Introduction
It is well known that peripheral artery disease
(PAD) is defined as the partial or complete obstruction of one or
multiple peripheral arteries. Previous studies have indicated that
>200 million individuals worldwide are affected by PAD, a
disease which integrates a large specter of symptoms (1). Studies have shown that due to their
important role in inflammation, leucocytes play an important role
in the development of atherosclerosis. Furthermore, as the
neutrophil-to-lymphocyte ratio (NLR) mirrors the severity of
inflammation, studies have also concluded that the NLR is
associated with a high risk of cardiovascular pathology, as well as
a higher mortality rate among patients with PAD (2,3).
Furthermore, NLR and PLR could predict poor outcome in kidney
disease (4), acute limb ischemia
(5) and PAD (6).
As they have also been correlated with PAD, the
platelet-to-lymphocyte ratio (PLR) and lymphocyte-to-monocyte ratio
(LMR) are also of clinical relevance (7,8).
Both the NLR and PLR have predictive value regarding the need for
amputation in patients with diabetes, where higher values were
exhibited in patients requiring amputation than those requiring
debridement only (6-9).
As far as the LMR is concerned, there is still no sufficient data
regarding its correlation with PAD, despite the study of a
representative population from the USA, where monocytes were the
only leucocytes to be independently associated with PAD (6-9).
Nonetheless, considering that NLR, PLR and LMR
evaluation are low-cost, consistently reproducible and easily used
on a large scale in clinical practice, they may be considered as
important steps in assessing the possibility of developing vascular
events on the strength of post-operative complications. As a
result, the aim of the present study was to evaluate the
association between NLR, PLR, LMR and the amputation rate among
patients with PAD who underwent a revascularization procedure.
Materials and methods
Study population
A total of 203 patients with PAD and diabetes
mellitus, admitted to Targu Mures Emergency County Clinical
Hospital for a surgical intervention of revascularization between
January 2017 and June 2019, were included in this retrospective
study, of which 47 were treated in an endovascular manner and 156
underwent classical surgical intervention. The inclusion criteria
were as follows: i) Patients diagnosed with PAD, who underwent a
surgical revascularization procedure; ii) available smoking
history, where patients were ‘smoker’ were considered active
smokers as well as passive smokers; iii) in terms of hypertension,
patients with systolic arterial pressure values ≥140 mmHg,
diastolic ≥90 mm Hg or using anti-hypertensive medication; and iv)
regarding diabetes, patients with a resting glucose level of ≥126
mg/dl, a plasmatic glucose level of ≥200 mg/dl after 2 h from the
oral glucose tolerance test, symptomatic hyperglycemia with random
plasmatic glucose levels of ≥200 mg/dl, or those using
anti-diabetic medication. Exclusion criteria included: i) Patients
with other inflammatory conditions other vascular pathologies; ii)
patients <18 years of age; and iii) patients with incomplete
leucocytes count data.
Data collection
The clinical characteristics of the patients, more
specifically, age, sex, body mass index (BMI), smoking history,
hypertension, chronic renal disease, heart failure, history of
myocardial infarction, history of stroke and previous medication,
were collected from medical files. Pre-operative results consisting
of the number of neutrophils, lymphocytes, thrombocytes and
monocytes were collected and evaluated. Data related to the type of
revascularization intervention and the need for postoperative
amputation were also noted. After the determination of NLR, PLR and
LMR, their association with the amputation rate was evaluated.
Study design
A retrospective study was conducted, which analyzed
data from 203 patients with PAD who underwent a revascularization
procedure; two groups were assigned based on the 203 consecutive
patients diagnosed with PAD, who were admitted for a
revascularization procedure: i) Patients requiring an amputation
procedure following revascularization intervention (n=47); and ii)
patients who did not require amputation (n=156).
Statistical analysis:
Descriptive and analytical statistics were performed
using SPSS v17.0 (SPSS, Inc.), GraphPad Prism 8 (GraphPad Software,
Inc.) and XLSTAT-Lite 2015 software for Windows 10 Pro. Grubbs test
was performed to eliminate aberrant values. Categorical variables
are presented as absolute values or percentages, and non-Gaussian
distribution data are presented as median values [confidence
intervals (CI)]. Kolmogorov-Smirnov test was performed to determine
distribution normality. In order to compare the clinical traits of
the patients, and the use of medication prior to hospital
admission, Fisher's exact test was performed for categorical
variables, and the Mann Whitney U test for ordinal values. The Mann
Whitney test was also used to compare the leucocyte ratios between
the two patient groups. Spearman's receiver operating
characteristic (ROC) curve analysis was used to determine the
cut-off values. Spearman's correlation coefficient was used to
determine correlations between the NLR, PLR, LMR and Fontaine
class, the number of affected vessels, high-density lipoprotein
(HDL) and low-density lipoprotein (LDL) values. P<0.05 was
considered to indicate a statistically significant difference.
