Introduction
The spleen is the largest lymphoid organ in the
body, accounting for ~25% of total lymphoid tissue (1). Its function and structure are similar
to those of lymph nodes, making the spleen an important immune
organ with numerous lymphocytes and macrophages (2). Existing studies have confirmed that
the spleen plays an important role in anti-infection, immune
regulation, anti-tumor activity and hematopoiesis. Increasingly,
research has revealed the importance of preserving splenic
function, especially due to its anti-infection and anti-tumor
activities (1,3,4).
Total splenectomy may lead to infection for patients with splenic
diseases. Although partial splenic embolization has solved the
complications after total splenectomy, splenic embolization itself
may lead to an abscess, spleen rupture and complications after
embolization. Therefore, partial splenectomy is a good option for
select patients and preserving splenic function is a good option.
Presently, there are few reports and studies on laparoscopic
partial splenectomy and previous reports are mainly single-case
reports. After seven years of research and experience summary, the
authors performed laparoscopic partial splenectomy in 22 patients
with different types of splenic lesions to evaluate the clinical
efficacy of laparoscopic partial splenectomy.
Materials and methods
General information
Between March 2015 and May 2022, 22 patients
underwent partial splenectomies at Zhangye Second People's
Hospital. Patients meeting the following criteria were included in
the study: i) abdominal pain, abdominal distension, clinical
symptoms, lesions >5.0 cm in diameter, no basic diseases, no
lung diseases, cerebrovascular diseases, no major upper abdominal
surgery history and benign lesions considered in preoperative
imaging data; and ii) Traumatic rupture of the spleen, with
American Association of Trauma Surgery (AAST) spleen trauma grade
I-Ⅲ (5,6). Partial splenectomy is an option for
patients with ineffective conservative treatment or inability to
perform splenorrhaphy. The exclusion criteria were as follows: i)
Tumor located in splenic hilum; ii) hypersplenism; iii) severe
abdominal adhesion; and iv) splenic trauma grade of AAST IV-V. The
present study was officially approved by the Ethics Committee of
Zhangye Second People's Hospital (approval number: A032) and
written informed consent was obtained from each patient.
Surgical method
After initiation of general anesthesia, patients
were placed in a supine position, with the left hypochondriac area
elevated. The operator stood between the patient's legs, the
laparoscope was on the right side of the patient and the first
assistant stood on the left side of the patient. A 1 cm arc
incision was made at the upper edge of the umbilical cord and a
10-mm trocar (Ethicon US, LLC) was used to facilitate abdominal
cavity entry. A CO2 pneumoperitoneum was established,
with pressure maintained at 10-12 mmHg. A small opening was made 5
cm above the umbilical cord and a 12-mm trocar was used to create a
main entry point. Subsequently, another two holes were made using
5-mm trocars, one 5 cm under the front costal edge of the left
axilla and another under the xiphoid. After entering the abdominal
cavity, the condition of the hepatobiliary pancreatic
gastrointestinal tract was investigated. Then, ligaments around the
spleen were freed, the location of the splenic tumor was explored
via laparoscopy and the suspended splenic artery at the upper edge
of the pancreas was exposed. Tissues around the splenic hilum were
separated using an ultrasonic knife to expose secondary branches of
the splenic artery.
The main trunk of the splenic artery was clamped
with a vascular clamp to temporarily block blood flow, creating an
ischemic area around the spleen. After a pre-resection line was
cleared, the splenic segment and splenic lobe were disconnected
from top to bottom, close to the splenic hilum. At the same time,
the blood supply of the spleen lesion was observed to ensure the
ischemic region included the lesion. An ultrasonic knife was used
to cut 0.5-1.0 cm from the ischemic line to the diseased side to
perform partial splenectomy. Subsequently, the main splenic artery
clamp was released and the remnant spleen segment was hemostatic.
Biological hemostatic materials were placed on the wound surface of
the remnant spleen. Specimens were removed after expanding the
trocar incision created at the upper edge of the umbilical cord. A
drainage tube was placed on the wound surface under the left
diaphragm.
