Hypospadias is a congenital malformation, in which
the meatus is opening on the ventral aspect of the penis, at
different possible levels. Usually, the malformation is more
complex and may be associated with penile curvature, glans
deformation, narrow meatus or megameatus, and anomalies of the
skin. Severe cases can present other urogenital or chromosomal
anomalies. There are a number of unknown aspects of this
malformation's etiology and development (1,2).
Hypospadias repair may be a routine operation in distal cases and
can be very challenging in proximal cases, even for a trained
surgeon. There is no consensus on the treatment options for
hypospadias and the development of treatment guidelines remains an
unsolved file in medicine.
Furthermore, how the penis look is an important
somatic and psychological facet of every boy or every family. In
these conditions, it is obvious it became a subject of interest in
medicine and a number of doctors from different specialties
(especially pediatric surgeons or urologists) have tried to solve
the problem (3-5).
In the last 10 years, according to the PubMed
platform, an average of 313 (±38) studies were published each year
(based on a search for the keyword ‘hypospadias’), the number of
papers increasing each year. This pathology represents one of the
most debated problems and not only among pediatric surgeons
(6). For every pediatric surgeon,
urologist, and specialist in this field, it is essential to know
what is new about hypospadias and be up to date. The present study
aims to present this pathology's current perspectives and the most
important achievements in hypospadias research during 2021.
The present study protocol was registered with the
International Platform of Registered Systematic Review and
Meta-Analysis Protocols (INPLASY) on 23 November 2022 and was last
updated on 23 November 2022 (registration number
INPLASY2022110117). It was performed in accordance with the
Preferred Reporting Items for Systematic reviews and Meta-Analyses
extension for Scoping Reviews (PRISMA ScR) guidelines.
The present study chose the three most popular
platforms (PubMed, Scopus and Web of Science) and searched for the
keyword ‘hypospadias’. All the publications were restricted to
2021. All the results were downloaded in CVS format (or directly as
xls format in the case of the Web of Science platform) and
processed using Microsoft Excel software. The articles from PubMed
were used as a base of the research, PubMed being considered the
most accessible and most frequently used database. The duplicate
records were removed compared to the results from the other two
platforms. The remaining articles were analyzed individually and
manually by the three reviewers.
The present study included all the articles which
were published in 2021 in the research field of hypospadias with
valuable information relating to surgical techniques, postoperative
care, complications, anesthesia, anatomical factors, genetics,
environmental factors, endocrinology, associated malformations,
questionnaires and recommendations, management, biological
materials, animal models, retrospective studies of centers, social
media, bibliometrics, small gestational age, neoplasm, or
fertility. Articles which were written in English were accepted.
Papers in other languages were accepted if they had an English
abstract with valorous information. Papers which were published in
a year other than 2021, were outside of the research field, or were
referring to other pathologies were excluded. However, those
articles which were published in print format in 2022 and online in
2021 were considered as 2021 articles. Books, commentaries,
responses to other papers, errata and withdrawn articles were
excluded.
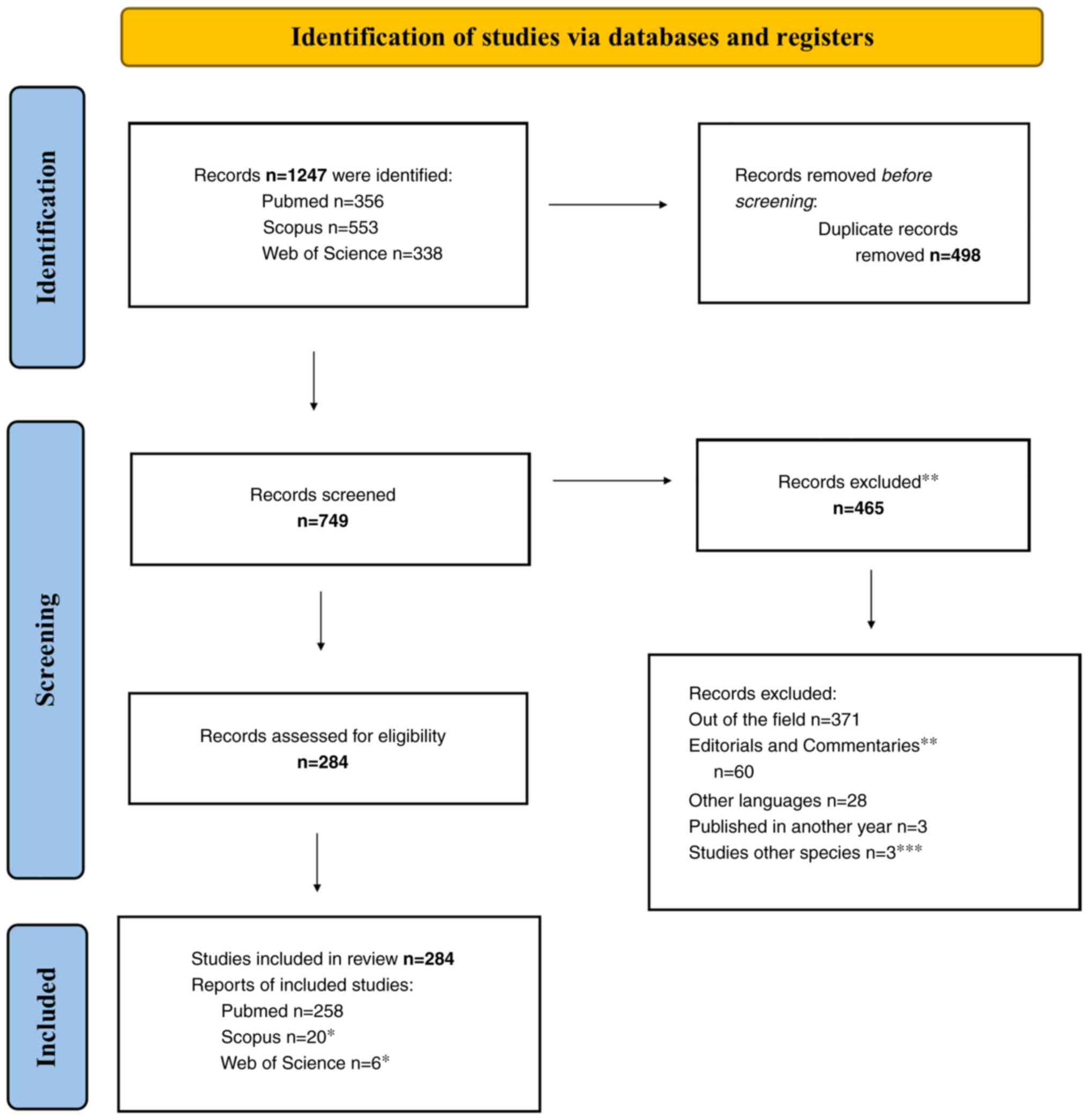
Source selection (both at title/abstract screening
and full-text screening) was performed by the three reviewers
independently (HG, ZB and ED). Any disagreements were solved by
consensus or by the decision of the fourth reviewer (ZD). The
process was accompanied by a flowchart detailing the flow from the
search, through source selection, duplicates, retrievals, and any
additions. The workflow is shown in Fig. 1.
The present study extracted from every qualified
paper the essential ideas and conclusions. Then, this information
was arranged and grouped into categories, some of them even into
subcategories. The main information of the papers on the same topic
with similar conclusions was merged, reformulated, and included in
the corresponding table. The databases were accessed for the last
time on the 20 November 2022. The number of references and the
number of included articles differ as in the introduction some
papers were cited to describe hypospadias in general.
The conclusions from the included articles relating
to hypospadias research were categorized into 18 chapters: Surgical
techniques (Subgroups: proximal hypospadias repair, distal
hypospadias repair, covering tissue, curvature, fistula and
stenosis, reoperative techniques, others), Postoperative care,
Complications, Anesthesia, Anatomical factors, Genetics (reviews,
genetical research on a population or on hospitalized patients,
genetic counseling, genetic syndromes and malformations, genetical
and histological analyses), Environmental factors, Endocrinology,
Associated malformations, Questionnaires and recommendations,
Management, Biological materials, Animal models, Retrospective
studies of centers, Social media, Bibliometrics, Small gestational
age, Neoplasm, and fertility.
A total of 284 articles were included. These were
published in 142 different journals in 2021. The most accessed
journal on this topic was the Journal of Paediatric Urology
with 54 articles (37.75% of the analyzed publications), followed by
the World Journal of Urology (nine articles), the African
Journal of Urology (eight articles), Journal of Paediatric
Surgery (eight articles), Urology (seven articles),
Research and Reports in Urology (seven articles), Journal
of Urology (seven articles), Frontiers in Pediatrics
(seven articles), Andrologia (six articles), Cureus
(five articles). All the other publications had fewer than five
papers.
The studies were classified in the described manner
and 71 referring to surgical techniques (Subgroups: 27, proximal
hypospadias repair; 18, distal hypospadias repair; seven, covering
tissue; four, curvature; nine, fistula and stenosis; three,
reoperative techniques; and three, others), 18 to postoperative
care, 16 to complications, 13 to anesthesia, 22 to anatomical
factors, 41 to genetics (three, reviews; 21, genetical factors;
six, genetical research on a population or on hospitalized
patients; four, genetic counseling; five, genetic syndromes and
malformations; and two, genetical and histological analyses), 19 to
environmental factors, 11 to endocrinology, nine to associated
malformations, 20 to questionnaires and recommendations, six to
management, six to biological materials, 11 to animal models, 11 to
retrospective studies of centers, three to social media, three to
bibliometrics, two to small gestational age and two to neoplasm and
fertility.
Surgical techniques represents the most important
chapter. A number of them refer to proximal hypospadias repair,
which is considered the most challenging among surgeons. There were
no new techniques described, but modifications were mentioned by
different authors in hope of an improved outcome and reducing the
complication rate (7-9).
The majority of studies concluded that two-stage surgery leads to
improved results compared with one stage (9-12).
The options described are modified Koyanagi technique (13-15),
transverse preputial island flap urethroplasty (10,12,16),
inlay (17-19),
or buccal mucosa graft (20,21).
Tunica vaginalis represents a good coverage material (22-24).
Scrotal raphe may be considered as a reserved option in cases of
lack of skin (25). The
urethroplasty in proximal hypospadias has improved results when
stops at the balanic sulcus. There is only one study that proposes
a three-stage urethroplasty (26).
Referring to distal hypospadias, tubularized incised
urethroplasty remains the most common and indicated operation
(27-31).
Dorsal inlay graft urethroplasty (17,19),
onlay preputial flap (19) and
hybrid Mathieu urethroplasty are mentioned techniques (32,33).
A number of authors in the last years prefer the simple advancement
of the meatus instead of a proper urethroplasty.
Neourethral covering tissues are effective to
prevent complications: tunica vaginalis, dartos, or Buck's fascia
are well-known, they can be used in one or two layers. Dorsal
plication remains the most used and simple approach to ventral
curvature (34).
Post-operatory care was also a debated issue. In
some authors' opinion, stented or un-stented repair may lead to a
similar outcome, especially in the case of distal hypospadias
(28,85). The type of the dressings was not
considered as important, although a number of substances were
enumerated by different authors to increase their efficacy. Using
compound Chamomile and Lidocaine hydrochloride gel, Aloe vera, or
autologous platelet gel might decrease pain and edema, reduce
inflammation and fibrosis, tubular finger oxygen-enriched oil
inside-coated device decrease complications (86,87).
Hyperbaric oxygen therapy may help in wound healing (88,89).
The number of diapers used is not important for the surgical
outcome, but a good washing of genitalia before and after surgery
may be effective (90). The use of
opioids or perioperative antibiotics is not relevant for surgical
success (91-93).
Postoperative C-Reactive Protein value (24 h after surgery) is a
reliable marker for a possible complication after hypospadias
surgery (94).
The most common complications after hypospadias
repair remain fistula or stenosis. In some cases, they are easy to
treat, but some of them require special interventions with grafts
or dilatations and perineal diversion of the urine (28,102,103). For urethra suturing, interrupted
sutures are an improvement on running sutures and PDS an
improvement on Vicryl (82,104).
Wound dehiscence also remains a debated problem.
Factors affecting glanular dehiscence are anatomical (glans width
<14 mm, urethral plate width <7 mm), age (before 6 months of
age and after puberty), and anesthesia (caudal block). All of these
required reinterventions (42,105). Reoperation rate after distal
hypospadias repair ranges from 3.3-6.7% (106,107). Other related complications are
penile curvature that appears in 25% of cases (>30˚) (43,102,108-110),
hairy urethra (111,112), erectile dysfunctions (113,114) and lower urinary tract symptoms
(115). There were similar
complications every surgeon is acquainted with.
General anesthesia remains the most widely accepted
type of anesthesia in hypospadias repair (29,123-125).
It is difficult to recommend regional anesthesia for pediatric
penoscrotal procedures (127).
The usefulness of caudal block-type anesthesia in postoperative
pain control and its potential to favor complications represent a
common topic. According to Routh (127) caudal block ‘is not a cause of
complication-according to the data- and it is not a key to
success’. A restrictive regimen is preferred over the conventional
intraoperative fluid regimen during hypospadias surgery (128).
