Introduction
Cancer is one of the greatest challenges to public
health, as it has been the leading cause of mortality for several
decades (1). Worldwide, cervical
and prostate cancers represent two cancers with high incidence in
women and men, respectively (2).
The introduction of early detection strategies and improvements in
cancer therapy have made it possible, in developed countries, to
reduce the incidence of cancer and improve patient survival
(1); however, current treatments
are expensive and have serious adverse effects (3). Due to the aforementioned, the search
for new treatments has increased considerably and new proposals
have focused on developing more effective treatments with fewer
adverse effects and with greater accessibility for the population.
Drug repositioning is important for optimizing the preclinical
process of new drug development, as it saves time and costs
compared with traditional processes for de novo drug
discovery (4). The purpose of
synthesizing new compounds from existing drugs, such as dapsone
(DDS), is to improve their activity and reduce their adverse
effects. In 1961, Ross (5) first
suggested the use of DDS as a safer and cheaper option compared
with other systemic antibiotics for the treatment of acne vulgaris
and recommended an oral dose of 50-150 mg of DDS per day, which
showed no side effects after seven days (5). DDS is also recognized for treating
leprosy and is used for a variety of other dermatological
conditions, including dermatitis herpetiformis (6). As an antibacterial drug, DDS inhibits
the synthesis of dihydrofolic acid through the inhibition of
para-aminobenzoic acid at the dihydropteroate synthetase
active site (7). In acne vulgaris,
in addition to its antimicrobial effect, DDS has an
anti-inflammatory effect (8) and
has been found to inhibit chemoattractant signaling (9-11).
Some evidence also suggests that DDS might have inhibitory effects
on myeloperoxidase in neutrophils, causing inflammation and tissue
damage (7). According to the
Biopharmaceutics Classification System (BCS), DDS is classified as
a class II lipophilic drug with low solubility and high
permeability (12) and, at high
doses, it has significant adverse effects, such as hemolysis and
methemoglobinemia (13). To date,
there have been few studies evaluating the effects of DDS on types
of cancer. An in vitro study highlighted DDS as an adjunct
in the treatment of glioblastoma, possibly by blocking neutrophil
migration to the tumor directed by low IL-8 and VEGF expressions,
as well as low leukotriene synthesis (11). In the present study, the synthetic
derivative of DDS (DDS-13) was selected because it has not been
tested biologically or functionally to evaluate its pharmacological
properties against other types of cancer. Therefore, the present
study focused on evaluating the anticancer effects of DDS and its
synthetic derivative DDS-13 in an in vitro study. The
chemical structures of the compounds are shown in the results
section (Fig. 1).
Materials and methods
Chemistry. Reagents
DDS (CAS 80-08-0), methyl caprylate (CAS 111-11-5)
and triethylamine (CAS 121-44-8) were purchased from MilliporeSigma
and used without prior purification. All of the solvents which were
used were ACS-grade and purchased from J.T. Baker, Inc. The
solvents were dried and purified in accordance with standard
procedures (14). The
microwave-assisted synthesis was performed using a CEM Discovery
BenchMate apparatus (CEM Corporation). Iodine vapor was used as a
detecting agent. The melting points were measured by means of
Dynalon Afon DMP100 apparatus (Dynalab Corp.) and reported without
correction. 1H and 13C nuclear magnetic
resonance (NMR) experiments were recorded (dissolving the sample in
0.5 ml od acetone-d6) on a 500 MHz Bruker Advance
III (Bruker Corporation) with a pulse field gradient at 500 MHz for
1H and 125 MHz for 13C. Chemical shifts are
given in values of ppm, referenced to tetramethylsilane as an
internal standard. The coupling patterns are expressed as singulete
(s), doublet (d), or a combination of the two.
Fourier-transform infrared spectroscopy (FT-IR) was performed using
a PerkinElmer 1320 (PerkinElmer, Inc.) with a sodium chloride
cell.
Synthesis of the DDS-derived compound. The
derivative DDS-13 was selected as a potential candidate from a
group of dapsone-derived compounds with different characteristics
and chemical properties (data not shown), which was synthesized by
our research group. To obtain DDS-13, an N-acylation
reaction was carried out using a procedure reported by Lidstrom
et al (3rd edition) (15).
In a 25 ml round flask containing a magnetic stir bar, DDS (1.2
mmol) was dissolved in 3 ml of acetone and Et3N (2.0
mmol) was added dropwise while stirring for 30 min at room
temperature. Then, methyl caprylate (0.08 mmol) was added. The
mixture was heated to 70˚C using 100 W of power for 5 h. The
solvent was removed using a rotary evaporator and the solid was
crystallized using a hexane:acetone (8:2) system. The reaction was
monitored using thin-layer chromatography on Merck silica gel 60
F254 plates (MilliporeSigma).
N,N'-(sulfonylbis(4,1-phenylene))dioctanamide
(DDS-13) resulted in an amorphous white solid with a 75% yield;
m.p. 158-160˚C. IR (υ, cm-1): 3233, 3060, 1912, 1626,
1587, 1435, 1307, 1274, 1136, 825. 1H-NMR
(acetone-d6, 500 MHz): δ: 7.77 (ddd,
J=8.75, 2.60, 1.9 Hz, 2H), 7.59 (ddd, J=8.75, 2.60,
1.90 Hz, 2H), 6.76 (ddd, J=8.8, 2.25, 0.45 Hz, 2H), 6.71
(ddd, J=8.9, 2.25, 1.15 HZ, 2H), 5.42 (w. s, 2H), 2.82 (w.
s, 20H), 2.79 (w. s, 6H), 1.26 (w. s, 4H). 13C-NMR
(acetone-d6, 125 MHz) δ: 168.7, 152.5, 145.6,
130.2, 129.5, 123.6, 78.3, 53.0, 51.0, 32.9, 29.3, 24.2, 13.6.
