Introduction
Trabeculectomy (TRAB) is one of the most frequently
performed and an effective surgical methods to manage glaucoma
worldwide (1,2). Its success depends on the formation
and maintenance of the filtering bleb. Bleb scarring is the leading
cause of surgical failure. Antimetabolites, including mitomycin C
and 5-fluorouracil (5-FU), are commonly used intraoperatively or
postoperatively to prevent bleb scarring. Since fibrosis after
surgery may not be completely prevented, an effective method for
clinicians to observe potential signs of scarring is essential for
appropriate postoperative management. The literature revealed that
bleb morphology is an indicator to predict long-term prognosis,
besides intraocular pressure (IOP) (3,4). The
bleb morphological features may get worse before the IOP worsens
(5). Multiple studies have focused
on developing a classification system to evaluate the bleb,
resulting in the invention of different classical bleb grading
systems (3,4,6,7).
Several classifications have been applied in various studies and
have indicated good interobserver agreements, such as the Moorfield
Bleb Grading System (MBGS) (6),
the Indiana Bleb Appearance Grading Scale (IBAGS) (4), the Mainz Bleb Appearance Grading
System (MaBAGS) (7) and the
Wuerzburg Bleb Classification System (WBCS) (3,8)
(Table I). Compared with other
grading systems, the WBCS is much simpler to apply in clinical
practice. It was developed in 1998 and evaluates blebs according to
four parameters, namely vascularity, corkscrew vessels,
encapsulation and microcysts (3).
Previous cross-sectional and retrospective studies suggested that
the WBCS correlates well with the IOP after TRAB (3,8,9).
 | Table IWuerzburg bleb classification
system. |
Table I
Wuerzburg bleb classification
system.
| Item | Scoring |
|---|
| Vascularity | 3=avascular |
| | 2=similar to
adjacent conjunctiva |
| | 1=increased |
| | 0=massive |
| Corkscrew
vessels | 3=none |
| | 2=in one third |
| | 1=in two
thirds |
| | 0=entire bleb |
| Encapsulation | 3=none |
| | 2=in one third |
| | 1=in two
thirds |
| | 0=entire bleb |
| Microcysts | 3=entire bleb |
| | 2=lateral or medial
of the flap |
| | 1=over the scleral
flap |
| | 0=none |
Since bleb grading systems are based on the
slit-lamp examination or photograph, apparent defects are detected
it has obvious shortcomings when assessing the internal bleb
structure (7,10,11).
In the last few years, imaging techniques have been utilized to
investigate the bleb structure. Anterior segment optical coherence
tomography (ASOCT) has become the most favorable procedure, as it
allows quick, non-contact, high-resolution bleb imaging. It
provides details of bleb structure, such as the thickness of the
bleb wall, microcysts and subconjunctival cavity. Numerous studies
have investigated the morphologic characteristics of blebs using
ASOCT to identify the parameters that correlate with IOP or
surgical outcomes (12,13). ASOCT is also useful for assisting
the bleb intervention in clinical practice (14).
In the present study, it was hypothesized that the
combination of ASOCT and WBCS provides more comprehensive bleb data
and is easier to apply in clinical practice and research compared
with evaluations using the ASOCT or WBCS alone. To the best of our
knowledge, the present study was the first to evaluate the
correlation between ASOCT-assisted WBCS and IOP, as well as the
predictive value of ASOCT-assisted WBCS for long-term surgical
outcomes. We also found the parameter that is most valuable for
predicting long-term surgical success in the present study.
Patients and methods
Patient selection
The present study was a prospective, observational
study. Patients that were admitted to The Third People's Hospital
of Chengdu (Chengdu, China) for TRAB surgery from January to June
2021 were recruited. The inclusion criteria were as follows: i)
Aged between 18 and 80 years; ii) diagnosed with primary glaucoma,
including primary open-angle glaucoma, chronic primary
angle-closure glaucoma and normal-tension glaucoma; iii) IOP >21
mmHg with medication or medication intolerance; iv) no previous
glaucoma laser treatment in the last month; v) no previous
intraocular surgery in the last 3 months; vi) without any systemic
disease that would affect wound healing and participating in the
routine follow-ups; and vii) no allergic history of
antimetabolites. The protocol was approved by the Ethical and
Research Committee of The Third People's Hospital of Chengdu
(Chengdu, China) and written informed consent was provided by each
patient.
Preoperative data
Demographic information of the patients was
recorded, including age, sex, number of anti-glaucoma drops, as
well as any related ocular or systemic disease history. All
patients underwent an exhaustive ophthalmic examination
preoperatively, including best-corrected visual acuity (BCVA), the
average IOP of three instances using a tonometer (Reichert 7
auto-tonometer; Reichert, Inc.), central corneal thickness, visual
field (Humphrey® Field Analyzer 3; Carl Zeiss Meditec,
Inc.), disc damage likelihood scale (DDLS) and average retinal
nerve fiber layer thickness measured by OCT (Cirrus HD-OCT; Carl
Zeiss Meditec, Inc.).
Trabeculectomy and follow-ups
The patients in the present study were subjected to
standard clinical practice. All of the eyes underwent fornix-based
trabeculectomy with 5-FU (10 ml/0.25 mg; Jinyao Meditec) by an
experienced glaucoma specialist. Any anti-glaucoma drops with
Prostaglandin analogue were ceased 3 days before the surgery.
Postoperative medications included topical steroid drops
(prednisolone acetate, 1%) four times per day, which was tapered
off between 4-6 weeks, and antibiotic drops (levofloxacin, 0.5%)
four times per day for 2-3 weeks. Follow-up visits were set at 2
weeks and 1, 2, 3, 6 and 12 months following surgery. Examinations
at each visit included BCVA, IOP, slit-lamp examination and bleb
imaging using ASOCT. Visual field and DDLS were measured at
postoperative month (POM) 6 and 12.