There are some anatomical factors associated with
hypospadias and the severity of the malformation. Glans width,
urethral plate width and shape and history of previous surgery are
the most important factors in hypospadias (136). In addition, the anogenital
distance and penile length are diminished in children having this
malformation (137). Small glans
are associated with the severity of hypospadias (138). Penile curvature accompanies
almost all cases of hypospadias. To objectively measure the penile
curvature different degrees were defined, but it is difficult to
standardize them (139,140). A paper proposes a 3D-printed
penile model from a set of five pictures obtained from a lateral
view (141).
Microvascular density in the prepuce is not clear
which is correlated with the severity of the malformation (142). Magnetic resonance imaging is a
solution to a improved view of anatomical components of the penis,
even from the intrauterine stage, but we cannot imagine this
procedure performed on every child presenting hypospadias (143,144). Artificial intelligence is not
advanced enough to recognize and classify hypospadias (145). As another observation, 2/3 of the
patients having prostatic utricle cysts present hypospadias
(146).
The appetite for quantification is present in
hypospadias. The Hypospadias Objective Penile Evaluation (HOPE)
score, the Plate Objective Scoring Tool (POST), or the
Glans-Meatus-Shaft score are proposed for an improved evaluation of
hypospadias (30,147,148). Risk factors associated with
complications were severe ventral curvature (the main factor),
followed by urethral stricture, dehiscence, and reoperation
(107).
Maternal exposure to different chemicals can induce
malformation of the penis. The most incriminated chemicals in this
process are bisphenol, inorganic solvents, alkyl phenolic
compounds, phthalates, benzophenones, parabens, siloxanes,
pesticides or herbicides, diethylstilbestrol, cadmium, DDT,
vinclozolin (fungicide), petroleum solvents and SO2
(194-201).
Some studies are more general and incriminate the air pollution,
heat, or the proximity of a vineyard in the development of
hypospadias (202-204).
In regard to endocrinological factors, two main
hypotheses were identified. One is that prenatal factors: diabetes,
intake of progestins, estrogens, β-blockers, assisted reproductive
technology, and diethylstilbestrol (treatment in grandmothers can
lead to a greater risk for hypospadias in offspring and grandsons)
(207,213-217).
The other is that in some penile malformations, preoperatory
testosterone treatment is conducted for improved results (218-220).
The best-known associated malformation with proximal
hypospadias is cryptorchidism (223). Hypospadias is frequently
associated with cardiac, renal and skeletal malformations (224). There is also a correlation
between anorectal malformation complexity and associated urologic
abnormalities (225). In
addition, a number of genetic syndromes are associated with
hypospadias, some of which are described in the Genetics section
(section 9). A peculiarity is cases of hypospadias with disorders
of sex development. Severe genital ambiguity requires complex
genetic and anatomic investigation to declare the patient as a male
(226-228).
Other observations note that talipes, hypospadias and septal heart
defects are more frequent mild defects associated with prematurity
and gonadal neoplastic lesions appearing frequently together with
hypospadias (229).
Some papers refer to the outcome following
hypospadias surgery. Some authors call for standardization of
penile appearance. The Penile Perception Score-PPS, Hypospadias
Objective Score Evaluation-HOSE, International Index of Erectile
Function-5-IIEF5, or Health-related quality of life (HRQoL) were
conceived for that purpose (6,233).
These scores are different from the point of view of patients,
parents, or surgeons so there is no standard yet. Curvature and
shortening are the anatomical modifications most perceived by the
patients (234). Voiding,
erectile problems, social interaction and psychological issues are
the functional problems after surgery (233,235).
For most families, a boy having hypospadias is a
psychological trauma. Usually, parents do not know about this
malformation and have to be informed, and this is not always, in
terms of time and explanation, what they expect. The need for
reintervention is perceived in the majority of cases as a trauma
for patients and parents (3,38).
An article claims that hypospadias and neurologic impairment may
share common etiologic factors, thus every patient with hypospadias
should be evaluated for neurodevelopmental status (243). Timing for complex malformations
has to be considered individually in every case. Delayed surgery in
children with hypospadias is also determined by the economy of the
area where the family lives and the educational level of the
parents (240).
In a hospital register, it is not easy to classify
hypospadias properly, although there are algorithms for
identification (248). Another
question is: ‘What are the specialties of the surgeons who are
managing these cases?’ Usually, they are pediatric surgeons or
pediatric urologists (depending on the country) (249). Regardless of the specialty, the
repair of hypospadias requires an experienced doctor. The learning
curve seems quite long; surgeons are considered experienced in the
field after treating a minimum of 50 cases, supervised by an
experienced surgeon (7). When the
child becomes an adult, it is better to be managed by urologists
trained in genitourinary reconstructive surgery (250). It is important to inform general
practitioners, and pediatricians about the management of
hypospadias, as it seems that a number of them do have not adequate
knowledge about the condition (251).
Biological engineering materials and products are
becoming increasingly popular in hypospadias repair and the present
study enumerated some of them which were used in urethroplasties.
Acellular dermal matrix grafts (with Collagen-Binding VEGF),
harvested from the bladder or derm were successfully used in the
urethral reconstruction and authors claim that the results were
comparable with tunica vaginalis (253). Tissue sealants such as fibrin
glue, cyanoacrylate glue, Bio Glue, and cryocalcium glue were used
to reduce fistula-related complications (254).
Experiments on animals are rare, poorly reported,
less detailed and not reproducible (as a review found) (259). A single urethral reconstruction
is reported in a rabbit model. It used a decellularized intestinal
submucosa, seeded with urothelial cells (260). Specific genes were discovered and
involved in hypospadias formation in rats and mice (261-264).
Prenatal atrazine and vinclozolin exposure can affect penile and
testicular development (265).
On social media (Facebook, Twitter and others), the
problem of hypospadias is debated, but much of the shared content
does not have supporting evidence and is not affiliated with
medical journals, hospitals, or academic institutions. For parents
with insufficient medical knowledge, it could be difficult to
identify whether the articles shared on social media are a reliable
resource for health. YouTube videos present different surgical
treatments for this malformation, but the majority of the content
is non-medical and may lead to health misinformation (280-282).
As can be seen, hundreds of papers are written every
year about hypospadias, referring to all aspects of the pathology.
2021 was mostly a year of accumulation, with a number of papers
comparing and hoping for new surgical techniques with improved
outcomes, clarifying the relevant anatomical, etiological and
genetic factors, assuming the complications, and describing
solutions to prevent or treat them. As a limitation of the present
study, quality assessment of the included articles was not
performed.
According to the findings of the present study, it
is possible to highlight the following ideas considering that these
might have direct clinical significance: Promising modifications in
proximal hypospadias repair were presented and transverse preputial
island flap urethroplasty with incised urethral diversion appeared
a superior option compared with transurethral diversion (8). Two-stage urethroplasty had improved
results compared with one-stage surgery (10,12,16,35,36).
Tubed pedicled preputial island flap, Duckett's procedure, was
associated with a high complication rate (44). Predictors of a successful outcome
of tubularized incised plate (TIP) repair in cases of distal
hypospadias were described by different authors (53,86).
Dorsal inlay graft urethroplasty was considered a superior
technique compared with onlay preputial flap (LOF) (19). With the exception of the long-term
outcomes in cosmetic and functional evaluation, Mathieu incised
plate technique had improved outcomes compared with the TIP
technique (63). For the treatment
of congenital ventral penile curvatures, dorsal plication was
defined as a relatively simple and successful method with low risks
(34). There were no differences
in outcomes between pre-pubertal and post-pubertal boys after the
correction of penile curvature using corporal plication (70). In order to decrease the rate of
complications new dressing techniques, and topical agents were
mentioned along the hyperbaric oxygen therapy (88,89,96,97,99).
Perioperative prophylactic antibiotics appeared not to reduce the
possibility of infections (101).
A total of 25% of adults presenting with bulbar strictures had a
hypospadias surgery in childhood (117). Penile curvature could appear in
25% of patients within the first 2 years (102,108,110). According to postoperative care,
surgeons appear more concerned about the cosmesis than do the
parents. Photo documentation of cosmesis (and to evaluate penile
curvature) is appropriate at present (5). Self-reported outcomes in adolescent
patients with TIP repair were similar to those in a control group
(31). Delayed surgery could be
determined by the region's economy, the parent's educational level
and the urethral opening site (29). There were noteworthy pediatric
urologic issues, including hypospadias, on social media and they
are debated, but most of them are not very relevant. There is a
scarcity of high-quality videos on YouTube describing hypospadias
repair techniques, and their quality regarding educational content
appears unsatisfactory (280-282).
The novelty of the present study consisted of the
lack of similar analyses. To the best of the authors' knowledge, no
similarly conceptualized studies have been previously performed in
this research field. As a scoping review, the present study
represented a well-structured and reproducible mapping of the
literature. It aimed to define and clarify key concepts, theories,
the most important results and achievements, and to present them in
a transparent way, highlighting areas where researchers could
identify gaps in the current literature that may require further
inquiry. The present study presented sources of evidence that
inform practice in the field, eases further investigations and
saves time and resources. Hypospadias research in 2021 represents a
very complex field. A comprehensive scoping review such as the
present constitutes essential information for every pediatric
surgeon, urologist, and specialist in this field.
According to the papers published in 2021, promising
modifications of existing surgical techniques were presented with
improved outcomes for the proximal and distal types of hypospadias
forms. The present study highlighted and clarified the presented
relevant anatomical, etiological and genetic factors. For an
improved understanding of the aspects of peri- and postoperative
management of hypospadias the antibiotherapy, analgesia, dressing
techniques and the future use of novel bioengineering agents to
prevent, reduce or treat the occurring complications, were also
discussed.
Not applicable.
Funding: No funding was received.
Data sharing is not applicable to this article, as
no data sets were generated or analyzed during the current
study.
HG and ZB were responsible for conceptualization and
methodology. ZB was responsible for software. HG, ZB, ED and ZD
were responsible for validation. ZB was responsible for formal
analysis. HG was responsible for investigation. ED and ZD were
responsible for data curation. HG wrote the original draft. HG, ZB,
ED and ZD wrote, reviewed and edited the manuscript. ZB was
responsible for visualization and supervision. HG was responsible
for project administration. All authors read and approved the final
manuscript. Data authentication is not applicable.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
|
1
|
van der Horst HJR and de Wall LL:
Hypospadias, all there is to know. Eur J Pediatr. 176:435–441.
2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kaefer M: Hypospadias. Semin Pediatr Surg.
30(151080)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Snodgrass P, Snodgrass W and Bush N:
Parental concerns of boys with hypospadias. Res Rep Urol. 13:73–77.
2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
van Engelen H, Custers JAE, Kortmann BM,
Oerlemans AJM, van Rooij IALM and Verhaak CM: Parental decisional
regret after surgical treatment in young boys born with
hypospadias. J Pediatr Urol. 17:691.e1–691.e7. 2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Costa E, Fraga JC, Salle JP and Rosito N:
Does parental opinion differ from the health care team regarding
cosmesis after hypospadias repair? Rev Assoc Med Bras (1992).
67:33–38. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ceccarelli PL, Lucaccioni L, Poluzzi F,
Bianchini A, Biondini D, Iughetti L and Predieri B: Hypospadias:
Clinical approach, surgical technique and long-term outcome. BMC
Pediatr. 21(523)2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Hisamatsu E, Sugita Y, Haruna A, Shibata R
and Yoshino K: The learning curve in proximal hypospadias repair. J
Pediatr Urol. 17:330.e1–330.e6. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Wang C, Ma N, Wang W, Endo Y, Chen W and
Li S: Incised urethral diversion reduces the rate of fistula after
one-stage hypospadias repair: A single-center retrospective
controlled study. World J Urol. 39:4235–4240. 2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Babu R and Chandrasekharam VVS:
Meta-analysis comparing the outcomes of single stage (foreskin
pedicled tube) versus two stage (foreskin free graft & foreskin
pedicled flap) repair for proximal hypospadias in the last decade.
J Pediatr Urol. 17:681–689. 2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ali MM, El-Hawy MM, Galal EM, Tawfiek ER
and Anwar AZ: Results of two-stage transverse preputial island flap
urethroplasty for proximal hypospadias with chordee that mandate
division of the urethral plate. Cent European J Urol. 74:89–94.
2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Chan YY, D'Oro A, Yerkes EB, Rosoklija I,
Balmert LC, Lindgren BW, Gong EM, Liu DB, Johnson EK, Chu DI and
Cheng EY: Challenging proximal hypospadias repairs: An evolution of
technique for two stage repairs. J Pediatr Urol. 17:225.e1–225.e8.
2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zhu X, Huang L, Wang J, Zhu H, Chen C,
Wang L, Deng Y, Ma G, Guo Y and Ge Z: Comparative study of
one-stage and the novel two-stage urethroplasty using the
transected urethral plate and transverse preputial island flap
(TPIF) for severe hypospadias: A single-center experience. Transl
Pediatr. 10:843–850. 2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Madec FX, Desplanches M, Chabaud M, Irtan
S, Suply E and Audry G: Koyanagi urethroplasty for proximal
hypospadias: A stage procedure? Prog Urol. 32:312–318.
2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Vu TH, Viet Nguyen H, Quy Hong Q, Quang
Pham H, Thanh Pham T, Hai Do Đ and Đo Truong T: Results of the
one-stage proximal hypospadias repair with modified Koyanagi
technique: A prospective cohort study in a single Vietnam centre.
Ann Med Surg (Lond). 71(103012)2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Acimi S, Abderrahmane N, Debbous L, Acimi
MA and Mansouri J: Koyanagi-snow-hayashi urethroplasty in severe
hypospadias repair: Between hope and reality. Urology. 152:129–135.
