Introduction
Breast cancer is the most common cancer type
worldwide (1). The treatment goal
for breast cancer is not only to prolong survival but also to
improve the quality of life of patients (2). The quality of life of patients with
cancer is closely associated with their experience of pain
(3). Pain is the most common
complaint from patients with cancer (4). High pain intensity is associated with
a low quality of life. It was reported that >70% of patients
with cancer experience severe pain despite various pain management
approaches (5). The World Health
Organization has recommended an analgesic ladder, which includes a
three-step strategy from non-opioid analgesics to weak or strong
opioid therapies (6). Certain
researchers have suggested adding a fourth step to involve
interventional treatments in order to provide adequate control for
severe or sudden onset cancer pain (7). One of the interventional approaches
is neuraxial analgesia with epidural or intrathecal injection of
opioids. Neuraxial analgesia was proven to have good efficacy and
safety for cancer pain management and provides adequate pain
control and improvement of the quality of life (8). Neuraxial analgesia involves injection
of anesthetic medication into the epidural space (epidural
anesthesia) or the subarachnoid space (intrathecal anesthesia).
Most epidural analgesia procedures are performed with the catheter
inserted in the lower thoracic or lumbar spine areas and then
advanced in a cephalad direction to reach a level that requires
analgesia (9-12).
However, this approach cannot always be successfully completed in
patients with stenosis or compression in the epidural or
subarachnoid spaces due to tumor metastasis or invasion into the
spine, which may block the catheter advance. The present case study
reports on a patient with breast cancer and spine metastasis, in
whom adequate pain relief was successfully achieved by performing
thoracic spine puncture and advancing the catheter in a caudal
direction to reach the area of pain.
Case report
A 59-year-old female patient was admitted to the
Third Affiliated Hospital of Sun Yat-sen University, Yuedong
Hospital (Meizhou, China) in September 2021 due to chest and upper
back pain for >3 months after receiving the multi-line
chemotherapy for postoperative recurrent left breast adenocarcinoma
(T4aN3cM1, stage IV, Luminal B, Her2 negative). The patient denied
a history of hypertension, diabetes or chronic obstructive
pulmonary disease. In 2006, the patient had been diagnosed with
left breast adenocarcinoma and received modified radical
mastectomy. Postoperatively, the patient received chemotherapy
(cyclophosphamide, doxorubicin and fluorouracil, followed by
long-term tamoxifen therapy) and was followed up in the clinic. In
2014, the patient was found to have cancer recurrence. Epidermal
growth factor receptor-2 was negative. The patient received a total
of 35 rounds of chemotherapy, including fluorouracil,
cyclophosphamide, doxorubicin, platinum, vinorelbine, lobaplatin
and paclitaxel, as well as endocrine therapy with exemestane, with
poor responses. Additional endocrine therapy with cyclin-dependent
kinase 4 and -6 inhibitor was recommended but was refused by the
patient due to its high cost. During the current hospital
admission, the patient complained of intermittent severe pain with
an intensity of up to 10 on the visual analogue scale (VAS) in the
left chest and up her back (the body surface is projected between
the ribs T5 and T6) several times a day. Oral 80 mg oxycodone was
prescribed, which was able to decrease the pain intensity to 5.
