Introduction
‘The best way to predict the future is to
create it.’ Abraham Lincoln Ankylosing spondylitis (AS) represents
a chronic inflammatory disease with incompletely known etiology,
which usually affects young men. It progresses to significant
disabilities due to skeletal disorders which include: Reduced
spinal mobility, peripheral joint injuries and extra-articular
damage (including visceral lesions) resulting in decreased quality
of life and labor productivity among these patients (1). Although the pathogenesis of AS remains
incompletely elucidated, the currently accepted hypothesis is that
AS develops through complex interactions between immune-mediated
mechanisms and genetic conditions, environmental factors, microbial
infection and endocrine disorders (2).
Various reviews and meta-analyses report that AS is
associated with a 1.5- to 2-fold higher mortality rate by
comparison with the general population, mostly linked to
cardiovascular (CV) complications (3).
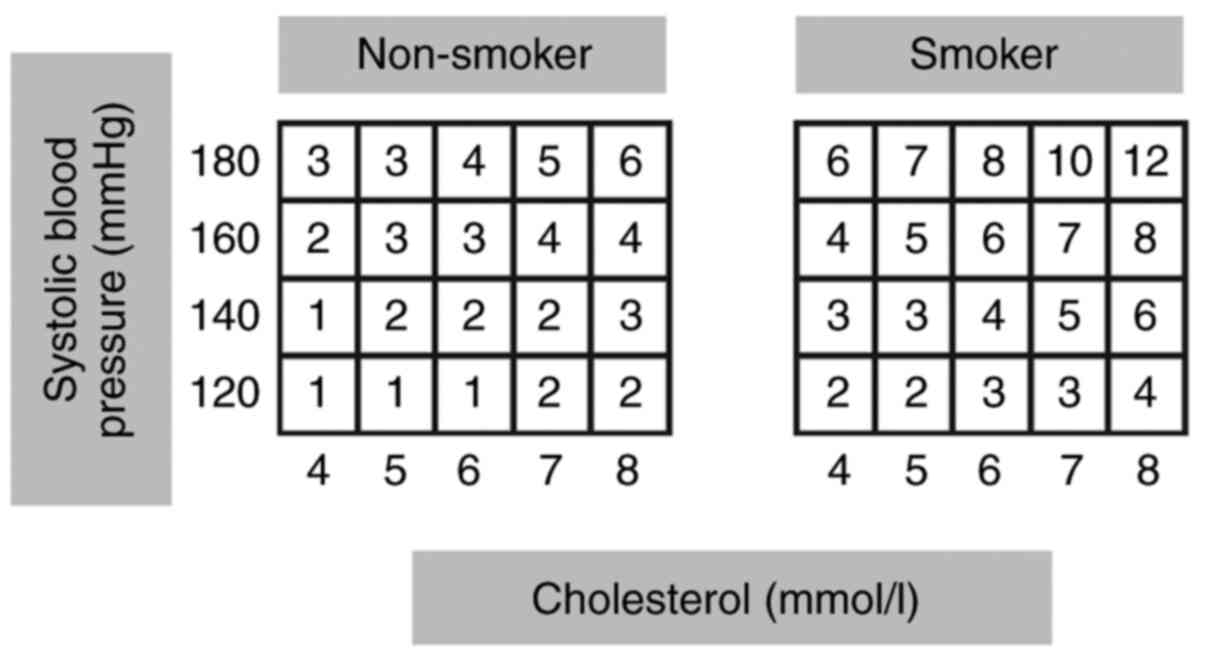
The ‘European Society of Cardiology’ (ESC) clinical
practice guidelines on CV disease prevention recommend using the
Systematic Coronary Risk Evaluation (SCORE), as a predictive model
to estimate the 10-year risk of fatal CV disease (mortality from
myocardial infarction, stroke, aortic aneurysm or others),
including the following variables: Age, sex, total cholesterol,
smoking status and systolic blood pressure levels-age having the
most significant impact in this model (4).
Although risk assessment tools can be useful aids
for physicians in establishing a patient therapeutic plan, the
‘SCORE’ presents with certain significant limitations in its
ability to identify high CV risk patients when applied to the
population under 50 years of age, thus impeding them from the
initiation of primary prevention (5,6).
Pharmacological intervention, especially statin therapy, used to
reduce CV risk is indicated only among those considered to be at
high risk of CV events; thus, a large proportion of young AS
patients can be neglected (7,8).
The 2016 ESC guidelines proposed the use of a
relative risk (RR) chart rather than the traditional SCORE model in
patients younger than 50 years. Unlike the SCORE, the RR estimates
the relative, not absolute risk, showing the likelihood of
developing a fatal CV disease in an individual with traditional CV
risk factors compared to another that does not have any risk
factors (4,9). This fact constitutes a central point
of concern in AS, a disease associated with early atherosclerosis
characterized by oxidative stress and inflammation (10,11).