2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lin H, Wang YY, Li SB, Chen ZT and Su LJ:
Staged transverse preputial island flap urethroplasty for some
proximal hypospadias with moderate-to-severe chordee. BMC Urol.
21(182)2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Silay MS, 't Hoen L, Bhatt N, Quaedackers
J, Bogaert G, Dogan HS, Nijman RJM, Rawashdeh Y, Stein R, Tekgul S
and Radmayr C: Are there any benefits of using an inlay graft in
the treatment of primary hypospadias in children? A systematic
review and metanalysis. J Pediatr Urol. 17:303–315. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Swatesutipun V, Yoosuksomboon N and Zaontz
MR: A novel transurethral approach to inlay oral mucosal graft
urethroplasty technique for meatal and fossa navicularis stricture
resulting from distal hypospadias repair. J Pediatr Urol.
17:585–586. 2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Omran M, Sakr A, Elgalaly H, Fawzy A and
Abdalla M: Narrow urethral plate augmentation in anterior and
middle hypospadias repair: Onlay flap vs Inlay graft. A prospective
randomized comparative study. J Pediatr Urol. 17:216.e1–216.e8.
2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Chen S, Li Y, Ma N, Wang W, Xu L and Yang
Z: Staged buccal mucosa graft urethroplasty for proximal
hypospadias in children: A short- to mid-term follow-up
retrospective study. Eur J Pediatr Surg. 31:420–426.
2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Shandilya G, Kureel SN, Gupta A, Singh GP,
Pandey A, Rawat JD and Wakhlu A: Bracka urethroplasty with buccal
mucosa graft: Ergonomic management of penile skin dartos in the
first stage to facilitate second-stage neourethral coverage. J
Indian Assoc Pediatr Surg. 26:11–15. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Tiwari C and Borkar N: Evaluation of
tunica vaginalis free graft as a better alternative to tunica
vaginalis pedicled flap for providing waterproof cover in stage II
hypospadias repair. Afr J Paediatr Surg. 18:90–93. 2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Favorito LA, da Silva Filho FS and de
Resende Junior JA: A new option to prevent fistulas in anterior
urethroplasty in patients with kippered urethra: The tunica
vaginalis flap. Int Braz J Urol. 47:1032–1036. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Radhakrishnan CN and Radhakrishna V: The
tunica-vaginalis flap to prevent postoperative fistula following
severe hypospadias repair: Has the search for Holy Grail ended?
Actas Urol Esp (Engl Ed). 45:552–556. 2021.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Obaidullah Shami HB, Obaid O, Alvi HF,
Mahboob M and Akbar F: Outcomes of islanded scrotal raphe flap
employment for skin shortage in complicated hypospadias repair. J
Plast Reconstr Aesthet Surg. 74:3386–3393. 2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Jordan A, Sumfest J and Desantis J: A new
3-stage approach for reoperative hypospadias. Ann Plast Surg.
88:544–548. 2022.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Taneli C, Tanriverdi HI, Genc A, Sencan A,
Gunsar C and Yilmaz O: Tubularized reconstructed plate
urethroplasty: An alternative technique for distal hypospadias
repair. Urology. 148:243–249. 2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Abdel-Hamid El-Hawy M, Ali MM, Abdelhamid
AM, Fawzy AM, Hussein A and Elsharkawy MSM: Long-term outcome of
non-stented tubularized incised plate urethroplasty for distal
hypospadias repair: A complication analysis. Cent European J Urol.
74:595–600. 2021.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Zhang J, Zhu S, Zhang L, Fu W, Hu J, Zhang
Z and Jia W: The association between caudal block and urethroplasty
complications of distal tubularized incised plate repair:
Experience from a South China National Children's Medical Center.
Transl Androl Urol. 10:2084–2090. 2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Galal M, Taha DE, Elabden KZ, Nabeeh H and
Abdelbaky T: The effect of pre-incision urethral plate width and
glanular width on the outcome of tubularized incised urethral plate
repair surgery in distal penile hypospadias, a prospective study.
Urol J. 19:50–55. 2021.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Ludovica D, Bianco M, Pelizzari A, Mandato
F, Esposito C and Castagnetti M: Self-reported outcomes after the
onset of puberty in patients undergoing primary distal hypospadias
repair by the tubularized incised plate technique combined with
preputial reconstruction vs circumcision: A norm related study. J
Pediatr Surg. 56:1411–1416. 2021.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Khirallah M and El-Dossuky N: Hybrid
mathieu urethroplasty: A simple modification outcomes. Res Rep
Urol. 13:473–478. 2021.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Xie QG, Xia K, Li XP, Luo P, Li ZQ, Su C
and Deng CH: Application of the Mathieu combined tunnel technique
for repairing glans dehiscence after failed hypospadias repair.
Asian J Androl. 24:311–316. 2022.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Akdemir F, Kayıgil Ö and Okulu E: DORSAL
plication technique for the treatment of congenital ventral penile
curvature: Long-term outcomes of 72 cases. J Sex Med. 18:1715–1720.
2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Zhu XJ, Dong J, Ge Z and Guo YF: Staged
urethroplasty by tubularization of reconstructed urethral plate
using the preputial island flap for severe hypospadias. Zhonghua
Nan Ke Xue. 27:134–139. 2021.PubMed/NCBI(In Chinese).
|
|
36
|
Ali MM and Anwar AZ: Experience with
modified two stage inner preputial flap for repair of proximal
hypospadias with chordee: A single institution study with
intermediate follow up. J Pediatr Surg. 57:1404–1408.
2022.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Aziz Tamer FA, El Zalabany Ahmed M and
Lolah Magdy M: The modified Koyanagi technique versus two-staged
urethroplasty using buccal mucosal graft in managing proximal
hypospadias: A randomized clinical trial. Egypt J Surg. 40:633–639.
2021.
|
|
38
|
Lu J, Cen J, Wang W, Zhao H, Li P, Mo J,
Chen Z, Tang Y, Wei J, Luo J, et al: Localization of external
urethral orifice in coronary sulcus during urethroplasty in case of
severe hypospadias accompanied by prostatic utricle cyst. BMC Urol.
21(149)2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Akkary R, Ripepi M, Akokpe O, Louati H,
Klipfel C and Geiss S: Two simple modifications can potentially
change the future of proximal hypospadias surgery. Our series and a
review of the literature. Int J Pediatr Adolesc Med. 8:172–176.
2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Ding Y, Gu S, Xia X and Yu Z: Comparison
of penile appearance and outcomes between prefabricated urethra and
pre-implanted urethral plate for treatment of children with severe
hypospadias: A retrospective study. Front Pediatr.
9(719551)2021.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Chen S, Yang Z, Ma N, Wang WX, Xu LS, Liu
QY and Li YQ: Scrotal septal flap and two-stage operation for
complex hypospadias: A retrospective study. World J Clin Cases.
9:2983–2993. 2021.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Lyu YQ, Yu L, Xie H, Huang YC, Li XX, Sun
L, Liang Y and Chen F: Spongiosum-combined glanuloplasty reduces
glans complications after proximal hypospadias repair. Asian J
Androl. 23:532–536. 2021.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Karakuş SC and Süzen A: Vertical
plication: A penile curvature correction technique that reduces the
need for urethral plate transection in penoscrotal hypospadias. J
Pediatr Urol. 17:516.e1–516.e5. 2021.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Ndiaye M, Sow Y, Sarr A, Thiam A, Faye ST,
Ndour NS, Sine B, Zé-Ondo C, Sow O, Ndiath A, et al: Hypospadias
treatment by tubulated pedicled preputial island flap according to
the DUCKETT technique: Single-center experience in sub-Saharan
Africa. Afr J Urol. 27(156)2021.
|
|
45
|
Rawashdeh YF, Hvistendal GM and Olsen LH:
Foreskin transplantation between monozygotic twins discordant for
hypospadias. Ugeskr Laeger. 183(V10200788)2021.PubMed/NCBI(In Danish).
|
|
46
|
Blanc T, Peycelon M, Siddiqui M, Muller C,
Paye-Jaouen A and El-Ghoneimi A: Double-face preputial island flap
revisited: Is it a reliable one-stage repair for severe
hypospadias? World J Urol. 39:1613–1624. 2021.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Fahiem-Ul-Hassan M, Jadhav V,
Munianjanappa N, Saroja M and Santhanakrishnan R: Outcome of Buck's
fascia repair with wingless glanuloplasty in distal penile
hypospadias. Afr J Urol. 27(73)2021.
|
|
48
|
Keshk TAEH, El Sheikh YMO, El Rahman MA,
Rezq HSA and Dawod HAA: New modification of Koyanagi technique
using dartos muscle flap in management of proximal hypospadias.
Egypt J Hosp Med. 84:1832–1838. 2021.
|
|
49
|
Tudu HC, Mishra A, Mohanty SK, Prashanthi
N, Roy I, Bhardwaj P and Pujari PS: Outcome of proximal hypospadias
repair in children using standard surgical technique with
intermediate vascularised flap-a retrospective cohort study. J Clin
Diagn Res. 15:9–12. 2021.
|
|
50
|
Long CJ, van Batavia J, Wisniewski AB,
Aston CE, Baskin L, Cheng EY, Lakshmanan Y, Meyer T, Kropp B,
Palmer B, et al: Post-operative complications following
masculinizing genitoplasty in moderate to severe genital atypia:
Results from a multicenter, observational prospective cohort study.
J Pediatr Urol. 17:379–386. 2021.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Askarpour S, Peyvasteh M, Mohamadi A and
Khoshkhabar M: Comparative study of modifying meatal advancement
glandular with release chordi versus snodgrass surgical methods
regarding the repair of distal hypospadias. World J Plast Surg.
10:73–77. 2021.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Edan OAA: Urethral mobilization and
advancement technique in distal types of hypospadias: Short-term
local experience. Ann Pediatr Surgery. 17(60)2021.
|
|
53
|
Noureldin YA, Gharib TM, El Attar KA, El
Karamany TM and Al Adl AM: Extended TIP vs standard TIP for primary
distal hypospadias repair: Randomized study for comparing
functional and cosmetic outcomes. Scand J Urol. 55:466–473.
2021.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Abdelhalim KM, Abdelwahab HA, Abdelgawad
E, Kadry AM and Sherief MH: Predictors of successful outcome of
tubularized incised plate for primary distal hypospadias repair.
Afr J Urol. 27(164)2021.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Shoukry A, Abbas A, Abdelwahab M, Ghoneima
W, Shouman A, El Ghoneimy M, Morsi H, Badawy H, Eissa M and
Aboulela W: Glans-urethral meatus-shaft score and penile parameters
as preoperative assessment tools for hypospadias surgery outcome.
Afr J Urol. 27(102)2021.
|
|
56
|
Macedo A Jr, Ottoni SL, Di Migueli RDD, de
Mattos RM, Garrone G and Leal da Cruz M: A different approach to
distal hypospadias repair: The GUD (glandular urethral disassembly)
technique. J Pediatr Urol. 17:690.e1–690.e6. 2021.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Özbey H, Ayryan E, Staroverov O and
Morozov DA: Anatomical modeling of the foreskin for the
reconstruction of glanular hypospadias. J Pediatr Urol. 17:335–337.
2021.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Permana W, Djojodimedjo T and Renaldo J:
Tubularized incised plate urethroplasty for megameatus intact
prepuce hypospadias variant: First reported case in Indonesia. Int
J Surg Case Rep. 80(105698)2021.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Ahmed S, Noureldin YA, Sherif H, Zahran A
and Omar R: Cosmetic outcomes of grafted tubularized incised plate
urethroplasty in primary distal penile hypospadias: Prospective
comparative study with the classic snodgrass repair. Afr J Urol.
27(152)2021.
|
|
60
|
Kızılöz H, Okçelik S and Temel MC: MAGPI
under local anaesthesia without catheter as an alternative to
standard TIP procedure in distal hypospadias repair. Andrologia.
53(e13949)2021.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Alshammari D and Harper L:
Deepithelialized glans reconfiguration (DeGRe) for distal
hypospadias repair. J Pediatr Urol. 17:59.e1–59.e8. 2021.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Zhang B, Bi YL and Ruan SS: Application
and efficacy of reconstructing forked corpus spongiosum in
distal/midshaft hypospadias repair. Asian J Androl. 23:47–51.
2021.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Mohajerzadeh L, Moghadam AD, Tabari AK,
Rouzrokh M and Moghimi N: Comparing mathieu and tubularized
incised-plate urethroplasties for repairing distal penile
hypospadias: A single-center experience with long-term outcome.
Iran J Pediatr. 31(e111184)2021.
|
|
64
|
Benson CR, Li G and Brandes SB: Long term
outcomes of one-stage augmentation anterior urethroplasty: A
systematic review and meta-analysis. Int Braz J Urol. 47:237–250.
2021.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Tessier B, Sfar S, Garnier S, Coffy A,
Borrego P, Gaspari L, Paris F and Kalfa N: A cover flap reduces the
rate of fistula after urethroplasty whatever the severity of
hypospadias. World J Urol. 39:2691–2695. 2021.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Rudin YE, Maruhnenko DV, Rudin AY, Aliev
DK, Lagutin GV and Vardak AB: Augmentation of the urethral plate in
the glans penis area and the distal urethra-effective method of
fistula correction in children with hypospadias. Androl Gen Surg.
