Introduction
Syphilis is a sexually transmitted disease whose
pathogen is Treponema pallidum, a gram-negative spirochete.
The gateway is the tegument or mucous membranes at the level of
minimal lesions (1). From a
pathophysiological point of view, the main process triggered by
Treponema pallidum infection is an obliteration of terminal
arterioles, with inflammatory changes and necrosis. In the central
nervous system, infection causes chronic inflammation of the
meninges and blood arteries, which over time may be complicated by
parenchymal lesions (1).
Early invasion (not necessarily ‘involvement’) of
the central nervous system, is thought to occur in numerous (if not
most) patients infected with syphilis. Thus, it is not surprising
that neurological manifestations of syphilis may occur at any stage
of infection (2). While
neurosyphilis itself is a complication of syphilis, untreated
neurosyphilis may lead to devastating neurological sequelae,
including permanent paralysis, dementia and death. Treatment should
be initiated immediately, and certain complications may be
reversible. The success of therapy has an inverse relationship with
the duration of untreated infection (3). As there is no single highly sensitive
and specific diagnostic test, it is based on clinical
manifestations and cerebrospinal fluid (CSF) abnormalities
(4).
The present article reviews the clinical
manifestations, diagnostic process and first-line treatment of
neurosyphilis, with a focus on the neurological symptoms, important
to the clinician.
Case reports
Case 1
The first case was a 28-year-old male, with no
personal pathological history, who presented at the Neurology
Clinic of ‘Sf. Ap Andrei’ Emergency County Clinical Hospital
(Constanta, Romania) in July 2022 due to Jacksonian epileptic
episodes in the left arm, which had begun ~2 weeks previously, and
the patient was under a treatment recommended by the neurologist
with Levetiracetam (500 mg every 12 h). The patient was
hospitalized at the Neurology Department of the Emergency Clinical
Hospital (Constanta, Romania) for 5 days.
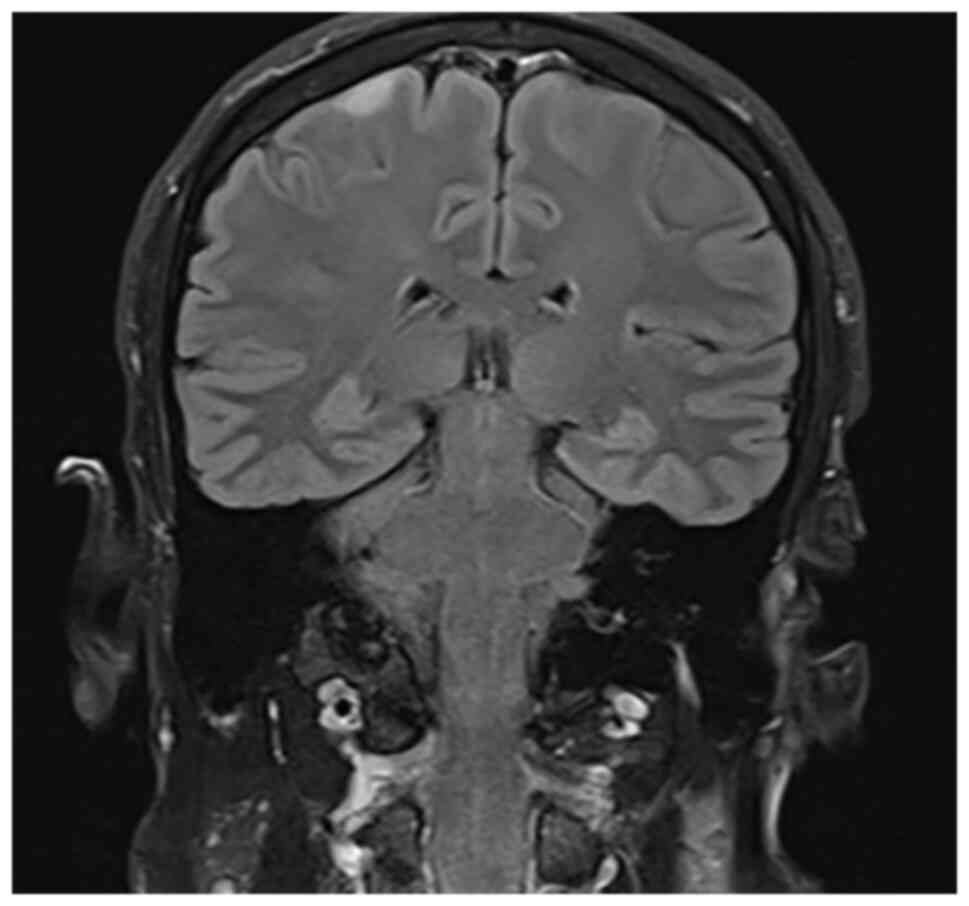
At the time of admission, an objective neurological
examination revealed Jacksonian epileptic seizures in the left
upper limb without any other neurological symptoms. A native brain
MRI and magnetic resonance angiography with venous time were
performed (which indicated a cortical, parietal, well-defined
lesion that had not absorbed the gadolinium-based contrast
substance; (Fig. 1) and an
electroencephalogram was performed (which indicated a microvoltage
pathway of 11.5 c/sec, modulated in spindles, without graphs
suggestive of a lesional pathway). The blood test results are
provided in Table I; the presence
of treponema pallidum antibodies in serum and cerebrospinal fluid
was evident at high levels.