We propose the use of additional tools, such as
carotid intima-media thickness (evaluated by ultrasound) (12); conduction abnormalities on ECG
(13); aortitis (14), aortic valve disease (15), cardiomyopathy or myocardial
dysfunction (16) (in particular an
abnormal relaxation pattern of the left ventricle) that can be
diagnosed by transthoracic echocardiography (TTE).
There is also recent evidence that C-reactive
protein (CRP) plays an important role in the immune response and is
a possible marker of vascular inflammation and vessel
damage-causing ischemic heart disease (IHD) (17).
Thus, the aim of the study was to determine whether
the classic risk charts may underestimate the CV risk in young
patients with AS and also to promote the necessity of new risk
assessment models and methods to achieve primary prevention of CV
disease in this population.
Patients and methods
Our study included 70 consecutive patients ≤50 years
of age (range, 35-50 years) of both genders, living in rural and
urban areas, previously diagnosed with AS according to the 1984
modified New York criteria (18).
All subjects were Romanians, and they were assessed over a 4-year
period (January 2016 to December 2019) at the Constanta County
Emergency Hospital. Exclusion criteria were patients diagnosed with
IHD, cerebrovascular disease (CVD), heart failure (HF), peripheral
artery disease (PAD), diabetes mellitus (DM) and chronic kidney
disease (CKD).
The Bath Ankylosing Spondylitis Disease Activity
Index (BASDAI) (http://www.basdai.com), Bath
Ankylosing Spondylitis Functional Index (BASFI) (http://basdai.com/BASFI.php) and Ankylosing
Spondilitis Disease Activity Score (ASDAS) (https://www.asas-group.org/instruments/asdas-calculator/)
were calculated in order to evaluate function and disability; these
scores are routinely used in clinical practice to measure the
disease activity in AS patients.
We calculated the CV risk by using the SCORE system
based on total cholesterol (TC) alone, applied for the high-risk
population, such as the Romanian population. Estimation of CV risk
was also conducted with the RR chart score, considering the
following variables: Smoking, systolic blood pressure and total
cholesterol values (Fig. 1). Both
CV risk assessment systems are included in the 2016 ESC guidelines
and are used to facilitate risk estimation in apparently healthy
individuals (4).
This study also included the prevalence of the most
common extra-articular manifestations in AS, such as uveitis,
inflammatory bowel disease and psoriasis (Table I).
 | Table IMain epidemiological, clinical and
ultrasound features of the AS group. |
Table I
Main epidemiological, clinical and
ultrasound features of the AS group.
| Variable | AS group (N=70) |
|---|
| Men/women, n (%) | 54 (77.1)/16
(22.9) |
| Age at diagnosis
(years), mean ± SD | 32.34±5.34 |
| Disease duration
(years), median (IQR) | 16.30
(4.00-27.00) |
| Rural/Urban, n
(%) | 18 (25.7)/52
(74.3) |
| Early ill health
retirement, n (%) | 33 (47.1) |
| BASDAI, mean ±
SD | 5.05±2.11 |
| BASDAI >4, n
(%) | 32 (45.7) |
| BASFI, mean ± SD | 4.36±1.96 |
| ASDAS-CRP, mean ±
SD | 3.25±0.99 |
| ASDAS-ESR, mean ±
SD | 3.36±1.02 |
| Syndesmophytes, n
(%) | 48 (68.6) |
| Extra-articular
manifestations, n (%) | 39 (55.71) |
| Inflammatory bowel
disease, n (%) | 12 (17.1) |
| Psoriasis, n
(%) | 7(10) |
| Uveitis, n (%) | 20 (28.6) |
| HLA-B27 positive, n
(%) | 55 (78.6) |
| CRP >3 mg/l at
time of diagnosis, n (%) | 55 (78.6) |
| ESR, mean ± SD - at
time of diagnosis | 30.40±16 |
| Therapy, n (%) | |
|
NSAIDs
>20 days/month | 25 (35.7) |
|
Biologic
treatment | 43 (61.4) |
|
Corticosteroids | 14(20) |
| History of classic
CV risk factors, n (%) | |
|
Current
smokers | 31 (44.3) |
|
Have ever
smoked | 11 (15.7) |
|
Obesity | 22 (31.4) |
|
Hypercholesterolemia | 14(20) |
|
Hypertension | 11 (15.7) |
|
Family
history of CV disease | 28(40) |
|
Carotid
plaques | 22 (31.4) |
|
Diastolic
dysfunction - grade I | 27 (38.6) |
|
Aortic
regurgitation (grade II-IV) | 14(20) |
| SCORE-TC, n
(%) | |
|
Low
(<1%) | 46 (65.71) |
|
Moderate (≥1
and <5%) | 24 (34.28) |
|
High (≥5 and
<10%) | 0 |
|
Very high
(≥10%) | 0 |
Statistical analysis
Data analysis was performed by using IBM SPSS
Statistics version 23 (IBM Corp). The procedures used were:
Descriptive statistics, parametric statistical tests (independent
sample t-test), non-parametric statistical tests [Chi-square test
of the association, with the evaluation of odds ratio (OR)],
adjustments for accounted variables. The significance level used in
the analysis (P-value) was 0.05. Continuous variables were reported
as mean ± standard deviation (SD) or median [interquartile range
(IQR)] and categorical variables as a number of patients
(percentage). ‘Receiver operating characteristic’ (ROC) curve [with
95% confidence interval (CI)], area under the curve (AUC) and
Youden index values were used to assess the sensitivity,
specificity, percentage of correctly classified patients, for each
CV risk model and the significant risk factors.
