Introduction
Cancer patients have a high incidence of
thromboembolism (1). Thrombosis
associated with cancer or cancer therapy is collectively referred
to as ‘cancer-associated thrombosis (CAT)’ (1). CAT includes venous thromboembolism
(VTE), arterial thromboembolism, nonbacterial thrombotic
endocarditis (2-4),
and disseminated intravascular coagulation. Among CAT, VTE is most
common and includes deep vein thrombosis and pulmonary embolism.
The development of CAT can be triggered by immune-related adverse
events of immune checkpoint inhibitor (ICI), which has brought
about a major revolution in cancer treatment in recent years
(5-9).
Regardless of the path of onset, the presence of CAT complicates
subsequent cancer treatment because it worsens the patient's
general condition and dysfunction of important organs. As a result,
long-term survival may be thwarted. For the treatment of CAT, low
molecular heparin and direct oral anticoagulants (DOACs), which
selectively inhibit thrombin or blood coagulation factor Xa (FXa),
have proven useful (10-12).
We show herein a case of metastatic lung
adenocarcinoma with nonbacterial thrombotic endocarditis and
repeated arterial thromboembolism at multiple sites after ICI
treatment. This patient was treated with the DOAC, ‘apixaban’
following heparin treatment. Apixaban is a DOAC that strongly and
