Introduction
The advancement of technology has led to the
development of various new stents for intracranial aneurysms (IA)
treatment. The Neuroform Atlas® stent (Stryker
Neurovascular, Fremont, CA, USA) is one of the most recently
developed laser-cut stents with an open-cell strut, and it is the
successor of the Neuroform EZ® stent (Stryker
Neurovascular). Compared with its former generation, it has the
significant improvements of a lower-profile delivery system via a
0.42-mm or 0.43-mm inner diameter microcatheter, enhanced
trackability, smaller cell size, and increased conformability to
vessel walls (1). Recently
published prospective trials showed the efficacy and safety of
Neuroform Atlas® stents in treating IA with an excellent
rate of procedure success and acceptable procedure-related
complications (2-4).
Among the procedural difficulties, several cases have been reported
where stent migration or stent deployment in unexpected landing
sites occurred during the procedure (2,5-14).
Fracture and deformation of intracranial stents have rarely been
reported. The authors report a stretched and partially fractured
Neuroform Atlas® stent due to unexpected partial
withdrawal of the stent-engaged microcatheter during deployment for
coil embolization of an unruptured intracranial aneurysm.
Case report
A 42-year-old female patient had been diagnosed with
an unruptured IA at the paraclinoid segment of the left internal
carotid artery (ICA) on magnetic resonance angiography (MRA) after
her health check-up. She had no neurological symptoms and signs
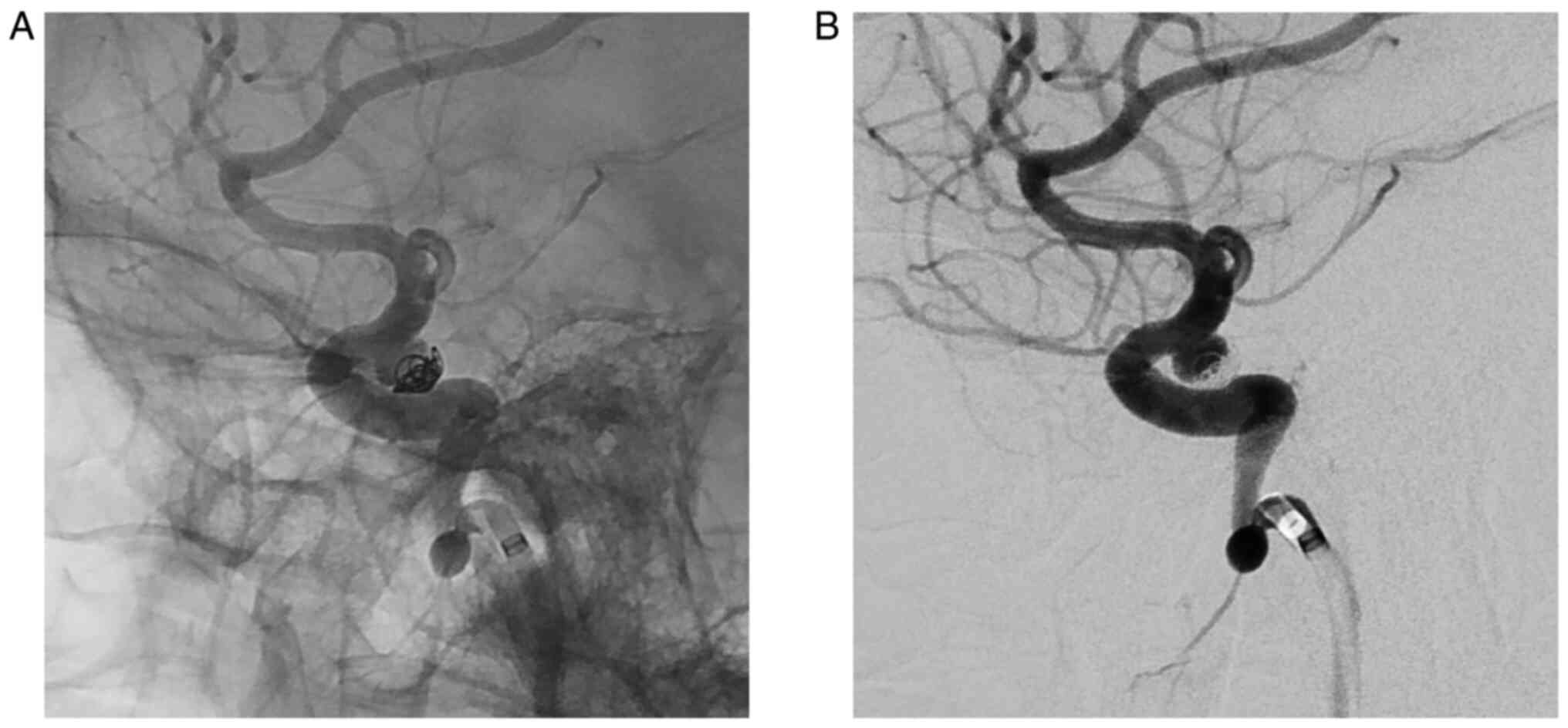
without a history of underlying disease or smoking. On digital
subtraction angiography, the location of the IA was the left
superior hypophyseal artery with a posterior-medial direction. The
sizes of the IA were 4.7 mm in maximal diameter and 2.4 mm in neck
diameter. She had undergone coil embolization for the IA on April
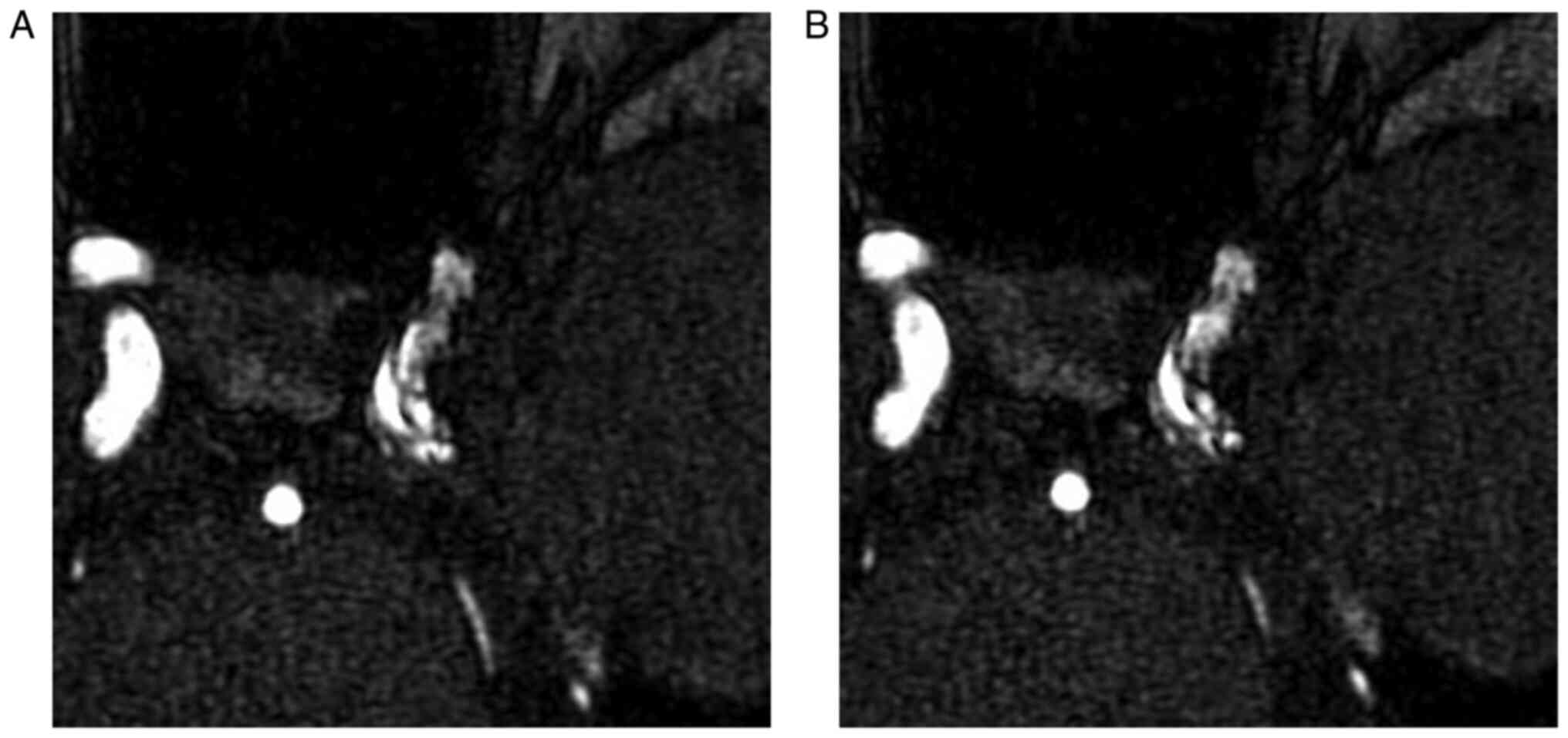
2015. During five years of the follow-up period, we detected the
major recurrence of the IA on MRA and digital subtraction
angiography (Fig. 1). Because the
surgical access and aneurysm exposure for aneurysm clipping was not
easy, we decided to perform a second coil embolization for the
recurred IA using the stent-assisted catheter jailing technique due