22:62–70. 2021.
|
|
67
|
Verma A, Murtaza S, Kundal VK, Sen A and
Gali D: Comparison of dartos flap and spongioplasty in snodgrass
urethroplasty in distal penile hypospadias. World J Pediatr Surg.
4(e000294)2021.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Naumeri F, Munir MA, Ahmad HM, Sharif M,
Awan NU and Butt G: Comparison of urethrocutaneous fistula rate
after single dartos and double dartos tubularized incised plate
urethroplasty in pediatric hypospadias. Cureus.
13(e13378)2021.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Zhang Y, Chao M, Zhang WP, Tang YM, Chen
HC, Zhang KP, Lu RG, Zhang XS and Lou DH: Using Buck's fascia as an
integral covering in urethroplasty to restore the anatomical
structure of the penis in one-stage hypospadias repair: A
multicenter chinese study comprising 1,386 surgeries. Front
Pediatr. 9(695912)2021.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Cetin S, Budak FC, Tan MO, Biri H, Sen I,
Kupeli AB, Bozkirli I and Gurocak OS: Comparison of corporal
plication for the correction of congenital penile curvature in
pre-pubertal and post-pubertal patients: Does age matter?
Andrologia. 53(e13965)2021.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Kozyrev GV, Manasherova DT and
Abdulkarimov GA: Ventral penis curvature correction in children
with hypospadias. Urologiia. 74–77. 2021.PubMed/NCBI(In Russian).
|
|
72
|
Zhou G, Xu W, Yin J, Sun J, Yang Z and Li
S: Single-stage versus staged interposition urethroplasty for
glandular hypospadias with severe penile curvature: 15-Year
experience. World J Urol. 40:155–160. 2022.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Furr JR, Wisenbaugh ES and Gelman J:
Long-term outcomes for 2-stage urethroplasty: An analysis of risk
factors for urethral stricture recurrence. World J Urol.
39:3903–3911. 2021.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Favre GA, Villa SG, Scherñuk J, Tobia IP
and Giudice CR: Glans preservation in surgical treatment of distal
urethral strictures with dorsal buccal mucosa graft onlay by
subcoronal approach. Urology. 152:148–152. 2021.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Mershon JP and Baradaran N: Recurrent
anterior urethral stricture: challenges and solutions. Res Rep
Urol. 13:237–249. 2021.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Singh J: Urethrocutaneous fistula repair
following hypospadias surgery using the PATIO technique for small
fistulae: A single centre experience. J Pediatr Urol.
18:60.e1–60.e7. 2022.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Bar-Yosef Y, Ben-Chaim J, Ekstein M,
Ben-David R, Savin Z, Yossepowitch O, Mano R and Dekalo S:
Concomitant repair of meatal stenosis and urethral fistula does not
increase the risk of fistula recurrence post hypospadias surgery.
Urology. 160:187–190. 2022.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Chatterjee US, Basu AK and Bhaumik K:
Needling for suture track fistula. J Indian Assoc Pediatr Surg.
26:203–205. 2021.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Shirazi M, Chowdhury U, Ahmed F,
Rajabalian MB, Nikbakht HA, Al-Naggar K and Al-Shami E: Optimal
clamping time in meatotomy procedure for children with meatal
stenosis: Experience with 120 cases. Arch Ital Urol Androl.
93:244–247. 2021.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Shaw NM, Mallahan C, Joshi P, Venkatesan K
and Kulkarni S: Novel use of Asopa technique for penile
urethrocutaneous fistula repair. Int Urol Nephrol. 53:1127–1133.
2021.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Yadav S, Bamaniya M, Agarwal V, Tomar V,
Gupta A and Kumawat G: Dorsal midline incision: A versatile
technique for correction of meatal stenosis during hypospadias
repair. J Clin Urol. 14:43–46. 2021.
|
|
82
|
Samir M, Mahmoud MA, Azazy S and Tawfick
A: Does the suturing technique (continuous versus interrupted) have
an impact on the outcome of tubularized incised plate in
hypospadias repair with adequate urethral plate? A prospective
randomized study. J Pediatr Urol. 17:519.e1–519.e7. 2021.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Spinoit AF, Sinatti C, Lambert E, Pauwaert
K, Verla W, van Laecke E and Hoebeke P: How I do it: Buttonholing
the preputial hood in hypospadias repair-related ventral skin
shortage. J Pediatr Urol. 17:332–334. 2021.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Mohamed Ali Alaraby SO, Abdeljaleel IA,
Hamza AA and Elawad Elhassan AE: A comparative study of
polydioxanone (PDS) and polyglactin (Vicryl) in hypospadias repair.
Afr J Paediatr Surg. 18:53–57. 2021.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Scarpa MG, Codrich D, Iaquinto M, Guida E,
Cerrina A and Schleef J: Medium-term outcome after stented and
un-stented distal urethroplasty: A retrospective analysis on
redo-urethroplasty need and cosmetic results. Actas Actas Urol Esp
(Engl Ed). 45:642–647. 2021.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Zhang SY, Han C, Zhou HX, Li P, Ma LF, Tao
T, Zhou XG, Tao YD, Zhu WW, Zhao Y, et al: Clinical evaluation of
compound chamomile and lidocaine hydrochloride gel for
postoperative hypospadias in children. Zhonghua Nan Ke Xue.
27:815–818. 2021.PubMed/NCBI(In Chinese).
|
|
87
|
Doluoglu OG, Yıldız Y, Tokat E, Ozgur BC,
Kılınc MF, Inan MA, Gonul II and Hoscan MB: The histopathological
effect of aloe vera on the wound healing process in a surgically
created tubularized incised plate urethroplasty model on rats. J
Invest Surg. 35:1062–1066. 2022.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Oley MH, Oley MC, Iskandar AAA, Toreh C,
Tulong MT and Faruk M: Hyperbaric oxygen therapy for reconstructive
urology wounds: A case series. Res Rep Urol. 13:841–852.
2021.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Anand S, Krishnan N and Bajpai M: Utility
and safety of hyperbaric oxygen therapy as a rescue treatment in
complicated cases of hypospadias: A systematic review and
meta-analysis. J Pediatr Urol. 18:39–46. 2022.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Anand S: Single-diaper, double-diaper, or
no diaper: Does it make any difference following the repair of
hypospadias? J Pediatr Urol. 17(885)2021.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Donnelly L, Feustel PJ, Cangero T and
Kogan B: Postoperative pediatric urology opioid prescriptions at a
tertiary academic medical center. J Pediatr Urol. 17:633.e1–633.e6.
2021.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Cornwell LB, Campbell PC, Ewing E and
Swords KA: Children undergoing outpatient complex penile surgery
and hypospadias repair may not require opioid analgesics. J Pediatr
Surg. 57:678–682. 2022.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Basin MF, Baker ZG, Trabold M, Zhu T,
Kelley-Quon LI, Bhaskar N, Vazirani R, Chen J and Kokorowski PJ:
The impact of patient age and procedure type on postoperative
opioid use following ambulatory pediatric urologic procedures.
Pediatr Surg Int. 37:1127–1133. 2021.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Ji F, Tang H, Wu C, Chen L, Wang H and Yan
B: Predictive value of C-reactive protein for early postoperative
complications in children after hypospadias surgery. Front Pediatr.
9(690863)2021.PubMed/NCBI View Article : Google Scholar
|
|
95
|
Karakaya AE, Güler AG and Doǧan AB:
Dressing or not after tubularized incised plate urethroplasty. Urol
Int. 105:1029–1033. 2021.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Esposito C, Coppola V, Del Conte F, Cerulo
M, Esposito G, Crocetto F, Castagnetti M, Calignano A and Escolino
M: Evaluation of a new tubular finger oxygen-enriched oil
inside-coated dressing device in pediatric patients undergoing
distal hypospadias repair: A prospective randomized clinical trial
part II. Front Pediatr. 9(638406)2021.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Esposito C, Del Conte F, Cerulo M, Coppola
V, Esposito G, Ricciardi E, Crocetto F, Castagnetti M, Calignano A
and Escolino M: Evaluation of efficacy of oxygen-enriched oil-based
gel dressing in patients who underwent surgical repair of distal
hypospadias: A prospective randomised clinical trial. World J Urol.
39:2205–2215. 2021.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Anand S: Tissue glue-based dressings
following hypospadias repair: A game-changer or a useless gimmick!
J Pediatr Urol. 17:679–680. 2021.PubMed/NCBI View Article : Google Scholar
|
|
99
|
Elsayem K, Darwish AS, AbouZeid AA, Kamel
N, Dahab MM and El-Naggar O: Autologous platelet gel improves
outcomes in tubularized incised plate repair of hypospadias. J
Pediatr Surg. 57:488–491. 2022.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Murakami H, Seo S, Ochi T, Yazaki Y,
Takeda M and Yamataka A: A useful tip for preventing surgical site
infections after hypospadias repair. A single surgeon's experience
of 376 cases. Afr J Paediatr Surg. 18:5–8. 2021.PubMed/NCBI View Article : Google Scholar
|
|
101
|
Canon SJ, Smith JC, Sullivan E, Patel A
and Zamilpa I: Comparative analysis of perioperative prophylactic
antibiotics in prevention of surgical site infections in stented,
distal hypospadias repair. J Pediatr Urol. 17:256.e1–256.e5.
2021.PubMed/NCBI View Article : Google Scholar
|
|
102
|
Kim JK, Shiff M, Chua ME, Zu'bi F, Ming
JM, Pokarowski M and Farhat WA: Time to event analysis for
post-hypospadias repair complications: A single-surgeon experience.
World J Urol. 39:3913–3919. 2021.PubMed/NCBI View Article : Google Scholar
|
|
103
|
Arslan Alıcı Ç, Karkın EB and Tokar B: An
atypical complication after hypospadias repair: A combined dorsal
and lateral subcoronal urethrocutaneous fistulas. Andrologia.
54(e14276)2022.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Shirazi M, Haghpanah A, Dehghani A,
Haghpanah S, Ghahartars M and Rahmanian M: Comparison of
post-urethroplasty complication rates in pediatric cases with
hypospadias using Vicryl or polydioxanone sutures. Asian J Urol.
9:165–169. 2022.PubMed/NCBI View Article : Google Scholar
|
|
105
|
Karabulut R, Turkyilmaz Z, Atan A, Kaya C
and Sonmez K: What are the factors affecting glanular dehiscence
after hypospadias surgery? Actas Urol Esp (Engl Ed). 46:4–15.
2022.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
106
|
Nguyen S, Durbin-Johnson B and Kurzrock
EA: Reoperation after hypospadias repair: Long-term analysis. J
Urol. 205:1778–1784. 2021.PubMed/NCBI View Article : Google Scholar
|
|
107
|
Ru W, Tang D, Wu D, Tao C, Chen G, Wei J,
Tian H and Shu Q: Identification of risk factors associated with
numerous reoperations following primary hypospadias repair. J
Pediatr Urol. 17:61.e1–61.e5. 2021.PubMed/NCBI View Article : Google Scholar
|
|
108
|
Snodgrass W and Bush N: Recurrent ventral
curvature after proximal TIP hypospadias repair. J Pediatr Urol.
17:222.e1–222.e5. 2021.PubMed/NCBI View Article : Google Scholar
|
|
109
|
Ben-David R, Kupershmidt A, Dekalo S,
Herzberg H, Mano R, Dubi-Sobol A, Ben-Chaim J and Bar-Yosef Y:
Dorsal penile curvature and megameatus intact prepuce hypospadias:
A common association in a rare variant of hypospadias. J Pediatr
Urol. 17:517.e1–517.e4. 2021.PubMed/NCBI View Article : Google Scholar
|
|
110
|
Spinoit AF, Waterschoot M, Sinatti C,
Abbas T, Callens N, Cools M, Hamid R, Hanna MK, Joshi P, Misseri R,
et al: Fertility and sexuality issues in congenital lifelong
urology patients: male aspects. World J Urol. 39:1013–1019.
2021.PubMed/NCBI View Article : Google Scholar
|
|
111
|
Varea-Malo R, Martínez Revuelta D,
Campos-Juanatey F, Calleja Hermosa P and Correas Gómez MA:
Long-term undesirable consequences of penile skin island flap to
correct penoescrotal transposition: A case report and review of
literature. Case Rep Urol. 2021(6656540)2021.PubMed/NCBI View Article : Google Scholar
|
|
112
|
Kumar S, Mittal A, Panwar VK and Mandal
AK: Laser epilation of luminal hair following skin graft
urethroplasty for hypospadias: The hair snare. BMJ Case Rep.
14(e244123)2021.PubMed/NCBI View Article : Google Scholar
|
|
113
|
Özbey H and Morozov D: Hypospadias
surgery, erectile dysfunction and the distal ligament. J Pediatr
Urol. 17:592–593. 2021.PubMed/NCBI View Article : Google Scholar
|
|
114
|
Husmann DA: Erectile dysfunction in
patients undergoing multiple attempts at hypospadias repair:
Etiologies and concerns. J Pediatr Urol. 17:166.e1–166.e7.
2021.PubMed/NCBI View Article : Google Scholar
|
|
115
|
Chapman DW, Bekkema J and Rourke K:
Urinary symptom nonresponse (‘LUTS failure’) after urethroplasty:
Incidence and Associations. J Urol. 206:986–993. 2021.PubMed/NCBI View Article : Google Scholar
|
|
116
|
Favre G, Gil S, Carminatti T, Tobia I and
Giudice C and Giudice C: Predictors of complex urethral surgery in
anterior urethral stricture disease. Arch Esp Urol. 74:547–553.