reversibly directly inhibits FXa, and exerts antithrombotic effects
by suppressing thrombin production through inhibition of FXa. The
CAT was considered an immune-related adverse event, and more than
3-year control was achieved by administration of apixaban, a DOAC,
after heparin therapy.
Case report
A 56-year-old man was referred to Mito Kyodo General
Hospital (Mito, Japan) in August 2020 because of an abnormal
opacity on a chest radiograph taken during annual mass screening. A
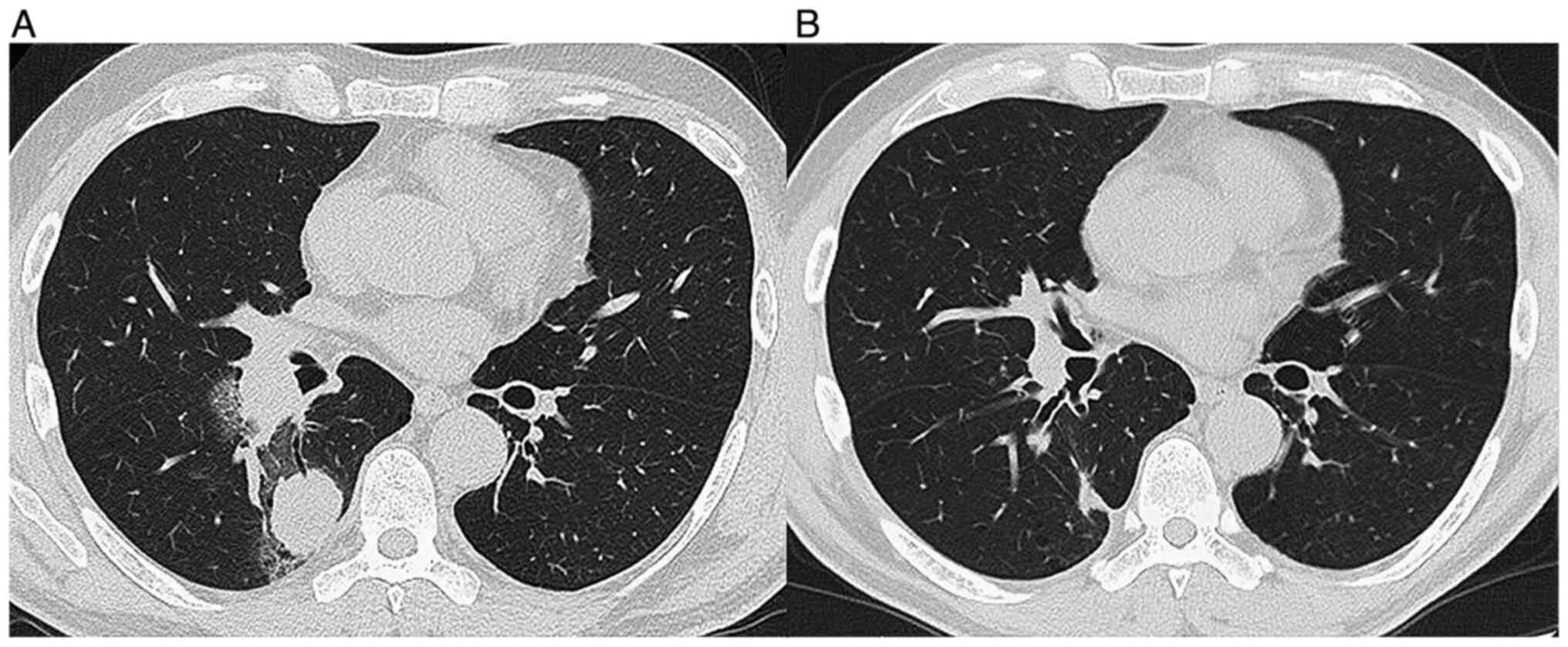
chest CT image showed a nodule in the right lung and ipsilateral
hilar lymphadenopathy (Fig. 1A).
Although he was diagnosed with bronchial asthma at the age of 29,
he had no previous history of arrhythmia, heart disease, or
diseases that caused thromboembolism. There was no family history
of genetic diseases. The patient had a 27 pack-year smoking
history. At the time of admission, his body temperature was 36.8
degrees, heart rate was 84/min, blood pressure was 138/83 mmHg, and
respiratory rate was 16/min. Physical examination detected no
abnormalities. A biopsy specimen obtained by bronchoscopy was
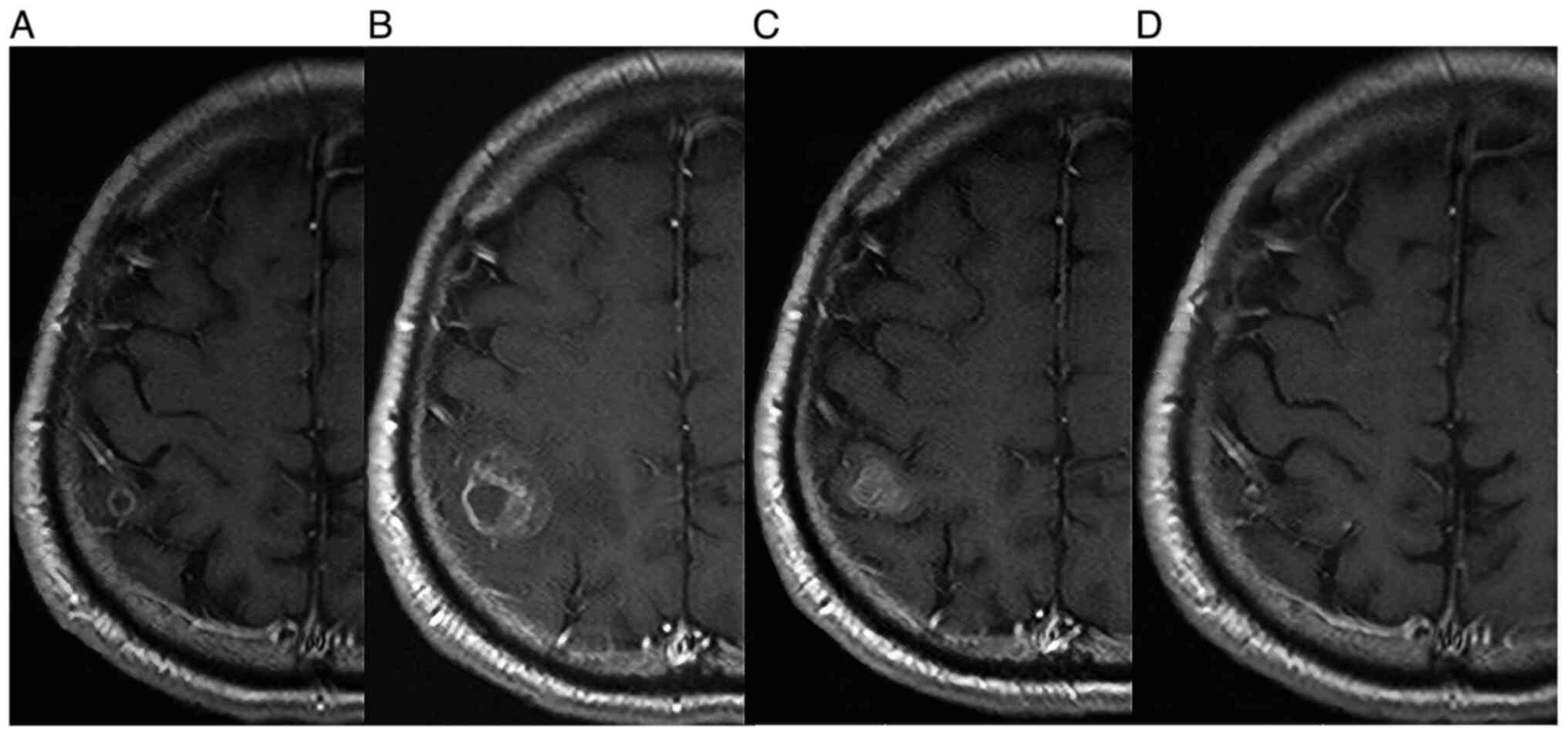
diagnosed histologically as lung adenocarcinoma. As two brain
metastatic lesions in the right temporal and right occipital lobes
were detected (Fig. 2A), his