However, the patient experienced severe side effects, including
nausea, vomiting, poor appetite, insomnia and dizziness. Physical
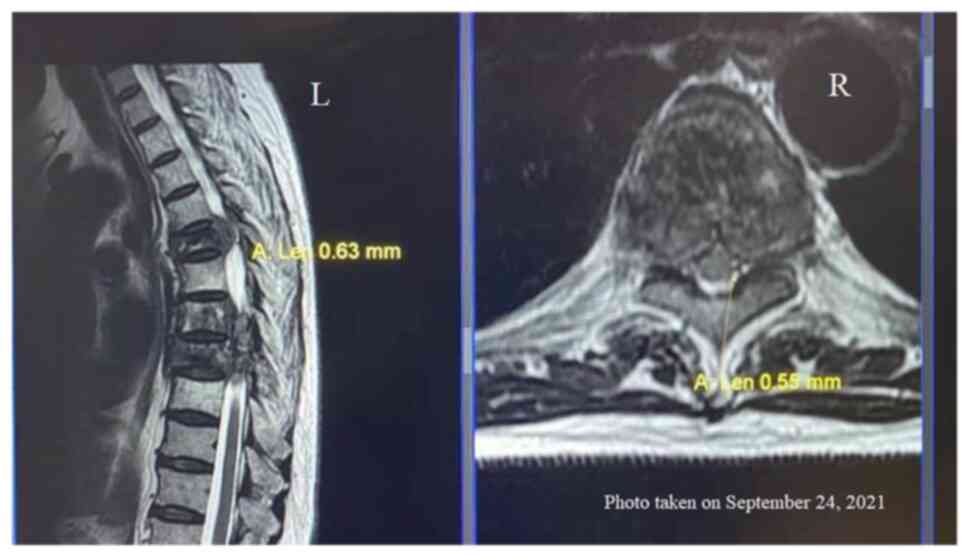
examination showed normal vital signs. Magnetic resonance imaging
examination revealed multiple bony metastases in the T5, T7 and T8
vertebral bodies and bilateral pedicles, as well as in the left 7th
and 8th posterior ribs. T5 and T8 spinal stenoses and spinal cord
compressions were also present. The epidural space at the T5 level
was narrowed to 0.55 mm (Fig. 1).
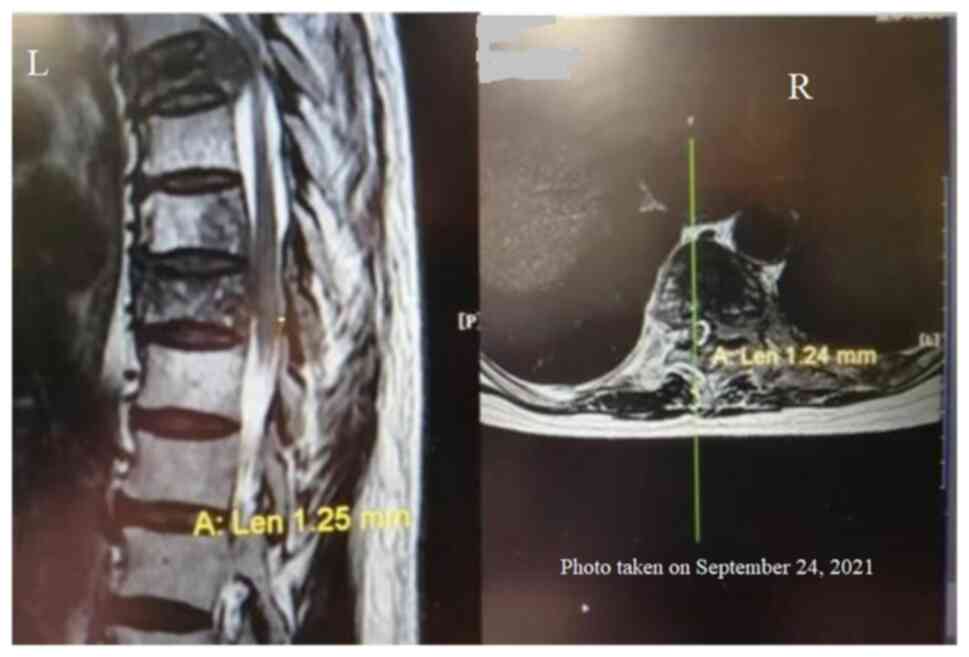
The spinal cord at the T8 level was severely compressed, with the
narrowest subarachnoid space at 1.24 mm (Fig. 2), a narrow epidural space of 0.55
mm (Fig. 3) and a right shift of
the spinal cord. Other parts of the spinal cord were unremarkable.
The admission diagnoses included the following: i) Postoperative
recurrence of invasive ductal adenocarcinoma of the left breast
(T4aN3cM1, stage IV, Luminal B, Her2 negative); ii) spinal
metastases; and iii) cancer pain.
The patient received oral oxycodone but was unable
to tolerate it and was unable to maintain her routine daily life
activities. Oxycodone caused severe side effects in this patient.
After the hospital admission and necessary tests, it was determined
that there was no contraindication for epidural analgesia.