2021.PubMed/NCBI
|
|
117
|
Faraj S, Loubersac T, Bouchot O, Heloury Y
and Leclair MD: Adults with previous hypospadias surgery during
childhood: Beware of bulbar strictures. J Pediatr Urol.
18:4.e1–4.e8. 2022.PubMed/NCBI View Article : Google Scholar
|
|
118
|
Ali D and Hanna MK: Symptomatic corpus
spongiosum defect in adolescents and young adults who underwent
distal hypospadias repair during childhood. J Pediatr Urol.
17:814.e1–814.e5. 2021.PubMed/NCBI View Article : Google Scholar
|
|
119
|
Tack LJW, Springer A, Riedl S, Tonnhofer
U, Hiess M, Weninger J, Mahmoud A, Van Laecke E, Hoebeke P, Cools M
and Spinoit AF: Adolescent and young adult urogenital outcome
following childhood hypospadias repair: Perfection revisited. J
Urol. 206:734–744. 2021.PubMed/NCBI View Article : Google Scholar
|
|
120
|
Godfrey LM: Mental health outcomes among
individuals with 46,XY disorders of sex development: A systematic
review. J Health Psychol. 26:40–59. 2021.PubMed/NCBI View Article : Google Scholar
|
|
121
|
Sembiring G and Sigumonrong Y: Efficacy of
preoperative testosterone therapy in hypospadias: A systematic
review and meta-analysis. Ann Pediatr Surg. 17(56)2021.
|
|
122
|
Lucas-Herald AK, Montezano AC, Alves-Lopes
R, Haddow L, Alimussina M, O'Toole S, Flett M, Lee B, Amjad SB,
Steven M, et al: Vascular dysfunction and increased cardiovascular
risk in hypospadias. Eur Heart J. 43:1832–1845. 2022.PubMed/NCBI View Article : Google Scholar
|
|
123
|
Alizadeh F, Amraei M, Haghdani S and
Honarmand A: The effect of caudal epidural block on the surgical
complications of hypospadias repair in children aged 6 to 35
months: A randomized controlled trial. J Pediatr Urol.
18:59.e1–59.e6. 2022.PubMed/NCBI View Article : Google Scholar
|
|
124
|
Koul A, Shukla D, Aggrawal SK and Sethi N:
Incidence of urethrocutaneous fistula following distal hypospadias
repair with and without caudal epidural block: A randomized pilot
study. J Pediatr Urol. 18:58.e1–58.e7. 2022.PubMed/NCBI View Article : Google Scholar
|
|
125
|
Adler AC, Chandrakantan A, Lee AD, Koh CJ,
Janzen NK and Austin PF: Effect of caudal vs penile block on the
incidence of hypospadias complications following primary repairs: A
retrospective cohort study. J Urol. 205:1454–1459. 2021.PubMed/NCBI View Article : Google Scholar
|
|
126
|
Osmani F, Ferrer F and Barnett NR:
Regional anesthesia for ambulatory pediatric penoscrotal
procedures. J Pediatr Urol. 17:836–844. 2021.PubMed/NCBI View Article : Google Scholar
|
|
127
|
Routh JC: Caudal blocks and hypospadias
repair complications-much ado about nothing or the real deal? J
Urol. 205:1252–1253. 2021.PubMed/NCBI View Article : Google Scholar
|
|
128
|
Elsonbaty M, Abdullah S and Elsonbaty A:
Lung ultrasound assisted comparison of volume effects of fluid
replacement regimens in pediatric patients undergoing penile
hypospadias repair: A randomized controlled trial. Anesth Pain Med.
11(e115152)2021.PubMed/NCBI View Article : Google Scholar
|
|
129
|
Kandirici A, Mutlu M and Yiğit D: Does
block anesthesia used in hypospadias surgery increase complication
rates? İzmir Dr Behçet Uz Çocuk Hast Dergis. 11:328–332. 2021.
|
|
130
|
Sisay A, Girma B, Negusie T, Abdi S, Horsa
B and Ayele K: Inadvertent life-threatening total spinal anesthesia
following caudal block in a preschool child underwent urologic
surgery: A rare case report. Int J Surg Case Rep.
88(106541)2021.PubMed/NCBI View Article : Google Scholar
|
|
131
|
Ponde V, Singh N, Nair A, Ongaigui CJ and
Nagdev T: Comparison of landmark-guided, nerve stimulation-guided,
and ultrasound-guided techniques for pediatric caudal epidural
anesthesia: A prospective randomized controlled trial. Clin J Pain.
38:114–118. 2021.PubMed/NCBI View Article : Google Scholar
|
|
132
|
Ahmed WAI, Shokier MHEHAEW, Kasem AAA, El
Aziz MHA and Saed SGA: Comparative study between ultrasound-guided
pudendal nerve block and caudal epidural block anesthesia in
children undergoing hypospadias surgery. Ain-Shams J Anesthesiol.
13(50)2021.PubMed/NCBI View Article : Google Scholar
|
|
133
|
Wang Y, Jia YP, Zhao LY, He QJ, Qi JL,
Zhou R, Yang T, Zhao ZX and Wei HQ: Effects of three different
doses of dexmedetomidine and ropivacaine on analgesia and the
stress response in hypospadias surgery: A randomized trial. Front
Pharmacol. 12(612216)2021.PubMed/NCBI View Article : Google Scholar
|
|
134
|
Hassan AH, Amer IA and Abdelkareem AM:
Comparative study between different additives to levobupivacaine in
caudal block for postoperative pain management in pediatrics
undergoing hypospadias repair: Randomized controlled study. Egypt J
Hosp Med. 83:1120–1128. 2021.
|
|
135
|
Karami T, Hoshyar H and Tavana AM:
Comparing caudal block and penile block using rectal acetaminophen
in postoperative analgesia of hypospadias repair: A randomized
clinical trial study. Int J Surg Open. 29:9–13. 2021.
|
|
136
|
Goel HK, Tirthraj CM, Kabra S, Gahlawat S,
Sharma U and Sood R: Factors affecting outcome of adult hypospadias
single stage repair: A prospective observational study. Turk J
Urol. 47:420–426. 2021.PubMed/NCBI View Article : Google Scholar
|
|
137
|
Abbas TO and Ali M: Scrotal base distance:
A new key genital measurement in males with hypospadias and
cryptorchidism. Curr Urol. 15:214–218. 2021.PubMed/NCBI View Article : Google Scholar
|
|
138
|
Sennert M, Wirmer J and Hadidi AT:
Preoperative glans & penile dimensions in different hypospadias
grades. J Pediatr Urol. 18:47–53. 2022.PubMed/NCBI View Article : Google Scholar
|
|
139
|
Abbas TO: Evaluation of penile curvature
in patients with hypospadias; gaps in the current practice and
future perspectives. J Pediatr Urol. 18:151–159. 2022.PubMed/NCBI View Article : Google Scholar
|
|
140
|
Abbas TO: The rising need for preoperative
objective quantification of curvature in patients with hypospadias.
J Pediatr Urol. 17:599–600. 2021.PubMed/NCBI View Article : Google Scholar
|
|
141
|
Fernandez N, Flórez-Valencia L, Prada JG,
Chua M and Villanueva C: Standardization of penile angle estimation
with a semi-automated algorithm. J Pediatr Urol. 17:226.e1–226.e6.
2021.PubMed/NCBI View Article : Google Scholar
|
|
142
|
Zhao Z, Liu GC, Zhang LY, Fu W, Jia W and
Hu JH: Mean microvessel density of the prepuce and its relationship
with the severity of hypospadias and early postoperative
complications. Zhonghua Nan Ke Xue. 27:725–728. 2021.PubMed/NCBI(In Chinese).
|
|
143
|
Li K, Zhang X, Yan G, Zheng W and Zou Y:
Prenatal diagnosis and classification of fetal hypospadias: The
role and value of magnetic resonance imaging. J Magn Reson Imaging.
53:1862–1870. 2021.PubMed/NCBI View Article : Google Scholar
|
|
144
|
Chaudhary G, Yhoshu E, Chauhan U, Ahmed I,
Gupta MK, Piplani R and Balija SS: Anatomical study of hypospadias
penis using magnetic resonance imaging in children. J Pediatr Urol.
18:57.e1–57.e7. 2022.PubMed/NCBI View Article : Google Scholar
|
|
145
|
Fernandez N, Lorenzo AJ, Rickard M, Chua
M, Pippi-Salle JL, Perez J, Braga LH and Matava C: Digital pattern
recognition for the identification and classification of
hypospadias using artificial intelligence vs experienced pediatric
urologist. Urology. 147:264–269. 2021.PubMed/NCBI View Article : Google Scholar
|
|
146
|
Dai LN, He R, Wu SF, Zhao HT and Sun J:
Surgical treatment for prostatic utricle cyst in children: A
single-center report of 15 patients. Int J Urol. 28:689–694.
2021.PubMed/NCBI View Article : Google Scholar
|
|
147
|
Abbas TO: The plate objective scoring tool
(POST): Further reflections and extended applications. Res Rep
Urol. 13:783–791. 2021.PubMed/NCBI View Article : Google Scholar
|
|
148
|
D'Oro A, Chan YY, Rosoklija I, Meyer T,
Shannon R, Johnson EK, Liu DB, Gong EM, Maizels M, Matoka DJ, et
al: Association between intra-operative meatal mismatch and
urethrocutaneous fistula development in hypospadias repair. J
Pediatr Urol. 17:223.e1–223.e8. 2021.PubMed/NCBI View Article : Google Scholar
|
|
149
|
Gopal M: Ano-scrotal distance (ASD): Is it
a marker for the severity of chordee? J Pediatr Urol. 17:672–673.
2021.PubMed/NCBI View Article : Google Scholar
|
|
150
|
Yeşildal C, Yilmaz Ö, Akan S, Küçükodaci
Z, Yenigürbüz S and Ediz C: Is primary adult hypospadiatic prepuce
different from healthy prepuce in terms of microvascular density
and androgen-estrogen-progesterone receptors? Andrologia.
53(e13857)2021.PubMed/NCBI View Article : Google Scholar
|
|
151
|
Seleim HM: Topographic labeling of glans
penis and corpus spongiosum when planning surgery for distal
hypospadias. Res Rep Urol. 13:167–173. 2021.PubMed/NCBI View Article : Google Scholar
|
|
152
|
Abdullaev Z, Agzamkhodjaev S, Chung JM and
Lee SD: Risk factors for fistula recurrence after urethrocutaneous
fistulectomy in children with hypospadias. Turk J Urol. 47:237–241.
2021.PubMed/NCBI View Article : Google Scholar
|
|
153
|
Özbey H, Devecioğlu D and Staroverov O: A
closer look at iatrogenic hypospadias. Andrologia.
53(e13803)2021.PubMed/NCBI View Article : Google Scholar
|
|
154
|
Gao F, Gong C and Li L: Advance in
research on the role of MAMLD1 gene in disorders of sex
development. Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 38:912–916.
2021.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
155
|
Ibba A, Del Pistoia M, Balsamo A, Baronio
F, Capalbo D, Russo G, DE Sanctis L and Bizzarri C: Differences of
sex development in the newborn: From clinical scenario to molecular
diagnosis. Minerva Pediatr (Torino). 73:606–620. 2021.PubMed/NCBI View Article : Google Scholar
|
|
156
|
Nassau DE, Best JC, Cohen J, Gonzalez DC,
Alam A and Ramasamy R: Androgenization in Klinefelter syndrome:
Clinical spectrum from infancy through young adulthood. J Pediatr
Urol. 17:346–352. 2021.PubMed/NCBI View Article : Google Scholar
|
|
157
|
Nordenskjöld A and Holmdahl G: Role of
genetic counseling for patients with hypospadias and their
families. Eur J Pediatr Surg. 31:492–496. 2021.PubMed/NCBI View Article : Google Scholar
|
|
158
|
Fendereski K, Carey J, Timme K, Hayes K,
Robnett J and Schaeffer A: 46 XY undervirulized male DSD: Reporting
a patient with prenatally diagnosed disorder/difference of sex
development (DSD) with heterozygous LHCGR mutations. Urol Case Rep.
41(101971)2021.PubMed/NCBI View Article : Google Scholar
|
|
159
|
Alfei E, Cattaneo E, Spaccini L, Iascone
M, Veggiotti P and Doneda C: Progressive clinical and
neuroradiological findings in a child with BCL11B missense
mutation: Expanding the phenotypic spectrum of related disorder.
Neuropediatrics. 53:283–286. 2022.PubMed/NCBI View Article : Google Scholar
|
|
160
|
Li M, Che F, Qiu S and Wang Z:
Identification of a novel variant of SRD5A2 gene in a child
featuring steroid 5α-reductase type 2 deficiency. Zhonghua Yi Xue
Yi Chuan Xue Za Zhi. 38:1233–1236. 2021.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
161
|
Strong A, March ME, Cardinale CJ, Kim SE,
Merves J, Whitworth H, Raffini L, Larosa C, Copelovitch L, Hou C,
et al: A novel MBTPS2 variant associated with BRESHECK syndrome
impairs sterol-regulated transcription and the endoplasmic
reticulum stress response. Am J Med Genet A. 188:463–472.