Results
The main demographics, clinical and ultrasound
features of the study group are summarized in Table I.
There was a significant statistical difference
between sex distributions among the study group, with male
domination (77.1%) with the age of onset peaking in the second and
third decade of life (mean age, 32.34 years) (Table I).
The majority of patients (n=46, 65.71%) had a low
risk according to the SCORE chart, and only 24 (34.28) were found
to have moderate CV risk; no patients presented with high or very
high CV risk.
A total of 10 patients (21.74%) of the 46 considered
at low risk based on the SCORE system had carotid plaques. A total
of 12 patients (50%) of the remaining 24 patients with moderate CV
risk were found to have carotid plaques (Table I).
Based on 2016 ESC guidelines, patients were
considered to have high/very high CV risk if the SCORE was ≥5 (none
in our study group) or if they had carotid plaques assessed with
ultrasounds.
According to the definition, 22 of all 70 patients
were at high/very high CV risk because of the presence of carotid
plaques.
On the contrary, when we compared the RR chart score
with the presence of carotid plaque, we found that only 4 of 30
(13.3%) patients with RR=1 had carotid plaques, and we observe that
the frequency was higher in those with RR>1 (18 of 40, 45%)
(Table II).
 | Table IIRelative risk (RR) chart
score-presence of carotid plaques. |
Table II
Relative risk (RR) chart
score-presence of carotid plaques.
| | Frequency | Percentage | Carotid plaques n
(%) |
|---|
| RR=1 | 30 | 42.86 | 4 (13.3%) |
| RR>1 | 40 | 57.14 | 18 (45%) |
| Total | 70 | 100 | 22 |
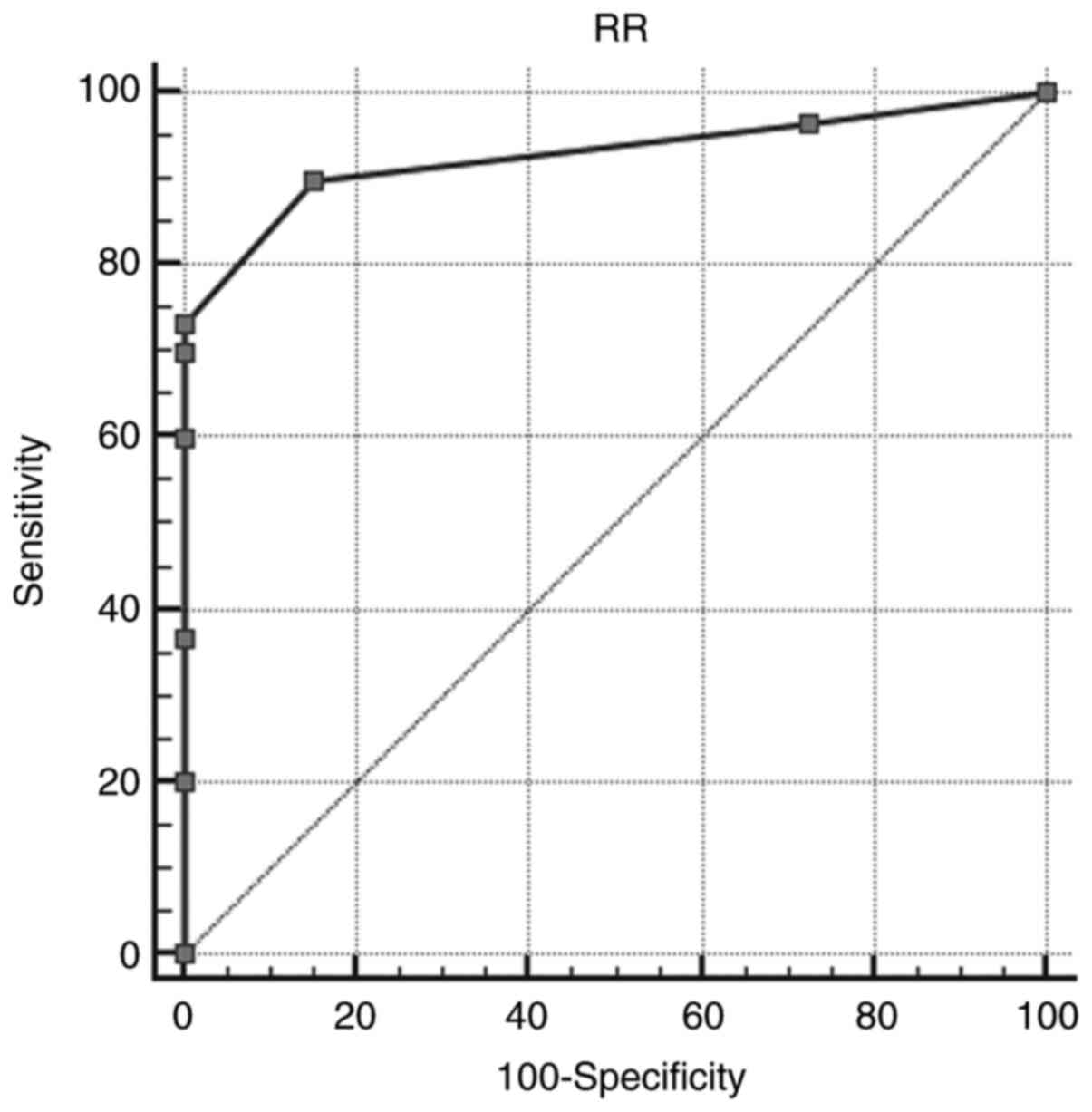
The area under the ROC curve (A=0.930) was greater
than A0=0.5; the calculated probability associated with
A was P<0.0001 (<α=0.05), and Youden index J=0.7500. Under
these conditions, we can appreciate that the relative risk (RR) has
the ability to distinguish between the two groups-the presence or
absence of carotid plaques (sensitivity=90%, specificity=85.00%,
associated criterion RR>2) (Fig.
2).
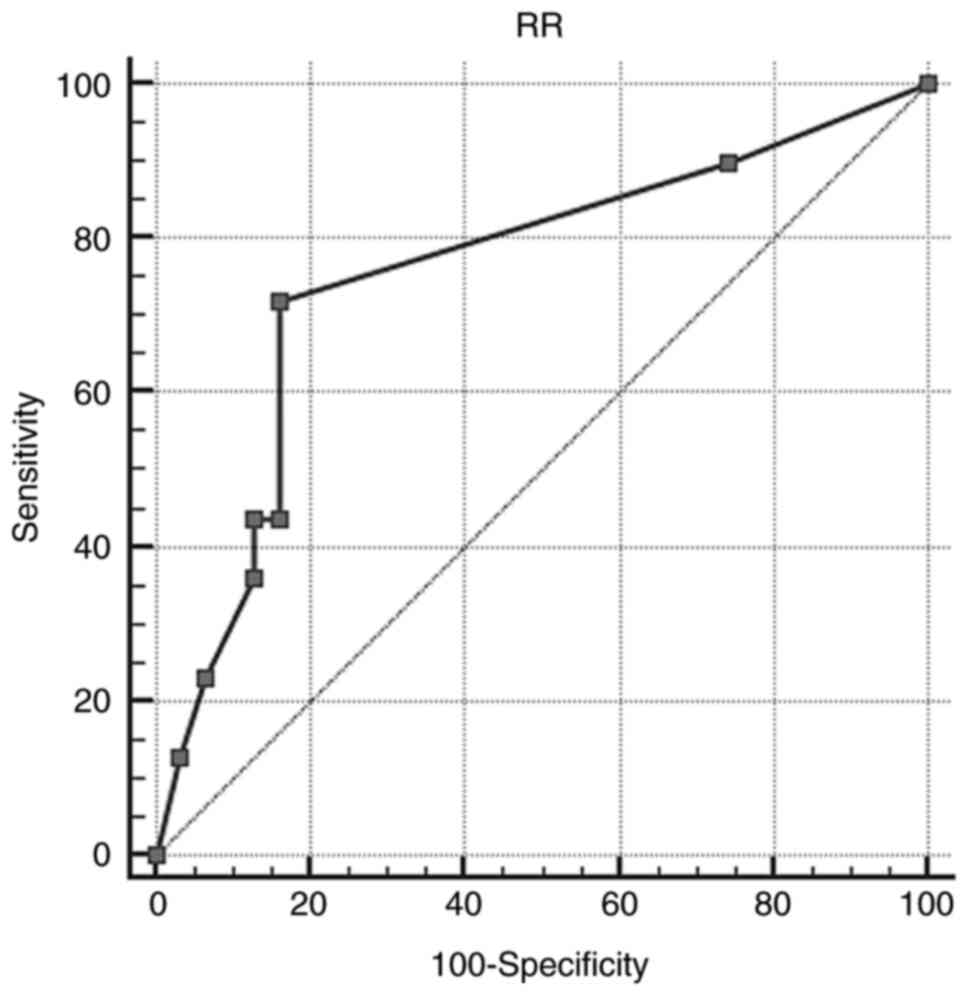
The area under the ROC curve (A=0.755) was greater
than A0=0.5; the calculated probability associated with
A was P<0.0001 (<α=0.05), and Youden index J=0.5567. Under
these conditions we can conclude that the relative risk has the
ability to distinguish between the two groups CRP >3 mg/dl or ≤3
mg/dl (sensitivity=71.79%, specificity=83.87%, associated criterion
>2) (Fig. 3).