clinical stage was determined to be T2aN2M1b stage IVB. Treatment
was initiated with pembrolizumab alone (200 mg at a time as an
intravenous drip at 3-week intervals), considering the result of
high PD-L (75%) in the biopsied cancer tissue and the patient's
preference to receive ICI monotherapy. MRI taken in October 2020
revealed an increase of the occipital lobe lesion (Fig. 2B), despite a decrease of the
temporal lobe lesion. The patient's general condition was good
without symptoms, so he was considered to be experiencing
pseudo-progression. MRI taken in November 2020 showed the shrinkage
of this metastatic lesion (Fig.
2C). In an MRI taken in January 2021, complete disappearance of
the lesion was confirmed (Fig.
2D). In CT taken at the same time, intrathoracic lesions also
disappeared (Fig. 1B), and a
complete response was achieved. However, pembrolizumab was
discontinued due to the appearance of ground glass opacity in both
lungs (Fig. 3A) in CT scan taken
in December 2020. The patient was evaluated to have a Grade 2
(National Cancer Institute Common Terminology Criteria for Adverse
Events, version 5.0) pulmonary immune-related adverse effect
(irAE), and steroids were not administered. It was followed
closely, and the ground glass opacity improved, but recurrence of
ipsilateral lymph node lesion (Fig.