Results
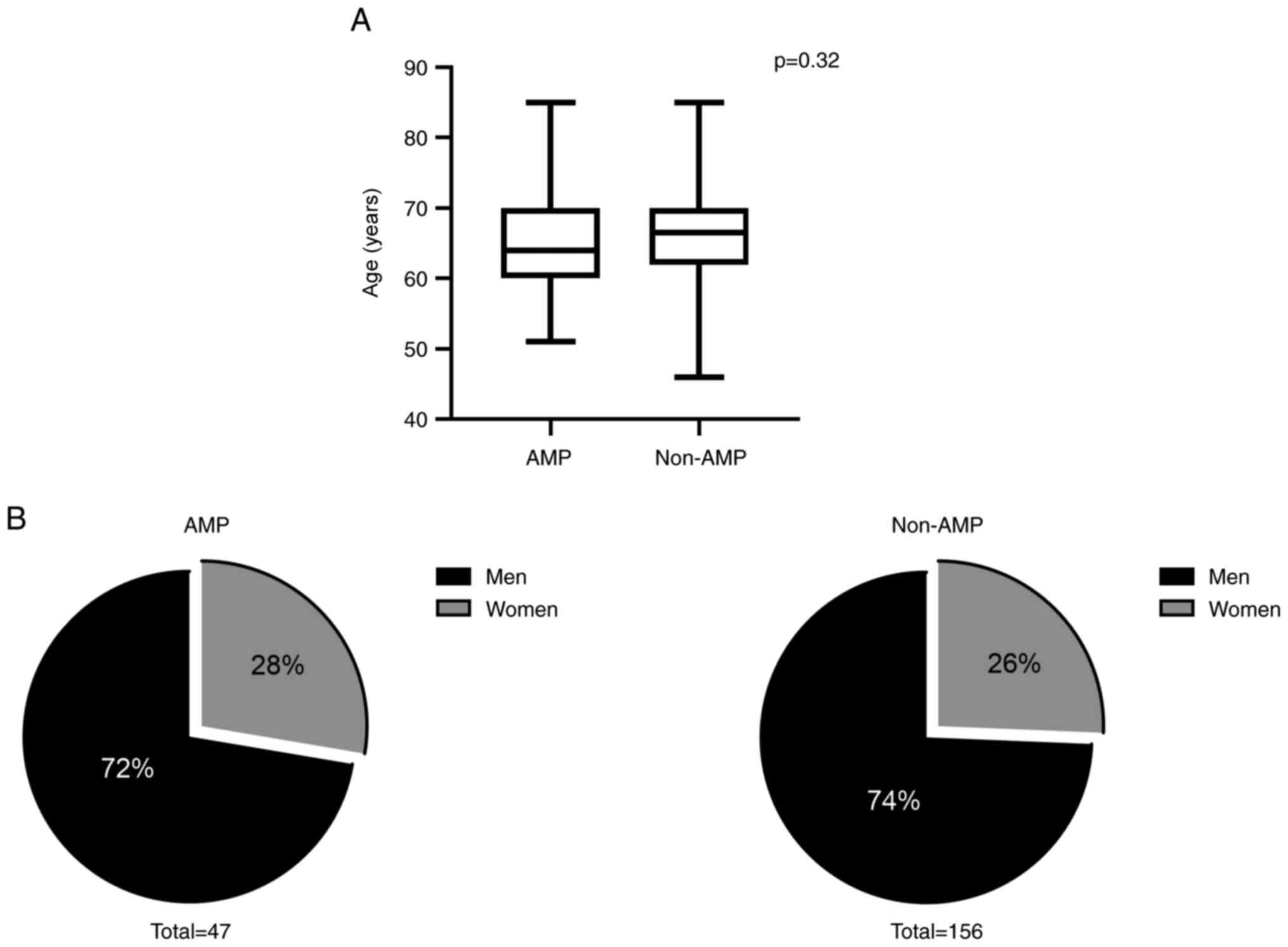
Although the average patient age of the
non-amputation group (66.5 years; 95% CI, 62-70) was higher than
that of the amputation group (64 years; 95% CI, 60-70), the
difference was not statistically significant (P=0.32; Fig. 1A), so age did not influence the
technique of amputation/non-amputation selected.
Regarding the sex distribution, there was no
significant difference between the amputation group, which
consisted of 72% male patients, and the non-amputation group, where
male patients represented 74% of the group (P=0.85; Fig. 1B), suggesting that the sex of the
patient did not influence the choice of surgery.