 | Table IBiological data of case no. 1
determined in July 2022. |
Table I
Biological data of case no. 1
determined in July 2022.
| Parameter | Value |
|---|
| RPR (NV:
Negative) | 1.34 |
| Treponema
pallidum antibody in CSF (NV: Negative) | 1/128 |
| Treponema
pallidum antibody in serum (NV: Negative) | 1/2560 |
| Treponema
pallidum antibody IgG in serum (NV: 2.5 units) | 11.3 |
| Treponema
pallidum antibody IgG in CSF (NV: <40 units) | 42.4 |
| Q IgG (NV: <3
units) | 4.4 |
Following the investigations, without having a
precise diagnosis, two days after admission, the neurologist
decided to perform serological tests [Rapid Plasma Reagin (RPR),
quantitative Treponema pallidum antibodies (3) and PCR HIV tests 1+2].
The results revealed positive RPR (1:34) and
anti-Treponema pallidum antibody levels above the normal
limit, which helped to differentiate between syphilis infection and
a false-positive screening test. Considering previous information
lumbar puncture was performed and the CSF was macroscopically
opalescent, slightly hemorrhagic. In the complete CSF examination,
the level of Treponema pallidum antibodies was 1/128, and in
the serum, the value of Treponema pallidum antibodies was
1/2,560 units. The presence of Treponema pallidum antibodies
in serum and CSF was evident at high levels; the values of specific
or major parameters for the diagnosis of neurosyphilis, which were
analyzed from CSF and serum, are listed in Table II.
 | Table IIBiological data of case no. 1
determined in July 2022. |
Table II
Biological data of case no. 1
determined in July 2022.
| Parameter | Value |
|---|
| B12 vitamin, pg/ml
(NV: 197-771) | 282 |
| Thyroid-stimulating
hormone, µUI/ml (NV: 0.27-4.2) | 0.693 |
| Free thyroxine, ng/dl
(NV: 12-22) | 13.2 |
On admission, the differential diagnosis included
tests to exclude vitamin B12 deficiency, hypothyroidism or
hyperthyroidism, and a test to identify mutations associated with
cardiovascular disease-thrombophilia. As presented in Table II, the values for both vitamin B12
and thyroid tests were within normal limits.
The genetic test for thrombophilia identified the
following genotypes: Heterozygous for the G1691A (Leiden) mutation
of factor V and homozygous for the A1298C mutation of
methylenetetrahydrofolate reductase (5). Based on the investigations performed
and the results received during hospitalization, the diagnosis of
neurosyphilis was confirmed.
From the patient's detailed history acquired by
interview, the following information was obtained: Unmarried
patient, currently living alone, affirmative with permanent
protected sexual contact since the beginning of sexual activity,
currently working as a nurse. At the dermatovenerological
consultation, the doctor recommended treatment with Penicillin G
crystalline 4,000,000 IU for 4 h for 14 days, followed by
Benzathine Penicillin 240,000 IU intramuscularly in 3 doses at
5-day intervals.
During hospitalization, no improvement in the
Jacksonian episodes was observed, and accordingly, antiepileptic
medication was increased from 500 mg every 12 h to 1,000 mg every
12 h/day. Following the change in dose, the Jacksonian episodes
completely disappeared. At five days after admission, the patient
was released from the neurology clinic with a recommendation to
continue antiepileptic treatment. The patient was followed in the
private system by the attending doctor.
