Introduction
During tooth development, immature tooth pulp
frequently becomes infected due to trauma, caries and the fracture
of abnormal central cusps. The abnormal central cusp is a common
malformation during tooth development. Previous studies have
reported high frequencies of abnormal central cusps in mandibular
second premolar teeth (1). During
chewing and biting, the abnormal cusp is easily exposed to the pulp
or dentinal tubules due to abrasion or fracture, resulting in pulp
infection, necrosis and symptoms of periapical inflammation
(2).
Due to incomplete root development with wide-open
apical foramen, conventional root canal treatment in immature teeth
with a necrotic pulp is not feasible. Typically, conventional
apexification uses calcium hydroxide as an intracanal medicament to
induce a hard tissue barrier and apical closure (3). An alternative treatment strategy in
such cases is to create an artificial apical plug with the apical
mineral trioxide aggregate (MTA) barrier technique (4). Although these treatments may
eliminate the infection from the periapical tissues, the effects
are limited. As a result, the root cannot continue to develop. In
addition, root fractures are more common due to thin dentinal walls
and an unfavorable crown-to-root ratio (5).
In 2012, the American Association of Endodontics
(AAE) (6) listed regenerative
endodontic procedures (REPs) in the treatment guidelines and
recommended them for treating pulp necrosis of immature teeth
(7). REPs are able to protect the
vitality of undifferentiated mesenchymal stem cells as far as
possible and provide a suitable microenvironment for the
proliferation and differentiation of these stem cells to replace
the dentin, cementum and pulp in the damaged tooth to promote root
development and restore the vitality of the tooth pulp (8).
In recent years, REPs have been highly successful;
however, certain failures have also been reported (9). Regarding alternative interventions
after treatment failure, no reports are currently available, to the
best of our knowledge. The present study reported on the 7-year
follow-up of a 10-year-old male patient with four second premolar
teeth subjected to REPs for periapical periodontitis due to
fracture of abnormal central cusp.
Case report
A 10-year-old male patient presented to the
Pediatric Dentistry Department of the Affiliated Hospital of
Qingdao University (Qingdao, China) in August 2015 with spontaneous
pain in the left mandibular second premolar tooth for one month.
The left maxillofacial area had begun to swell one day
previously.
During the clinical evaluation, an extraoral
examination revealed that the left maxillofacial area had a slight
asymmetry and swelling. Intraoral examinations indicated the
presence of a fractured abnormal central cusp on the left
mandibular second premolar tooth. In addition, mild buccal
vestibular swelling was observed. The abnormal central cusp of
teeth #15, #25 and #45 had different degrees of wear. In the
diagnostic tests, as the apical foramen is not yet formed in
immature teeth, electric pulp testing is not applicable (10). The pulp vitality testing of teeth
was performed using cold pulp testing. This technique is performed
by drying the tooth surface, placing carbon dioxide snow on the
buccal surface of the tested tooth and observing the patient's
response (11). The same method
was used to test normal adjacent teeth for comparison. Tooth #35
had significant pain on percussion and responded negatively to cold
pulp tests using carbon dioxide snow, consistently with the normal
adjacent teeth. At the time of probing the worn central cusps of
the other second premolars, no perforations were found and the
patient exhibited no signs of discomfort. Furthermore, teeth #15,
#25 and #45 exhibited a sensitive positive response to the cold
pulp testing, consistently with the normal teeth. Radiographically,
tooth #35 had an open apex with periapical radiolucency. Pulpal
necrosis with periapical periodontitis was the final diagnosis
based on the clinical presentation. After explaining the treatment
plan, risks and benefits to the parents, they selected REP on tooth
#35. Since teeth #15, #25 and #45 were not clinically symptomatic
and exhibited pulp vitality, a treatment plan using composite resin
to protect the abnormal central cusps was recommended. However, the
patient was too young to cooperate in completing the treatment and
the patient's parents decided to temporarily abandon the preventive
treatment and have regular follow-up observations.
At the first treatment appointment, the root canal
debridement was completed after local anesthesia and rubber dam
isolation. The root canal system was irrigated thoroughly and
slowly with 20 ml of 1.5% sodium hypochlorite solution (Longly
Biotechnology Co., Ltd), followed by 20 ml of sterile saline
solution for 5 min. After irrigation, the root canals were dried
with absorbent paper points (Dayading Co., Ltd) prior to being
filled with creamy calcium hydroxide (Pulpdent Corp.).
Subsequently, Cavit (3M ESPE Dental Products) was used to seal the
access cavity as a temporary restoration and the procedure was
repeated one week later.
At the second appointment, the facial swelling had
disappeared and there was no sensitivity to percussion in the
clinical examination. After isolating with a rubber dam and
removing the temporary sealing material, the interim intracanal
medicament was irrigated with 1.5% sodium hypochlorite (Longly
Biotechnology Co., Ltd) with ultrasonic agitation for 20 sec each
time, 3 times in total (frequency, 28-35 kHz; power, 10 W). A
creamy mix of triple antibiotic paste was prepared by mixing 50 mg
of each of ciprofloxacin (Jiangbo Co., Ltd), metronidazole
(Kangmei, Inc.) and amoxicillin (Hengshan Pharm Co., Ltd) with 1 ml
of saline solution. After irrigating the root canal with saline
solution and drying it with paper points, the triple antibiotic
paste was placed into the root canal. Cavit was used as a temporary
sealant of the access cavity and an appointment was made for a
return visit two weeks later.