In silico prediction of physicochemical and
pharmacokinetic properties. Bioactivity and cheminformatics
prediction (including absorption, distribution, metabolism,
excretion, and toxicity, pharmacokinetic and medicinal chemistry
properties) were calculated using canonical simplified
molecular-input line-entry system sequences retrieved from the pdb
files of the density functional theory-optimized structures using
Avogadro software version 1.2.0 (https://avogadro.uptodown.com/windows). The chemical
space analysis was focused on four physicochemical properties of
pharmaceutical relevance, molecular weight, topological polar
surface area (TPSA), partition coefficient (cLogP) and solubility
Log S (ESOL), which were predicted using the SwissADME web tool
(http://www.swissadme.ch/index.php;
access date: 02 March 2023). Bioavailability radars and Lipinski's
(16), Ghose's (17), Veber's (18), Egan's (19) and Muegge's (20) rules were also calculated using
SwissADME.
Biology. Reagents
Stock solutions of DDS and its synthetic derivative
were prepared in dimethyl sulfoxide (DMSO) at a concentration of 1
mg/ml, then stored at -20˚C. The final concentrations of DMSO were
below 0.1% (v/v) for all experiments. The reagent ethanol
(MilliporeSigma) was included as a deathtime control using
concentrations ranging from 4-13% (v/v).
Cell cultures and growth conditions. The
human metastatic prostate carcinoma (DU145) and the human
adenocarcinoma cervix (HeLa) cell lines were obtained from American
Type Culture Collection with the following registration numbers:
HTB-81 and CRM-CCL-2, respectively. These were grown in an adherent
monolayer culture in Dulbecco's Minimum Essential Medium (DMEM) and
both were supplemented with 10% heat-inactivated fetal bovine serum
(FBS), 1% L-glutamine and 1% penicillin/streptomycin in a
humidified atmosphere (5% CO2; 37˚C). All media and
supplements were purchased from MilliporeSigma. The primary dermal
fibroblast cell line-HDFa was obtained from ATCC with the
registration number PCS-201-012 and it was used to validate the
cytotoxicity results using concentrations ranging from 12.5-100
µM.
Cell viability assay.
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT;
Invitrogen; Thermo Fisher Scientific, Inc.) was used to measure the
cytotoxicity of the tested compounds. Briefly, the cells were
seeded in 96-well plates (20,000 cells/well). Following overnight
incubation at 37˚C, the cells were treated with or without the
tested compounds (at different concentrations ranging from 0.01-100
µM). Untreated cells containing fresh medium were used as lifetime
controls and fresh medium alone was used as a blank. Following the
24- and 48-h treatments, the cells were incubated with MTT at a
final concentration of 0.5 mg/ml for 2.5 h in 5% CO2 at
37˚C. Finally, a solution of 100% DMSO (50 µl) was added to
solubilize the purple formazan. The absorbance of the converted dye
was measured the next day at 570 nm using a spectrophotometer
(Smartreader 96; Accuris Instruments). MTT data are expressed as
the mean ± SD of at least three independent experiments
(triplicates). The absorption readings were converted into percent
of cells. The IC50 values representing the
concentrations (µM) of the tested compounds reducing the cell
viability by 50%, were calculated using an IC50
calculator, AAT Bioquest (https://www.aatbio.com/tools/ic50-calculator).
Morphological evaluation of cell cultures.
Papanicolaou's stain was used to morphologically evaluate the
possible type of cell death induced by each of the treatments (DDS
and DDS-13) in the different cell lines (HDFa, DU145 and HeLa).
Untreated cells were used as controls and cells treated with DDS
and DDS-13 at concentrations of 0.01 and 100 µM were assessed. A
total of 20,000 cells per well were plated on Chamber Slide devices
(Nunc Lab-Tek II, Thermo Fisher Scientific, Inc.) and incubated at
37˚C for 48 h. The cells were then fixed in 96% ethanol and stained
with Papanicolaou according to a modified procedure (21): Cells were stained with hematoxylin
(MilliporeSigma) for 2 min, followed by two slow dips under tap
water, a slow dip under 1% ammoniacal water and two slow dips under
tap water, and then stained with OG-6 (MilliporeSigma) for 2 min
and with EA-50 (Merck KGaA) for 2 min, followed by a slow dip under
96% ethanol and another under 100% ethanol. The samples were
cleared in xylene (MilliporeSigma) and mounted with rapid mounting
medium (Entellan; MilliporeSigma). These were observed under a
light microscope (Primo Star; Zeiss AG) and analyzed by a
specialized pathologist.
Statistical analysis
The comparison of the means was performed using
Student's t-test and a one-way ANOVA (with Bonferroni's post-hoc
test) with Sigma Plot v12.5 (Systat Software Inc.) and GraphPad
Prism (GraphPad Software; Dotmatics). Data are presented as the
mean ± standard deviations. P<0.05 was considered to indicate a
statistically significant difference.
Results
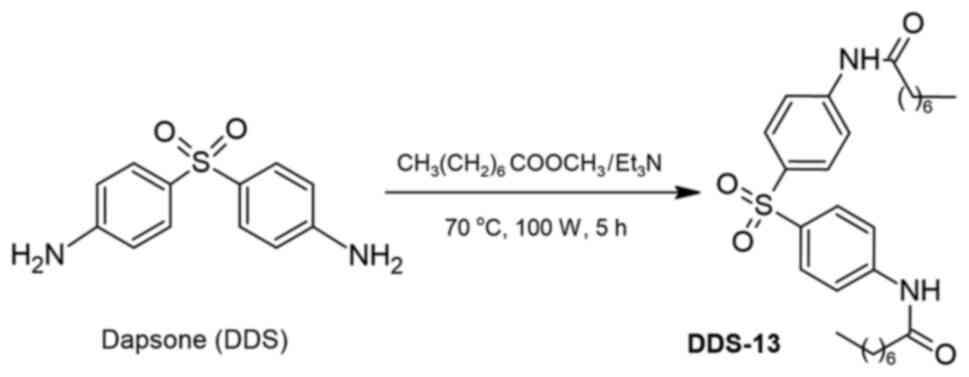
Chemistry. Chemical synthesis
DDS-13 was obtained through the condensation of DDS
and methyl caprylate, using a combination of triethylamine
(Et3N) and acetone as the solvent, with reaction times
of up to 5 h under microwave irradiation. The compound was obtained
as a white solid with a 75% yield. The derivative structure was
confirmed through NMR and FT-IR (Fig.
S3, Fig. S4 and Fig. S5). Fig. 1 shows the chemical structures of
the obtained compounds.
