Introduction
A multilocular thymic cyst (MTC) is a rare
mediastinal tumor which is recognized by a radiologic finding of a
multiloculated cyst-like structure in the anterior mediastinum
(1). It often develops following
inflammatory diseases such as Sjogren's syndrome, human
immunodeficiency virus (HIV) infection and acquired
immunodeficiency syndrome (AIDS) (1). Because similar radiologic features
can be observed in other tumors, such as thymoma, thymic carcinoma,
Hodgkin lymphoma, and seminoma (2), a pathological examination is
necessary for final diagnosis. Particularly, with the improvement
in AIDS prognosis, HIV-associated tumor cases have been increasing,
and caution needs to be exercised in differential diagnosis
(3). MTC in people living with
HIV/AIDS (PLWHA) often involves other HIV/AIDS-related symptoms
such as lymphoid interstitial pneumonia (LIP) and parotid gland
enlargement (4), and asymptomatic
cases are rare.
Since the beginning of the coronavirus disease of
2019 (COVID-19) pandemic, COVID-19 has been associated with
incidentalomas (5,6), as well as various complications owing
to its pro-inflammatory behavior (7), including formation of the cystic
lesions such as hepatic cyst enlargement (8) and pneumatocele formation (9,10).
Severity of COVID-19 is known to be modified by co-infected
pathogens, and individuals who are HIV-infected are reported to be
at higher risk of severe disease (11,12).
However, the relationship between COVID-19 and MTC development in
PLWHA remains unknown. Here, we present a case of asymptomatic MTC
that was incidentally found on a computed tomography (CT) scan
during COVID-19 treatment in a male patient who was HIV
positive.
Case report
A 52-year-old man with a 20-year history of HIV
infection who was undergoing antiretroviral therapy was admitted to
our hospital with a COVID-19 pneumonia. On CT scan performed on day
9 of COVID-19, an anterior mediastinal tumor was incidentally
detected (Fig. 1). There was no
history of smoking, and the clinical history included type-1
