Introduction
Biliary tract cancer (BTC) is a sporadic but highly
aggressive disease that consists of intrahepatic cholangiocarcinoma
(ICC), extrahepatic cholangiocarcinoma (ECC) and gallbladder cancer
(GBC). In most countries, many patients suffer from locally
advanced or metastatic disease at the time of diagnosis due to a
lack of early recognizable symptoms, and therefore eventually
receive palliative treatments with a dismal prognosis.
Cisplatin plus gemcitabine (GC) is widely used as
the standard first-line treatment in patients with unresectable BTC
(1,2), and there is a shortage of available
antitumor regimens as second-line/later treatment. In the era of
individualized cancer therapy, clinical trials of antiangiogenic
therapies and immune checkpoint inhibitor (ICI) treatments have
achieved impressive results in solid malignancies including lung
cancer and HCC (3,4).
Antiangiogenic therapies target vascular endothelial
growth factor receptor (VEGFR), which could normalize tumor
vasculature and improve treatment outcome. Based on data from phase
2 non-first line studies, VEGFR-targeted tyrosine kinase inhibitors
(TKIs) have shown potential efficacy and manageable safety in ICC
(Apatinib, NCT03251443) and BTC (Lenvatinib, NCT02579616;
Regorafenib, NCT02053376) (5-8).
However, the benefits obtained from antiangiogenic therapy in this
setting are limited, and predictive biomarkers for this class of
agents remain elusive.
Checkpoint inhibition, represented by PD-1 blockade,
also entered into clinical studies in advanced BTC. Pembrolizumab
exhibited ORR in only 6-13% of patients in clinical trials
KEYNOTE-028 and KEYNOTE-158(9),
and nivolumab showed similar efficacy, with an ORR of 11% in
patients with refractory BTC (10).
VEGFR-targeted TKIs combined with PD-1 inhibitors
have been approved to effectively target various solid tumors.
Lenvatinib has shown effective anti-tumor activity in combination
with pembrolizumab (LEP) in HCC, and LEP was granted as a
‘breakthrough designation’ in HCC, endometrial carcinoma and renal
cell cancer by the FDA (11).
Encouraged by the success of the combined therapy in the
above-mentioned solid malignancies, the LEP combination showed
promising efficacy and manageable toxicity in previously treated
advanced BTC in phase II LEAP-005 study. For these patients, the
DCR was 21.0% with duration of response (DOR) ranging from 2.1 to
6.2 months (up to April 10, 2020) (12). So far, the most favorable result
was observed in regorafenib plus avelumab in a phase II trial, the
median time to PFS and OS were 2.5 (95% CI, 1.9-5.5) months and
11.9 (95% CI, 6.2-NA) months, respectively (13). Moreover, the combination enabled a
longer OS in BTC patients compared with regorafenib monotherapy.
The conjunction of pembrolizumab and ramucirumab, however, did not
perform well in JVDF study with a poor ORR of only 4%, a median PFS
(mPFS) of 1.6 months, and a median OS (mOS) of 6.4 months (14).
So far, data on PD-1 inhibitor plus antiangiogenic
treatment published for treating advanced BTC are still limited.
This retrospective study was performed to evaluate the efficacy and
safety of PD-1 inhibitor plus antiangiogenic treatment in 68
patients with unresectable BTC in the real-world setting.
Materials and methods
Patients
This was a retrospective analysis of data from
patients with unresectable BTC who were treated with PD-1 inhibitor
plus antiangiogenic agent from March 26th, 2019 to November 1st,
2021 across the centers in China: i) Sir Run Run Shaw Hospital,
Zhejiang University; ii) The First Affiliated Hospital, Zhejiang
University; iii) The Second Affiliated Hospital, Zhejiang
University. A total of 68 patients with advanced BTC who received
PD-1 inhibitor plus antiangiogenic agent were eligible based on the
following criteria: i) BTC diagnosis based on histology; ii)
patients not available for radical operation; iii) at least one
measurable lesion as conformed by Response Evaluation Criteria in
Solid Tumors, version 1.1 (RECIST v1.1). Exclusion criteria were:
i) combined therapy for only one cycle; ii) no available follow-up
data; iii) no available data for baseline assessment and response
assessment; iv) combination with chemotherapy, peptide vaccines, or
bi-specific/tri-specific antibodies.
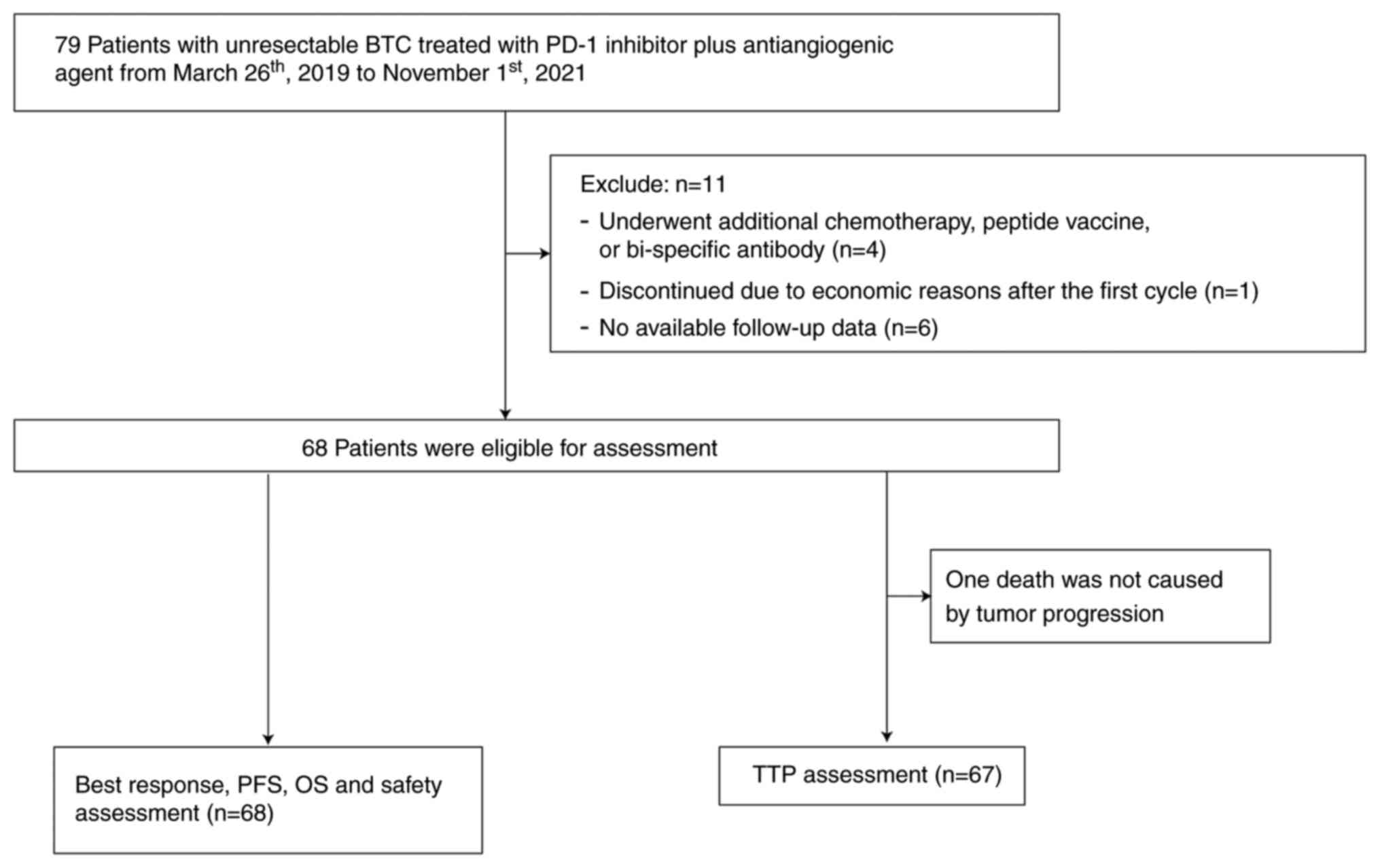