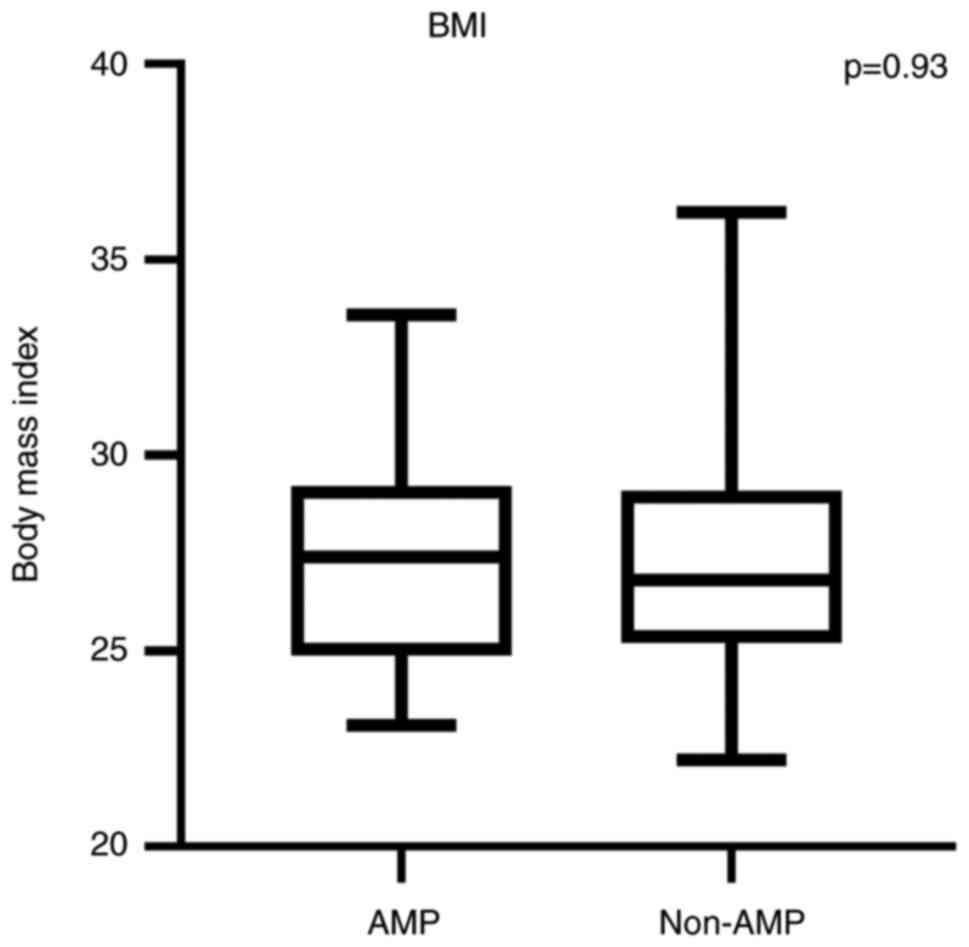
According to the BMI classification, which was
applied to the entire study group, both amputation (27.4; 95% CI,
24.9-29.2) and non-amputation (26.8; 95% CI, 25.2-29.1) group
patients were within the overweight category, with median values of
the BMI ranging between 25 and 30 kg/m2. Although there
was a difference between the two median values, this could not be
considered significant (P=0.93; Fig.
2), meaning that the BMI categorization did not affect the
choice of amputation vs. non-amputation procedure.
Therefore, it can be concluded that demographic
features such as age, sex, and body mass index did not influence
the choice of amputation/non-amputation method.
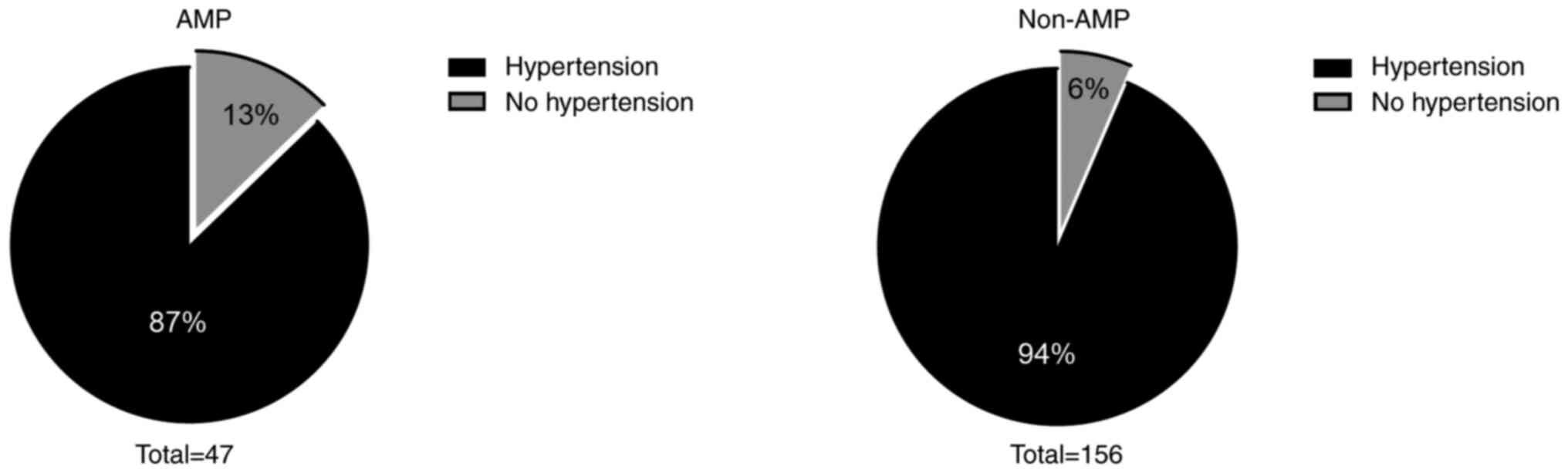
The study also revealed a similar percentage of
patients (53 vs. 58%, respectively; P=0.61) who were either active
smokers or passive smokers in both groups. When taking into
consideration the hypertensive condition of the patients, 87% in
the amputation group were smokers, compared with 94% in the
non-amputation group, though the difference was not significant
(P=0.21; Fig. 3). In conclusion,
smoking status and arterial hypertension did not influence the
choice of procedure.