diabetes mellitus (Islet Antigen-2 antibody positive),
hypertension, renal failure, and syphilis. The patient was
asymptomatic with no notable findings on physical examination.
Blood examination showed renal dysfunction (urea nitrogen, 25.7
mg/dl; creatinine, 2.41 mg/dl) and hyperglycemia (fasting blood
sugar, 112 mg/dl; hemoglobin A1c, 8.3%; glycoalbumin, 21.0%). Rapid
plasma reagin, Treponema pallidum antibody, HIV antigen, and HIV
antibody tests were positive. Anti-acetylcholine receptor antibody
test was negative, ruling out the possibility of myasthenia gravis.
There was no significant elevation in tumor markers, including
human chorionic gonadotropin β, alpha-fetoprotein, squamous cell
carcinoma antigen, cytokeratin 19 fragments, and carcinoembryonic
antigen. Regarding HIV control, the cluster of differentiation 4
count was decreased (576/µl), and the HIV RNA load was less than 20
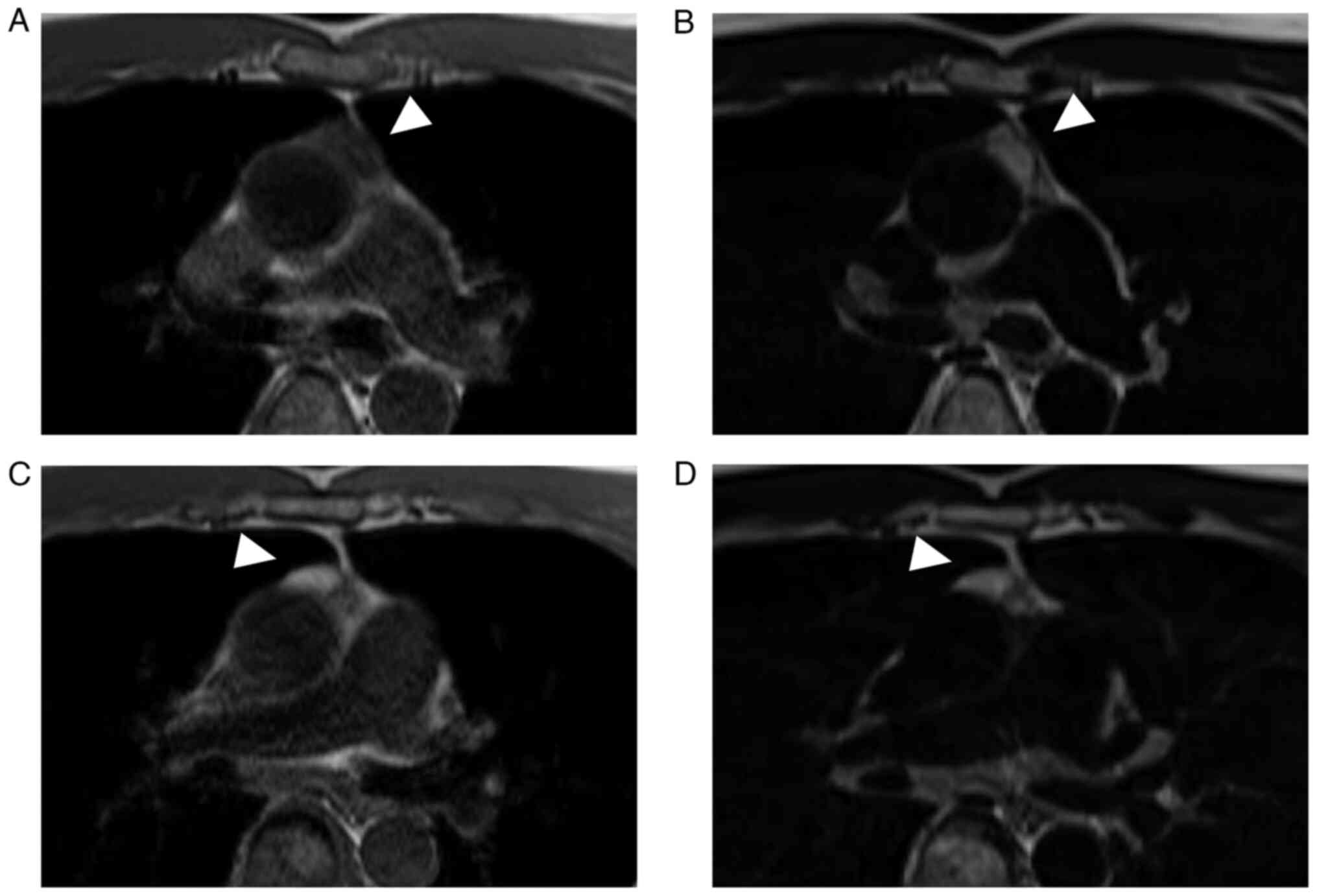
copies/ml. Magnetic resonance imaging revealed a 28-mm bilocular
cyst. One of the two chambers showed low intensity on T1-weighted
images and high intensity on T2-weighted images, whereas the other
chamber showed high intensity on both T1-weighted and T2-weighted
images. No infiltration of the capsule or adjacent organs was
observed (Fig. 2). As malignancy
could not be excluded, robot-assisted thoracoscopic resection of
the anterior mediastinal tumor was performed.
Intraoperatively, the tumor was a cystic lesion
within the thymus located just anterior to the pericardium and
caudal to the left brachiocephalic vein. There were diffuse smaller
cystic lesions within the thymus, and the non-cystic thymic tissue
exhibited an uneven surface, suggesting hyperplasia. Thymectomy was
performed. The resected tissue was composed of multiple cysts of
various sizes containing exudative turbid yellow fluid (total
protein, 6.3 g/dl; lactate dehydrogenase, 1676 U/L) with lymphocyte
predominance (white blood cells, 44.0x103/l; lymphocyte,
94%).