Therefore, a decision was made for epidural catheter placement to
reach the T5 level and provide analgesic infusion to relieve the
pain and improve the quality of life. The traditional approach of
epidural analgesia is to perform a lower thoracic or lumbar spine
puncture first and then insert the epidural catheter in a cephalad
direction to reach the epidural space at the T5 level. However,
considering that the patient had spinal stenosis and compression at
the T8 level but the area of pain was at the T5 level, an epidural
catheter entered through the lumbar area and directed cephalad
would not have been able to pass the T8 level and reach the T5
level; it was thus decided to perform the thoracic spine puncture
at the T1-2 level and direct the epidural catheter caudally to
reach the T5 level.
The procedure was explained to the patient and the
patient's family and written informed consent was obtained from
them. In the operating room, the patient was placed in the left
lateral decubital position. Routine disinfection was performed and
surgical drapes were applied. The spinous processes of the T1 and
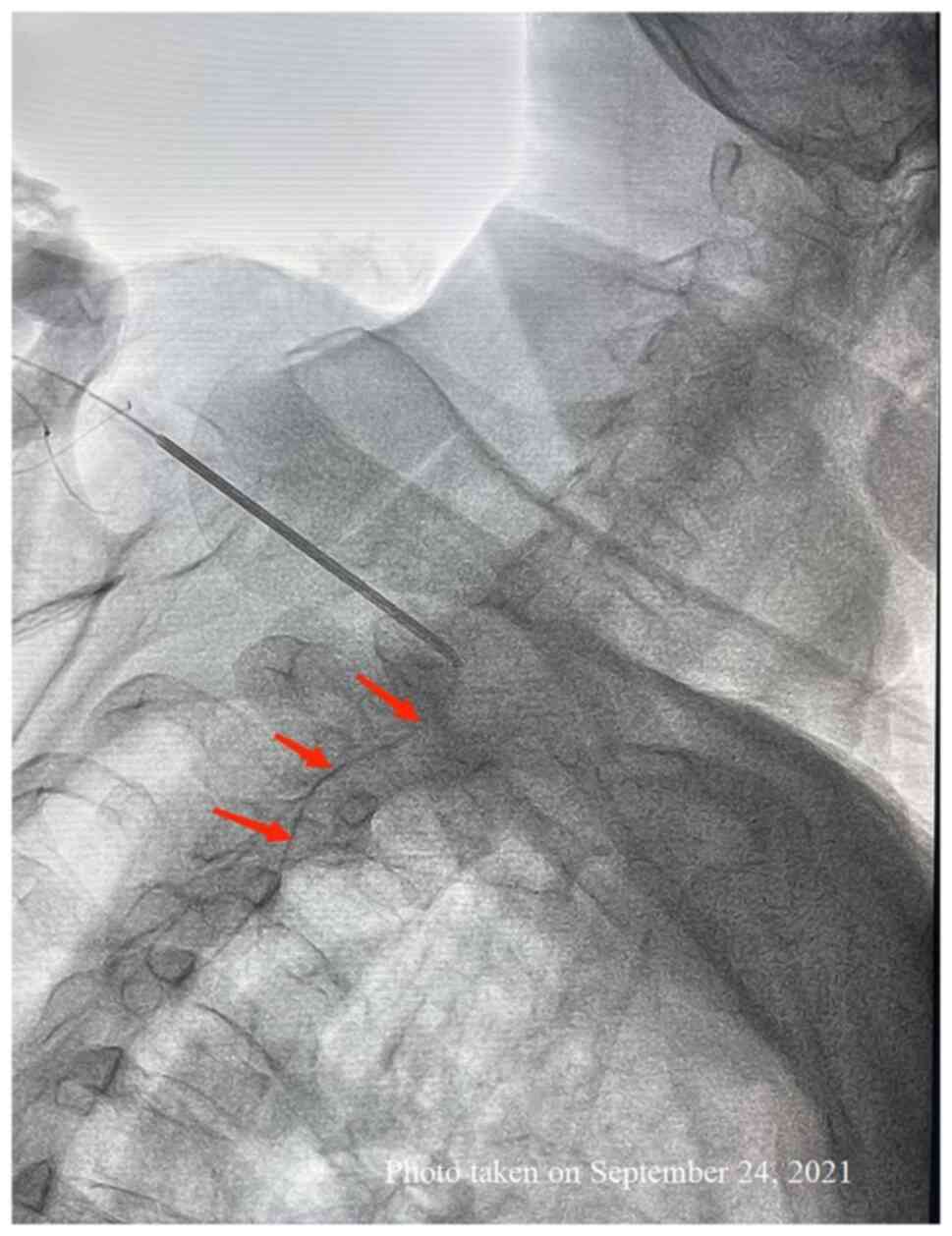
T2 were identified under digital subtraction angiography (DSA). A
hollow spine puncture needle was connected to a glass syringe with
negative pressure and entered into the skin at 2 cm lateral to the
spinous process. The bevel of the needle formed a 30-degree angle
to the coronal plane. After the needle was inserted by ~5.5 cm, a
‘pop’ sensation occurred and the negative pressure in the glass
syringe disappeared, suggesting that the needle had reached the
epidural space. The glass syringe was removed and a soft catheter
was inserted through the spine puncture needle and advanced
caudally with its tip, finally reaching the level of the T5
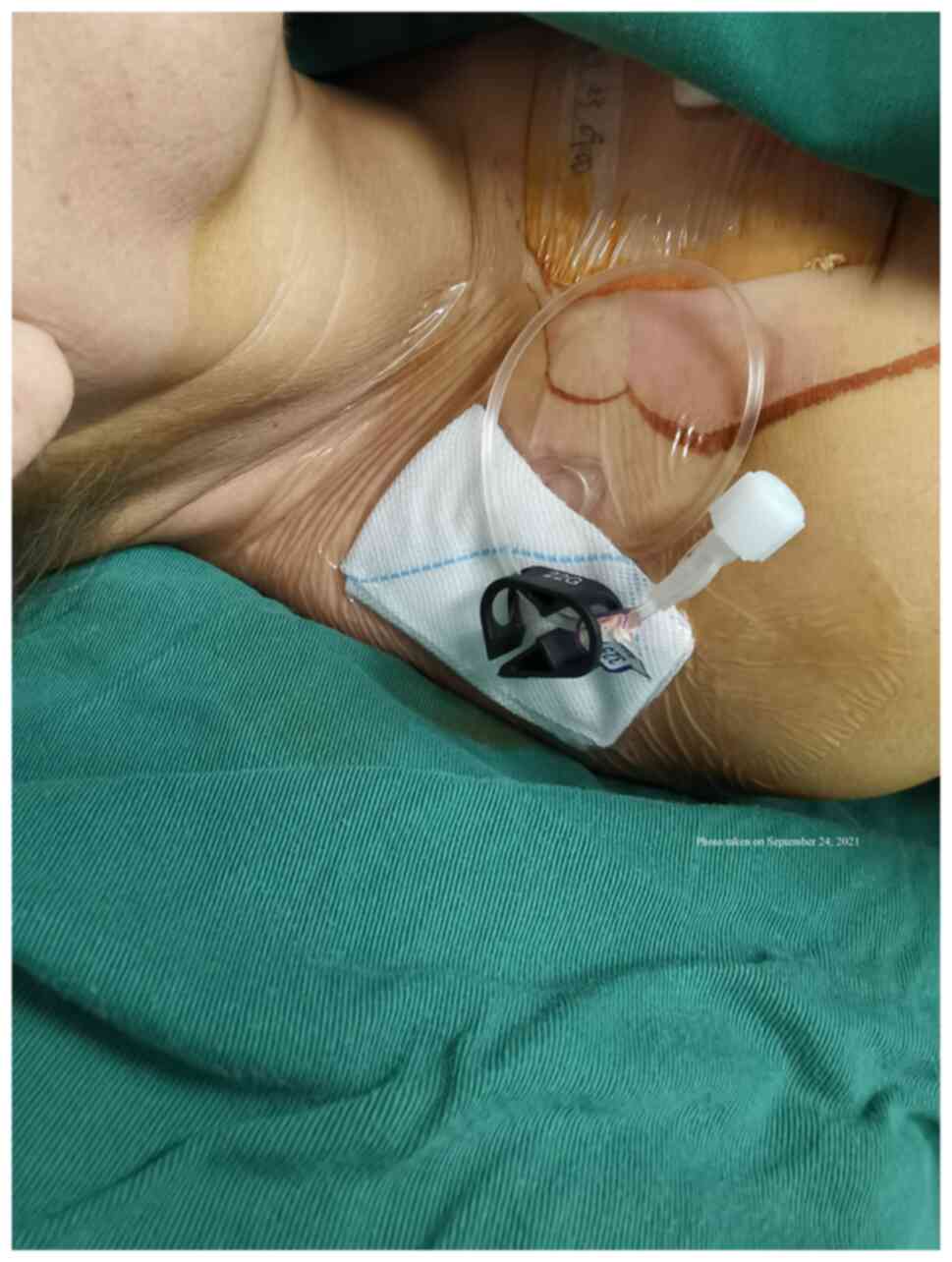
vertebral body. The spine puncture needle was removed. The other
end of the soft catheter was connected to an infusion port for drug
delivery. Both the catheter and the port were sutured in a
subcutaneous pocket above the right shoulder and lateral to the
right side of the neck. The skin was sutured and covered by sterile
gauze (Fig. 4). The vital signs of
the patient were stable throughout the procedure.