In total, data of 11 patients were excluded: 4
because they underwent additional chemotherapy, peptide vaccine, or
bi-specific antibody; 1 because he discontinued for economic
reasons after the first medication; 6 because they had no available
follow-up data. Data from the remaining 68 patients were analyzed.
Data including clinical information and follow-up data were
gathered from patients' electronic health records. This study was
carried out in accordance with the ethical guidelines of the
Declaration of Helsinki and was approved by the ethics committee of
the three participating hospitals (approval no. 2021332 for Sir Run
Run Shaw Hospital, Zhejiang University; approval no. 2021734 for
The First Affiliated Hospital, Zhejiang University; approval no.
I20211065 for The Second Affiliated Hospital, Zhejiang
University).
Treatment procedure
PD-1 inhibitors plus antiangiogenic agents were
applied as off-label therapies for BTC in our cohort. The treatment
strategy was designed based on previous treatment strategies,
individual characteristics, patient willingness and economic
condition. PD-1 inhibitors included camrelizumab, sintilimab,
toripalimab, tislelizumab, pembrolizumab and nivolumab, which were
administrated intravenously according to the following doses:
camrelizumab 200 mg, sintilimab 200 mg, toripalimab 240 mg,
tislelizumab 200 mg, pembrolizumab 200 mg every 3 weeks, or
nivolumab 3 mg/kg every 2 weeks. Antiangiogenic agents included
lenvatinib, apatinib, anlotinib, sorafenib, bevacizumab and
fruquintinib, which were administered orally except bevacizumab.
Lenvatinib was given 8 mg/day (body weight <60 kg) or 12 mg/day
(body weight ≥60 kg). The initial dose of sorafenib was 400 mg/day
and increased to 400 mg/12 h if tolerable. The patients received
apatinib at a dosage of 250 mg daily, anlotinib at a dosage of 8 mg
(2 weeks on/1 week off), or bevacizumab at a dosage of 7.5 mg/kg
every 3 weeks intravenously. Fruquintinib was administered at 5
mg/day, day1-14/21 days in this cohort. All patients continued
combination treatment until disease progression or unacceptable
toxicity.
Assessments
Tumors were assessed using dynamic computed
tomography (CT) and/or magnetic resonance imaging (MRI) at baseline
and every 8 to 12 weeks until disease progression or treatment
discontinuation. Tumor responses were evaluated according to RECIST
v1.1: (1) complete response (CR)
as the complete disappearance of all target lesions; (2) partial response (PR) as a ≥30%
decrease of the diameter of the target lesions; (3) stable disease (SD) as insufficient
shrinkage to qualify as PR but insufficient increase to qualify as
PD; (4) progressive disease (PD)
as ≥20% increase of the diameter of the target lesions, or new
lesions development.
The therapeutic efficacy assessment included the ORR
and DCR, and the survival analysis included TTP, PFS and OS. ORR
was defined as the sum of CR and PR, and DCR was defined as the sum
of CR, PR and SD. TTP was calculated from admission to progression
confirmed by radiology. PFS was calculated from initial dose to
clinical or radiographic progression or death. OS was calculated
from initial dose to the date of death of any cause.
Treatment-related adverse event (TRAE) data were collected and
evaluated according to the Common Terminology Criteria for Adverse
Events, version 5.0.
Statistical analysis
Clinical characteristic categorical variables were
analyzed by Pearson's χ2 test or Fisher's exact test.
Treatment strategy categorical variables were analyzed using the
logistic regression model. Survival data were estimated using the
Kaplan-Meier method, univariate analysis and multi-univariate
analysis were performed using Log-rank test and Cox regression
model, respectively. Statistical analysis was performed by IBM SPSS
version 23.
Results
Baseline characteristics and
therapeutic strategies
In this retrospective cohort, sixty-eight
unresectable BTC patients who had received PD-1 inhibitor plus
antiangiogenic therapy (Fig. 1),
with a median follow-up of 7.9 (95% CI, 6.9-9.0) months by the time
of data lock (November 1st, 2021). Baseline patient disposition is
summarized in Table I. Of the 68
patients, thirty-six patients are male (52.9%) and thirty-two are
female (47.1%) with a median age of 65 (range 33-82 years).
