Introduction
Hypopharyngeal cancer is a rare, aggressive
pathology usually detected in advanced stages due to the absence of
specific symptoms. Because of this late diagnosis, the treatment
modalities are usually reduced (1).
One of the most important decision-making factors involving
treatment options for patients is the associated survival rate.
However, there are pathologies, including hypopharyngeal cancer in
which the treatment modalities (primary surgery, partial or total
pharyngectomy with laryngectomy followed by radiation therapy; or
non-surgical, chemoradiation therapy; initial radiation therapy
followed by surgery) have similar survival probabilities and in
situations like this, quality of life (QoL) becomes an essential
criterion in treatment selection (2,3).
In Europe, this malignancy has an incidence rate of
1.3/100.000, with a 5-year relative survival rate of only 25%
(4). Hypopharyngeal cancer is
associated with a high rate of mortality (up to 30% in the first
year of diagnosis) and a low rate of survival to 5 years (<40%
of all patients) (1). Factors
closely associated with this pathology are tobacco use and alcohol
consumption (4); however, other
factors, such as genetic predisposition, diet, human papilloma
virus infection, Plummer-Vinson or Paterson-Brown-Kelly syndrome
are also associated with the development of this disease (1). Furthermore, additional environmental
and clinical risk factors, including asbestos (5), formaldehyde and coal dust (6), cannot be ruled out, and the clinician
must take into consideration that the reverse situation, where
genetic predisposition is augmented by environmental factors, is
even more common and complicated (7).
Due to the lack of early symptoms in this region, up
to 75% of newly diagnosed patients are in stage III and IV
(8). Another important aspect is
that upstaging to stage T4b is usually done during the surgery when
the involvement of the prevertebral fascia is revealed (1). Some of the most common symptoms in
advanced stages are presence of neck mass, airway distress,
dysphagia, gastroesophageal reflux and sore throat or referred
otalgia (1). Non-surgical treatment
options include primary radiotherapy (RT), chemo-radiation (CRT)
and surgical options, laser surgery (early stages) or a total
laryngectomy with partial or total pharyngectomy (9).
Case report
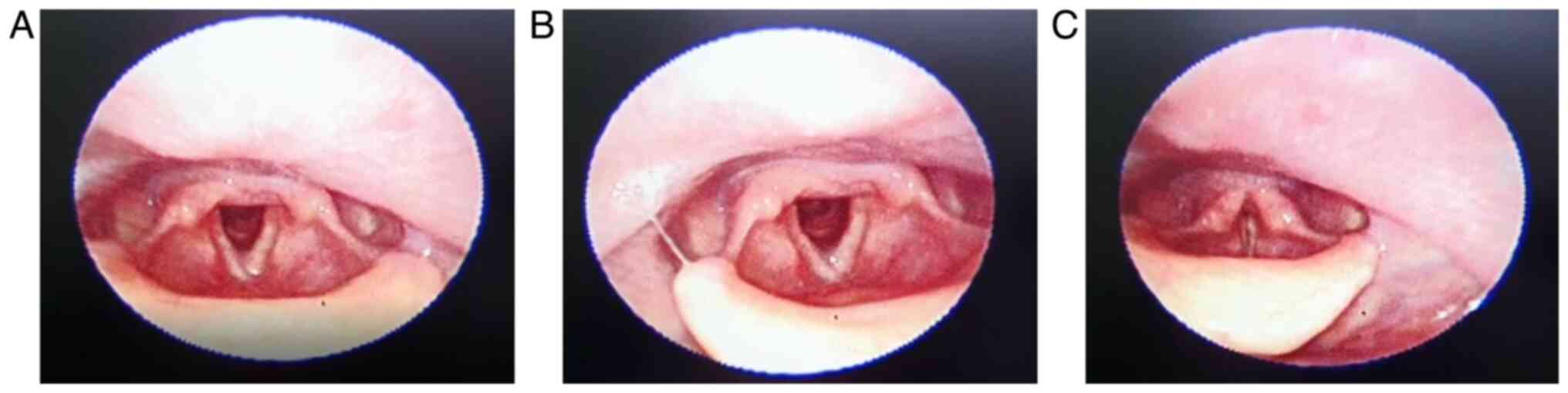
The present case report followed the evolution of a
58-year-old male patient, with a history of smoking and alcohol
consumption, that was diagnosed and treated for squamous cell
carcinoma (SCC) of the hypopharynx between September 2019 and March
2021 at the Carol Davila Central University Emergency Military
Hospital, Bucharest. The patient was admitted to the emergency unit
for airway distress, dysphonia and dysphagia and was moved to the
ear, nose and throat (ENT) clinic for investigations and treatment.