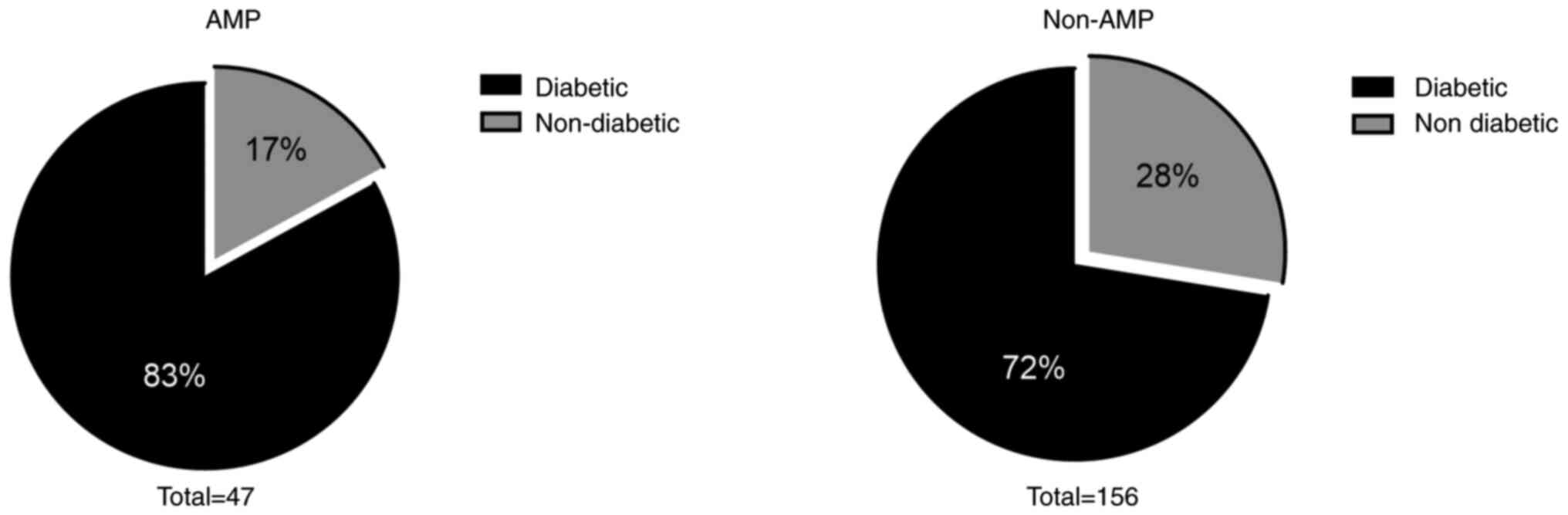
Diabetes mellitus type 2, a risk factor for PAD, was
more frequent in the amputation group than in the non-amputation
group, though once again, the difference was not significant (83%
vs. 72%, respectively; P=0.18; Fig.
4). In terms of other encountered comorbidities, there were no
significant differences between the two groups regarding the
distribution of a history of myocardial infarction or stroke, heart
failure or chronic kidney disease (all P>0.05; Table I). Therefore, prior diabetes and
the aforementioned comorbidities had no effect on the choice of
procedure performed.
 | Table IDistribution of comorbidities in
patients with peripheral artery disease. |
Table I
Distribution of comorbidities in
patients with peripheral artery disease.
| Comorbidity | AMP, % (n=47) | Non-AMP, %
(n=156) | P-value |
|---|
| Previous myocardial
infarction | 25.53 | 23.71 | 0.84 |
| Heart failure | 55.31 | 65.38 | 0.23 |
| Previous stroke | 19.14 | 17.30 | 0.82 |
| Chronic kidney
disease | 8.51 | 16.02 | 0.24 |
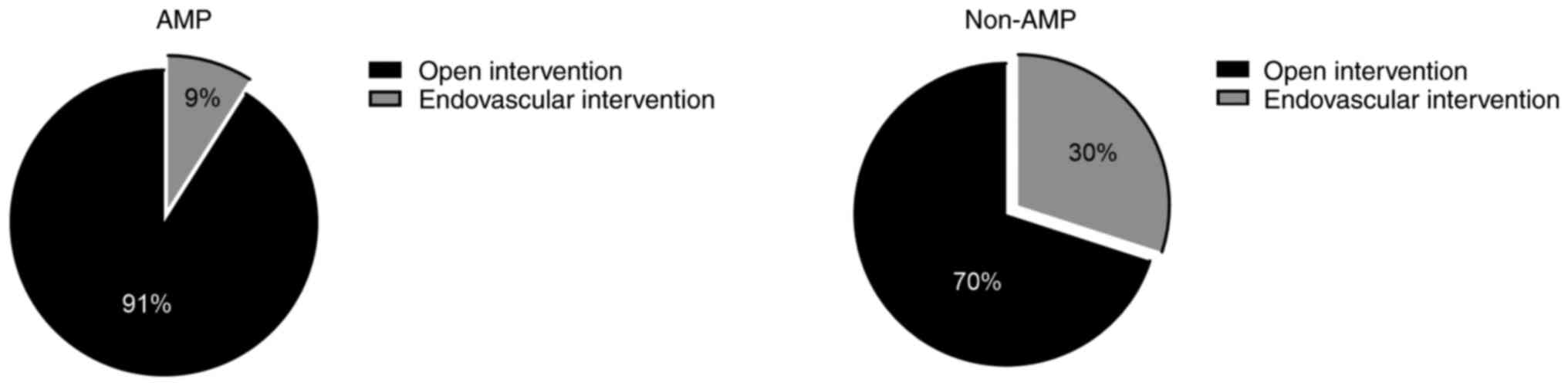
Regarding the type of revascularization procedure,
91% of patients in the amputation group underwent open surgery
(femuro-popliteal bypass and endarterectomy), while 70% of patients
in the non-amputation group underwent the same intervention type
(Fig. 5). Moreover, the percentage
of patients using medication on the administration to the hospital
was similar in both groups (all P>0.05), with >80% of the
patients receiving Cilostazol and >90% using statins and
antiplatelet treatment. On the other hand, Pentoxifylline was
administered to a lower number of patients (Table II).