Case 2
The second case was a 76-year-old male patient,
known to have arterial hypertension grade II with a high risk, who
was admitted to the Neurology Department of the Emergency Clinical
Hospital (Constanta, Romania) due to generalized tonic-clonic
episodes, accompanied by urinary sphincter relaxation and lingual
traumatic mark, occurring at home during the day of presentation.
The patient was admitted to ‘Sf. Ap Andrei’ Emergency County
Clinical Hospital (Constanta, Romania) in February 2020 and was
released after 25 days of hospitalization.
On admission, the neurological examination revealed
that the patient was conscious, psychomotor agitated and had
difficulty mobilizing the right limbs on paresis tests. The native
brain computed tomography (CT) indicated a subacute ischemic lesion
in the left middle cerebral artery territory, supratentorial
sequelae and leukoaraiosis. Biological analysis blood tests
indicated that hyperglycemia and inflammatory syndrome were
present.
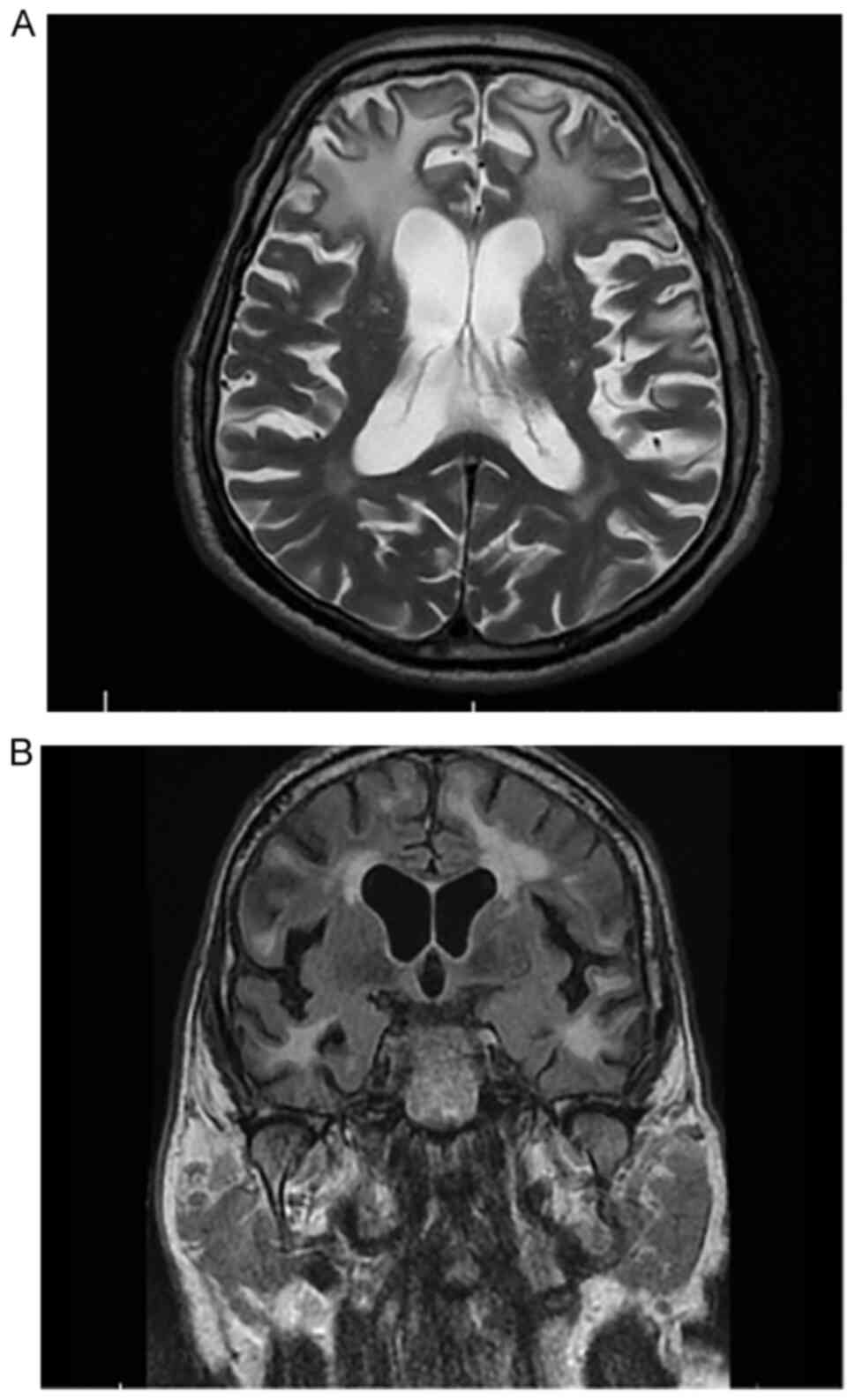
At two days after admission, the patient underwent
brain MRI, which suggested progressive multifocal
leukoencephalopathy (Fig. 2A and
B) and inflammatory mastoid cell
changes.
