Introduction
With ~429 million confirmed cases of infection by
the end of February, 2022, the novel coronavirus, which causes
coronavirus disease 2019 (COVID-19), has negatively affected
patients and healthcare systems worldwide (1). Patients with COVID-19 present with a
wide spectrum of respiratory symptoms, ranging from mild flu-like
symptoms to severe and potentially life-threatening pneumonia
(2). Furthermore, some patients
report gastrointestinal symptoms, such as nausea, vomiting,
diarrhea and abdominal pain in addition to the aforementioned
respiratory symptoms or, in rare cases, as a distinct presentation
of illness (3).
In several studies, severe acute respiratory
syndrome coronavirus 2 (SARS-CoV-2) RNA has been found in stool
samples from infected individuals, and its viral receptor,
angiotensin-converting enzyme 2 (ACE2), is known to be
overexpressed all across the length of the gut mucosa, with an
increased expression in the small bowel and colon (3). These data suggest that SARS-CoV-2 can
infect and multiply effectively in the gastrointestinal system,
which may have consequences for disease treatment, transmission and
infection control (4).
Even though abdominal pain syndrome suggests acute
appendicitis, it is crucial to consider SARS-CoV-2 infection as a
potential diagnosis during this pandemic era. Prior to emergency
surgery, screening for a co-infection may change the patient
circuit and force a re-evaluation of the therapeutic strategy. In
rare situations, it may even lead to a differential diagnosis that
requires a markedly different medical therapy rather than surgery
(5). However, there have been
reports of a few cases of acute appendicitis associated with
SARS-CoV-2 infection (6). Due to
the high infectivity and potential for extensive lung damage,
healthcare professionals have to react quickly to treat individuals
who have been diagnosed with COVID-19, while they are concurrently
suffering from other diseases, such as acute appendicitis (7).
The gold standard of treatment for acute
appendicitis is appendectomy. Ηowever, research has indicated that
conservative care with intravenous antibiotics can result in
equivalent results and can be used as a substitute in some
individuals (8). Appendectomy in
patients with acute appendicitis who suffer from COVID-19 is
challenging, since it entails significant surgical risks for the
patients, as well as dangers for healthcare workers who are exposed
to SARS-CoV-2. While medical treatment decreases the morbidity and
mortality associated with surgery, it comes with a high possibility
of treatment failures, which can lead to perforation, peritonitis
and even death (9).
The present study describes five cases of adult
patients with COVID-19 with simultaneous acute appendicitis in an
aim to provide further insight into the diagnosis and management of
adult patients with COVID-19 with acute appendicitis.
Case report
Case 1
A 19-year-old male, with no significant previous
medical history, presented to the emergency department (ED) of
Laiko General Hospital (Athens, Greece) with complaints of acute
epigastric pain, nausea and multiple episodes of non-projectile,
non-bilious vomiting and diarrhea 12 h prior. The pain was sharp,
with radiation to his right lower abdominal quadrant (RLAQ) and was
aggravated by movement. He reported no fever or respiratory
symptoms, such as sore throat, dyspnea and cough.
Upon an examination, the patient appeared to be
fatigued; however, he had normal vital signs. An abdominal
examination revealed superficial and deep tenderness on the RLAQ
