Introduction
Tuberculum sellae meningioma (TSM) originates from
tuberculum sellae, sphenoid plateau and optic chiasmatic sulcus
(1), accounting for 4-10% of
intracranial meningiomas (2,3).
Generally, the incidence rate of TSM is relatively high in
middle-aged people and women, meanwhile, it is rather rare in
childhood patients (2,3). The growth and expansion of TSM will
compress or surround the optic nerve and optic chiasmatic sulcus,
resulting in the occurrence of corresponding clinical symptoms,
such as varying degrees of vision and visual field disorders,
headache, dizziness and endocrine dysfunction (4). Due to the location of TSM, it is
located in the midline of the skull base and adjacent to numerous
important structures, such as the optic nerve, carotid artery and
anterior cerebral artery, pituitary and pituitary stalk and
hypothalamus (5,6), it increases the risk and challenge of
complete surgical resection of TSM (7,8).
In the past few decades, the traditional
microscope-assisted craniotomy has been the standard method for
surgical resection of TSM, but it requires significant frontal lobe
retraction, removal of the frontal sinus and manipulation of the
optic chiasm, which may cause frontal lobe injury, venous
infarction, infection and even death (9-11).
With the development of endoscope technology, endoscope-assisted
surgery has also been widely used to resect TSM, which has the
advantages of less damage to brain tissue, no obvious traction of
surrounding tissue and can remove bone and dura mate invaded by the
tumor (12,13). In addition, surgical approaches for
resection of TMS include the pterional approach, eyelid approach,
longitudinal fissure approach, supraorbital keyhole approach and
extended transsphenoidal approach, among which supraorbital
approach and extended transsphenoidal approach are the most
recognized and are often compared in terms of characteristics,
contraindications and effects (2,5,10).
The present study retrospectively analyzed 17 cases that used the
endoscopic supraorbital keyhole approach and 19 cases that used the
endoscopic extended transsphenoidal approach for the treatment of
TSM and compared the characteristics of the two surgical approaches
to seek the standard of the preferred surgical approach.
Patients and methods
Patients
A total of 36 cases with TSM treated in Department
of Neurosurgery, Chongqing General Hospital (Chongqing, China)
between April 2014 and August 2020 were analyzed retrospectively,
and the medical records, imaging examination, tumor
characteristics, complications and surgical results were collected.
Inclusion criteria were a complete medical records and follow-up; a
complete set of preoperative and postoperative images; the
diagnosis of a TSM; and detailed video of the surgical procedure.
The exclusion criteria were inflammation in the nasal cavity and
paranasal sinuses; coagulation dysfunction; malignant tumor; and
poor physical condition. There were 4 males and 32 females, ranging
in age from 32-68 years old, with an average mean of 48 years and a
median of 45 years. The main clinical symptom of all patients was a
decreased visual acuity to some extent. The course of the disease
was from 3 months to 6 years. All patients were diagnosed with TSM
by clinical imaging (brain MRI (MAGNETOM Skyra 3.0T) and computed
tomography angiography) and pathological examination.
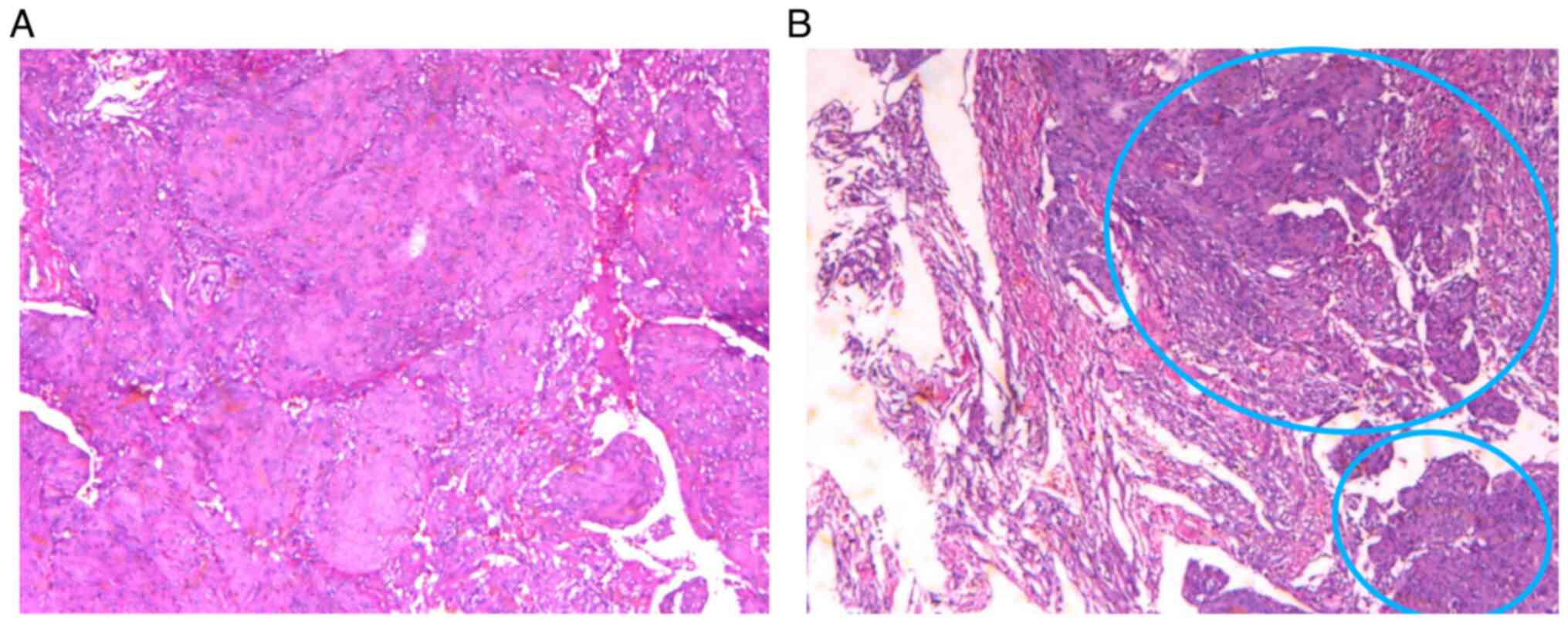
The resected tumor tissue was examined by routine
pathological examination and H&E staining. The tumor samples
were first fixed with 4% formaldehyde solution at room temperature
for 24 h, then embedded and fixed in paraffin. Then cut the
specimen into 4-µm sections and incubated at 60˚C in xylene for 2
h. Then, at room temperature, the sections were stained with 0.5%
hematoxylin for 3 min and then with 0.5% eosin for 3 min. Then, the
stained sections were observed with optical microscope to obtain
histopathological micrographs.
