|
1
|
Wang K, Sun X, Cao Y, Dai L, Sun F, Yu P
and Dong L: Risk factors for renal involvement and severe kidney
disease in 2731 Chinese children with Henoch-Schönlein purpura: A
retrospective study. Medicine (Baltimore).
97(e12520)2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Chimenz R, Cannavò L, Spinuzza A, Fede C,
Cucinotta U, Pensabene L, Betta P, Gitto E, Concolino D and Cuppari
C: Unusual presentation of Henoch-Schönlein purpura. J Biol Regul
Homeost Agents. 33 (5 Suppl 1):S69–S74. 2019.PubMed/NCBI
|
|
3
|
Gómez S, Pérez M, Pellegrini M, Isern E,
Quintana C, Artacho P, Bertolini M, Pomerantz B and Gadda N:
Henoch-Schonlein purpura in pediatrics: Ten years of experience at
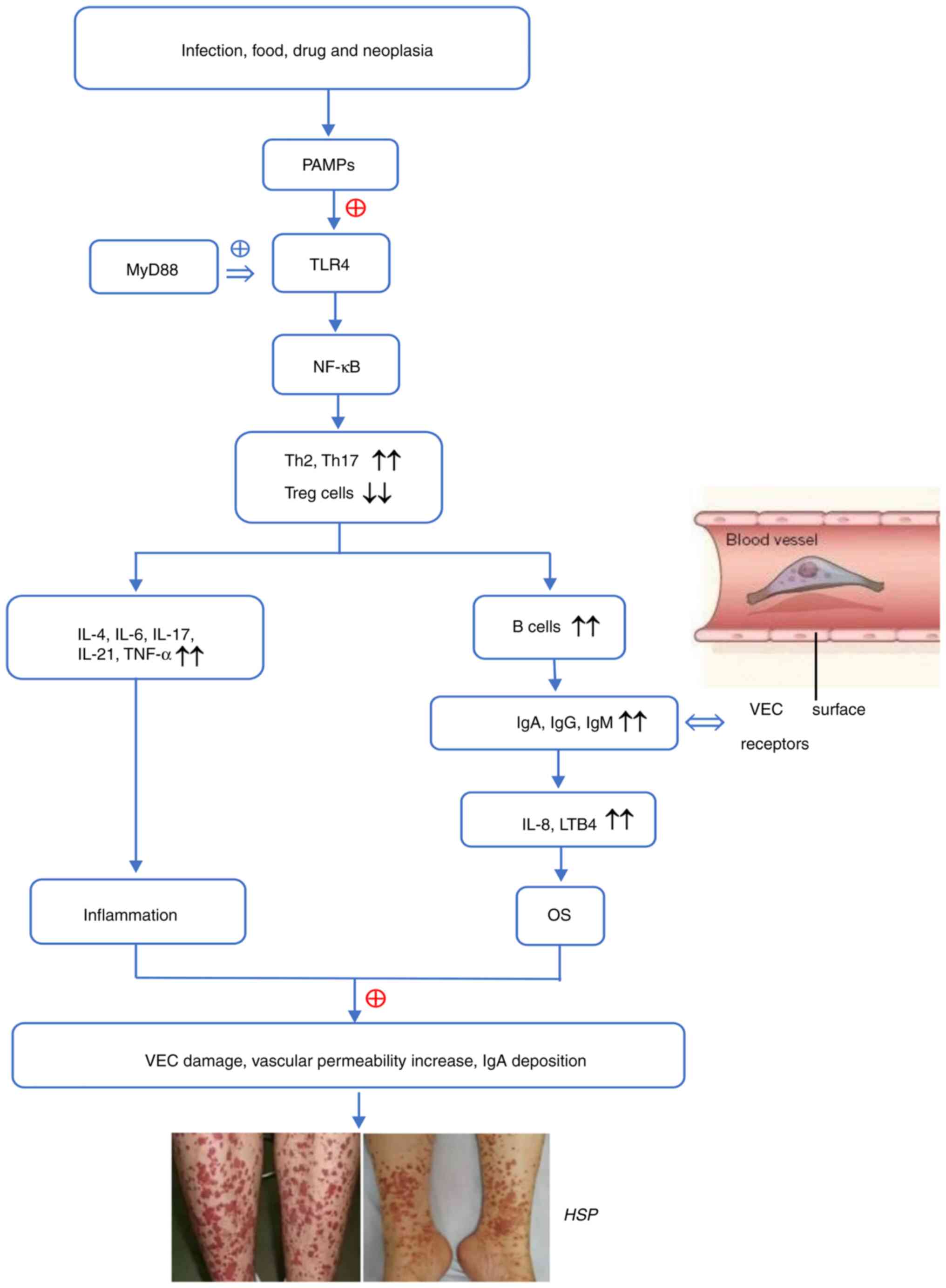
a moderate risk office of a general hospital. Arch Argent Pediatr.
118:31–37. 2020.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
4
|
Yang HR: What we know about
Henoch-Schönlein purpura in children up to date? J Korean Med Sci.
33(e199)2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zhu Y, Dong Y, Wu L and Deng F: Changes of
inflammatory mediators and oxidative stress indicators in children
with Henoch-Schönlein purpura and clinical effects of hemoperfusion
in the treatment of severe Henoch-Schönlein purpura with
gastrointestinal involvement in children. BMC Pediatr.
19(409)2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zhang N, Guo PJ, Liu PL, Yang HR, Xiao J,
Li XP, Huang JB and Zheng YZ: Comparison of age-based clinical and
abnormal immune parameters in patients with Henoch-Schönlein
purpura. Zhonghua Xue Ye Xue Za Zhi. 38:60–64. 2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
7
|
Niknam N, Ha L and Gautam-Goyal P: Adult
onset immunoglobulin A vasculitis (Henoch-Schonlein purpura) with
alveolar hemorrhage. IDCases. 12:47–48. 2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tan J, Tang Y, Zhong Z, Yan S, Tan L,
Tarun P and Qin W: The efficacy and safety of immunosuppressive
agents plus steroids compared with steroids alone in the treatment
of Henoch-Schönlein purpura nephritis: A meta-analysis. Int Urol
Nephrol. 51:975–985. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Roman C, Dima B, Muyshont L, Schurmans T
and Gilliaux O: Indications and efficiency of dapsone in IgA
vasculitis (Henoch-Schonlein purpura): Case series and a review of
the literature. Eur J Pediatr. 178:1275–1281. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Vonend C, Rifkin SI, Baliga RS and
Weinstein SS: Henoch-Schönlein purpura and recurrent renal failure.