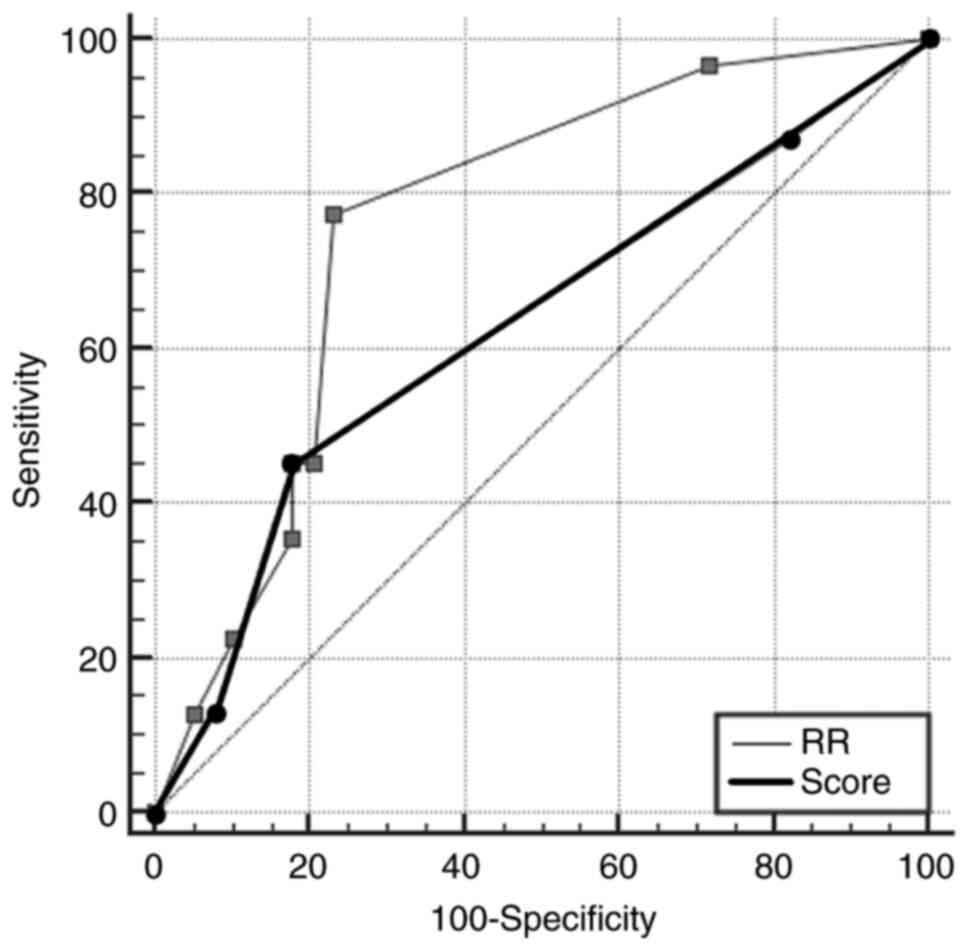
The area under the ROC curve in the case of RR
(ARR=0.764) differed significantly from the area under
the ROC curve in the case of SCORE (AS=0.627); the
difference between the area=0.137 and P=0.0160 (<α=0.05). Under
these conditions, we can appreciate that the RR variable has the
ability to distinguish better between the two groups (CRP >3
mg/dl vs. CRP ≤3 mg/dl) than the SCORE variable (Fig. 4).
According to our results, the SCORE system
underestimates the risk in the case of the patients with carotid
plaques. In contrast, the sensitivity of the RR chart was higher
(90%) if the carotid ultrasound was performed in young AS patients,
with a high sensitivity (85%). Moreover, RR>1 is associated with
CRP>3 mg/dl, making this chart a better CV risk predictive
system.
The relative risk (RR) chart score, the value of CRP
>3 mg/dl at the period of disease diagnosis throughout the
performance of carotid ultrasound can establish the presence of
high/very high cardiovascular risk.
