Introduction
Transoral endoscopic thyroid surgery via a
vestibular approach is currently considered a feasible and safe
surgical method (1). Transoral
vestibular approach thyroid surgery has become the most common
established remote access technique to avoid the traditional
transcervical incision or any other cutaneous incision since its
initial description (2).
Nonetheless, in some patients with thyroid disease, born with short
chins and mandibular retrusion, chin augmentation techniques have
achieved improved outcomes with high patient satisfaction (3). If transoral endoscopic thyroid
surgery via a vestibular approach is performed in these patients,
chin augmentation genioplasty performed in same incision and same
period prevents further trauma (1). As infection rates seem to be as low
as in conventional open thyroid surgery, infection does not to be a
specific problem of transoral thyroid surgery (4). However, the feasibility of transoral
endoscopic thyroid surgery via a vestibular approach with chin
augmentation genioplasty remains unclear and the safety of this
approach should be established. To the best of our knowledge, there
are no reports available in the literature to show the operation of
transoral endoscopic thyroid surgery via a vestibular approach and
chin augmentation genioplasty together. The main concerns for
surgeons may be the insurgence of infection and implant
displacement. To address these issues, the present study reports 3
cases in which these two surgical approaches were compared.
Material and methods
Patients
The following patient inclusion criteria were used
in the present study: i) Diagnosis of papillary thyroid cancer
(PTC), with or without lateral lymph node metastasis, and
microgenia; ii) a strong desire for good facial aesthetics; iii)
microgenia urgently needing surgical treatment; and iv) thyroid
tumor and lymph node without severe invasion. The exclusion
criteria were as follow: i) Previous neck surgery history; ii)
metastatic lymph nodes in the level I or V region; iii) metastatic
lymph nodes fused or fixed in the neck; iv) invasion of surrounding
tissues, such as recurrent laryngeal nerve or tracheal; and v) oral
abscess or previous radiation to head and neck. A total of 3 female
patients with PTC and microgenia were diagnosed and treated from
July 2020 to March 2022 in Zhongshan Hospital, Xiamen University