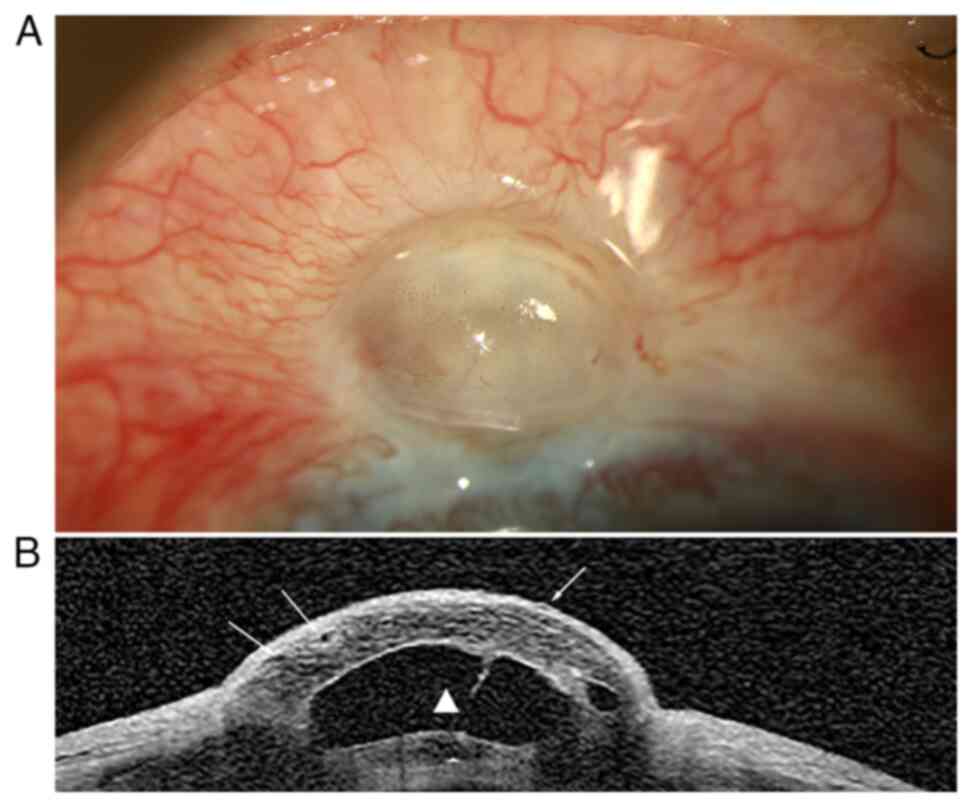
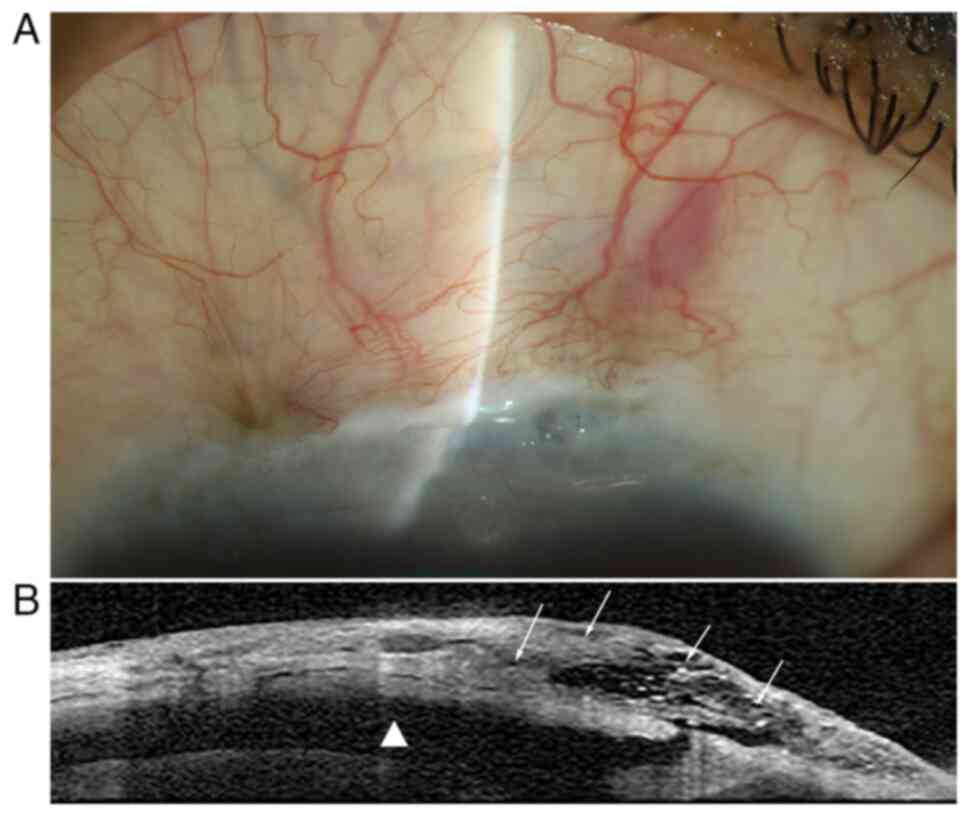
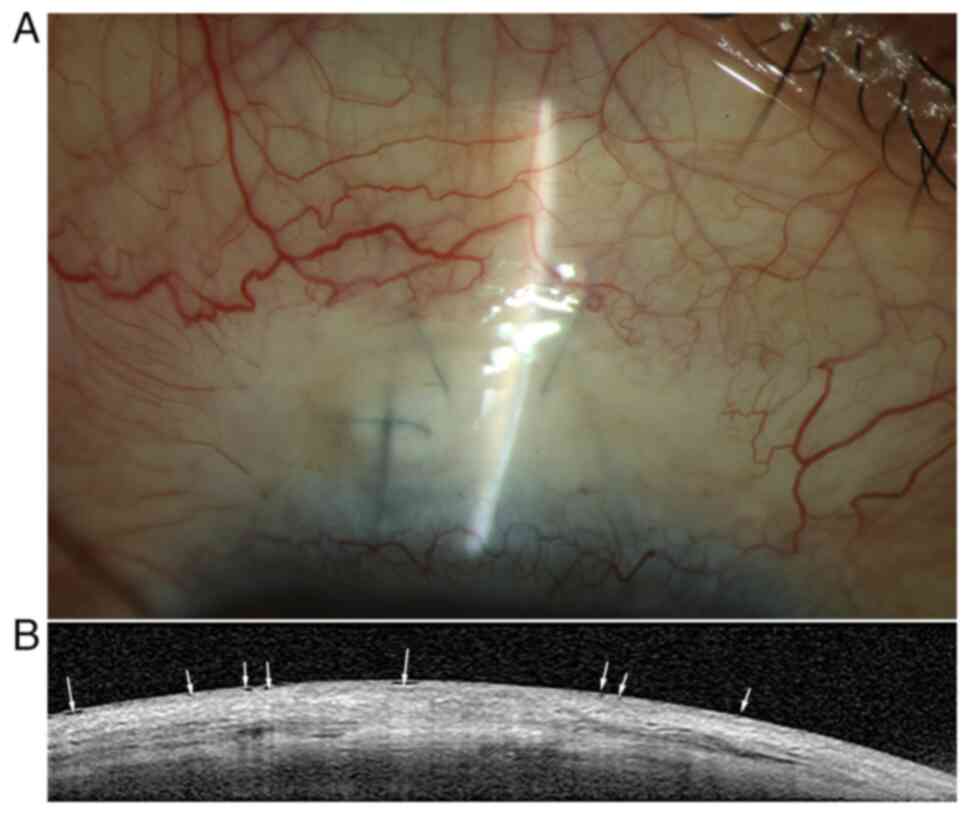
ASOCT-assisted WBCS. ASOCT images of blebs
were acquired by a single technician blinded to the clinical
examination result using the SPECTRALIS® Anterior
Segment Module system (OCT; Heidelberg Engineering, Inc.). The
patients were requested to look down, following which the examiner
lifted the upper eyelids gently for optimal exposure. Raster
10-line horizontal scans (21 images; line length, 8.3 mm) that
centered on the apex of the bleb were acquired. A single
ophthalmologist scored two WBCS parameters (vascularity and
corkscrew vessels) under a slit-lamp and scored the other two
parameters (encapsulation and microcysts) using ASOCT images
(representative images provided in Fig. 1, Fig.