After a successful thoracic spine puncture and
caudally directed epidural catheter placement (Fig. 5), the drug delivery port was
connected to an analgesic pump, which contained 30 mg morphine, 200
mg ropivacaine and 30 mg dexamethasone in 250 ml normal saline. The
first bolus was given at 5 ml. The infusion rate was at 1 ml/h. The
patient could increase the dose by himself, and each demand dose
was set at 2 ml with a lockout interval of 20 min.
Postoperatively, the patient stopped taking oral
analgesics and only used the epidural drug infusion system. The
pain was successfully controlled at a VAS of 2, with a small number
of episodes of sudden onset of severe pain. The symptoms of nausea,
vomiting, reduced appetite and dizziness were also improved in the
patient. The patient was satisfied with the pain control and
discharged three days after the procedure. During the two-month
follow-up period, the patient did not exhibit any signs of
infection or gastrointestinal discomfort. The pain intensity was 2.
Both appetite and body weight were improved, and BMI increased from
20.8 to 21.0 kg/m2.
Discussion
Cancer pain has a marked impact on the quality of
life of patients. The World Health Organization has recommended an
analgesic ladder, which includes a three-step strategy from
non-opioid analgesics to weak or strong opioid therapies (6). However, certain patients still have
severe pain after conventional analgesic treatments. Epidural drug
infusion therapy is one interventional approach. Most epidural
analgesia procedures are performed with a catheter inserted in the
lower thoracic or lumbar spine areas and then advanced in the
cephalad direction (13). A
previous case report described a patient with metastatic spinal
cord compression who received cervical epidural analgesia due to
neck pain (14). Furthermore,
thoracic epidural analgesia was performed in patients during chest
or abdominal surgeries or with rib fractures (15). All the above were successful. The
present study reported on a patient with chest and upper back pain
due to metastatic breast cancer. The upper thoracic spine puncture
was successfully performed between the T1 and T2 vertebrae and the
epidural catheter was advanced in a caudal direction to reach the
T5 level, which provided adequate analgesia.
The patient of the present study had breast cancer
recurrence and metastases after the initial surgery and
chemotherapy. The patient had complaints of severe chest and upper
back pain due to cancer metastases, as well as spinal stenosis in
the thoracic spine area. Oral oxycodone therapy did not relieve the
patient's pain but had severe side effects. All of these factors
had markedly decreased the patient's quality of life. Epidural drug
infusion therapy was selected. Adequate pain relief by the epidural
drug infusion in the patient necessitated placing the tip of the
infusion catheter at the level of pain. A traditional method is to
perform the lumbar puncture first (16) and then the infusion catheter was
inserted in a cephalad direction to reach the thoracic T5 level in
the present patient. However, for the present case, this
traditional approach to place the infusion catheter may have been
difficult, since the patient had severe spinal compression with
stenosis in both the subarachnoid and epidural spaces at the T8
level. The stenosis and compression at T8 may have blocked a
cephalad advanced epidural catheter from reaching the T5 level. It
was also considered that the insertion of the epidural catheter at
the T4-5 level may have had a risk of catheter dislodgement due to
the short distance of implantation in the epidural space. If the
catheter had been left too long in the epidural space, it may have
passed the T5 level and resulted in incomplete analgesia in the T5
area. In addition, it may have been inappropriate to insert the
infusion catheter at the T5, T7 and T8 levels, since it may have
caused spinal cord injury and paraplegia from subarachnoid puncture
and spinal ependymoma (17).
