human breast cancer. Cancer Discov.
1:338–351. 2011.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Finn RS, Dering J, Conklin D, Kalous O,
Cohen DJ, Desai AJ, Ginther C, Atefi M, Chen I, Fowst C, et al: PD
0332991, a selective cyclin D kinase 4/6 inhibitor, preferentially
inhibits proliferation of luminal estrogen receptor-positive human
breast cancer cell lines in vitro. Breast Cancer Res.
11(R77)2009.PubMed/NCBI View
Article : Google Scholar
|
|
15
|
Finn RS, Crown JP, Lang I, Boer K,
Bondarenko IM, Kulyk SO, Ettl J, Patel R, Pinter T, Schmidt M, et
al: The cyclin-dependent kinase 4/6 inhibitor palbociclib in
combination with letrozole versus letrozole alone as first-line
treatment of oestrogen receptor-positive, HER2-negative, advanced
breast cancer (PALOMA-1/TRIO-18): A randomised phase 2 study.
Lancet Oncol. 16:25–35. 2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Hortobagyi GN, Stemmer SM, Burris HA, Yap
YS, Sonke GS, Paluch-Shimon S, Campone M, Blackwell KL, André F,
Winer EP, et al: Ribociclib as first-line therapy for HR-positive,
advanced breast cancer. N Engl J Med. 375:1738–1748.
2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Cersosimo RJ: Cyclin-dependent kinase 4/6
inhibitors for the management of advanced or metastatic breast
cancer in women. Am J Health Syst Pharm. 76:1183–1202.
2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Guo L, Hu Y, Chen X, Li Q, Wei B and Ma X:
Safety and efficacy profile of cyclin-dependent kinases 4/6
inhibitor palbociclib in cancer therapy: A meta-analysis of
clinical trials. Cancer Med. 8:1389–1400. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Pfizer Inc: IBRANCE 75/100/125 mg full
prescribing information. http://labeling.pfizer.com/ShowLabeling.aspx?id=2191.
Accessed September 15, 2020.
|
|
20
|
Novartis Pharmaceuticals Corporation:
Kisqali 200 mg prescribing information. https://www.novartis.us/sites/www.novartis.us/files/kisqali.pdf.
Accessed September 15, 2020.
|
|
21
|
Sonke GS, Hart LL, Campone M, Erdkamp F,
Janni W, Verma S, Villanueva C, Jakobsen E, Alba E, Wist E, et al:
Ribociclib with letrozole vs. letrozole alone in elderly patients
with hormone receptor-positive, HER2-negative breast cancer in the
randomized MONALEESA-2 trial. Breast Cancer Res Treat. 167:659–669.
2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Diéras V, Rugo HS, Schnell P, Gelmon K,
Cristofanilli M, Loi S, Colleoni M, Lu DR, Mori A, Gauthier E, et
al: Long-term pooled safety analysis of palbociclib in combination
with endocrine therapy for HR+/HER2-advanced breast cancer. J Natl
Cancer Inst. 111:419–430. 2019.PubMed/NCBI View Article : Google Scholar
|