to the wide-necked aneurysm, the angle of the parent artery
curvature, and to prevent recurrence.
The endovascular procedure was performed under
general anesthesia using a biplane digital subtraction angiography
suite (Artis Q, Siemens Healthineers AG, Erlangen, Germany).
Aspirin (100 mg/day) and clopidogrel (75 mg/day) were administered
for 14 days before treatment. Anticoagulation using intravenous
heparinization was used to maintain an activated clotting time of
250-300 sec during the procedure. After positioning a 6F-guiding
catheter (Envoy® DA, Codman Neuro, Raynham, MA, USA),
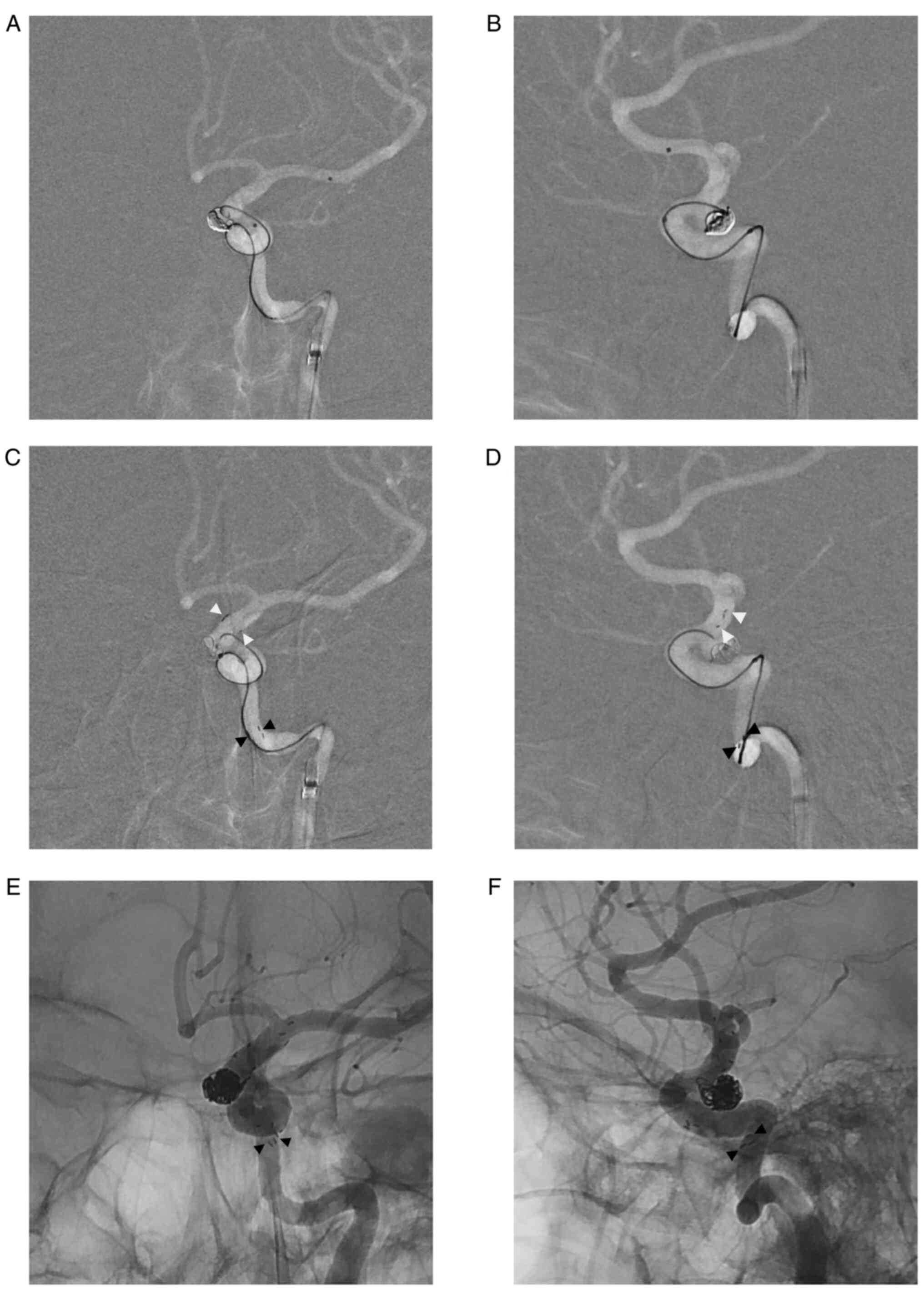
two 0.42-mm microcatheters (Excelsior®
SL-10®, Stryker Neurovascular) were navigated to the
aneurysm sac (for aneurysm selection) and the proximal left middle
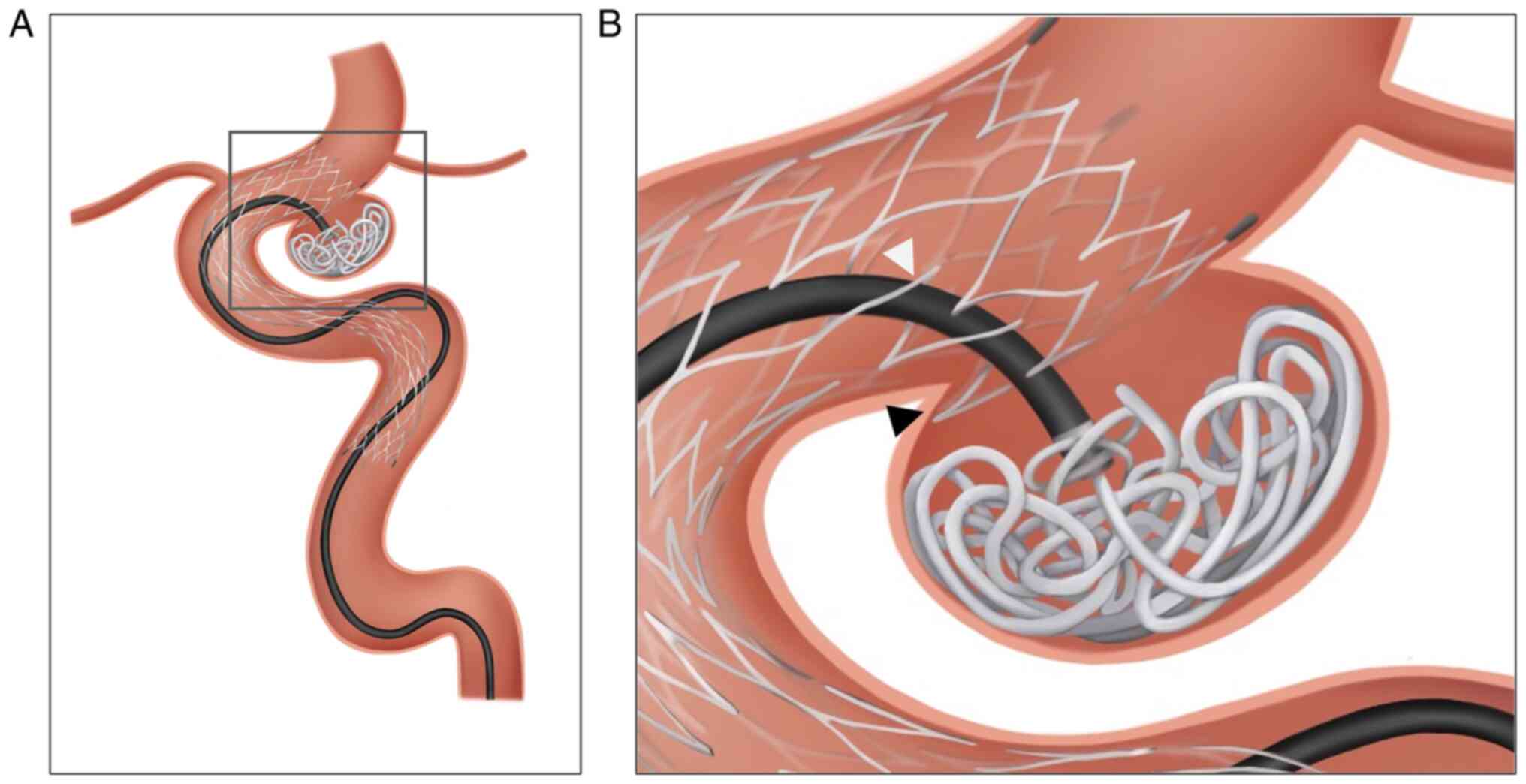
cerebral artery (for stent delivery) (Fig. 2A and B). Several loops of detachable coils
(HyperSoft™ 3D, MicroVention Inc.) were inserted into
the aneurysm sac, and stent-assisted neck protection with catheter
jailing technique was performed using the Neuroform
Atlas® stent (4 mm in diameter and 21 mm in length).