with guarding and rebound tenderness. Laboratory investigations
revealed an increased leukocyte count (16.11 k/µl; reference range,
4.5-11 k/µl) with neutrophilia (88.8%; reference range, 40-74%) and
lymphopenia (0.9 k/µl; reference range, 1.2-3.4 k/µl), elevated
C-reactive protein (CRP) levels (6.69 mg/l; reference range, 0-5
mg/l), elevated total bilirubin levels (1.27 mg/dl; reference
range, 0.3-1.2 mg/dl), elevated creatine kinase (CK) levels (231
U/l; reference range, 38-190 U/l) and elevated ferritin levels (452
ng/ml; reference range, 30-400 ng/ml). Pancreatic enzyme, urine
analysis, liver enzyme and renal function test results were within
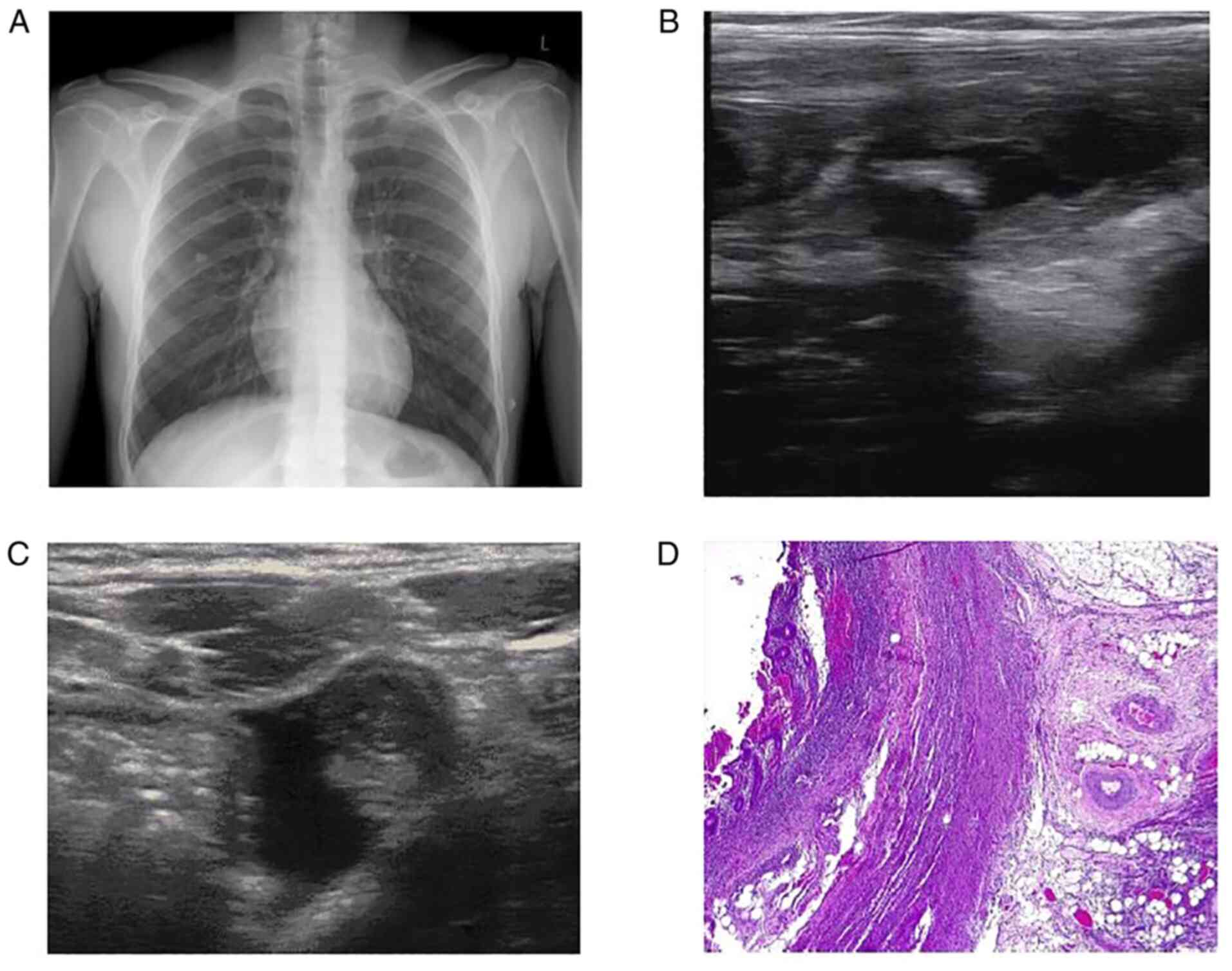
the normal range. In addition, his chest X-ray was normal (Fig. 1A).
The patient underwent abdominal and pelvic
ultrasonography (U/S), which revealed a hyperechoic shadowing
lesion consistent with an appendicolith (Fig. 1B) and a dilated appendix, that was
measured up to 0.8 cm in the transverse dimension with surrounding
fluid (Fig. 1C). The Alvarado
total score was 8 out of 10 based on the symptoms and laboratory
tests that supported the diagnosis of acute appendicitis. A reverse
transcription-PCR (RT-PCR) test for COVID-19 was conducted as per
the hospital's protocol surgery, the result of which was positive.
With all COVID-19 precautions taken, an open appendectomy was
conducted under general anesthesia. The histopathological
examination of the appendicular tissue revealed acute appendicitis
with massive inflammatory infiltrate of the appendicular wall and
mesenterium (Fig. 1D).
The patient received intravenous antibiotic therapy
with cefoxitine at 1 g three times daily and metronidazole at 500
mg three times daily. His clinical condition gradually improved. A
post-operative follow-up was uneventful and the patient was
transferred to the COVID-19 unit of the hospital for further
management. The patient had a good evolution. He never presented
symptoms indicative of respiratory involvement, nor did he receive
any specific therapy for COVID-19.
Case 2
A 62-year-old male patient with a previous medical
history of cholecystectomy presented to the ED of Laiko General
Hospital with complaints of fever, diffuse abdominal pain and
nausea 2 days prior. The pain had migrated to the RLAQ. The patient
had close contact with a patient with COVID-19 4 days prior;
however, he reported no respiratory symptoms.
Upon an examination, the patient was found to be
febrile, but the other vital signs were normal. The chest
examination was unremarkable. An abdominal examination revealed
superficial and deep tenderness on the RLAQ with guarding and
rebound tenderness. Laboratory investigations revealed a normal
leukocyte count (10.87 k/µl; reference range, 4.5-11 k/µl) with
neutrophilia (87%; reference range, 40-74%) and lymphopenia (0.840
k/µl; reference range, 1.2-3.4 k/µl), significantly elevated CRP
levels (229.75 mg/l; reference range, 0-5 mg/l), elevated alanine
aminotranferase (ALT) levels (70 U/l; reference range, <41 U/l)
and aspartate aminotransferase (AST) levels (55 U/l; reference,
15-40 U/l), increased gamma-glutamyl transferase (GGT) levels (349
U/l; reference range, 8-61 U/l), elevated CK levels (225 U/l;
reference range, 38-190 U/l) and elevated ferritin levels (1,200
ng/ml; reference range, 30-400 ng/ml). Pancreatic enzyme, urine
analysis and renal function test results were within the normal
range. An arterial blood gases analysis revealed a partial pressure
of oxygen (pO2) of 81 mmHg, a partial pressure of carbon
dioxide (pCO2) of 34 mmHg, pH 7.50 and HCO3
26.5 mmol/l in room air.