(Xiamen, China). All patients were diagnosed with papillary thyroid
cancer based on fine-needle aspiration. Case no. 1 and 3 presented
with papillary thyroid cancer, while case no. 2 presented with
papillary thyroid cancer with lateral lymph node metastasis.
The chins of the patients were evaluated
preoperatively and postoperatively by a plastic surgeon and
recorded using image documentation. For the follow-up, patient
satisfaction and complications were also recorded. Patient
demographics, outcomes and post-surgery complications were
collected retrospectively. The study protocol was approved by The
Ethics and Scientific Review Board of Zhongshan Hospital of Xiamen
University (Xiamen, China; approval no. 2021-078). Written informed
consent was obtained from all the participants. All methods were
performed following the relevant guidelines and regulations of the
Declaration of Helsinki (5).
Surgical technique
A prophylactic antibiotic (100 ml cefazolin sodium 2
g in 0.9% normal saline) was administered intravenously 30 min
before the incision (6). Each
patient was placed in the supine position and a pillow was placed
under the patient's shoulder to slightly extend the neck. An
endotracheal tube embedded with neuromonitoring electrodes was used
for general anesthesia via the oral route by positioning on the
right side of the mouth. A 20-mm transverse incision was made in
the midline of the oral vestibule, right above the inferior labial
frenulum. Electrocautery was used to divide the submucosa and
mentalis muscle to allow access to the edge of the mandible. A
total of 20 ml of a diluted epinephrine-saline solution
(1:2,000,000; Yuanda Pharmaceutical China Co., Ltd.) was injected
through the lower lip down to the tip of the chin and upper neck
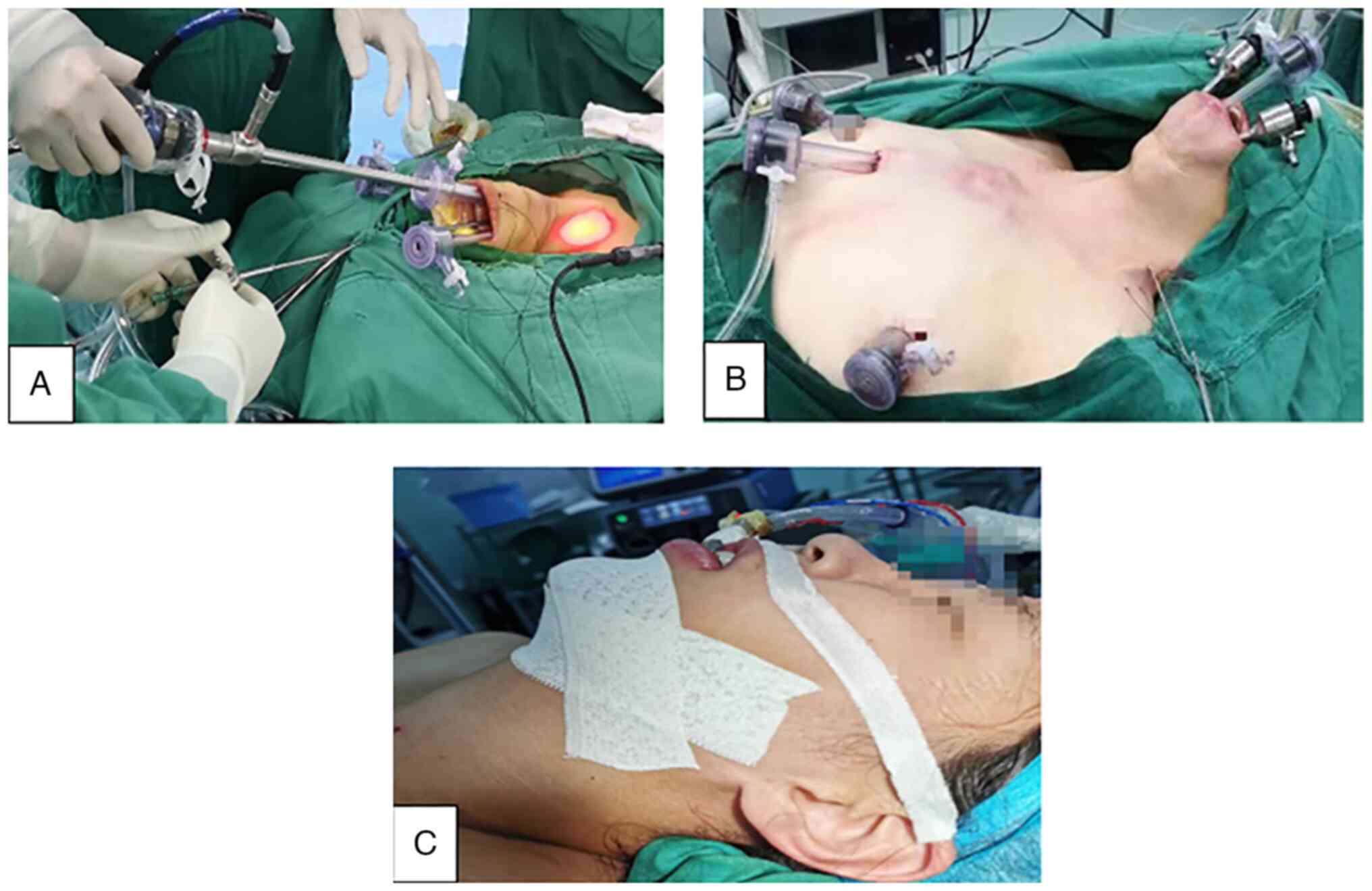
after the incision of the vestibule. Case no. 1 and 3 were operated
on using transoral endoscopic thyroid surgery via the vestibular
approach (Fig. 1A). Case no. 2 was
operated on using endoscopic lateral neck dissection via the breast
and transoral approaches (ELNDBTOA) (Fig. 1B) (7). After endoscopic thyroid surgery, the
endoscopic working space was washed with 1,000 ml of warm distilled
water. A 3-0 Quill//' absorbable suture was used to suture the
belt-shaped muscle and the drainage tube was placed in the
submental area or through the mammary areolar incision (8).