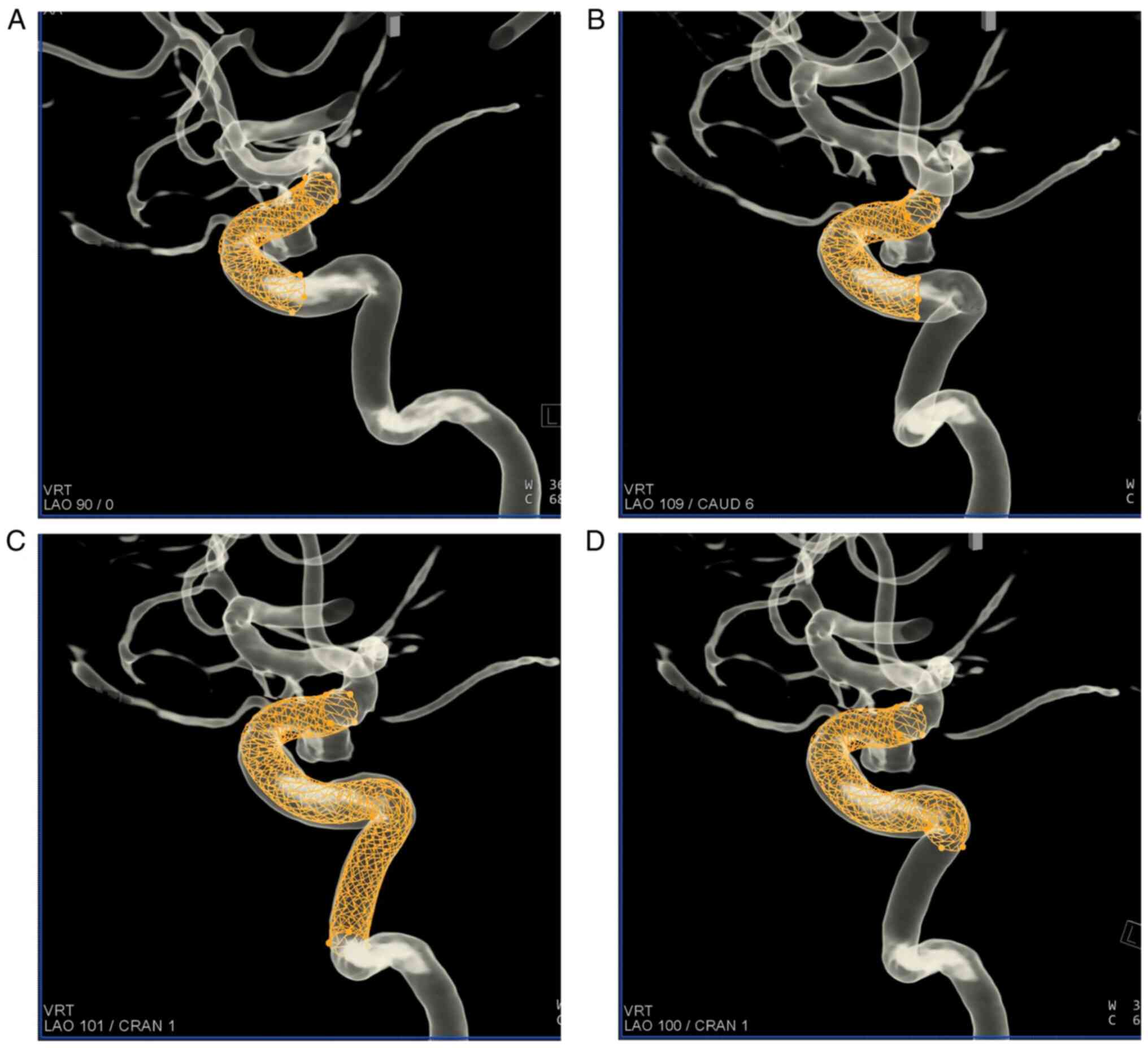
We estimated the length of the stent, and the stent
length was calculated using the Syngo Dyna3D system (Siemens
Healthineers AG). The planned landing site of stent deployment was
from the distal part of the posterior communicating artery to the
distal cavernous segment of the left ICA (Fig. 3A). The distal end of the stent was
flared in the expected site, and approximately one-third of the
stent was partially deployed as usual. Suddenly, the stent-delivery
microcatheter partially withdrew to the proximal part of the parent
artery. The distal end of the stent was positioned distal to the
aneurysm neck, but the proximal end of the stent was still
undeployed in the microcatheter. Because of its open-cell strut, we
could not resheath the stent and carefully deployed the rest of the
stent. The proximal end of the stent was placed on the lacerum
segment of the ICA (Fig. 2C and
D), and the estimated length from
the proximal to the distal marker of the stent was 40 mm-twice the
normal length (21 mm) (Fig. 3B and
C). We considered the
possibilities of a stent fracture or stretching of the stent. To
stabilize the damaged stent and remodel the aneurysm neck, we
inserted an additional stent (Neuroform Atlas® stent,
4x21 mm) into the distal part of the deployed stent with
telescoping manner. Successful coil embolization was achieved with
a small neck remnant. During the procedure, the proximal end of the
stent was gradually moved distally. Finally, it was in the proximal
cavernous segment of the ICA with a length of 30 mm (Fig. 2E, F and 3D).
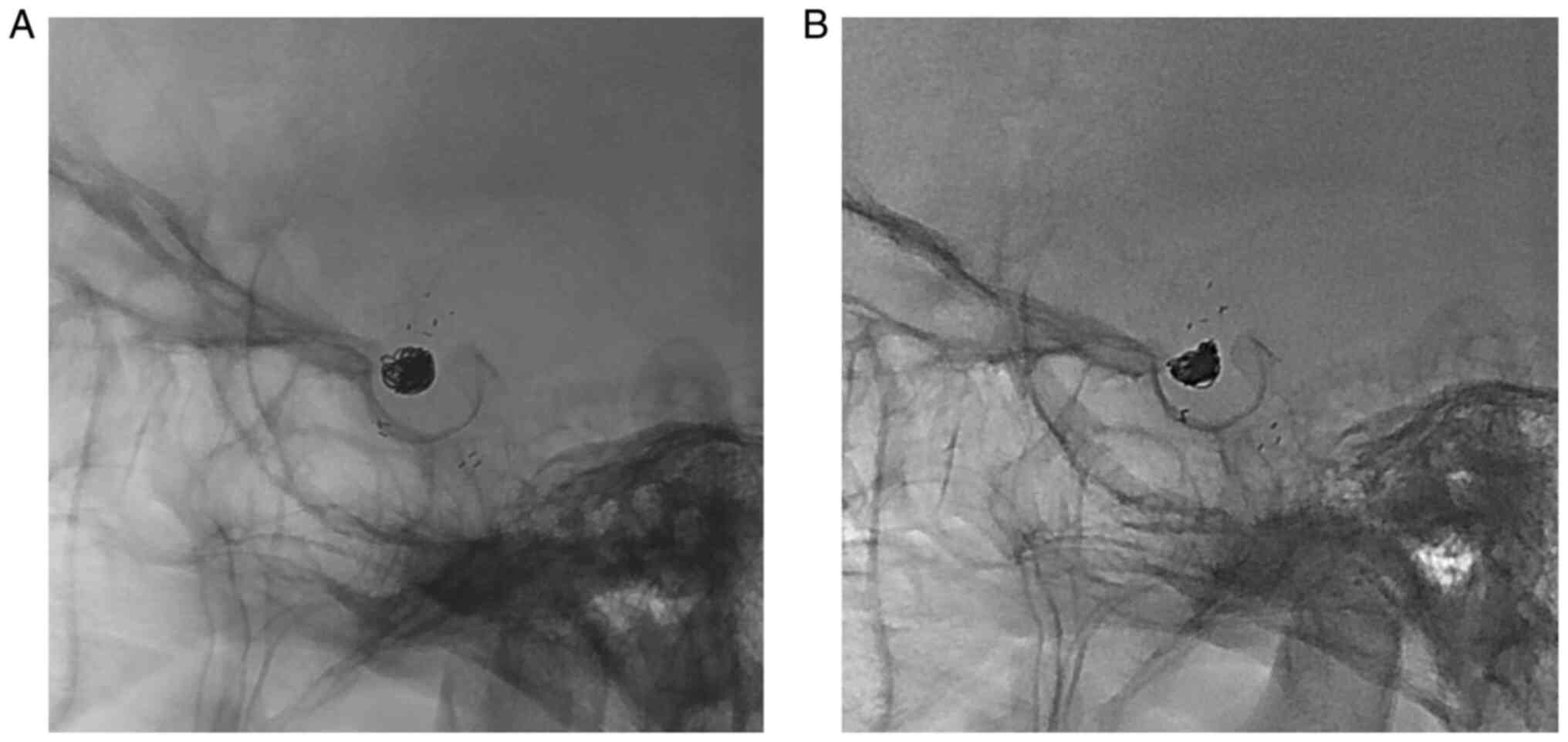
The patient recovered from the intervention without
any neurological deficit. We continued the dual antiplatelet
regimen and performed fluoroscopy and MRA 1 year postoperatively.