Emergency tracheostomy and biopsy of the lesion were performed,
along with computed tomography of the head and neck. ENT assessment
revealed a hypopharyngeal tumor located in the right piriform sinus
and lateral pharyngeal wall, which spread to the right vocal cord
with a mass effect and reduced respiratory flow (Fig. 1). Computed tomography revealed
pharyngeal wall thickening, with a reduced pharyngeal lumen and a
nonhomogeneous anterior laryngeal mass of 2.2-2.4 cm, with uneven
margins, between the median part of the thyroid cartilages with a
lithic effect on them. The histopathology report diagnosed the mass
as SCC, well differentiated and invasive.
Patient evaluations included laboratory testing for
the following: Complete blood count; coagulation profile (INR, TQ
and AP); erythrocyte sedimentation rate (ESR), glucose, urea,
creatinine levels; bilirubin; serum alanine aminotransferase (ALT);
serum aspartate aminotransferase (AST), sodium, potassium, serum
amylase and C-reactive protein (CRP). Questionnaires were used to
assess patient outcome, including Adult Comorbidity Evaluation-27
(ACE-27) for significant ailments (10), Karnofsky Performance Status Scale
(KPSS) (11) for functional
impairment and better understand patient requirements and the
European Organization for Research and Treatment of Cancer Quality
of Life Questionnaire (12) with
the Head and Neck Cancer Module (EORTC QLQ-H&N35), with the
commission's approval for use.
Treatment options were based on parameters, such as
age, comorbidities, the personal absence history of cancer,
objective tumor parameters [histology, location, TNM classification
Stage IV A (T4aN0M0) (13),
ACE27-2/moderate], clinical and imaging aspects, and also
subjective parameters, including personal choice, expected result
and QoL (4). Optimal treatment
strategies were discussed by a multidisciplinary team, who
considered all aforementioned factors. The treatment regimen used
was concurrent (C)CRT, using the volumetric modulated arc therapy
(VMAT), as radiation technique in a total dose of 70.2 Gy in 39
fractions, five fractions per week (1.8 Gy/fr) and six series of
chemotherapy using cisplatin (70 mg/session). The patient did not
require dose alteration for sensory neuropathy, neutropenia or
grade 3 toxicity. The patient was assessed for treatment response
via clinical/endoscopic examination and computed
tomography/magnetic resonance imaging during radiation and
chemotherapy at 3, 6 and 12 months following completion of
treatment. Following treatment, the patient was in complete
remission able to speak and breathe without the tracheal cuff.
Tracheostomy modifies the QoL through the inability
to speak, difficulties swallowing and body image alterations
(14). To prevent further
complications, such as bleeding, accidental decannulation and
occlusion, it is essential that the patient benefits from discharge
training and help from a family member (15). In the present study, the patient and
his wife were trained during the hospital stay for tracheostomy
care and discharge education. No complaints or complications
involving the tracheostomy were observed. The clinical trials that
support the use of induction chemotherapy for hypopharyngeal cancer
are not consistent as they have failed to exhibit a significant
improvement and as a result, CCRT is used as a therapeutic option
for a greater local and regional control (16,17).
Follow-up surveillance after the completion of
chemoradiation was at 3, 6, 9, 12 and 18 months, showing remission
with no distant metastasis evaluated through the imaging reports
(magnetic resonance imaging and computed tomography). The future
plan for the patient is closing the tracheostomy, 2 months after
cuff removal.