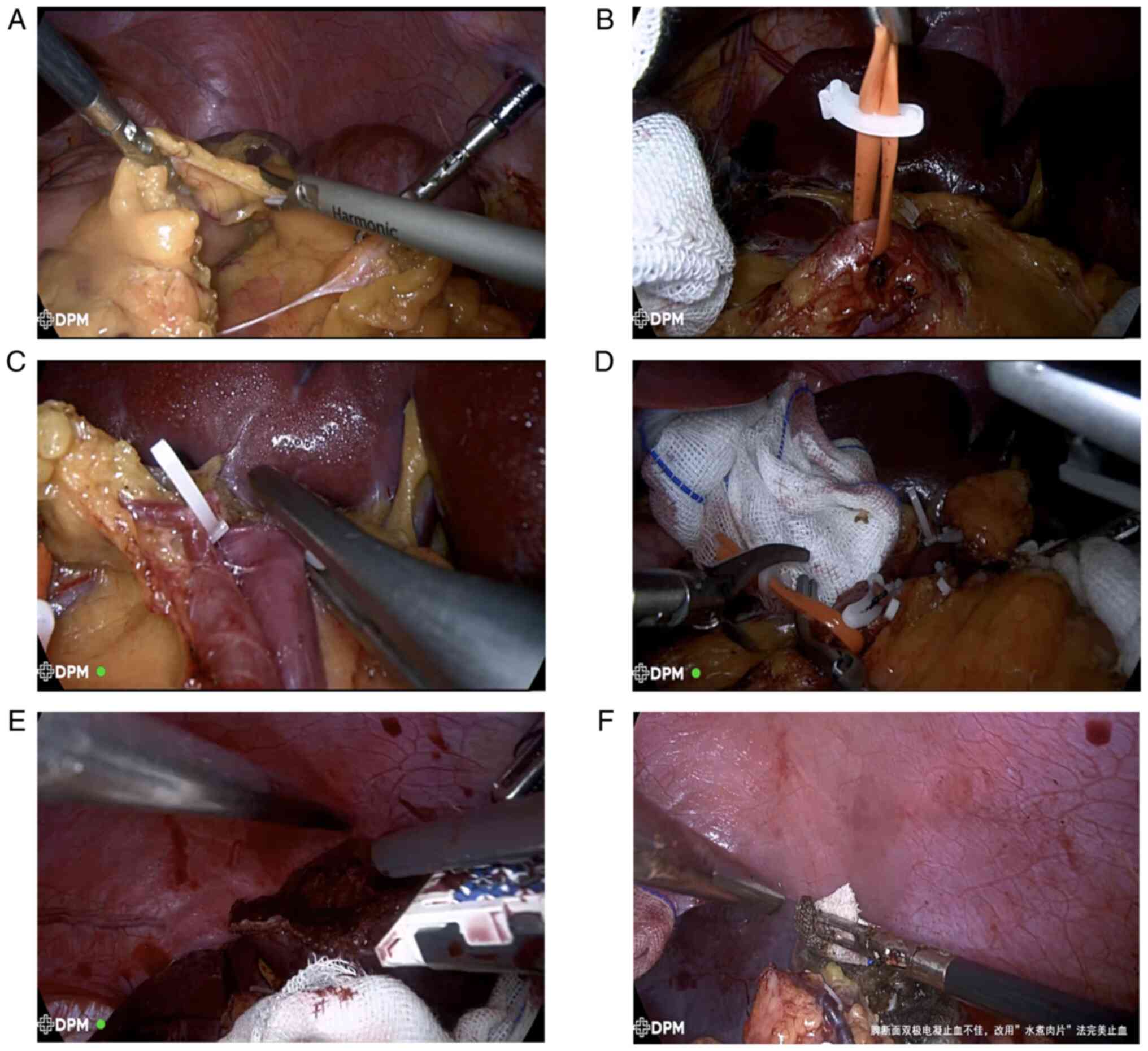
As an example, a giant, 8x9 cm splenic cyst at the
middle and lower pole of the spleen was stripped completely and
partial splenectomy was completed. First, the surrounding omentum
and ligaments were separated to expose the splenic cyst (Fig. 1A). Next, the suspended splenic
artery was disconnected at the upper edge of the pancreas (Fig. 1B), close to the splenic hilum. A
secondary blood vessel branch was isolated and disconnected from
the lower level of the spleen using an endoscope Hem-o-lok clamp
(Teleflex; Fig. 1C). Then a
vascular clamp was used to temporarily block the main trunk of the
splenic artery (Fig. 1D) before
completely peeling the splenic cyst. A disposable cutting occluder
was used to remove tissue located between the spleen and the cyst
(Fig. 1E). Finally, the bleeding
was stopped using the ‘boiled meat slice’ method (Fig. 1F). The method involved the
temporary compression of the bleeding region using a small gauze
strip rolled into a peanut shape. Subsequently, ‘peanuts’ (0.8x0.5
cm) were clamped to the spleen section while an assistant
continuously dropped normal saline to maintain gauze wetness. The
coagulation power was adjusted to 120 W. The coagulation hook that
contacted metal at the front of the intestinal clamp or coagulation
wire was connected to the intestinal clamp. Locally, ‘peanuts’ were
boiled on the spleen section and bleeding was stopped. Notably,
this method uses wet ‘peanut’ gauze as the transmission medium,
which expands the scope of electrocoagulation, avoids the formation
of eschar and tears and is very effective for maintaining
hemostasis during laparoscopic partial splenectomy, thus
effectively ensuring the safety of surgery. The method effectively
and accurately facilitated residual spleen wound hemostasis.
Results
In the present study, nine male and 13 female
patients were enrolled, with a mean age of 37.5±14.9 years (range:
16-61 years). Diameters of lesions ranged from 5.0 to 11.3 cm.
There were 14 cases of splenic cyst, five cases of splenic
hemangioma, one case of splenic hamartoma and two cases of splenic
rupture. The operation was successfully completed in 22 patients,
including 11 with lesions located at the upper pole of the spleen,
nine at the lower pole of the spleen, one at the middle upper pole
of the spleen and one at the middle lower pole of the spleen. The
operation time ranged between 75 to 180 min (mean: 120±17 min).