Ren Fail. 32:888–891. 2010.PubMed/NCBI View Article : Google Scholar
|
|
11
|
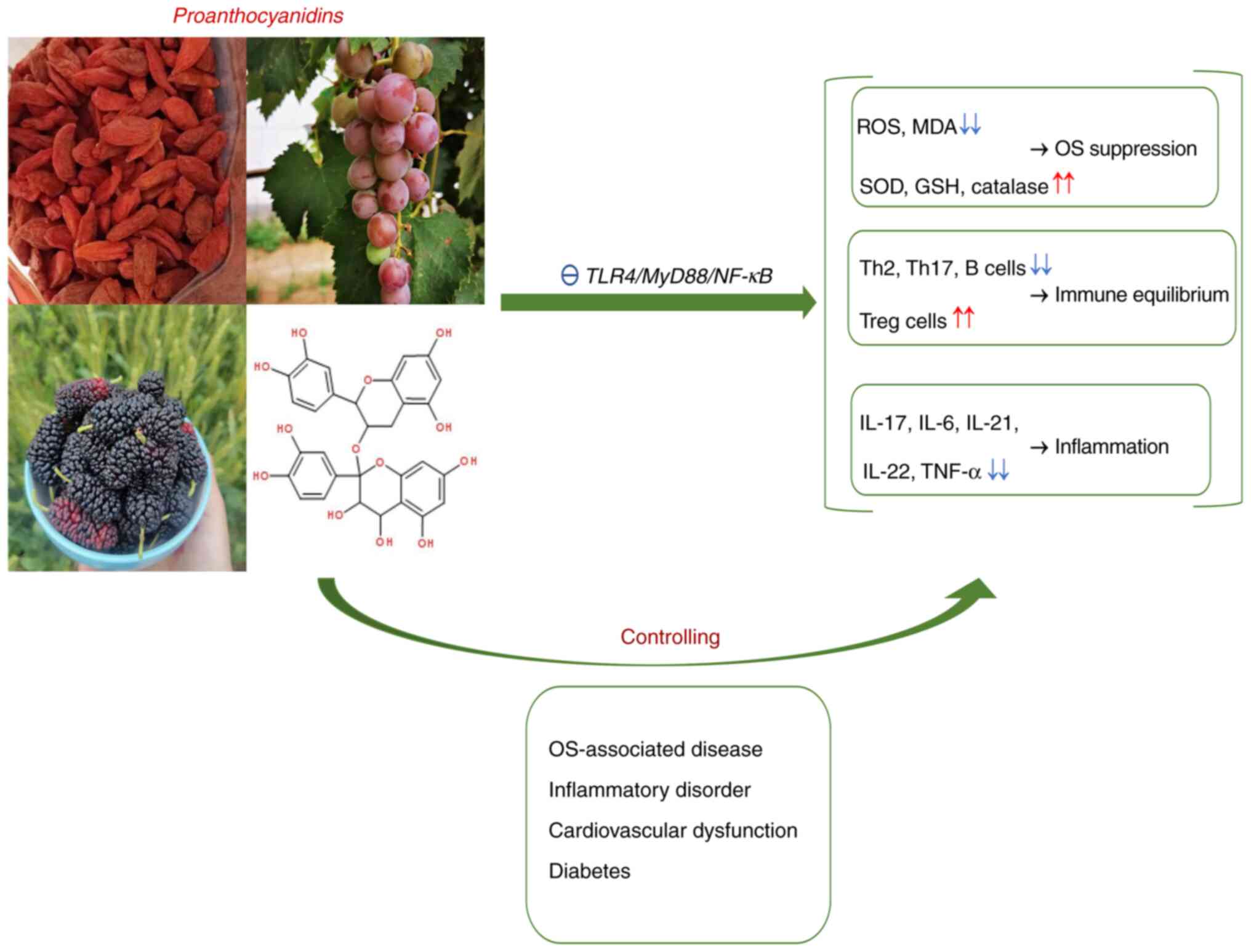
Oni L and Sampath S: Childhood IgA
vasculitis (Henoch Schonlein Purpura)-advances and knowledge gaps.
Front Pediatr. 7(257)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Fan L, Yan H, Zhen X, Wu X, Hao J, Hou L
and Han L: Safety and efficacy evaluation of traditional chinese
medicine (Qingre-Lishi-Yishen Formula) based on treatment of
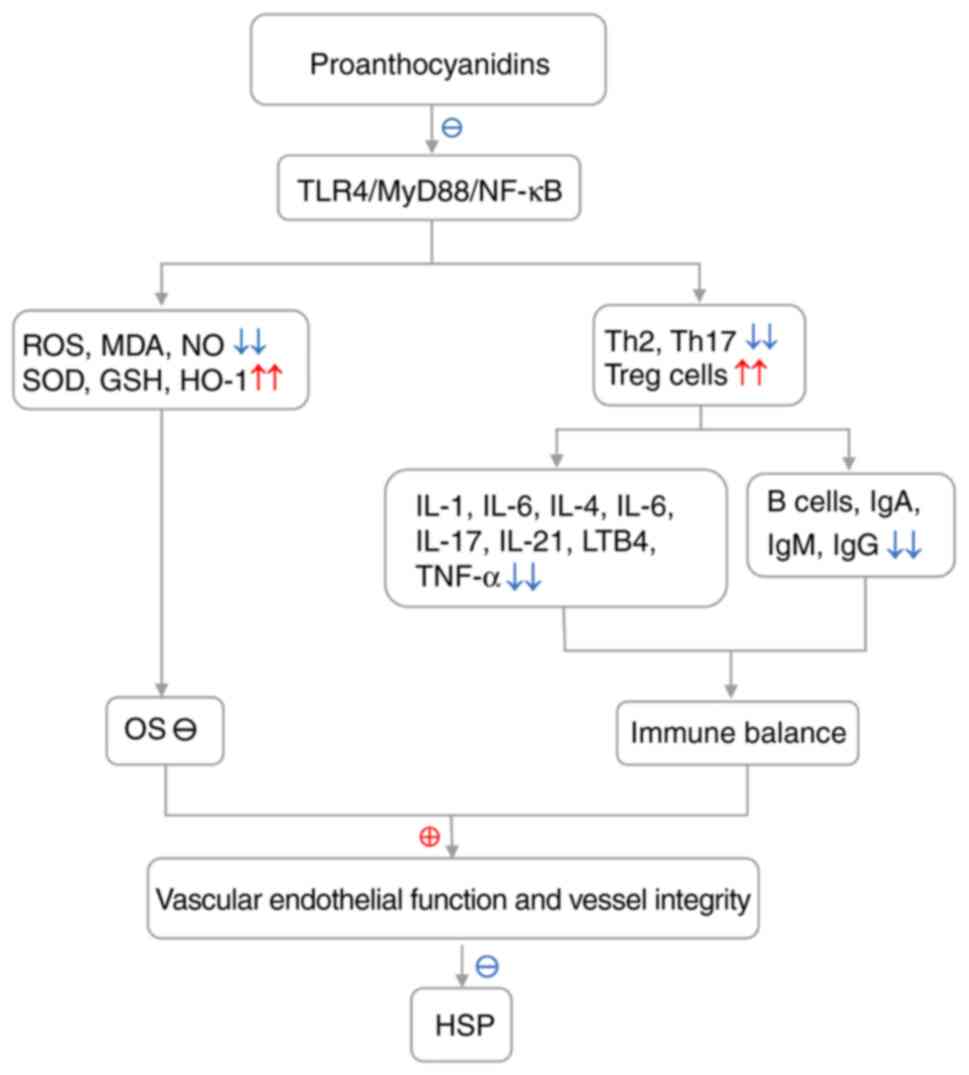
regular glucocorticoid combined with cyclophosphamide pulse in
children suffered from moderately Severe Henoch-Schonlein Purpura
nephritis with nephrotic proteinuria. Evid Based Complement
Alternat Med. 2020(3920735)2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Nichols JA and Katiyar SK: Skin
photoprotection by natural polyphenols: Anti-inflammatory,
antioxidant and DNA repair mechanisms. Arch Dermatol Res.