At the third appointment, the patient was
asymptomatic. Local anesthesia was achieved using an inferior
alveolar nerve block with 3% mepivacaine plain (SEPTODONT, Inc),
followed by rubber dam isolation. After flushing with 1.5% sodium
hypochlorite with thorough ultrasonic agitation for 20 sec each
time, 3 times in total (ultrasonic frequency, 28-35 kHz; power, 10
W), no significant bleeding or inflammatory exudation were
observed. The filing was then overextended to induce bleeding by
irritating the periapical tissues so that the blood entered the
root canal system. Following the formation of a stable blood clot,
it was covered with a coating of light-cured calcium hydroxide
(Pulpdent Corp.) and composite resin (3M ESPE Dental Products
Division) was used to reconstruct the tooth.
However, the other second premolars developed
symptoms during the REP for tooth #35. The diagnosis was
symptomatic apical periodontitis of varying degrees, accompanied by
the symptoms of infection in the maxillofacial space. After
consultation with the patient's parents, the remaining teeth were
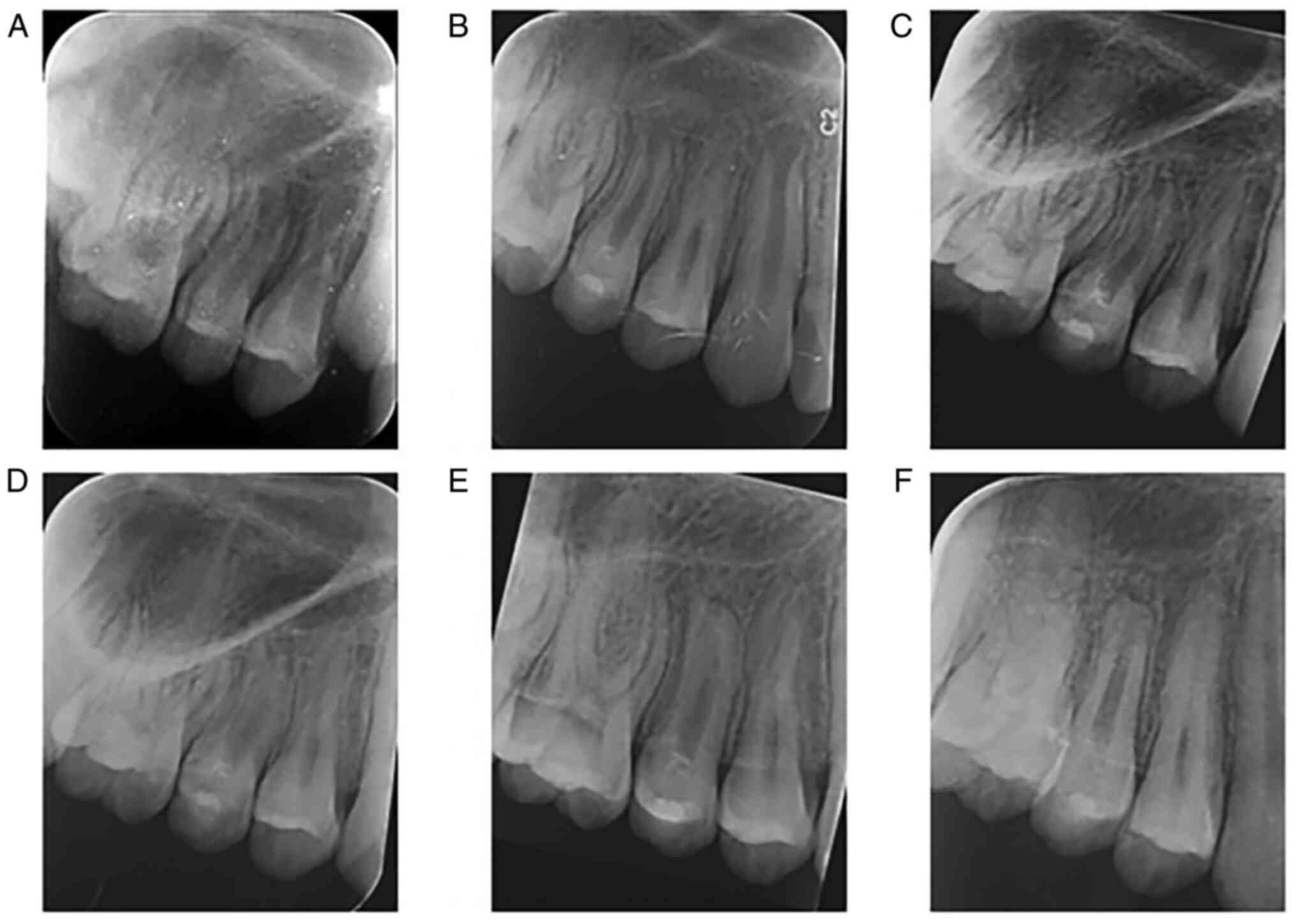
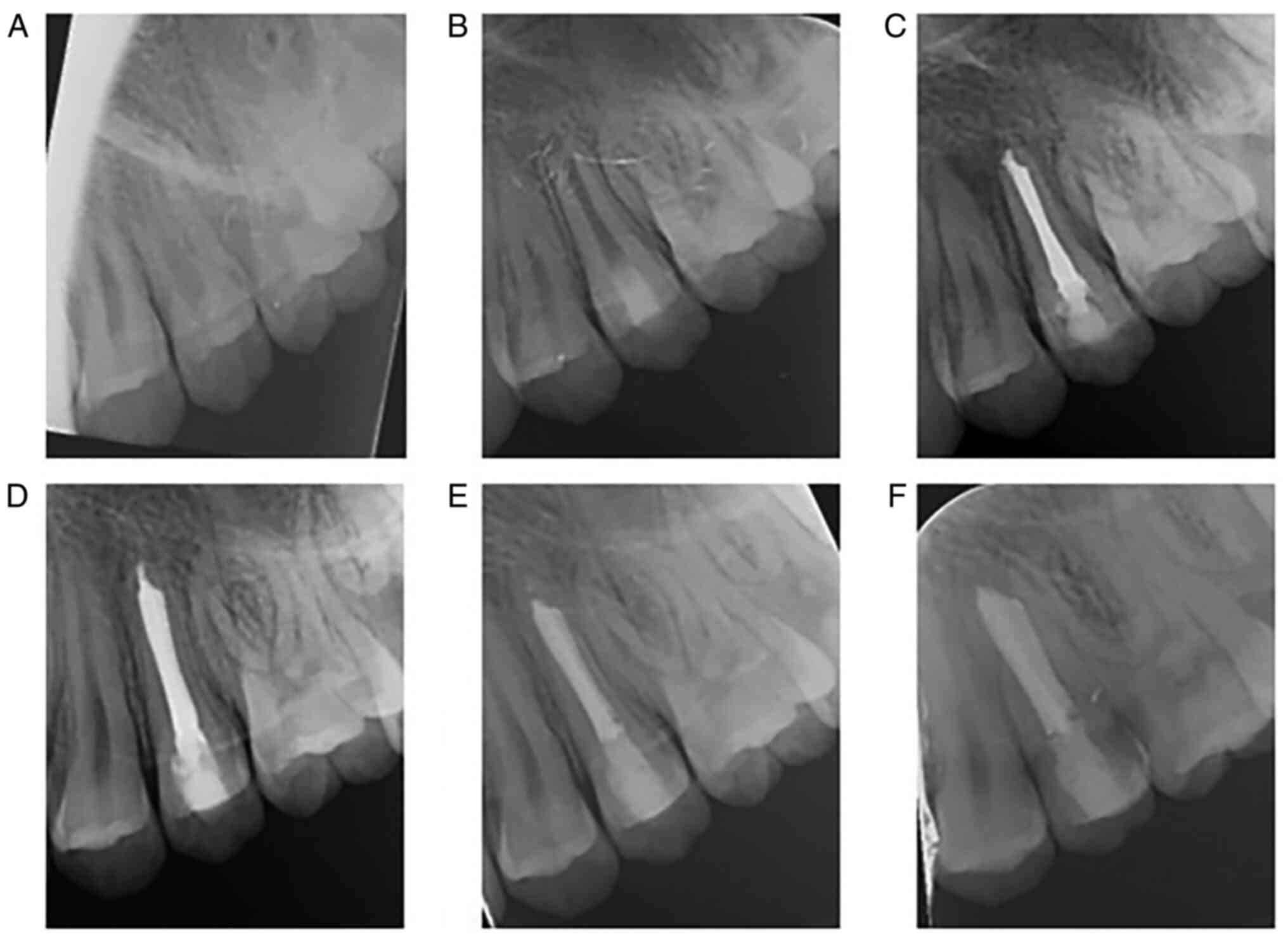
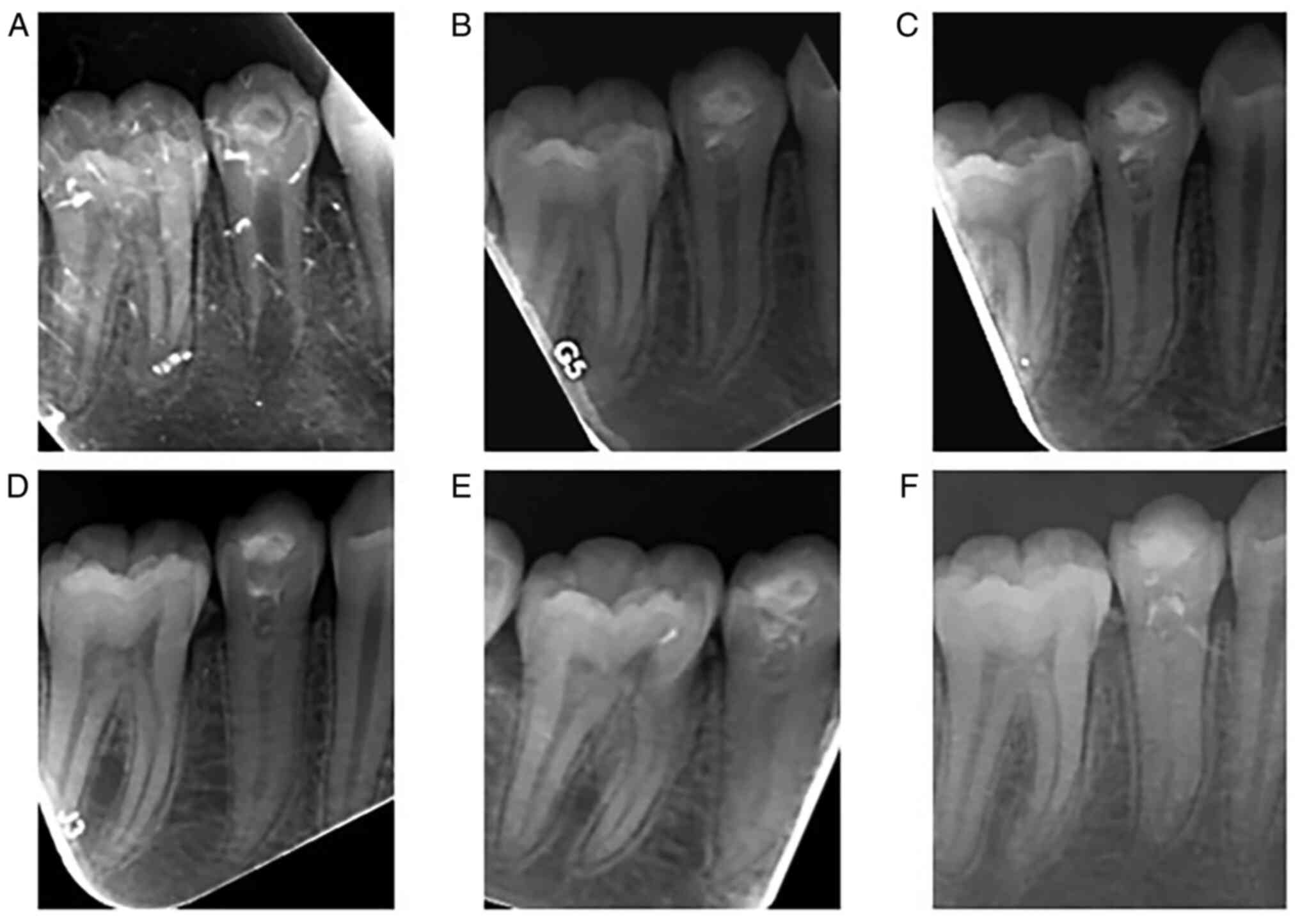
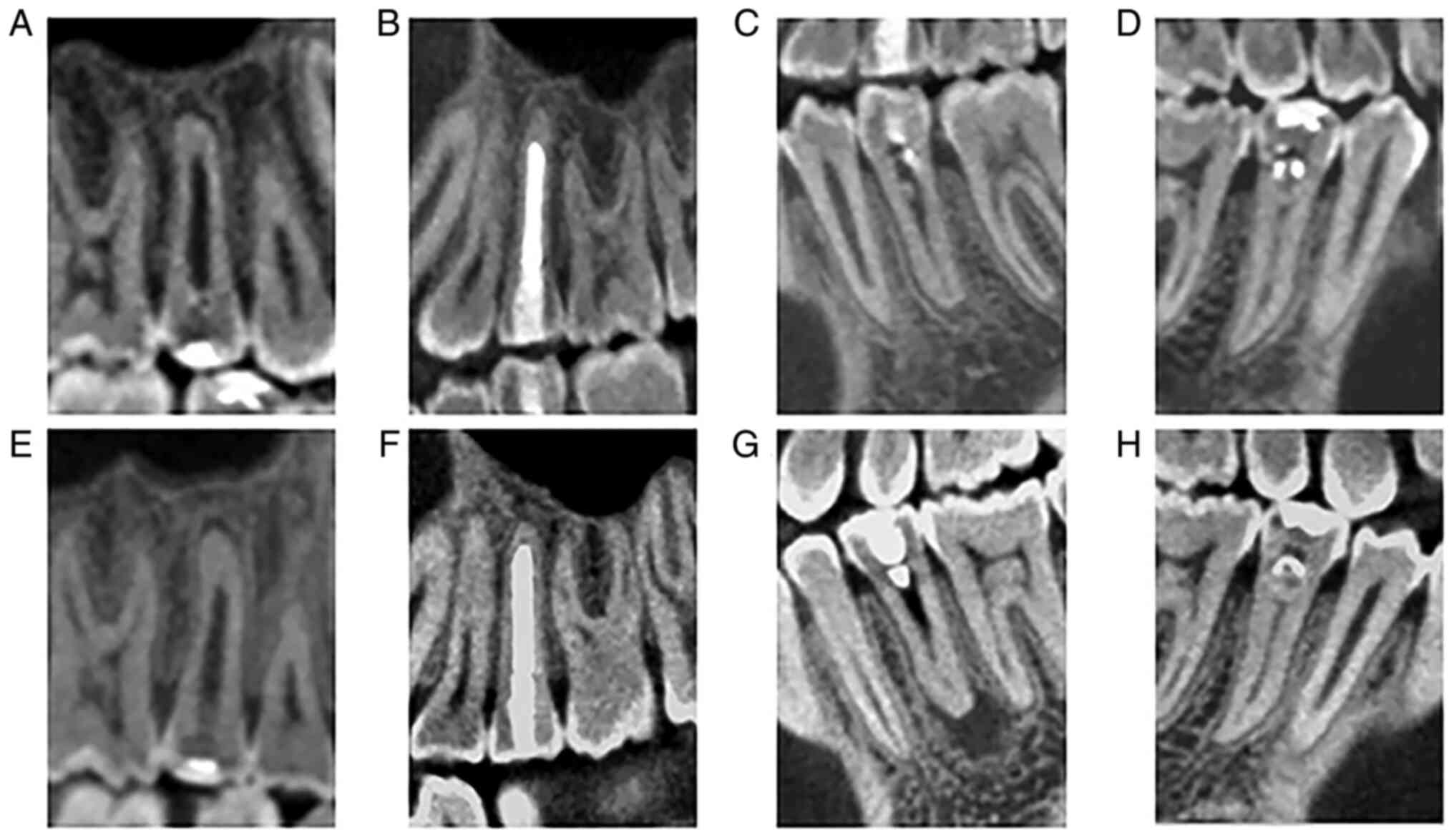
treated with REPs. At each follow-up visit, periapical radiographs
of the affected teeth were acquired (Fig. 1, Fig.