2 and Fig. 3) without knowing
the IOP. The scoring of microcysts was based on their extent and
location on the ASOCT images. Images of blebs were also acquired
under a slit-lamp (BX900; Haag-Streit).
Surgical outcomes. The surgical outcomes of
each eye at 1 year were defined as follows: i) Success (5≤21 mmHg
IOP without topical glaucoma medication or bleb needling); or ii)
failure (5≤21 mmHg IOP with topical glaucoma medication or bleb
needling, or IOP >21 mmHg).
Statistical analysis
Variables were presented as the mean ± the standard
deviation (for normal distributions) or medians and interquartile
ranges (IQR; for non-normal distributions). The Shapiro-Wilk test
was used to evaluate the normality of data distribution. Spearman's
coefficient was used to assess the correlations between WBCS scores
and IOP. The Friedman test followed by the Nemenyi test was used to
compare the difference of scores among visits, while
repeated-measures ANOVA followed by the Bonferroni test was used to
compare IOP among visits. Comparisons between two outcome groups
were analyzed using the Mann-Whitney U-test. The data were analyzed
using SPSS version 20.0 (IBM Corp.). P<0.05 was considered to
indicate statistical significance.
Results
Demographic and preoperative
information
A total of 32 patients (32 eyes) were included in
the present study. Table II
summarizes the baseline demographic and preoperative clinical
characteristics. The average age of all individuals was 59 (53.5,
63.2) years, with 9 males and 23 females participating.
 | Table IIDemographic data and preoperative
information of the patients (n=32). |
Table II
Demographic data and preoperative
information of the patients (n=32).
| Characteristic | Value |
|---|
| Sex | |
|
Male | 9 (28.1) |
|
Female | 23 (71.9) |
| Age, years | 59 (53.5,
63.2) |
| Diagnosis | |
|
Primary
open-angle glaucoma | 14 (43.8) |
|
Primary
angle-closure glaucoma | 18 (56.2) |
| No. of topical
glaucoma medications | 2 (2, 3) |
| Preoperative
examination | |
|
BCVA,
decimal | 0.7±0.3 |
|
IOP,
mmHg | 35.9±11.6 |
|
Visual field
mean deviation, dB | -17.3±9.0 |
|
DDLS | 5 (4.25, 6.75) |
|
ARNFL
thickness, µm | 65 (60, 85) |
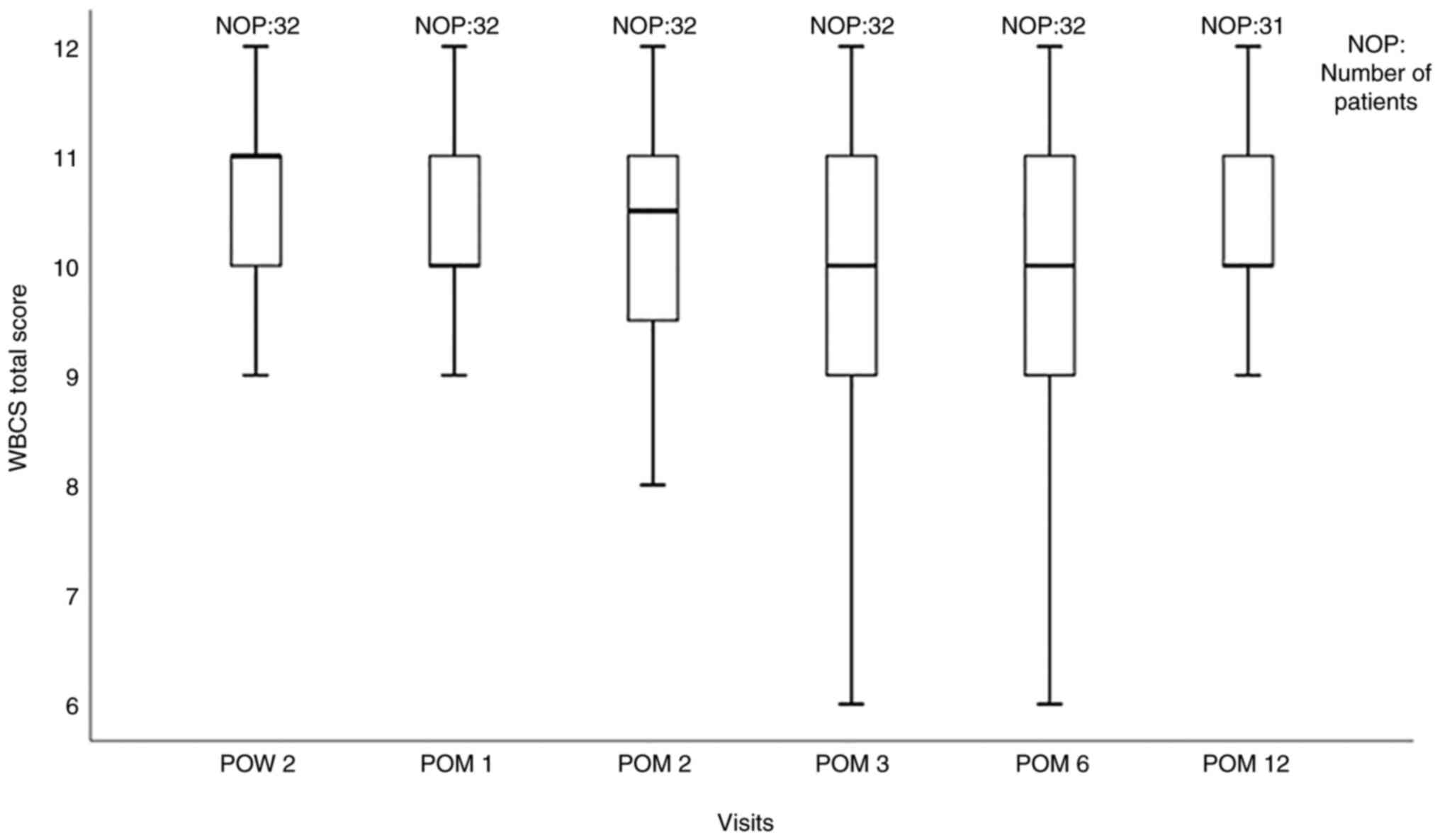
WBCS scores
The median WBCS total score was 11.0 (IQR, 10-11) at
postoperative week (POW) 2, 10 (IQR, 10-11) at POM 1, 10.5 (IQR,
9.25-11) at POM 2, 10 (IQR, 9-11) at POM 3, 10 (IQR, 9-11) at POM 6
and 10 (IQR, 10-11) at POM 12. A box-and-whiskers diagram indicated
that the total score was the highest at POW 2, then declined at POM
1 and stabilized after POM 3 (Fig.