On day 3 after admission, the neurologist decided to
perform RPR and HIV 1+2 serum testing, which revealed an intensely
positive serum RPR test (Table
III) and negativity for HIV 1+2.
 | Table IIIBiological data of case no. 2,
determined in February 2020. |
Table III
Biological data of case no. 2,
determined in February 2020.
| Parameter | Value |
|---|
| RPR (NV:
Negative) | 1:1 (+++/++++), 1:2
(+++), 1/4 (++) |
| Treponema
pallidum antibody in CSF (NV: Negative) | 1/160 |
| HIV(1+2) (NV:
Negative) | Negative |
After seven days following lumbar puncture,
macroscopically, the CSF was transparent and clear and the presence
of Treponema pallidum antibodies was identified (1/160), as
well as slight glycophoria, slightly increased proteinuria and a
positive RPR test.
Considering the above results, a
dermatovenerological consultation was performed and the doctor
initiated treatment with Penicillin G crystalline 4,000,000 IU at 4
h, for 14 days, followed by Benzatin Penicillin 240,000 IU
intramuscularly in 3 doses at a 5-day interval.
As the patient's cognitive status was unsatisfactory
during hospitalization, a psychological consultation was performed
and the clinical psychologist performed the Mini-Mental State
Examination (MMSE) (6), which had
a score of 11 points and classified the patient in a stage of
severe cognitive deterioration.
At 20 days after admission and after 14 days of
treatment, the evolution was favorable, without the appearance of
other acute events or tonic-clonic episodes. The
dermato-venerologist advised the continuation of the intramuscular
Benzatin Penicillin 240,000 IU, 3 doses at 5-day intervals.
An electroencephalogram was performed, which
indicated a pathway of 67 c/sec in both the anterior and posterior
derivatives. Temporal flattened pathway (lesional), Theta band
pathway (lesional), slow alpha and no epileptiform elements were
observed during recording. On the day of release, the patient had
neurologically improved, was cooperative and temporo-spatially
disoriented, without neck roll and without motor deficits. The
patient was followed in the private system by the attending
doctor.
Case 3
The third patient was a 51-year-old male, navigator,
known to have recurrent transient aphasic episodes who presented to
the ‘Sf. Ap Andrei’ Emergency County Clinical Hospital (Constanta,
Romania) in April 2013 for sudden established speech difficulty
without other signs of neurological impairment at the time of
admission. After a native and contrast CT scan (the result of which
was within age limits), an electroencephalogram (without
epileptiform graphoelements) and cerebrovascular treatment, the
speech disorder improved and the patient was discharged with
recommendations of medication with antiplatelet (100 mg, 1 cp/day),
anticonvulsant (200 mg, 1 cp/day) and antihypertensive (10 mg, 1
cp/day) drugs. The patient was admitted to ‘Sf. Ap Andrei’
Emergency County Clinical Hospital from Constanta, Romania on
19-04-2014 and discharged on 05-05-2014.
At six months after the initial presentation, the
patient returned to the hospital due to left leg motor weakness.
Neurological objective examination indicated that the patient was
conscious, uncooperative, head and eyeballs deviated to the right
and the patient exhibited left central facial paresis, left
hemiplegia (left upper limb: 0/5; left lower limb, 0/5) and
bilateral indifferent plantar cutaneous reflex; these symptoms
completely remitted 24 h after admission. At the time of admission,
a CT scan excluded acute diseases or sequelae. From a biological
perspective, since the hemolucogram indicated significant
leukocytosis, antibiotic therapy with Cephalosporin III, 1 g every
12 h for 7 days, was initiated.