302:71–83. 2010.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Tong H, Song X, Sun X, Sun G and Du F:
Immunomodulatory and antitumor activities of grape seed
proanthocyanidins. J Agric Food Chem. 59:11543–1157.
2011.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Huang S, Yang N, Liu Y, Hu L, Zhao J, Gao
J, Li Y, Li C, Zhang X and Huang T: Grape seed proanthocyanidins
inhibit angiogenesis via the downregulation of both vascular
endothelial growth factor and angiopoietin signaling. Nutr Res.
32:530–536. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
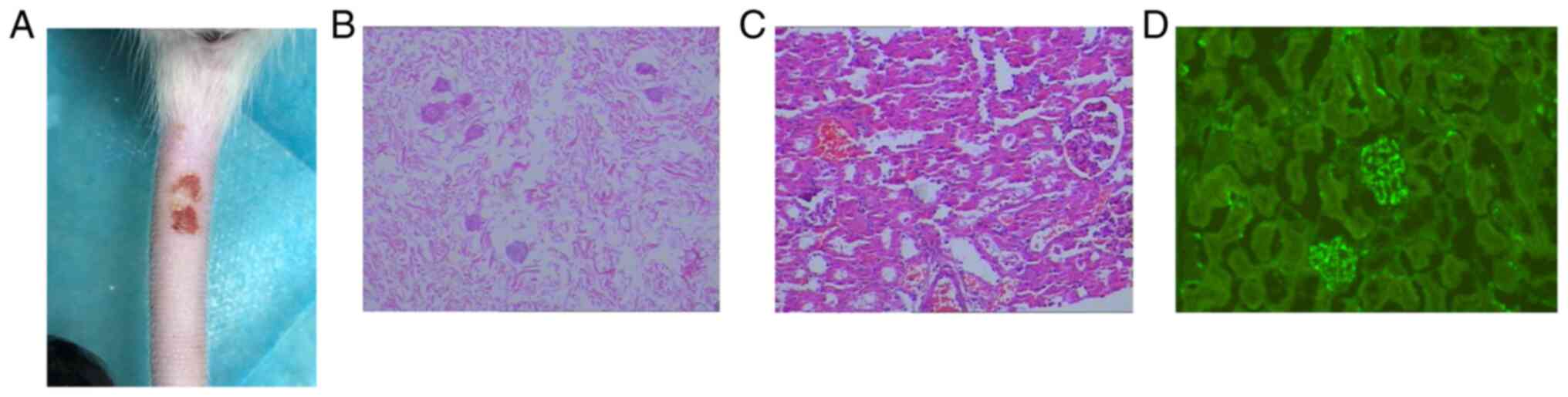
Wen W, Lu J, Zhang K and Chen S: Grape
seed extract inhibits angiogenesis via suppression of the vascular
endothelial growth factor receptor signaling pathway. Cancer Prev
Res (Phila). 1:554–561. 2008.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wu L, Huang Z, Qin P, Yao Y, Meng X, Zou
J, Zhu K and Ren G: Chemical characterization of a procyanidin-rich
extract from sorghum bran and its effect on oxidative stress and
tumor inhibition in vivo. J Agric Food Chem. 59:8609–8615.
2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Yang L, Xian D, Xiong X, Lai R, Song J and
Zhong J: Proanthocyanidins against oxidative stress: From molecular
mechanisms to clinical applications. Biomed Res Int.
2018(8584136)2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Mantena SK and Katiyar SK: Grape seed
proanthocyanidins inhibit UV-radiation-induced oxidative stress and
activation of MAPK and NF-kappaB signaling in human epidermal
keratinocytes. Free Radic Biol Med. 40:1603–1614. 2006.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Koudoufio M, Feldman F, Ahmarani L, Delvin
E, Spahis S, Desjardins Y and Levy E: Intestinal protection by
proanthocyanidins involves anti-oxidative and anti-inflammatory
actions in association with an improvement of insulin sensitivity,
lipid and glucose homeostasis. Sci Rep. 11(3878)2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Baldivia DDS, Leite DF, Castro DTH, Campos
JF, Santos UPD, Paredes-Gamero EJ, Carollo CA, Silva DB, de Picoli
Souza K and Dos Santos EL: Evaluation of in vitro antioxidant and
anticancer properties of the aqueous extract from the stem bark of
stryphnodendron adstringens. Int J Mol Sci. 19(2432)2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Alsharairi NA: Insights into the
mechanisms of action of proanthocyanidins and anthocyanins in the
treatment of nicotine-induced non-small cell lung cancer. Int J Mol
Sci. 23(7905)2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Lau KK, Suzuki H, Novak J and Wyatt RJ:
Pathogenesis of Henoch-Schönlein purpura nephritis. Pediatr
Nephrol. 25:19–26. 2010.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Keskin N, Civilibal M, Elevli M, Koldas M,
Duru NS and Ozturk H: Elevated plasma advanced oxidation protein
products in children with Henoch-Schonlein purpura. Pediatr
Nephrol. 26:1989–1993. 2011.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Xu H, Jiang G, Shen H, Li W, Mao J and Pan
Y: Association of TLR4 gene polymorphisms with childhood
Henoch-Schönlein purpura in a Chinese population. Rheumatol Int.