3B) in CT scan taken in February 2021, 2 months after stopping
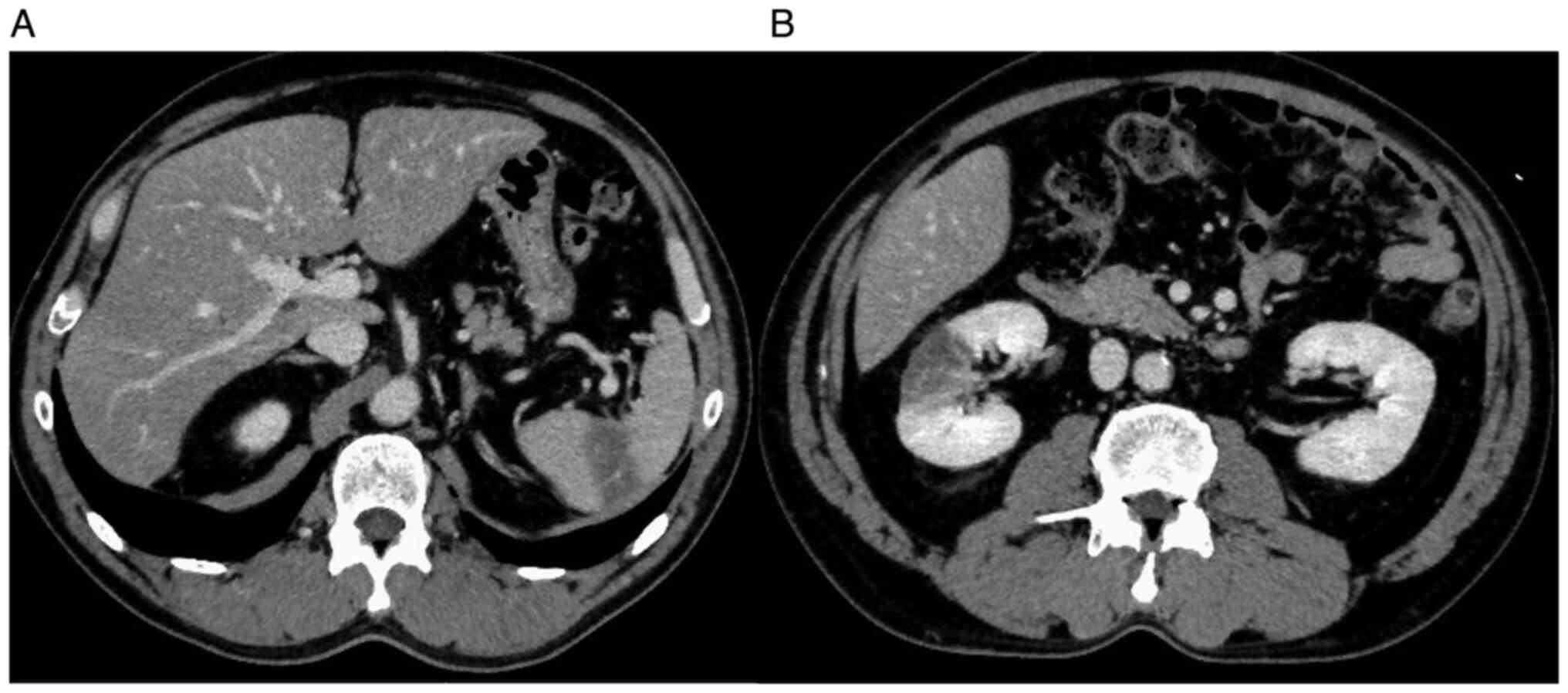
pembrolizumab. At that time, the patient developed back pain, and
CT confirmed arterial thromboembolisms in the right kidney and
spleen (Fig. 4). These arterial
thromboembolisms occurred 4 times during the subsequent 4 months.
Ultrasound examination did not show any thrombus formation in the
veins of the lower extremities, but echocardiography performed at
that time confirmed a 3 mm-sized vegetation attached to the aortic
valve (Fig. 5). Continuous
intravenous infusion of unfractionated heparin (20,000 units per
day) was given for each episode of four repeated arterial
thromboembolisms. After discharge, the patient underwent
subcutaneous self-injection of heparin (18,000 units per day from
February 2020 to July 2021) at home. Four courses of intravenous
pemetrexed (500 mg/m2) and bevacizumab (15 mg/kg)
repeated every 4 weeks were given for lung adenocarcinoma, and a
complete response was achieved. Anticancer treatment was terminated
due to the patient's request to discontinue treatment. Subcutaneous
injections of heparin were administered for five months, until
arterial thromboembolisms were considered controlled without
recurrence. Considering side effects such as induration at the
injection site and the complexity of the self-injection,
subcutaneous heparin injections were changed to a DOAC, apixaban (5
mg orally twice a day) in July 2021. In an echocardiography
performed in January 2022, the vegetation at the aortic valve had
disappeared. The patient continued to receive apixaban at the same
dose and remain in good condition with no thromboembolism or
recurrence of cancer until November 2023, more than three years
after the diagnosis of lung adenocarcinoma. The clinical course is
shown in Fig. 6. The patient has
visited the hospital once every two months so far, and will
continue to visit the hospital once every two months for follow-up
observation.