Therefore, it was concluded that the best approach was to perform
the thoracic puncture at the T1-2 level and advance the infusion
catheter in a caudal direction in the epidural space to reach the
T5 level. During the DSA-guided procedure, the head of the patient
was placed in a forward-flexed position. Successful placement of
the infusion catheter was achieved after multiple fine adjustments
of the direction and angle of the catheter.
Most previous studies reported on the implantation
of the injection port in the waist or the lower abdominal areas
(18,19). In the patient of the present study,
the infusion port was implanted in the depression where the right
trapezius meets the clavicle, which is easier to secure to the skin
due to its proximity to the site of pleural puncture. It also
facilitated postoperative care. Compared to implantation in the
waist (19), based on previous
experience and literature (20),
this location made the patient feel more comfortable and the
infusion port was not as easy to contaminate in the shower. There
is no consensus on the analgesic drugs used for cancer pain control
among clinicians involved in patient care. Opioids have been the
mainstay analgesics. In the present case, a small dose of
dexamethasone (~3 mg/day) was also included to prevent nausea and
vomiting, which were the main side effects of the opioid treatment.
Simultaneously, dexamethasone may also reduce cancer pain scores
and decrease the amount of opioids required to obtain adequate pain
relief.
Contraindications to intrathecal drug infusion
include local skin infection and coagulation dysfunctions. During
the thoracic puncture and advance of the infusion catheter in the
epidural space, care should be taken to avoid catheter knotting or
misalignment. Postoperatively, patients should be monitored for
cerebrospinal fluid leakage, infection and spinal hematoma
formation (19,21).
As a single case report, the present study had the
limitations of single patient description, retrospective review of
the clinical information and short-term follow-up. The procedure
used in the present study also had a high medical expense, with
potential side effects, including infection and cerebrospinal fluid
leakage. Patients under this treatment also require frequent
hospital visits to ensure adequate analgesia and safety. Currently,
this patient is being followed up in the clinic to observe opioid
consumption and pain control. In the future, this analgesic
approach will be applied to further suitable candidates. The
present case study aimed to introduce this analgesic approach to
clinicians. Once additional cases are reported, further experience
and clinical evidence may be accumulated to refine this treatment
method to benefit more patients.
In conclusion, epidural analgesic infusion may be
suitable for certain patients with cancer metastasis for adequate
pain relief. In patients with chest and upper back pain, the
traditional approach of lower thoracic or lumbar spine puncture and
cephalad advance of infusion catheter may not be possible due to
thoracic spinal metastasis and stenosis. In the current case
report, thoracic spine puncture was performed at the T1-2 level and
the infusion catheter was advanced in a caudal direction to reach
the T5 level. Successful pain control in this patient indicated
that this may be a feasible and safe approach to achieve adequate
analgesia and improve the quality of life of patients with similar
conditions. Future prospective studies are warranted to confirm the
present results.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
SY, QY and YZha conceived and designed the study.
SY, QY, YZho and KZ performed the literature search. KZ acquired
data and drafted the manuscript. SY, YZha and YZho established the
clinical diagnosis and assisted in revising the manuscript. SY, KZ
and QY wrote the original draft. SY, QY and YZha wrote, reviewed
and edited the manuscript. SY, YZ and QY confirm the authenticity
of all the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee and
Institutional Review Board of the Third Affiliated Hospital of Sun
Yat-sen University-Yuedong Hospital (approval no. 2021-18; Meizhou,
China).
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
World Health Organization, Breast Cancer.
https://www.who.int/news-room/fact-sheets/detail/breast-cancer,
2021. Accessed on January 8, 2022.
|
|
2
|
Harbeck N, Penault-Llorca F, Cortes J,
Gnant M, Houssami N, Poortmans P, Ruddy K, Tsang J and Cardoso F:
Breast cancer. Nat Rev Dis Primers. 5(66)2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rodriguez C, Ji M, Wang HL, Padhya T and
McMillan SC: Cancer pain and quality of life. J Hosp Palliat Nurs.