The fluoroscopy showed no change in length from the proximal to the
distal marker of the stent (Fig.
4). The stretched Neuroform Atlas® stent was
confirmed on magnetic resonance time of flight (MR-TOF) imaging
(Fig. 5). The MR-TOF images showed
stent struts with poor wall apposition in the cavernous ICA.
Additionally, we noticed a gap between the vessel wall and the
stent strut due to ovalization of the stent. The stent struts were
observed as longitudinally elongated shapes without definite
disconnection. The patient has no neurological symptoms and
complications until the last follow-up date.
Discussion
This is the first report of stretched and partially
fractured Neuroform Atlas® stent. The authors suggested
that this rare procedure-related complication was a result of
several factors of unique stent designs, unexpected withdrawal of
the microcatheter, coiling technique, and vascular anatomy.
As the stent-assisted technique is commonly used for
coil embolization for IAs, various laser-cut stents have been
developed in the past two decades. The laser-cut stents are divided
into closed-cell stents and open-cell stents. The advantages of the
closed-cell stent are the ability to resheath the partially
deployed stent and less frequent coil prolapse into the stent. The
major disadvantage of the closed-cell stent is poor wall
apposition. It causes the gap between the stent and vessel wall
such as ovalization on greater curvature and hugging on lesser
curvature of a sharply curved vessel. In contrast, the open-cell
stent has the great advantage of good apposition to the vessel wall
on the curved vasculature. The open-cell stent also has good
conformability with less straightening of the angle between the
parent artery and the branching artery compared to the closed-cell
stent. The disadvantages of the open-cell stent are the kinking
phenomenon of the strut into the vessel lumen along the lesser
curvature, the gator backing phenomenon of struts herniating onto
the aneurysm neck, and the inability to resheath the partially
deployed stent (10,11).
The Neuroform Atlas® stent is one of the
newest stents that strengthen the advantages of the open-cell
stent. It is a self-expandable, low-profile open-cell stent with a
hybrid design delivered with a 0.42-mm or 0.43-mm microcatheter.
Its low-profile character with thinner struts, fewer strut
connections, and increased flexibility improve the stent's
trackability and navigation to target vessels (4). Its smaller cell size compared with
earlier generations enhances the scaffolding effect with regard to
the coil mesh (8). Its unique
design with 8 or 12 struts reinforces wall apposition and
conformability of the stent (8).
Although there were several improvements compared with the earlier
generation, its open-cell nature still has disadvantages-the
kinking phenomenon, the gator backing phenomenon, and the inability
to resheath.
The reported literature confirms the efficacy and
safety of the Neuroform Atlas® stent for coil
embolization of IA. The procedure-related major adverse events and
thromboembolic complications were acceptable, and most of the
literature showed very high rates of technical success (Table I) (2-23).
However, a few cases were reported with suboptimal deployment in
unexpected locations and stent migration during the procedure
(2,5-14).
The suboptimal stent deployment occurred because of the
microcatheter's sudden uncontrolled movement to the proximal part
of the target artery during the opening and deployment of the
stent. Due to its open-cell design, a partially deployed stent
should be fully deployed even when it is positioned at a suboptimal
location.
 | Table ISummary of complications and technical
success in previous reports. |
Table I
Summary of complications and technical
success in previous reports.
| Authors | Year | Number of Aneurysm, n
(ruptured) | Use of multiple
stents, n (%) | Major complications,
n (%) | Thrombosis, n
(%) | Technical success,
% | Suboptimal deployment
or migration of stent during procedure, n | (Ref.) |
|---|
| Cay et al | 2018 | 55 (0) | - | - | - | 100 | - | (16) |
| Ulfert et
al | 2018 | 37(2) | 0 (0) | Any stroke: 1
(2.7) | - | 100 | - | (22) |
| Goertz et
al | 2019 | 37(14) | 8 (21.6) | Ischemic stroke: 1
(2.7) | 1 (2.7) | 100 | N/A | (17) |
| Ten Brinck et
al | 2019 | 27(10) | 10 (37.0) | Any stroke: 4
(14.8) | 4 (14.8) | 100 | Suboptimal
deployment: 1 | (14) |
| Tsai et
al | 2019 | 58(2) | 18 (29.1) | Procedural rupture: 1
(1.7) | 3 (5.2) | 100 | - | (21) |
| Quintana et
al | 2019 | 30 (0) | 4 (13.3) | Any stroke: 2
(6.7) | 1 (3.3) | 96.7 | Migration: 1 | (12) |
| Ciccio et
al | 2019 | 55(3) | 55(100) | Any stroke: 7
(12.5) | 8 (14.5) | 100 | Migration: 2 | (9) |
| Zadiat et
al | 2020 | 182 (0) | 29 (15.9) | Major ipsilateral
stroke: 8 (4.4) Neurological death: 1 (0.5) | | 100 | - | (3) |
| Caragliano et
al | 2020 | 113(24) | 25 (22.1) | Intra-procedural
Cx: 7 (6.2) | 4 (3.5) | 100 | Migration: 3 | (8) |
| Russo et
al | 2020 | 61(61) | N/A | Procedural
morbidity: 2 (3.2) | 22 (36.1) | 100 | - | (20) |
| Sweid et
al | 2020 | 69(25) | 11 (16.0) | Asymptomatic major
Cx: 7 (10.1) | 6 (8.7) | 98.6 | Suboptimal
deployment: 1 | (13) |
| Burkhardt et
al | 2020 | 128(17) | 110 (7.8) | Procedural
morbidity: 4 (3.1) | 6 (4.7) | 97.7 | Migration: 1 | (7) |
| Aydin et
al | 2020 | 30(3) | 30(100) | Any Stroke: 2
(6.7) | - | 100 | - | (15) |
| Kim et
al | 2020 | 33(11) | 0 (0) | - | 1 (3.3) | 100 | Suboptimal
deployment: 1 | (10) |
| Baek et
al | 2020 | 55 (0) | 0 (0) | Any Stroke: 1
(1.8) | 1 (1.8) | 98.2 | Suboptimal
deployment: 1 | (6) |
| Kwon and Chung | 2021 | 130 (0) | 3 (2.3) | Any stroke: 6
(4.6) | 5 (3.8) | 99.2 | Suboptimal
positioning: 1 | (11) |
| Arslan et
al | 2021 | 119(8) | 14 (11.8) | Any stroke: 3
(2.5) | 2 (1.7) | 99.2 | Suboptimal
position: 1 | (5) |
| Jankowitz et
al | 2021 | 116 (0) | 40 (34.5) | Major ipsilateral
stroke: 4 (3.4) Neurological death: 1 (0.9) | - | 100 | - | (4) |
| Kim and Chung | 2021 | 15 (0) | 15(100) | - | 1 (6.6) | 100 | - | (23) |
| Monteiro et
al | 2021 | 64 (0) | N/A | Procedural rupture:
2 (3.1) | - | 100 | - | (19) |
| Lefevre et
al | 2021 | 105 (0) | 21(20) | Any stroke: 5
(4.9) | 2 (1.9) | 94.7 | Suboptimal
position: 7 | (2) |
| Kato et
al | 2021 | 156(4) | N/A | Any stroke:
3(2) | 2 (1.3) | N/A | N/A | (18) |
Unexpected catheter movement to the proximal parent
artery occurred in this case, as in previously reported articles.