Forty-seven patients (69.1%) had an Eastern Cooperative Oncology
Group performance status (PS) of 2 or 3. Fifty-one patients (75.0%)
had ICC, seven (10.3%) had ECC, and ten (14.7%) had GBC. According
to TNM staging, fourteen patients were in stage III, and fifty-four
patients in stage IV. Half of patients experienced post-operative
recurrence. Fifty-two patients (76.5%) had intrahepatic metastasis,
and lymph node (57.4%) was the most frequent site for extrahepatic
disease followed by peritoneum (26.5%), lung (19.1%) and
intra-abdominal implantation (19.1%). More than half of the
patients (69.1%) in the study had undergone prior systemic
therapies. In addition, twenty-three patients (33.8%) received
non-surgical local treatment previously, including locoregional
therapy and radiotherapy.
 | Table IBaseline characteristics. |
Table I
Baseline characteristics.
| Variable | Value |
|---|
| Median age, years
(range) | 65 (33-82) |
| Patients aged ≥60
years, n (%) | 40 (58.8) |
| Sex, n (%) | |
|
Male | 36 (52.9) |
|
Female | 32 (47.1) |
| ECOG PS, n (%) | |
|
0-1 | 21 (30.9) |
|
2-3 | 47 (69.1) |
| Alcohol status, n
(%) | |
|
Current or
ex-drinker | 8 (11.8) |
|
Never-drinker | 60 (88.2) |
| Histology, n (%) | |
|
ICC | 51 (75.0) |
|
ECC | 7 (10.3) |
|
GBC | 10 (14.7) |
| Tumor stage, n
(%) | |
|
Stage
III | 14 (20.6) |
|
Stage
IV | 54 (79.4) |
| Metastasis present, n
(%) | |
|
Intrahepatic
metastasis | 52 (76.5) |
|
Lymph node
metastasis | 39 (57.4) |
|
Lung
metastasis | 13 (19.1) |
|
Bone
metastasis | 5 (7.4) |
|
Peritoneum
metastasis | 18 (26.5) |
|
Intra-abdominal
implantation | 13 (19.1) |
| Previous treatment
lines, n (%) | |
|
0 | 27 (30.9) |
|
≥1 | 41 (69.1) |
| Previous therapy, n
(%) | |
|
Immunotherapy | 16 (23.5) |
|
Antiangiogenic
therapy | 9 (13.2) |
|
Local
treatment (non-surgical) | 23 (33.8) |
|
Surgery | 34 (50.0) |
In the study, patients were given different
combination strategies of six types of PD-1 inhibitors plus six
types of antiangiogenic agents (Table
II). The three most frequently used PD-1 inhibitors were
camrelizumab (39.7%), sintilimab (22.1%) and toripalimab (19.1%).
Synchronously, the majority of patients were treated with
lenvatinib (51.5%), apatinib (26.5%) and anlotinib (14.7%). These
angiogenetic drugs consisted of anti-VEGFR2 antibody (3.0%) and
multitargeted TKIs (97.1%).
 | Table IIThe combination immune checkpoint
inhibitor and antiangiogenic therapy strategies. |
Table II
The combination immune checkpoint
inhibitor and antiangiogenic therapy strategies.
| Drug | Value, n (%) |
|---|
| Immune checkpoint
inhibitor | |
|
Camrelizumab | 27 (39.7) |
|
Sintilimab | 15 (22.1) |
|
Toripalimab | 13 (19.1) |
|
Tislelizumab | 10 (14.7) |
|
Pembrolizumab | 2 (2.9) |
|
Nivolumab | 1 (1.5) |
| Antiangiogenic
drug | |
|
Lenvatinib | 35 (51.5) |
|
Apatinib | 18 (26.5) |
|
Anlotinib | 10 (14.7) |
|
Sorafenib | 2 (2.9) |
|
Bevacizumab | 2 (2.9) |
|
Fruquintinib | 1 (1.5) |
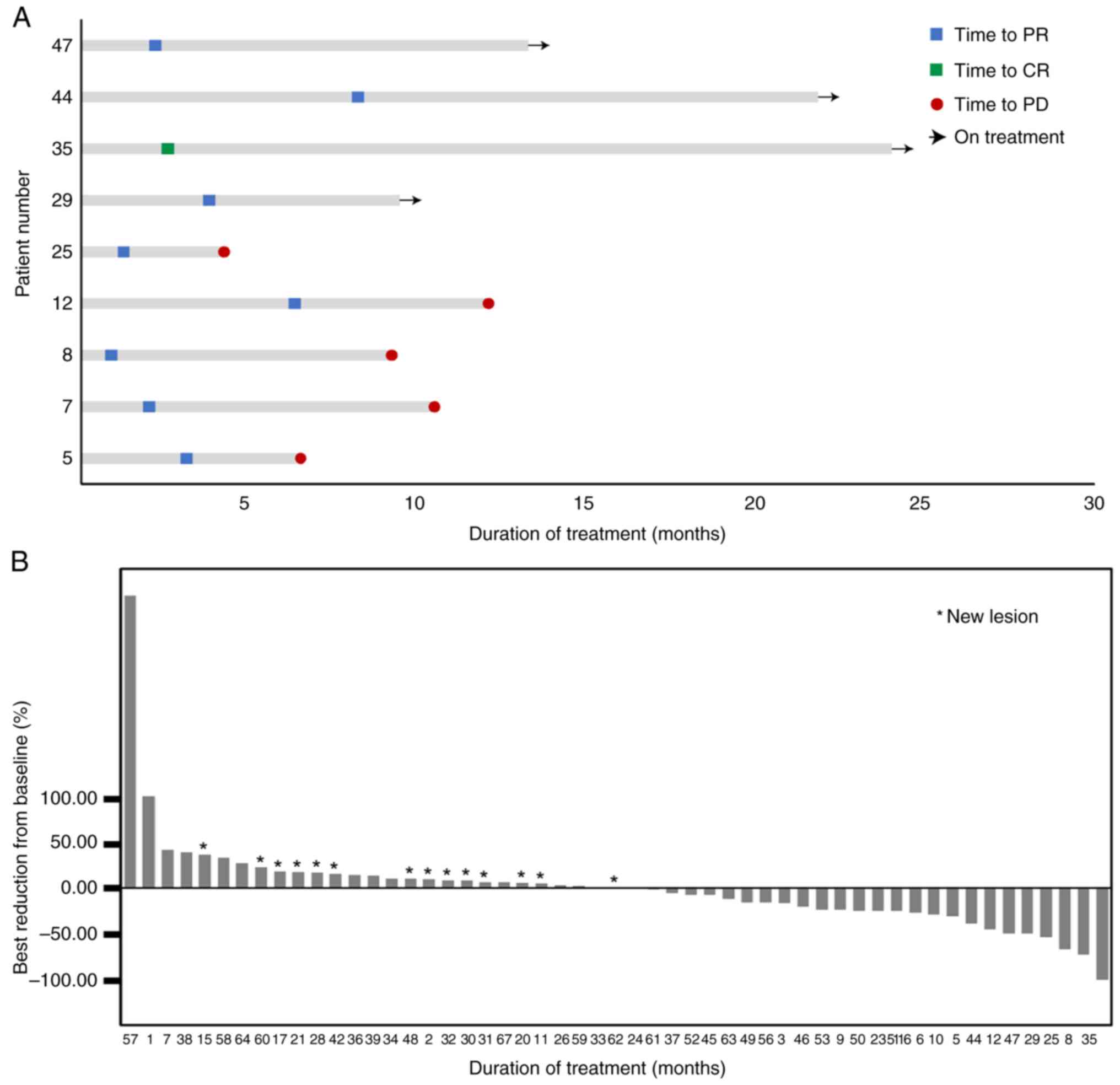
Treatment outcomes. Tumor
response
In our cohort, the ORR was 13.2% (n=9) with 1
patient achieving CR, and the swimmer plot showed the median DOR
(mDOR) was 8.4 (95% CI, 4.9-11.9) months in these patients
(Fig. 2A). Besides, forty-two
participants (61.8%) had SD and the DCR was 75.0% (Table III). Waterfall plot presented the
best percentage change from baseline in tumor measurement (Fig. 2B). Twenty-four (35.3%) patients
exhibited a decrease in tumor size from baseline. None of the
evaluated baseline characteristics was significantly associated
with objective response (Table
IV).