Before the operation, according to the basic
conditions of the patients and the conditions of the tumor,
appropriate surgical approaches were selected by several surgeons
after discussion, resulting in 17 cases utilizing the endoscopic
supraorbital keyhole approach and 19 cases utilizing the endoscopic
extended transsphenoidal approach.
The tumor diameter (d) was calculated using the
formula d=ABC1/3, where A, B and C were the maximum diameter of the
tumor in axial, sagittal and coronal positions on the preoperative
head MRI enhanced scanning image respectively. The maximum diameter
of the tumor in the endoscopic supraorbital keyhole approach group
was 2.8-4.7 cm, with a mean diameter of 3.4 cm, while the maximum
diameter of the tumor in the endoscopic extended transsphenoidal
approach group was 2.4-3.7 cm, with a mean diameter of 2.8 cm. The
resection degree of TSM was divided into gross total resection
(GTR), near total resection (NTR) and subtotal resection (STR)
(14,15). In GTR, the tumor was completely
(100%) resected and the dura at the tumorous contact was resected
under naked eye. In NTR, >90% of tumors were resected when
comparing preoperative and postoperative imaging. In STR, <90%
of tumors were resected when comparing preoperative and
postoperative imaging. The endoscope used was a dedicated
indocyanine green fluorescence integrated endoscope (Karl Storz)
with a diameter of 4-mm and a length of 18-cm, which was coupled to
an IMAGF1 Scamera system (Karl Storz).
Operational methods. Endoscopic
supraorbital keyhole approach
Under general anesthesia, the patient was placed in
a supine position with the head frame fixed, and the head was
tilted back 10-15 and rotated 20 to the opposite side. Through
neuronavigation, the tumor was located and an arc-shaped incision
was made on the eyebrow along the eyebrow arch, with a length of
~4-cm. A milling cutter was used to mill the bone flap with a size
of ~3.5x2.0 cm. The dura mater was incised in an arc along the base
of the skull. Intracranial pressure was reduced by dehydration,
hyperventilation via mechanical ventilation and release of
cerebrospinal fluid. After the intracranial pressure was reduced,
the frontal lobe was gently pulled by the brain pressing plate for
the placement of the endoscope. During the observation, the
endoscope was often held by the left hand (a one-handed operation)
to facilitate the observation of tumors. When it was necessary to
operate with both hands, the endoscope could be fixed on the
endoscope holder, which is convenient for both hands to operate.
Then, the dura mater at the bottom of the tumor was cauterized by
bipolar electrocoagulation, and the tumor and its surrounding
nerves and blood vessels were separated. After fully separating the
tumor and the surrounding adherent tissue, the tumor was removed.
During the operation, the surgeons were careful to avoid the
important nerves and blood vessels surrounding the tumor, such as
the optic nerve, optic chiasm, internal carotid artery and anterior
cerebral artery. After complete hemostasis, hemostatic gauze was
placed in the tumor cavity, and the tumor cavity and the surgical
area were repeatedly washed with normal saline. The dura mater was
closed and sutured, artificial dura mater was used to repair the
dura mater, the bone flap was repositioned and fixed and the dura
mater was sutured in layers.
Endoscopic extended transsphenoidal approach.
After general anesthesia, the patient was placed in a supine
position, with the head tilted back 10-15, the tumor was located
under neuronavigation and the nasal cavity was disinfected.
Subsequently, 0.01% hypertonic norepinephrine saline brain cotton
was used to converge the nasal mucosa in two steps to expand the
surgical channel. A binostril approach was used. Both nasal
cavities were examined by using a 0, 18-cm long, 4-mm diameter
rigid endoscope. The method of holding or fixing the endoscope
during operation was the same as that in the supraorbital keyhole
approach. The right middle turbinate was removed under endoscopy,
then a pedicled nasal septum mucosal flap was prepared and placed
in the posterior nasal canal to be used for skull base repair at
the end of surgery. The endoscope was inserted along the right-side
nasal cavity, the opening of the sphenoid sinus was found and the
mucosa above the opening of the sphenoid sinus was cut. The
sphenoid sinus, the bottom of the saddle and the base of the
anterior skull were drilled with a burr, and a 1.5-2.5
cm2 bone window was opened to expose the dura and
intercavernous sinus. After the dura mater and arachnoid were
opened, the tumor was exposed. Then, the tumor was decompressed,
removed with a curet and tumor forceps and then separated from the
edge. During the operation, the bilateral optic nerve, optic
chiasm, internal carotid artery, anterior communicating artery,
pituitary stalk and pituitary gland needed protection. After
thorough hemostasis, the tumor cavity was first filled with
hemostatic gauze and a gelatin sponge, the double-layer artificial
dura mater was used for repair, the absorbable hemostatic gauze and
gelatin sponge were used for filling and then they are covered
using a pedicled nasal septum mucosal flap. Finally,
chlortetracycline gauze and a double chamber catheter were used to
compress the nasal cavity.