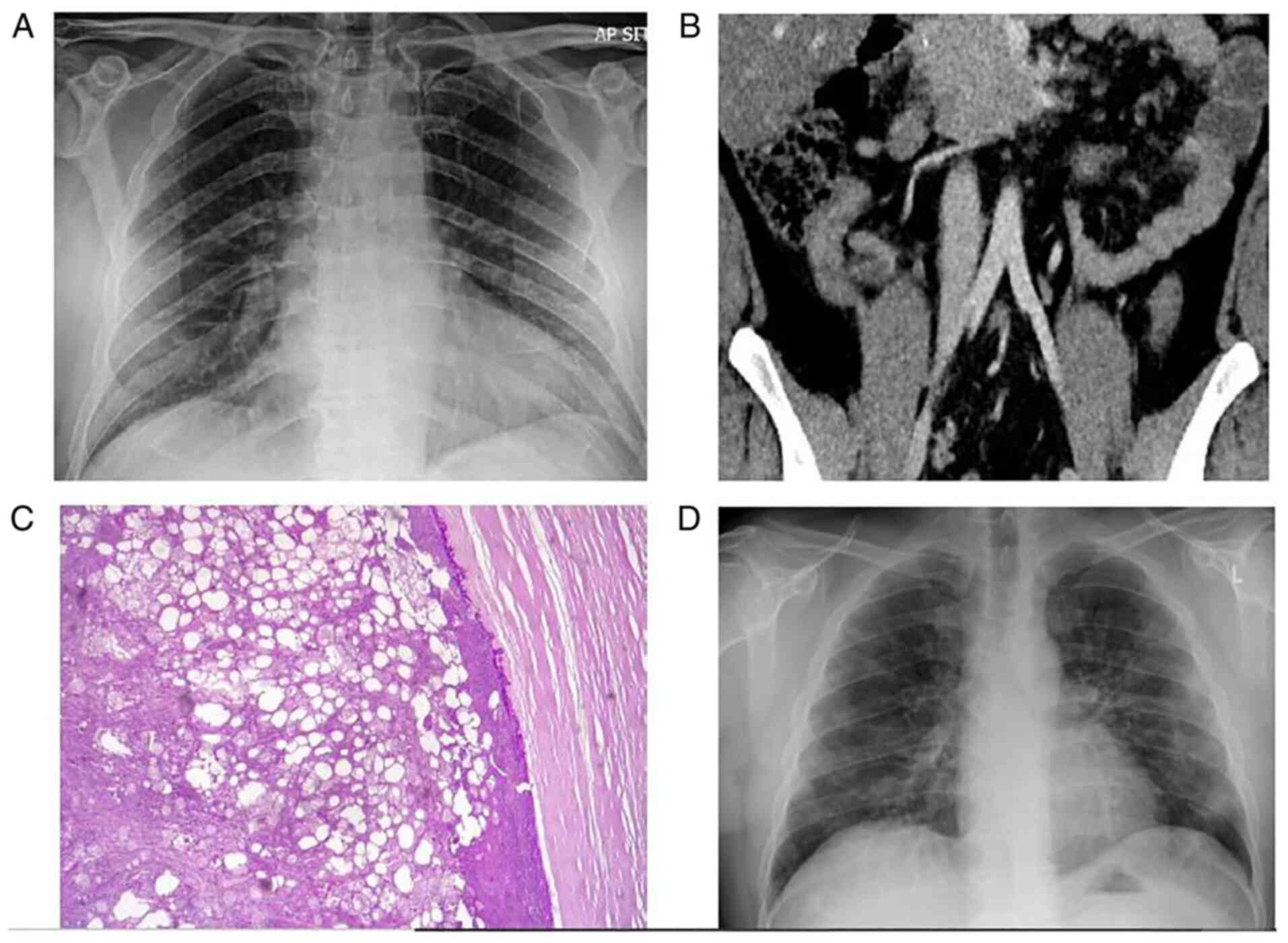
A chest X-ray was performed, which revealed mild
infiltrates in both lower lung lobes (Fig. 2A). The Alvarado total score was 9
out of 10 based on the symptoms and laboratory tests that supported
the diagnosis of acute appendicitis. The patient underwent an
abdominal computed tomography (CT) scan, which revealed the mild
dilation of the appendix and wall thickening (Fig. 2B). An RT-PCR test for COVID-19 was
conducted and the result was positive. With all COVID-19
precautions taken, an open appendectomy was conducted under general
anesthesia. The histopathological examination of the appendicular
tissue revealed acute appendicitis with peri-appendicitis (Fig. 2C).
The patient received intravenous antibiotic therapy
with cefoxitine at 1 g three times daily and metronidazole at 500
mg three times daily. His clinical condition gradually improved.
The post-operative follow-up was uneventful and the patient was
transferred to the COVID-19 unit for further management. On the
third post-operative day, the patient presented with dyspnea and
respiratory deterioration with an oxygen saturation of 92% in room
air. A new arterial bloοd gas analysis revealed a pO2 of
61 mmHg, a pCO2 of 33 mmHg, pH 7.49 and HCO3
25.1 mmol/l in room air. A new chest radiograph revealed worsening
infiltrates (Fig. 2D). The patient
received therapy with intravenous dexamethasone at 6 mg once daily
and remdesivir at 200 mg on the first day, followed by 100 mg daily
for the following 4 days. He also received oxygen therapy with a
nasal cannula delivering oxygen at a rate of 3 l/min. His clinical
condition and oxygen levels gradually improved. No other
complications occurred, and the patient was discharged following a
9-day hospitalization.
Case 3
A 51-year-old female patient presented to the ED of
Laiko General Hospital with complaints of diffuse abdominal pain
for 8 h prior to admission. The pain had migrated to the RLAQ. The
patient had experienced a mild COVID-19 infection, with fever and a
sore throat, 15 days prior to her presentation at the hospital.
Upon the visit to the ED, she did not report fever, respiratory or
other gastrointestinal symptoms. She had a previous medical history
of hypothyroidism and partial nephrectomy of the left kidney due to
renal cancer. Her current medications included levothyroxine at 100
µg daily.
Upon an examination, the patient was afebrile and
all her vital signs were normal. Chest examination was
unremarkable. Abdominal examination revealed superficial and deep
tenderness on the RLAQ with guarding and rebound tenderness.
Laboratory investigations revealed an increased leukocyte count
(14.86 k/µl; reference range, 4.5-11 k/µl) with an elevated
neutrophil count (9.881 k/µl; reference range, 1.5-6.6 k/µl) and a
normal lymphocyte count (28.5%; reference range, 19-48%), elevated
CRP levels (53.48 mg/l; reference range, 0-5 mg/,), elevated total
bilirubin levels (2.45 mg/dl; reference range, 0.3-1.2 mg/dl),
elevated ALT levels (60 U/l; reference range, <33 U/l) and AST
levels (70 U/l; reference range, 11-35 U/l), increased GGT levels
(363 U/l; reference range, 5-36 U/l), elevated CK levels (178 U/l;
reference range, 26-167 U/l) and elevated ferritin levels (678
ng/ml; reference range, 30-400 ng/ml). Pancreatic enzyme, urine
analysis, and renal function test results were within the normal
range.