Discussion
There is growing evidence that atherosclerosis
represent an inflammatory disease (19). The role of inflammation in the
development of heart disease has only recently been recognized
(20). Inflammatory rheumatic
disorders can be considered a ‘natural experiment’ in the
interaction between chronic inflammation and cardiovascular (CV)
disease (21). This interaction
could elucidate the fundamental mechanisms by which inflammation
accelerates the development of atherosclerosis and the onset of CV
disease (22).
Although the best-documented condition remains
rheumatoid arthritis, evidence shows that individuals suffering
from ankylosing spondylitis (AS) and psoriatic arthritis also have
an increased risk of developing CV disease (23,24).
Extra-articular manifestations of AS, such as uveitis, inflammatory
bowel disease, cardiovascular, pulmonary or renal involvement may
vary in frequency and severity (25,26),
but among the visceral manifestations, the CV damage has particular
importance, as it influences the evolution and prognosis of the
disease (27).
The socioeconomic impact of AS is represented by the
prevalence of the disease (~1% of the adult population) (28), the onset at a young age (20-40
years) in the most productive period of life, the rapidly
progressive ankylosis and disability that result in the retirement
of almost 5% of patients in the first year after diagnosis. A high
rate of early ill health retirement [33 (47.1%)] in our population
confirms the importance of early diagnosis and prevention of these
young patients (29).
Cardiovascular morbidity is elevated in AS patients,
with an increased prevalence of CV disease in all stages of
atherogenesis, from endothelial dysfunction to carotid thickening
and/or plaque and even to acute myocardial infarction or stroke
(30). In addition, even after
adjusting for traditional CV risk factors, the CV risk burden
persists, being attributed to a pro-inflammatory state of AS
(31,32).
Prediction of CV risk is an extremely important
aspect of CV prevention. Even though significant developments have
been made in recent years, risk scores for primary prevention need
to be improved, especially in patients under 50 years of age, and
new prediction models need to be developed and validated (33). There is a divergence in knowledge
for both primary and secondary prevention concerning the risk of CV
events in young patients with AS (34,35),
either on the short or on the long term, especially in different
age groups and genders (36).
Risk estimation is not an exact science since the
different combinations of risk factors interact in complex ways;
they vary as a person ages (especially the predisposing factors
that aggravate independent factors) (37,38).
The models and charts used are only approximations to reality and
must be interpreted in light of the physician's knowledge and
experience (39).
In the present study, we aimed to assess whether the
most used system to assess CV risk, the Systematic Coronary Risk
Evaluation (SCORE) chart, may underestimate the absolute risk of
developing a fatal CV disease in the case of patients under 50
years of age, previously diagnosed with AS. We concluded that RR
was superior to SCORE when trying to identify young patients with
high CV risk; in this regard AS patients with RR>1 were almost
four times more likely to have subclinical atherosclerosis than
those with RR=1 (45 vs. 13.3%), making them at high risk. The
effect of additional risk factors such as CRP and intima-media
thickness (IMT) need to be considered. Their contribution to
absolute CV risk estimations for patients with AS is important.
Our study exhibited that most of the AS patients do
not exhibit the traditional CV risk factors used by the standard
score charts. Yet, many of them are at high risk of developing CV
disease, when we consider other parameters such as CRP levels or
carotid plaques. Thus, the present study contributes to a deeper
understanding of CV risk in AS, allowing the development of
innovative patient-specific CV risk models.
To conclude, the present research pointed out that
there is still a growing need for the improvement of CV risk
prediction models suited for young patients with chronic
inflammatory diseases. The effect of the additional risk factors
such as CRP and IMT need to be considered. In this respect, further
studies need to be carried out by clinical researchers together
with statisticians and epidemiologists.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Data used in the current original study are
available in the patients' archive files, Constanta County
Emergency Hospital, Romania. Any further information regarding the
present study is available from the corresponding author upon
reasonable request.
Authors' contributions
MI, APSu and IM designed the study and collected
data from the recruited cases. PI and VA analyzed the data and
performed the statistics. APSt and IRP analyzed and wrote the
Results and Discussion sections and performed the literature
review, prepared the manuscript, translated it and managed all the
correspondence for publishing. All authors read and approved the
final manuscript for publishing.
Ethics approval and consent to
participate
This non-interventional study was approved by the
local Ethics Commission of Constanța County Emergency Hospital,
Romania (no. 32/06.09.2018).
Patient consent for publication
Not applicable.
Competing interests
There are no competing interests regarding the
authors of this research.
References
|
1
|
Zhu W, He X, Cheng K, Zhang L, Chen D,
Wang X, Qiu G, Cao X and Weng X: Ankylosing spondylitis: Etiology,
pathogenesis, and treatments. Bone Res. 7(22)2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ranganathan V, Gracey E, Brown MA, Inman
RD and Haroon N: Pathogenesis of ankylosing spondylitis-recent
advances and future directions. Nat Rev Rheumatol. 13:359–367.