 | Table IITreatment type of patients with
peripheral artery disease on entry to hospital. |
Table II
Treatment type of patients with
peripheral artery disease on entry to hospital.
| Treatment type | AMP, % (n=47) | Non-AMP, %
(n=156) | P-value |
|---|
| Cilostazol | 82.97 | 80.76 | 0.83 |
| Pentoxifylline | 10.63 | 17.30 | 0.36 |
| Antiplatelet | 100 | 98.07 | >0.99 |
| Anticoagulant | 44.68 | 54.58 | 0.24 |
| Statins | 97.87 | 95.51 | 0.68 |
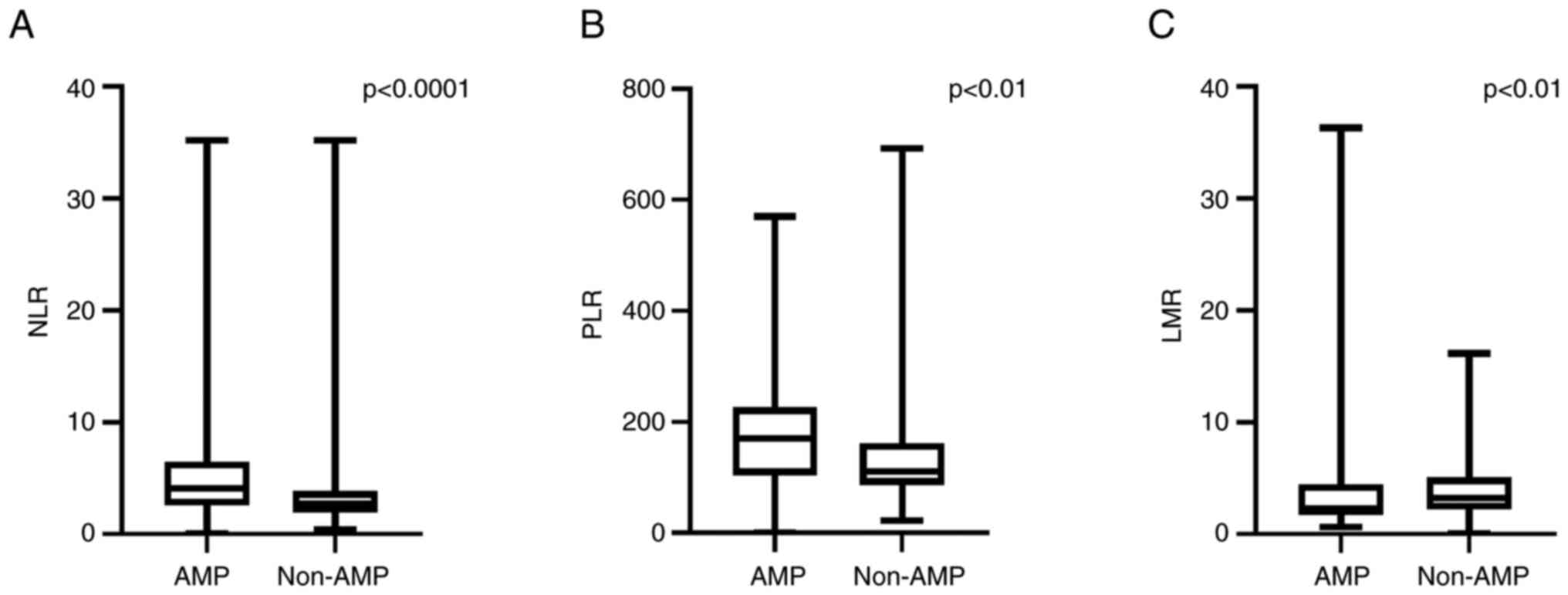
Higher NLR values were observed in patients who
underwent post-operative amputation (4.11; 95% CI, 2.57-6.47) in
comparison to patients who underwent a successful revascularization
procedure (2.68; 95% CI, 1.91-3.85) (P<0.0001; Fig. 6A). Moreover, an increase in PLR in
patients who required amputation compared with those who did not
required amputation after surgical revascularization of the
inferior extremity was observed (170.2; 95% CI, 104.00-226.5 vs.
110.9; 95% CI, 87.31-162.30) (P<0.01: Fig. 6B). By contrast, LMR was reduced in
patients who underwent amputation compared with patients who did
not require amputation (2.12; 95% CI, 1.67-4.40 vs. 3.22;
95% CI 2.22-5.08) (P<0.01; Fig.