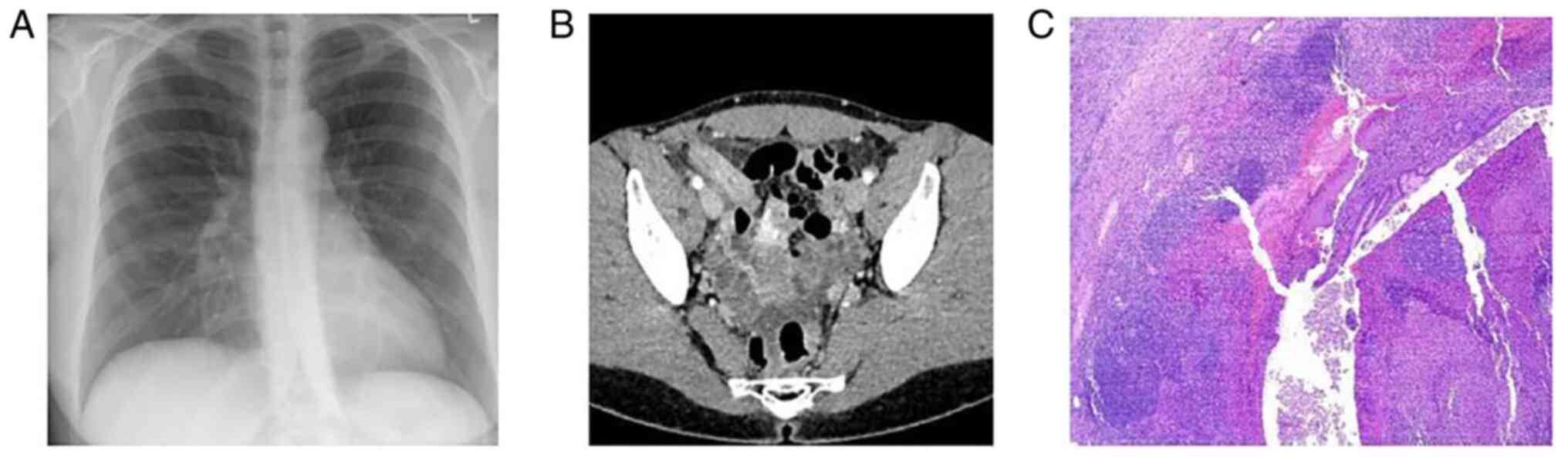
A chest X-ray was performed, which was normal
(Fig. 3A). The Alvarado total
score was 6 out of 10 based on the symptoms and laboratory tests.
The patient had possible appendicitis according to the Alvarado
score. The patient underwent an abdominal CT scan, which revealed
an enlarged appendix, with marked wall thickening and stranding of
the surrounding fat (Fig. 3B).
RT-PCR analysis for COVID-19 was conducted and the result was
positive. With all COVID-19 precautions taken, a laparoscopic
appendectomy was conducted under general anesthesia. The
histopathological examination of appendicular tissue revealed acute
appendicitis with heavily inflamed mucosa, with accompanying
extensive ulceration and hemorrhage (Fig. 3C).
The patient received intravenous antibiotic therapy
with cefoxitine at 1 g three times daily and metronidazole at 500
mg three times daily. Her clinical condition gradually improved.
The post-operative follow-up was uneventful and the patient was
transferred to the COVID-19 unit for further management. No other
complications occurred, and the patient was discharged following a
3-day hospitalization.
Case 4
A 23-year-old male patient with an insignificant
previous medical history presented to the ED of Laiko General
Hospital with complaints of diffuse abdominal pain for 12 h prior
to admission. The pain had migrated to the RLAQ. The patient had
close contact with a patient infected with COVID-19 3 days prior.
Ηe did not report fever, respiratory or other gastrointestinal
symptoms.
Upon an examination, the patient was afebrile and
all his vital signs were normal. The chest examination was
unremarkable. An abdominal examination revealed superficial and
deep tenderness on the RLAQ with guarding and rebound tenderness.
Laboratory investigations revealed an increased leukocyte count
(13.17 k/µl; reference range, 4.5-11 k/µl) with neutrophilia
(84.9%; reference range, 40-74%) and lymphopenia (1.17 k/µj;
reference range, 1.2-3.4 k/µl), elevated CRP levels (6.23 mg/l;
reference range, 0-5 mg/l) and elevated ferritin levels (434 ng/ml;
reference range, 30-400 ng/ml). Pancreatic enzyme, liver enzyme,
urine analysis and renal function test results were within the
normal range.