2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Castañeda S, Martín-Martínez MA,
González-Juanatey C, Llorca J, García-Yébenes MJ, Pérez-Vicente S,
Sánchez-Costa JT, Díaz-Gonzalez F and González-Gay MA: CARMA
Project Collaborative Group. Cardiovascular morbidity and
associated risk factors in Spanish patients with chronic
inflammatory rheumatic diseases attending rheumatology clinics:
Baseline data of the CARMA Project. Semin Arthritis Rheum.
44:618–26. 2015.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Authors/Task Force Members. Piepoli MF,
Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney MT,
Corrà U, Cosyns B, et al: 2016 European Guidelines on
cardiovascular disease prevention in clinical practice: The Sixth
Joint Task Force of the European Society of Cardiology and Other
Societies on Cardiovascular Disease Prevention in Clinical Practice
(constituted by representatives of 10 societies and by invited
experts) Developed with the special contribution of the European
Association for Cardiovascular Prevention & Rehabilitation
(EACPR). Atherosclerosis. 252:207–274. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Rocha E: Cardiovascular risk scores:
Usefulness and limitations. Rev Port Cardiol. 35:15–8.
2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Navarini L, Caso F, Costa L, Currado D,
Stola L, Perrotta F, Delfino L, Sperti M, Deriu MA, Ruscitti P, et
al: Cardiovascular risk prediction in ankylosing spondylitis: From
traditional scores to machine learning assessment. Rheumatol Ther.
7:867–882. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Paredes S, Rocha T, Mendes D, Carvalho P,
Henriques J, Morais J, Ferreira J and Mendes M: New approaches for
improving cardiovascular risk assessment. Rev Port Cardiol.
35:5–13. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Soulaidopoulos S, Nikiphorou E,
Dimitroulas T and Kitas GD: The role of statins in disease
modification and cardiovascular risk in rheumatoid arthritis. Front
Med (Lausanne). 5(24)2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Rueda-Gotor J, Genre F, Corrales A, Blanco
R, Fuentevilla P, Portilla V, Expósito R, Arnaiz CM, Pina T,
González-Juanatey C, et al: Relative risk chart score for the
assessment of the cardiovascular risk in young patients with
ankylosing spondylitis. Int J Rheumatol.
2018(1847894)2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mathieu S and Soubrier M: Cardiovascular
events in ankylosing spondylitis: A 2018 meta-analysis. Ann Rheum
Dis. 78(e57)2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Taurog JD, Chhabra A and Colbert RA:
Ankylosing spondylitis and axial spondyloarthritis. N Engl J Med.
375(1303)2016.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yuan Y, Yang J, Zhang X, Han R, Chen M, Hu
X, Ma Y, Wu M, Wang M, Xu S and Pan F: Carotid intima-media
thickness in patients with ankylosing spondylitis: A systematic
review and updated meta-analysis. J Atheroscler Thromb. 26:260–271.
2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Bengtsson K, Klingberg E, Deminger A,
Wallberg H, Jacobsson LTH, Bergfeldt L and Forsblad-d'Elia H:
Cardiac conduction disturbances in patients with ankylosing
spondylitis: Results from a 5-year follow-up cohort study. RMD
Open. 5(e001053)2019.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Palazzi C, Salvarani C, D'Angelo S and
Olivieri I: Aortitis and periaortitis in ankylosing spondylitis.
Joint Bone Spine. 78:451–455. 2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Klingberg E, Sveälv BG, Täng MS,
Bech-Hanssen O, Forsblad-d'Elia H and Bergfeldt L: Aortic
regurgitation is common in ankylosing spondylitis: Time for routine
echocardiography evaluation? Am J Med. 128:1244–1250.e1.
2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Midtbø H, Semb AG, Matre K, Rollefstad S,
Berg IJ and Gerdts E: Left ventricular systolic myocardial function
in ankylosing spondylitis. Arthritis Care Res (Hoboken).
71:1276–1283. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Cozlea DL, Farcas DM, Nagy A, Keresztesi
AA, Tifrea R, Cozlea L and Carașca E: The impact of C reactive
protein on global cardiovascular risk on patients with coronary
artery disease. Curr Health Sci J. 39:225–31. 2013.PubMed/NCBI
|
|
18
|
Van der Linden S, Valkenburg HA and Cats
A: Evaluation of diagnostic criteria for ankylosing spondylitis. A
proposal for modification of the New York criteria. Arthritis
Rheum. 27:361–368. 1984.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Libby P: Inflammation in atherosclerosis.