Among the cases considered, the mean volume of intraoperative
bleeding was 178±70 ml, ranging from 80-300 ml. The mean duration
of postoperative hospitalization was 6±2 days (Table I).
 | Table IClinical characteristics of
patients. |
Table I
Clinical characteristics of
patients.
| No | ID | Sex | Diagnosis | Age (years) | Hospitalization
days | Intraoperative
bleeding (ml) | Operation time
(min) |
|---|
| 1 | F53949 | Female | Splenic cyst | 26 | 6 | 118 | 150 |
| 2 | 982899 | Female | Splenic cyst | 33 | 5 | 120 | 125 |
| 3 | D99769 | Female | Splenic cyst | 32 | 7 | 122 | 130 |
| 4 | C92692 | Female | Splenic cyst | 28 | 6 | 116 | 148 |
| 5 | A72050 | Female | Splenic cyst | 27 | 6 | 120 | 90 |
| 6 | C99435 | Male | Splenic cyst | 20 | 3 | 112 | 125 |
| 7 | D02342 | Male | Splenic cyst | 34 | 5 | 122 | 186 |
| 8 | G01752 | Male | Splenic cyst | 60 | 5 | 118 | 120 |
| 9 | E12069 | Male | Splenic cyst | 28 | 6 | 115 | 159 |
| 10 | F46177 | Male | Splenic
hemangioma | 23 | 6 | 122 | 275 |
| 11 | G06071 | Male | Splenic
hamartoma | 61 | 10 | 115 | 260 |
| 12 | G17533 | Female | Splenic
hemangioma | 60 | 4 | 120 | 110 |
| 13 | 0008584 | Female | Splenic rupture | 57 | 8 | 116 | 285 |
| 14 | 0022364 | Male | Splenic rupture | 46 | 9 | 180 | 300 |
| 15 | 0041969 | Male | Splenic
hemangioma | 55 | 5 | 125 | 276 |
| 16 | 0031650 | Male | Splenic
hemangioma | 58 | 6 | 123 | 280 |
| 17 | 0042793 | Female | Splenic cyst | 40 | 4 | 75 | 80 |
| 18 | 0041220 | Female | Splenic cyst | 43 | 6 | 120 | 116 |
| 19 | 0042752 | Female | Splenic cyst | 27 | 5 | 118 | 158 |
| 20 | 0041052 | Female | Splenic cyst | 16 | 5 | 120 | 170 |
| 21 | 0041159 | Female | Splenic
hemangioma | 26 | 11 | 123 | 210 |
| 22 | 0041210 | Female | Splenic cyst | 25 | 6 | 122 | 175 |
After recovering gastrointestinal functioning,
patients were allowed to consume liquids and were encouraged to get
out of bed. Postoperative recovery was good and no complications
were reported. Postoperative pathology revealed 14 cases of splenic
cyst, five cases of splenic hemangioma, one case of splenic
hamartoma and two cases of splenic rupture; one patient was
diagnosed with nontraumatic splenic rupture preoperatively and one
patient with no previous traumatic history experienced spontaneous
rupture of splenic hemangioma. Emergency laparoscopic partial
splenectomy was performed. During the operation, 200 ml of old
hematocele was found in the abdominal cavity and the upper
diaphragm surface of the 6x6.5-cm mass had ruptured and was