6C). Therefore, while the NLR and PLR values were higher in
amputated patients, LMR was lower in these patients.
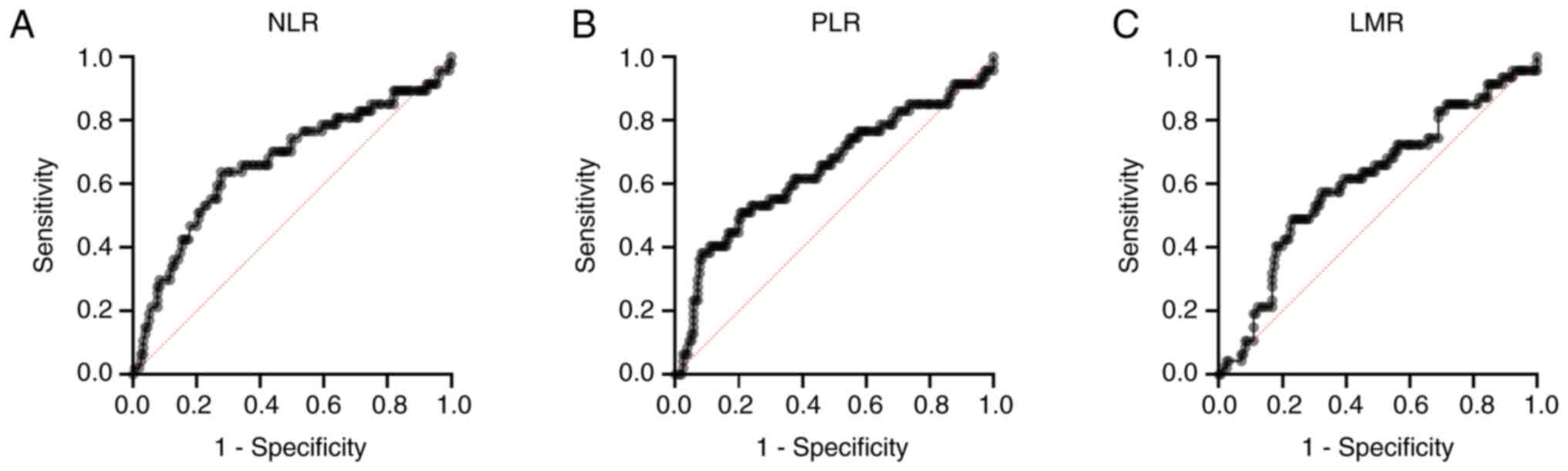
Based on ROC curve analysis, the NLR cut-off value
for predicting amputation requirement in patients with PAD was
3.485 (sensitivity, 60.42%; specificity, 72.44%), the PLR cut-off
value was 152 (sensitivity, 54.17%; specificity 71.79%), and the
LMR cut-off value was 2.55 (sensitivity, 56.25%; specificity
66.88%) (Fig. 7). The study
revealed that none of the three ratios were correlated with
Fontaine class, the number of affected vessels, HDL or LDL levels
(all P>0.05; Table III).
 | Table IIICorrelation between NLR, LMR and PLR,
and Fontaine class, number of affected vessels, LDL and HDL. |
Table III
Correlation between NLR, LMR and PLR,
and Fontaine class, number of affected vessels, LDL and HDL.
| | P-value |
|---|
| Parameter | Fontaine class | Number of affected
vessels | LDL (mg/dl) | HDL (mg/dl) |
|---|
| NLR | 0.91 | 0.91 | 0.79 | 0.23 |
| PLR | 0.53 | 0.49 | 0.17 | 0.55 |
| LMR | 0.74 | 0.25 | 0.54 | 0.17 |
In terms of comorbidities, risk factors, type of
surgery, Fontaine Classification, number of affected vessels, and
history of medication, no statistically significant differences
were observed between the two groups. However, a high NLR and PLR
value, and a lower LMR value, were associated with amputation
post-revascularization as shown in Figs. 6 and 7.
Discussion
Peripheral arterial disease is a public health
problem, affecting many patients through its debilitating nature.
Numerous studies have incriminated the systemic inflammatory
response in the initiation and progression of PAD (7,8).
Given the role of the inflammatory system in the development of
this disease, the present study aimed to investigate the
relationship between PAD and NLR, PLR and LMR, which are considered
markers of inflammation (7-9).
Despite the need for amputation after
revascularization, the primary clinical features of patients in the
amputation and non-amputation groups was similar in the present
study. The non-significant difference in risk factors
(hypertension, diabetes and smoking) for PAD suggests that these
factors did not dictate the rate of amputation in patients who have
undergone revascularization.
More than half of the patients included in the
present study were smokers. Amongst the risk factors, it is
important to highlight the importance of smoking in the development
of PAD, which is noted as one of the most important risk factors in
all studies (10). Even though
different studies approach different stages of smoking state (e.g.,
current, past or never) it has been highlighted that a history of
smoking doubles the risk of PAD compared with non-smokers (10,11).