2022.PubMed/NCBI View Article : Google Scholar
|
|
162
|
Arsov T, Kelecic J, Frkovic SH, Sestan M,
Kifer N, Andrews D, Adamski M, Jelusic M and Cook MC: Expanding the
clinical spectrum of pathogenic variation in NR2F2: Asplenia. Eur J
Med Genet. 64(104347)2021.PubMed/NCBI View Article : Google Scholar
|
|
163
|
Thomas MM, Ashaat EA, Otaify GA, Ismail S,
Essawi ML, Abdel-Hamid MS, Hassan HA, Alsaiedi SA, Aglan M, El Ruby
MO and Temtamy S: First report of two egyptian patients with
desbuquois dysplasia due to homozygous CANT1 mutations. Mol
Syndromol. 12:279–288. 2021.PubMed/NCBI View Article : Google Scholar
|
|
164
|
Bouhouche A, Albaroudi N, El Alaoui MA,
Askander O, Habbadi Z, El Hassani A, Iraqi H, El Fahime E and
Belmekki M: Identification of the novel SDR42E1 gene that affects
steroid biosynthesis associated with the oculocutaneous genital
syndrome. Exp Eye Res. 209(108671)2021.PubMed/NCBI View Article : Google Scholar
|
|
165
|
Luo Q, Zhang Q, Shen J, Guan W, Li M,
Zhang J and Tan Z: Expanding mutational spectrum of HRAS by a
patient with schimmelpenning-feuerstein-mims syndrome. J Dermatol.
48:1273–1276. 2021.PubMed/NCBI View Article : Google Scholar
|
|
166
|
Akramov NR, Shavaliev RF and Osipova IV:
.: New mutation in WT1 gene in a boy with an incomplete form of
Denys-Drash syndrome: A CARE-compliant case report. Medicine
(Baltimore). 100(e25864)2021.PubMed/NCBI View Article : Google Scholar
|
|
167
|
Elghezal H, Alfayez K, Ben Abdallah I,
Alfares A, Almazyad A, Al Jasser A, Almobadel N, Alsuhaibani O and
Alhashem A: Hypospadias in ring X syndrome. Eur J Med Genet.
64(104225)2021.PubMed/NCBI View Article : Google Scholar
|
|
168
|
Ravirajendran S, Palaniyandi V, Arora A,
Ramanan V and Kumaresan N: Mullerian remnants presenting as a
pelvic cyst in a young adult with 45X0/46XY mixed gonadal
dysgenesis. Urol Ann. 13:76–79. 2021.PubMed/NCBI View Article : Google Scholar
|
|
169
|
Correya M, Babu R, Archana B and
Ravirajendiran S: Disorders of sexual differentiation: Report of
two rare cases. Indian J Pathol Microbiol. 64:390–393.
2021.PubMed/NCBI View Article : Google Scholar
|
|
170
|
Chen L, Huang H, Zhang H, Zhu G and Zhu M:
Three cases of 3β-hydroxysteroid dehydrogenase deficiency: Clinical
analysis. Adv Clin Exp Med. 30:289–299. 2021.PubMed/NCBI View Article : Google Scholar
|
|
171
|
Saida K, Fukuda T, Scott DA, Sengoku T,
Ogata K, Nicosia A, Hernandez-Garcia A, Lalani SR, Azamian MS,
Streff H, et al: OTUD5 variants associated with X-linked
intellectual disability and congenital malformation. Front Cell Dev
Biol. 9(631428)2021.PubMed/NCBI View Article : Google Scholar
|
|
172
|
Çiftci N, Kayaş L, Çamtosun E and Akıncı
A: 46,XY sex development defect due to a novel homozygous (splice
site) c.673_1G>C variation in the HSD17B3 gene: Case report. J
Clin Res Pediatr Endocrinol. 14:233–238. 2022.PubMed/NCBI View Article : Google Scholar
|
|
173
|
Laan M, Kasak L, Timinskas K, Grigorova M,
Venclovas Č, Renaux A, Lenaerts T and Punab M: NR5A1 c.991-1G>C
splice-site variant causes familial 46,XY partial gonadal
dysgenesis with incomplete penetrance. Clin Endocrinol (Oxf).
94:656–666. 2021.PubMed/NCBI View Article : Google Scholar
|
|
174
|
Gerber JA, Sheth KR and Austin PF: Robinow
syndrome: Genital analysis, genetic heterogeneity, and associated
psychological impact. Am J Med Genet A. 185:3601–3605.
2021.PubMed/NCBI View Article : Google Scholar
|
|
175
|
Sheppard SE, Barrett B, Muraresku C,
McKnight H, De Leon DD, Lord K and Ganetzky R: Heterozygous
recurrent HNF4A variant p.Arg85Trp causes Fanconi renotubular
syndrome 4 with maturity onset diabetes of the young, an autosomal
dominant phenocopy of Fanconi Bickel syndrome with colobomas. Am J
Med Genet A. 185:566–570. 2021.PubMed/NCBI View Article : Google Scholar
|
|
176
|
Tripolszki K, Sasaki E, Hotakainen R,
Kassim AH, Pereira C, Rolfs A, Bauer P, Reardon W and
Bertoli-Avella AM: An X-linked syndrome with severe
neurodevelopmental delay, hydrocephalus, and early lethality caused
by a missense variation in the OTUD5 gene. Clin Genet. 99:303–308.
2021.PubMed/NCBI View Article : Google Scholar
|
|
177
|
Hage M, Drui D, Francou B, Mercier S,
Guiochon-Mantel A, Belaisch-Allart J, Péréon Y, Cazabat L, De
Mazancourt P and Raffin-Sanson ML: Structural analysis of the
impact of a novel androgen receptor gene mutation in two adult
patients with mild androgen insensitivity syndrome. Andrologia.
53(e13865)2021.PubMed/NCBI View Article : Google Scholar
|
|
178
|
Basa M, Vukovic R, Sarajlija A, Milenkovic
T, Djordjevic M, Vucetic B and Martic J: Ambiguous genitalia and
lissencephaly in A 46,XY neonate with a novel variant of aristaless
gene. Acta Endocrinol (Buchar). 17:402–405. 2021.PubMed/NCBI View Article : Google Scholar
|
|
179
|
Kherouatou-Chaoui N, Chellat-Rezgoune D,
Rezgoune ML, Mc Elreavey K, Touabti LS, Abadi N and Satta D: SRY
and NR5A1 gene mutation in Algerian children and adolescents with
DSD and testicular dysgenesis. Afr Health Sci. 21:1491–1497.
2021.PubMed/NCBI View Article : Google Scholar
|
|
180
|
Chen J, Cui X, Li A, Li G and Sun F:
Association of a GATA binding protein 4 polymorphism with the risk
of hypospadias in the Chinese children. Urol Int. 105:1018–1023.
2021.PubMed/NCBI View Article : Google Scholar
|
|
181
|
Wong YS, Pang KKY and Tam YH: Surgery in
Chinese children affected by 45,X/46,XY disorders of sex
development: A 20-year experience in a single center. J Pediatr
Surg. 57:1398–1403. 2022.PubMed/NCBI View Article : Google Scholar
|
|
182
|
Deng F, Zhao J, Jia W, Fu K, Zuo X, Huang
L, Wang N, Xia H, Zhang Y, Fu W and Liu G: Increased hypospadias
risk by GREM1 rs3743104[G] in the southern Han Chinese population.
Aging (Albany NY). 13:13898–13908. 2021.PubMed/NCBI View Article : Google Scholar
|
|
183
|
Siregar S, Sibarani J, Noegroho BS,
Firmansyah I and Maskoen AM: Polymorphism of PvuII, Xba1, and SNP
12 estrogen receptor 1 (ESR1) in hipospadias patients at tertiary
hospital center. Res Rep Urol. 13:105–110. 2021.PubMed/NCBI View Article : Google Scholar
|
|
184
|
Saraç M, Canpolat Ş, Önalan Etem E,
Tektemur A, Tartar T, Bakal U and Kazez A: The role of sonic
hedgehog homologue signal pathway in hypospadias aetiology. J
Pediatr Urol. 17:630.e1–630.e7. 2021.PubMed/NCBI View Article : Google Scholar
|
|
185
|
Tenenbaum-Rakover Y, Admoni O, Elias-Assad
G, London S, Noufi-Barhoum M, Ludar H, Almagor T, Zehavi Y, Sultan
C, Bertalan R, et al: The evolving role of whole-exome sequencing
in the management of disorders of sex development. Endocr Connect.
10:620–629. 2021.PubMed/NCBI View Article : Google Scholar
|
|
186
|
Ea V, Bergougnoux A, Philibert P,
Servant-Fauconnet N, Faure A, Breaud J, Gaspari L, Sultan C, Paris
F and Kalfa N: How far should we explore hypospadias?
Next-generation sequencing applied to a large cohort of hypospadiac
patients. Eur Urol. 79:507–515. 2021.PubMed/NCBI View Article : Google Scholar
|
|
187
|
Schmidt J, Schreiber G, Altmüller J,
Thiele H, Nürnberg P, Li Y, Kaulfuß S, Funke R, Wilken B, Yigit G
and Wollnik B: Familial cleft tongue caused by a unique translation
initiation codon variant in TP63. Eur J Hum Genet. 30:211–218.
2022.PubMed/NCBI View Article : Google Scholar
|
|
188
|
Ding Y, Cao BY, Su C, Liu M, Chen JJ, Fan
LJ and Gong CX: Clinical and genetic analysis of Noonan syndrome in
20 children. Zhonghua Er Ke Za Zhi. 59:588–593. 2021.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
189
|
Lourenço CSFP, Carriço AL and Valente
FMDS: Prenatal diagnosis of aberrant right subclavian artery:
Association with genetic abnormalities. Rev Bras Ginecol Obstet.
43:452–456. 2021.PubMed/NCBI View Article : Google Scholar
|
|
190
|
Konishi A, Ida S, Matsui F, Etani Y and
Kawai M: Male assignment in 5α-reductase type 2 deficiency with
female external genitalia. Pediatr Int. 63:592–594. 2021.PubMed/NCBI View Article : Google Scholar
|
|
191
|
Rjiba K, Ayech H, Kraiem O, Slimani W,
Jelloul A, Ben Hadj Hmida I, Mahdhaoui N, Saad A and Mougou-Zerelli
S: Disorders of sex development in Wolf-Hirschhorn syndrome: A
genotype-phenotype correlation and MSX1 as candidate gene. Mol
Cytogenet. 14(12)2021.PubMed/NCBI View Article : Google Scholar
|
|
192
|
Yuri P, Gunadi Lestari RP, Fardilla FP and
Dachlan I: Expression of mRNA vascular endothelial growth factor in
hypospadias patients. BMC Urol. 21(163)2021.PubMed/NCBI View Article : Google Scholar
|
|
193
|
Kong X, Luo J, Xiang H, Wang S, Shen L,
Long C, Liu F, Lin T, He D, Liu X and Wei GH: Expression of Mafb is
down-regulated in the foreskin of children with hypospadias. J
Pediatr Urol. 17:70.e1–70.e6. 2021.PubMed/NCBI View Article : Google Scholar
|
|
194
|
Spinder N, Bergman JEH, van Tongeren M,
Boezen HM, Kromhout H and de Walle HEK: Maternal occupational
exposure to endocrine-disrupting chemicals and urogenital anomalies
in the offspring. Hum Reprod. 37:142–151. 2021.PubMed/NCBI View Article : Google Scholar
|
|
195
|
Rodprasert W, Toppari J and Virtanen HE:
Endocrine disrupting chemicals and reproductive health in boys and
men. Front Endocrinol (Lausanne). 12(706532)2021.PubMed/NCBI View Article : Google Scholar
|
|
196
|
Mattiske DM and Pask AJ: Endocrine
disrupting chemicals in the pathogenesis of hypospadias;
developmental and toxicological perspectives. Curr Res Toxicol.
2:179–191. 2021.PubMed/NCBI View Article : Google Scholar
|
|
197
|
Laws MJ, Neff AM, Brehm E, Warner GR and
Flaws JA: Endocrine disrupting chemicals and reproductive disorders
in women, men, and animal models. Adv Pharmacol. 92:151–190.
2021.PubMed/NCBI View Article : Google Scholar
|
|
198
|
Stukenborg JB, Mitchell RT and Söder O:
Endocrine disruptors and the male reproductive system. Best Pract
Res Clin Endocrinol Metab. 35(101567)2021.PubMed/NCBI View Article : Google Scholar
|
|
199
|
Schiesaro MG, Amato AML, Maneschi C,
Sciabica V, Pigatto E and Sanna M: The male reproductive system and
endocrine disruptors. Endocr Metab Immune Disord Drug Targets.
22:686–703. 2022.PubMed/NCBI View Article : Google Scholar
|
|
200
|
Wu Y, Wang J, Wei Y, Chen J, Kang L, Long
C, Wu S, Shen L and Wei G: Contribution of prenatal
endocrine-disrupting chemical exposure to genital anomalies in
males: The pooled results from current evidence. Chemosphere.
286(131844)2022.PubMed/NCBI View Article : Google Scholar
|
|
201
|
Gaspari L, Tessier B, Paris F, Bergougnoux
A, Hamamah S, Sultan C and Kalfa N: endocrine-disrupting chemicals
and disorders of penile development in humans. Sex Dev. 15:213–228.