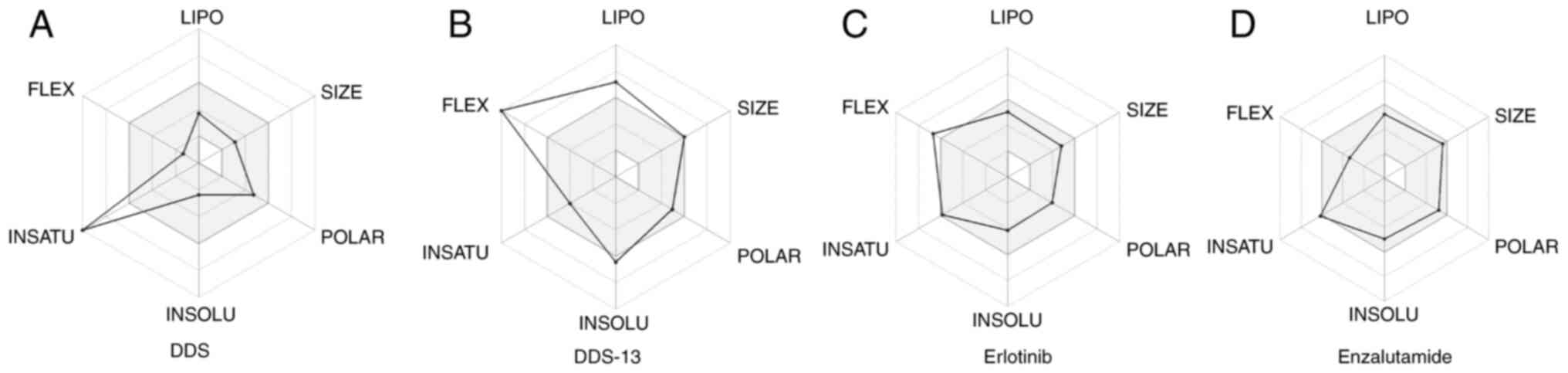
In silico analysis. The SwissADME web tool
(22) was used as a prediction
model for the identification of the physicochemical and
pharmacokinetic properties of DDS-13 (see details in the Methods
section). The bioavailability radars for DDS (Fig. 2A) and the reference drugs erlotinib
(Fig. 2C) and enzalutamide
(Fig. 2D) were shown to be outside
the optimal ranges for one physicochemical property: DDS and
enzalutamide in saturation and erlotinib in flexibility. The
synthetic derivative DDS-13 (Fig.
2B) was shown to be outside of the optimal ranges for three
physicochemical properties: lipophilicity, solubility and
flexibility. Table I shows the
structural and physicochemical properties, where only the DDS-13
derivative slightly exceeded the molecular weight limits (>500
g/mol) according to the reference established by the prediction
model. All compounds possessed an adequate TPSA (<130
Å2) for membrane permeation. As for the ESOL, it was
established that the reference and DDS drugs showed improved
solubility than DDS-13.
 | Table IStructural and physicochemical
properties of DDS, DDS-13, erlotinib and enzalutamide
compounds. |
Table I
Structural and physicochemical
properties of DDS, DDS-13, erlotinib and enzalutamide
compounds.
| | Log
Po/w | |
Drug-likenessa | |
|---|
| Compound | Molecular weight,
g/mol | TPSA
Å2 | WLOGP | MLOGP | Log S (ESOL) | HBAs | HBDs | Rotatable
bonds | Lipinski | Ghose | Veber | Egan | Muegge | Bioavailability
score |
|---|
| DDS | 248.3 | 94.56 | 0.97 | 1.87 | -2.38 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0.55 |
| DDS-13 | 500.69 | 100.72 | 7.06 | 4.55 | -6.46 | 4 | 2 | 18 | 2 | 4 | 1 | 1 | 2 | 0.17 |
| Erlotinib | 393.44 | 74.73 | 3.31 | 1.48 | -4.11 | 6 | 1 | 10 | 0 | 0 | 0 | 0 | 0 | 0.55 |
| Enzalutamide | 464.44 | 108.53 | 3.61 | 2.73 | -4.94 | 7 | 1 | 5 | 0 | 0 | 0 | 0 | 0 | 0.55 |
Among the pharmacokinetic properties (Table II), it was observed that the
octanol/water partition coefficient (cLogPo/w or WLOGP),
as considered by Egan, or the Moriguchi octanol-water partition
coefficient, as considered by Lipinski, demonstrated that the
reference and DDS drugs may have exhibited improved
gastrointestinal (GI) absorption than the DDS-13 derivative.
Erlotinib is the only reference drug with permeability to the
blood-brain barrier (BBB).
 | Table IIPharmacokinetic properties and
medicinal chemistry of DDS, DDS-13, Erlotinib and Enzalutamide
compounds. |
Table II
Pharmacokinetic properties and
medicinal chemistry of DDS, DDS-13, Erlotinib and Enzalutamide
compounds.
| |
Pharmacokinetics | Medicinal
chemistry |
|---|
| Compound | GI absorption | BBB permeant | P-gp substrate | CY1A2
inhibitor | CYP2C19
inhibitor | CYP2C9
inhibitor | CYP2D6
inhibitor | CYP3A4
inhibitor | PAINS | Brenk | Lead-likeness |
|---|
| DDS | High | No | No | No | No | No | No | No | 0 | 1 | 1 |
| DDS-13 | Low | No | No | No | Yes | Yes | No | Yes | 0 | 0 | 3 |
| Erlotinib | High | Yes | No | Yes | Yes | Yes | Yes | Yes | 0 | 1 | 2 |
| Enzalutamide | High | No | No | No | Yes | Yes | No | Yes | 0 | 1 | 2 |
Biology. In vitro analysis
For the evaluation of the cytotoxic effects of DDS
and its synthetic derivative DDS-13, the experimental study was
performed on cancer cell lines of solid prostate (DU145) and
cervical (HeLa) tumors. In the first stage, to evaluate whether
there were differences between the durations of exposition to the
treatment, DU145 and HeLa cells were exposed to 0.01, 0.1, 1, 10
and 100 µM of DDS (T) and the cell viability was determined at 24
and 48 h. To determine the percentage of cell viability, the
optical density (OD), a lifetime control (CNT) and a blank (B) were
used. The formula of cell viability
(%)=(ODT-ODB)/(ODCNT-ODB)
x100 was used for the determination. Table III shows the comparison of the
cell viability percentage with DDS at various concentrations at the
24- and 48-h time points. There were no significant differences in
the different concentrations between the two time points
(P>0.05), except for the 100 µM concentration (P=0.03). In
general, the highest cytotoxic effect was observed at 48 h. Based
on these first results, subsequent analyses were performed to
evaluate the different concentrations of each compound at only at
the 48-h time point.