Discussion
The patient's case was characterized by several
noteworthy features: i) Pseudo-progression of a brain tumor, ii)
repeated thromboembolism in multiple organs and a small vegetation
attached to the aortic valve, iii) long-term control of
thromboembolism with apixaban after heparin therapy, iv) good
response to lung cancer treatment and recurrence-free survival 36
months after diagnosis.
Cerebral pseudo-progression is rare (13-15).
To date, only single case reports or series of cases of cerebral
pseudo-progression have been published, and the incidence of
cerebral pseudo-progression after ICI treatment has not been
determined. Urban et al reported that five of twelve
patients with cerebral pseudo-progression had non-small cell lung
cancer (15). In this patient, ICI
treatment resulted in shrinkage of one of two metastatic lesions
and enlargement of the other. Careful follow-up without anticancer
treatment or steroid treatment confirmed disappearance of
metastatic lesions after several months. Craniotomy and tissue
collection were not performed, but pseudo-progression was
diagnosed.
In patients with lung cancer, as with other
carcinomas, the development of thromboembolism in the brain and
extracerebral organs is common (1). Since cancer-bearing patients often
have abnormalities of the fibrinolytic coagulation system (1), the thromboembolisms were presumed to
be related to the abnormalities. Hypercoagulability is triggered by
the production of mucins by cancer cells, which react with
leukocytes and platelet selectins to form platelet-rich
microthrombi (1). In general,
patients with CAT have a poor prognosis because CAT are often
associated with advanced cancer, complicating treatment of the
underlying disease (16).
Moreover, nonbacterial thrombotic endocarditis with vegetations
attached to the mitral or the aortic valve has been described in
cancer patients (2-4).
Our patient had no further risk factors for developing
thromboembolism such as diabetes or arrhythmia. He had had no
thromboembolism before the start of ICI treatment, and early
echocardiography performed at the time of cerebral thromboembolism
revealed no vegetation in the aortic valve. Therefore, it was
suggested that the later vegetation was caused by CAT or was
related to ICI treatment, but the exact cause was not
determined.
Treatment of thromboembolism in cancer-bearing
patients requires both anticoagulant therapy and treatment for the
underlying malignant disease. At present, low molecular weight
heparin has a lower risk of causing bleeding than unfractionated
heparin, and low molecular weight heparin appears to be more
effective for venous thromboembolism in cancer patients (10-12).
In contrast, warfarin is not sufficiently effective against
thromboembolism in cancer patients (10-12).
Because low molecular weight heparin is not covered by health
insurance in our country, our patient's condition was controlled by
continuous intravenous infusion of unfractionated heparin, followed
by self-subcutaneous injection of unfractionated heparin and later
apixaban. There was no recurrence of CAT during the long-term
follow-up with these treatments or after discontinuation of the
treatments. In recent years, guidelines and reviews for
thromboembolism in cancer-bearing patients have evaluated the
administration of DOACs for thromboembolism in cancer-bearing
patients, and their superiority and inferiority to conventional
treatments have been discussed (10-12).
Advantages of DOACs include i) no need to adjust dosage, ii) no
need to draw blood to assess efficacy, iii) rapid onset of action,
and iv) fewer drug interactions, and v) no need to adjust the
patient's diet during treatment. In contrast, drawbacks have been
pointed out: i) Administration is contraindicated in patients with
severe renal impairment, ii) there is no direct Xa inhibitor
reversal agent, and iii) DOACs are relatively expensive. Among
DOACs, rivaroxaban and edoxaban have been considered effective, but
the administration of apixaban has been shown to have a lower
bleeding risk (17). Tachihara
et al described two patients who developed VTE two to three
years after diagnosis of lung cancer (18). One of them had asymptomatic lower
extremity deep vein thrombosis, the other patient had pulmonary
embolism and lower extremity deep vein thrombosis. However, neither
patient experienced arterial thromboembolisms (18). Both received heparin injections and
one patient received EGFR-tyrosine kinase inhibitors with long-term
response (18). Moreover, Nonagase
et al presented an EGFR-mutated patient with lower extremity
deep vein thrombosis, who was treated with intravenous
unfractionated heparin and survived for ten months after lung
cancer diagnosis (19). According
to a case report by Soga et al, a gastric cancer patient
developed VTE recurrence and nonbacterial thrombotic endocarditis
despite administration of apixaban for VTE (4). That patient underwent valve
replacement, gastric cancer resection, and then subcutaneous
heparin self-injection, and survived for 18 months (4). Although such cases have been
reported, to the best of our knowledge, ours is the first report of
a patient with multiple arterial thromboembolisms and without
cancer recurrence whose condition was controlled with DOAC for more
than three years.