 | Table IIIResults of tumor response and
prognosis. |
Table III
Results of tumor response and
prognosis.
| Variable | Value |
|---|
| CR, n (%) | 1 (1.5) |
| PR, n (%) | 8 (11.8) |
| SD, n (%) | 12 (17.6) |
| ORR, n (%) | 9 (13.2) |
| DCR, n (%) | 51 (75.0) |
| mTTP, months (95%
CI) | 8.2 (4.9-11.6) |
| mPFS, months (95%
CI) | 5.5 (3.3-7.8) |
| mOS, months (95%
CI) | 10.7
(2.3-19.0) |
 | Table IVUnivariate analyses of the effects of
baseline characteristics on tumor response. |
Table IV
Univariate analyses of the effects of
baseline characteristics on tumor response.
| | ORR |
|---|
| Baseline
characteristics | P-value | OR | 95% CI |
|---|
| Age | 0.109 | 3.4 | 0.7-14.8 |
| Sex | 0.585 | 0.7 | 0.2-2.8 |
| PS | 0.098 | 3.4 | 0.8-14.1 |
| Alcohol | 0.309 | 0.4 | 0.1-2.4 |
| Histology | 0.995 | | |
|
ICC | 0.999 |
3.0x108 | NA |
|
ECC | 0.999 |
2.7x108 | NA |
|
GBC | 1 (Ref) | | |
| Tumor stage | 0.319 | 2.2 | 0.5-10.1 |
| Extrahepatic
metastasis | 0.800 | 1.2 | 0.2-6.8 |
| Lymph node
metastasis | 0.907 | 1.1 | 0.3-4.5 |
| Lung
metastasis | 0.520 | 2.0 | 0.2-18.0 |
| Bone
metastasis | 0.999 |
2.7x108 | NA |
| Peritoneum
metastasis | 0.757 | 1.3 | 0.2-6.9 |
| Intra-abdominal
implantation | 0.520 | 2.0 | 0.2-17.9 |
| Macrovascular
invasion | 0.931 | 0.9 | 0.1-8.5 |
| Previous
immunotherapy | 0.921 | 1.1 | 0.2-5.9 |
| Previous
antiangiogenic therapy | 0.840 | 1.3 | 0.1-11.4 |
| Previous treatment
lines | 0.304 | 2.1 | 0.5-8.7 |
| Previous
non-surgical local therapy | 0.473 | 1.7 | 0.4-7.0 |
| Previous
surgery | 0.721 | 0.8 | 0.2-3.2 |
Survival and disease progression. In the
cohort, one death was not caused by tumor progression, and median
TTP (mTTP) was 8.2 (95% CI, 4.9-11.6) months for the remaining 67
patients; mPFS and mOS were 5.5 (95% CI, 3.3-7.8) months and 10.7
(95% CI, 2.3-19.0) months, respectively, for all patients (Table III). Up to the end of follow-up,
54 patients (79.4%) had PD and 36 deaths had occurred (52.9%).
Univariate analyses showed that only tumor stage was significantly
associated with TTP and PFS. The mTTP of patients in stage III and
stage IV were 24.0 and 6.3 month, respectively (P=0.042). The mPFS
of patients in stage III and stage IV were 7.83 and 4.37 month,
respectively (P=0.035). Therefore, patients in stage III had longer
TTP and PFS compared to patients in stage IV. None of the evaluated
baseline characteristics were independent prognostic factors for OS
(Table V).
 | Table VUnivariate analyses of the effects of
baseline characteristics on TTP, PFS and OS. |
Table V
Univariate analyses of the effects of
baseline characteristics on TTP, PFS and OS.