 | Table IIIAnalysis of the cytotoxic
concentrations between the time points of 24 and 48 h with the DDS
compound in DU145 and HeLa cell lines. |
Table III
Analysis of the cytotoxic
concentrations between the time points of 24 and 48 h with the DDS
compound in DU145 and HeLa cell lines.
| | Cell viability for
different concentrations of DDS, % | |
|---|
| Cell line | Time (h) | 0.01 µM | 0.1 µM | 1 µM | 10 µM | 100 µM | P-value |
|---|
| DU145 | 24 | 93.4±4.9 | 70.3±3.3 | 86.3±5.0 | 72.8±3.7 | 60±2.9 | 0.002a |
| | 48 | 110.4±3.3 | 77.7±6.5 | 106.3±6.6 | 83.0±7.6 | 59.1±4.8 | 0.002a |
| | | P=0.057 | P=0.29 | P=0.078 | P=0.234 | P=0.843 | |
| HeLa | 24 | 95.4±3.3 | 78.2±3.6 | 98.3±6.6 | 81.0±4.8 | 68.9±2.9 | 0.005a |
| | 48 | 103.0±3.5 | 69.0±6.5 | 93.8±6.5 | 74.3±7.9 | 34.5±8.0 |
<0.001a |
| | | P=0.16 | P=0.224 | P=0.564 | P=0.414 | P=0.03a | |
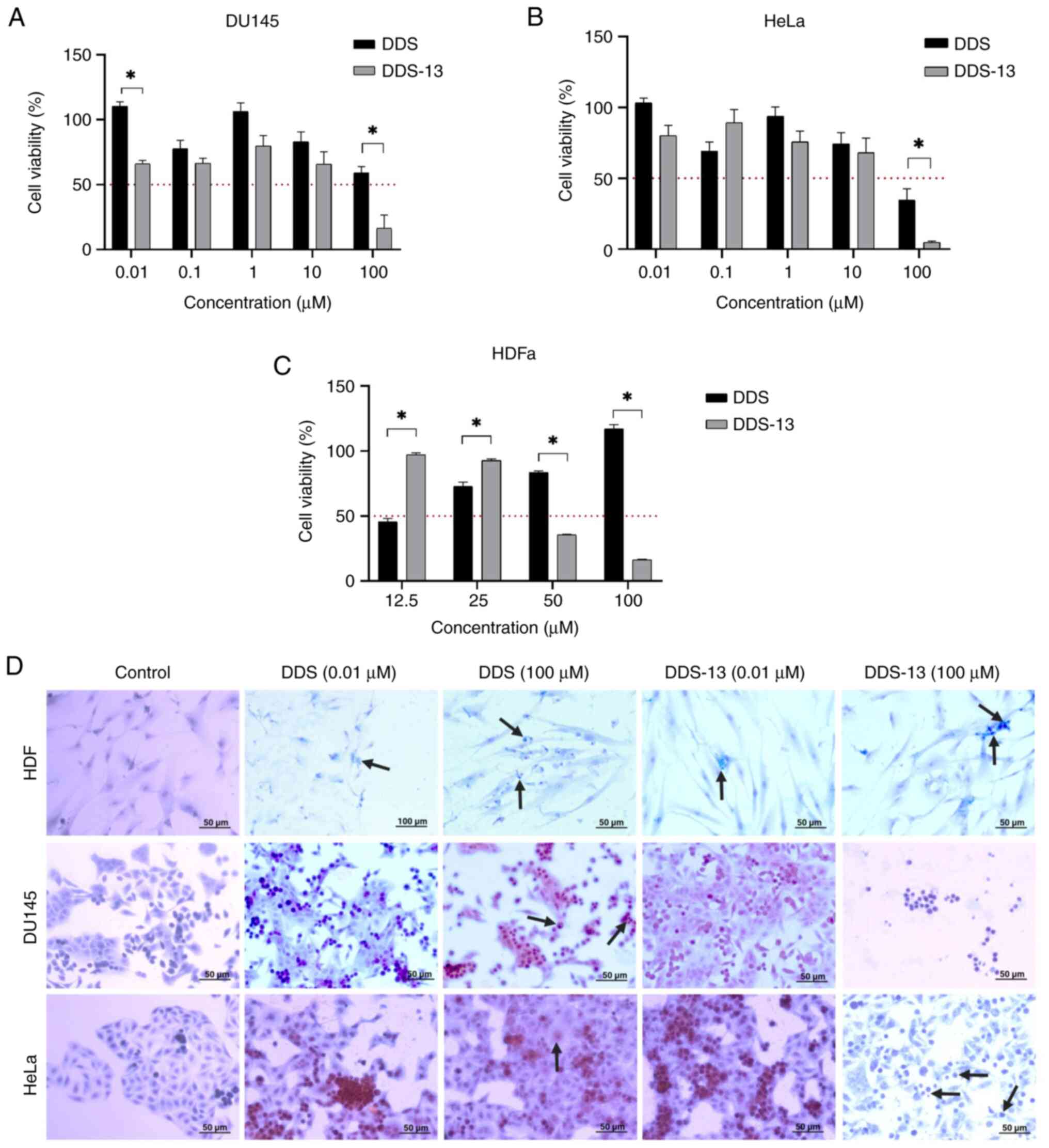
Table IV shows a
comparison of the cell viability percentages of the different
concentrations (0.01-100 µM) for both DDS and DDS-13, in DU145 and
HeLa cell lines at the 48-h time point. A comparison of the
different concentrations of each compound showed significant
differences in the two cell lines used (P<0.05). In the DU145
cell line, DDS-13 reduced the cell viability percentage, unlike the
DDS, at the following concentrations: 0.01 µM (44.2%), 0.1 µM
(11.2%), 1 µM (26.5%), 10 µM (17.3%) and 100 µM (42.6%). There were
significant differences between DDS and DDS-13 (Fig. 3A) at the concentrations of 0.01 µM
(P=0.005) and 100 µM (P=0.003). The mean inhibitory concentration
(IC50) is also highlighted in Table IV and was calculated at 11.11 for
DDS and 19.06 µM for DDS-13. In the HeLa cell line, the rates of
reduction in the cell viability percentage at the different
concentrations of DDS-13 were as follows: 0.01 µM (23%), 1 µM
(18.1%), 10 µM (6.2%) and 100 µM (29.7%). At the 0.1 µM
concentration, there was no reduction in the cell viability
percentage. A significant difference between DDS and DDS-13
(Fig. 3B) at a concentration of
100 µM was also observed (P=0.035). The IC50 for DDS was
13.07 µM and that for DDS-13 was 67.91 µM. Overall, the greatest
decrease in cell viability percentage for both DDS and DDS-13 was
observed at 100 µM in both cell lines.