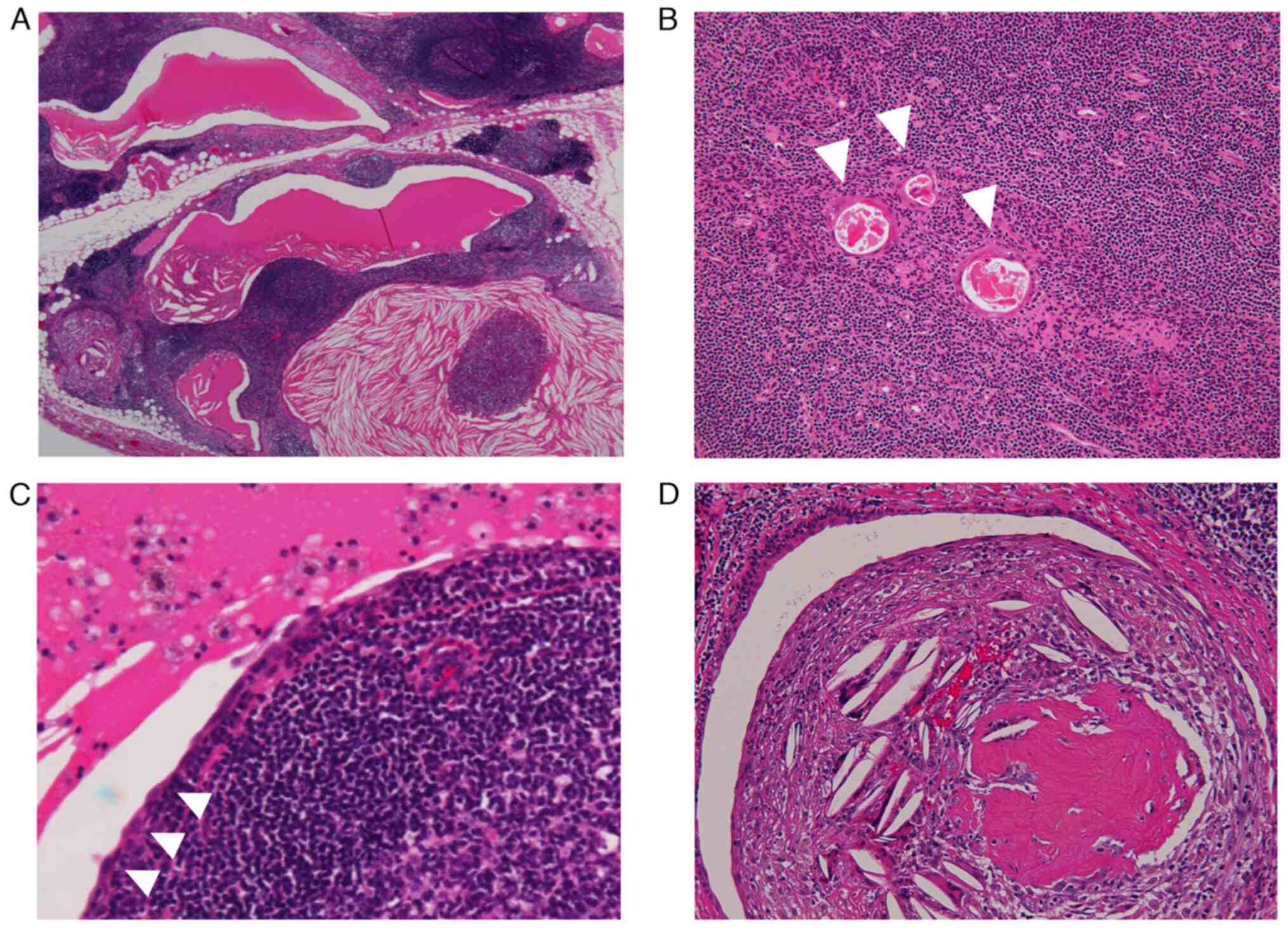
Hematoxylin and eosin staining was performed on the
formalin-fixed paraffin-embedded surgically resected thymic tissue
sections of 4 µm thickness. A light microscope was used for
observation. Pathologically, the cysts were lined with squamous or
cuboidal epithelium. The cyst wall was primarily composed of thymic
tissue with follicular hyperplasia, and Hassall's corpuscles were
noted. Cholesterol granuloma formation adjacent to the cysts was
also observed. Signs of malignancy were not observed (Fig. 3). Based on these findings, the
patient was diagnosed with MTC. The postoperative course was
uneventful, and the patient is currently being followed up at an
outpatient clinic; to date there are no signs of recurrence.