| | TTP | PFS | OS |
|---|
| Baseline
characteristics | P-value | HR | 95% CI | P-value | HR | 95% CI | P-value | HR | 95% CI |
|---|
| Age | 0.283 | 0.7 | 0.4-1.3 | 0.182 | 0.7 | 0.4-1.2 | 0.989 | 1.0 | 0.5-1.9 |
| Sex | 0.938 | 1.0 | 0.6-1.8 | 0.867 | 1.0 | 0.6-1.8 | 0.933 | 1.0 | 0.5-1.9 |
| PS | 0.301 | 0.7 | 0.4-1.3 | 0.623 | 1.2 | 0.6-2,6 | 0.098 | 1.9 | 0.9-3.9 |
| Alcohol | 0.093 | 0.4 | 0.1-1.2 | 0.144 | 0.5 | 0.2-1.2 | 0.859 | 0.9 | 0.4-2.4 |
| Histology | 0.606 | | | 0.951 | | | 0.133 | | |
|
ICC | 1 (Ref) | | | 1 (Ref) | | | 1 (Ref) | | |
|
ECC | 0.805 | 0.9 | 0.3-2.5 | 0.753 | 1.2 | 0.5-3.0 | 0.284 | 1.8 | 0.6-5.2 |
|
GBC | 0.322 | 0.6 | 0.2-1.7 | 0.991 | 1.0 | 0.4-2.2 | 0.064 | 2.2 | 1.0-5.2 |
| Tumor stage | 0.042 | 2.5 | 1.0-5.9 | 0.035 | 2.3 | 1.1-4.9 | 0.244 | 1.8 | 0.7-4.5 |
| Extrahepatic
metastasis | 0.143 | 1.9 | 0.9-4.5 | 0.206 | 1.6 | 0.8-3.3 | 0.417 | 1.5 | 0.6-3.8 |
| Lymph node
metastasis | 0.673 | 1.1 | 0.6-2.1 | 0.833 | 0.8 | 0.5-1.4 | 0.599 | 1.2 | 0.6-2.3 |
| Lung
metastasis | 0.205 | 1.6 | 0.8-3.2 | 0.168 | 1.6 | 0.8-3.0 | 0.579 | 0.8 | 0.3-1.9 |
| Bone
metastasis | 0.741 | 0.8 | 0.3-2.7 | 0.381 | 1.5 | 0.6-3.9 | 0.269 | 1.8 | 0.6-5.1 |
| Peritoneum
metastasis | 0.739 | 0.9 | 0.5-1.7 | 0.084 | 1.7 | 0.9-3.0 | 0.225 | 1.5 | 0.8-3.1 |
| Intra-abdominal
implantation | 0.281 | 0.7 | 0.3-1.4 | 0.400 | 1.3 | 0.7-2.5 | 0.826 | 1.1 | 0.5-2.4 |
| Macrovascular
invasion | 0.288 | 0.5 | 0.2-1.7 | 0.722 | 0.8 | 0.3-2.2 | 0.733 | 0.8 | 0.2-2.7 |
| Previous
immunotherapy | 0.114 | 1.7 | 0.9-3.4 | 0.302 | 1.4 | 0.7-2.6 | 0.248 | 1.5 | 0.7-3.2 |
| Previous
antiangiogenic therapy | 0.506 | 0.7 | 0.3-1.8 | 0.984 | 1.0 | 0.5-2.1 | 0.461 | 0.7 | 0.2-1.9 |
| Previous treatment
lines | 0.422 | 1.3 | 0.7-2.4 | 0.067 | 1.7 | 1.0-3.1 | 0.239 | 1.5 | 0.8-3.1 |
| Previous
non-surgical local therapy | 0.477 | 1.3 | 0.7-2.3 | 0.705 | 0.9 | 0.5-1.6 | 0.916 | 1.0 | 0.5-2.0 |
| Previous
surgery | 0.377 | 1.3 | 0.7-2.4 | 0.836 | 1.1 | 0.6-1.8 | 0.749 | 0.9 | 0.5-1.7 |
Relation of treatment strategy and efficacy and
prognosis. In this study, 39.7% of patients used Camrelizumab
as the PD-1 inhibitor and 51.5% of patients used Lenvatinib as the
antiangiogenic drug. Since this is a small cohort of only 68
patients, it was divided into Camrelizumab-based group and the
other PD-1 inhibitors group in the subgroup analysis of PD-1
inhibitors, and it was divided into Lenvatinib-based group and the
other antiangiogenic drugs group in the subgroup analysis of
antiangiogenic drugs. Univariate and multivariate analyses were
conducted to identify the relationship between drug types and
treatment responses, TTP, PFS and OS. Univariate analyses showed
that types of antiangiogenic drugs was significantly associated
with PFS (P=0.037), but multivariate analyses did not show
significance. No significant difference was found in ORR, TTP, or
OS among different PD-1 inhibitors and antiangiogenic drugs
(Table VI).
 | Table VIThe influence of therapy strategies
on tumor response, TTP, PFS and OS. |
Table VI
The influence of therapy strategies
on tumor response, TTP, PFS and OS.
| | ORR | TTP | PFS | OS |
|---|
| Treatment
strategy | P-value | HR | 95% CI | P-value | HR | 95% CI | P-value | HR | 95% CI | P-value | HR | 95% CI |
|---|
| PD-1 inhibitors
(Camrelizumab vs. other) | 0.300 | 2.4 | 0.5-12.8 | 0.273 | 1.4 | 0.7-2.8 | 0.077 | 1.6 | 0.9-2,9 | 0.975 | 1.0 | 0.5-2.0 |
| Antiangiogenic
drugs (Lenvatinib vs. the other) | 0.394 | 0.5 | 0.1-2.3 | 0.374 | 1.3 | 0.7-2.5 | 0.26 5 | 0.7 | 0.4-1.3 | 0.146 | 0. 6 | 0.3-1.2 |
Adverse events
A total of fifty-eight patients (85.3%) experienced
at least one TRAE (Table VII).
The most frequent types of AEs were elevated liver enzymes (39.7%),
thrombocytopenia (32.4%), hyperbilirubinemia (29.4%), rash (20.6%),
anemia (19.1%) and anorexia (19.1%). Twenty-five patients reported
grade 3/4 AEs, and the three most common ≥3-grade AEs were
hypertension (5.9%), anemia (5.9%) and thrombocytopenia (4.4%). One
patient had a confirmed fatal TRAE which was hepatic failure caused
by autoimmune hepatitis. During our observation period, 23 (33.8%)
patients required dose delay, dose reduction, or discontinued
treatment due to TRAE.
 | Table VIITreatment-related adverse events
according to category and grade. |
Table VII
Treatment-related adverse events
according to category and grade.