2, Fig. 3 and Fig. 4). All periapical radiographs were
taken using a Minray (Soredex) at 5 mA and 70 kV with an exposure
time of 0.12 sec. The periapical radiographs were calibrated using
Turboreg (Biomedical Imaging Group, Swiss Federal Institute of
Technology) which is a plug-in for Image J software (version 1.41;
National Institutes of Health) to reduce the bias caused by
variations in the projection angle (12). Subsequently, the changes in root
length, apical foramen size and radiographic root area (RRA)
(13) were measured using Image J
software to quantitatively analyze the tooth root development
(Table I, Table II and Table III). The same researcher took all
the measurements and the average of three measurements was used to
report the final value. A 20% cut-off was set as a clinically
meaningful threshold in the radiographic variables (14,15).
 | Table IChanges in the radiographic root area
of the affected tooth before and after regenerative endodontic
procedures (%). |
Table I
Changes in the radiographic root area
of the affected tooth before and after regenerative endodontic
procedures (%).
| Tooth ID | 12 M | 24 M | 36 M | 48 M | 60 M |
|---|
| #15 | 50.65 | 67.98 | 77.12 | 84.11 | 84.66 |
| #25 | 20.10 | 20.61 | 32.70 | 33.30 | 33.38 |
| #35 | 70.67 | 98.02 | 110.48 | 112.88 | 114.04 |
| #45 | 34.99 | 72.42 | 81.36 | 81.59 | 81.20 |
 | Table IIChanges in the root length of the
affected tooth before and after regenerative endodontic procedures
(%). |
Table II
Changes in the root length of the
affected tooth before and after regenerative endodontic procedures
(%).
| Tooth ID | 12 M | 24 M | 36 M | 48 M | 60 M |
|---|
| #15 | 20.98 | 21.65 | 30.92 | 31.67 | 31.14 |
| #25 | 5.96 | 11.20 | 12.35 | 13.92 | 13.84 |
| #35 | 20.12 | 26.34 | 27.10 | 27.98 | 28.15 |
| #45 | 14.89 | 29.88 | 29.91 | 30.11 | 30.75 |
 | Table IIIChanges in the apical foramen of the
affected tooth before and after regenerative endodontic procedures
(%). |
Table III
Changes in the apical foramen of the
affected tooth before and after regenerative endodontic procedures
(%).
| Tooth ID | 12 M | 24 M | 36 M | 48 M | 60 M |
|---|
| #15 | 38.52 | 61.97 | 68.25 | 69.45 | 72.46 |
| #25 | 19.90 | 39.53 | 79.36 | 81.70 | 81.84 |
| #35 | 45.40 | 59.08 | 82.34 | 100 | 100 |
| #45 | 47.50 | 70.00 | 76.64 | 78.32 | 78.56 |
At the one-year follow-up visit, the clinical
symptoms of teeth #15 and #45 had completely disappeared and the
responses to cold pulp testing were negative. The X-ray film
indicated an increase in root length, as well as a narrowing of the
root canal width and the apical foramen, all of which indicated
that the root was still developing (Figs. 1B and 4B). The REPs for teeth #15 and #45 were
effective, and since the roots were not mature, it was decided to
continue follow-up observations of these teeth without further
treatment and consider root canal treatment when root development
was completed. A sinus tract associated with tooth #35 was observed
(Fig. 3B). After consultation with
the parents, the second REPs were performed. In addition to
repeating the previous procedure, as recommended by the AAE
(6), 20 ml of 1.5% sodium
hypochlorite was used for irrigation, followed by 20 ml of 17% EDTA
for 5 min during root canal disinfection. Meanwhile, when the other
teeth were examined, tooth #25 was painful, indicating periapical
inflammation (Fig. 2B).
Apexification with calcium hydroxide was performed to avoid further
extension of periapical inflammation (Fig. 2C). When the apical foramen of tooth
#25 was closed, it was treated with conventional endodontic
treatment, which entailed adequate cleaning, shape and filling.