Results
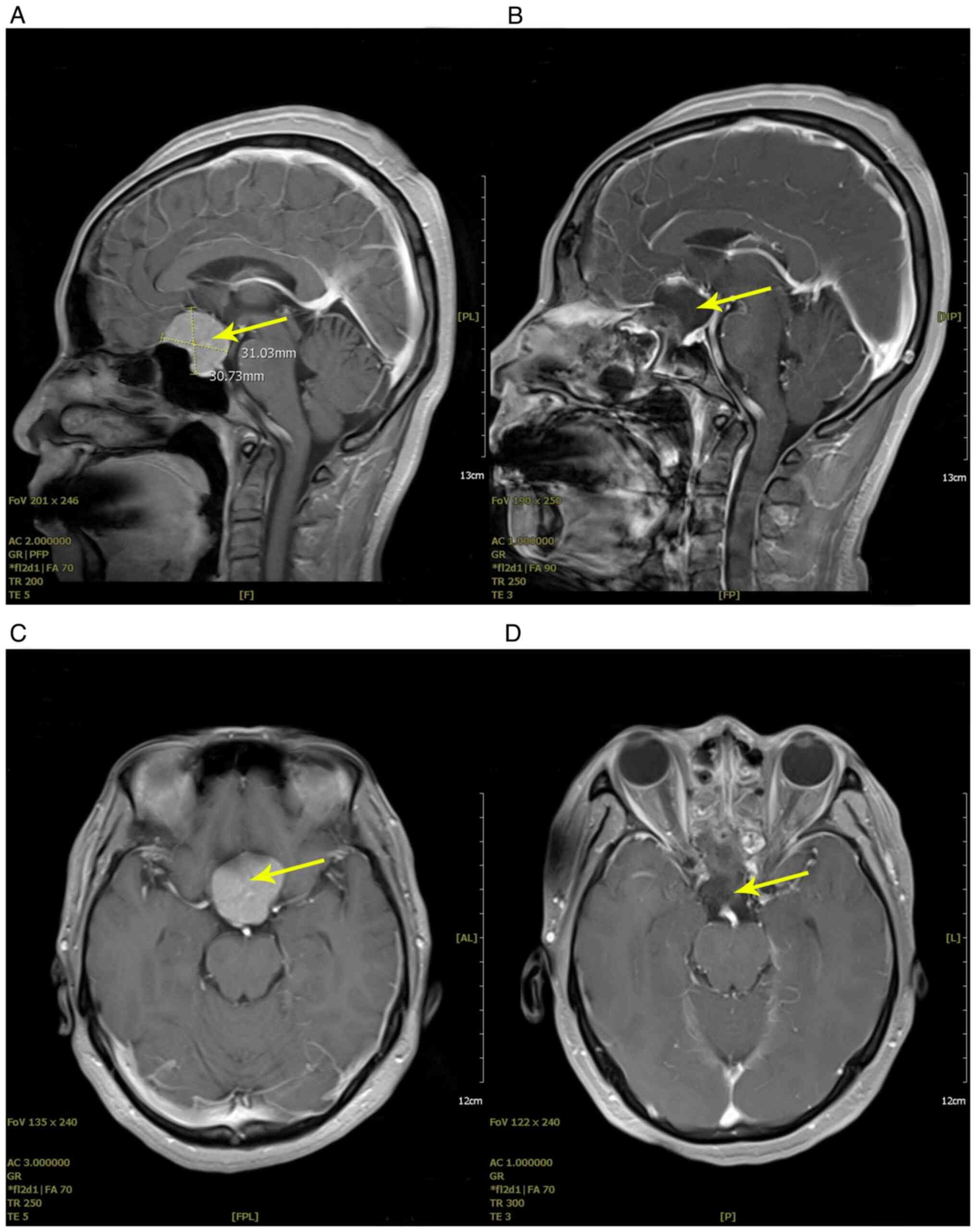
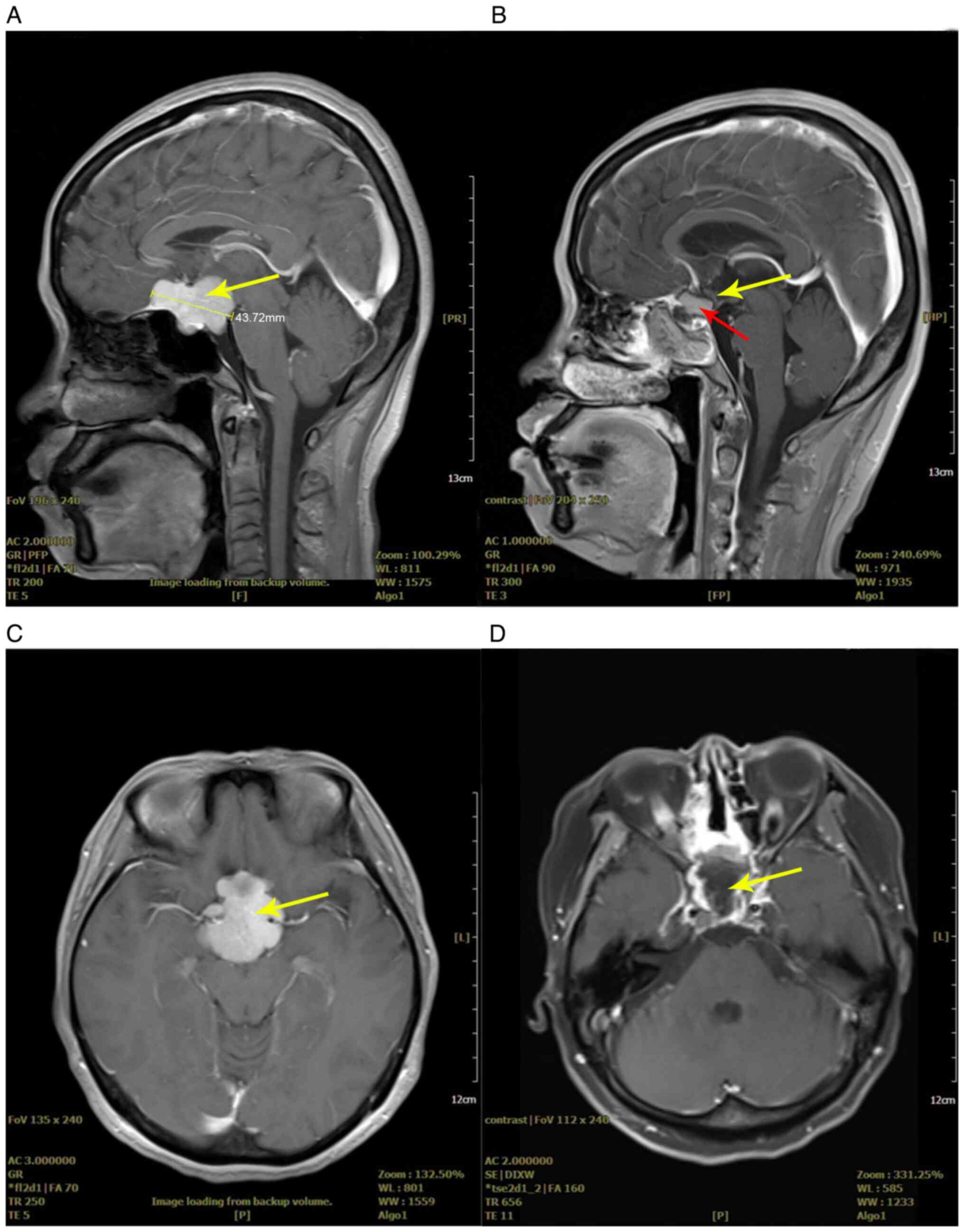
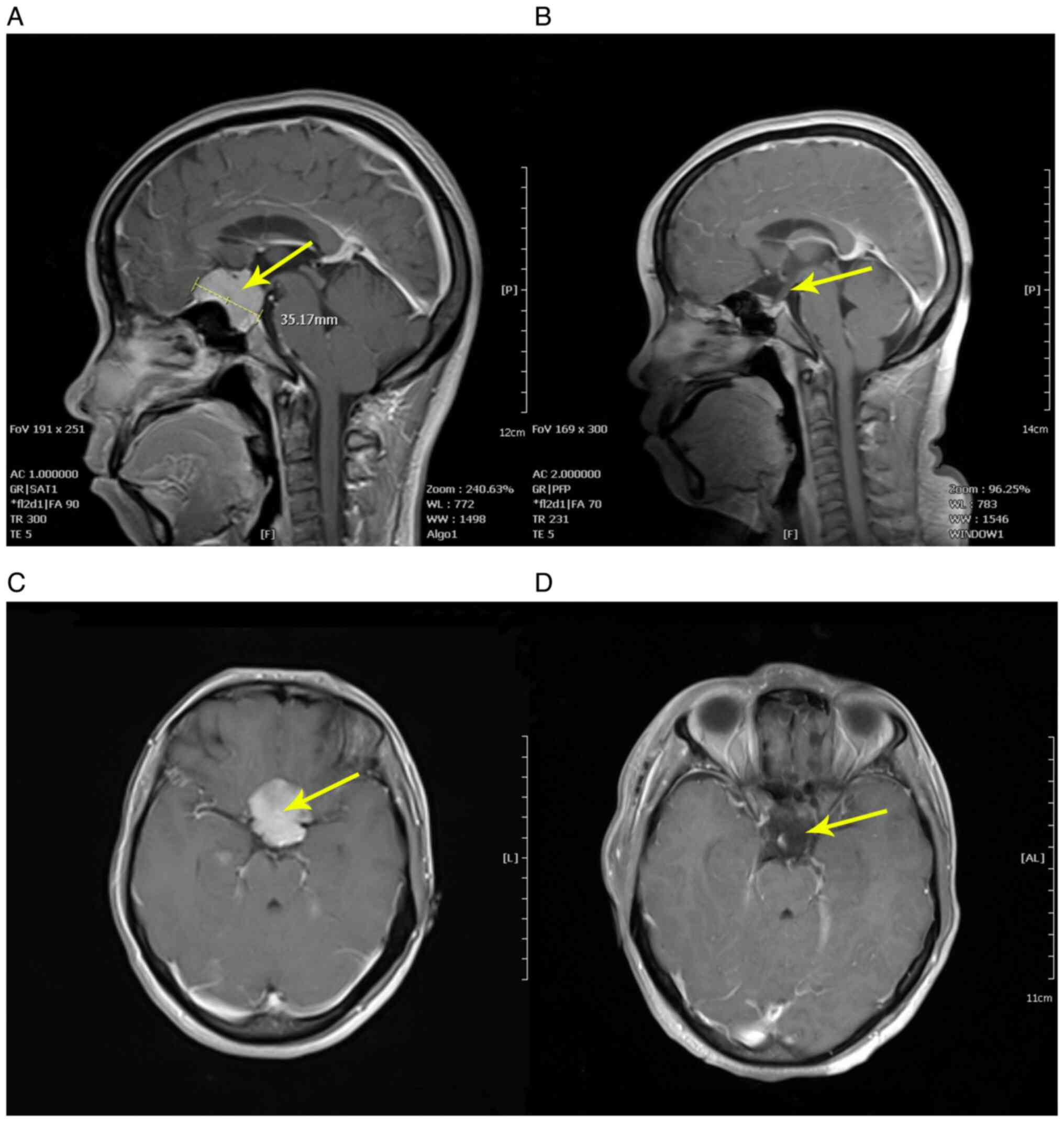
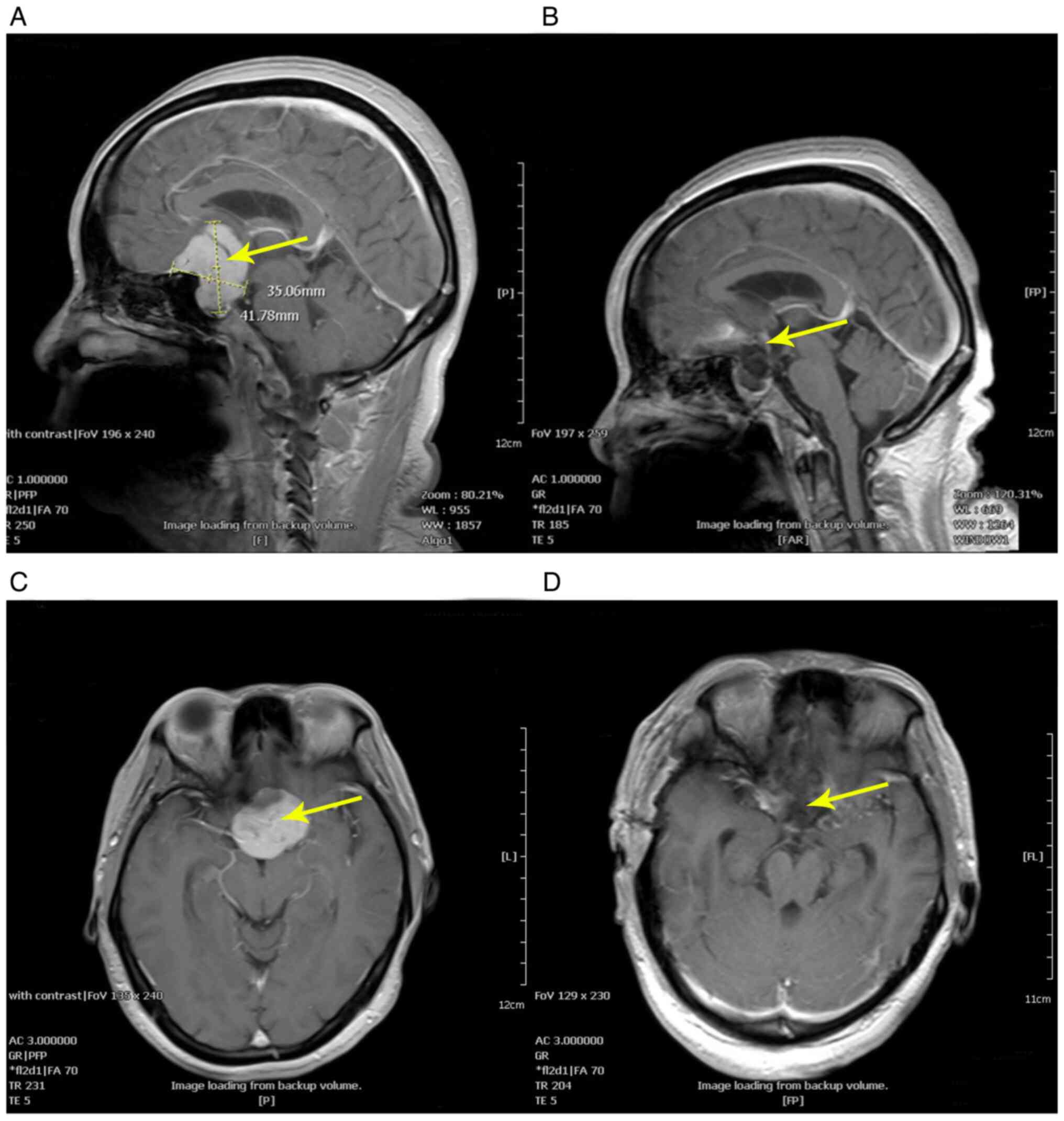
The tumor diameter in the endoscopic supraorbital
keyhole approach group ranged from 2.8-4.7 cm (mean, 3.4 cm), while
the tumor diameter in the endoscopic extended transsphenoidal
approach group ranged from 2.4-3.7 cm (mean, 2.8 cm). According to
the postoperative pathological results, all cases were diagnosed as
TSM (representative staining in Fig.