actively bleeding. The pathology was spleen cavernous hemangioma
with postoperative rupture and bleeding. The patient recovered well
after 12 months of follow-up. The patients were followed up for 10
to 12 months; regular checks of platelet levels revealed that they
were in the normal range and computed tomography (CT) showed no
recurrence.
Discussion
Laparoscopic partial splenectomy preserves both
normal immune functioning of the spleen and effectively minimizes
the occurrence of portal vein thrombosis, splenic vein thrombosis
and pulmonary hypertension (7,8).
Partial splenectomy can preserve splenic function as much as
possible and allows for lesion removal. Prior researchers have
maintained that at least one-fourth of the spleen must be retained
to maintain normal immune function of the spleen (9,10).
Laparoscopic partial splenectomy potentially preserves the normal
immune function of the spleen, avoiding the possibility of
dangerous infection and effectively reduces the occurrence of
postoperative complications of the blood system, including
thrombocytosis, venous thrombosis and atherosclerosis.
Generally, splenic incisure is used, with splenic
hilum and splenic incisure typically placed in a location based on
the vascular gap between the upper and lower lobes of the spleen,
where the secondary splenic vessels are free. The use of
laparoscopic magnification and the careful dissection and treatment
of secondary splenic pedicle vessels are important surgical steps
that help ensure the success of the operation. The greatest
challenge of laparoscopic partial splenectomy is the dissection of
splenic portal vessels, the disconnection of splenic parenchyma and
the management of wound bleeding. If properly handled, proper wound
management can effectively reduce intraoperative and postoperative
bleeding and improve surgical success (11). If intraoperative bleeding occurs,
it is important not to be stopped blindly. The authors suggest
using the ‘boiled meat slice’ hemostasis method to stop remnant
spleen wound bleeding effectively and accurately. The authors
removed large cysts completely, preserved splenic function in two
cases of giant splenic middle upper pole and middle lower pole cyst
resection and completed partial splenectomy. Bipolar
electrocoagulation hemostasis was not satisfactory
intraoperatively; therefore, the ‘boiled pork slices’ method was
used to stop remnant spleen bleeding, producing a good hemostatic
effect.