4). The Friedman test followed by the Nemenyi test did not
indicate any significant difference between any two postoperative
visits within 1 year (P>0.05).
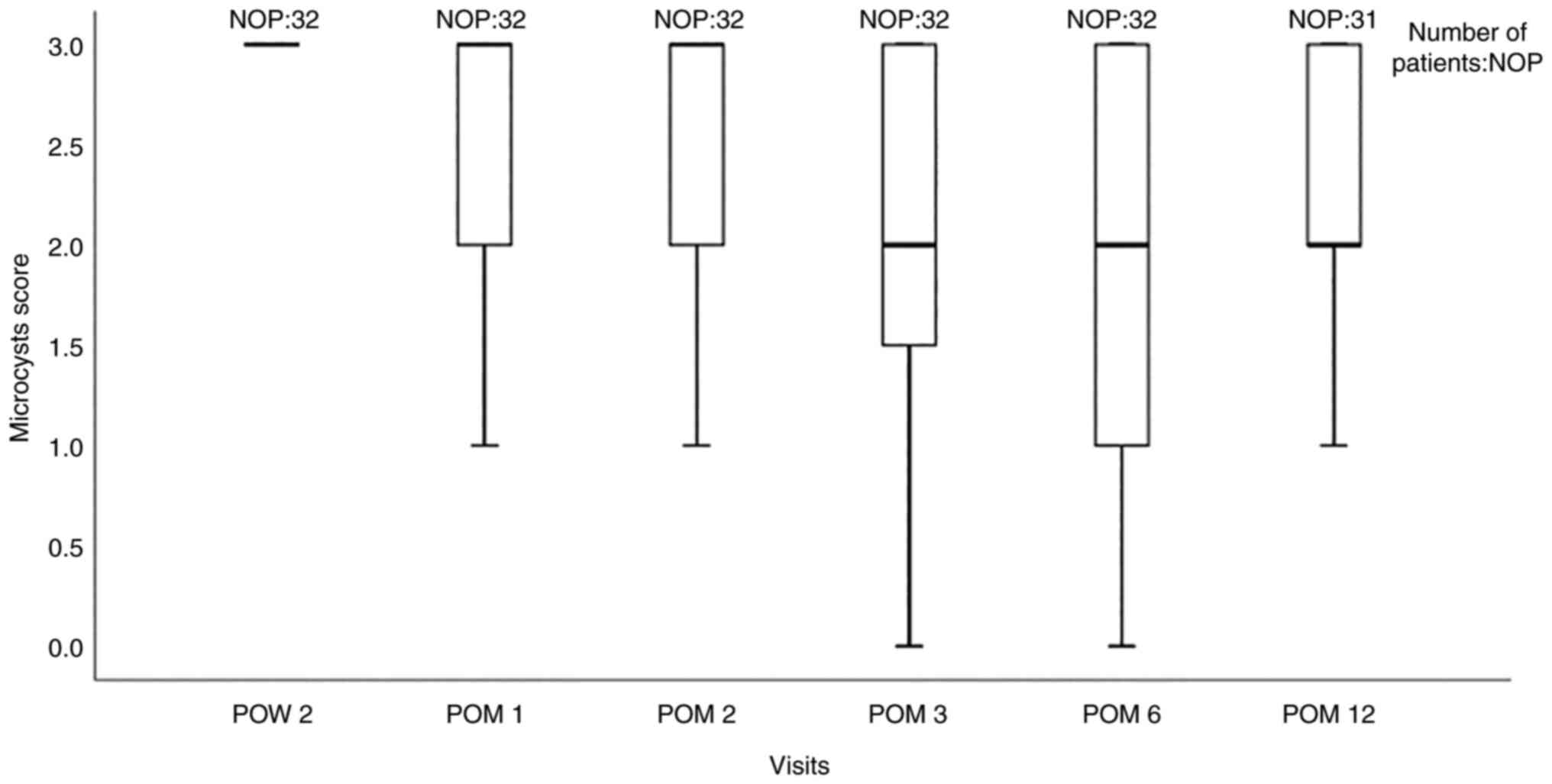
Among the four single parameters in the WBCS, there
were no significant differences in vascularity (median, 2;
P>0.05), corkscrew vessels (median, 3; P>0.05) nor
encapsulation (median, 3; P>0.05) scores between any two visits.
The microcysts score had a median of 3 (IQR, 3-3) at POW 2 and 3
(IQR, 2-3) at POM 1, and then gradually declined from 3 (IQR, 2-3)
at POM 2 to 2 (IQR, 1.25-3) at POM 3. The microcysts score became
more stable after POM 3 (Fig. 5).
The Friedman test found a significant difference in microcysts
scores (P<0.001) and a subsequent Nemenyi test found differences
between POW 2 and POM 3 (P=0.034) and POM 12 (P=0.05),
respectively.