1). According to preoperative and postoperative cranial MRI
images (Fig. 2, Fig. 3, Fig.
4 and Fig. 5), in the
endoscopic supraorbital keyhole approach group, there were 16 cases
(94.1%) that achieved GTR and only 1 case (5.9%) that achieved NTR.
In the endoscopic extended transsphenoidal approach group, there
were 18 cases (94.7%) that achieved GTR and only 1 case (5.3%) that
achieved NTR. The postoperative visual acuity recovery showed that
in the endoscopic supraorbital keyhole approach group, 23 eyes were
improved, 8 eyes were maintained, 3 eyes deteriorated and the
visual recovery was ~67.6%. In the endoscopic extended
transsphenoidal approach group, 32 eyes were improved, 4 eyes were
maintained, 2 eyes deteriorated and the visual recovery was ~84.2%.
In the supraorbital keyhole approach group, there was no
cerebrospinal fluid leakage, while in the extended transsphenoidal
approach group, cerebrospinal fluid leakage occurred in 3 cases
(15.8%). However, anosmia occurred in 1 case (5.9%) via the
endoscopic supraorbital keyhole approach. No vascular injury,
frontal lobe contusion or intracranial infection occurred in all
cases. In these two groups, no tumor recurrence was found during
the follow-up of ~5 years.
Discussion
Surgical management of TSM. TSM was first
described by James Stewart in the second half of the 19th century
(16). Initially, for the removal
of TSM, both the subfrontal approach and the pterional approach
were favored by neurosurgeons (17,18),
and they are two commonly used approaches at present. However,
there are numerous hidden dangers with these two approaches; for
example, the bilateral subfrontal approach may bring greater risks
of cerebrospinal fluid leakage, olfactory nerve injury and
postoperative brain edema (5,19),
while the pterional approach cannot clearly display the underside
and intersection of the ipsilateral optic nerve, resulting in a
decrease in the postoperative visual acuity of 10-20% of patients
(10,19,20).
Subsequently, with the improvement of skull base technology, the
supraorbital, orbitozygomatic and orbitotemporal approaches are
recommended, because they can increase the surgical exposure area
and minimize the degree of frontal lobe retraction (21).
However, all of the above approaches belong to the
traditional craniotomy approach, which has the limitations of large
trauma, increased postoperative complications and a long recovery
period (17-21).
Therefore, a minimally invasive approach is required. Perneczky
(22) proposed the concepts of
keyhole surgery through a brow skin incision with a small
supraorbital incision, which is a minimally invasive approach also
known as the supraorbital keyhole approach. The supraorbital
keyhole approach not only overcomes the shortcomings of the
traditional approach but also conforms to the current concept of
minimally invasive neurosurgery and cosmetic requirements. Until
now, the supraorbital keyhole approach has been a standard approach
for the treatment of TSM (23-25).
In addition, with the development of endoscope
technology, the extended transsphenoidal approach has also become
another standard approach for the treatment of TSM. This can not
only achieve a high total tumor resection rate, but also protects
and improves the optic nerve/optic chiasma function (1). Compared with a microscope, an
endoscope has the characteristics of a brighter light, a wider and
deeper field of vision and a more unobstructed field of vision,
which means endoscopes are widely used in skull base surgery
(14). Therefore, the endoscopic
supraorbital keyhole approach and endoscopic extended
transsphenoidal approach are effective methods for the resection of
TSM and have attracted attention. However, there are different
opinions on the choice of these two surgical methods based on the
following indications, tumor resection scope and postoperative
complications.
Endoscopic supraorbital keyhole
approach vs. extended transsphenoidal approach
Both the endoscopic supraorbital keyhole approach
and the extended transsphenoidal approach have gradually become
standard surgical methods for the treatment of TSM and have been
recognized by surgeons. Linsler et al (14) has reported that 16 patients with
TSM underwent endoscopic supraorbital keyhole approach surgery,
where 14 patients (87.5%) achieved GTR and 2 patients achieved NTR.
Among them, 5 cases (31.3%) had visual loss before the operation.
After surgery, 6 eyes (60%) had improved, 4 eyes (40%) were
maintained and no eyes had deteriorated. Notably, the extension
lateral to the internal carotid artery was revealed in 81% (13 of
the 16 patients) of these cases during surgery. Furthermore,
previous literature has indicated that the endoscopic supraorbital
keyhole approach can not only remove the lateral growth of TSM but
also directly remove the crawling thin tumor vascular tissue
surrounding TSM, which improves control of the lateral extension of
the tumor to the sphenoid wing and cavernous sinus (26,27).
Furthermore, after full exposure, the surgeon can reassess the
extent of tumor invasion of the cavernous sinus and determine the
appropriate resection range (14,28,29).
In conclusion, the endoscopic supraorbital approach can remove
laterally extended TSM, with a high GTR rate and fewer
postoperative complications, but the visual protection effect needs
to be improved.