2021.PubMed/NCBI View Article : Google Scholar
|
|
202
|
Huang X, Chen J, Zeng D, Lin Z, Herbert C,
Cottrell L, Liu L, Ash A and Wang B: The association between
ambient air pollution and birth defects in five major ethnic groups
in Liuzhou, China. BMC Pediatr. 21(232)2021.PubMed/NCBI View Article : Google Scholar
|
|
203
|
Xing Z, Zhang S, Jiang YT, Wang XX and Cui
H: Association between prenatal air pollution exposure and risk of
hypospadias in offspring: A systematic review and meta-analysis of
observational studies. Aging (Albany NY). 13:8865–8879.
2021.PubMed/NCBI View Article : Google Scholar
|
|
204
|
Bougnères P, Porcher R, Esterle L, Baker
D, de la Vaissière A, Meurisse S, Valtat S, Castell AL, Mouriquand
P and Valleron AJ: Exploring the risk of hypospadias in children
born from mothers living close to a vineyard. PLoS One.
16(e0249800)2021.PubMed/NCBI View Article : Google Scholar
|
|
205
|
Mesquita I, Lorigo M and Cairrao E: Update
about the disrupting-effects of phthalates on the human
reproductive system. Mol Reprod Dev. 88:650–672. 2021.PubMed/NCBI View Article : Google Scholar
|
|
206
|
Soyer-Gobillard MO, Gaspari L, Paris F,
Kalfa N, Hamamah S, Courtet P and Sultan C: Prenatal exposure to
diethylstilbestrol and multigenerational psychiatric disorders: An
informative family. Int J Environ Res Public Health.
18(9965)2021.PubMed/NCBI View Article : Google Scholar
|
|
207
|
Zhang ZC, Liu X, Wei C, Luo J, Shi Y, Lin
T, He D and Wei G: Assisted reproductive technologies and the risk
of congenital urogenital tract malformations: A systematic review
and meta-analysis. J Pediatr Urol. 17:9–20. 2021.PubMed/NCBI View Article : Google Scholar
|
|
208
|
Zhang S, Yue DM, Zhang JY, Huang YH, Li J,
Liu S, Chen YL, Li LL, Jiang CZ, Chen ZJ, et al: Maternal exposure
to sulfur dioxide before and after conception and the risk of
hypospadias in offspring. Ann N Y Acad Sci. 1502:99–109.
2021.PubMed/NCBI View Article : Google Scholar
|
|
209
|
Rouget F, Bihannic A, Cordier S, Multigner
L, Meyer-Monath M, Mercier F, Pladys P and Garlantezec R: Petroleum
and chlorinated solvents in meconium and the risk of hypospadias: A
pilot study. Front Pediatr. 9(640064)2021.PubMed/NCBI View Article : Google Scholar
|
|
210
|
Haghighi MM, Wright CY, Ayer J, Urban MF,
Pham MD, Boeckmann M, Areal A, Wernecke B, Swift CP, Robinson M, et
al: Impacts of high environmental temperatures on congenital
anomalies: A systematic review. Int J Environ Res Public Health.
18(4910)2021.PubMed/NCBI View Article : Google Scholar
|
|
211
|
Gadagbui BK, York RG, Dourson ML, McGinnis
PM and Cope RB: Analysis for data-derived extrapolation factors for
procymidone. Regul Toxicol Pharmacol. 124(104972)2021.PubMed/NCBI View Article : Google Scholar
|
|
212
|
Lin HC, Guo JM, Ge P and Ou P: Association
between prenatal exposure to ambient particulate matter and risk of
hypospadias in offspring: A systematic review and meta-analysis.
Environ Res. 192(110190)2021.PubMed/NCBI View Article : Google Scholar
|
|
213
|
Akay MA and Yıldız GE: Impact of
gestational and parental factors and maternal intake of
progesterone on the development of hypospadias: A retrospective
case-control study. Taiwan J Obstet Gynecol. 60:894–898.
2021.PubMed/NCBI View Article : Google Scholar
|
|
214
|
Chung EH, Harris BS, Muasher SJ and Kuller
JA: The risk of congenital anomalies by fertility treatment
modality. Obstet Gynecol Surv. 76:37–47. 2021.PubMed/NCBI View Article : Google Scholar
|
|
215
|
Baskin L, Sinclair A, Derpinghaus A, Cao
M, Li Y, Overland M, Aksel S and Cunha GR: Estrogens and
development of the mouse and human external genitalia.
Differentiation. 118:82–106. 2021.PubMed/NCBI View Article : Google Scholar
|
|
216
|
Wu Y, Yao J wei, Xu L jie, Chen M and Wan
L: Risk of congenital malformations in offspring of women using
β-blockers during early pregnancy: An updated meta-analysis of
observational studies. Br J Clin Pharmacol. 87:806–815.
2021.PubMed/NCBI View Article : Google Scholar
|
|
217
|
Schraw JM, Langlois PH and Lupo PJ:
Comprehensive assessment of the associations between maternal
diabetes and structural birth defects in offspring: A phenome-wide
association study. Ann Epidemiol. 53:14–20.e8. 2021.PubMed/NCBI View Article : Google Scholar
|
|
218
|
Liu Y, Fan L, Wang X and Gong C: Exploring
the efficacy of testosterone undecanoate in male children with
5α-reductase deficiency. Pediatr Investig. 5:249–254.
2021.PubMed/NCBI View Article : Google Scholar
|
|
219
|
Li B, Kong I, McGrath M, Farrokhyar F and
Braga LH: Evaluating the literature on preoperative androgen
stimulation for hypospadias repair using the fragility index-can we
trust observational studies? J Pediatr Urol. 17:661–669.
2021.PubMed/NCBI View Article : Google Scholar
|
|
220
|
Concepción-Zavaleta MJ, García-Villasante
EJ, Zavaleta-Gutiérrez FE, Barrantes Ticlla JL and Massucco
Revoredo FG: Late diagnosis of partial androgen insensitivity
syndrome in a peruvian child. Cureus. 13(e16565)2021.PubMed/NCBI View Article : Google Scholar
|
|
221
|
Khokar DS and Patel RV: Can testosterone
alter the degree of hypospadias? A comprehensive study. J Indian
Assoc Pediatr Surg. 26:38–43. 2021.PubMed/NCBI View Article : Google Scholar
|
|
222
|
Chukwubuike KE: Single dose of
testosterone in children with hypospadias: Any effect on the
diameter of the glans penis? Afr J Urol. 27(34)2021.
|
|
223
|
D'Oro A, Rosoklija I, Yerkes EB, Lindgren
BW, Rychlik K and Cheng EY: Proximal hypospadias and acquired
cryptorchidism: Incidence, morphology and potential clinical
implications. J Urol. 206:1291–1299. 2021.PubMed/NCBI View Article : Google Scholar
|
|
224
|
Ludorf KL, Benjamin RH, Navarro Sanchez
ML, McLean SD, Northrup H, Mitchell LE, Langlois PH, Canfield MA,
Scheuerle AE, Scott DA, et al: Patterns of co-occurring birth
defects among infants with hypospadias. J Pediatr Urol.
17:64.e1–64.e8. 2021.PubMed/NCBI View Article : Google Scholar
|
|
225
|
Fuchs ME, Halleran DR, Bourgeois T,
Sebastião Y, Weaver L, Farrell N, Vilanova-Sánchez A, Gasior A,
Halaweish I, Jayanthi VR, et al: Correlation of anorectal
malformation complexity and associated urologic abnormalities. J
Pediatr Surg. 56:1988–1992. 2021.PubMed/NCBI View Article : Google Scholar
|
|
226
|
de Jesus Escano MR, Mejia Sang ME,
Reyes-Mugica M, Colaco M and Fox J: Ovotesticular disorder of sex
development: Approach and management of an index case in the
dominican republic. Cureus. 13(e18512)2021.PubMed/NCBI View Article : Google Scholar
|
|
227
|
Nelwan D, Mount C, Morganstern B and Chan
JT: Infant with severe penoscrotal hypospadias: A complex case of
genital ambiguity and mistaken identity. Cureus.
13(e15191)2021.PubMed/NCBI View Article : Google Scholar
|
|
228
|
Ashfaq S, Siddiqui A, Shafiq W and Azmat
U: A rare presentation of disorder of sex development. Cureus.
13(e12782)2021.PubMed/NCBI View Article : Google Scholar
|
|
229
|
Rittler M, Campaña H, Heisecke S,
Ratowiecki J, Elias D, Gimenez L, Poletta FA, Gili J, Pawluk M,
Santos MR, et al: Lethality of birth defects in live born infants
categorized by gestational age and birth weight. Am J Perinatol:
Oct 11, 2021 (Epub ahead of print).
|
|
230
|
Álvarez-Álvarez A, Costa-Romero M, Suárez
Saavedra S, Rial JC, Lois Bermejo AM, García González N and
Fernández-Rodríguez H: Dandy-Walker malformation associated with
extracranial abnormalities in a newborn. Arch Argent Pediatr.
119:e526–e530. 2021.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
231
|
Viet Nguyen H, Hong Vu T, Quy Hong Q,
Quang Pham H and Bich Nguyen N: Hypospadias associated with partial
bifid phallus: A case report. Urol Case Rep.
39(101840)2021.PubMed/NCBI View Article : Google Scholar
|
|
232
|
Çelik G, Batu Oto B, Kızılay O,
Kılıçarslan O and Toptan HH: An unusual ophthalmic presentation of
Wolf-Hirschhorn syndrome. Ophthalmic Genet. 42:326–328.
2021.PubMed/NCBI View Article : Google Scholar
|
|
233
|
Bhatia VP, Mittal AG, Austin PF and
Hilliard ME: The hypospadias-specific health-related quality of
life conceptual framework: A scoping review of the literature. Qual
Life Res. 30:1537–1546. 2021.PubMed/NCBI View Article : Google Scholar
|
|
234
|
Hoare DT, Bekkema J and Rourke KF:
Prospective assessment of patient-perceived short-term changes in
penile appearance after urethroplasty. Urology. 158:222–227.
2021.PubMed/NCBI View Article : Google Scholar
|
|
235
|
Bhatia VP, Hilliard ME, Austin PF and
Mittal AG: Evaluating quality of patient-reported outcome measures
in patients with hypospadias. J Pediatr Urol. 17:50–58.
2021.PubMed/NCBI View Article : Google Scholar
|
|
236
|
Chang C, Reifsnyder JE, Fahmy AG and Hanna
MK: The adolescent glans penis: Functional and aesthetic issues
following childhood hypospadias repair. J Pediatr Urol.
17:609.e1–609.e8. 2021.PubMed/NCBI View Article : Google Scholar
|
|
237
|
Sinatti C, Schechter MY, Spinoit AF and
Hoebeke P: Long-term outcome of urethral and genital reconstruction
in hypospadias and exstrophy-epispadias complex. Curr Opin Urol.
31:480–485. 2021.PubMed/NCBI View Article : Google Scholar
|
|
238
|
Calleja Hermosa P, Campos-Juanatey F,
Varea Malo R, Correas Gómez MÁ and Gutiérrez Baños JL: Trauma and
Reconstructive Urology Working Party of the European Association of
Urology Young Academic Urologists. Sexual function after anterior
urethroplasty: A systematic review. Transl Androl Urol.
10:2554–2573. 2021.PubMed/NCBI View Article : Google Scholar
|
|
239
|
Mallenahalli S, Fang AH, Tong CMC and
Dangle PP: A review of literature on long-term outcomes of proximal
hypospadias-urinary, sexual, and psychosocial. Curr Sex Health Rep.
13:38–44. 2021.
|
|
240
|
Zhang ZC, Liu X, Chen HS, Shi Y, Lin T, He
DW, Wei GH and Luo YT: Analysis of the social and clinical factors
affecting the age of children when receiving surgery for
hypospadias: A retrospective study of 1611 cases in a single
center. Asian J Androl. 23:527–531. 2021.PubMed/NCBI View Article : Google Scholar
|
|
241
|
Bennecke E, Bernstein S, Lee P, van de
Grift TC, Nordenskjöld A, Rapp M, Simmonds M, Streuli JC, Thyen U
and Wiesemann C: dsd-LIFE Group. Early genital surgery in
disorders/differences of sex development: Patients' perspectives.
Arch Sex Behav. 50:913–923. 2021.PubMed/NCBI View Article : Google Scholar
|
|
242
|
Bangalore Krishna K, Kogan BA, Mazur T,
Hoebeke P, Bogaert G and Lee PA: Individualized care for patients
with intersex (differences of sex development): Part
4/5.considering the ifs, whens, and whats regarding
sexual-reproductive system surgery. J Pediatr Urol. 17:338–345.
2021.PubMed/NCBI View Article : Google Scholar
|
|
243
|
Cakmak M, Gollu G, Ates U, Ergun E,
Khanmammadov F, Sozduyar S, Telli O, Kose K, Dilsiz H, Cakmak A, et
al: Hypospadias and the use of the ages and stages questionnaire to
evaluate neurodevelopmental status of boys with hypospadias. Eur J
Pediatr Surg. 32:274–279. 2022.PubMed/NCBI View Article : Google Scholar
|
|
244
|
van de Grift TC, Rapp M, Holmdahl G,
Duranteau L and Nordenskjold A: dsd-LIFE group. Masculinizing
surgery in disorders/differences of sex development: Clinician- and
participant-evaluated appearance and function. BJU Int.