| | Grade, n (%) |
|---|
| Event | Any | 3/4 | 5 |
|---|
| Elevated liver
enzymes | 27 (39.7) | 2 (2.9) | 0 (0.0) |
|
Thrombocytopenia | 22 (32.4) | 3 (4.4) | 0 (0.0) |
|
Hyperbilirubinemia | 20 (29.4) | 2 (2.9) | 0 (0.0) |
| Rash | 14 (20.6) | 2 (2.9) | 0 (0.0) |
| Anemia | 13 (19.1) | 4 (5.9) | 0 (0.0) |
| Anorexia | 13 (19.1) | 0 (0.0) | 0 (0.0) |
| Hypertension | 10 (14.7) | 4 (5.9) | 0 (0.0) |
| Leukopenia | 10 (14.7) | 1 (1.5) | 0 (0.0) |
| Diarrhea | 10 (14.7) | 0 (0.0) | 0 (0.0) |
| Fatigue | 7 (10.3) | 2 (2.9) | 0 (0.0) |
| Hand-foot
syndrome | 7 (10.3) | 2 (2.9) | 0 (0.0) |
| Pruritus | 6 (8.8) | 1 (1.5) | 0 (0.0) |
| Constipation | 6 (8.8) | 0 (0.0) | 0 (0.0) |
| Hypothyroidism | 4 (5.9) | 0 (0.0) | 0 (0.0) |
|
Nausea/vomiting | 3 (4.4) | 1 (1.5) | 0 (0.0) |
| Oral mucositis | 3 (4.4) | 0 (0.0) | 0 (0.0) |
| Enterocolitis | 2 (2.9) | 2 (2.9) | 0 (0.0) |
| Hemorrhage | 2 (2.9) | 0 (0.0) | 0 (0.0) |
| Autoimmune
hepatitis | 1 (1.5) | 0 (0.0) | 1 (1.5) |
| Interstitial
pneumonia | 1 (1.5) | 1 (1.5) | 0 (0.0) |
| Myocarditis | 1 (1.5) | 1 (1.5) | 0 (0.0) |
| Renal
dysfunction | 1 (1.5) | 0 (0.0) | 0 (0.0) |
Discussion
With broader accesses to tumor diagnostics and a
deep understanding of tumor microenvironment, the strategies using
antiangiogenic therapies and ICI have been realized for several
solid malignancies, while BTC remains a cancer type with scarce
therapeutic options. We conducted a retrospective study in patients
with unresectable BTC, not only to study the efficacy and safety of
PD-1 inhibitor plus antiangiogenic treatment but also to promote
the implementation of correlative clinical trials in the real
world.
The ORR of PD-1 inhibitors plus antiangiogenic
agents was 13.2% for unresectable BTC in our study, which was
similar to the ORR (4.0-13.8%) of the combination regimens for
unresectable BTC reported in clinical trials (12-14).
Furthermore, our cohort showed the DCR achieved 75.0%, mPFS and mOS
were 5.5 months and 10.7 months, respectively. In LEAP-005, the DCR
was 21.00%, and in REGOMUNE, mPFS and mOS were 2.5 months and 11.9
months, respectively (12,13). Compared with the very limited
prospective studies mentioned above, the result of our study
appears to be more optimistic possibly because we enrolled more
patients with better outcomes who had not previously received
systemic therapy as those patients reported in prospective studies.
In addition, the strategy chosen for patients in the clinic not
only follows the guidance but also takes cost, drug accessibility
and patient willingness into consideration.
Nowadays, systemic treatment in BTC is dominated by
chemotherapy with ongoing clinical trials on precision therapy and
immunotherapy. The efficacy of antiangiogenic treatments with
antibodies (e.g. bevacizumab and ramucirumab) or TKIs (e.g.
sorafenib and regorafenib) and anti-PD-1 therapy (e.g.
pembrolizumab and nivolumab) has been investigated in combination
with chemotherapy. There is accumulating evidence that chemotherapy
might have a synergistic effect with immunotherapy on advanced BTC
(15-17).
A recent phase II study of the combination of pembrolizumab with
capecitabine and oxaliplatin has shown moderate efficacy with DCR
of 81.8% and mPFS was 4.1 months, which is not as good as the
result of another phase II study of nivolumab plus GC (DCR 92.6%,
mPFS 6.1 months) (18,19). The value of immunotherapy
predictive response biomarkers such as PD-L1 in BTC has not been
confirmed in clinical settings due to the high genetic
heterogeneity in BTC and the lack of heterogeneous subgroups of
patients in cohorts. Besides, PD-1 inhibitors combined with
antiangiogenic therapies, including the regimens in our study, are
not as effective as the combination with chemotherapy. Unlike
immunotherapy, the combination of antiangiogenic treatment with
conventional chemotherapy did not confer any advantage in phase II
AIO study as there was no difference in the mPFS and mOS for
gemcitabine plus sorafenib versus GC (mPFS, 3.0 vs. 4.9 months,
P=0.859; mOS, 8.4 versus 11.2 months, P=0.775) (20), and the result in our study also
compares favorably to which of group gemcitabine plus sorafenib.
Due to limited data, more studies are needed to reveal whether the
regimen of antiangiogenic agent plus chemotherapy is recommended in
this setting.
It is noteworthy that our study enrolled 27 patients
who were not previously treated at baseline, and the efficacy of
PD-1 inhibitors combined with antiangiogenic agents as first-line
therapy are as follows: the ORR and DCR achieved 18.5 and 80.8%,
respectively; mPFS and mOS were 9.1 (95% CI, 5.0-13.1) months and
18.3 (95% CI, 4.0-32.8) months, respectively. As the standard
first-line regimen for unresectable or recurrent BTC, GC therapy
had a DCR of 81.4%, a mPFS of 8.0 (95% CI, 6.6-8.6) months, and a
mOS of 11.7 (95% CI, 9.5-14.3) months (1). Therefore, our results suggested that
the new strategy of PD-1 inhibitor combined with antiangiogenic
agent as first-line treatment might be superior to standard
chemotherapy. Based on TOPAZ-1 study, durvalumab in combination
with GC has been recommended as standard first-line therapy for
recurrent BTC recently (16). Data
showed that the ORR in TOPAZ-1 study was higher than the ORR in our
study (26.7% vs. 18.5%), however, mPFS and mOS in TOPAZ-1 study
were shorter than those in our study (mPFS, 7.2 vs. 9.1 months;
mOS, 12.8 vs. 18.3 months). The difference of efficacy and
prognosis might be attributed to the treatment strategy, enrollment
criteria and later therapy. Besides, clinical trials of
chemotherapy with antiangiogenic therapy as first-line therapy for
BTC are under investigation. A phase II study found that mPFS in
ramucirumab plus GC group and merestinib plus GC group were 6.5
(80% CI, 5.7-7.1) months and 7.0 (80% CI, 6.2-7.1) months,
respectively (21), which were
shorter than those in our cohort. However, the efficacy of the
first-line therapy in our study and first-line therapy of
camrelizumab plus oxaliplatin-based chemotherapy in a phase 2 trial
are comparable based on confirmed ORR (18.5% vs. 16.3%) and DCR
(80.8% vs. 75.0%) (22). Thus, as
the first-line therapy, PD-1 inhibitor combined with antiangiogenic
agent might provide promising efficacy in advanced BTC patients and
offer an alternative for advanced BTC who cannot tolerate
chemotherapy. Further prospective studies are needed to confirm
this finding.