Meanwhile, the endoscopic extended transsphenoidal
approach for TSM has also been used by surgeons. Chowdhury et
al (30) reported 6 patients
who underwent an endoscopic extended transsphenoidal approach for
the removal of a TSM tumor, including 5 cases (83.3%) of GTR and 1
case (16.7%) of NTR. In addition, 2 cases (33.3%) showed improved
vision, 3 cases (50%) of maintained vision, 1 case (16.7%) of
deteriorated vision and 1 case (16.7%) of cerebrospinal fluid
leakage. Yu et al (1)
demonstrated that 40 patients with TSM underwent an endoscopic
extended transsphenoidal approach surgery, and their postoperative
results are GTR in 38 cases (95%), NTR in 2 cases (5%), improvement
of visual function in 38 cases (95%), cerebrospinal fluid leakage
in 3 cases (7.5%), meningitis in 2 cases (5%) and anosmia in 8
cases (20%). Gardner et al (31) reported that 13 patients with TSM
were treated with endoscopic extended transsphenoidal approach
surgery, of which 12 cases achieved GTR (92.3%) and 1 case achieved
NTR (7.7%), while vision was alleviated or improved in all cases, 5
cases (38.4%) had cerebrospinal fluid leakage. The above surgical
results indicates that the endoscopic extended transsphenoidal
approach has a good effect on GTR rate and vision in the treatment
of TSM. This depends on the unique advantages of this approach,
such as transforming deep skull base tumors into shallow eminence
tumors, directly blocking the blood supply of the tumors, causing
less interference to the optic nerve, and making it easier to
decompress the optic canal without shrinking the frontal lobe and
easy to remove the affected dura and bones (15,32).
Abhinav et al (33) describe the optic canal anatomy from
an endonasal perspective and the necessity of distinguishing the
preforaminal intracranial segment of the optic nerve from the
intracanalicular segment of the optic nerve. The authors describe
that through the maximal bony decompression of the optic canal,
division of the falciform ligament and opening the dural sheath, a
270˚ decompression of the optic canal can be achieved. This
suggests that the endoscopic endonasal approach is helpful for
optic nerve decompression and suprasellar tumor resection. However,
the endoscopic extended transsphenoidal approach will increase the
risk of cerebrospinal fluid leakage, and cannot completely avoid
symptoms such as anosmia, anterior pituitary or posterior pituitary
dysfunction (1,34). In conclusion, these two approaches
are not always perfect, and both have limitations and
contraindications. The biggest limitation of the endoscopic
supraorbital approach is that it is easy to confuse the bottom of
the frontal lobe and increase the difficulty of removing the skull
base dura, while the endoscopic extended transsphenoidal approach
cannot reach and remove the transverse extension tumor behind the
internal carotid artery.
Selection of surgical methods
From the comparison of the above two approaches, it
can be seen that there is no marked difference in the surgical
effect between the endoscopic supraorbital approach and the
endoscopic extended transsphenoidal approach for the resection of
TSM; however, they do have different advantages and limitations
(details are presented in Table
I). Combined with previous surgical experience and relevant
literature, the present study suggested three main reasons for
choosing the supraorbital keyhole approach or expanded
transsphenoidal approach. First, according to the actual condition
of the patient, the selection of surgical methods should be based
on the specific characteristics of TSM and the physical condition
of the patient, including tumor size, growth site, whether it is
wrapped by blood vessels, distal extension, the relationship
between tumor and bone and a physical examination of the patient.
The endoscopic supraorbital keyhole approach is more suitable for
patients with TSM who are older, have poor a general condition,
have a close relationship between the tumor and the blood vessels
of the skull base and has a tumor growing laterally to the internal
carotid artery. The endoscopic extended transsphenoidal approach
should be used to treat small TSM without lateral extension or
vascular wrapping. The wishes of the patient are also important.
Some patients are willing to accept the supraorbital keyhole
approach, and some patients are more willing to accept the expanded
transsphenoidal approach. Secondly, the proficiency of the surgeon
in the two surgical methods is an important reason for surgery
selection. Finally, the surgical conditions and related equipment
also affect the selection of surgical methods. These two surgical
methods are complementary, so neurosurgeons should master both of
these methods, which is conducive to the correct selection of
appropriate surgical methods for different patients to achieve the
best surgical results.
 | Table IAdvantages and limitations of
supraorbital keyhole approach and extended transsphenoidal
approach. |
Table I
Advantages and limitations of
supraorbital keyhole approach and extended transsphenoidal
approach.
| A, Endoscopic
supraorbital keyhole approach |
|---|
| Advantages | Limitations |
|---|
| Low incidence of
cerebrospinal fluid leakage | It was easy to cause
contusion at the bottom of the frontal lobe |
| It was helpful for
surgeons to remove the lateral extension of of the patient's
tumor | Difficulty in dural
management of the skull base |
| It could directly
handle the thin layer of tumor vascular tissue creeping surrounding
the tumor. Under the condition of vascular wrapping, vascular
control during tumor resection was easier | |
| It could completely
avoid nasal symptoms, and the incidence of anosmia or anterior or
posterior pituitary dysfunction was low | |
| The patient recovered
quickly | |
| B, Endoscopic
extended transsphenoidal approach |
| Advantages | Limitations |
| It could transform
deep skull base tumors into superficial convex tumors and directly
block the tumor blood supply | A nasal approach
had inherent anatomical limitations and could not reach the tumors
extending outside the internal carotid artery. It was difficult to
deal with tumors outside the internal carotid artery |
| No significant
frontal lobe retraction was required, the interference to the optic
nerve was minimal and the patient's vision recovered well after
surgery | High incidence of
cerebrospinal fluid leakage after the operation |
| Optic canal
decompression was easier | High incidence of
olfactory impairment |
| Invasive skull and
dura mater could be removed | It was difficult to
remove tumors with a diameter >4 cm, or that have lateral
extension and vascular wrapping |
| Endoscopic vision
was wide and surgical vision is clear | |
Neuroendoscopy and visual effect
Compared with the microscope, neuroendoscopy has the
advantages of a wide field of vision, a bright light, no
obstruction and no dead angle, which can improve the safety of
surgery and avoid the occurrence of related complications, such as
arterial injury, visual degradation, pseudobulbar palsy and dural
injury in parasellar and suprasellar areas (35). In addition, an endoscope can
provide a certain angle, which is more conducive to observing the
parasellar and suprasellar areas, to improve removal of the tumor.
It is worth emphasizing that visual impairment is the most common
symptom of TSM, and the majority of patients with TSM have a
preexisting visual impairment caused by TSM before treatment to
varying degrees. The degree of visual acuity recovery is mainly
associated with three factors: Simpson's grade (15), the degree of optic nerve
involvement (36) and the
timeframe of preoperative visual acuity decline (37,38).