Diabetes mellitus is also considered to be
associated with a high risk of developing PAD; Murabito et
al (12) revealed an
association between diabetes and age and sex, but not in
multivariate models. Patients with type 2 diabetes mellitus were
found to have a higher risk of PAD development. Via multivariate
analysis, Rhee and Kim (13)
revealed that diabetes mellitus was associated with PAD, whereas
recently diagnosed diabetes mellitus had limited significance, and
TTGO was not associated with PAD.
Arterial hypertension was also amongst the
incriminated risk factors, with a study showing a significant and
independent association between systolic arterial pressure and PAD,
while diastolic pressure was not significantly associated with PAD
(12).
In spite of the necessity for post-operative
amputation, the primary clinical traits of the patients in the
present study were similar in both the amputation and
non-amputation groups. The amputation ratio of the patients who
underwent the revascularization procedure was high, with 23.17% of
the patients requiring postoperative amputation. However, the
non-significant difference of these risk factors for PAD may
suggest that they do not dictate the amputation ratio in patients
who underwent the revascularization procedure. Furthermore, the
association between medication at admission to hospital and PAD
suggests that no previous therapy could reduce amputation risk. The
results of the present study should be carefully interpreted, as in
both studied groups, >80% of the patients were receiving
Cilostazol treatment, >90% were following a statins and
antiplatelet treatment plan, and only Pentoxifylline was
administered to a small number of patients.
Inflammation plays an important role in PAD,
contributing to the onset and progression of atherosclerosis, as
well as to the rupture of atherosclerotic plaques (14,15).
Although inflammation is known to cause changes in the number of
neutrophils, lymphocytes, monocytes and platelets, the significance
of NLR, PLR and LMR is not well understood. Neutrophils release
inflammatory mediators that influence endothelial dysfunction, and
play an important role in increasing platelet count by stimulating
megakaryocytes, creating a prothrombotic status (16). The role of platelets in the
progression of atherosclerosis has been highlighted by
demonstrating an interaction between platelets and endothelial
cells and leukocytes, but also by highlighting the release of
inflammatory substances by platelets, resulting in the adhesion and
migration of monocytes (16,17).
Being involved in immune system regulation, the
lymphocyte plays a crucial role in modulating the inflammatory
response during atherosclerosis (14). Inflammation increases lymphocyte
apoptosis, with low lymphocyte counts reflecting a repressed immune
response, which has been shown to be associated with more severe
clinical outcomes in various cardiovascular diseases (14-16).
Monocytes also play an important role in the formation of atheroma
plaque. Their recruitment and development into macrophages are the
first events in atherosclerosis, which indicates the importance of
inflammation in the onset of the pathology. Being involved in all
stages of atherosclerotic progression, the number of monocytes is a
useful marker for the evaluation of atherosclerosis (16).
Moreover, in the present study, the PLR and LMR were
correlated with PAD. Both NLR and PLR had predictive values
regarding the need for amputation in patients with diabetes, with
higher values in the patients who required amputation than in those
requiring debridement. As far as LMR is concerned, there is still
no sufficient data regarding its correlation with PAD, although in
a study conducted on a representative population from the USA,
monocytes where the only leucocytes to be independently associated
with PAD (9).
Previous studies regarding PAD with chronic
evolution revealed that the NLR is an independent predictor for
lesion complexity, highlighted by the TransAtlantic Inter Society
Consensus-II (TASC-II) (6)
classification, whereas Fontaine classification was not associated
with this report (18). Moreover,
a higher NLR was independently associated with a high probability
of mortality in patients with chronic ischemia of the limbs or
intermittent claudication, in a study conducted on 149 patients
with chronic critical ischemia of the limbs (19).
It should also be highlighted that in the present
study, NLR, PLR and LMR were not correlated with either Fontaine
classification or with the number of affected vessels. Similar to
the findings of the present study, a prospective study conducted on
a smaller number of patients was not able to confirm the
association between NLR and Fontaine classification (6). As a consequence, it should be taken
into account that the NLR was correlated with TASC-II
classification in a previous study (6). The aforementioned data suggest that
the present study cannot entirely indicate the symptomatology or
the number of lesions, but can predict the complexity of the
existing arterial lesions in PAD.
Hirsch et al (20) indicated that 29% of the population
are affected by PAD of the inferior limbs, and the fact that PAD
prevalence raises with age, it is important to take into account
both the need for improved prognostic indicators for patients with
PAD, as well as the use of common inflammatory markers, such as
those deriving from complete blood counts.
The primary limitation of the present retrospective
study is the small amount of patients recruited, which is due to
its nature as a single center study. Although NLR, PLR and LMR
modifications can predict the amputation rate in PAD patients who
underwent a revascularization procedure, the prognostic value of
the study could not be evaluated. In order to confirm these
results, future studies should be conducted with an increased
number of patients. The retrospective projection of the study and
the single blood sample taken for the assessment of NLR, PLR and
LMR, are also considered study limitations.
In conclusion, the present study data confirm that
in patients with PAD, higher NLR and PLR, as well as reduced LMR,
are associated with a greater amputation rate following
revascularization, despite the lack of correlation between these
ratios, Fontaine classification and the number of affected vessels.
The preoperative modifications reported for NLR, PLR and LMR may
predict the requirement for amputation in patients with PAD who
underwent a revascularization procedure.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MC designed the study, participated in the
collection of data, interpretation of data and writing of the
manuscript. ER, RN and IB contributed to the collection of data.