Hyperprogressive disease (HPD) is a new pattern of
response consisting in a sudden acceleration of tumor growth in
ICIs (23). The incidence of HPD
across solid tumors is reported between 4-29% (24). The diagnostic criteria for HPD
remains controversial and the most widely used criteria contain
RECIST and tumor growth rate (TGR) or tumor growth kinetic of the
target lesions according to RECIST 1.1 criteria per month)
(25,26). So far, there is a lack of available
published data on HPD in clinical studies conducted of BTC
treatment. In our retrospective analysis, 2 patients had an initial
progressive disease defined by visualization of the significantly
increased target lesion (100 and 320%, respectively) based on
RECIST within 2 months of treatment. The TGR of these two patient
after treatment is more than twice the previous rate. Thus, 2
(2.9%) patients with BTC experienced HPD in our study.
The frequency of TRAEs in our study were comparable
to the known AEs of PD-1 inhibitor and antiangiogenic agent. Grade
≥3 TRAEs to the combined strategy of PD-1/PD-L1 inhibitor with
antiangiogenic agent occurred from 17.6 to 48.4% in clinical trials
of BTC (12-14),
similar with which reported in our study (36.8%). Thrombocytopenia
is one of known AEs to anti-PD-1 therapy, rash and hypertension are
common AEs to antiangiogenic therapy. Though elevated liver enzymes
and hyperbilirubinemia were the most common AEs in this study, a
number of patients with BTC suffer from complications of liver
insufficiency due to primary disease progression. In addition, most
TRAEs observed in the study including hypertension, rash and
hand-foot syndrome, were related to antiangiogenic agents. Further
research is required to identify predictive biomarkers to improve
assessment before enrollment to ensure safety of patients who
receive the combination therapy.
There are a few limitations in our study. First,
it's a retrospective study with a small sample of patients, which
inevitably caused bias. Second, we observed OS from thirty-five
patients (51.5%) in this cohort and insufficient follow-up
information is an inevitable issue. Hopefully, prospective clinical
trials including LEAP-005 study is providing novel findings. Third,
all of the combined regimens were heterogeneous and off-label used
in the study, though different combinations have been shown to have
no significant effect on the efficacy and prognosis of BTC, there
is currently a lack of independent prospective studies to provide
appropriate drug strategies. Finally, biomarkers were not recorded
and analyzed to select the molecular subgroups that are most likely
to benefit from the combined regimens in our study.
Immunotherapy represented by PD-1 inhibitors has
shown initial effect in advanced BTC, and the combination of drugs
is worth further exploration. In addition, biomarkers are required
to select the molecular subgroups most likely to benefit from
immunotherapy and immunotherapy-based combinations. With the
collective data of PD-1 inhibitor combined with antiangiogenic
agent, the combination regimens might exhibit active clinical
activity for BTC.
In conclusion, in this multicenter and retrospective
study, we evaluated the efficacy and safety of the combination of
PD-1 inhibitor and antiangiogenic therapy in patients with
unresectable BTC in a real-world setting. These promising data
might provide opportunities for chemo-free therapy in advanced BTC
patients, and the feasibility of the combination therapy in the
clinic is waiting to be validated by further prospective studies
with larger-scale samples and biomarker detections.
Acknowledgements
Not applicable.
Funding
Funding: This work was supported by the National Natural Science
Foundation of China (grant no. 81803070), and Zhejiang Provincial
Natural Science Foundation of China under Grant (grant no.
LSY19H160006).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Author's contributions
ZW, XuZ, XiZ, YW, YZ, WH, HP and JY contributed to
the study conception and design. Material preparation, data
collection and analysis were performed by ZW, XuZ and XiZ. The
first draft of the manuscript was written by ZW and JY, and all
authors commented on previous versions of the manuscript. JY, XuZ
and XiZ confirm the authenticity of all the raw data. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
This study was performed in line with the principles
of the Declaration of Helsinki. Approval was granted by the
Institutional Review Board of Sir Run Run Shaw Hospital (Hangzhou,
China; approval no. 2021332), The First Affiliated Hospital,
Zhejiang University (Hangzhou, China; approval no. 2021734) and The
Second Affiliated Hospital, Zhejiang University (Hangzhou, China;
approval no. I20211065).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Valle J, Wasan H, Palmer DH, Cunningham D,
Anthoney A, Maraveyas A, Madhusudan S, Iveson T, Hughes S, Pereira
SP, et al: Cisplatin plus gemcitabine versus gemcitabine for
biliary tract cancer. N Engl J Med. 362:1273–1281. 2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Eckel F and Schmid RM: Chemotherapy in
advanced biliary tract carcinoma: A pooled analysis of clinical
trials. Br J Cancer. 96:896–902. 2007.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chu T, Zhong R, Zhong H, Zhang B, Zhang W,
Shi C, Qian J, Zhang Y, Chang Q, Zhang X, et al: Phase 1b study of
sintilimab plus anlotinib as first-line therapy in patients with
advanced NSCLC. J Thorac Oncol. 16:643–652. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Yau T, Park JW, Finn RS, Cheng AL,
Mathurin P, Edeline J, Kudo M, Harding JJ, Merle P, Rosmorduc O, et
al: Nivolumab versus sorafenib in advanced hepatocellular carcinoma
(CheckMate 459): A randomised, multicentre, open-label, phase 3
trial. Lancet Oncol. 23:77–90. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Mao J, Yang X, Lin J, Yang X, Wang D,
Zhang L, Bai Y, Bian J, Long J, Xie F, et al: Apatinib as
non-first-line treatment in patients with Intrahepatic
Cholangiocarcinoma. J Cancer. 12:1555–1562. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ueno M, Ikeda M, Sasaki T, Nagashima F,
Mizuno N, Shimizu S, Ikezawa H, Hayata N, Nakajima R and Morizane
C: Phase 2 study of lenvatinib monotherapy as second-line treatment
in unresectable biliary tract cancer: Primary analysis results. BMC
Cancer. 20(1105)2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kim RD, Sanoff HK, Poklepovic AS, Soares
H, Kim J, Lyu J, Liu Y, Nixon AB and Kim DW: A multi-institutional
phase 2 trial of regorafenib in refractory advanced biliary tract
cancer. Cancer. 126:3464–3470. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Sun W, Patel A, Normolle D, Patel K, Ohr
J, Lee JJ, Bahary N, Chu E, Streeter N and Drummond S: A phase 2
trial of regorafenib as a single agent in patients with
chemotherapy-refractory, advanced, and metastatic biliary tract
adenocarcinoma. Cancer. 125:902–909. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Piha-Paul SA, Oh D, Ueno M, Malka D, Chung
HC, Nagrial A, Kelley RK, Ros W, Italiano A, Nakagawa K, et al:
Efficacy and safety of pembrolizumab for the treatment of advanced
biliary cancer: Results from the KEYNOTE-158 and KEYNOTE-028
studies. Int J Cancer. 147:2190–2198. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kim RD, Chung V, Alese OB, El-Rayes BF, Li
D, Al-Toubah TE, Schell MJ, Zhou JM, Mahipal A, Kim BH and Kim DW:
A Phase 2 multi-institutional study of nivolumab for patients with
advanced refractory biliary tract cancer. JAMA Oncol. 6:888–894.