The latter two factors cannot be changed, but Simpson's grade can
be controlled by the surgeon. That is, the more thoroughly the
tumor is removed, the more conducive it is to the recovery of
vision, so the auxiliary visualization tool is particularly
important (39). Komotar et
al (40) reported that there
is no difference in vision recovery between endoscopic
transsphenoidal surgery and microscopic transcranial surgery (69.1
and 58.7%, respectively). Hence, an endoscope is also a good
auxiliary visualization tool. However, an endoscope also has
various shortcomings. For example, the endoscope occupies the
operational space during operation and the endoscope can only
provide two-dimensional images. In addition, intraoperative
bleeding may pollute the endoscope lens, affecting the image
quality of the endoscope and the continuity of the operation.
Limitations
The present study has certain limitations. The
present study was a descriptive study that focused on the
preliminary results of the two surgical methods in Chongqing
General Hospital. In addition, the follow-up time was relatively
short and a small number of patients were included, so no
statistical analysis was carried out. At the same time, it was
designed as a non-randomized retrospective study and did not
completely rule out potential selection biases.
The present study reviewed 36 cases with TSM treated
by the endoscopic supraorbital keyhole approach or the endoscopic
extended transsphenoidal approach, analyzed the postoperative
effects of the two surgical methods, compared the two surgical
methods and put forward the basic criteria for the selection of
surgical methods. First of all, there was little difference between
the two surgical methods in terms of the GTR rate (94.1 vs. 94.7%),
but there were some differences in visual acuity recovery (67.6 vs.
84.2%) and postoperative complications. The visual acuity of the
patients in the endoscopic extended transsphenoidal approach group
recovered well, while the probability of cerebrospinal fluid
leakage caused the by endoscopic supraorbital approach was small.
Secondly, the endoscopic supraorbital keyhole approach was
conducive to the lateral extension of TSM (especially when the
tumor reached the lateral side of the internal carotid artery),
while the endoscopic extended transsphenoidal approach first
blocked the blood supply of the tumor, reduced the difficulty of
tumor resection and had little interference with the optic nerve.
Finally, the important basis for selecting an appropriate approach
is the specific characteristics of TSM and the physical condition
of patients, including tumor size, growth site, whether it is
wrapped by blood vessels, distal extension, the relationship
between tumor and bone and physical examination of patients. The
endoscopic supraorbital keyhole approach is more suitable for
patients with TSM who are older, have poor general conditions, have
a close relationship between the tumor and the blood vessels of the
skull base and the tumor grows laterally to the internal carotid
artery. It is suggested that the endoscopic extended
transsphenoidal approach should be used to treat small TSM without
lateral extension or vascular wrapping. In fact, these two surgical
methods complement each other, so neurosurgeons should master these
two methods, which is conducive to the correct selection of
surgical methods suitable for different patients to achieve the
best surgical results.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
NW, JW, PW, HJ, JL, CT, GZ and XT participated in
the conception, design and data acquisition of the article. HJ
participated in drafting and revising the manuscript. NW critically
revised the article. NW ensured that questions related to the
integrity of any part of the work were appropriately investigated
and resolved. HJ, JL, CT, GZ and XT confirm the authenticity of all
the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The Ethics Committee of Chongqing General Hospital
waived the requirement for additional ethical review as this report
is retrospective and not based on any specific patient priorities,
experiences or preferences. Informed consent for participation in
the study or use of the medical data was obtained from the
patients.
Patient consent for publication
Written informed consent was obtained from the
patients for the publication of anonymized data and any
accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yu P, Xu T, Wu X, Liu Z and Wang Y and
Wang Y: The expanded endoscopic endonasal approach for treatment of
tuberculum sellae meningiomas in a series of 40 consecutive cases.
Sci Rep. 11(4993)2021.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Sankhla SK, Jayashankar N, Khan MA and
Khan GM: Surgical management of tuberculum sellae meningioma: Our
experience and review of the literature. Neurol India.
69:1592–1600. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Khan OH, Krischek B, Holliman D,
Klironomos G, Kucharczyk W, Vescan A, Gentili F and Zadeh G: Pure
endoscopic expanded endonasal approach for olfactory groove and
tuberculum sellae meningiomas. J Clin Neurosci. 21:927–933.
2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Wang ZC: Neurosurgery. Hubei Science and
Technology Publishing House, Wuhan, 1998 (In Chinese).
|
|
5
|
Mahmoud M, Nader R and Al-Mefty O: Optic
canal involvement in tuberculum sellae meningiomas: Influence on
approach, recurrence, and visual recovery. Neurosurgery 67 (3 Suppl
Operative): onsS108-S118. discussion ons118-9, 2010.
|
|
6
|
Rubin G, Ben David U, Gornish M and
Rappaport ZH: Meningiomas of the anterior cranial fossa floor.
Review of 67 cases. Acta Neurochir (Wien). 129:26–30.
1994.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhang C, Ding J, Liu Y, Tuoheti M, Yang X,
Wang J and Wu Y: Endoscopic endonasal approach for resection of
tuberculum sellae meningioma: A promising surgical approach. J
Craniofac Surg. 31:1815–1818. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tang H, Sun H, Xie L, Tang Q, Gong Y, Mao
Y, Xie Q, Zheng M, Wang D, Zhu H, et al: Intraoperative ultrasound
assistance in resection of intracranial meningiomas. Chin J Cancer
Res. 25:339–345. 2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Nakamura M, Roser F, Jacobs C, Vorkapic P
and Samii M: Medial sphenoid wing meningiomas: Clinical outcome and
recurrence rate. Neurosurgery. 58:626–639. 2006.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Nakamura M, Roser F, Struck M, Vorkapic P
and Samii M: Tuberculum sellae meningiomas: Clinical outcome
considering different surgical approaches. Neurosurgery.
59:1019–1028. 2006.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Nakamura M, Struck M, Roser F, Vorkapic P
and Samii M: Olfactory groove meningiomas: Clinical outcome and
recurrence rates after tumor removal through the frontolateral and
bifrontal approach. Neurosurgery. 60:844–852. 2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Jho HD and Carrau RL: Endoscopy assisted
transsphenoidal surgery for pituitary adenoma. Acta Neurochir
(Wien). 138:1416–1425. 1996.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Adappa ND, Learned KO, Palmer JN, Newman
JG and Lee JY: Radiographic enhancement of the nasoseptal flap does
not predict postoperative cerebrospinal fluid leaks in endoscopic
skull base reconstruction. Laryngoscope. 122:1226–1234.