The plastic surgeon of the hospital started to
perform the chin augmentation genioplasty. The silastic was
sculpted to meet the shape of the chin. Oral regions were second
sterilized with iodophor (Shanghai Likang Disinfection High Tech
Co., Ltd). The surgical technique involved the creation of an
optimized pocket in which the silastic could be placed. The
silastic was sutured to the surrounding tissue with 3-0 Ethicon
Vicryl to minimize the risk of implant migration. The muscles of
the vestibule were sutured with 3-0 absorbable thread and the oral
mucosal incision was closed using 4-0 absorbable sutures. The chin
was fixed with adhesive tape to also prevent implant migration
(Fig. 1C).
Postoperative follow-up. Ultrasonography was
performed to assess the thyroid bed and lateral neck compartment 6
months after operation. Cosmetic results were evaluated on a verbal
response scale (9). The verbal
response scale included four options: 1=Poor; 2=acceptable; 3=good;
and 4=excellent. All patients were asked to grade the cosmetic
result at 1 month after operation.
Results
Patient demographic and clinicopathologic details
are listed in Table I. None of the
patients developed major complications (e.g., postoperative
bleeding, neck infection, chyle leakage, vocal cord paralysis or
hypoparathyroidism). All patients developed transient skin numbness
in the mandibular area and patient no.1 recovered within 4 months,