In the three-year follow-up, the root development of
teeth #15, #25, #35 and #45 was basically complete (Figs. 1D, 2D, 3D
and 4D). At the five-year
follow-up visits, cone-beam computed tomography (CBCT) examinations
were performed to better observe the development of the roots of
the affected teeth (Fig. 5A-D).
All CBCT images were acquired using an iCAT 17-19 (KaVo) set at 5
mA and 120 kV with an exposure time of 14.7 sec with a voxel size
of 0.25 mm. Tooth #35 still had a small periapical radiolucency but
the patient had no other symptoms and was scheduled for regular
visits. The patient was unable to have a follow-up visit in the
sixth year due to being away at school. In the seventh year, the
patient was seen again for an examination of the affected teeth.
The patient was re-examined by CBCT and it was found that the other
affected teeth remained stable with no significant changes;
however, the size of periapical radiolucency of #35 was enlarged
(Fig. 5E-H). Since the root was
developed, prompt root canal treatment was recommended.
Discussion
According to the objectives of REPs described by the
AAE and Geisler (16), the primary
goal is to eliminate the symptoms and promote periapical healing in
the affected tooth. The second goal is to induce root canal wall
thickening and root lengthening. The third goal is to elicit a
positive response to the pulp vitality tests, which indicates pulp
tissue regeneration. In the present case, the primary and secondary
objectives were achieved in teeth #15 and #45. The REPs of teeth
#25 and #35 had unfavorable outcomes. However, a thickening of the
canal walls, apical closure and prolongation of the root was
observed. The European Society of Endodontology (ESE) lists the
above three objectives as the success criteria for REPs (17). Wei et al (18) concluded that the positive responses
of pulp vitality tests after REPs may be a false-positive reaction
of the tissue in the root canal due to the affected vessels and
nerves, necessitating histological studies to confirm pulp tissue
regeneration. Therefore, the evaluation of the success of REPs
according to the AAE is more appropriate for clinical
assessments.
Concerning previous studies on REPs with follow-ups
and qualitative analyses, Chan et al (19) reported an average increase of 8.1%
in root length, a 34% decrease in apical diameter and increase of
11.6% in RRA per tooth during the 30-month follow-up. A previously
published systematic review indicated only 16.1% of root
lengthening, 39.8% of root thickening, a 34.9% increase in RRA and
a 90.7% increase in incidence of apical closure when 20% of the
radiographic changes were used as cut-off points (20). Similar to previous studies,
significant changes were detected. The RRA changes of teeth #15,
#25, #35 and #45 reached a threshold at one year after the
treatment and gradually increased at the follow-ups, remaining
stable after the third year of treatment. However, from the
periapical radiograph, the change in root length and the size of
the apical foramen were most significant three years after
treatment, which remained stable during the later follow-up.
During the follow-up, it was revealed that the REPs
had unfavorable outcomes in teeth #25 and #35. In chronic
inflammatory reactions in the periapical area, it was not possible
to control the inflammatory process in the root canals and the
long-term inflammatory environment led to failure of the REPs. The
main reason for failure in these cases was the bacterial residue
after root canal disinfection and cleaning. In the process of REPs,
bacteria in the root canals are able to survive in locations that
are difficult to reach by disinfecting agents, resisting chemical
disinfection to cause reinfection of the root canal (21). The commonly used clinical root
canal disinfectant is a 1-5 mg/ml antibiotic dressing, as
recommended by the AAE (6). For
the present case, the AAE guidelines were also followed. The triple
antibiotic paste was used as the intra-canal medicament, which is
more effective than calcium hydroxide (22). In addition, in a large number of
previous cases, it was found that triple antibiotics had a better
antibacterial capacity and lower likelihood of root canal
calcification than calcium hydroxide. However, it has the
disadvantages of tooth discoloration, toxicity to stem cells of the
apical papilla (SCAP) and difficulty of removal from the root canal
(23,24). Calcium hydroxide does not have
these disadvantages and is the preferred root canal medicament
recommended by the ESE (17). It
has been suggested that in persistent infections, extended
disinfection times to achieve complete disinfection may lead to
successful treatment outcomes (25). The second REPs of tooth #35 ended
in apical inflammation despite enhanced endodontic disinfection,
which may be attributed to residual bacteria in the root canal that
are resistant to the currently available disinfecting agents.
Therefore, the bacteria in the root canals of teeth with failed
REPs require to be further studied to propose a new disinfection
protocol.
There is still a lack of extensive literature on
cases of failed REP. A current systematic review (26) analyzed 67 cases of REP failure and
indicated that in most cases of failed REP, MTA apical induction
angioplasty had been opted for, while the remaining cases were
treated by conventional endodontic techniques, apical induction
angioplasty or the second REPs. The cases associated with the
second REPs all exhibited enhanced disinfection of the root canal,
either by application of calcium hydroxide in the root canal
(27) or a combination of 2%
chlorhexidine and calcium hydroxide with antimicrobial properties
as an intracanal medicament (28).
Follow-up examinations revealed significant healing of periapical
lesions, apical foramen narrowing and root maturation.