After carefully reviewing the cases considered, the
authors consider that partial splenectomy can be performed in
patients with the following conditions: Benign splenic tumors,
tumors >5 cm, partial splenic rupture and tumors of splenic
trauma grade AAST I-Ⅲ (12).
Patients who cannot undergo conservative or splenic repair surgery
may be able to undergo partial splenectomy (13). Preoperative evaluation for
laparoscopic partial splenectomy is very important. Patients should
routinely undergo abdominal enhanced CT, abdominal ultrasound,
routine blood tests, macro-biochemistry tests, coagulation tests,
tumor tests and other related laboratory tests before surgery to
ensure that their general condition is understood, to determine the
location of lesions, judge the benign and malignant degree of
tumors and estimate the size of the residual spleen. If conditions
permit, CT angiography may further clarify the distribution and
routing of splenic vessels, which may help surgeons formulate a
personalized surgical plan. Further, in the treatment of splenic
trauma, one should actively prepare blood and improve
cross-matching preoperatively and complete the AAST grading
assessment of splenic trauma promptly. Partial splenectomy is not
recommended for patients with unstable hemodynamics.
Among existing spleen-conserving operations,
laparoscopic partial splenectomy is the most difficult. Mistakes
have the potential to lead to intraoperative and postoperative
bleeding, infection, residual spleen torsion and pancreatic leakage
(14-16).
In laparoscopic partial splenectomy, attention should be paid to
the following: i) The procedure must be performed with skill, using
minimally invasive techniques and cases should be strictly
screened; ii) for treating the residual spleen, the authors'
innovative ‘boiled meat slice’ method should be mastered to stop
bleeding. This surgical technique can play an improved role in
hemostasis, greatly reducing the difficulty and complications of
this laparoscopic surgery, which is also the authors' innovation,
thus improving operative success. This method can also be used to
stop bleeding in liver surgery. Further, after accurate hemostasis,
biological hemostatic materials can be placed on the wound surface
of the remnant spleen to prevent and treat postoperative bleeding;
iii) the operation should be gently performed with accurate
dissection. Disorderly poking, grasping and repeated operation
should be avoided; iv) during the operation, disposable cutting and
closing devices may be used to cut spleen tissue and blood vessels,
reducing the operation time and preventing remnant spleen blood
vessel bleeding; v) adequate arterial blood supply to the remnant
spleen should be ensured, not just short gastric blood supply; vi)
after ligation of the secondary blood supply vessels of the spleen,
the splenic ischemic line can help determine splenic sectioning;
vii) splenic fixation prevents the residual spleen from torsion;
viii) to ensure adequate postoperative physiological splenic
functioning, at least 30% of the spleen should be retained; and ix)
during the operation, it should be carefully checked whether there
is an accessory spleen. If one is present, it should be
removed.
In conclusion, laparoscopic partial splenectomy not
only allows for the retention of normal splenic functioning but
also speeds recovery and minimizes trauma, bleeding, pain and
complications. It is an effective method for treating benign tumors
and partial traumatic rupture of the spleen. The authors use
laparoscopy to perform partial splenectomy, which can be used to
treat hemangioma, cyst, general rupture injury, hamartoma and other
diseases. To ensure safety, patients must be strictly evaluated and
screened preoperatively and careful preparation must be performed.
If necessary, multiple disciplinary team consultations may be
conducted to assess traumatic or complex cases to predict the
possibility of surgical pitfalls and complications that may occur
during and after the operation. If bleeding cannot be controlled
during the operation, total splenectomy or conversion to laparotomy
should be considered. The principle of ‘life first, spleen second’
should always be followed. However, the ‘boiled meat slice method’
can often be used to stop remnant spleen bleeding, allowing
surgeons to achieve an improved result with minimal effort.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
DX and PL contributed to the drafting of the
manuscript and the design of the study. JY and YY contributed
substantially to the conceptualization and design of the study. DX
and YY confirm the authenticity of all the raw data. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was conducted according to the
guidelines of the Declaration of Helsinki and was approved by the
Ethics Committee of Zhangye Second People's Hospital, Zhangye
Gansu, China (approval number A032). Written informed consent was
obtained from the patients.