Arterioscler Thromb Vasc Biol. 32:2045–2051. 2012.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Steven S, Frenis K, Oelze M, Kalinovic S,
Kuntic M, Bayo Jimenez MT, Vujacic-Mirski K, Helmstädter J,
Kröller-Schön S, Münzel T and Daiber A: Vascular inflammation and
oxidative stress: Major triggers for cardiovascular disease. Oxid
Med Cell Longev. 2019(7092151)2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Crowson CS, Liao KP, Davis JM III, Solomon
DH, Matteson EL, Knutson KL, Hlatky MA and Gabriel SE: Rheumatoid
arthritis and cardiovascular disease. Am Heart J. 166:622–628.e1.
2013.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Marchio P, Guerra-Ojeda S, Vila JM,
Aldasoro M, Victor VM and Mauricio MD: Targeting early
atherosclerosis: A focus on oxidative stress and inflammation. Oxid
Med Cell Longev. 2019(8563845)2019.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Montecucco F and Mach F: Common
inflammatory mediators orchestrate pathophysiological processes in
rheumatoid arthritis and atherosclerosis. Rheumatology (Oxford).
48:11–22. 2009.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Han C, Robinson DWJ, Hackett MV, Paramore
LC, Fraeman KH and Bala MV: Cardiovascular disease and risk factors
in patients with rheumatoid arthritis, psoriatic arthritis, and
ankylosing spondylitis. J Rheumatol. 33:2167–72. 2006.PubMed/NCBI
|
|
25
|
El Maghraoui A: Extra-articular
manifestations of ankylosing spondylitis: Prevalence,
characteristics and therapeutic implications. Eur J Intern Med.
22:554–560. 2011.PubMed/NCBI View Article : Google Scholar
|
|
26
|
de Winter JJ, van Mens LJ, van der Heijde
D, Landewé R and Baeten DL: Prevalence of peripheral and
extra-articular disease in ankylosing spondylitis versus
non-radiographic axial spondyloarthritis: A meta-analysis.
Arthritis Res Ther. 18(196)2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Ozkan Y: Cardiac involvement in ankylosing
spondylitis. J Clin Med Res. 8:427–430. 2016.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Dean LE, Jones GT, MacDonald AG, Downham
C, Sturrock RD and Macfarlane GJ: Global prevalence of ankylosing
spondylitis. Rheumatology (Oxford). 53:650–657. 2014.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Boonen A: Socioeconomic consequences of
ankylosing spondylitis. Clin Exp Rheumatol. 20 (Suppl 28):S23–S26.
2002.PubMed/NCBI
|
|
30
|
Frostegård J: Immunity, atherosclerosis
and cardiovascular disease. BMC Med. 11(117)2013.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Legge A and Hanly JG: Managing premature
atherosclerosis in patients with chronic inflammatory diseases.
CMAJ. 190:E430–E439. 2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Lostun A, Lostun G and Hainarosie R: A
retrospective study of non-violent deaths and diagnosis
discrepancies over a period of three years. Rev Chim. 67:1587–1590.
2016.
|
|
33
|
Niiranen TJ and Vasan RS: Epidemiology of
cardiovascular disease: Recent novel outlooks on risk factors and
clinical approaches. Expert Rev Cardiovasc Ther. 14:855–869.
2016.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Tournadre A, Mathieu S and Soubrier M:
Managing cardiovascular risk in patients with inflammatory
arthritis: Practical considerations. Ther Adv Musculoskelet Dis.
8:180–191. 2016.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Shen J, Shang Q and Tam LS: Targeting
inflammation in the prevention of cardiovascular disease in
patients with inflammatory arthritis. Transl Res. 167:138–151.
2016.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Landi M, Maldonado-Ficco H, Perez-Alamino
R, Maldonado-Cocco JA, Citera G, Arturi P, Sampaio-Barros PD,
Flores Alvarado DE, Burgos-Vargas R, Santos E, et al: Gender
differences among patients with primary ankylosing spondylitis and
spondylitis associated with psoriasis and inflammatory bowel
disease in an iberoamerican spondyloarthritis cohort. Medicine
(Baltimore). 95(e5652)2016.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Agca R, Heslinga SC, Rollefstad S,
Heslinga M, McInnes IB, Peters MJ, Kvien TK, Dougados M, Radner H,
Atzeni F, et al: EULAR recommendations for cardiovascular disease
risk management in patients with rheumatoid arthritis and other
forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum
Dis. 76:17–28. 2016.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Nitipir C, Orlov-Slavu C, Olaru M,
Parosanu A, Popa AM, Iaciu C, Popescu BC, Barbu MA, Pirlog C, Calu
V, et al: The Importance of dose intensity when administering
cytotoxic chemotherapy in NSCLC-A matter as actual now as in the
past. Processes. 8(936)2020.
|
|
39
|
Serban D, Smarandache AM, Cristian D,
Tudor C, Duta L and Dascalu AM: Medical errors and patient safety
culture-shifting the healthcare paradigm in Romanian hospitals. Rom
J Leg Med. 28:195–201. 2020.
|