IOP
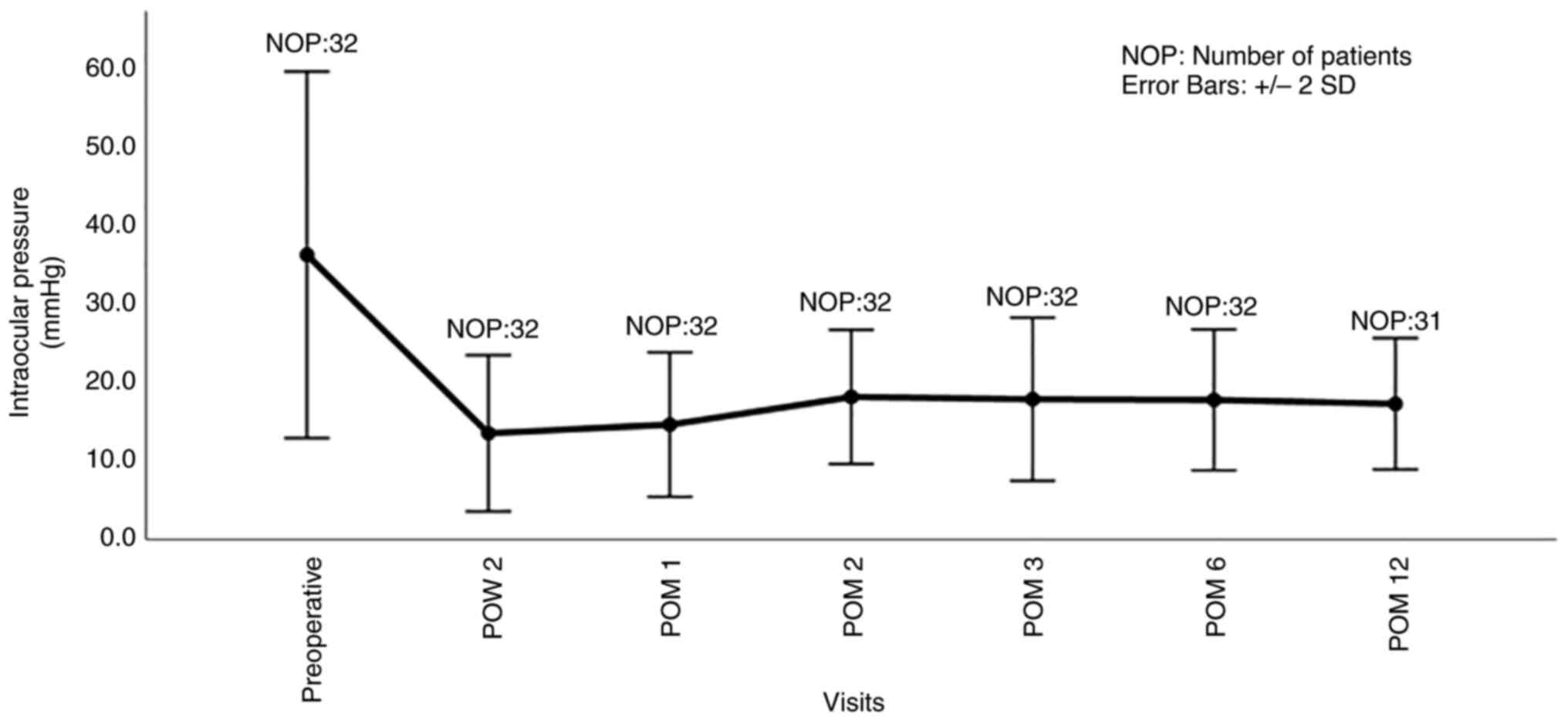
The lowest IOP during 1 year following surgery was
13.4±4.9 mmHg at POW 2. Subsequently, the IOP gradually increased
to 14.5±4.6 mmHg at POM 1 and 18.0±4.2 mmHg at POM 2, before
becoming more stable with 17.7±5.1 mmHg at POM 3, 17.6±4.5 mmHg at
POM 6 and 17.1±4.5 mmHg at the end of the study period. The IOP at
the six postoperative follow-ups was significantly decreased
compared with the preoperative IOP (P<0.001). Among the six
postoperative visits, significant differences were found between
POW 2 and POM 2 (P=0.001), POM 3 (P=0.024) and POM 6 (P=0.013), as
well as between POM 1 and POM 2 (P=0.003) (Fig. 6).
Correlation of WBCS scores and
IOP
The correlation between the WBCS (total scores and
scores of single parameters) and IOP at each visit was analyzed.
Negative correlations between total scores and IOP at each visit
(r<-0.4; P<0.05), except at POW 2, were found. Among
the four single parameters, the microcysts score correlated with
the IOP at each visit except POW 2. The correlation was strongest
at the final visit (r=-0.640; P<0.001). The vascularity
score negatively correlated with the IOP at POM 3 (r=-0.433;
P=0.013) and POM 6 (r=-0.664; P<0.001). The corkscrew
score negatively correlated with IOP at the early visit after
surgery (r=-0.378; P=0.033; POW 2). The encapsulation score
negatively correlated with IOP at POW 2 (r=-0.413; P=0.019)
and POM 3 (r=-0.397; P=0.025) (Table III).
 | Table IIIWuerzburg bleb classification system
scores that correlated with intraocular pressure. |
Table III
Wuerzburg bleb classification system
scores that correlated with intraocular pressure.
| Follow-up
time/parameter | r | P-value |
|---|
| POW 2 | | |
|
Corkscrew
vessels | -0.378 | 0.033 |
|
Encapsulation | -0.413 | 0.019 |
| POM 1 | | |
|
Total
score | -0.451 | 0.010 |
|
Microcysts | -0.364 | 0.040 |
| POM 2 | | |
|
Total
score | -0.502 | 0.003 |
|
Microcysts | -0.410 | 0.020 |
| POM 3 | | |
|
Total
score | -0.642 | <0.001 |
|
Vascularity | -0.433 | 0.013 |
|
Encapsulation | -0.397 | 0.025 |
|
Microcysts | -0.554 | 0.001 |
| POM 6 | | |
|
Total
score | -0.628 | <0.001 |
|
Vascularity | -0.664 | <0.001 |
|
Microcysts | -0.488 | 0.005 |
| POM 12 | | |
|
Total
score | -0.726 | <0.001 |
|
Microcysts | -0.640 | <0.001 |
Surgical outcomes and
complications
With regards to surgical outcomes, 15/32 (43.8%)
patients achieved success, while 17/32 (56.2%) patients failed to
meet the success criteria. Among the latter group, 13 patients had
an IOP of ≤21 mmHg with medication or bleb needling, three patients
had an IOP of >21 mmHg with medication, while one patient had
another glaucoma surgery at POM 7 for losing IOP control. As for
surgical complications, one patient (3.1%) had branch retinal vein
occlusion and macular edema at 6 months following surgery.
Temporary exudative choroiditis occurred in two patients (6.3%). A
temporary shallow anterior chamber occurred in one patient (3.1%)
(data not shown).
Postoperative antimetabolites and
medication
A total of 12 eyes (37.5%) had been treated with
bleb needling and subconjunctival injection of 5-FU (0.005 mg/0.2
ml; Jinyao Meditec) once, since signs of encapsulation had been
observed. At the final visit, seven eyes (21.9%) received one
topical medication and two eyes (6.25%) received two topical
medications (data not shown).
Correlations of WBCS with surgical
outcomes
The prognostic value of ASOCT-assisted WBCS depends
on its correlation with long-term outcomes. Table IV presents the parameters that
correlated with such outcomes. The WBCS total score and microcysts
score were highly correlated with outcomes (r<-0.4;
P<0.05), except at POW 2 and POM 1. The encapsulation score
correlated with the outcome at POM 2 and 3. The vascularity score
correlated with the outcome at POM 6.
 | Table IVWuerzburg bleb classification system
scores that correlated with outcomes. |
Table IV
Wuerzburg bleb classification system
scores that correlated with outcomes.
| Follow-up
time/parameter | r | P-value |
|---|
| POM 2 | | |
|
Total
score | -0.630 | <0.001 |
|
Encapsulation | -0.403 | <0.001 |
|
Microcysts | -0.592 | <0.001 |
| POM 3 | | |
|
Total
score | -0.500 | 0.004 |
|
Encapsulation | -0.403 | 0.022 |
|
Microcysts | -0.586 | <0.001 |
| POM 6 | | |
|
Total
score | -0.663 | <0.001 |
|
Vascularity | -0.443 | <0.001 |
|
Microcysts | -0.664 | <0.001 |
| POM 12 | | |
|
Total
score | -0.488 | 0.005 |
|
Microcysts | -0.415 | 0.020 |
The difference in all parameters between the two
outcome groups (success or failure) was measured. Table V presents the parameters that
differed significantly between groups (P<0.05). The result was
consistent with that of the Spearman analysis and indicated that
the WBCS total score and microcysts score were significantly higher
in the success group compared with the failure group at POM 2, 3, 6
and 12 (P<0.05). The vascularity score was significantly higher
in the success group compared with the failure group at POM 6
(P=0.014) and the encapsulation score was significantly higher in
the success group compared with the failure group at POM 2 and 3
(both P=0.025).