patient no. 2 within 1 month and patient no. 3 within 2 months,
which is similar to ordinary endoscopic transoral thyroid surgery
(8). The longest follow-up period
was 22 months (range, 2-22 months). The incisions in the oral
cavity and breast healed well in all the patients according to the
SCAR (Scar Cosmesis Assessment and Rating) scale (10).
 | Table IPatient demographics and
clinicopathologic details. |
Table I
Patient demographics and
clinicopathologic details.
| | Case no. |
|---|
| Patient
characteristics | 1 | 2 | 3 |
|---|
| Age, years | 29 | 17 | 25 |
| Sex | Female | Female | Female |
| Tumor location | Right | Right | Left |
| Lateral neck lymph
node metastasis | No | Yes | No |
| Retrieved LN | 7 | 66 | 8 |
| Metastatic LN | 0 | 17 | 1 |
| TNM stage | T1N0M0 | T3N1bM0 | T1N1aM0 |
| Operation time,
min | 177 | 437 | 110 |
| Operative bleeding,
ml | 15 | 50 | 10 |
| Follow-up,
months | 22 | 9 | 2 |
| Postoperative
infection | No | No | No |
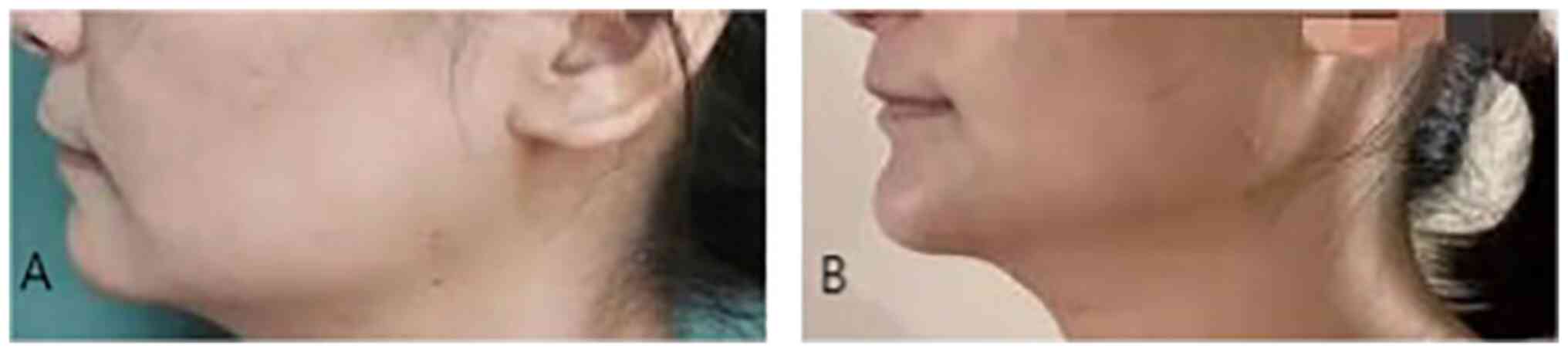
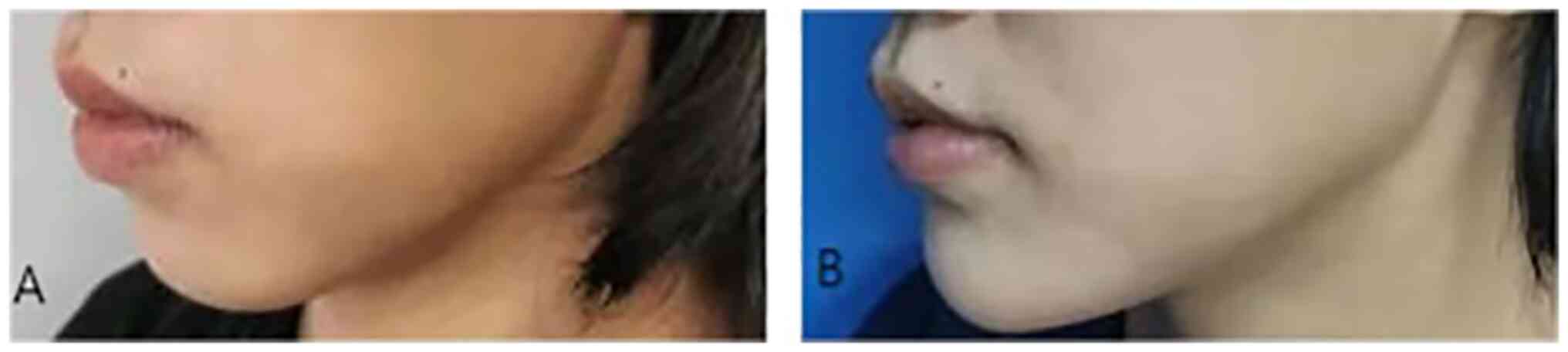
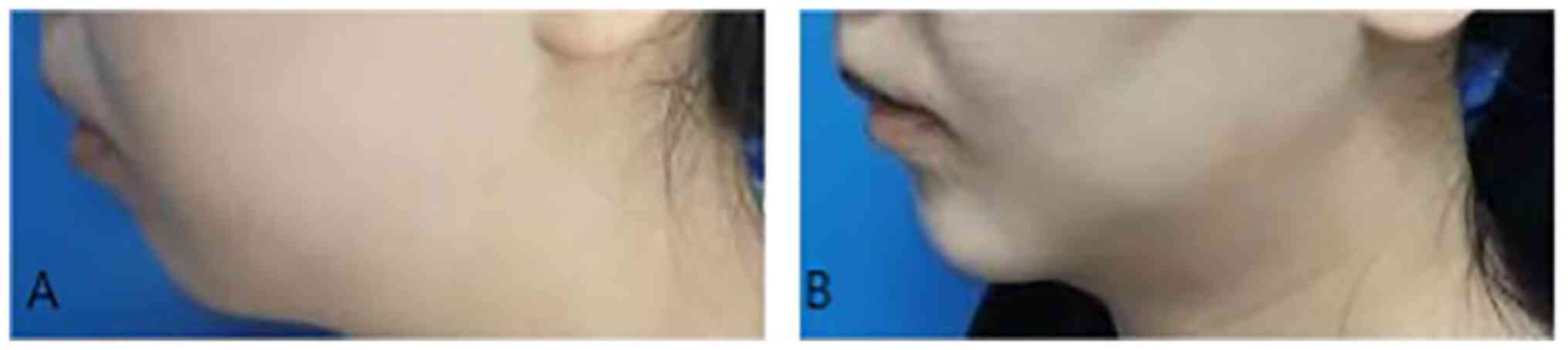
There were no complications, such as infection or
displacement of the implant. All patients were satisfied with the
cosmetic outcomes (Fig. 2,
Fig. 3 and Fig. 4). There was no evidence of local
recurrence or distant metastases. The verbal response scale of
cosmetic results in all three patients were 4 grade.