In the present case, different interventions were
selected depending on the root development of teeth #25 and #35
after the failure of the first REPs. The second REP was performed
for tooth #35 with a large root canal apical and thin root canal
wall. Root formation depended on the odontogenic differentiation of
SCAPs induced by Hertwig's epithelial root sheath (HERS). Since the
apex is wider and the number of apical stem cells of the former is
higher, the success rate of REPs is higher for teeth with
undeveloped roots. Therefore, the size of the apical foramen may
affect the postoperative success of the second REPs (29). For cases where the apical foramen
is too small to provide an abundant blood supply, the AAE
recommends the use of platelet-rich plasma, platelet-rich fibrin or
autologous fibrin matrix as an alternative stent scaffold (6). In addition, the survival rate of HERS
and SCAPs is affected by the duration and severity of the
inflammatory reaction in the periapical tissue and the sustained
inflammatory signaling in the root canal may interfere with the
differentiation and maturation of SCAPs, leading to the retardation
of root development (30-32).
The success rate of the second REPs may be lower than that of the
initial attempt due to the risk of damage to the apical papilla and
HERS during the previous sterilization process. To the best of our
knowledge, no previous reports have suggested factors affecting the
success of the second REPs.
Regular follow-up of the pulp after REPs is
essential. In the present case, teeth #25 and #35 exhibited
inflammatory symptoms one to two years after the completion of
treatment. The failure of the second REPs was observed in tooth #35
at the 7-year follow-up. A systematic review reported that the time
from the initiation of REPs to confirmation of failure cases ranged
from 3 weeks to 8 years (26). One
study indicated that the success rate of REPs decreased from 87 to
77% at follow-ups, ranging from 24 to 36 months (33). The success rate of the treatment
gradually decreased over time. Therefore, it is recommended that if
the root is almost or fully developed and resistant to fracture, a
complete root canal treatment may be considered to avoid the
possible residual bacteria in the root canal that may cause a
recurrence of apical inflammation. In addition, although it is
difficult to ask the patient and their parents to attend regular
follow-up sessions, it is necessary to strongly emphasize the
importance of regular visits to discover signs of failure in teeth
that require further treatment.
In summary, REPs are able to promote root
development of in immature teeth, with important applications in
young patients. After the failure of REP, other interventions are
available to promote apical inflammation regression after enhancing
root canal disinfection. Calcium hydroxide apexification or the
second REPs may be alternative interventions for teeth with an
unfavorable outcome after REPs. It is required to further describe
alternative interventions to provide recommendations with precision
and predictability for alternative interventions after failure.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and material
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JYa and XHG performed the literature
search/selection/review, collected clinical information and drafted
the manuscript. RH provided critical pathological reports and
diagnostic consulting. LBX collated the figures and data. LM
conceived the study and revised the manuscript. JYu analysed and
interpreted the data and figures. JYu and LM confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Human Research Ethics
Committee of The Affiliated Hospital of Qingdao University
(approval no. QYFY WZLL 26895).
Patient consent for publication
Written consent for publication of the patient's
data/images in this case report was obtained from a parent of the
patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Levitan ME and Himel VT: Dens evaginatus:
Literature review, pathophysiology, and comprehensive treatment
regimen. J Endod. 32:1–9. 2006.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Cho SY: Dental abscess in a tooth with
intact dens evaginatus. Int J Paediatr Dent. 16:135–138.
2006.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rafter M: Apexification: A review. Dent
Traumatol. 21:1–8. 2005.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kim SG, Malek M, Sigurdsson A, Lin LM and
Kahler B: Regenerative endodontics: A comprehensive review. Int
Endod J. 51:1367–1388. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Nagy MM, Tawfik HE, Hashem AA and
Abu-Seida AM: Regenerative potential of immature permanent teeth
with necrotic pulps after different regenerative protocols. J
Endod. 40:192–198. 2014.PubMed/NCBI View Article : Google Scholar
|
|
6
|
American Association of Endodontists: AAE
Clinical Considerations for a Regenerative Procedures. American
Association of Endodontists, Chicago, IL, 2021. https://www.aae.org/specialty/wp-content/uploads/sites/2/2021/08/Clinical Considerations ApprovedByREC062921.pdf.
Accessed February 8, 2021.
|
|
7
|
Meschi N, Palma PJ and Cabanillas-Balsera
D: Effectiveness of revitalization in treating apical
periodontitis: A systematic review and meta-analysis. Int Endod J:
May 17, 2022 (Epub ahead of print).
|
|
8
|
Hargreaves KM, Diogenes A and Teixeira FB:
Treatment options: Biological basis of regenerative endodontic
procedures. J Endod. 39 (3 Suppl):S30–S43. 2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Torabinejad M, Nosrat A, Verma P and
Udochukwu O: Regenerative endodontic treatment or mineral trioxide
aggregate apical plug in teeth with necrotic pulps and open apices:
A systematic review and meta-analysis. J Endod. 43:1806–1820.
2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Jafarzadeh H and Abbott PV: Review of pulp
sensibility tests. Part II: Electric pulp tests and test cavities.
Int Endod J. 43:945–958. 2010.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Jafarzadeh H and Abbott PV: Review of pulp
sensibility tests. Part I: General information and thermal tests.