 | Table IVConcentration analysis of DDS and
DDS-13 compounds in DU145 and HeLa cell lines at the 48-h time
point. |
Table IV
Concentration analysis of DDS and
DDS-13 compounds in DU145 and HeLa cell lines at the 48-h time
point.
| | Cell viability for
different concentrations of DDS, % | |
|---|
| Cell line | Treatment | 0.01 µM | 0.1 µM | 1 µM | 10 µM | 100 µM | P-value | IC50
(µM) |
|---|
| DU145 | DDS | 110.4±3.3 | 77.7±6.5 | 106.3±6.6 | 83.0±7.6 | 59.1±4.8 | 0.002a | 11.11 |
| | DDS-13 | 66.2±2.5 | 66.5±3.8 | 79.8±8.0 | 65.7±9.6 | 16.5±10.1 | 0.002a | 19.06 |
| | |
P=0.005a | P=0.171 | P=0.070 | P=0.185 |
P=0.033a | | |
| HeLa | DDS | 103.0±3.5 | 69.0±6.5 | 93.8±6.5 | 74.3±7.9 | 34.5±8.0 |
<0.001a | 13.07 |
| | DDS-13 | 80.0±7.3 | 89.2±9.1 | 75.7±7.6 | 68.1±10.1 | 4.8±0.8 |
<0.001a | 67.91 |
| | | P=0.058 | P=0.127 | P=0.125 | P=0.567 |
P=0.035a | | |
To evaluate the cytotoxicity of the compounds of
interest (DDS and DDS-13) on non-cancerous cells, the primary
dermal fibroblast cell line (HDFa) was used due to its availability
in the Molecular Medicine Laboratory (Autonomous University of
Zacatecas, Zacatecas, Mexico). The studied concentrations included
concentrations below and above the IC50 calculated
previously for each cancer cell line. These were 12.5, 25, 50 and
100 µM. Fig. 3C shows the results
obtained for the cell viability percentage with each of the
compounds in the HDFa cell line. It was observed that there was
cytotoxicity with DDS-13 at concentrations of 50 µM (reduction of
64.2% in cell viability) and 100 µM (reduction of 83.6% in cell
viability). It was observed that there was no cytotoxicity with DDS
at most concentrations, except for 12.5 µM (a reduction of 54.4% in
cell viability). There were significant differences between DDS and
DDS-13 at all tested concentrations, but mostly at concentrations
of 50 and 100 µM (P<0.001). The IC50 for DDS-13 was
40.92 µM.
Papanicolaou staining was used to assess the type of
cell death in cells treated with DDS and DDS-13. No cell death was
observed in untreated cells, as opposed to in treated cells
(Fig. 3D). In cancer cells (DU145
and HeLa) treated with DDS (0.01 and 100 µM), hyperchromatic nuclei
with sparse dense cytoplasm were observed, suggesting cell death by
apoptosis. The process was more evident at higher concentrations.
The same effect occurred with cancer cells treated with DDS-13,
where the foci of cell death by apoptosis were greater and the cell
density was considerably lower, specifically at the 100 µM
concentration. In non-cancerous cells treated with DDS and DDS-13,
some foci of cell death by apoptosis were also observed in a
smaller proportion; however, cell density did not decrease with any
of the treatments.
Discussion
Globally, cancer represents a major health problem
due to its high mortality rate (3). In terms of drug discovery, drug
repositioning has gained increasing importance because it helps to
circumvent preclinical optimization (23). The present study focused on
evaluating DDS and its synthetic derivative, DDS-13, in an in
vitro study to contribute to the proposal of candidate
treatments with potential cytotoxic effects on cancer cells. To
date, there is little information on the effects of DDS and its
synthetic derivatives on cancer. DDS is chemically known as
4,4'-diaminodiphenylsulfone; it is an old antibiotic drug that
belongs to the group of synthetic sulfones (24). Due to its side effects, namely,
methemoglobinemia and hemolytic anemia, DDS is mainly used in
topical preparations for the treatment of dermatological diseases
(7). One strategy for the
structural modification of drugs containing amine functionalities,
as is the case for DDS, consists of derivatization to imines or
amides. From a synthetic point of view, the imine group has the
advantage of being easily accessible, which can improve biological
activity and solubility compared with precursor amines (25,26).
In the present study, DDS-13 was selected from a group of synthetic
derivatives of DDS obtained by our working group. This derivative
has not been functionally or biologically tested to evaluate its
potential pharmacological properties against cancer. DDS and its
synthetic derivative DDS-13 were evaluated in silico, and
they were compared with two reference drugs approved by the US Food
and Drug Administration (FDA): Erlotinib and enzalutamide, which
have antineoplastic activities in cervical (27) and prostate cancer (28), the two types of cancer evaluated in
the present study. In the results of the in silico analysis,
it was observed that DDS-13 had more physicochemical properties out
of range than DDS and the reference drugs (Table I). Erlotinib and DDS-13 were shown
to be outside of the optimal ranges, with rotatable bonds greater
than nine in the flexibility property and with DDS and enzalutamide
in the saturation property. Other properties of DDS-13 which were
found to be out of range were lipophilicity (WLOGP=7.06) and
solubility (Log S=-6.46). Drug likeness qualitatively assesses the
likelihood of a molecule becoming an oral drug with respect to its
bioavailability. This section gives access to five different
rule-based filters (Lipinski, Ghose, Veber, Egan and Muegge) with
different ranges of properties that define a molecule as drug-like.