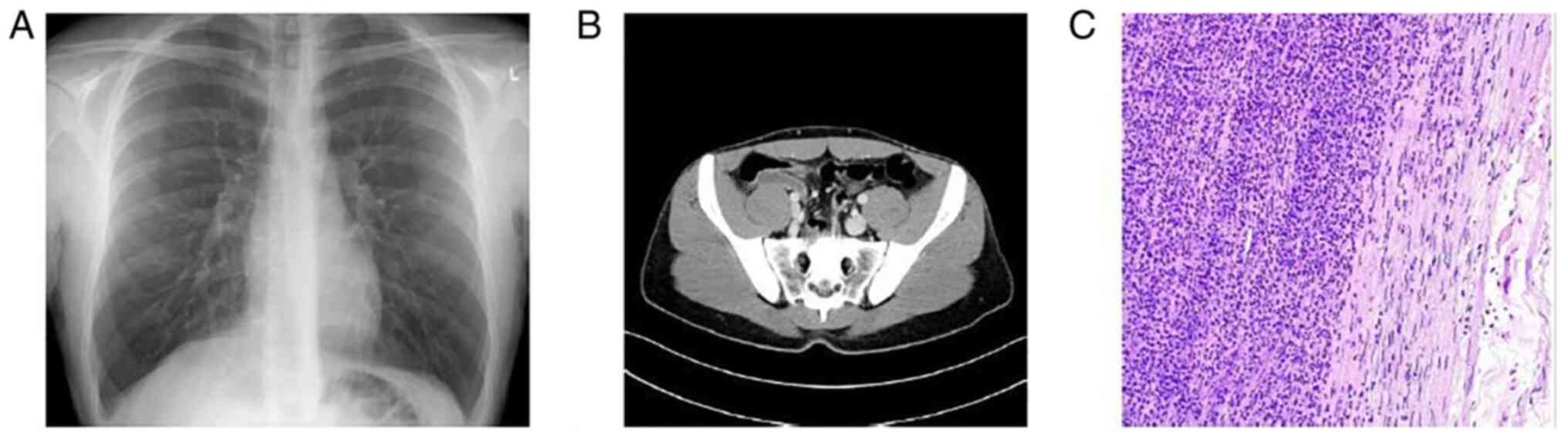
A chest X-ray was performed, which was normal
(Fig. 4A). The Alvarado total
score was 7 out of 10 based on the symptoms and laboratory tests.
The patient had probable appendicitis according to the Alvarado
score. He underwent an abdominal CT scan, which revealed an
inflamed appendix originating from the cecum in deep pelvic
position (Fig. 4B). An RT-PCR test
for COVID-19 was conducted and the result was positive. With all
COVID-19 precautions taken, an open appendectomy was conducted
under general anesthesia. The histopathological examination of
appendicular tissue revealed acute appendicitis with intense
neutropilic infiltration of the appendix wall (Fig. 4C).
The patient received intravenous antibiotic therapy
with cefoxitine at 1 g three times daily and metronidazole at 500
mg three times daily. His clinical condition gradually improved.
The post-operative follow-up was uneventful and the patient was
transferred to the COVID-19 unit for further management. No other
complications occurred, and the patient was discharged following a
4-day hospitalization. He never presented with any symptoms
indicative of respiratory involvement, nor did he receive any
specific therapy for COVID-19.
Case 5
A 60-year-old male patient presented to the ED of
Laiko General Hospital with complaints of fever and diffuse
abdominal pain for 3 days prior to admission. The pain had migrated
to the RLAQ. He did not report any respiratory or other
gastrointestinal symptoms. He had a previous medical history of
diabetes mellitus type 2, arterial hypertension, hyperlipidemia,
depression and cholecystectomy. His current medications included
metformin at 500 mg twice daily, ramipril at 2.5 mg once daily,
pitavastatin at 1 mg once daily and escitalopram at 10 mg once
daily.
Upon an examination, the patient was febrile, but
all the other vital signs were normal. The chest examination was
unremarkable. An abdominal examination revealed superficial and
deep tenderness on the RLAQ with guarding and rebound tenderness.
Laboratory investigations revealed an increased leukocyte count
(12.02 k/µl; reference range, 4.5-11 k/µl) with neutrophilia
(85.9%; reference range, 40-74%) and lymphopenia (1.009 k/µl;
reference range, 1.2-3.4 k/µl), elevated CRP levels (147.13 mg/l;
reference range, 0-5 mg/l), elevated CK levels (316 U/l; reference
range, 38-190 U/l) and elevated ferritin levels (850 ng/ml;
reference range, 30-400 ng/ml). Pancreatic enzyme, liver enzyme,
urine analysis and renal function test results were within the
normal range.
A chest X-ray was performed, which was normal
(Fig. 5A). The Alvarado total
score was 8 out of 10 based on the symptoms and laboratory tests.
The patient had probable appendicitis according to the Alvarado
score. The patient underwent an abdominal CT scan, which revealed
an appendiceal enlargement with intraluminal calcified fecalith and
marked inflammatory changes in the surrounding mesenteric fat with
possible microperforation (Fig.
5B). An RT-PCR test for COVID-19 was conducted and the result
was positive. With all COVID-19 precautions taken, a laparoscopic
appendectomy was conducted under general anesthesia. The
histopathological examination of appendicular tissue revealed acute
gangrenous appendicitis (Fig.
5C).
The patient received intravenous antibiotic therapy
with cefoxitine at 1 g three times daily and metronidazole at 500
mg three times daily. His clinical condition gradually improved.
The post-operative follow-up was uneventful and the patient was
transferred to the COVID-19 unit for further management. No other
complications occurred, and the patient was discharged following a
5-day hospitalization. He never presented with any symptoms
indicative of respiratory involvement, and he did not receive any
specific therapy for COVID-19.
Histopathological analysis
The tissue specimens from the patients were
formalin-fixed and paraffin-embedded, as to standard histopathology
laboratory routine (FFPE). The fixative used was 10% formalin
solution, neutral buffered, 10%, for 24 h at room temperature. The
thickness of the sections used was 4 µm. Histochemical staining
with hematoxylin and eosin (supplied by Dako; Agilent Technologies,
Inc.) was performed by using a DAKO Coverstainer for approximately
1 h and 15 min at room temperature. Finally, microscopic evaluation
was carried out using a light microscope (Olympus BX51; Olympus
Corporation).
Discussion
Patient characteristics and clinical
presentation
COVID-19-associated acute appendicitis occurs in
young adults, middle-aged individuals and the elderly. It can
affect both males and females. Almost all the patients described
herein presented with abdominal pain and complaints of various
other typical symptoms, such as nausea and vomiting. As regards
respiratory systems, some patients did not present with any
respiratory symptoms, whereas others had more severe symptoms and
suffered from COVID-19-related pneumonia. The diagnosis of acute
appendicitis may precede the diagnosis of SARS-CoV-2 infection, may
follow the diagnosis of SARS-CoV-2 infection or may be simultaneous
to the diagnosis of SARS-CoV-2 infection (6,10-17).