Hemoglobin levels varied throughout the study, from
12.7 g/dl in the initial visit, which decreased during CCRT
(11.8-10.2 g/dl) and increased after treatment completion (11.2
g/dl after 8 months and 13 g/dl after 14 months). Leucocyte count
decreased during CCRT; however, no significant alterations were
observed before or after this interval. Platelet number was in
between limits during the study, and inconclusive as an independent
factor. Other variables, such as INR, TQ, AP, ESR, glucose, urea,
creatinine levels, bilirubin, serum alanine aminotransferase, serum
aspartate aminotransferase, sodium, potassium, serum amylase and
C-reactive protein had variations within limit standards in all
evaluations. A common side effect of radiation therapy is the
sensory impairment of the mucosa, which is an important etiological
mechanism in swallowing disorders and aspiration (1,18). In
addition, both surgical treatment and radiation therapy can alter
laryngeal innervation and functions (10) (Table
I).
 | Table IRaw score variations for EORTC
QLQ-H&N35. |
Table I
Raw score variations for EORTC
QLQ-H&N35.
| Symptom/item | Raw score at initial
visit | Raw score before
CRT | Raw score after
CRT | Raw score 1 year
after CRT |
|---|
| Pain | 2.00 | 1.75 | 1.00 | 1.00 |
| Swallowing | 3.00 | 2.00 | 1.25 | 1.00 |
| Teeth | 1.00 | 1.00 | 1.00 | 1.00 |
| Opening mouth | 1.00 | 1.00 | 1.00 | 1.00 |
| Dry mouth | 1.00 | 1.00 | 2.00 | 1.00 |
| Sticky saliva | 1.00 | 1.00 | 2.00 | 1.00 |
| Senses | 1.00 | 1.00 | 1.5 | 1.00 |
| Coughing | 3.00 | 3.00 | 2.00 | 1.00 |
| Felt ill | 4.00 | 2.00 | 1.00 | 1.00 |
| Speech | 4.00 | 4.00 | 2.33 | 1.66 |
| Social eating | 3.25 | 3.00 | 1.25 | 1.00 |
| Social contact | 3.00 | 3.40 | 2.60 | 2.60 |
| Sexuality | - | - | - | - |
| Pain killers | 2.00 | 2.00 | 1.00 | 1.00 |
| Nutritional
supplements | 1.00 | 1.00 | 1.00 | 1.00 |
| Feeding tube | 1.00 | 1.00 | 1.00 | 1.00 |
| Weight loss | 2.00 | 2.00 | 1.00 | 1.00 |
| Weight gain | 1.00 | 1.00 | 2.00 | 2.00 |
The patient completed the Romanian version of the
EORTC QLQ-H&N35 questionnaire at each visit in the ENT clinic,
which consists of 35 items allocated in 11 single item scales
(teeth, opening mouth and dry mouth) and seven multi-item scales,
measuring symptoms, such as pain, swallowing, taste and smell and
speech. The questionnaire is reliable and valid, according to
previous studies (19,20). The scores of the questionnaire range
from 0-100. In the symptom scales, higher values correspond to a
lower QoL and a greater issue (12). The items with the highest consistent
raw scores were swallowing, speech and social contact and
discomfort, with values that decreased with time. Social contact
was partially modified by the global pandemic and legal
restrictions. In addition, the patient chose not to answer the
sexuality section.
ACE-27 is used to evaluate future development of
severe acute toxicities in patients with head and neck cancer
treated with chemoradiation therapy (10). This tool can also be used in
patients who receive primary surgical treatment for SCC, as a
prognostic indicator of mortality and complications (21). Higher grading of pre-existent
pathologies is associated with higher chances of severe acute
toxicities, postoperative surgical complications and mortality rate
(17,18). In the present study, ACE-27
indicated a moderate decompensation (grade 2) for cardiovascular
system. KPSS values varied from 20% in the initial visit (the
patient required active treatment) to 70% in the last visit (he
managed to care for himself although he could not actively work
anymore) (Fig. 2).
Discussion
Given the assumption that both treatment and
technique help performance, and medical research can sometimes
require a high degree of abstraction (22); studies so far were not able to show
a significant improvement of the survival rates and local control
using various regimens of induction chemotherapy in comparison to
the concurrent CRT, the last one remains the standard of care in
organ conservation for advanced hypopharyngeal cancer (16).
Other studies have already proven that ACE-27 score,
BMI, hemoglobin and albumin levels are independent variables of
prognosis in cancer and are useful in estimating survival and
distinguishing between risk groups (9,21,23,24).