Discussion
MTC is a rare disease, accounting for approximately
3% of anterior mediastinal tumors (13). It is recognized by a multiloculated
cyst-like structure in the anterior mediastinum on CT, and a
pathological examination is necessary for final diagnosis.
Pathologically, the inner surface of the cysts is lined by
cuboidal, squamous, or columnar epithelia. The cyst wall comprises
thymic tissue containing Hassall's corpuscles and hyperplastic
lymphoid follicles with a well-formed germinal center.
Hyalinization, calcification, and cholesterol granuloma formation
can also be observed within the cyst walls (1,14).
MTC is associated with inflammatory diseases, including human
immunodeficiency virus (HIV) infection and acquired
immunodeficiency syndrome (AIDS). In our case, MTC developed in a
man who was HIV positive. Although a bilocular cyst in the anterior
mediastinum was observed on imaging, the resected thymic tissue
exhibited a multiloculated cyst formation. The pathological
findings were consistent with typical MTC characteristics.
To further understand the clinical characteristics
of MTC in PLWHA, a literature review was conducted. Literature was
collected through a PubMed search under the following query:
((multilocular thymic cyst[Title]) OR (multilocular thymic
cysts[Title])) AND ((hiv[Title]) OR (human immunodeficiency
virus[Title]) OR (acquired immunodeficiency syndrome[title]) OR
(aids[title])). A total of seven studies reported 15 cases reported
on MTC in PLWHA (4,15-20).
The main clinical characteristics of the 16 cases, including ours,
are listed in Table S1 and its
summary is presented in Table I.
MTC in PLWHA is most commonly reported in children, with 12 of the
16 cases occurring at the age of 15 years or younger. Four cases
including ours occur in adults, with age of onset in middle age
ranging from 35 to 52 years old (4,16,19).
Most of the cases had only mildly reduced CD4 counts, with a median
CD4 count of 308/µl. Median time from HIV infection to MTC
development was 9 years, with 10 of 16 cases developed within 10
years after HIV infection. Our case has a 21-year history of HIV
infection and a relatively high CD4 count of 576/µl, which is
atypical compared to previous cases. Most patients had
comorbidities or symptoms such as LIP and parotid gland
enlargement, and only one patient was asymptomatic (15). Asymptomatic case was a pediatric
case, with no obvious differences in CD4 counts or duration of HIV
infection compared to other cases. Seven of the 16 patients
underwent tumor resection, and the others were followed up without
surgical intervention. There have been no reports of postoperative
recurrence. In five of the nine patients who did not undergo
surgical intervention, the tumor resolved or decreased in size. One
patient showed tumor enlargement during the first six months after
diagnosis, but the size stabilized thereafter (15). Of the remaining three cases, tumor
diameter remained unchanged in one case and the post-diagnostic
course was not stated in two cases (4,15,19).
Although MTC must be differentiated from other malignant tumors, it
is associated with a good prognosis when accurately diagnosed using
needle biopsy or based on findings during resection.
 | Table ISummary of 16 cases (15 previous cases
and the present case) of multilocular thymic cyst in people living
with HIV/acquired immunodeficiency syndrome. |
Table I
Summary of 16 cases (15 previous cases
and the present case) of multilocular thymic cyst in people living
with HIV/acquired immunodeficiency syndrome.