The distal end of the stent was maintained in the position of the
location of opening; however, the proximal end of the stent, still
in the stent-delivery microcatheter, was partially withdrawn to the
proximal part. During deployment of the stent using the jailing
technique with the aneurysm-selecting microcatheter, the stent
strut may have been hooked by the microcatheter already inserted in
the IA. Under the firmly positioned aneurysm-selecting
microcatheter, the partially deployed stent slipped, and the stent
and the microcatheter could have become caught on each other like a
hook (Fig. 6A). From the hooked
point of the proximal part of the stent, the stent-delivery
microcatheter was possibly partially withdrawn, and the stent could
have been stretched. The stretched stent resulted in gaps between
the stent and the vessel wall at the steep curvature of the ICA. In
addition to the above hypothesis, the gator backing phenomenon of
the stent strut into the IA could have exacerbated the hooking
effect on the stent (Fig. 6B).
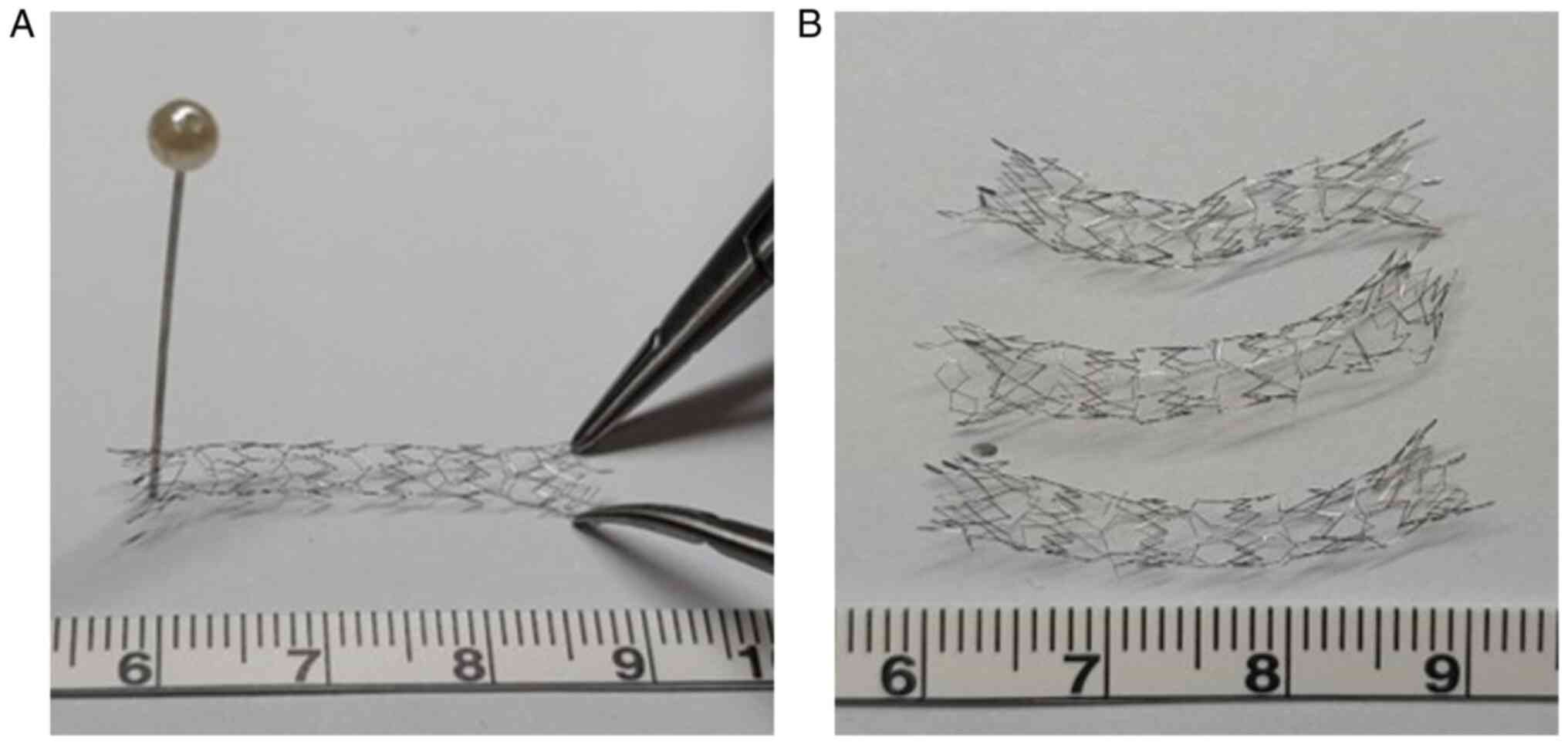
To confirm our hypothesis, we performed a simple
experiment using three Neuroform Atlas® stents (4x21
mm). We fixed one strut on the distal part of the stent and pulled
the proximal end of the stent using two pairs of microforceps
(Fig. 7A). All the stents
increased in length. The stents were stretched and partially
fractured and were about 30 mm in length with two or three
disconnections of the struts (Fig.
7B).
Fracture and deformation of intracranial stents have
rarely been reported. In contrast, fracture and deformation of
stents in extracranial carotid and vertebral arteries, coronary
arteries, and peripheral arteries have been established (24-26).
The stent fracture results from multiple complex factors involving
stent mechanics, vessel anatomy, and physiological factors.