Patient consent for publication
Written consent was obtained for publication of the
patients' data/images in this manuscript. The proof of consent to
publish from the patients can be requested at any time.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lewis SM, Williams A and Eisenbarth SC:
Structure and function of the immune system in the spleen. Sci
Immunol. 4(eaau6085)2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Riva MA, Ferraina F, Paleari A, Lenti MV
and Di Sabatino A: From sadness to stiffness: The spleen's
progress. Intern Emerg Med. 14:739–743. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ghosh D and Stumhofer JS: The spleen:
‘Epicenter’ in malaria infection and immunity. J Leukoc Biol.
110:753–769. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Bronte V and Pittet MJ: The spleen in
local and systemic regulation of immunity. Immunity. 39:806–818.
2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Gasparetto A, Hunter D, Sapoval M, Sharma
S and Golzarian J: Splenic embolization in trauma: Results of a
survey from an international cohort. Emerg Radiol. 28:955–963.
2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Tinkoff G, Esposito TJ, Reed J, Kilgo P,
Fildes J, Pasquale M and Meredith JW: American Association for the
surgery of trauma organ injury scale I. Spleen, liver, and kidney,
validation based on the National trauma data bank. J Am Coll Surg.
207:646–655. 2008.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Romboli A, Annicchiarico A, Morini A,
Castro Ruiz C, Pagliai L, Montali F and Costi R: Laparoscopic
partial splenectomy: A critical appraisal of an emerging technique.
A review of the first 457 published cases. J Laparoendosc Adv Surg
Tech A. 31:1130–1142. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Di Mauro D, Fasano A, Gelsomino M and
Manzelli A: Laparoscopic partial splenectomy using the harmonic
scalpel for parenchymal transection: Two case reports and review of
the literature. Acta Biomed. 92(e2021137)2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Li Q, Liu Z, Hu M, Ou M, Liu K, Lin W, Wu
F and Cao M: Laparoscopic partial splenectomy of benign tumors
assisted by microwave ablation. J Cancer Res Ther. 16:1002–1006.
2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kimura K, Kurashima Y, Tanaka K, Nakanishi
Y, Asano T, Ebihara Y, Noji T, Murakami S, Nakamura T, Tsuchikawa
T, et al: Laparoscopic partial splenectomy for splenic
lymphangioma: A case report. Surg Case Rep. 6(140)2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ouyang G, Li Y, Cai Y, Wang X, Cai H and
Peng B: Laparoscopic partial splenectomy with temporary occlusion
of the trunk of the splenic artery in fifty-one cases: Experience
at a single center. Surg Endosc. 35:367–373. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Hemachandran N, Gamanagatti S, Sharma R,
Shanmuganathan K, Kumar A, Gupta A and Kumar S: Revised AAST scale
for splenic injury: Does addition of arterial phase on CT have an
impact on the grade? Emerg Radiol. 28:47–54. 2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lee R, Jeon CH, Kim CW, Kwon H, Kim JH,
Kim H, Park SJ, Kim GH and Park CY: Clinical results of distal
embolization in Grade V splenic injury: Four-year experience from a
single regional trauma center. J Vasc Interv Radiol.
31:1570–1577.e2. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Chen J, Yu S and Xu L: Laparoscopic
partial splenectomy: A safe and feasible treatment for splenic
benign lesions. Surg Laparosc Endosc Percutan Tech. 28:287–290.
2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Fedele S, Bizzoca C, Aquilino F and
Vincenti L: Laparoscopic partial splenectomy for symptomatic benign
cystic lesions: Technical notes. Updates Surg. 74:1153–1156.
2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
De Pastena M, Nijkamp MW, van Gulik TG,
Busch OR, Hermanides HS and Besselink MG: Laparoscopic
hemi-splenectomy. Surg Today. 48:735–738. 2018.PubMed/NCBI View Article : Google Scholar
|