| Characteristics | Total |
|---|
| Median age, years
(range) | 10 (2-52) |
| Age, n (%) | |
|
<15
years | 12(75) |
|
15-35
years | 0 (0) |
|
>35
years | 4(25) |
| Male sex, n (%) | 11 (68.8) |
| Median
CD4+ T-cell count, n (IQR) | 308 (191-416) |
| Median HIV-positive
years, years (IQR) | 9 (3-11.5) |
| Associated symptoms,
n (%) | |
|
LIP | 7 (43.8) |
|
Lymphadenopathy | 6 (37.5) |
|
Parotid
gland enlargement | 5 (31.3) |
|
Hepatic
enlargement | 5 (31.3) |
|
Chest
pain | 4(25) |
|
Fever | 2 (12.5) |
|
Cough | 1 (6.3) |
|
None | 1 (6.3) |
| Surgical
intervention, n (%) | |
|
Yes | 7 (43.8) |
|
No | 9 (56.2) |
Our case was atypical for an HIV-related MTC because
it did not involve the typical comorbidities associated with HIV
infection. Considering that MTC was detected on the 9th day of
SARS-CoV-2 infection, it is possible that the MTC was associated
with COVID-19. While there have been no reports of MTC development
related to COVID-19, cystic lesions such as hepatic cyst
enlargement (8) and pneumatocele
formation (9,10) have been found to be associated with
COVID-19. Furthermore, patients with COVID-19 commonly exhibit
thymus hyperplasia, which is seen in the context of MTC (21). Our case alone cannot prove the
etiological relationship between COVID-19 and MTC development;
however, previous reports suggest the possibility for this
relationship. Biologically, the expression of
angiotensin-converting enzyme 2 and type 2 transmembrane serine
proteases, which are SARS-CoV-2 receptors and proteases (22), has not yet been quantified in the
thymus, and the affinity of SARS-CoV-2 for the thymus remains
unknown. More case reports on MTC development in patients with
COVID-19 and related biological investigations are needed for
further discussion on the relationship between COVID-19 and MTC
development.
In conclusion, we encountered a rare case of MTC
detected during COVID-19 evaluation and treatment in an adult
living with HIV. More reports on MTC cases in patients with
COVID-19 are needed to elucidate the relationship between MTC and
COVID-19.
Supplementary Material
Description of 16 cases (15 previous
cases and our case) of MTC in PLWHA.
Acknowledgements
Not applicable.
Funding
Funding: This study was supported by the National Center for
Global Health and Medicine COVID-19 Gift Fund.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HH and RS acquired data and wrote the manuscript. KM
and HM analyzed and interpreted pathology data. TI and SN made
substantial contributions to conception and design. HH and RS
confirm the authenticity of all the raw data. All authors read and
approved the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this report and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Suster S and Rosai J: Multilocular thymic
cyst: An acquired reactive process. Study of 18 cases. Am J Surg
Pathol. 15:388–398. 1991.PubMed/NCBI
|
|
2
|
Oramas DM and Moran CA: Multilocular
thymic cyst (MTC) and other tumors with MTC features: Pitfalls in
diagnosis. Semin Diagn Pathol. 39:105–112. 2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Yarchoan R, Ramaswami R and Lurain K:
HIV-associated malignancies at 40: much accomplished but much to
do. Glob Health Med. 3:184–186. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Leonidas JC, Berdon WE, Valderrama E,
Neveling U, Schuval S, Weiss SJ, Hilfer C and Godine L: Human
immunodeficiency virus infection and multilocular thymic cysts.
Radiology. 198:377–379. 1996.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Gokce A, Hatipoglu M, Kandemir NO and
Akkas Y: Thoracic incidentaloma in a chest computed tomography scan
of a patient with COVID-19. Br J Hosp Med (Lond). 82:1–3.
2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Huynh I: When COVID-19 saves lives:
Accidental cancer diagnosis in an epidemic context. Ethics Med
Public Health. 18(100666)2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Anka AU, Tahir MI, Abubakar SD, Alsabbagh
M, Zian Z, Hamedifar H, Sabzevari A and Azizi G: Coronavirus
disease 2019 (COVID-19): An overview of the immunopathology,
serological diagnosis and management. Scand J Immunol.