37:1909–1915. 2017.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Canpinar H, Ozaltin F, Bilginer Y,
Bakkaloğlu A and Ozen S: Toll-like receptors 2 and 4 cell surface
expression reflects endotoxin tolerance in Henoch-Schönlein
purpura. Turk J Pediatr. 52:22–27. 2010.PubMed/NCBI
|
|
27
|
Donadio ME, Loiacono E, Peruzzi L, Amore
A, Camilla R, Chiale F, Vergano L, Boido A, Conrieri M, Bianciotto
M, et al: Toll-like receptors, immunoproteasome and regulatory T
cells in children with Henoch-Schönlein purpura and primary IgA
nephropathy. Pediatr Nephrol. 29:1545–1551. 2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Chang H, Zhang QY, Lin Y, Cheng N and
Zhang SQ: Correlation of TLR2 and TLR4 expressions in peripheral
blood mononuclear cells to Th1- and Th2-type immune responses in
children with Henoch-Schönlein Purpura. Int J Clin Exp Med.
8:13532–13539. 2015.PubMed/NCBI
|
|
29
|
Chang H, Yu DS, Liu XQ, Zhang QY, Cheng N,
Zhang SQ and Qu ZH: Clinical significance of TLR3 and TLR4 in
peripheral blood mononuclear cells from children with
Henoch-Schönlein purpura nephritis. Exp Ther Med. 7:1703–1707.
2014.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Zhou L, Xu F, Chang C, Tao Y, Song L and
Li X: Interleukin-17-producing CD4+ T lymphocytes are increased in
patients with primary immune thrombocytopenia. Blood Coagul
Fibrinolysis. 27:301–307. 2016.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Barnabei L, Laplantine E, Mbongo W,
Rieux-Laucat F and Weil R: NF-κB: At the borders of autoimmunity
and inflammation. Front Immunol. 12(716469)2021.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Yu H, Lin L, Zhang Z, Zhang H and Hu H:
Targeting NF-κB pathway for the therapy of diseases: Mechanism and
clinical study. Signal Transduct Target Ther. 5(209)2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Oh H and Ghosh S: NF-κB: Roles and
regulation in different CD4(+) T-cell subsets. Immunol Rev.
252:41–51. 2013.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Pandiyan P and Zhu J: Origin and functions
of pro-inflammatory cytokine producing Foxp3+ regulatory T cells.
Cytokine. 76:13–24. 2015.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Chang H, Lin Y, Lei K, Wang F, Zhang QQ
and Zhang QY: Role of hypomethylation of suppressor of cytokine
signaling in T helper 17 cell/regulatory T cell imbalance in
children with Henoch-Schönlein purpura. Zhongguo Dang Dai Er Ke Za
Zhi. 21:38–44. 2019.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
36
|
Li-Weber M, Giaisi M, Baumann S, Pálfi K
and Krammer PH: NF-kappa B synergizes with NF-AT and NF-IL6 in
activation of the IL-4 gene in T cells. Eur J Immunol.
34:1111–1118. 2004.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Li YY, Li CR, Wang GB, Yang J and Zu Y:
Investigation of the change in CD4+ T cell subset in children with
Henoch-Schonlein purpura. Rheumatol Int. 32:3785–3792.
2012.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Yang J, Li CR, Zu Y, Wang GB and Li YB:
Role of regulatory T cells in pathogenesis of Henoch-Schonlein
purpura in children. Zhonghua Er Ke Za Zhi. 44:411–414.
2006.PubMed/NCBI(In Chinese).
|
|
39
|
Gujer C, Sundling C, Seder RA, Karlsson
Hedestam GB and Loré K: Human and rhesus plasmacytoid dendritic
cell and B-cell responses to Toll-like receptor stimulation.
Immunology. 134:257–269. 2011.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Ohue Y and Nishikawa H: Regulatory T
(Treg) cells in cancer: Can Treg cells be a new therapeutic target?
Cancer Sci. 110:2080–2089. 2019.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Adeegbe DO and Nishikawa H: Natural and
induced T regulatory cells in cancer. Front Immunol.
4(190)2013.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Weng L, Cao X, Han L, Zhao H, Qiu S, Yan
Y, Wang X, Chen X, Zheng W, Xu X, et al: Association of increased
Treg and Th17 with pathogenesis of moyamoya disease. Sci Rep.
7(3071)2017.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Wang CM, Luo Y, Wang YC and Sheng GY:
Roles of follicular helper T cells and follicular regulatory T
cells in pathogenesis of Henoch-Schönlein purpura in children.
Zhongguo Dang Dai Er Ke Za Zhi. 17:1084–1087. 2015.PubMed/NCBI(In Chinese).
|
|
44
|
Yang YH, Lai HJ, Huang CM, Wang LC, Lin YT
and Chiang BL: Sera from children with active Henoch-Schönlein
purpura can enhance the production of interleukin 8 by human
umbilical venous endothelial cells. Ann Rheum Dis. 63:1511–1513.
2004.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Yang YH, Huang YH, Lin YL, Wang LC, Chuang
YH, Yu HH, Lin YT and Chiang BL: Circulating IgA from acute stage
of childhood Henoch-Schönlein purpura can enhance endothelial
interleukin (IL)-8 production through MEK/ERK signalling pathway.
Clin Exp Immunol. 144:247–253. 2006.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Heineke MH, Ballering AV, Jamin A, Ben
Mkaddem S, Monteiro RC and Van Egmond M: New insights in the
pathogenesis of immunoglobulin A vasculitis (Henoch-Schönlein
purpura). Autoimmun Rev. 16:1246–1253. 2017.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Wu JJ, Zhu YT and Hu YM: Mechanism of
feedback regulation of neutrophil inflammation in Henoch-Schönlein
purpura. Eur Rev Med Pharmacol Sci. 20:4277–4285. 2016.PubMed/NCBI
|
|
48
|
Ray PD, Huang BW and Tsuji Y: Reactive
oxygen species (ROS) homeostasis and redox regulation in cellular
signaling. Cell Signal. 24:981–990. 2012.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Schieber M and Chandel NS: ROS function in
redox signaling and oxidative stress. Curr Biol. 24:R453–R462.
2014.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Cesselli D, Aleksova A, Sponga S,
Cervellin C, Di Loreto C, Tell G and Beltrami AP: Cardiac cell
senescence and redox signaling. Front Cardiovasc Med.
4(38)2017.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Ciccarese F, Raimondi V, Sharova E,
Silic-Benussi M and Ciminale V: Nanoparticles as tools to target
redox homeostasis in cancer cells. Antioxidants (Basel).