Although good results were achieved in this patient,
caution should be exercised regarding the indications for
administering antineoplastic agents to cancer-bearing patients with
thromboembolism. Optimal therapies and timing of treatment as well
as the optimal administration of DOAC in these patients remain to
be established. Whether CAT or irAE, thromboembolism in patients
with non-small cell lung cancer could be controlled with an
effective immune checkpoint inhibitor-combined chemotherapy in
addition to appropriate anticoagulant therapy, and long-term
survival of these patients could be achieved as in our patient.
Although uncommon, the clinical course of this patient was
considered to be suggestive for the treatment of patients with a
similar course.
In NSCLC, personalized medicine is making remarkable
progress with the discovery of new pathological and serum
biomarkers and the clinical introduction of drugs that are
compatible with these biomarkers (20,21).
However, biomarkers related to paraneoplastic syndromes including
CAT are still in the development stage. Progress in translational
research in this area is strongly desired.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
TK, YS, HS and NH designed the study. TK, YS, GO,
SO, SH, MT, EO and HS collected the data. TK, YS and HS analyzed
the data. TK, YS,HS and NH prepared the manuscript. HS and NH
supervised the study. HS and NH confirm the authenticity of all the
raw data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Institutional
Review Board of the Mito Medical Center, University of Tsukuba-Mito
Kyodo General Hospital (approval no. 16-39).
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of their data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Akinbo DB and Ajayi OI: Thrombotic
pathogenesis and laboratory diagnosis in cancer patients, an
update. Int J Gen Med. 16:259–272. 2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Benedetti M, Morroni S, Fiaschini P, Coiro
S and Savino K: Nonbacterial thrombotic endocarditis with multiple
systemic emboli in a patient with primary lung cancer. J Cardiovasc
Echogr. 32:129–131. 2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Scalia GM, Tandon AK and Robertson JA:
Stroke, aortic vegetations and disseminated adenocarcinoma-a case
of marantic endocarditis. Heart Lung Circ. 21:234–236.
2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Soga Y, Taira K, Sugimoto A, Kurosawa M,
Kira H, Su T, Doi K, Nakano A and Himura Y: Mitral valve
nonbacterial thrombotic endocarditis: A rare multi-surgery-tolerant
survivor of Trousseau's syndrome. Surg Case Rep.
4(104)2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Moik F and Ay C: Venous and arterial
thromboembolism in patients with cancer treated with targeted
anti-cancer therapies. Thromb Res. 213 (Suppl 1):S58–S65.
2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Cheng Y, Ouyang W, Jie C, Zhang J, Yu J
and Xie C: A case of late and lethal Trousseau's syndrome induced
by pembrolizumab in lung adenocarcinoma. Immunotherapy. 15:71–75.
2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Zhao L, Zheng H, Zhu L and Jiang P:
Trousseau's syndrome in a non-small cell lung cancer patient
aggravated by pembrolizumab. J Oncol Pharm Pract. 29:233–238.
2023.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Shionoya Y, Hirohashi Y, Takahashi H,
Hashimoto M, Nishiyama K, Takakuwa Y, Nakatsugawa M, Kubo T,
Kanaseki T, Tsukahara T and Torigoe T: Possible pseudo-progression
of non-small cell lung carcinoma in a patient with clinical
hyper-progression associated with trousseau syndrome who was
treated with pembrolizumab: A case report. Anticancer Res.