21:116–123. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Costa WA, Monteiro MN, Queiroz JF and
Gonçalves AK: Pain and quality of life in breast cancer patients.
Clinics (Sao Paulo). 72:758–763. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Neufeld NJ, Elnahal SM and Alvarez RH:
Cancer pain: A review of epidemiology, clinical quality and value
impact. Future Oncol. 13:833–841. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Anekar AA and Cascella M: WHO analgesic
ladder. In: StatPearls [Internet]. Treasure Island (FL): StatPearls
Publishing, 2021.
|
|
7
|
Scarborough BM and Smith CB: Optimal pain
management for patients with cancer in the modern era. CA Cancer J
Clin. 68:182–196. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Smyth CE, Jarvis V and Poulin P: Brief
review: Neuraxial analgesia in refractory malignant pain. Can J
Anaesth. 61:141–153. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Xu ZZ, Li HJ, Li MH, Huang SM, Li X, Liu
QH, Li J, Li XY, Wang DX and Sessler DI: Epidural
anesthesia-analgesia and recurrence-free survival after lung cancer
surgery: A randomized trial. Anesthesiology. 135:419–432.
2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kinoshita J, Fushida S, Kaji M, Oyama K,
Fujimoto D, Hirono Y, Tsukada T, Fujimura T, Ohyama S, Yabushita K,
et al: A randomized controlled trial of postoperative intravenous
acetaminophen plus thoracic epidural analgesia vs thoracic epidural
analgesia alone after gastrectomy for gastric cancer. Gastric
Cancer. 22:392–402. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sjøgren P, Gefke K, Banning AM, Parslov M
and Overgaard Olsen LB: Lumbar epidurography and epidural analgesia
in cancer patients. Pain. 36:305–309. 1989.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ju Y, Tian D, Tan Y and Fu Z: Palliative
care with cervical intrathecal infusion and external pump for a
late-stage cancer patient with refractory pain: A case report.
Medicine (Baltimore). 97(e9714)2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Uehara Y, Matsumoto Y, Kosugi T, Sone M,
Nakamura N, Mizushima A, Miyashita M, Morita T, Yamaguchi T and
Satomi E: Availability of and factors related to interventional
procedures for refractory pain in patients with cancer: A
nationwide survey. BMC Palliat Care. 21(166)2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Menon M, Taha N, Purohit N, Kothari V and
Singh S: Continuous cervical epidural analgesia in metastatic
spinal cord compression. Indian J Palliat Care. 22:507–510.
2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Manion SC and Brennan TJ: Thoracic
epidural analgesia and acute pain management. Anesthesiology.
115:181–188. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Qin W, Zhao L, Liu B, Yang Y, Mao P, Xu L,
Li P, Shang Y, Zhang L and Fan B: Comparison of external system and
implanted system in intrathecal therapy for refractory cancer pain
in China: A retrospective study. Brain Behav.
13(e2851)2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Quintana AN, Guragain R, Dean S, Moore A
and Lee L: Spinal ependymoma identified following spinal anesthesia
for cesarean delivery. Cureus. 13(e12558)2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kim JH, Jung JY and Cho MS: Continuous
intrathecal morphine administration for cancer pain management
using an intrathecal catheter connected to a subcutaneous injection
port: A retrospective analysis of 22 terminal cancer patients in
Korean population. Korean J Pain. 26:32–38. 2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Abd-Sayed A, Fiala K, Weisbein J, Chopra
P, Lam C, Kalia H, Jassal N, Gulati A, Sayed D and Deer T:
Intrathecal drug delivery systems survey: Trends in utilization in
pain practice. J Pain Res. 15:1305–1314. 2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
De Andres J, Hayek S, Perruchoud C,
Lawrence MM, Reina MA, De Andres-Serrano C, Rubio-Haro R, Hunt M
and Yaksh TL: Intrathecal drug delivery: Advances and applications
in the management of chronic pain patient. Front Pain Res
(Lausanne). 3(900566)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Suksompong S, von Bormann S and von
Bormann B: Regional catheters for postoperative pain control:
Review and observational data. Anesth Pain Med.
10(e99745)2020.PubMed/NCBI View Article : Google Scholar
|