9(211)2020.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Nakai K and Tsuruta D: What are reactive
oxygen species, free radicals, and oxidative stress in skin
diseases? Int J Mol Sci. 22(10799)2021.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Sharifi-Rad M, Anil Kumar NV, Zucca P,
Varoni EM, Dini L, Panzarini E, Rajkovic J, Tsouh Fokou PV, Azzini
E, Peluso I, et al: Lifestyle, oxidative stress, and antioxidants:
Back and forth in the pathophysiology of chronic diseases. Front
Physiol. 11(694)2020.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Li Y and Pagano PJ: Microvascular NADPH
oxidase in health and disease. Free Radic Biol Med. 109:33–47.
2017.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Schröder K: NADPH oxidases: Current
aspects and tools. Redox Biol. 34(101512)2020.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Murphy MP: How mitochondria produce
reactive oxygen species. Biochem J. 417:1–13. 2009.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Arazi H, Eghbali E and Suzuki K: Creatine
supplementation, physical exercise and oxidative stress markers: A
review of the mechanisms and effectiveness. Nutrients.
13(869)2021.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Kim YW, West XZ and Byzova TV:
Inflammation and oxidative stress in angiogenesis and vascular
disease. J Mol Med (Berl). 91:323–328. 2013.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Salazar G: NADPH Oxidases and mitochondria
in vascular senescence. Int J Mol Sci. 19(1327)2018.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Zhu Y, Dong Y, Xu DL, Jiang JY, Wu L, Ke
RJ, Fang SH and Peng Y: Clinical effect and mechanism of
hemoperfusion in treatment of children with severe abdominal
Henoch-Schönlein purpura. Zhongguo Dang Dai Er Ke Za Zhi.
20:378–382. 2018.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
61
|
Gurses D, Parlaz N, Bor-Kucukatay M,
Kucukatay V and Erken G: Evaluation of oxidative stress and
erythrocyte properties in children with henoch-shoenlein purpura.
Iran J Pediatr. 24:166–172. 2014.PubMed/NCBI
|
|
62
|
Ece A, Kelekçi S, Kocamaz H, Hekimoğlu A,
Balik H, Yolbaş I and Erel O: Antioxidant enzyme activities, lipid
peroxidation, and total antioxidant status in children with
Henoch-Schönlein purpura. Clin Rheumatol. 27:163–169.
2008.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Higashi Y, Maruhashi T, Noma K and Kihara
Y: Oxidative stress and endothelial dysfunction: Clinical evidence
and therapeutic implications. Trends Cardiovasc Med. 24:165–169.
2014.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Mai J, Virtue A, Shen J, Wang H and Yang
XF: An evolving new paradigm: Endothelial cells-conditional innate
immune cells. J Hematol Oncol. 6(61)2013.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Hou X, Yang S and Yin J: Blocking the
REDD1/TXNIP axis ameliorates LPS-induced vascular endothelial cell
injury through repressing oxidative stress and apoptosis. Am J
Physiol Cell Physiol. 316:C104–C110. 2019.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Wu H, Wen Y, Yue C, Li X and Gao R: Serum
TNF-α level is associated with disease severity in adult patients
with immunoglobulin a vasculitis nephritis. Dis Markers.
2020(5514145)2020.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Yuan P, Bo Y, Ming G, Wen-Jun F, Qin Z and
Bo H: Apoptosis of human umbilical vein endothelial cells (HUVEC)
induced by IgA1 isolated from Henoch-Schonlein purpura children.
Asian Pac J Allergy Immunol. 32:34–38. 2014.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Montezano AC and Touyz RM: Reactive oxygen
species and endothelial function-role of nitric oxide synthase
uncoupling and Nox family nicotinamide adenine dinucleotide
phosphate oxidases. Basic Clin Pharmacol Toxicol. 110:87–94.
2012.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Elalfy MS, Elhenawy YI, Deifalla S, Hegazy
M, Sabra A and Abdelaziz Y: Oxidant/antioxidant status in children
and adolescents with immune thrombocytopenia (ITP) and the role of
an adjuvant antioxidant therapy. Pediatr Blood Cancer. 62:830–837.
2015.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Carta S, Semino C, Sitia R and Rubartelli
A: Dysregulated IL-1β secretion in autoinflammatory diseases: A
matter of stress? Front Immunol. 8(345)2017.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Noval Rivas M, Wakita D, Franklin MK,
Carvalho TT, Abolhesn A, Gomez AC, Fishbein MC, Chen S, Lehman TJ,
Sato K, et al: Intestinal permeability and IgA provoke immune
vasculitis linked to cardiovascular inflammation. Immunity.
51:508–521.e6. 2019.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Sugino H, Sawada Y and Nakamura M: IgA
Vasculitis: Etiology, treatment, biomarkers and epigenetic changes.
Int J Mol Sci. 22(7538)2021.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Lavieri R, Piccioli P, Carta S, Delfino L,
Castellani P and Rubartelli A: TLR costimulation causes oxidative
stress with unbalance of proinflammatory and anti-inflammatory
cytokine production. J Immunol. 192:5373–5381. 2014.PubMed/NCBI View Article : Google Scholar
|
|
74
|
Gong L, Lei Y, Liu Y, Tan F, Li S, Wang X,
Xu M, Cai W, Du B, Xu F, et al: Vaccarin prevents ox-LDL-induced
HUVEC EndMT, inflammation and apoptosis by suppressing ROS/p38 MAPK
signaling. Am J Transl Res. 11:2140–2154. 2019.PubMed/NCBI
|
|
75
|
Duan T, Du Y, Xing C, Wang HY and Wang RF:
Toll-like receptor signaling and its role in cell-mediated
immunity. Front Immunol. 13(812774)2022.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Aluri J, Cooper MA and Schuettpelz LG:
Toll-Like receptor signaling in the establishment and function of
the immune system. Cells. 10(1374)2021.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Vijay K: Toll-like receptors in immunity
and inflammatory diseases: Past, present, and future. Int
Immunopharmacol. 59:391–412. 2018.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Kuzmich NN, Sivak KV, Chubarev VN, Porozov
YB, Savateeva-Lyubimova TN and Peri F: TLR4 signaling pathway
modulators as potential therapeutics in inflammation and sepsis.
Vaccines (Basel). 5(34)2017.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Yao C, Oh JH, Lee DH, Bae JS, Jin CL, Park
CH and Chung JH: Toll-like receptor family members in skin
fibroblasts are functional and have a higher expression compared to
skin keratinocytes. Int J Mol Med. 35:1443–1450. 2015.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Krishnan JS, KSelvarajoo K, Tsuchiya M,
Lee G and Choi S: Toll-like receptor signal transduction. Exp Mol
Med. 39:421–438. 2007.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Rong Z, Huang Y, Cai H, Chen M, Wang H,
Liu G, Zhang Z and Wu J: Gut microbiota disorders promote
inflammation and aggravate spinal cord injury through the
TLR4/MyD88 signaling pathway. Front Nutr. 8(702659)2021.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Yamamoto M, Sato S, Hemmi H, Uematsu S,
Hoshino K, Kaisho T, Takeuchi O, Takeda K and Akira S: TRAM is
specifically involved in the Toll-like receptor 4-mediated
MyD88-independent signaling pathway. Nat Immunol. 4:1144–1150.