COVID-19-associated acute appendicitis has also been reported
during pregnancy (17).
Diagnostic workup
The diagnosis of SARS-CoV-2 infection in the
patients reported herein was confirmed by sending nasopharyngeal
samples for the RT-PCR analysis of COVID-19 (6,10,11,13-17).
In a previous study, SARS-CoV-2 infection was established by a
positive RT-PCR test of an appendicular tissue sample (12). Laboratory test results have
revealed increased white blood cell counts in the majority of cases
(6,11,14,16),
while lymphopenia, a hallmark of COVID-19 infection (18), has been observed in some cases
(6,15,17),
including the cases described in the present study. The diagnosis
of COVID-19-associated acute appendicitis is established either by
an abdominal U/S (6) or by an
abdominal CT scan (10-16).
In a previous study reporting a case of a pregnant woman, abdominal
magnetic resonance imaging was performed to confirm the diagnosis
(17). In all cases, resected
appendicular tissues were sent for a histological examination,
which revealed acute appendicitis (6,11-17).
Management of acute appendicitis
The majority of the cases in the present study were
managed with appendectomy, either open or laparoscopic (6,11-17).
Conservative successful treatment only with intravenous antibiotics
has also been described in one case (10).
Outcomes
All patients with COVID-19-associated acute
appendicitis reported in the literature have had an uneventful
post-operative follow-up and favorable outcomes, even in cases of
perforation (11,16-17)
and sepsis (12). The cases of
COVID-19-associated acute appendicitis found in the literature are
summarized in Table I.
 | Table ICases of COVID-19-associated acute
appendicitis identified in the literature. |
Table I
Cases of COVID-19-associated acute
appendicitis identified in the literature.
| Case no. | Author/(Refs.) | Age/sex | Diagnosis of
appendicitis | Respiratory
symptoms | Treatment of acute
appendicitis | Outcome |
|---|
| 1 | Malbul et al
(6) | 25/M | Abdominal U/S | Cough | Open
appendectomy | Recovery |
| 2 | Suwanwongse and
Shabarek (10) | 47/M | Abdominal CT | Cough, dyspnea | Conservative
management | Recovery |
| 3 | Vudayagiri and Gusz
al (11) | 27/M | Abdominal CT | None | Laparoscopic
appendectomy | Recovery |
| 4 | Ahmad et al
(12) | 28/M | Abdominal CT | None | Open
appendectomy | Recovery |
| 5 | Romero-Velez et
al (13) | 23/M | Abdominal CT | None | Laparoscopic
appendectomy | Recovery |
| 6 | Elbakouri et
al (14) | 37/F | Abdominal CT | None | Appendectomy | Recovery |
| 7 | Ngaserin et
al (15) | 21/M | Abdominal CT | None | Laparoscopic
appendectomy | Recovery |
| 8 | Kim et al
(16) | 84/F | Abdominal CT | None | Laparoscopic
appendectomy | Recovery |
| 9 | Kim et al
(16) | 69/M | Abdominal CT | Dyspnea | Laparoscopic
appendectomy | Recovery |
| 10 | Sanders-Davis and
Ritchie (17) | 35/F | Abdominal MRI | Dyspnea | Open
appendectomy | Recovery |
| 11 | The present
study | 19/M | Abdominal U/S | None | Open
appendectomy | Recovery |
| 12 | The present
study | 62/M | Abdominal CT | Dyspnea | Open
appendectomy | Recovery |
| 13 | The present
study | 51/F | Abdominal CT | None | Laparoscopic
appendectomy | Recovery |
| 14 | The present
study | 23/M | Abdominal CT | None | Open
appendectomy | Recovery |
| 15 | The present
study | 60/M | Abdominal CT | None | Open
appendectomy | Recovery |
Pathogenetic mechanisms
Due to high expression of the viral receptor, ACE2,
in the gut wall, SARS-CoV-2 may infect the intestinal wall,
compromising barrier function and facilitating microbial
translocation (19). The discovery
of the atypical histological appearance of appendicular tissue,
particularly infrequent microthrombi, the fibrinoid necrosis of
blood vessels and perivascular lymphocytic inflammatory
infiltration, which are indicative of SARS-CoV-2 infection, support
the association between SARS-CoV-2 infection and acute appendicitis
(12). Lymphocytic infiltration
and fibrinous microthrombi are notable characteristics in various
reports of lung specimens in patients with COVID-19(20).
Another feature supporting the association between
SARS-CoV-2 infection and acute appendicitis is the laboratory
findings of lymphopenia, and elevated ferritin and increased CK
levels, that have been reported in COVID-19(21). The transmission route to the
appendix is unknown. The presence of SARS-CoV-2 RNA in stool
samples from individuals with gastrointestinal symptoms suggests
that fecal-oral transmission may be a possibility. Oropharyngeal
contamination can potentially bring infection into the
gastrointestinal tract, allowing for bacterial translocation and
appendicitis (22). Moreover, it
has been reported that viral infections can cause acute
appendicitis via several mechanisms, including lymphoid
hyperplasia, which induces appendix blockage, and mucosal
ulcerations, leading to subsequent bacterial infection (23).
Safety and management concerns
During the COVID-19 pandemic, it has been reported
that the abdominal CT scan has an efficacy of 87.5% in diagnosing
acute appendicitis, compared to 69.8% before the pandemic (24). An abdominal CT scan is widely used
for diagnosis during the pandemic, and the rate of uncomplicated
appendicitis has increased from 54.05 to 69.64%. This may help to
lower the risk of viral transmission during surgery in patients
with COVID-19 and symptoms consistent with acute appendicitis
(25). An abdominal CT scan should
be used as a tool for early and accurate diagnosis and treatment,
since the prevalence of delayed diagnosis and complicated
appendicitis has increased during the pandemic, and may prevent
unnecessary operations.
There is no available evidence to indicate that
COVID-19 is transmitted by surgical smoke (26,27).