93(e12998)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
D'Amico FE, Glavas D, Noaro G, Bassi D,
Boetto R, Gringeri E, De Luca M and Cillo U: Case report: Liver
cysts and SARS-CoV-2: No evidence of virus in cystic fluid. Front
Surg. 8(677889)2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Shi H, Han X, Jiang N, Cao Y, Alwalid O,
Gu J, Fan Y and Zheng C: Radiological findings from 81 patients
with COVID-19 pneumonia in Wuhan, China: A descriptive study.
Lancet Infect Dis. 20:425–434. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Hamad AM and El-Saka HA: Post COVID-19
large pneumatocele: Clinical and pathological perspectives.
Interact Cardiovasc Thorac Surg. 33:322–324. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Malekifar P, Pakzad R, Shahbahrami R,
Zandi M, Jafarpour A, Rezayat SA, Akbarpour S, Shabestari AN,
Pakzad I, Hesari E, et al: Viral coinfection among COVID-19 Patient
Groups: An update systematic review and meta-analysis. Biomed Res
Int. 2021(5313832)2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Soltani S, Zakeri A, Zandi M, Kesheh MM,
Tabibzadeh A, Dastranj M, Faramarzi S, Didehdar M, Hafezi H,
Hosseini P and Farahani A: The role of bacterial and fungal human
respiratory microbiota in COVID-19 Patients. Biomed Res Int.
2021(6670798)2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Davis RD Jr, Oldham HN Jr and Sabiston DC
Jr: Primary cysts and neoplasms of the mediastinum: Recent changes
in clinical presentation, methods of diagnosis, management, and
results. Ann Thorac Surg. 44:229–237. 1987.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Izumi H, Nobukawa B, Takahashi K, Kumasaka
T, Miyamoto H, Yamazaki A, Sonobe S, Uekusa T and Suda K:
Multilocular thymic cyst associated with follicular hyperplasia:
Clinicopathologic study of 4 resected cases. Hum Pathol.
36:841–844. 2005.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kontny HU, Sleasman JW, Kingma DW, Jaffe
ES, Avila NA, Pizzo PA and Mueller BU: Multilocular thymic cysts in
children with human immunodeficiency virus infection: Clinical and
pathologic aspects. J Pediatr. 131:264–270. 1997.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Shi X, Nasseri F, Berger DM and Nachiappan
AC: Large multilocular thymic cyst: A rare finding in an HIV
positive adult female. J Clin Imaging Sci. 2(55)2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Tamagno M, Bibas BJ, Bernardi F, Lian YC,
Bammann RH, Fernandez A and Jatene FB: Giant multilocular thymic
cyst in an HIV-infected adolescent. J Pediatr Surg. 46:1842–1845.
2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Mishalani SH, Lones MA and Said JW:
Multilocular thymic cyst. A novel thymic lesion associated with
human immunodeficiency virus infection. Arch Pathol Lab Med.
119:467–470. 1995.PubMed/NCBI
|
|
19
|
Chhieng DC, Demaria S, Yee HT and Yang GC:
Multilocular thymic cyst with follicular lymphoid hyperplasia in a
male infected with HIV. A case report with fine needle aspiration
cytology. Acta Cytol. 43:1119–1123. 1999.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Shalaby-Rana E, Selby D, Ivy P, Schutzbank
T, Chan M, Chandra R and Majd M: Multilocular thymic cyst in a
child with acquired immunodeficiency syndrome. Pediatr Infect Dis
J. 15:83–86. 1996.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Cuvelier P, Roux H, Couëdel-Courteille A,
Dutrieux J, Naudin C, Charmeteau de Muylder B, Cheynier R, Squara P
and Marullo S: Protective reactive thymus hyperplasia in COVID-19
acute respiratory distress syndrome. Crit Care.
25(4)2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Hoffmann M, Kleine-Weber H, Schroeder S,
Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH,
Nitsche A, et al: SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2
and is blocked by a clinically proven protease inhibitor. Cell.
181:271–280.e8. 2020.PubMed/NCBI View Article : Google Scholar
|