2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hao Z and Wang P: Lenvatinib in management
of solid tumors. Oncologist. 25:e302–e310. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lwin Z, Gomez-Roca C, Saada-Bouzid E, Im
SA, Castanon E, Senellart H, Graham D, Voss M, Doherty M, Lopez J,
et al: LBA41 LEAP-005: Phase II study of apa (len) plus
pembrolizumab (pembro) in patients (pts) with previously treated
advanced solid tumours. Ann Oncol. 31(S1170)2020.
|
|
13
|
Cousin S, Cantarel C, Guegan JP, Mazard T,
Gomez-Roca C, Metges JP, Bellera C, Adenis A, Korakis I, Poureau
PG, et al: Regorafenib-avelumab combination in patients with
biliary tract cancer (REGOMUNE): A single-arm, open-label, phase II
trial. Eur J Cancer. 162:161–169. 2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Arkenau H, Martin-Liberal J, Calvo E,
Penel N, Krebs MG, Herbst RS, Walgren RA, Widau RC, Mi G, Jin J, et
al: Ramucirumab plus pembrolizumab in patients with previously
treated advanced or metastatic biliary tract cancer: Nonrandomized,
open-label, phase I trial (JVDF). Oncologist. 23:1407–e136.
2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ueno M, Ikeda M, Morizane C, Kobayashi S,
Ohno I, Kondo S, Okano N, Kimura K, Asada S, Namba Y, et al:
Nivolumab alone or in combination with cisplatin plus gemcitabine
in Japanese patients with unresectable or recurrent biliary tract
cancer: A non-randomised, multicentre, open-label, phase 1 study.
Lancet Gastroenterol Hepatol. 4:611–621. 2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Oh DY, He AR, Qin S, Chen LT, Okusaka T,
Vogel A, Kim JW, Suksombooncharoen T, Lee MA, Kitano M, et al: A
phase 3 randomized, double-blind, placebo-controlled study of
durvalumab in combination with gemcitabine plus cisplatin (GemCis)
in patients (pts) with advanced biliary tract cancer (BTC):
TOPAZ-1. J Clin Oncol. 40(378)2022.
|
|
17
|
Salas-Benito D, Pérez-Gracia JL,
Ponz-Sarvisé M, Rodriguez-Ruiz ME, Martínez-Forero I, Castañón E,
López-Picazo JM, Sanmamed MF and Melero I: Paradigms on
immunotherapy combinations with chemotherapy. Cancer Discov.
11:1353–1367. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Monge C, Pehrsson EC, Xie C, Duffy AG,
Mabry D, Wood BJ, Kleiner DE, Steinberg SM, Figg WD, Redd B, et al:
A phase II study of pembrolizumab in combination with capecitabine
and oxaliplatin with molecular profiling in patients with advanced
biliary tract carcinoma. Oncologist. 27:e273–e285. 2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Feng K, Liu Y, Zhao Y, Yang Q, Dong L, Liu
J, Li X, Zhao Z, Mei Q and Han W: Efficacy and biomarker analysis
of nivolumab plus gemcitabine and cisplatin in patients with
unresectable or metastatic biliary tract cancers: Results from a
phase II study. J Immunother Cancer. 8(e000367)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Moehler M, Maderer A, Schimanski C,
Kanzler S, Denzer U, Kolligs FT, Ebert MP, Distelrath A, Geissler
M, Trojan J, et al: Gemcitabine plus sorafenib versus gemcitabine
alone in advanced biliary tract cancer: A double-blind
placebo-controlled multicentre phase II AIO study with biomarker
and serum programme. Eur J Cancer. 50:3125–3135. 2014.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Valle JW, Vogel A, Denlinger CS, He AR,
Bai LY, Orlova R, Van Cutsem E, Adeva J, Chen LT, Obermannova R, et
al: Addition of ramucirumab or merestinib to standard first-line
chemotherapy for locally advanced or metastatic biliary tract
cancer: A randomised, double-blind, multicentre, phase 2 study.
Lancet Oncol. 22:1468–1482. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Chen X, Qin S, Gu S, Ren Z, Chen Z, Xiong
J, Liu Y, Meng Z, Zhang X, Wang L, et al: Camrelizumab plus
oxaliplatin-based chemotherapy as first-line therapy for advanced
biliary tract cancer: A multicenter, phase 2 trial. Int J Cancer.
149:1944–1954. 2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Champiat S, Dercle L, Ammari S, Massard C,
Hollebecque A, Postel-Vinay S, Chaput N, Eggermont A, Marabelle A,
Soria JC and Ferté C: Hyperprogressive disease is a new pattern of
progression in cancer patients treated by Anti-PD-1/PD-L1. Clin
Cancer Res. 23:1920–1928. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Martin-Romano P, Castanon E, Ammari S,
Champiat S, Hollebecque A, Postel-Vinay S, Baldini C, Varga A,
Michot JM, Vuagnat P, et al: Evidence of pseudoprogression in
patients treated with PD1/PDL1 antibodies across tumor types.
Cancer Med. 9:2643–2652. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Kanjanapan Y, Day D, Wang L, Al-Sawaihey
H, Abbas E, Namini A, Siu LL, Hansen A, Razak AA, Spreafico A, et
al: Hyperprogressive disease in early-phase immunotherapy trials:
Clinical predictors and association with immune-related toxicities.
Cancer. 125:1341–1349. 2019.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Saâda-Bouzid E, Defaucheux C, Karabajakian
A, Coloma VP, Servois V, Paoletti X, Even C, Fayette J, Guigay J,
Loirat D, et al: Hyperprogression during anti-PD-1/PD-L1 therapy in
patients with recurrent and/or metastatic head and neck squamous
cell carcinoma. Ann Oncol. 28:1605–1611. 2017.PubMed/NCBI View Article : Google Scholar
|