Closed-cell stents are more prone to fracture because of their
increased rigidity. Additionally, small stent size, overlapping
stents, nitinol use, and the use of drug-eluting stents are
considered risk factors for stent fracture (26,27).
Anatomical factors such as vessel calcification, tortuosity, and
excessive angulation are well-known risk factors (26,28).
Several clinical and laboratory studies have shown that repeated
motion of vessels, such as cardiac motion, neck flexion and
extension, and joint movement play an important role in stent
fracture (29). However, the stent
fractures occurred during the follow-up period, and the risk
factors of stent fractures were not considered during the
procedure.
Most of the deformation of the stent had been
observed during our procedure. The Neuroform Atlas®
stent has been developed to increase deliverability and wall
apposition with the use of thinner struts and fewer strut
connections. But this low-profile nature could predispose stents to
longitudinal stent deformation (LSD), defined as either shortening
or elongation along the longitudinal axis. LSD is known to be more
common in cases with balloon expansion of the stent, tortuous and
complex vascular anatomy, calcification of the vessel wall, the use
of additional devices for the interventional procedure, and devices
with fewer strut connections (26,30).
Williams et al reported that the proposed mechanisms of LSD are
strongly related to compression of the guide catheter and/or
microcatheter, passing or withdrawal of a secondary device into or
through the stent, and post-dilation of the balloon (31).
This case revealed that unexpected microcatheter
withdrawal when using the catheter jailing technique could result
in the stretching and fracture of the Neuroform Atlas®
stent. Although the Neuroform Atlas® stent has a unique
design of low-profile open-cell struts, the quality problem or
structural characteristic of the stent was not the cause of this
complication. Instead, it may result from the combination of
several factors; the steep curvature of the vessel; low-profile
open-cell struts of the stent; unexpected microcatheter withdrawal
during stent deployment; and hooking of the aneurysm selecting
microcatheter with stent strut. Among these factors, unexpected
microcatheter withdrawal was the most important, resulting in this
complication that could have been avoided. Because unexpected
microcatheter withdrawal occurs more frequently in tortuous
vessels, physicians should be aware of this possibility when
treating patients with complex vascular architecture using the
catheter jailing technique. To avoid unexpected microcatheter
movement and incorrect stent deployment, the stent should be
deployed with appropriate tension of the push wire, careful
unsheathing of the microcatheter, and verified firm landing of the
distal stent end (10,11). To prevent the thromboembolic event,
we maintain the dual antiplatelet regimen with aspirin (100 mg/day)
and clopidogrel (75 mg/day) during the follow-up period. Because we
have no reliable evidence for the optimal duration of dual
antiplatelet therapy in this circumstance, we are planning to
continue dual antiplatelet regimen as long as the drug-induced
complications do not occur.
In conclusion, stretching and partial fracture of
the Neuroform Atlas® stent is a rare complication that
may occur in coil embolization for IA with stent-assisted and
catheter jailing techniques. We presumed it might result from the
combination of several factors; curved vessel; open-cell stent;
unexpected microcatheter withdrawal during stent deployment; and
hooking of the aneurysm selecting microcatheter with stent strut.
Physicians should note the possibility of this complication when
unexpected microcatheter withdrawal occurs during stent deployment
when using the catheter jailing technique. Understanding the stent
design and careful manipulation in stent deployment could prevent
this complication, which can be challenging to resolve.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Authors' contributions
HS introduced and designed the concept of this
study. HK and HS confirm the authenticity of all the raw data. HK
and HS obtained and analyzed the patient's information and wrote
the manuscript. HS reviewed the discussion part of the clinical
manifestations, imaging features and brief experiment. All authors
have read and approved the final manuscript.
Ethics approval and consent to
participate
The IRB committee of Kyung Hee University Hospital
at Gangdong exempted this case study from the IRB review approval
as following the enforcement rules (article 13 and 33 of the
Bioethics and Biosafety Act) and article 7 of the KHNMC SOP.
Patient consent for publication
Written informed consent for publication of the
clinical details and clinical images was obtained from the
individual participant.
Competing interests
The authors declare that they have no competing
interests.
Authors' information
Dr Hak Cheol Ko, ORCID: 0000-0001-8745-3309; Dr Hee
Sup Shin, ORCID: 0000-0002-5286-8448.
References
|
1
|
Jankowitz BT, Hanel R, Jadhav AP, Loy DN,
Frei D, Siddiqui AH, Puri AS, Khaldi A, Turk AS, Malek AM, et al:
Neuroform Atlas stent system for the treatment of intracranial
aneurysm: Primary results of the atlas humanitarian device
exemption cohort. J Neurointerv Surg. 11:801–806. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Lefevre PH, Schramm P, Kemmling A, Barreau
X, Marnat G, Piotin M, Berlis A, Wanke I, Bonafe A and Houdart E:
ATLAS EU PMCF Investigators. Multi-centric european post-market
follow-up study of the Neuroform Atlas stent system: Primary
results. J Neurointerv Surg. 14:694–698. 2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Zaidat OO, Hanel RA, Sauvageau EA,
Aghaebrahim A, Lin E, Jadhav AP, Jovin TG, Khaldi A, Gupta RG,
Johnson A, et al: Pivotal trial of the Neuroform Atlas stent for
treatment of anterior circulation aneurysms: One-year outcomes.
Stroke. 51:2087–2094. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Jankowitz BT, Jadhav AP, Gross B, Jovin
TG, Alhajeri AA, Fraser JF, Hanel RA, Sauvageau E, Aghaebrahim A,
Frei D, et al: Pivotal trial of the Neuroform Atlas stent for
treatment of posterior circulation aneurysms: One-year outcomes. J
Neurointerv Surg. 14:143–148. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Arslan G, Maus V, Weber W, Berlis A,
Maurer C and Fischer S: Two-center experience with Neuroform Atlas
stent-assisted coil occlusion of broad-based intracranial
aneurysms. Neuroradiology. 63:1093–1101. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Baek JW, Jin SC, Kim JH, Yoo MW, Jeong HW,
Seo JH, Han JY, Heo YJ and Kim ST: Initial multicentre experience
using the neuroform atlas stent for the treatment of un-ruptured
saccular cerebral aneurysms. Br J Neurosurg. 34:333–338.
2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Burkhardt JK, Srinivasan V, Srivatsan A,
Albuquerque F, Ducruet AF, Hendricks B, Gross BA, Jankowitz BT,
Thomas AJ, Ogilvy CS, et al: Multicenter postmarket analysis of the
neuroform atlas stent for stent-assisted coil embolization of
intracranial aneurysms. AJNR Am J Neuroradiol. 41:1037–1042.