DDS-13 exhibited violations in these filters, unlike DDS or the
reference drugs. The present study studied the pharmacokinetic
properties and DDS-13 and none of the studied molecules crossed the
BBB, except for erlotinib (Table
II). In medicinal chemistry, the Brenk filters helped to define
the lead-likeness criteria in order to establish whether a molecule
was suitable for optimization. The present study observed that all
compounds presented violations in at least one of the filters,
which was more evident with DDS-13. The predictions for BBB
permeation and passive human gastrointestinal absorption consisted
of the readout of the BOILED-Egg model (29) (Fig.
S1). It was observed that DDS-13 demonstrated less
bioavailability by oral absorption than the other compounds. DDS
had higher bioavailability by gastrointestinal absorption than the
reference drug enzalutamide. Erlotinib, enzalutamide and DDS are
classified as class II drugs according to the BCS, with low
solubility and high permeability (12). However, these rules of thumb only
consider a passive diffusion mechanism through the GI barrier;
therefore, the limitations of our derivative can be solved by a
different administration route, through formulation or by
considering an ATP-dependent transport.
In the in vitro model, the cytotoxic effects
of DDS and DDS-13 were demonstrated at concentrations of 10 and 100
µM in the DU145 and HeLa cell lines, with the greatest cytotoxic
effect observed at a concentration of 100 µM (cell viability
reduction of >50%). The synthetic derivative DDS-13 showed
greater cytotoxic effects than DDS in both the DU145 (3.5x
reduction in cell viability) and HeLa (7x reduction in cell
viability) cell lines (P<0.05). In the HeLa cell line, the
cytotoxic effect was more pronounced. This correlated with the
result seen with Papanicolaou staining, where morphological cell
death at the 100 µM concentration was higher and cell density was
lower (Fig. 3D). Then, four
concentrations (12.5-100 µM) above the IC50
concentrations previously seen in cancer cell lines were included
to evaluate the cytotoxicity on a non-cancerous cell line (HDFa).
The results indicated that DDS-13 had no cytotoxic effect on this
cell line in a concentration range from 12.5 to 25 µM
(IC50=40.92 µM). The IC50 concentration for
HDFa cells was >IC50 concentration seen in the DU145
cell line (19.06 µM). These results suggested that DDS-13 appeared
to be a good candidate for additional assays due to its cytotoxic
effect only on the DU145 cell line and not on primary fibroblasts
within the aforementioned range of concentrations. A limitation of
the present study was that it did not complement the cytotoxic
effect of DDS-13 on DU145 and HeLa cells in the concentration range
of 12.5-25 µM; however, these evaluations can be integrated into
further studies. The significant killing of cancer cells by DDS-13
was observed at a concentration of 100 µM; at this concentration,
the survival of non-cancerous cells was similar to that of
cancerous cells (DU145 cells). The same was observed
morphologically by Papanicolaou staining (Fig. 3D) and cell death at this
concentration was higher.
Therefore, it may be pertinent to study cell
survival by considering a wider range of concentrations (10-100 µM)
in both cancerous and non-cancerous cells to determine whether
there is a concentration range that is more cytotoxic to cancer
cell than non-cancer cell lines. Regarding DDS, the IC50
calculated in the HeLa cell line (13.07 µM) was lower than the
IC50 concentration observed in the HDFa cells. The high
DDS cytotoxic effect observed on HeLa cells (Fig. 3B) positions DDS as an improved
candidate compared with DDS-13 for preclinical studies of cervical
cancer, because it had no cytotoxic effect on HDFa cells in a range
of concentrations from 25-100 µM. Similarly, for prostate cancer,
DDS showed an IC50 of 11.11 µM in the DU145 cell line,
which is well below the concentrations tested as non-cytotoxic for
HDFa (25, 50 and 100 µM). These results may be considered as a
basis on which to increase the DDS concentrations to 100 µM, with
the object of evaluating whether its specific cytotoxic effect on
prostate tumor cells would be greater. In HDFa cells, DDS-13 showed
a safety margin in the normal HDFa cells only between 12.5-50 µM,
compared with the dose-dependent selectivity of DDS. However,
morphologically, it is important to stress that with both DDS and
DDS-13, cell density was not significantly reduced, as was observed
in cancer cell lines (Fig. 3D).
The antitumor effects of DDS and/or DDS-13 are not well known. A
study conducted in 2016 by Boccellino et al (9) highlighted that DDS could present an
antitumor effect by blocking IL8 and reducing growth factors, such
as the VEGF, in an in vitro model; however, this mechanism
has not been proved. Regarding synthetic DDS derivatives, three
studies have been conducted, one of them by Karpel-Massler et
al (2017) (11), which
highlights the reduction in anchorage-independent growth, the
decrease in clonogenic survival and the reduction of directed
migration in a glioblastoma cell line. The derivatives evaluated in
that study were different from those evaluated in the present
study. The 2017 study (11)
suggested possible effects of DDS in cancer; however, it did not
demonstrate these mechanisms. The concentrations evaluated in this
previous study were similar to those evaluated in the present
study. Pillai et al (30)
evaluated synthetic DDS derivatives different from those in the
present study, as well as their in vitro anticancer activity
against the Hep G2 (hepatocellular carcinoma) and C6 (glioblastoma)
cell lines, suggesting specificity of the compounds for cancer
cells over normal liver cells. They proposed apoptotic cell death
as a mechanism of cytotoxic action for their derivatives. The
present study decided to include Papanicolaou staining to
morphologically compare cells with DDS and DDS-13 (0.01 and 100
µM); the findings indicated that the likely mechanism of cell death
is given by apoptosis due to specific features, such as shrinkage
of the nuclei, sparse dense cytoplasm, hyperchromatic nuclei and
signs of pre-apoptotic bodies. These results need to be validated
with additional studies.