2012.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Linsler S, Fischer G, Skliarenko V, Stadie
A and Oertel J: Endoscopic assisted supraorbital keyhole approach
or endoscopic endonasal approach in cases of tuberculum sellae
meningioma: Which surgical route should be favored? World
Neurosurg. 104:601–611. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Simpson D: The recurrence of intracranial
meningiomas after surgical treatment. J Neurol Neurosurg
Psychiatry. 20:22–39. 1957.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cushing H and Eisenhardt L: Meningiomas
arising from the tuberculum sellae: With the syndrome of primary
optic atrophy and bitemporal field defects combined with a normal
sella turcica in a middle-aged person. Arch Ophthalmol. 1:168–206.
1929.
|
|
17
|
Shrivastava RK, Segal S, Camins MB, Sen C
and Post KD: Harvey Cushing's Meningiomas text and the historical
origin of resectability criteria for the anterior one third of the
superior sagittal sinus. J Neurosurg. 99:787–791. 2003.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hayhurst C and Teo C: Tuberculum sella
meningioma. Otolaryngol Clin North Am. 44:953–963, viii-ix.
2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Chokyu I, Goto T, Ishibashi K, Nagata T
and Ohata K: Bilateral subfrontal approach for tuberculum sellae
meningiomas in long-term postoperative visual outcome. J Neurosurg.
115:802–810. 2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Fahlbusch R and Schott W: Pterional
surgery of meningiomas of the tuberculum sellae and planum
sphenoidale: Surgical results with special consideration of
ophthalmological and endocrinological outcomes. J Neurosurg.
96:235–243. 2002.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Soni RS, Patel SK, Husain Q, Dahodwala MQ,
Eloy JA and Liu JK: From above or below: The controversy and
historical evolution of tuberculum sellae meningioma resection from
open to endoscopic skull base approach. J Clin Neurosci.
21:559–568. 2014.
|
|
22
|
Perneczky A: Keyhole concept in
neurosurgery: With endoscope-assisted microsurgery and case
studies. Thieme, Stuttgart, New York, 1999.
|
|
23
|
Fischer G, Stadie A, Reisch R, Hopf NJ,
Fries G, Böcher-Schwarz H, van Lindert E, Ungersböck K, Knosp E,
Oertel J and Perneczky A: The keyhole concept in aneurysm surgery:
Results of the past 20 years. Neurosurgery. 68 (1 Suppl
Operative):S45–S51. 2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Reisch R and Perneczky A: Ten-year
experience with the supraorbital subfrontal approach through an
eyebrow skin incision. Neurosurgery. 57 (4 Suppl):S242–S255;
discussion 242-55. 2005.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Reisch R, Perneczky A and Filippi R:
Surgical technique of the supraorbital key-hole craniotomy. Surg
Neurol. 59:223–227. 2003.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Hernesniemi J, Ishii K, Niemelä M, Smrcka
M, Kivipelto L, Fujiki M and Shen H: Lateral supraorbital approach
as an alternative to the classical pterional approach. Acta
Neurochir Suppl. 94:17–21. 2005.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Kong DS, Hong CK, Hong SD, Nam DH, Lee JI,
Seol HJ, Oh J, Kim DG and Kim YH: Selection of endoscopic or
transcranial surgery for tuberculum sellae meningiomas according to
specific anatomical features: A retrospective multicenter analysis
(KOSEN-002). J Neurosurg. 130:838–847. 2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Marx S, Clemens S and Schroeder HWS: The
value of endoscope assistance during transcranial surgery for
tuberculum sellae meningiomas. J Neurosurg. 128:32–39.
2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Godano U: Transcranial approaches for
tuberculum sellae meningiomas in the endoscopic era. J Neurosurg
Sci. 65:457–459. 2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Chowdhury FH, Haque MR, Goel AH and Kawsar
KA: Endoscopic endonasal extended transsphenoidal removal of
tuberculum sellae meningioma (TSM): An experience of six cases. Br
J Neurosurg. 26:692–699. 2012.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Gardner PA, Kassam AB, Thomas A, Snyderman
CH, Carrau RL, Mintz AH and Prevedello DM: Endoscopic endonasal
resection of anterior cranial base meningiomas. Neurosurgery.
63:36–52; discussion 52-4. 2008.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Koutourousiou M, Fernandez-Miranda JC,
Stefko ST, Wang EW, Snyderman CH and Gardner PA: Endoscopic
endonasal surgery for suprasellar meningiomas: Experience with 75
patients. J Neurosurg. 120:1326–1339. 2014.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Abhinav K, Acosta Y, Wang WH, Bonilla LR,
Koutourousiou M, Wang E, Synderman C, Gardner P and
Fernandez-Miranda JC: Endoscopic endonasal approach to the optic
canal: Anatomic considerations and surgical relevance.
Neurosurgery. 11 Suppl 3:431–445; discussion 445-6. 2015.PubMed/NCBI View Article : Google Scholar
|
|
34
|
de Divitiis E, Cavallo LM, Esposito F,
Stella L and Messina A: Extended endoscopic transsphenoidal
approach for tuberculum sellae meningiomas. Neurosurgery. 61 (5
Suppl 2):S229–S237; discussion 237-8. 2007.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Black PM, Zervas NT and Candia GL:
Incidence and management of complications of transsphenoidal
operation for pituitary adenomas. Neurosurgery. 20:920–924.
1987.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Jallu A, Kanaan I, Rahm B and Siqueira E:
Suprasellar meningioma and blindness: A unique experience in Saudi
Arabia. Surg Neurol. 45:320–323. 1996.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Grisoli F, Diaz-Vasquez P, Riss M,
Vincentelli F, Leclercq TA, Hassoun J and Salamon G: Microsurgical
management of tuberculum sellae meningiomas. Results in 28
consecutive cases. Surg Neurol. 26:37–44. 1986.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Park CK, Jung HW, Yang SY, Seol HJ, Paek
SH and Kim DG: Surgically treated tuberculum sellae and diaphragm
sellae meningiomas: The importance of short-term visual outcome.
Neurosurgery. 59:238–243. 2006.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Lee JH, Jeun SS, Evans J and Kosmorsky G:
Surgical management of clinoidal meningiomas. Neurosurgery.
48:1012–1021. 2001.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Komotar RJ, Starke RM, Raper DM, Anand VK
and Schwartz TH: Endoscopic endonasal versus open transcranial
resection of anterior midline skull base meningiomas. World
Neurosurg. 77:713–724. 2012.PubMed/NCBI View Article : Google Scholar
|