During admission, examination of the neurological
condition revealed tetraataxia, intermediate poorly reactive pupils
and mild anisocoria more in the right eye than in the left. As the
neurologist did not have a definite diagnosis after the
investigations, the patient was serologically tested for HIV 1+2,
hepatitis B surface antigen and anti-HCV, all with negative
results, and syphilis (RPR positive). Later, a lumbar puncture was
performed, and the following was detected: Clear, colorless fluid,
increased proteinuria (950 mg/l); 52 elements/mmc (96%
mononucleated, 4% polymorphonucleated) and positive CSF (RPR
++++).
A dermato-venerological consultation followed, based
on which treatment with crystalline Penicillin G was initiated at
4,000,000 IU/4 h, for 14 days, followed by Benzathine Penicillin
240,000 IU intramuscular, 3 doses at 5-day intervals. At 16 days
after admission, the patient was released. At the time of
neurological re-examination, the clinical status had improved.
Therapeutic management at discharge included anticonvulsant drugs
(200 mg; 1/2 cp in the morning, 1/2 cp at lunch and 1 cp in the
evening), with the recommendation to prohibit the consumption of
alcohol, coffee and cola, working at height and driving.
In the same year, six months after being diagnosed
with neurosyphilis, the patient presented at the hospital with mild
cognitive impairment. The clinical neurological examination
revealed the following: Mild anisocoria (right eye > left eye),
negative paresis tests, positive non-systematized Romberg, globally
exacerbated osteotendinous reflexes, except for the Achilles
reflexes, which were diminished bilaterally, bilateral flexion
plantar cubitus reflex, mild dysmetria on the bilateral knee
flexion test and painful distal tactile hypoesthesia.
The MMSE was also performed with a result of 22
points, representing mild cognitive impairment, which was the
reason for the addition of Pramiracetam (600 mg, 1 cp every 12 h)
to the treatment. In April 2016, May 2017 and May 2020, tests for
RPR and Treponema pallidum antibodies were repeated, both
with positive results. In Table
IV, the evolution of the two infection indicators over the
years is presented. The condition affected the patient's ability to
continue performing his job and in 2018 he retired.
 | Table IVBiological data of case no. 3. |
Table IV
Biological data of case no. 3.
| Parameter (NV) | April 2016 | May 2017 | May 2020 |
|---|
| RPR (NV:
Negative) | 1:1(++++); 1:2(+++);
1:4(++); 1:8(+); 1:16(+/-) | 1:1(++); 1:2(++);
1:4(+); 1:8(+/-) | 1:1(++); 1:2(+);
1:4(+/-) |
| Treponema pallidum
antibody in serum (NV: Negative) | 1:80(++++);
1:160(+++); 1:320(++) | 1:80(++++);
1:160(++++); 1:320(++++) | 1:80(++++);
1:160(++++); 1:320(++++) |
At the last neurological evaluation, in July 2021,
the patient's general condition was unchanged from the previous
examination, with no changes in the biological parameters examined.
The recommended treatment was valproic acid 500 mg per day in a
single dose, carbamazepine 200 mg per day in a single dose, to
which lorazepam 1 mg and 1 cp per day was added, as the patient had
experienced periods of anxiety, which started six years previously
but had progressed recently prior to the presentation at the
hospital. The patient was followed up in the private system by the
attending doctor.
Discussion
As the clinical diagnosis of neurosyphilis remains
far from optimal, the current study presented cases of patients
diagnosed with neurosyphilis and briefly summarized the
neurological manifestations that may occur during the course of the
disease, which may help to diagnose the condition more rapidly.
Neurosyphilis is one of the most complex manifestations to diagnose
in patients without a known history of syphilis infection, due to
its broad possible presentations. The most common manifestations of
neurosyphilis include tabes dorsalis, generalized paralysis and
meningo-vascular neurosyphilis (7,8).
Tabes dorsalis occurs 20-30 years after infection
and consists of demyelination of the posterior medullary cords and
posterior spinal nerve roots (1).