In vivo studies have shown that inhibition of
CYP2C19, CYP2C9 and CYP3A4 isoenzymes, as seen in the present in
silico analysis with DDS-13, is one major cause of
pharmacokinetic-related drug-drug interactions (31). These lead to various adverse
effects, such as toxicity due to decreased clearance and
accumulation of the drug or its metabolites. These cytochromes have
been reported to be differentially expressed in types of cancer
(32,33). Additional studies will be needed in
order to confirm the DDS-13 effect of these isoenzymes. Another
study by Guzmán-Ávila et al (34) showed that the evaluated synthetic
derivatives demonstrated antioxidant activity in an in
silico model. Synthetic derivatives are different from the one
evaluated in the present study. Regarding analyses of the structure
of DDS-13, there are only two early studies, which reported
similar, but not the same, structural characteristics of the
compound synthesis and these did not address anything about their
possible effects (35,36). In the same manner, this synthetic
derivative has not been evaluated in cancer. Therefore, DDS-13 has
not previously been synthesized as it was in the present study, nor
has it been biologically evaluated. From the results of the present
study, cytotoxic effects of DDS and DDS-13 were demonstrated on
DU145 and HeLa cell lines, supporting the antitumor properties of
these molecules specifically for prostate or cervical tumors. In
accordance with the differential effects which were identified, it
is highly probable that the chemical structures of each of them are
involved in their different mechanisms of action.
Finally, is important to note that the present study
observed a non-linear trend at low concentrations (0.01 and 0.1 µM)
of DDS and DDS-13 in both cancer cell lines which were evaluated.
These trends were contrary to those observed from the 1 µM
concentration level and above. In principle, this finding would
rule out these concentrations for the evaluation of the cytotoxic
effect; however, since it was a reproducible finding in both cell
lines, with both compounds and during all the experiments,
additional viability assays were performed in which ethanol
dilutions (4-13 µM) were included for quality control of the
cytotoxic assays. However, in future studies it would be desirable
to include chemotherapeutic drugs, such as enzalutamide, as a
cytotoxicity control for comparative purpose. On the three cell
lines which were used, a dose-dependent cytotoxic effect was
observed with ethanol (Fig. S2).
This effect was different from that observed with DDS-13 and DDS in
the cancer cell lines. Exactly what occurs at these concentrations
in the cancer cell lines included in the present study is unclear,
but different mechanisms of action are probably triggered due to
the chemical and physicochemical properties of each compound.
Additional studies will be needed in order to identify whether the
effect observed in our study corresponds to dual effects or
mechanisms of DDS and DDS-13 at low concentrations, or even these
effects are maintained with other DDS derivatives.
In conclusion, DDS and its synthetic derivative
DDS-13 showed cytotoxic effects in in vitro models of
prostate and cervical cancer. DDS-13 showed cytotoxic effects in
the DU145 cell line, proving to be a good candidate for prostate
cancer, with no cytotoxic effect in non-cancerous cells. DDS showed
a cytotoxic effect in both the DU145 and HeLa cell lines, proving
to be a good candidate for both prostate and cervical cancer. The
present study demonstrated improved results in cervical cancer
cells, without a cytotoxic effect on non-cancerous cells. DDS-13
presented different pharmacokinetic properties compared with DDS,
making it a new and interesting candidate for evaluation in
preclinical models of cancer treatment. The proposal of this
synthetic derivative could contribute to the discovery of new
cancer treatments to counteract the adverse effects and costs of
current treatment schemes. Further in vitro and in
vivo studies are needed in order to elucidate a possible
mechanism of action and to validate the antitumor effect.
Supplementary Material
BOILED-Egg model for the DDS, DDS-13,
Erlotinib and Enzalutamide compounds. DDS, dapsone.
Control of cytotoxicity in DU145, HeLa
and HDFa cell lines. *P<0.05.
Fourier-transform infrared
spectroscopy of dapsone-13.
1H-nuclear magnetic
resonance dapsone-13.
13C-nuclear magnetic
resonance dapsone-13.
Acknowledgements
Not applicable.
Funding
Funding: The present study was funded by the Academic Unit of
Human Medicine and Health Sciences of the Autonomous University of
Zacatecas and by CONACYT via a scholarship fund (grant no.
2021-000018-02NACF-15274).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
MMF and VF designed the study. GC, IG, VF, RM, MD
and MMV performed the experiments and analyzed the data. ID and IR
contributed substantially to the data interpretation and
participated in critical manuscript revision. GC, VF, IG, MMF wrote
the manuscript. GC, MMF, MC, ID and IR searched the literature and
revised the manuscript. All authors read and approved the final
manuscript. MMF and VF confirm the authenticity of all the raw
data.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Catherine Sánchez N: Knowing and
understanding the cancer cell: physiopathology of cancer. Rev Méd
Clin Las Condes. 24:553–562. 2013.
|
|
2
|
World Health Organization (WHO):
International Agency for Research on Cancer. WHO, Geneva, 2020.
https://gco.iarc.fr/today/online-analysis-multi-bars.
|
|
3
|
Ghose S, Radhakrishnan V and Bhattacharya
S: Ethics of cancer care: Beyond biology and medicine.
Ecancermedicalscience. 13(911)2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Jarada TN, Rokne JG and Alhajj R: A review
of computational drug repositioning: Strategies, approaches,
opportunities, challenges, and directions. J Cheminform.
12(46)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ross CM: The treatment of acne vulgaris
with dapsone. Br J Dermatol. 73:367–370. 1961.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Reunala T, Hervonen K and Salmi T:
Dermatitis herpetiformis: An update on diagnosis and management. Am
J Clin Dermatol. 22:329–338. 2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Wozel G and Blasum C: Dapsone in
dermatology and beyond. Arch Dermatol Res. 306:103–124.
2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Molinelli E, Paolinelli M, Campanati A,
Brisigotti V and Offidani A: Metabolic, pharmacokinetic, and
toxicological issues surrounding dapsone. Expert Opin Drug Metab
Toxicol. 15:367–379. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Boccellino M, Quagliuolo L, Alaia C,
Grimaldi A, Addeo R, Nicoletti GF, Kast RE and Caraglia M: The
strange connection between epidermal growth factor receptor
tyrosine kinase inhibitors and dapsone: From rash mitigation to the
increase in anti-tumor activity. Curr Med Res Opin. 32:1839–1848.