Int Endod J. 43:738–762. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Bose R, Nummikoski P and Hargreaves K: A
retrospective evaluation of radiographic outcomes in immature teeth
with necrotic root canal systems treated with regenerative
endodontic procedures. J Endod. 35:1343–1349. 2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Flake NM, Gibbs JL, Diogenes A, Hargreaves
KM and Khan AA: A standardized novel method to measure radiographic
root changes after endodontic therapy in immature teeth. J Endod.
40:46–50. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Alobaid AS, Cortes LM, Lo J, Nguyen TT,
Albert J, Abu-Melha AS, Lin LM and Gibbs JL: Radiographic and
clinical outcomes of the treatment of immature permanent teeth by
revascularization or apexification: A pilot retrospective cohort
study. J Endod. 40:1063–1070. 2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Saoud TM, Zaazou A, Nabil A, Moussa S, Lin
LM and Gibbs JL: Clinical and radiographic outcomes of traumatized
immature permanent necrotic teeth after
revascularization/revitalization therapy. J Endod. 40:1946–1952.
2014.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Geisler TM: Clinical considerations for
regenerative endodontic procedures. Dent Clin North Am. 56:603–626.
2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Galler KM, Krastl G, Simon S, Van Gorp G,
Meschi N, Vahedi B and Lambrechts P: European Society of
Endodontology position statement: Revitalization procedures. Int
Endod J. 49:717–723. 2016.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Wei X, Yang M, Yue L, Huang D, Zhou X,
Wang X, Zhang Q, Qiu L, Huang Z, Wang H, et al: Expert consensus on
regenerative endodontic procedures. Int J Oral Sci.
14(55)2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Chan EK, Desmeules M, Cielecki M, Dabbagh
B and Ferraz Dos Santos B: Longitudinal cohort study of
regenerative endodontic treatment for immature necrotic permanent
teeth. J Endod. 43:395–400. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Ong TK, Lim GS, Singh M and Fial AV:
Quantitative assessment of root development after regenerative
endodontic therapy: A systematic review and meta-analysis. J Endod.
46:1856–1866 e2. 2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ricucci D and Siqueira JF Jr: Fate of the
tissue in lateral canals and apical ramifications in response to
pathologic conditions and treatment procedures. J Endod. 36:1–15.
2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Abbaszadegan A, Dadolahi S, Gholami A,
Moein MR, Hamedani S, Ghasemi Y and Abbott PV: Antimicrobial and
cytotoxic activity of cinnamomum zeylanicum, calcium hydroxide, and
triple antibiotic paste as root canal dressing materials. J Contemp
Dent Pract. 17:105–113. 2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Ruparel NB, Teixeira FB, Ferraz CC and
Diogenes A: Direct effect of intracanal medicaments on survival of
stem cells of the apical papilla. J Endod. 38:1372–1375.
2012.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Montero-Miralles P, Martin-Gonzalez J,
Alonso-Ezpeleta O, Jimenez-Sanchez MC, Velasco-Ortega E and
Segura-Egea JJ: Effectiveness and clinical implications of the use
of topical antibiotics in regenerative endodontic procedures: A
review. Int Endod J. 51:981–988. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Lui JN, Lim WY and Ricucci D: An
Immunofluorescence study to analyze wound healing outcomes of
regenerative endodontics in an immature premolar with chronic
apical abscess. J Endod. 46:627–640. 2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Almutairi W, Yassen GH, Aminoshariae A,
Williams KA and Mickel A: Regenerative endodontics: A systematic
analysis of the failed cases. J Endod. 45:567–577. 2019.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Zizka R, Sedy J and Voborna I: Retreatment
of failed revascularization/revitalization of immature permanent
tooth-A case report. J Clin Exp Dent. 10:e185–e188. 2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Brogni JK, Vitali FC, Cardoso IV, Dos
Santos JD, Prado M, Alves AMH and Duque TM: A second attempt at
pulp revascularisation on an immature traumatised anterior tooth: A
case report with two-year follow-up. Aust Endod J. 47:90–96.
2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Fang Y, Wang X, Zhu J, Su C, Yang Y and
Meng L: Influence of apical diameter on the outcome of regenerative
endodontic treatment in teeth with pulp necrosis: A review. J
Endod. 44:414–431. 2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Chen MY, Chen KL, Chen CA, Tayebaty F,
Rosenberg PA and Lin LM: Responses of immature permanent teeth with
infected necrotic pulp tissue and apical periodontitis/abscess to
revascularization procedures. Int Endod J. 45:294–305.
2012.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Petridis X, van der Sluis LWM, Dijkstra
RJB, Brinker MGL, van der Mei HC and Harmsen MC: Secreted products
of oral bacteria and biofilms impede mineralization of apical
papilla stem cells in TLR-, species-, and culture-dependent
fashion. Sci Rep. 8(12529)2018.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Rakhimova O, Schmidt A, Landstrom M,
Johansson A, Kelk P and Romani Vestman N: Cytokine secretion,
viability, and real-time proliferation of apical-papilla stem cells
upon exposure to oral bacteria. Front Cell Infect Microbiol.
10(620801)2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Casey SM, Fox D, Duong W, Bui N, Latifi N,
Ramesh V, Podborits E, Flake NM, Khan AA and Gibbs JL: Patient
centered outcomes among a cohort receiving regenerative endodontic
procedures or apexification treatments. J Endod. 48:345–354.
2022.PubMed/NCBI View Article : Google Scholar
|