Discussion
In 2009, Wilhelm and Metzig (11) made the first known attempt at
transoral endoscopic thyroid surgery in Germany. The surgery was
performed via a sublingual approach combined with a vestibular
approach. This approach presented several advantages compared with
transoral thyroid surgery such as moving the incision site out of
the visible cervical region to meet the higher cosmetic demands of
patients, and it was further developed into a total vestibular
approach (1). Transoral endoscopic
thyroid surgery via the vestibular approach was appropriate for
treating PTC without lateral lymph node metastasis, while for PTC
with lateral lymph node metastasis, the ELNDBTOA was performed in
the general surgery department of Zhongshan Hospital, Xiamen
University (7). According to the
present clinical observation, some patients suffered from thyroid
cancer and microgenia simultaneously in ZhongShan Hospital, Xiamen
University.
Facial aesthetics can affect a patient's appearance
and self-esteem, and the chin is an important feature in the
aesthetic perception of the face. A deficient chin may be short or
shrink back, which is diagnosed as microgenia. Genioplasty is an
efficient treatment option for the correction of chin deformities
(12). Since transoral endoscopic
thyroid surgery via the vestibular approach and chin augmentation
genioplasty both involve the chin, it was hypothesized that it was
possible to perform these two operations at the same time.
A wide variety of materials such as silastic (solid
silicone), mersilene mesh (polyester fiber mesh), supramid
(polymide nylon mesh), proplast (polytef), medpor (porous
polyethylene) and Gore-Tex (polytetrafluoroethylene) in chin
augmentation are currently available (13). These materials vary in density,
ability to be sculpted, tissue reaction, resorption, migration, the
incidence of infection, extrusion rate and ease of removal.
Silastic augmentation genioplasty is a common procedure, with
consistent aesthetic results in properly selected patients who have
short chins and mandibular retrusion (13). Silastic augmentation genioplasty
may be the best choice if there are any concerns regarding
infection or potential future infection (13). It is also inexpensive and easily
sculpted; therefore, it was selected for the present study.
Common complications of chin implantation include,
in decreasing order of importance, asymmetry, malposition,
infection, extrusion, mental nerve dysfunction and chin ptosis
(14,15). A case series of 324 chin implants
found an infection rate of 0.62%, while another case series of 125
consecutive patients reported no infections (16,17).
It has been suggested that the infection rate may increase after
the proposed combination surgery since transoral endoscopic thyroid
surgery via a vestibular approach and the ELNDBTOA are long
surgeries. Nonetheless, the present cases did not present with
related complications. The absence of related complications might
be due to the small number of cases considered in the present study
and the short follow-up time. One drawback of a silastic chin
prosthetic is the risk of resorption at the implant-bone interface
(18). Porous polyethylene
typically presents a higher risk of infection and was therefore not
used in the present study (19).
Perhaps another attractive alternative chin implant material may be
developed in the future. Further investigation is needed to
elucidate this new technique and assess the rates of infection and
extrusion.
Despite the study being limited to these 3 selected
patients with PTC and microgenia, the follow-up to the initial
description of the new technique established the safety and
efficacy of the procedure. This new combined technique needs to be
further explored to confirm its feasibility and safety.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YYW analyzed the data and wrote, prepared and
submitted the manuscript. GW conceived the study and designed and
performed all the surgeries of transoral thyroid surgery. YYW, FL,
WY and SL collected and analyzed the data and revised the
manuscript critically. YZ prepared the figures, collected and
analyzed the data and performed all the surgeries of chin silastic
augmentation genioplasty. YL collected and analyzed the data and
prepared the figures. GW and YZ confirm the authenticity of all the
raw data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study protocol was approved by The Ethics and
Scientific Review Board of the Zhongshan Hospital of Xiamen
University (Xiamen, China; approval no. 2021-078).
Patient consent for publication
All patients provided verbal and written consent for
publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Anuwong A, Ketwong K, Jitpratoom P,
Sasanakietkul T and Duh QY: Safety and outcomes of the transoral
endoscopic thyroidectomy vestibular approach. JAMA Surg. 153:21–27.