However, it has been reported that as the novel coronavirus has a
structure that is comparable to viruses that have been reported to
be transmitted by surgical smoke, such as Corynebacterium,
human papillomavirus, poliovirus, human immunodeficiency virus and
hepatitis B virus, there is a potential danger of viral
transmission. When operating on COVID-19-infected patients, it is
thus suggested to perform laparoscopic surgery rather than open
surgery using a negative pressure operating room set-up, patient
mobility and operation theater equipment (28).
In patients infected with COVID-19, post-operative
consequences need to be considered. It has been demonstrated that
the 30-day post-operative mortality rate of emergency surgery was
greater than that of elective surgery for patients infected with
COVID-19 prior to surgery. Furthermore, the mortality rate for
patients with pulmonary complications has been shown to be 39.6%
greater than the rate for patients without respiratory
complications, which was 4.6% (29). To date, to the best of our
knowledge, there are no large studies available in patients with
COVID-19 suffering from acute appendicitis to estimate the
mortality rate and the rate of complications in these patients
compared to those with acute appendicitis without COVID-19.
Furthermore, therapy with steroids, which is
administered in cases of severe COVID-19 infection, inhibits
collagen production and wound maturation, and also interferes with
the normal wound healing process (30). As a result, it is important to take
into account the likelihood of incomplete wound healing in
steroid-treated individuals. When a patient is on ventilator
support, the risk of wound complications is also increased
(31). Post-operative pneumonia,
reintubation and inability to wean are all risk factors for wound
dehiscence (32). As a result,
risk factors for wound complications in patients with COVID-19 need
to be considered.
In conclusion, since SARS-CoV-2 infection and acute
appendicitis share symptoms including fever, anorexia, nausea,
vomiting and even severe abdominal pain, the clinical diagnosis for
the surgical abdomen in patients with COVID-19 is of limited
effectiveness. SARS-CoV-2 may possibly be one of the causes of
acute abdominal cases, such as acute appendicitis. Signs and
symptoms are typically non-specific, and they may hide
life-threatening conditions. Although gastrointestinal symptoms are
less common in COVID-19, this infection cannot be ruled out and
should be explored in every case. In patients with SARS-CoV-2
infection, a high index of suspicion for surgical issues is
necessary. Furthermore, postponing surgical abdomen treatment may
result in major complications and an increased risk of mortality.
On the contrary, in patients with COVID-19, unnecessary surgery
leads to iatrogenic morbidity and mortality, an increased demand on
healthcare resources and an increased risk for healthcare
professionals working in operative areas. Therefore, a surveillance
system and defined rules are required for handling suspected
COVID-19 cases that require immediate surgery to prevent the spread
of the virus.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
VEG, CD and PP conceptualized the study. PS, SA, AA
and GS obtained the medical images and prepared the table. VEG, SM,
AP, AG and SC advised on patient care and medical treatment, and
wrote and prepared the draft of the manuscript. NT and DAS analyzed
the data and provided critical revisions. PS, SA and AA prepared
the figures. VEG and SM confirm the authenticity of all the raw
data. All authors contributed to manuscript revision and have read
and approved the final version of the manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patients described in the present case report.
Patient consent for publication
Written informed consent was obtained from the
patients for the publication of the present case report and
accompanying images. A copy of the written consent is available for
review by the Editor-in-Chief of this journal on request.
Competing interests
DAS is the Editor-in-Chief for the journal, but had
no personal involvement in the reviewing process, or any influence
in terms of adjudicating on the final decision, for this article.
The other authors declare that they have no competing
interests.
References
|
1
|
Mishra A, Basumallick S, Lu A, Chiu H,
Shah MA, Shukla Y and Tiwari A: The healthier healthcare management
models for COVID-19. J Infect Public Health. 14:927–937.
2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He
JX, Liu L, Shan H, Lei CL, Hui DSC, et al: Clinical characteristics
of coronavirus disease 2019 in China. N Engl J Med. 382:1708–1720.
2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Caio G, Lungaro L, Cultrera R, De Giorgio
R and Volta U: Coronaviruses and gastrointestinal symptoms: An old
liaison for the new SARS-CoV-2. Gastroenterol Hepatol Bed Bench.
13:341–350. 2020.PubMed/NCBI
|
|
4
|
Sultan S, Altayar O, Siddique SM, Davitkov
P, Feuerstein JD, Lim JK, Falck-Ytter Y and El-Serag HB: AGA
Institute. Electronic address: simpleewilson@gastro.org. AGA
institute rapid review of the gastrointestinal and liver
manifestations of COVID-19, meta-analysis of international data,
and recommendations for the consultative management of patients
with COVID-19. Gastroenterology. 159:320–334.e27. 2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Pautrat K and Chergui N: SARS-CoV-2
infection may result in appendicular syndrome: Chest CT scan before
appendectomy. J Visc Surg. 157 (3S1):S63–S64. 2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Malbul K, Katwal S, Maharjan S, Shrestha
S, Dhital R and Rajbhandari AP: Appendicitis as a presentation of
COVID-19: A case report. Ann Med Surg (Lond).
69(102719)2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Iyengar K, Mabrouk A, Jain VK, Venkatesan
A and Vaishya R: Learning opportunities from COVID-19 and future
effects on health care system. Diabetes Metab Syndr. 14:943–946.
2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Hansson J, Körner U, Khorram-Manesh A,
Solberg A and Lundholm K: Randomized clinical trial of antibiotic
therapy versus appendicectomy as primary treatment of acute
appendicitis in unselected patients. Br J Surg. 96:473–481.
2009.PubMed/NCBI View
Article : Google Scholar
|
|
9
|
Hansson J, Körner U, Ludwigs K, Johnsson
E, Jönsson C and Lundholm K: Antibiotics as first-line therapy for
acute appendicitis: Evidence for a change in clinical practice.