 | Table VComparison of WBCS scores between the
two outcome groups. |
Table V
Comparison of WBCS scores between the
two outcome groups.
| A, WBCS total
score |
|---|
| | Median
(interquartile range) | |
|---|
| Follow-up time | Success group | Failure group | P-value |
|---|
| POW 2 | 11 (10, 11) | 11 (10.5, 11) | 0.772 |
| POM 1 | 11 (10, 11) | 10 (9.5, 11) | 0.059 |
| POM 2 | 11 (11, 12) | 10 (9, 10) | <0.001 |
| POM 3 | 11 (10, 11) | 9 (7.5, 10.5) | 0.005 |
| POM 6 | 11 (10, 12) | 9 (8, 10.5) | <0.001 |
| POM 12 | 11 (10, 11) | 10 (9, 10.75) | 0.008 |
| B, WBCS vascularity
score |
| | Median
(interquartile range) | |
| Follow-up time | Success group | Failure group | P-value |
| POW 2 | 2 (2, 3) | 2 (2, 2.5) | 0.674 |
| POM 1 | 2 (2, 3) | 2 (1.5, 3) | 1.000 |
| POM 2 | 2 (2, 3) | 2 (1, 3) | 0.348 |
| POM 3 | 2 (2, 3) | 2 (1, 3) | 0.641 |
| POM 6 | 2 (2, 3) | 2 (1, 2) | 0.014 |
| POM 12 | 2 (2, 3) | 2 (2, 2) | 0.261 |
| C, WBCS
encapsulation score |
| | Median
(interquartile range) | |
| Follow-up time | Success group | Failure group | P-value |
| POW 2 | 3 (3, 3) | 3 (3, 3) | 0.177 |
| POM 1 | 3 (3, 3) | 3 (2.5, 3) | 0.188 |
| POM 2 | 3 (3, 3) | 3 (2, 3) | 0.025 |
| POM 3 | 3 (3, 3) | 3 (2, 3) | 0.025 |
| POM 6 | 3 (3, 3) | 3 (3, 3) | 0.093 |
| POM 12 | 3 (3, 3) | 3 (3, 3) | 0.333 |
| D, WBCS microcysts
score |
| | Median
(interquartile range) | |
| Follow-up time | Success group | Failure group | P-value |
| POW 2 | 3 (2, 3) | 3 (3, 3) | 0.173 |
| POM 1 | 3 (2, 3) | 2 (2, 3) | 0.197 |
| POM 2 | 3 (3, 3) | 2 (1, 3) | 0.001 |
| POM 3 | 3 (2, 3) | 2 (1, 2) | 0.001 |
| POM 6 | 3 (2, 3) | 1 (1, 2) | <0.001 |
| POM 12 | 2 (2, 3) | 2 (1, 2) | 0.023 |
Discussion
Since postoperative bleb scarring is the leading
cause of trabeculectomy failure (15), appropriate management of blebs,
such as the use of anti-inflammation medication, bleb massage, bleb
needling or subconjunctival injection of antimetabolites at the
early stage of fibrosis, is necessary (14,16,17).
It is a challenge for ophthalmologists to find an objective,
effective and quick tool to assess the blebs within a limited
outpatient follow-up time to predict subsequent problems and
long-term effects, which would help guide the subsequent
management.
A number of studies have employed MBGS and IBAGS for
bleb evaluation (4,6,18).
MBGS grades blebs based on the severity of vascularity, bleb wall
thickness, height, diffusion and width, with each parameter being
scored from 1-10(6). IBAGS is very
simple to assess blebs in terms of bleb height, extent, vascularity
and the Seidel test, with each item being graded from 1-4(4). However, neither system evaluates
microcysts (10), which have been
proven to correlate with a lower IOP (18). Hereafter, Hoffmann et al
(7) developed the MaBAGS
classification, which involves the grading of microcysts. Contrary
to expectation, they found a low level of interobserver agreement
for the grading of microcysts. Previous studies have found WBCS is
practical in the clinic and suitable for immediate bleb evaluation
under the slit-lamp or from photography (3,8,9,14).
However, it is difficult to grade encapsulation and microcysts
without obtaining enough internal bleb information.
Ultrasound biomicroscopy was first used to evaluate
the internal bleb, but it is time-consuming and may cause infection
(19). ASOCT has been preferred
due to its high-resolution images and cross-sectional scanning
mode, which provide detailed insight into the inner structure of
the bleb (11,20-23).
In spite of several studies committed to developing standard
classifications of blebs based on ASOCT images, blebs with mixed
morphologies remain challenging to classify. Therefore, more
studies focused on combining the ASOCT and classical grading
systems from different perspectives are required. Oh et al
(24) investigated blebs with
IBAGS and ASOCT and found that a higher/bulged bleb may indicate a
lower IOP. Wen et al (25)
found that ASOCT and MBGS grades of vascularity are correlated.
In the present study, ASOCT was adopted for WBCS
assessment, since ASOCT may ideally help to grade two critical
parameters, namely encapsulation and microcysts. The grading result
was hypothesized to be more accurate and objective, and thus better
correlated with clinical outcomes, such as IOP.
The present results indicated that the WBCS total
scores negatively correlated with IOP at each visit, except POW 2,
which is similar to the results reported by Thatte et al
(9). The correlation became
stronger over the course of the 1-year follow-up. Furthermore,
compared with previous cross-sectional and retrospective studies
(3,8,9), the
findings of the present study indicated a stronger correlation
between WBCS and IOP.
The WBCS total score was good at POW 2, with the
median >10 points and also highest among all visits. The total
score decreased at POM 1 and then increased at POM 2. The natural
process of bleb formation may explain this trend (26,27).
It was observed in the present study that it takes an average time
of 1-2 months for a mature bleb to form. The initial bleb
morphology was mostly diffused and transparent, leading to better
scores in the early postoperative inflammation phase. When the
fibrosis started to develop in the proliferative phase, the scores
decreased due to increased vascularity and encapsulation. For
instance, at POM 1, six patients with increased bleb vascularity
were identified and several patients exhibited varying degrees of
bleb encapsulation. This may result in lower WBCS total scores. The
intervention that included bleb needling or modified medicine
following POM 1 may have contributed to the improvement of scores
at POM 2. The morphologic change of blebs became slower compared
with the previous state when the extended remodeling phase
gradually began, which may be why the total scores stabilized
following POM 3. In a prior study conducted by Klink et al
(8), the WBCS total score at 1
year was 9.8±1.3 in the success group and 9.3±1.4 in the failure
group. It may be hypothesized that in the present study, ASOCT
increased the accuracy of WBCS and may have helped to obtain a
higher score. Although the median of the total score was ~10 over
time, significant differences were found between the two outcome
groups at POM 2, 3, 6 and 12. A significant correlation between
WBCS total scores and outcomes at POM 2, 3, 6 and 12 was also
found, suggesting that a higher score may indicate a tendency for
an improved long-term prognosis. The agreements of the
aforementioned two statistical methods suggested that the WBCS
total score of POM 2 and the subsequent visits may predict
long-term surgical outcomes. A higher score may be associated with
better outcome.