In the present study, a good response in QoL was associated with
values that had lowering tendencies throughout evaluations. The
highest scores that accounted the most discomfort were in
swallowing, speech and social contact, similar to other QoL studies
(14,19,20).
The requirement for emergency tracheostomy did not predict future
complications; early tracheostomy care and discharge education had
an important role in maintaining good QoL. In addition, good
treatment response was associated with normal hemoglobin levels at
the end of treatment and within standard limits for platelet
number, coagulation profile, urea, creatinine levels, ALT, AST,
sodium, potassium, CRP and ESR, for the entire evaluation
period.
Further studies are required to validate the results
presented here. Prospective studies will apply this template on a
larger sample size from the QoL perspective and treatment
response.
Acknowledgements
This material is part of a larger, on-going doctoral
study by A.G. Vulcu Cordunianu, a PhD student at Titu Maiorescu
University of Bucharest, Romania, Medicine Doctoral School with
Cochior Daniel University Professor, PhD Habil, as thesis
coordinator.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and analyzed during the current
case are available from the corresponding author on reasonable
request.
Authors' contributions
AGVC and DC drafted the presentation and were
involved in the design and conception of the present study. GG and
AGVC obtained patient consent, acquired the data and confirmed
authenticity of all the raw data. MAC was responsible for data
analysis and performed the literature review. AGVC and MAC drafted
the initial manuscript. DC critically revised the manuscript for
important intellectual content. All authors have read and approved
the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
The patient provided written informed consent for
his data collection and submission for publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Vila PM and Uppaluri R: Neoplasms of the
hypopharynx and cervical esophagus. In: Cummings Otolaryngology
Head and Neck Surgery. Flint PW and Cummings CW (eds). 6th edition,
Vol II. pp1537-1553, Elsevier Saunders, Philadelphia, 2015.
|
|
2
|
Firkins J, Hansen L, Driessnack M and
Dieckmann N: Quality of life in ‘cronic’ cancer survivors: A
meta-analysis. J Cancer Survivorship. 14:504–517. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lewandowska A, Rudzki G, Lewandowski T,
Prochnicki M, Rudzki S, Laskowska B and Brudniak J: Quality of life
of cancer patients treated with chemotherapy. Int J Environ Res
Public Health. 17(6938)2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Machiels JP, René Leemans C, Golusinski W,
Grau C, Licitra L and Gregoire V: EHNS Executive Board. Electronic
address: simplesecretariat@ehns.org;
ESMO Guidelines Committee. Electronic address: simpleclinicalguidelines@esmo.org
and ESTRO Executive Board. Electronic address: simpleinfo@estro.org. Squamous
cell carcinoma of the oral cavity, larynx, oropharynx and
hypopharynx: EHNS-ESMO-ESTRO Clinical Practice Guidelines for
diagnosis, treatment and follow-up. Ann Oncol. 31:1462–1475.
2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Marchlang JL, Luce D, Leclerc A, Goldberg
P, Orlowski E, Bugel I and Brugère J: Laryngeal and hypopharyngeal
cancer and occupational exposure to asbestos and man-made vitreous
fibers: Results of a case-control study. Am J Ind Med. 37:581–589.
2000.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Laforest L, Luce D, Goldberg P, Begin D,
Gerin M, Demers PA, Brugere K and Leclerc A: Laryngeal and
hypopharyngeal cancers and occupational exposure to formaldehyde
and various dusts: A case-control study in France. Occup Environ
Med. 57:767–773. 2000.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Neagu A, Mocanu A, Bonciu A, Coada G and
Mocanu H: Prevalence of GJB2 gene mutations correlated to presence
of clinical and environmental risk factors in the etiology of
congenital sensorineural hearing loss of the Romanian population.
Exp Ther Med. 21(612)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Petersen JF, Timmermans AJ, van Dijk BAC,
Overbeek LIH, Smit LA, Hilgers FJM, Stuiver MM and van den Brekel
MWM: Trends in treatment, incidence and survival of hypopharynx
cancer: A 20-year population-based study in the Netherlands. Eur
Arch Otorhinolaryngol. 275:181–189. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Arends CR, Petersen JF, van der Noort V,
Timmermans AJ, Leemans CR, de Bree R, Van den Brekel MWM and
Stuiver MM: Survival predictions of hypopharynx cancer: Development
of a clinical prediction model. Laryngoscope. 130:2166–2172.