2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Tufano RP and Mohamed Ali K: The year in
surgical thyroidology: Recent technological developments and future
challenges. Thyroid. 32:14–18. 2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Oranges CM, Grufman V, di Summa PG,
Fritsche E and Kalbermatten DF: Chin augmentation techniques: A
systematic review. Plast Reconstr Surg: Dec 20, 2022 (Epub ahead of
print).
|
|
4
|
Karakas E, Klein G, Michlmayr L, Schardey
M and Schopf S: Endoscopic Thyroid and Parathyroid Surgery Study
Group. Transoral thyroid surgery vestibular approach: Is there an
increased risk of surgical site infections? Updates Surg.
74:303–308. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
World Medical Association: World Medical
Association Declaration of Helsinki. Ethical principles for medical
research involving human subjects. Bull World Health Organ.
79:373–374. 2001.PubMed/NCBI
|
|
6
|
Luo YZ, Fu YL, Wu GY, Fu JB, Lin SQ, Song
ZF, Chen JY, Yan W, Kuang PH, Lin ED, et al: Clinical experience in
transoral endoscopic thyroidectomy via sublingual and vestibular
approach: A report of 98 cases. Zhonghua Er Bi Yan Hou Tou Jing Wai
Ke Za Zhi. 55:899–904. 2020.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
7
|
Wu GY, Fu JB, Luo YZ, Yan W, Hong XQ,
Kuang PH, Lin ED, Lin FS, Song ZF, Chen JY and Fu YL: Endoscopic
lateral neck dissection via the breast and transoral approaches for
papillary thyroid carcinoma: A report of 10 cases. Zhonghua.
56:751–754. 2021.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
8
|
Zheng G, Ma C, Sun H, Wu G, Guo Y, Wu G
and Zheng H: Safety and surgical outcomes of transoral endoscopic
thyroidectomy vestibular approach for papillary thyroid cancer: A
two-centre study. Eur J Surg Oncol. 47:1346–1351. 2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Miccoli P, Berti P, Raffaelli M, Materazzi
G, Baldacci S and Rossi G: Comparison between minimally invasive
video-assisted thyroidectomy and conventional thyroidectomy: A
prospective randomized study. Surgery. 130:1039–1043.
2001.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kantor J: The SCAR (Scar Cosmesis
Assessment and Rating) scale: Development and validation of a new
outcome measure for postoperative scar assessment. Br J Dermatol.
175:1394–1396. 2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wilhelm T and Metzig A: Video. Endoscopic
minimally invasive thyroidectomy: First clinical experience. Surg
Endosc. 24:1757–1758. 2010.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Romo T III and Lanson BG: Chin
augmentation. Facial Plast Surg Clin North Am. 16:69–77.
2008.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Adams JS: Grafts and implants in nasal and
chin augmentation. A rational approach to material selection.
Otolaryngol Clin North Am. 20:913–930. 1987.PubMed/NCBI
|
|
14
|
Cuzalina LA and Hlavacek MR: Complications
of facial implants. Oral Maxillofac Surg Clin North Am. 21. 91–104,
vi-vii. 2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Zide BM: The mentalis muscle: An essential
component of chin and lower lip position. Plast Reconstr Surg.
105:1213–1215. 2000.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Aynehchi BB, Burstein DH, Parhiscar A and
Erlich MA: Vertical incision intraoral silicone chin augmentation.
Otolaryngol Head Neck Surg. 146:553–559. 2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Godin M, Costa L, Romo T, Truswell W, Wang
T and Williams E: Gore-Tex chin implants: A review of 324 cases.
Arch Facial Plast Surg. 5:224–227. 2003.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Rubin JP and Yaremchuk MJ: Complications
and toxicities of implantable biomaterials used in facial
reconstructive and aesthetic surgery: A comprehensive review of the
literature. Plast Reconstr Surg. 100:1336–1353. 1997.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ramieri V, Maffìa F, Vellone V, Marianetti
S and Marianetti TM: The Pyramid Chin Augmentation: A new
technique. J Craniofac Surg. 32:738–739. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Amin MB, Edge SB, Greene FL eds, et al:
AJCC Cancer Staging Manual. 8th ed. New York: Springer
International Publishing; 2017.
|