41:3699–3706. 2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Horio Y, Takamatsu K, Tamanoi D, Sato R,
Saruwatari K, Ikeda T, Nakane S, Nakajima M, Saeki S, Ichiyasu H,
et al: Trousseau's syndrome triggered by an immune checkpoint
blockade in a non-small cell lung cancer patient. Eur J Immunol.
48:1764–1767. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Ogata M, Ama Y, Ogata T, Hirabatake M,
Yasui H and Satake H: Direct oral anticoagulants for the treatment
of venous thromboembolism in patients with active cancer. In Vivo.
35:2747–2753. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Samaranayake CB, Anderson J, McCabe C,
Zahir SF, Upham JW and Keir G: Direct oral anticoagulants for
cancer-associated venous thromboembolisms: A systematic review and
network meta-analysis. Intern Med J. 52:272–281. 2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Frere C, Farge D, Schrag D, Prata PH and
Connors JM: Direct oral anticoagulant versus low molecular weight
heparin for the treatment of cancer-associated venous
thromboembolism: 2022 updated systematic review and meta-analysis
of randomized controlled trials. J Hematol Oncol.
15(69)2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Cohen JV, Alomari AK, Vortmeyer AO,
Jilaveanu LB, Goldberg SB, Mahajan A, Chiang VL and Kluger HM:
Melanoma brain metastasis pseudoprogression after pembrolizumab
treatment. Cancer Immunol Res. 4:179–182. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Vander Jagt TA, Davis LE, Thakur MD, Franz
C and Pollock JM: Pseudoprogression of CNS metastatic disease of
alveolar soft part sarcoma during anti-PDL1 treatment. Radiol Case
Rep. 13:882–885. 2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Urban H, Steidl E, Hattingen E, Filipski
K, Meissner M, Sebastian M, Koch A, Strzelczyk A, Forster MT,
Baumgarten P, et al: Immune Checkpoint inhibitor-induced cerebral
pseudoprogression: patterns and categorization. Front Immunol.
12(798811)2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Tanimura J, Yamamoto T and Hashimoto T:
Clinical features and prognostic factors in patients with
cancer-associated multiple ischemic stroke: A retrospective
observational study. J Stroke Cerebrovasc Dis.
31(106813)2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Riaz IB, Fuentes HE, Naqvi SAA, He H,
Sipra QR, Tafur AJ, Padranos L, Wysokinski WE, Marshall AL, Vandvik
PO, et al: Direct oral anticoagulants compared with dalteparin for
treatment of cancer-associated thrombosis: A living, interactive
systematic review and network meta-analysis. Mayo Clin Proc.
97:308–324. 2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tachihara M, Nikaido T, Wang X, Sato Y,
Ishii T, Saito K, Sekine S, Tanino Y, Ishida T and Munakata M: Four
cases of Trousseau's syndrome associated with lung adenocarcinoma.
Intern Med. 51:1099–1102. 2012.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Nonagase Y, Takeda M, Tanaka K, Hayashi H,
Iwasa T and Nakagawa K: Treatment of EGFR mutation-positive
non-small cell lung cancer complicated by Trousseau syndrome with
gefitinib followed by osimertinib: A case report. Oncotarget.
9:29532–29535. 2018.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Ortega MA, Navarro F, Pekarek L,
Fraile-Martínez O, García-Montero C, Saez MA, Arroyo M, Monserrat J
and Alvarez-Mon M: Exploring histopathological and serum biomarkers
in lung adenocarcinoma: Clinical applications and translational
opportunities (review). Int J Oncol. 61(154)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Ortega MA, Pekarek L, Navarro F,
Fraile-Martínez O, García-Montero C, Álvarez-Mon MÁ, Diez-Pedrero
R, Boyano-Adánez MDC, Guijarro LG, Barrena-Blázquez S, et al:
Updated views in targeted therapy in the patient with non-small
cell lung cancer. J Pers Med. 13(167)2023.PubMed/NCBI View Article : Google Scholar
|