2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Caragliano AA, Papa R, Pitrone A, Limbucci
N, Nappini S, Ruggiero M, Visconti E, Alexandre A, Menozzi R,
Lauretti D, et al: The low-profile Neuroform Atlas stent in the
treatment of wide-necked intracranial aneurysms-immediate and
midterm results: An Italian multicenter registry. J Neuroradiol.
47:421–427. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Ciccio G, Robert T, Smajda S, Fahed R,
Desilles JP, Redjem H, Escalard S, Mazighi M, Blanc R and Piotin M:
Double stent assisted coiling of intracranial bifurcation aneurysms
in Y and X configurations with the Neuroform ATLAS stent: Immediate
and mid term angiographic and clinical follow-up. J Neurointerv
Surg. 11:1239–1242. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kim CH, Kim YH, Sung SK, Son DW, Song GS
and Lee SW: Clinical safety and effectiveness of stent-assisted
coil embolization with Neuroform Atlas Stent in intracranial
aneurysm. J Korean Neurosurg Soc. 63:80–88. 2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Kwon O and Chung J: Outcomes of
stent-assisted coiling using the Neuroform Atlas stent in
unruptured wide-necked intracranial aneurysms. J Korean Neurosurg
Soc. 64:23–29. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Quintana EM, Valdes PV, Deza EM, García
AG, Rodríguez MC, Pérez JMJ, Chaviano J, Morales JCG, Batista KP
and García FA: Initial experience and one-year follow-up with
Neuroform Atlas stent system for the treatment of brain aneurysms.
Interv Neuroradiol. 25:521–529. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Sweid A, Herial N, Sajja K, Chalouhi N,
Velagapudi L, Doermann A, Kardon A, Tjoumakaris S, Zarzour H, Smith
MJ, et al: Early multicenter experience with the Neuroform Atlas
Stent: Feasibility, safety, and efficacy. Neurosurgery.
87:E321–E335. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ten Brinck MFM, de Vries J, Bartels R,
Grotenhuis JA and Boogaarts HD: NeuroForm Atlas Stent-assisted
coiling: Preliminary results. Neurosurgery. 84:179–189.
2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Aydin K, Balci S, Sencer S, Barburoglu M,
Umutlu MR and Arat A: Y-stent-assisted coiling with low-profile
Neuroform Atlas Stents for endovascular treatment of wide-necked
complex intracranial bifurcation aneurysms. Neurosurgery.
87:744–753. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cay F, Peker A and Arat A: Stent-assisted
coiling of cerebral aneurysms with the Neuroform Atlas stent.
Interv Neuroradiol. 24:263–269. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Goertz L, Dorn F, Siebert E, Herzberg M,
Borggrefe J, Schlamann M, Krischek B, Stavrinou P, Mpotsaris A,
Bohner G, et al: Safety and efficacy of the Neuroform Atlas for
stent-assisted coiling of intracranial aneurysms: A multicenter
experience. J Clin Neurosci. 68:86–91. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kato N, Nishimura K, Sonoda S, Kakizaki S,
Nagayama G, Aoki K, Maruyama F, Ikemura A, Kan I, Kodama T, et al:
Comparison of clinical outcomes after stent-assisted coiling with 3
types of self-expanding laser-cut stents in patients with
wide-necked intracranial aneurysms. World Neurosurg. 146:e701–e707.
2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Monteiro A, Cortez GM, Aghaebrahim A,
Sauvageau E and Hanel RA: Low-profile visualized intraluminal
support Jr Braided Stent versus Atlas self-expandable stent for
treatment of intracranial aneurysms: A single center experience.
Neurosurgery. 88:E170–E178. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Russo R, Bradac GB, Castellan L, Gallesio
I, Garbossa D, Iannucci G, Mardighian D, Menozzi R, Pitrone A,
Romano G, et al: Neuroform Atlas stent-assisted coiling of ruptured
intracranial aneurysms: A multicenter study. J Neuroradiol.
48:479–485. 2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Tsai JP, Hardman J, Moore NZ, Hussain MS,
Bain MD, Rasmussen PA, Masaryk TJ, Elgabaly MH, Sheikhi L and Toth
G: Early post-humanitarian device exemption experience with the
Neuroform Atlas stent. J Neurointerv Surg. 11:1141–1144.
2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Ulfert C, Pham M, Sonnberger M, Amaya F,
Trenkler J, Bendszus M and Möhlenbruch MA: The Neuroform Atlas
stent to assist coil embolization of intracranial aneurysms: A
multicentre experience. J Neurointerv Surg. 10:1192–1196.
2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kim D and Chung J: Y-stent-assisted
coiling with Neuroform Atlas stents for wide-necked intracranial
bifurcation aneurysms: A preliminary report. J Cerebrovasc Endovasc
Neurosurg. 24:1–9. 2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Adlakha S, Sheikh M, Wu J, Burket MW,
Pandya U, Colyer W, Eltahawy E and Cooper CJ: Stent fracture in the
coronary and peripheral arteries. J Interv Cardiol. 23:411–419.
2010.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Sfyroeras GS, Koutsiaris A, Karathanos C,
Giannakopoulos A and Giannoukas AD: Clinical relevance and
treatment of carotid stent fractures. J Vasc Surg. 51:1280–1285.
2010.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Wiktor DM, Waldo SW and Armstrong EJ:
Coronary stent failure: Fracture, compression, recoil, and
prolapse. Interv Cardiol Clin. 5:405–414. 2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Umeda H, Gochi T, Iwase M, Izawa H,
Shimizu T, Ishiki R, Inagaki H, Toyama J, Yokota M and Murohara T:
Frequency, predictors and outcome of stent fracture after
sirolimus-eluting stent implantation. Int J Cardiol. 133:321–326.
2009.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Shaikh F, Maddikunta R, Djelmami-Hani M,
Solis J, Allaqaband S and Bajwa T: Stent fracture, an incidental
finding or a significant marker of clinical in-stent restenosis?
Catheter Cardiovasc Interv. 71:614–618. 2008.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Ormiston JA, Webber B, Ubod B, White J and
Webster MW: Coronary stent durability and fracture: An independent
bench comparison of six contemporary designs using a repetitive
bend test. EuroIntervention. 10:1449–1455. 2015.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Ormiston JA, Webber B, Ubod B, White J and
Webster MW: Stent longitudinal strength assessed using point
compression: Insights from a second-generation, clinically related
bench test. Circ Cardiovasc Interv. 7:62–69. 2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Williams PD, Mamas MA, Morgan KP, El-Omar
M, Clarke B, Bainbridge A, Fath-Ordoubadi F and Fraser DG:
Longitudinal stent deformation: A retrospective analysis of
frequency and mechanisms. EuroIntervention. 8:267–274.
2012.PubMed/NCBI View Article : Google Scholar
|