Generalized paralysis (paralytic dementia) occurs 20-30 years after
infection and consists of a chronic progressive
meningo-encephalitis leading to the destruction of the cerebral
cortex in the frontal and temporal lobes (1). Meningo-vascular syphilis usually
occurs 5-12 years after infection and predominantly manifests as
microangiopathy, with fibroblastic proliferation of the intima,
thinning of the media and lymphocytic infiltration, with narrowing
or obliteration of the vascular lumen. It manifests as ischemic
strokes in the territory of the middle cerebral artery or branches
of the basilar trunk (1).
The topic of neurosyphilis, particularly in the
geriatric population, has been widely neglected in the literature
in recent years. This is also due to the widespread use of
antibiotics, which may ultimately prevent the occurrence of
syphilis (9). The first-line
treatment has been Penicillin G since 1943, which is when it was
first used to treat syphilis, and it is the only recommended
antibacterial drug for neurosyphilis (10).
The first case described in the present study was a
28-year-old male patient. Neurological manifestations were limited
to Jacksonian epileptic episodes, with sudden onset, without any
other subjective complaint. Based on the clinical manifestations,
for this particular case, it was recommended to perform both native
brain MRI and brain MR angiography with venous time. Based on this,
the diagnosis of superior sagittal sinus thrombosis was considered.
As the patient's condition changed during treatment with
antibiotics and levetiracetam for seizures, the patient's prognosis
is good. The neurologist recommended clinical and serological
monitoring at 3, 6, 9, 12, 18 and 24 months after treatment.
The second case presented was that of a 76-year-old
male with a clinical neurological condition, including severe
cognitive impairment, which had evolved rapidly at the time of
discharge from the Neurology Department of the Clinical Hospital
(Constanta, Romania), with a score of 11 points on the MMSE. Over
time, one of the complications that patients with neurosyphilis may
develop are psychiatric manifestations represented by manic
episodes, depression or psychosis, in addition to the appearance or
worsening of memory and judgment deficits, evolving towards severe
dementia (3,6). Cases of syphilitic dementia are still
reported in modern times.
The prognosis of the case remains uncertain because,
considering the advanced cognitive impairment but also the
conditions associated with neurosyphilis (type II diabetes mellitus
newly discovered and under treatment with oral antidiabetics,
hypertension, superficial thrombophlebitis in the internal
saphenous vein of the right leg), it is associated with a risk of
developing significant complications that may lead to death. The
third case of the present study was a 51-year-old patient whose
diagnosis was challenging due to the non-specific clinical signs.
From the first months after diagnosis, cognitive decline started to
increase. In 2014, the cognitive impairment was mild (with an MMSE
score of 22 points) and in 2016, two years after diagnosis, the
cognitive impairment had progressed slightly, with an MMSE score of
19 points.
All of the patients of the current study received
standard treatment with antibiotics from the penicillin class.
Neurosyphilis should be part of the differential diagnosis of every
patient with impaired cognition and behavioral disorders.
Neuropsychological assessments and CSF examinations are useful
tools for measuring cognitive decline and response to treatment
during follow-up (11). Regarding
the third clinical case presented, who exhibited mild deterioration
of cognition, considering the evolution of the patient from
diagnosis to present, the prognosis is favorable, and the patient
is in therapy (11).
An Estonian study by Liis et al (12) described the diagnosis of
neurosyphilis. Given that syphilis is easy to diagnose and treat at
this time, it should be considered and tested in patients with
cognitive and movement disorders. A 42-year-old male presented to
the Neurology clinic due to cognitive decline that had occurred ~1
year prior to presentation, hallucinations (rare), periods of
confusion (transient), gait disturbances and involuntary movements.
Focal slowing and epileptiform discharge in the right
frontotemporal regions were described electroencephalographically
(10). HIV 1 and 2 antibodies were
negative, but the RPR test as well as the T. pallidum
hemagglutination assay (TPHA) were positive in serum (RPR, 1:32;
TPHA, 1:520) as well as in CSF (RPR, 1:8; TPHA, 1:640). Based on
clinical imaging and laboratory data, neurosyphilis was diagnosed
and penicillin treatment was initiated. At follow-up, 6 months
later, the patient had mild dementia (MMSE, 25/30), but the
myoclonus and extrapyramidal symptoms had disappeared. Both the RPR
(1:2) and TPHA markers in the serum and CSF that were mentioned
above had turned negative.