2003.PubMed/NCBI View
Article : Google Scholar
|
|
83
|
Mills KH: TLR-dependent T cell activation
in autoimmunity. Nat Rev Immunol. 11:807–822. 2011.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Park HS, Jung HY, Park EY, Kim J, Lee WJ
and Bae YS: Cutting edge: Direct interaction of TLR4 with NAD(P)H
oxidase 4 isozyme is essential for lipopolysaccharide-induced
production of reactive oxygen species and activation of NF-kappa B.
J Immunol. 173:3589–3593. 2004.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Gill R, Tsung A and Billiar T: Linking
oxidative stress to inflammation: Toll-like receptors. Free Radic
Biol Med. 48:1121–1132. 2010.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Rauf A, Imran M, Abu-Izneid T,
Iahtisham-Ul-Haq Patel S, Pan X, Naz S, Sanches Silva A, Saeed F
and Rasul Suleria HA: Proanthocyanidins: A comprehensive review.
Biomed Pharmacother. 116(108999)2019.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Bensa M, Glavnik V and Vovk I: Leaves of
Invasive Plants-Japanese, bohemian and giant knotweed-the promising
new nource of Flavan-3-ols and proanthocyanidins. Plants (Basel).
9(118)2020.PubMed/NCBI View Article : Google Scholar
|
|
88
|
González-Quilen C, Rodríguez-Gallego E,
Beltrán-Debón R, Pinent M, Ardévol A, Blay MT and Terra X:
Health-promoting properties of proanthocyanidins for intestinal
dysfunction. Nutrients. 12(130)2020.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Li S, Xu M, Niu Q, Xu S, Ding Y, Yan Y,
Guo S and Li F: Efficacy of procyanidins against in vivo cellular
oxidative damage: A systematic review and meta-analysis. PLoS One.
10(e0139455)2015.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Ravindranathan P, Pasham D, Balaji U,
Cardenas J, Gu J, Toden S and Goel A: Mechanistic insights into
anticancer properties of oligomeric proanthocyanidins from grape
seeds in colorectal cancer. Carcinogenesis. 39:767–777.
2018.PubMed/NCBI View Article : Google Scholar
|
|
91
|
Nawrot-Hadzik I, Matkowski A,
Kubasiewicz-Ross P and Hadzik J: Proanthocyanidins and Flavan-3-ols
in the prevention and treatment of periodontitis-immunomodulatory
effects, animal and clinical Studies. Nutrients.
13(239)2021.PubMed/NCBI View Article : Google Scholar
|
|
92
|
Odai T, Terauchi M, Kato K, Hirose A and
Miyasaka N: Effects of grape seed proanthocyanidin extract on
vascular endothelial function in participants with prehypertension:
A randomized, double-blind, placebo-controlled study. Nutrients.
11(2844)2019.PubMed/NCBI View Article : Google Scholar
|
|
93
|
Zhang R, Kang X, Liu L, Wang X, Li H, Zhu
J, Cao Y and Zhu H: Gut microbiota modulation by plant polyphenols
in koi carp (Cyprinus carpio L.). Front Microbiol.
13(977292)2022.PubMed/NCBI View Article : Google Scholar
|
|
94
|
Suo H, Tian R, Li J, Zhang S, Cui Y, Li L
and Sun B: Compositional characterization study on
high-molecular-mass polymeric polyphenols in red wines by chemical
degradation. Food Res Int. 123:440–449. 2019.PubMed/NCBI View Article : Google Scholar
|
|
95
|
Yuan L, Wang Q, Zhang S and Zhang L:
Correlation between serum inflammatory factors TNF-α, IL-8, IL-10
and Henoch-Schonlein purpura with renal function impairment. Exp
Ther Med. 15:3924–3928. 2018.PubMed/NCBI View Article : Google Scholar
|
|
96
|
Park MK, Park JS, Cho ML, Oh HJ, Heo YJ,
Woo YJ, Heo YM, Park MJ, Park HS, Park SH, et al: Grape seed
proanthocyanidin extract (GSPE) differentially regulates Foxp3(+)
regulatory and IL-17(+) pathogenic T cell in autoimmune arthritis.
Immunol Lett. 135:50–58. 2011.PubMed/NCBI View Article : Google Scholar
|
|
97
|
Jhun JY, Moon SJ, Yoon BY, Byun JK, Kim
EK, Yang EJ, Ju JH, Hong YS, Min JK, Park SH, et al: Grape seed
proanthocyanidin extract-mediated regulation of STAT3 proteins
contributes to Treg differentiation and attenuates inflammation in
a murine model of obesity-associated arthritis. PLoS One.
8(e78843)2013.PubMed/NCBI View Article : Google Scholar
|
|
98
|
Park IJ, Cha SY, Kang M, So YS, Go HG, Mun
SP, Ryu KS and Jang HK: Effect of proanthocyanidin-rich extract
from Pinus radiata bark on immune response of
specific-pathogen-free White Leghorn chickens. Poult Sci.
90:977–982. 2011.PubMed/NCBI View Article : Google Scholar
|
|
99
|
Min HK, Kim SM, Baek SY, Woo JW, Park JS,
Cho ML, Lee J, Kwok SK, Kim SW and Park SH: Anthocyanin extracted
from black soybean seed coats prevents autoimmune arthritis by
suppressing the development of Th17 cells and synthesis of
proinflammatory cytokines by such cells, via inhibition of NF-κB.
PLoS One. 10(e0138201)2015.PubMed/NCBI View Article : Google Scholar
|
|
100
|
Takano F, Takata T, Yoshihara A, Nakamura
Y, Arima Y and Ohta T: Aqueous extract of peanut skin and its main
constituent procyanidin A1 suppress serum IgE and IgG1 levels in
mice-immunized with ovalbumin. Biol Pharm Bull. 30:922–927.
2007.PubMed/NCBI View Article : Google Scholar
|
|
101
|
Long M, Yang SH, Han JX, Li P, Zhang Y,
Dong S, Chen X, Guo J, Wang J and He JB: The protective effect of
grape-seed proanthocyanidin extract on oxidative damage induced by
zearalenone in kunming mice liver. Int J Mol Sci.