Furthermore, a correlation analysis was performed on
single parameters of WBCS with IOP and surgical outcomes, and it
was explored whether any of them may be potential ‘keys’ for
outcome prediction. The correlation between microcysts and IOP at
both early and late postoperative stages (POM 1, 2, 3, 6 and 12)
was significant, suggesting that patients with more microcysts had
lower IOP. This finding is consistent with previous reports
(3,18,28,29).
The difference in microcysts scores between the two outcome groups
at POM 2, 3, 6 and 12 was significant, and was also highly
correlated with surgical outcomes at these time-points
(r<-0.4; P<0.05). Therefore, it was concluded that the
detection of more microcysts at POM 2 and POM 3, 6 and 12 at the
following visits may imply a higher tendency of the long-term
success of TRAB and vice versa. The microcysts scores were
high at the early stage, then decreased after POM 2 and became
stable after POM 3. This finding differs from that of Klink et
al (8), who found that the
microcysts score was lowest following surgery, increased until POM
6 and then declined until POM 12. On the other hand, Kumaran et
al (18) discovered that the
percentage of patients with microcysts peaked at week 6 for eyes
treated with 5-FU, similarly to the observation of the present
study. According to earlier studies, the presence of microcysts
implies aqueous drainage beneath the conjunctiva, suggesting a
lower IOP (18,28). The results of the present study
support this theory. The decline of the microcysts score from POW 2
to POM 3 and subsequent visits was mostly in line with the rise of
IOP from POW 2 to POM 3. The current findings implied that ASOCT
may allow for better observation of microcysts than the traditional
examination method.
Congestion of the bleb area and growth of corkscrew
vessels (4,6,18,29)
represent the aggravation of vascularity, indicating the
possibility of TRAB failure. OCT angiography also demonstrated the
increase of vessel density during bleb fibrosis (20). To ensure the objectivity of
vascularity assessment, patients with acute angle-closure or
secondary glaucoma, and patients who had previous laser treatment
or intraocular surgery, were excluded. In addition, prostaglandin
analogue drops were ceased ≥3 days prior to surgery, since they may
incite conjunctival inflammation and adversely affect the outcome.
The association of bleb vascularity and IOP was investigated and
significant correlations at POM 3 and 6 were found. Similarly, Wen
et al (25) compared the
ASOCT bleb grading system with MBGS and found a worse ASOCT bleb
grade to be correlated with a high IOP at POM 4 and 6, though the
correlation was no longer significant at POM 12. Regarding the
relationship between vascularity and long-term surgical outcome,
Klink et al (8) reported
that the complete success group in their study had a higher score
for vascularity parameters compared with that of the qualified
success group and failure group. In the present study, only the
score of vascularity at POM 6 was found to significantly correlate
with surgical outcomes and differ significantly between the two
outcome groups. One explanation of the above fair correlation is
that WBCS may not have sufficient sensitivity to reveal a minimal
change of vascularity over time. Compared with MBGS, WBCS does not
evaluate the vascularity in different bleb areas, and thus, it may
not be able to detect the early vascularization in the bleb edge,
which leads to a relatively higher (better) score at the early
stage.
Certain eyes developed typical corkscrew vessels
(CS) in the present study. In a previous study, Klink et al
(8) found no significant
difference in CS between any two postoperative follow-ups within 1
year, while Furrer et al (3) found poor agreement between IOP and
CS. The present study only found that the correlation between CS
and IOP is significant at an early stage (POW 2) and no difference
was found among six follow-ups. In a previous study conducted by
Sacu et al (29), eyes with
CS had a higher risk of encapsulation. They suggested that the
development of CS may be due to the contraction of fibrous
subconjunctival tissue. The current study found CS in three eyes in
the first 2 weeks, and one or two eyes at POM 2, 3, 6 and 12. Most
of these eyes were found to have encapsulation at the same time,
which supports the speculation of Sacu et al (29). Although the current findings
suggest that more CS may be associated with a higher IOP in the
early stages, no further evidence of its prognostic value for
long-term outcomes was found.
Encapsulation was considered to be a significant
parameter that may indicate late bleb failure. A correlation
between encapsulation and IOP at POW 2 and POM 3 was found. This
was consistent with previous studies (8,11).
More serious encapsulation was associated with a higher IOP. It was
also found that encapsulation at POM 2 and 3 was associated with
worse surgical outcomes.
In addition, the encapsulation score at POM 2 and 3
was significantly lower in the success group (P<0.05). No
correlation was observed after POM 3. This may be explained by the
formation process of the encapsulated bleb, which was typically
from POW 2 to POM 2 following TRAB. The non-contractile
collagen-producing fibroblasts are the major component in the
encapsulation process (30).
Although the literature suggests that 5-FU is able to inhibit bleb
scarring, it cannot inhibit encapsulation (30). In the present study, patients with
encapsulation treated with bleb needling and subconjunctival
injection of 5-FU obtained improved encapsulation scores at the
next visit.
In sum, the present study demonstrated that
ASOCT-assisted WBCS is a simple and effective measurement of blebs
in clinical practice. It has a good correlation with IOP except in
the very early postoperative phase (within 1 month) and is well
correlated with surgical outcomes. Among the four single
parameters, microcysts correlated best with surgical outcomes, and
microcysts score may have the potential to predict future outcomes
as early as POM 2. One limitation of the present study is the
relatively small sample size. Besides, the interobserver agreement
of ASOCT-assisted WBCS was not evaluated. Further research is
needed to ascertain the present conclusion.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Health
Commission of Sichuan Province (grant no. 18PJ088).
Availability of data and materials
The datasets generated and/or analyzed during the
current study are not publicly available due to them containing
information that may compromise the privacy of research
participants, but are available from the corresponding author on
reasonable request.
Authors' contributions
JG performed the surgeries, designed and supervised
the study, provided critical revision of the manuscript and
followed up patients. YS participated in designing the study,
patient recruitment, data acquisition, preparation of the
manuscript and patient follow-up. JZ participated in patient
recruitment, data acquisition and patient follow-up. YH
participated in the data acquisition and interpretation of the
image data. ZW contributed to the design of the study and provided
critical revision of the manuscript. JG and YS confirm the
authenticity of the raw data. All authors have read and approved
the final manuscript.
Ethics approval and consent to
participate
The research adhered to the tenets of The
Declaration of Helsinki and the protocol was approved by the
Ethical and Research Committee of The Third People's Hospital of
Chengdu (Chengdu, China; grant no. 2021-S-167). Written informed
consent was provided by each patient.