2016.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kanoh S, Tanabe T and Rubin BK: Dapsone
inhibits IL-8 secretion from human bronchial epithelial cells
stimulated with lipopolysaccharide and resolves airway inflammation
in the ferret. Chest. 140:980–990. 2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Karpel-Massler G, Kast RE, Siegelin MD,
Dwucet A, Schneider E, Westhoff MA, Wirtz CR, Chen XY, Halatsch ME
and Bolm C: Anti-glioma activity of dapsone and its enhancement by
synthetic chemical modification. Neurochemical Res. 42:3382–3389.
2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lindenberg M, Kopp S and Dressman JB:
Classification of orally administered drugs on the World Health
Organization model list of essential medicines according to the
biopharmaceutics classification system. Eur J Pharm Biopharm.
58:265–278. 2004.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Gallardo CA, Fan BE, Lim KGE and Kuperan
P: Chronic dapsone use causing methemoglobinemia with oxidative
hemolysis and dyserythropoiesis. Am J Hematol. 96:1715–1716.
2021.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Vogel AI, Furniss BS, Hannaford AJ, Smith
PW and Tatchell AR: Vogel's textbook of practical organic
chemistry. 5th edition. John Wiley & Sons, New York, NY,
pp395-469, 1989.
|
|
15
|
Lidstrom P, Tierney J, Wathey B and
Westman J: Microwave assisted organic synthesis-a review.
Tetrahedron. 57:9225–9283. 2001.
|
|
16
|
Lipinski CA, Lombardo F, Dominy BW and
Feeney PJ: Experimental and computational approaches to estimate
solubility and permeability in drug discovery and development
settings. Adv Drug Deliv Rev. 46:3–26. 2001.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Ghose AK, Viswanadhan VN and Wendoloski
JJ: A knowledge-based approach in designing combinatorial or
medicinal chemistry libraries for drug discovery. 1. A qualitative
and quantitative characterization of known drug databases. J Comb
Chem. 1:55–68. 1999.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Veber DF, Johnson SR, Cheng HY, Smith BR,
Ward KW and Kopple KD: Molecular properties that influence the oral
bioavailability of drug candidates. J Med Chem. 45:2615–2623.
2002.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Egan WJ, Merz KM Jr and Baldwin JJ:
Prediction of drug absorption using multivariate statistics. J Med
Chem. 43:3867–3877. 2000.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Muegge I, Heald SL and Brittelli D: Simple
selection criteria for drug-like chemical matter. J Med Chem.
44:1841–1846. 2001.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Sathawane P, Kamal MM, Deotale PR and
Mankar H: Nuances of the Papanicolaou stain. Cytojournal.
19(43)2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Swiss Institute of Bioinformatics (SIB):
SwissADME. http://www.swissadme.ch/index.php#.
|
|
23
|
March-Vila E, Pinzi L, Sturm N, Tinivella
A, Engkvist O, Chen H and Rastelli G: On the integration of in
silico drug design methods for drug repurposing. Front Pharmacol.
8(298)2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
do Amaral LH, do Carmo FA, Amaro MI, de
Sousa VP, da Silva L, de Almeida GS, Rodrigues CR, Healy AM and
Cabral LM: Development and characterization of dapsone cocrystal
prepared by scalable production methods. AAPS PharmSciTech.
19:2687–2699. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Jornada DH, dos Santos Fernandes GF, Chiba
DE, de Melo TR, dos Santos JL and Chung MC: The prodrug approach: A
successful tool for improving drug solubility. Molecules.
21(42)2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Day TP, Sil D, Shukla NM, Anbanandam A,
Day VW and David SA: Imbuing aqueous solubility to amphotericin B
and nystatin with a vitamin. Mol Pharm. 8:297–301. 2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Schilder RJ, Sill MW, Lee YC and Mannel R:
A phase II trial of erlotinib in recurrent squamous cell carcinoma
of the cervix: A gynecologic oncology group study. Int J Gynecol
Cancer. 19:929–933. 2009.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Davis ID, Martin AJ, Stockler MR, Begbie
S, Chi KN, Chowdhury S, Coskinas X, Frydenberg M, Hague WE, Horvath
LG, et al: Enzalutamide with standard first-line therapy in
metastatic prostate cancer. N Engl J Med. 381:121–131.
2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Daina A and Zoete V: A BOILED-Egg to
predict gastrointestinal absorption and brain penetration of small
molecules. ChemMedChem. 11:1117–1121. 2016.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Pillai V, Kadu R, Buch L and Singh VK:
Derivatives of dapsone (dap): Synthesis and study on in vitro
anticancer activity and DNA laddering against Hep G2 and C6 human
cancer cell lines. ChemistrySelect. 2:4382–4391. 2017.
|
|
31
|
Huang SM, Strong JM, Zhang L, Reynolds KS,
Nallani S, Temple R, Abraham S, Habet SA, Baweja RK, Burckart GJ,
et al: New era in drug interaction evaluation: US food and drug
administration update on CYP enzymes, transporters, and the
guidance process. J Clin Pharmacol. 48:662–670. 2008.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Uetrecht J, Zahid N, Shear NH and Biggar
WD: Metabolism of dapsone to a hydroxylamine by human neutrophils
and mononuclear cells. J Pharmacol Exp Ther. 245:274–279.
1988.PubMed/NCBI
|
|
33
|
Tian D and Hu Z: CYP3A4-mediated
pharmacokinetic interactions in cancer therapy. Curr Drug Metab.
15:808–817. 2014.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Guzmán-Ávila R, Avelar M, Márquez EA,
Rivera-Leyva JC, Mora JR, Flores-Morales V and Rivera-Islas J:
Synthesis, in vitro, and in silico analysis of the antioxidative
activity of dapsone imine derivatives. Molecules.
26(5747)2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Zasosov VA: Diacyl derivatives of bis
(4-aminophenyl) sulfone. Zhurnal Obshchei Khimii. 17:471–476.
1947.
|
|
36
|
Hensel; Walter; Buechner O, inventor
Polyolefin molding compositions containing diamides, 1967.
|