17(808)2016.PubMed/NCBI View Article : Google Scholar
|
|
102
|
Han S, Gao H, Chen S, Wang Q, Li X, Du LJ,
Li J, Luo YY, Li JX, Zhao LC, et al: Procyanidin A1 Alleviates
Inflammatory Response induced by LPS through NF-κB, MAPK, and
Nrf2/HO-1 Pathways in RAW264.7 cells. Sci Rep.
9(15087)2019.PubMed/NCBI View Article : Google Scholar
|
|
103
|
Katiyar SK: Proanthocyanidins from grape
seeds inhibit UV-radiation-induced immune suppression in mice:
Detection and analysis of molecular and cellular targets. Photochem
Photobiol. 91:156–162. 2015.PubMed/NCBI View Article : Google Scholar
|
|
104
|
Kim SH, Bang J, Son CN, Baek WK and Kim
JM: Grape seed proanthocyanidin extract ameliorates murine
autoimmune arthritis through regulation of TLR4/MyD88/NF-κB
signaling pathway. Korean J Intern Med. 33:612–621. 2018.PubMed/NCBI View Article : Google Scholar
|
|
105
|
El-Shitany NA and Eid B: Proanthocyanidin
protects against cisplatin-induced oxidative liver damage through
inhibition of inflammation and NF-κβ/TLR-4 pathway. Environ
Toxicol. 32:1952–1963. 2017.PubMed/NCBI View Article : Google Scholar
|
|
106
|
Mittal A, Elmets CA and Katiyar SK:
Dietary feeding of proanthocyanidins from grape seeds prevents
photocarcinogenesis in SKH-1 hairless mice: Relationship to
decreased fat and lipid peroxidation. Carcinogenesis. 24:1379–1388.
2003.PubMed/NCBI View Article : Google Scholar
|
|
107
|
Rodríguez RM, Colom-Pellicer M, Blanco J,
Calvo E, Aragonès G and Mulero M: Grape-Seed procyanidin extract
(GSPE) Seasonal-Dependent modulation of glucose and lipid
metabolism in the liver of healthy F344 rats. Biomolecules.
12(839)2022.PubMed/NCBI View Article : Google Scholar
|
|
108
|
Sharma SD, Meeran SM and Katiyar SK:
Dietary grape seed proanthocyanidins inhibit UVB-induced oxidative
stress and activation of mitogen-activated protein kinases and
nuclear factor-kappaB signaling in in vivo SKH-1 hairless mice. Mol
Cancer Ther. 6:995–1005. 2007.PubMed/NCBI View Article : Google Scholar
|
|
109
|
Divya SP, Wang X, Pratheeshkumar P, Son
YO, Roy RV, Kim D, Dai J, Hitron JA, Wang L, Asha P, et al:
Blackberry extract inhibits UVB-induced oxidative damage and
inflammation through MAP kinases and NF-κB signaling pathways in
SKH-1 mice skin. Toxicol Appl Pharmacol. 284:92–99. 2015.PubMed/NCBI View Article : Google Scholar
|
|
110
|
Ma X, Wang R, Yu S, Lu G, Yu Y and Jiang
C: Anti-Inflammatory activity of oligomeric proanthocyanidins via
inhibition of NF-κB and MAPK in LPS-Stimulated MAC-T Cells. J
Microbiol Biotechnol. 30:1458–1466. 2020.PubMed/NCBI View Article : Google Scholar
|
|
111
|
Rajput SA, Sun L, Zhang NY, Khalil MM,
Ling Z, Chong L, Wang S, Rajput IR, Bloch DM, Khan FA, et al: Grape
seed proanthocyanidin extract alleviates aflatoxin B1-induced
immunotoxicity and oxidative stress via modulation of NF-κB and
Nrf2 signaling pathways in broilers. Toxins (Basel).
11(23)2019.PubMed/NCBI View Article : Google Scholar
|
|
112
|
Jia Z, Song Z, Zhao Y, Wang X and Liu P:
Grape seed proanthocyanidin extract protects human lens epithelial
cells from oxidative stress via reducing NF-кB and MAPK protein
expression. Mol Vis. 17:210–217. 2011.PubMed/NCBI
|
|
113
|
Schmuch J, Beckert S, Brandt S, Löhr G,
Hermann F, Schmidt TJ, Beikler T and Hensel A: Extract from
Rumex acetosa L. for prophylaxis of periodontitis:
Inhibition of bacterial in vitro adhesion and of gingipains of
Porphyromonas gingivalis by
epicatechin-3-O-(4β→8)-epicatechin-3-O-gallate
(procyanidin-B2-Di-gallate). PLoS One. 10(e0120130)2015.PubMed/NCBI View Article : Google Scholar
|
|
114
|
Steffen Y, Gruber C, Schewe T and Sies H:
Mono-O-methylated flavanols and other flavonoids as inhibitors of
endothelial NADPH oxidase. Arch Biochem Biophys. 469:209–219.
2008.PubMed/NCBI View Article : Google Scholar
|
|
115
|
Álvarez E, Rodiño-Janeiro BK, Jerez M,
Ucieda-Somoza R, Núñez MJ and González-Juanatey JR: Procyanidins
from grape pomace are suitable inhibitors of human endothelial
NADPH oxidase. J Cell Biochem. 113:1386–1396. 2012.PubMed/NCBI View Article : Google Scholar
|
|
116
|
Pinna C, Morazzoni P and Sala A:
Proanthocyanidins from Vitis vinifera inhibit oxidative
stress-induced vascular impairment in pulmonary arteries from
diabetic rats. Phytomedicine. 25:39–44. 2017.PubMed/NCBI View Article : Google Scholar
|
|
117
|
Weseler AR and Bast A: Masquelier's grape
seed extract: From basic flavonoid research to a well-characterized
food supplement with health benefits. Nutr J. 16(5)2017.PubMed/NCBI View Article : Google Scholar
|
|
118
|
Yang LJ, Zhu DN, Dang YL and Zhao X:
Treatment of condyloma acuminata in pregnant women with cryotherapy
combined with proanthocyanidins: Outcome and safety. Exp Ther Med.
11:2391–2394. 2016.PubMed/NCBI View Article : Google Scholar
|
|
119
|
Sano A: Safety assessment of 4-week oral
intake of proanthocyanidin-rich grape seed extract in healthy
subjects. Food Chem Toxicol. 108:519–523. 2017.PubMed/NCBI View Article : Google Scholar
|
|
120
|
Occhipinti A, Germano A and Maffei ME:
Prevention of urinary tract infection with oximacro, a cranberry
extract with a high content of A-type proanthocyanidins: A
pre-clinical double-blind controlled study. Urol J. 13:2640–2649.