Patient consent for publication
Consent for publication was obtained from the
patients whose images were included in this article.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Kalarn S, Le T and Rhee DJ: The role of
trabeculectomy in the era of minimally invasive glaucoma surgery.
Curr Opin Ophthalmol. 33:112–118. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Gedde SJ, Feuer WJ, Lim KS, Barton K,
Goyal S, Ahmed II and Brandt JD: Primary Tube Versus Trabeculectomy
Study Group. Treatment outcomes in the primary tube versus
trabeculectomy study after 5 years of follow-up. Ophthalmology.
129:1344–1356. 2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Furrer S, Menke MN, Funk J and
Toteberg-Harms M: Evaluation of filtering blebs using the
‘Wuerzburg bleb classification score’ compared to clinical
findings. BMC Ophthalmol. 12(24)2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Cantor LB, Mantravadi A, WuDunn D,
Swamynathan K and Cortes A: Morphologic classification of filtering
blebs after glaucoma filtration surgery: The indiana bleb
appearance grading scale. J Glaucoma. 12:266–271. 2003.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Picht G and Grehn F: Classification of
filtering blebs in trabeculectomy: Biomicroscopy and functionality.
Curr Opin Ophthalmol. 9:2–8. 1998.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wells AP, Crowston JG, Marks J, Kirwan JF,
Smith G, Clarke JC, Shah R, Vieira J, Bunce C, Murdoch I and Khaw
PT: A pilot study of a system for grading of drainage blebs after
glaucoma surgery. J Glaucoma. 13:454–460. 2004.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Hoffmann EM, Herzog D, Wasielica-Poslednik
J, Butsch C and Schuster AK: Bleb grading by photographs versus
bleb grading by slit-lamp examination. Acta Ophthalmol.
98:e607–e610. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Klink T, Kann G, Ellinger P, Klink J,
Grehn F and Guthoff R: The prognostic value of the wuerzburg bleb
classification score for the outcome of trabeculectomy.
Ophthalmologica. 225:55–60. 2011.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Thatte S, Rana R and Gaur N: Appraisal of
bleb using trio of intraocular pressure, morphology on slit lamp,
and gonioscopy. Ophthalmol Eye Dis. 8:41–48. 2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wells AP, Ashraff NN, Hall RC and Purdie
G: Comparison of two clinical Bleb grading systems. Ophthalmology.
113:77–83. 2006.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Waibel S, Spoerl E, Furashova O, Pillunat
LE and Pillunat KR: Bleb morphology after mitomycin-C augmented
trabeculectomy: Comparison between clinical evaluation and anterior
segment optical coherence tomography. J Glaucoma. 28:447–451.
2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Leung CK, Yick DW, Kwong YY, Li FC, Leung
DY, Mohamed S, Tham CC, Chung-chai C and Lam DS: Analysis of bleb
morphology after trabeculectomy with Visante anterior segment
optical coherence tomography. Br J Ophthalmol. 91:340–344.
2007.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Mastropasqua R, Fasanella V, Agnifili L,
Curcio C, Ciancaglini M and Mastropasqua L: Anterior segment
optical coherence tomography imaging of conjunctival filtering
blebs after glaucoma surgery. Biomed Res Int.
2014(610623)2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Guthoff R, Guthoff T, Hensler D, Grehn F
and Klink T: Bleb needling in encapsulated filtering blebs:
Evaluation by optical coherence tomography. Ophthalmologica.
224:204–208. 2010.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Liu X, Du L and Li N: The effects of
bevacizumab in augmenting trabeculectomy for glaucoma: A systematic
review and meta-analysis of randomized controlled trials. Medicine
(Baltimore). 95(e3223)2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Nakakura S, Noguchi A, Tanabe H, Tabuchi
H, Asaoka R and Kiuchi Y: Outcomes of wider area bleb revision
using bleb knife with adjunctive mitomycin C. J Glaucoma.
28:732–736. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Khaw PT, Chang L, Wong TT, Mead A, Daniels
JT and Cordeiro MF: Modulation of wound healing after glaucoma
surgery. Curr Opin Ophthalmol. 12:143–148. 2001.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Kumaran A, Husain R, Htoon HM and Aung T:
Longitudinal changes in bleb height, vascularity, and conjunctival
microcysts after trabeculectomy. J Glaucoma. 27:578–584.
2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Yamamoto T, Sakuma T and Kitazawa Y: An
ultrasound biomicroscopic study of filtering blebs after mitomycin
C trabeculectomy. Ophthalmology. 102:1770–1776. 1995.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Tominaga A, Miki A, Yamazaki Y, Matsushita
K and Otori Y: The assessment of the filtering bleb function with
anterior segment optical coherence tomography. J Glaucoma.
19:551–555. 2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Seo JH, Kim YA, Park KH and Lee Y:
Evaluation of functional filtering bleb using optical coherence
tomography angiography. Transl Vis Sci Technol.
8(14)2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Hamanaka T, Omata T, Sekimoto S, Sugiyama
T and Fujikoshi Y: Bleb analysis by using anterior segment optical
coherence tomography in two different methods of trabeculectomy.
Invest Ophthalmol Vis Sci. 54:6536–6541. 2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Lim SH: Clinical applications of anterior
segment optical coherence tomography. J Ophthalmol.
2015(605729)2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Oh LJ, Wong E, Lam J and Clement CI:
Comparison of bleb morphology between trabeculectomy and deep
sclerectomy using a clinical grading scale and anterior segment
optical coherence tomography. Clin Exp Ophthalmol. 45:701–707.
2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Wen JC, Stinnett SS and Asrani S:
Comparison of anterior segment optical coherence tomography bleb
grading, moorfields bleb grading system, and intraocular pressure
after trabeculectomy. J Glaucoma. 26:403–408. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Masoumpour MB, Nowroozzadeh MH and
Razeghinejad MR: Current and future techniques in wound healing
modulation after glaucoma filtering surgeries. Open Ophthalmol J.
10:68–85. 2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Seibold LK, Sherwood MB and Kahook MY:
Wound modulation after filtration surgery. Surv Ophthalmol.
57:530–550. 2012.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Nakano N, Hangai M, Nakanishi H, Inoue R,
Unoki N, Hirose F, Ojima T and Yoshimura N: Early trabeculectomy
bleb walls on anterior-segment optical coherence tomography.
Graefes Arch Clin Exp Ophthalmol. 248:1173–1182. 2010.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Sacu S, Rainer G, Findl O, Georgopoulos M
and Vass C: Correlation between the early morphological appearance
of filtering blebs and outcome of trabeculectomy with mitomycin C.
J Glaucoma. 12:430–435. 2003.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Ophir A: Encapsulated filtering bleb. A
selective review-new deductions. Eye (Lond). 6:348–352.
1992.PubMed/NCBI View Article : Google Scholar
|