IH, BS, LP and EH participated in statistical analysis and
interpretation of the results. AM, CM, NB and ITB participated in
the study design and writing of the manuscript. All authors read
and approved the final manuscript. All authors confirm the
authenticity all of the raw data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Fowkes FG, Rudan D, Rudan I, Aboyans V,
Denenberg JO, McDermott MM, Norman PE, Sampson UK, Williams LJ,
Mensah GA and Criqui MH: Comparison of global estimates of
prevalence and risk factors for peripheral artery disease in 2000
and 2010: A systematic review and analysis. Lancet. 382:1329–1340.
2013.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Swirski FK and Nahrendorf M: Leukocyte
behavior in atherosclerosis, myocardial infarction, and heart
failure. Science. 339:161–166. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Horne BD, Anderson JL, John JM, Weaver A,
Bair TL, Jensen KR, Renlund DG and Muhlestein JB: Intermountain
Heart Collaborative Study Group. Which white blood cell subtypes
predict increased cardiovascular risk? J Am Coll Cardiol.
45:1638–1643. 2005.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Mureșan AV, Russu E, Arbănași EM, Kaller
R, Hosu I, Arbănași EM and Voidăzan ST: The predictive value of
NLR, MLR, and PLR in the outcome of end-stage kidney disease
patients. Biomedicines. 10(1272)2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Arbănași EM, Mureșan AV, Coșarcă CM,
Kaller R, Bud TI, Hosu I, Voidăzan ST, Arbănași EM and Russu E:
Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio
impact on predicting outcomes in patients with acute limb ischemia.
Life (Basel). 12(822)2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Erturk M, Cakmak HA, Surgit O, Celik O,
Aksu HU, Akgul O, Gurdogan M, Bulut U, Ozalp B, Akbay E and
Yildirim A: Predictive value of elevated neutrophil to lymphocyte
ratio for long-term cardiovascular mortality in peripheral arterial
occlusive disease. J Cardiol. 64:371–376. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Taşoğlu I, Çiçek OF, Lafci G,
Kadiroğullari E, Sert DE, Demir A, Cavus U, Colak N, Songur M and
Hodo B: Usefulness of neutrophil/lymphocyte ratio as a predictor of
amputation after embolectomy for acute limb ischemia. Ann Vasc
Surg. 28:606–613. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Russu E, Mureșan AV, Arbănași EM, Kaller
R, Hosu I, Voidăzan S, Arbănași EM and Coșarcă CM: The predictive
role of NLR and PLR in outcome and patency of lower limb
revascularization in patients with femoropopliteal disease. J Clin
Med. 11(2620)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Nasir K, Guallar E, Navas-Acien A, Criqui
MH and Lima JA: Relationship of monocyte count and peripheral
arterial disease: Results from the national health and nutrition
examination survey 1999-2002. Arterioscler Thromb Vasc Biol.
25:1966–1971. 2005.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Thiruvoipati T, Kielhorn CE and Armstrong
EJ: Peripheral artery disease in patients with diabetes:
Epidemiology, mechanisms, and outcomes. World J Diabetes.
6:961–969. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Anand SS: Smoking: A dual pathogen for
arterial and venous thrombosis. Circulation. 135:17–20.
2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Murabito JM, D'Agostino RB, Silbershatz H
and Wilson WF: Intermittent claudication. A risk profile from the
Framingham heart study. Circulation. 96:44–49. 1997.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Rhee SY and Kim YS: Peripheral arterial
disease in patients with type 2 diabetes mellitus. Diabetes Metab
J. 39:283–290. 2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Unlü Y, Karapolat S, Karaca Y and
Kiziltunç A: Comparison of levels of inflammatory markers and
hemostatic factors in the patients with and without peripheral
arterial disease. Thromb Res. 117:357–364. 2006.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Gawaz M, Langer H and May AE: Platelets in
inflammation and atherogenesis. J Clin Invest. 115:3378–3384.
2005.PubMed/NCBI View
Article : Google Scholar
|
|
16
|
Libby P, Okamoto Y, Rocha VZ and Folco E:
Inflammation in atherosclerosis: Transition from theory to
practice. Circ J. 74:213–220. 2010.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Bakogiannis C, Sachse M, Stamatelopoulos K
and Stellos K: Platelet-derived chemokines in inflammation and
atherosclerosis. Cytokine. 122(154157)2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Demirtas S, Karahan O, Yazici S, Guclu O,
Caliskan A, Yavuz C, Kucuker A and Mavitas B: The relationship
between complete blood count parameters and Fontaine's stages in
patients with peripheral arterial disease. Vascular. 22:427–431.
2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Taşoğlu İ, Sert D, Colak N, Uzun A, Songur
M and Ecevit A: Neutrophil-lymphocyte ratio and the
platelet-lymphocyte ratio predict the limb survival in critical
limb ischemia. Clin Appl Thromb Hemost. 20:645–650. 2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Hirsch AT, Criqui MH, Treat-Jacobson D,
Regensteiner JG, Creager MA, Olin JW, Krook SH, Hunninghake DB,
Comerota AJ, Walsh ME, et al: Peripheral arterial disease
detection, awareness, and treatment in primary care. JAMA.
286:1317–1324. 2001.PubMed/NCBI View Article : Google Scholar
|