2016.PubMed/NCBI
|
|
121
|
Serrano J, Casanova-Martí À, Gil-Cardoso
K, Blay MT, Terra X, Pinent M and Ardévol A: Acutely administered
grape-seed proanthocyanidin extract acts as a satiating agent. Food
Funct. 7:483–490. 2016.PubMed/NCBI View Article : Google Scholar
|
|
122
|
Zhao Y, Xie Y, Li X, Song J, Guo M, Xian D
and Zhong J: The protective effect of proanthocyanidins on the
psoriasis-like cell models via PI3K/AKT and HO-1. Redox Rep.
27:200–211. 2022.PubMed/NCBI View Article : Google Scholar
|
|
123
|
Omma A, Colak S, Can Sandikci S, Yucel C,
Erden A, Sertoglu E and Ozgurtas T: Serum neopterin and ischemia
modified albumin levels are associated with the disease activity of
adult immunoglobulin A vasculitis (Henoch-Schönlein purpura). Int J
Rheum Dis. 22:1920–1925. 2019.PubMed/NCBI View Article : Google Scholar
|
|
124
|
Wang B, Shao-Kuan FR and Dong C:
Expression and significance of follicular helper T cells and
galactose-deficient IgA1 in children with Henoch-Schönlein purpura.
Zhongguo Dang Dai Er Ke Za Zhi. 22:473–477. 2020.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
125
|
Long M, Zhang Y, Li P, Yang SH, Zhang WK,
Han JX, Wang Y and He JB: Intervention of Grape seed
proanthocyanidin extract on the subchronic immune injury in mice
induced by Aflatoxin B1. Int J Mol Sci. 17(516)2016.PubMed/NCBI View Article : Google Scholar
|
|
126
|
Liu X, Qiu J, Zhao S, You B, Ji X, Wang Y,
Cui X, Wang Q and Gao H: Grape seed proanthocyanidin extract
alleviates ouabain-induced vascular remodeling through regulation
of endothelial function. Mol Med Rep. 6:949–954. 2012.PubMed/NCBI View Article : Google Scholar
|
|
127
|
Di Pietro GM, Castellazzi ML, Mastrangelo
A, Montini G, Marchisio P and Tagliabue C: Henoch-Schönlein Purpura
in children: Not only kidney but also lung. Pediatr Rheumatol
Online J. 17(75)2019.PubMed/NCBI View Article : Google Scholar
|
|
128
|
Padeh S and Passwell JH: Successful
treatment of chronic Henoch-Schonlein purpura with colchicine and
aspirin. Isr Med Assoc J. 2:482–483. 2000.PubMed/NCBI
|
|
129
|
Pan S and Zhong J: Construction and
identification of simplified rat model of Henoch-Schönlein Purpura.
Sichuan Med J. 42:669–672. 2021.(In Chinese).
|
|
130
|
Li Y, Feng X, Huang L, Zhu H, Xu Y, Sui X,
Xu Y, Han Y and Qin C: Hematologic and immunological
characteristics of Henoch-Schönlein purpura in rat and rabbit
models induced with ovalbumin based on type III hypersensitivity.
Sci Rep. 5(8862)2015.PubMed/NCBI View Article : Google Scholar
|
|
131
|
Kaegi C, Wuest B, Schreiner J, Steiner UC,
Vultaggio A, Matucci A, Crowley C and Boyman O: Systematic review
of safety and efficacy of rituximab in treating immune-mediated
disorders. Front Immunol. 10(1990)2019.PubMed/NCBI View Article : Google Scholar
|
|
132
|
Gohari A, Matsell DG, Mammen C and Goldman
RD: Henoch-Schönlein purpura in children: Use of corticosteroids
for prevention and treatment of renal disease. Can Fam Physician.
66:895–897. 2020.PubMed/NCBI View Article : Google Scholar
|
|
133
|
Du Y, Hou L, Zhao C, Han M and Wu Y:
Treatment of children with Henoch-Schönlein purpura nephritis with
mycophenolate mofetil. Pediatr Nephrol. 27:765–771. 2012.PubMed/NCBI View Article : Google Scholar
|
|
134
|
Nikibakhsh AA, Mahmoodzadeh H, Karamyyar
M, Hejazi S, Noroozi M, Macooie AA, Gholizadeh A and Gholizadeh L:
Treatment of complicated henoch-schönlein purpura with
mycophenolate mofetil: A retrospective case series report. Int J
Rheumatol. 2010(254316)2010.PubMed/NCBI View Article : Google Scholar
|
|
135
|
Fujimoto M, Katayama K, Nishikawa K,
Mizoguchi S, Oda K, Hirabayashi Y, Suzuki Y, Haruki A, Ito T,
Murata T, et al: A Kidney transplant recipient with recurrent
Henoch-Schönlein Purpura nephritis successfully treated with
steroid pulse therapy and epipharyngeal abrasive therapy. Nephron.
144 (Suppl 1):S54–S48. 2020.PubMed/NCBI View Article : Google Scholar
|
|
136
|
Kurnia B: Henoch-Schonlein purpura in
children: The role of corticosteroids. Open Access Maced J Med Sci.
7:1812–1814. 2019.PubMed/NCBI View Article : Google Scholar
|
|
137
|
Ozen S, Marks SD, Brogan P, Groot N, de
Graeff N, Avcin T, Bader-Meunier B, Dolezalova P, Feldman BM,
Kone-Paut I, et al: European consensus-based recommendations for
diagnosis and treatment of immunoglobulin A vasculitis-the SHARE
initiative. Rheumatology (Oxford). 58:1607–1616. 2019.PubMed/NCBI View Article : Google Scholar
|
|
138
|
Han F, Chen LL, Ren PP, Le JY, Choong PJ,
Wang HJ, Xu Y and Chen JH: Mycophenolate mofetil plus prednisone
for inducing remission of Henoch-Schönlein purpura nephritis: A
retrospective study. J Zhejiang Univ Sci B. 16:772–779.
2015.PubMed/NCBI View Article : Google Scholar
|
|
139
|
Lu Z, Song J, Mao J, Xia Y and Wang C:
Evaluation of mycophenolate mofetil and Low-dose steroid combined
therapy in moderately severe Henoch-Schönlein Purpura nephritis.
Med Sci Monit. 23:2333–2339. 2017.PubMed/NCBI View Article : Google Scholar
|
|
140
|
Hamilton P, Ogundare O, Raza A, Ponnusamy
A, Gorton J, Alachkar H, Choudhury J, Barratt J and Kalra PA:
Long-term therapeutic plasma exchange to prevent End-stage kidney
disease in adult severe resistant Henoch-Schonlein purpura
nephritis. Case Rep Nephrol. 2015(269895)2015.PubMed/NCBI View Article : Google Scholar
|