129:394–405. 2022.PubMed/NCBI View Article : Google Scholar
|
|
245
|
Gul M, Hildorf S and Silay MS: Sexual
functions and fertility outcomes after hypospadias repair. Int J
Impot Res. 33:149–163. 2021.PubMed/NCBI View Article : Google Scholar
|
|
246
|
Guner E and Kadioglu A: Specific
urogenital disease information-revealing male genital votive
offerings dedicated to gods in ancient age sanctuary medicine. Arch
Esp Urol. 74:239–246. 2021.PubMed/NCBI(In English, Spanish).
|
|
247
|
Buyukunal C, Zeller KA, Emre S and
Nakayama DK: The history of surgery in disorders of sexual
development. J Pediatr Surg. 56:429–433. 2021.PubMed/NCBI View Article : Google Scholar
|
|
248
|
Baker Z, Bhaskar N, Herbst KW, Hagadorn JI
and Kokorowski P: Sample size, power, and risk of misclassification
in pediatric urology hospital rankings. J Urol. 206:436–446.
2021.PubMed/NCBI View Article : Google Scholar
|
|
249
|
Maier M, Ebert AK, Baunacke M, Groeben C,
Eisenmenger N, Thomas C and Huber J: Health care reality of
selected pediatric urologic surgeries in Germany from 2006 to 2019.
Urologe A. 60:1291–1303. 2021.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
250
|
Scarberry KA, Gor RA and Kovell RC:
Management of the transitional urology patient: The role of the
adult reconstructive urologist. Curr Urol Rep.
22(15)2021.PubMed/NCBI View Article : Google Scholar
|
|
251
|
Mahalik S, Pati A and Das K: Awareness of
common pediatric surgical entities among practicing indian
pediatricians. J Indian Assoc Pediatr Surg. 26:89–93.
2021.PubMed/NCBI View Article : Google Scholar
|
|
252
|
Kharbanda EO, Vazquez-Benitez G, DeSilva
MB, Spaulding AB, Daley MF, Naleway AL, Irving SA, Klein NP, Tseng
HF, Jackson LA, et al: Developing algorithms for identifying major
structural birth defects using automated electronic health data.
Pharmacoepidemiol Drug Saf. 30:266–274. 2021.PubMed/NCBI View Article : Google Scholar
|
|
253
|
Wu S, He R, Sun J and Zhao H: Acellular
dermal matrix graft for ventral corporal lengthening orthoplasty in
2-stage proximal hypospadias repair. Transl Pediatr. 10:3151–3158.
2021.PubMed/NCBI View Article : Google Scholar
|
|
254
|
Singh A, Anand S, Goel P, Yadav DK and
Bajpai M: Can sealing promote healing?: A systematic review and
meta-analysis highlighting the adjunctive role of tissue sealant
application during urethroplasty for hypospadias. J Pediatr Urol.
17:805–812. 2021.PubMed/NCBI View Article : Google Scholar
|
|
255
|
Wang Y, Wang G, Hou X, Zhao Y, Chen B, Dai
J and Sun N: Urethral tissue reconstruction using the acellular
dermal matrix patch modified with collagen-binding VEGF in beagle
urethral injury models. Biomed Res Int.
2021(5502740)2021.PubMed/NCBI View Article : Google Scholar
|
|
256
|
Morgante D, Radford A, Abbas SK, Ingham E,
Subramaniam R and Southgate J: Augmentation of the insufficient
tissue bed for surgical repair of hypospadias using acellular
matrix grafts: A proof of concept study. J Tissue Eng.
12(2041731421998840)2021.PubMed/NCBI View Article : Google Scholar
|
|
257
|
Tawfeek AM, Mohareb AM, Higazy A, Farouk
A, Elsaeed KO, Tawfick A and Radwan A: Isoamyl 2-cyanoacrylate
interposition in the urethro-cutaneous fistula repair: A randomized
controlled trial. Afr J Urol. 27(94)2021.
|
|
258
|
Shenoy NS, Tiwari C, Gandhi S, Kumbhar V,
Joseph V, Basu S, Makan A and Shah H: Efficacy of fibrin sealant as
waterproof cover in improving outcome in hypospadias surgery. Afr J
Paediatr Surg. 18:215–218. 2021.PubMed/NCBI View Article : Google Scholar
|
|
259
|
Abbas TO, Elawad A, Kareem A, Pullattayil
S AK, Ali M and Alnaimi A: Preclinical experiments for hypospadias
surgery: Systematic review and quality assessment. Front Pediatr.
9(718647)2021.PubMed/NCBI View Article : Google Scholar
|
|
260
|
Amesty MV, Chamorro CI, López-Pereira P,
Martínez-Urrutia MJ, Sanz B, Rivas S, Lobato R and Fossum M:
Creation of tissue-engineered urethras for large urethral defect
repair in a rabbit experimental model. Front Pediatr.
9(691131)2021.PubMed/NCBI View Article : Google Scholar
|
|
261
|
Palermo CM, Foreman JE, Wikoff DS and Lea
I: Development of a putative adverse outcome pathway network for
male rat reproductive tract abnormalities with specific
considerations for the androgen sensitive window of development.
Curr Res Toxicol. 2:254–271. 2021.PubMed/NCBI View Article : Google Scholar
|
|
262
|
Alcantara MC, Suzuki K, Acebedo AR,
Sakamoto Y, Nishita M, Minami Y, Kikuchi A and Yamada G:
Stage-dependent function of Wnt5a during male external genitalia
development. Congenit Anom (Kyoto). 61:212–219. 2021.PubMed/NCBI View Article : Google Scholar
|
|
263
|
Xiang H, Wang S, Kong X, Yu Y, Shen L,
Long C, Liu X and Wei GH: c-Fos is upregulated in the genital
tubercle of DEHP-induced hypospadiac rats and the prepuce of
patients with hypospadias. Syst Biol Reprod Med. 67:193–200.
2021.PubMed/NCBI View Article : Google Scholar
|
|
264
|
Feng X, Huang E, Gao Y, Zhang Y and Zhou
Y: The effects of NONRATT008453.2 on autophagy in genital tubercle
fibroblasts of rats with hypospadias induced by dibutyl phthalate.
Birth Defects Res. 113:399–408. 2021.PubMed/NCBI View Article : Google Scholar
|
|
265
|
Yu H, Yang J, Zhang Y, Fu H, Yan Z and Zhu
Y: Vinclozolin-induced mouse penile malformation and ‘small testis’
via miR132, miR195a together with the Hippo signaling pathway.
Toxicology. 460(152842)2021.PubMed/NCBI View Article : Google Scholar
|
|
266
|
Abbas TO, Elawad A, Pullattayil S AK and
Pennisi CP: Quality of reporting in preclinical urethral tissue
engineering studies: A systematic review to assess adherence to the
ARRIVE guidelines. Animals (Basel). 11(2456)2021.PubMed/NCBI View Article : Google Scholar
|
|
267
|
Tan H, Wu G, Wang S, Lawless J, Sinn A,
Chen D and Zheng Z: Prenatal exposure to atrazine induces
cryptorchidism and hypospadias in F1 male mouse offspring. Birth
Defects Res. 113:469–484. 2021.PubMed/NCBI View Article : Google Scholar
|
|
268
|
Tokat E, Yildiz Y, Eser PE, Kilinc MF and
Doluoglu OG: Does intraurethral erythropoietin administration
effect wound healing after hypospadias correction? An experimental
rat study. Int Urol Nephrol. 53:2057–2062. 2021.PubMed/NCBI View Article : Google Scholar
|
|
269
|
Gulburun MA, Karabulut R, Turkyilmaz Z,
Eryilmaz S, Kaya C, Arslan B, Gulbahar O, Poyraz A and Sonmez K:
Protective effects of hydrogen rich saline solution on ventral
penile mathieu type flap with penile tourniquet application in
rats. J Pediatr Urol. 17:292.e1–292.e7. 2021.PubMed/NCBI View Article : Google Scholar
|
|
270
|
Fruntelată R, Stoica GA, Ciobanu MO,
Ciurea ME, Nica O and Stoica M: Retrospective study over the
hypospadias surgery in a single tertiary center. Curr Health Sci J.
47:177–183. 2021.PubMed/NCBI View Article : Google Scholar
|
|
271
|
Raheem AA, Banihani O, Abasher A, Alotay
A, Alyami FA, Alsaad TA, Alqarni N, Alsowayan O, Jamalalali YA,
Alhuwaiti M, et al: Pediatric urology surgical practice in the time
of COVID-19: Results from tertiary Saudi Arabia hospitals. Urol
Ann. 13:397–404. 2021.PubMed/NCBI View Article : Google Scholar
|
|
272
|
Jurat R, Rahimi MT and Barolia R: Surgical
outcomes and socio-demographic pattern of hypospadias patients
treated in a tertiary care center in Kabul, Afghanistan. J Pediatr
Urol. 17:674.e1–674.e7. 2021.PubMed/NCBI View Article : Google Scholar
|
|
273
|
Irene M, Osawa F, Kuria K and Lessan J:
Magnitude of post-urethroplasty urinary tract infections in
children with hypospadias at a tertiary hospital in Kenya. J
Pediatr Urol. 17:518.e1–518.e5. 2021.PubMed/NCBI View Article : Google Scholar
|
|
274
|
Khan S, Tafweez R, Haider A and Yaqoob M:
Spectrum of external genital anomalies in disorders of sex
development at children hospital & institute of child health,
Lahore, Pakistan. Pak J Med Sci. 37(244)2021.PubMed/NCBI View Article : Google Scholar
|
|
275
|
Ashwin Shekar P, Ansari MS, Yadav P and
Srivastava A: Presentation, treatment and outcomes of pediatric
anterior urethral strictures: 28 Years' experience from a referral
center. J Pediatr Urol. 17:398.e1–398.e9. 2021.PubMed/NCBI View Article : Google Scholar
|
|
276
|
Wiener JS, Huck N, Blais AS, Rickard M,
Lorenzo A, Di Carlo HNM, Mueller MG and Stein R: Challenges in
pediatric urologic practice: A lifelong view. World J Urol.
39:981–991. 2021.PubMed/NCBI View Article : Google Scholar
|
|
277
|
Ács N, Mátrai Á and Kaposi A: First data
from the new, unified database of the Hungarian case-control
surveillance of congenital abnormalities. J Matern Fetal Neonatal
Med. 34:2887–2892. 2021.PubMed/NCBI View Article : Google Scholar
|
|
278
|
Benavides E, Lupo PJ, Sosa M, Whitworth
KW, Canfield MA, Langlois PH and Schraw JM: Urban-rural residence
and birth defects prevalence in Texas: A phenome-wide association
study. Pediatr Res. 91:1587–1594. 2022.PubMed/NCBI View Article : Google Scholar
|
|
279
|
Arulanandam B, Dorais M, Li P and Poenaru
D: The burden of waiting: Wait times for pediatric surgical
procedures in Quebec and compliance with national benchmarks. Can J
Surg. 64:E14–E22. 2021.PubMed/NCBI View Article : Google Scholar
|
|
280
|
Karabay E, Karsiyakali N, Kayar K and
Koseoglu H: Hypospadias surgery on YouTube: Is it valid? Minerva
Pediatr (Torino). 73:236–242. 2021.PubMed/NCBI View Article : Google Scholar
|
|
281
|
Jones P, Rajasegaran A, Brassale S, Chen
Y, Haslam R, Austin C and Seideman CA: Assessment of the
educational value of distal hypospadias repair videos on YouTube.
Urology. 159:28–32. 2022.PubMed/NCBI View Article : Google Scholar
|
|
282
|
Cheng JW, Fernandez N, Shnorhavorian M,
Merguerian PA and Kieran K: Engagement of common pediatric urologic
conditions on social media. J Pediatr Urol. 18:236.e1–236.e7.
2022.PubMed/NCBI View Article : Google Scholar
|
|
283
|
Ghidini F and Castagnetti M: Pediatric
urology research in 2020: A bibliometric analysis of the top 100
most cited articles. Urologia. 89:474–480. 2022.PubMed/NCBI View Article : Google Scholar
|
|
284
|
Matta R and Schaeffer AJ: The top 100
cited articles in pediatric urology: A bibliometric analysis. J
Pediatr Urol. 17:709.e1–709.e12. 2021.PubMed/NCBI View Article : Google Scholar
|
|
285
|
Doğan G and İpek H: The evolution of
hypospadias publications: A bibliometric approach. Rev Int Androl.
19:224–233. 2021.PubMed/NCBI View Article : Google Scholar
|
|
286
|
Leitao Braga B, Lisboa Gomes N, Nishi MY,
Freire BL, Batista RL, D Faria Junior JA, Funari MFA, Figueredo
Benedetti AF, de Moraes Narcizo A, Cavalca Cardoso L, et al:
Variants in 46,XY DSD-related genes in syndromic and non-syndromic
small for gestational age children with hypospadias. Sex Dev.
16:27–33. 2022.PubMed/NCBI View Article : Google Scholar
|
|
287
|
Niu HL, Yi P, Gao Q, Wang FH, Chen ZR, Li
LP, Xia JQ, Cao Y and Zeng RX: Gonadal neoplastic related lesions
in children with disorders of sexual development: A
clinicopathological study of twelve cases. Zhonghua Bing Li Xue Za
Zhi. 50:1145–1150. 2021.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
288
|
Phillips L, Lundholm C, Örtqvist L,
Almqvist C, Nordenskjöld A and Skarin Nordenvall A: Fertility in
men with hypospadias: A nationwide register-based study using
dizygotic twinning rates as an indicator of semen quality.
Andrology. 9:810–816. 2021.PubMed/NCBI View Article : Google Scholar
|