2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Monteiro AR, Garcia AR, Pereira TC, Macedo
F, Soares RF, Pereira K, Serra T, Khouri L, Ribeiro J and Teixeira
MM: ACE-27 as a prognostic tool of severe acute toxicities in
patients with head and neck cancer treated with chemoradiotherapy:
A real-world, prospective, observational study. Support Care
Cancer. 29:1863–1871. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Friedlander AH and Ettinger RL: Karnofsky
performance status scale. Spec Care Dentist. 29:147–148.
2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Singer S, Arraras JI, Chie WC, Fisher SE,
Galalae R, Hammerlid E, Nicolatou-Galitis O, Schmalz C, Verdonck-de
Leeuw I, Gamper E, et al: Performance of the EORTC questionnaire
for the assessment of quality of life in head and neck cancer
patients EORTC QLQ-H&N35: A methodological review. Qual Life
Res. 22:1927–1941. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
American Joint Committee on Cancer:
Oropharynx and hypopharynx. In: AJCC Cancer Staging Manual. 8th
edition. Springer, New York, NY, p16123-16135, 2017.
|
|
14
|
Seyman CC and Celik SS: Effect of
protective cover on the quality of life of patients with
tracheostomy-A quasi-experimental study. J Perianesth Nurs.
35:430–436. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Colandrea M and Eckardt P: Improving
tracheostomy care delivery: Instituting clinical care pathways and
nursing education to improve patient outcomes. ORL Head Neck Nurs.
34:7–16. 2016.PubMed/NCBI
|
|
16
|
Lim SH, Sun JM, Hong J, Oh D, Ahn YC,
Chung MK, Jeong HS, Son YI, Ahn MJ, Baek CH, et al: Induction
chemotherapy followed by concurrent chemoradiotherapy versus CCRT
for locally advanced hypopharynx and base of tongue cancer. Korean
J Intern Med. 36 (Suppl 1):S217–S224. 2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Yokota T, Shibata M, Hamauchi S, Shirasu
H, Onozawa Y, Ogawa H, Onoe T, Kawakami T, Turuta M, Inoue H, et
al: Feasibility and efficacy of chemoradiotherapy with concurrent
split-dose cisplatin after induction chemotherapy with
docetaxel/cisplatin/5-fluorouracil for locally advanced head and
neck cancer. Mol Clin Oncol. 13(35)2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Pezdirec M, Strojan P and Boltezar IH:
Swallowing disorders after treatment for head and neck cancer.
Radiol Oncol. 53:225–230. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Sherman AC, Simonton S, Adams DC, Vural E,
Owens B and Hanna E: Assessing quality of life in patients with
head and neck cancer: cross-validation of the European Organization
for Research and Treatment of Cancer (EORTC) Quality of Life Head
and Neck module (QLQ-H&N35). Arch Otolaryngol Head Neck Surg.
126:459–467. 2000.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Gomes EPAA, Aranha AMF, Borges AH and
Volpato LER: Head and Neck cancer Patients' quality of life:
Analysis of three instruments. J Dent (Shiraz). 21:31–41.
2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Milne S, Parmar J and Ong TK: Adult
comorbidity Evaluation-27 as a predictor of postoperative
complications, two-year mortality, duration of hospital stay, and
readmission within 30 days in patients with squamous cell carcinoma
of the head and neck. Br J Oral Maxillofac Surg. 57:214–218.
2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Mocanu H, Mocanu AI, Drăgoi AM and
Rădulescu M: Long-term histological results of ossicular chain
reconstruction using bioceramic implants. Exp Ther Med.
21(260)2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Caro JJ, Salas M and Goss G: Anemia as
independent prognostic factor for survival in patients with cancer:
A systemic, quantitative review. Cancer. 91:2214–2221.
2001.PubMed/NCBI
|
|
24
|
Danan D, Shonka DC Jr, Selman Y, Chow Z,
Smolkin ME and Jameson MJ: Prognostic value of albumin in patients
with head and neck cancer. Laryngoscope. 126:1567–1571.
2016.PubMed/NCBI View Article : Google Scholar
|