World J Surg. 36:2028–2036. 2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Suwanwongse K and Shabarek N: Successful
conservative management of acute appendicitis in a coronavirus
disease 2019 (COVID-19) Patient. Cureus. 12(e7834)2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Vudayagiri L and Gusz J: COVID-19 positive
in nasopharyngeal swab but negative in peritoneal fluid: Case
report of perforated appendicitis. Cureus. 12(e9412)2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ahmad S, Ahmed RN, Jani P, Ullah M and
Aboulgheit H: SARS-CoV-2 isolation from an appendix. J Surg Case
Rep. 2020(rjaa245)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Romero-Velez G, Pereira X, Zenilman A and
Camacho D: SARS-Cov-2 was not found in the peritoneal fluid of an
asymptomatic patient undergoing laparoscopic appendectomy. Surg
Laparosc Endosc Percutan Tech. 30:e43–e45. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Elbakouri A, El Azhary A, Bouali M,
Bensardi F, Elhattabi K and Fadil A: Gastrointestinal
manifestations related to infection with SARS-COV-2: Appendicular
syndrome (A case report). Ann Med Surg (Lond).
65(102288)2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ngaserin SH, Koh FH, Ong BC and Chew MH:
COVID-19 not detected in peritoneal fluid: A case of laparoscopic
appendicectomy for acute appendicitis in a COVID-19-infected
patient. Langenbecks Arch Surg. 405:353–355. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kim IK, Kwag SJ, Kim HG, Ju YT, Lee SJ,
Park TJ, Jeong SH, Jung EJ and Lee JK: Perioperative considerations
for acute appendicitis in patients with coronavirus infection: Two
cases report. Ann Coloproctol: Dec 7, 2021 (Epub ahead of
print).
|
|
17
|
Sanders-Davis LJ and Ritchie J:
Appendicitis with concurrent COVID-19 infection in a patient during
the third trimester of pregnancy. BMJ Case Rep.
14(e242651)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Terpos E, Ntanasis-Stathopoulos I, Elalamy
I, Kastritis E, Sergentanis TN, Politou M, Psaltopoulou T,
Gerotziafas G and Dimopoulos MA: Hematological findings and
complications of COVID-19. Am J Hematol. 95:834–847.
2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Han C, Duan C, Zhang S, Spiegel B, Shi H,
Wang W, Zhang L, Lin R, Liu J, Ding Z and Hou X: Digestive Symptoms
in COVID-19 patients with mild disease severity: Clinical
presentation, stool viral RNA testing, and outcomes. Am J
Gastroenterol. 115:916–923. 2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Wichmann D, Sperhake JP, Lütgehetmann M,
Steurer S, Edler C, Heinemann A, Heinrich F, Mushumba H, Kniep I,
Schröder AS, et al: Autopsy findings and venous thromboembolism in
patients with COVID-19: A prospective cohort study. Ann Intern Med.
173:268–277. 2020.PubMed/NCBI View
Article : Google Scholar
|
|
21
|
Alroomi M, Rajan R, Omar AA, Alsaber A,
Pan J, Fatemi M, Zhanna KD, Aboelhassan W, Almutairi F, Alotaibi N,
et al: Ferritin level: A predictor of severity and mortality in
hospitalized COVID-19 patients. Immun Inflamm Dis. 9:1648–1655.
2021.PubMed/NCBI View
Article : Google Scholar
|
|
22
|
Hindson J: COVID-19: Faecal-oral
transmission? Nat Rev Gastroenterol Hepatol. 17(259)2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Abdalhadi A, Alkhatib M, Mismar AY, Awouda
W and Albarqouni L: Can COVID 19 present like appendicitis?
IDCases. 21(e00860)2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Brown MA: Imaging acute appendicitis.
Semin Ultrasound CT MR. 29:293–307. 2008.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Somers K, Abd Elwahab S, Raza MZ, O'Grady
S, DeMarchi J, Butt A, Burke J, Robb W, Power C, McCawley N, et al:
Impact of the COVID-19 pandemic on management and outcomes in acute
appendicitis: Should these new practices be the norm? Surgeon.
19:e310–e317. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Vaghef Davari F and Sharifi A:
Transmission possibility of COVID-19 via surgical smoke generated
by the use of laparoscopic approaches: A subject of debate during
the pandemic. J Laparoendosc Adv Surg Tech A. 31:1106–1113.
2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Cheruiyot I, Sehmi P, Ngure B, Misiani M,
Karau P, Olabu B, Henry BM, Lippi G, Cirocchi R and Ogeng'o J:
Laparoscopic surgery during the COVID-19 pandemic: Detection of
SARS-COV-2 in abdominal tissues, fluids, and surgical smoke.
Langenbecks Arch Surg. 406:1007–1014. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Mowbray NG, Ansell J, Horwood J, Cornish
J, Rizkallah P, Parker A, Wall P, Spinelli A and Torkington J: Safe
management of surgical smoke in the age of COVID-19. Br J Surg.
107:1406–1413. 2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
COVIDSurg Collaborative: Mortality and
pulmonary complications in patients undergoing surgery with
perioperative SARS-CoV-2 infection: An international cohort study.
Lancet. 396:27–38. 2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Liu D, Ahmet A, Ward L, Krishnamoorthy P,
Mandelcorn ED, Leigh R, Brown JP, Cohen A and Kim H: A practical
guide to the monitoring and management of the complications of
systemic corticosteroid therapy. Allergy Asthma Clin Immunol.
9(30)2013.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Sandy-Hodgetts K, Carville K and Leslie
GD: Determining risk factors for surgical wound dehiscence: A
literature review. Int Wound J. 12:265–275. 2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Webster C, Neumayer L, Smout R, Horn S,
Daley J, Henderson W and Khuri S: National Veterans Affairs
Surgical Quality Improvement Program. Prognostic models of
abdominal wound dehiscence after laparotomy. J Surg Res.
109:130–137. 2003.PubMed/NCBI View Article : Google Scholar
|