What makes the case reported by Liis et al
(12) and the cases presented
above similar is the cognitive impairment. In the case of the
76-year-old patient of the present study, cognitive decline was
clearly progressive during hospitalization, with an MMSE score of
11 points at discharge. For the third patient, a 51-year-old male,
the impairment was not as evident at the time of the first
admission to the neurology department, but later, 6 months after
the diagnosis of neurosyphilis, it was possible to observe minimal
cognitive decline, with slight progression in the following
years.
In conclusion, neurosyphilis may occur at any time
in the course of syphilis (13).
The diagnosis is based on clinical manifestations but particularly
on the paraclinical investigations that may be performed, including
imaging and analysis of cerebrospinal fluid. Nowadays, it is
important to remember that syphilis, and particularly
neurosyphilis, in its early stages may be overlooked and left
untreated; it may lead to changes in the neurological status of
patients that are irreversible and have an unfavorable therapeutic
response. As showcased by the three clinical cases, diagnosed at
different time-points (case 1 in 2022, case 2 in 2020 and case 3 in
2014) and with non-specific clinical presentation, Penicillin G at
high doses remains the first choice of therapy, to which
symptomatic medication may be added.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AA, RACB and LFM conceived and designed the study.
AZS performed the literature research. AA, RACB, LFM, AZS, DM, ACC
and SDA were involved in the interpretation of the results and in
the writing of the manuscript. AA, RACB, AZS and LFM checked and
confirm the authenticity of the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The current study was approved by the Ethics
Committee of the Constanta Clinical Hospital (Constanta, Romania;
approval no. 21/26.09.2022).
Patient consent for publication
All of the patients provided written informed
consent for publication of their data and images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Liao H, Zhang Y and Yue W: Case report: A
case report of neurosyphilis mimicking limbic encephalitis. Front
Neurol. 13(862175)2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
US Department of Health Human Services and
Centers for Disease Cont And Prevention: Sexually transmitted
disease surveillance 2012. Createspace Independent Publishing
Platform, North Charleston, SC, 2014.
|
|
3
|
Ropper AH: Neurosyphilis. N Engl J Med.
381:1358–1363. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Berger JR and Dean D: Neurosyphilis. Handb
Clin Neurol. 121:1461–1472. 2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Favaloro EJ: Genetic testing for
thrombophilia-related genes: Observations of testing patterns for
factor V Leiden (G1691A) and prothrombin gene ‘mutation’ (G20210A).
Semin Thromb Hemost. 45:730–742. 2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Trivedi D: Cochrane review summary:
Mini-mental state examination (MMSE) for the detection of dementia
in clinically unevaluated people aged 65 and over in community and
primary care populations. Prim Health Care Res Dev. 18:527–528.
2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Read PJ and Donovan B: Clinical aspects of
adult syphilis. Intern Med J. 42:614–620. 2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Shi M, Peng RR, Gao Z, Zhang S, Lu H, Guan
Z, Gao Y, Wang C and Zhou P: Risk profiles of neurosyphilis in
HIV-negative patients with primary, secondary and latent syphilis:
Implications for clinical intervention. J Eur Acad Dermatol
Venereol. 30:659–666. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Zheng D, Zhou D, Zhao Z, Liu Z, Xiao S,
Xing Y, Suo WZ and Liu J: The clinical presentation and imaging
manifestation of psychosis and dementia in general paresis: A
retrospective study of 116 cases. J Neuropsychiatry Clin Neurosci.
23:300–307. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Buitrago-Garcia D, Martí-Carvajal AJ,
Jimenez A, Conterno LO and Pardo R: Antibiotic therapy for adults
with neurosyphilis. Cochrane Libr. 5(CD011399)2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mehrabian S, Raycheva MR, Petrova EP,
Tsankov NK and Traykov LD: Neurosyphilis presenting with dementia,
chronic chorioretinitis and adverse reactions to treatment: A case
report. Cases J. 2(8334)2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Liis S, Mark B and Pille T: Neurosyphilis
as a great imitator: A case report. BMC Res Notes.
9(372)2016.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Tiecco G, Degli Antoni M, Storti S,
Marchese V, Focà E, Torti C, Castelli F and Quiros-Roldan E: A 2021
update on syphilis: Taking stock from pathogenesis to vaccines.
Pathogens. 10(1364)2021.PubMed/NCBI View Article : Google Scholar
|