Introduction
Since the initial reports in December, 2019 for a
novel type of viral pneumonia in the city of Wuhan, Hubei, China,
severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has
spread at an unprecedented rate (1). Current epidemiological data report
~660 million infections and ~6.7 million related deaths worldwide,
with a 7-day average of 500-600.000 new cases and an estimated
mortality rate of ~10%. Since its outbreak in 2019, the need to
develop strategies with which to attenuate the transmission
dynamics of SARS-CoV-2 (flattening the curve) has been recognized
(2,3). Moreover, it was evident from an early
stage that there was a need to stratify patients into risk groups
based on disease severity, which would assist clinicians to
identify patients at a risk of developing disease-related
complications, such as acute respiratory distress syndrome (ARDS)
(4-6).
For example, even during the first wave of the pandemic, it was
evident that older individuals (>65 years of age) were at a
higher risk of developing complications of the disease, with higher
mortality rates among infected older individuals than among younger
adults and children (7).
To date, several blood biomarkers associated with
the cascade of the inflammation processes have emerged as potential
contenders for determining the progression of coronavirus disease
2019 (COVID-19). Among these, N-terminal pro-B-type natriuretic
peptide (NT-pro-BNP) stands out as a crucial biomarker in
ventricular heart disorders, and its elevated levels have been
identified in the advanced stages of cardiovascular disease, as
well as in patients with COVID-19(7). Similarly, fibrinogen, a renowned
acute phase protein, is synthesized abundantly by the liver. It
plays a role in the formation of fibrin, constituting the final
step in the process of coagulation. Previous research has indicated
that changes in fibrinogen levels necessitate attention in patients
with COVID-19(8). Moreover, in
addition to fibrinogen, D-dimer, a product of fibrin degradation,
has also been assessed. Elevated D-dimer levels have been shown to
be associated with pulmonary complications in patients with
COVID-19 (9,10). Additionally, in relation to
pneumonia or pulmonary embolism in COVID-19, there has been an
observed elevation in troponin (Trop max) and ferritin levels
(11). In terms of other organ
systems, it is noteworthy that patients with COVID-19 display
significant alterations in liver functions, as evidenced by
increased levels of alanine transaminase (ALT), aspartate
transaminase (AST) and alkaline phosphatase (ALP), as well as
elevated creatine kinase (CK) and lactate dehydrogenase (LDH)
levels (11). These changes are
indicative of cellular inflammation and oxidative stress.
As regards biomarkers related to infections and
inflammation, procalcitonin (PCT) the 116 amino acid precursor of
the hormone calcitonin, has been considered a biomarker for the
early diagnosis of bacterial infections, including COVID-19
(12-14).
Moreover, C-reactive protein (CRP), an acute-phase protein that
serves as an early marker of inflammation or infection is routinely
measured in the early diagnosis of COVID-19, with its levels being
associated with disease severity (15). CRP has been found to have a
positive association with lung lesions in tomographic scans
(16,17). Previous studies have indicated an
association between increased CRP values upon admission and disease
severity in patients with COVID-19 (18,19).
In addition to the inflammation cascade, endothelial function or
dysfunction has emerged as a pathological characteristic regarding
COVID-19 progression and disease severity. Endothelial cells play a
crucial role in maintaining vascular integrity and participate in
inflammation processes. Endotheliopathy is observed in
cardiovascular diseases, diabetes, obesity and aging in patients
with predisposition characteristics for severe disease and is a
contributing factor to thrombo-inflammation (20). Although it remains unclear whether
endotheliopathy occurs due to the viral infection of endothelial
cells or is a consequence of induced inflammation, it significantly
contributes to thrombo-inflammation (21,22).
Thus, several interventions have been implemented to assess
endothelial markers in patients with COVID-19 (23,24).
Low levels of magnesium (Mg2+) induce a
pro-inflammatory, prothrombotic phenotype in endothelial cells
(25). In COVID-19, while serum
Mg2+ concentrations are lower in mild disease, there are
indications of hypomagnesemia in critically ill patients,
particularly those in intensive care units (ICUs) (26). Considering other factors, phosphate
levels, which contribute to the maintenance of body homeostasis
(bone, metabolism, intracellular signaling) have been previously
analyzed in relation to COVID-19 (27,28).
Finally, the association between the immune response and trace
elements has been previously suggested, highlighting the importance
of investigating any potential association between certain trace
elements and disease outcomes of patients in the ICU (29).
Overall, to date, studies have examined how all this
clinical information can be harnessed and organized to provide
essential information for optimum healthcare provision in COVID-19
(30,31). Nevertheless, it remains important
to comprehend whether there exist additional associations between
demographic factors, such as age and sex, and specific clinical
attributes, notably blood biomarkers, or any other factors that
could provide predictive information as to the outcome of COVID-19
disease severity (32-35).
Hence, the present study aimed to evaluate the predictive value of
clinical blood biomarkers with regard to the outcomes of
hospitalized patients with COVID-19, taking into account age and
sex. Moreover, in order to expand upon prior approaches, the
present study encompasses an assessment of biomarkers, including
PCT, troponin max, vitamin D (Vit-D), CRP, LDH, high-density
lipoprotein (HDL), NT-pro-BNP, ALT, AST, ALP and trace minerals
(i.e., Mg2+, phosphate, Ca2+, Na+,
K+), in order to determine potential associations,
together with the influence of sex and age during the course of the
hospitalization of patients with COVID-19 in the ICU.
Materials and methods
Study design and ethics approval
The present observational, single-center descriptive
study was conducted over a period of 2 years (April, 2020 to April,
2022) in the ICU ward of the Erzurum Regional Training and Research
Hospital in Erzurum, Turkey. The study complied with the rules of
the 1975 Declaration of Helsinki, as revised in 2013, and it was
approved by the Ethics Committee of Erzurum City Hospital and the
Turkish Ministry of Health, General Directorate of Health Services
(no. 2020-12-22T15_29_35). Written informed consent was obtained
from all patients prior to data collection. All data were collected
anonymously and contained non-identifiable information.
Data collection and analysis
All data are derived from patients admitted to the
ICU ward of the hospital and diagnosed with COVID-19 according to
the WHO COVID-19 interim guidelines (7th edition) with laboratory
confirmation of SARS-CoV-2 infection through nasopharyngeal/throat
swab test by reverse transcription-polymerase chain reaction
(RT-PCR) (36). Epidemiological,
clinical and laboratory data were extracted from the electronic
medical records of the hospital. These data included demographic
characteristics (age, sex), blood biomarker parameters, duration of
hospitalization (time from admission till the day of discharge) and
disease outcomes (survival or mortality). A total of three age
groups were considered: Young adults (aged 17-40 years),
middle-aged adults (aged 40-70 years) and elderly (aged >70
years). All the data were obtained from the registry system of the
hospital. Efforts were made to maintain consistent time intervals
for data sampling to ensure the comparability of the data. However,
any effects on these parameters that occurred prior to admission
could not be controlled. Therefore, to certain extent, the data
were collected at the same time intervals as the ICU admission and
on the first day of hospitalization. Blood data biomarkers referred
to PCT, Trop max, pro-BNP (max), fibrinogen, D-dimer Tmax,
ferritin, total plasma protein content, albumin, Vit-D, LDH,
transaminases (AST, ALT), ALP, low-density lipoprotein (LDL), HDL,
CRP and trace minerals (Ca2+, phosphate,
Mg2+, K+, Na+). All data were
grouped as to age, sex and length of stay in the ICU and compared
considering disease outcomes (survival or mortality).
Statistical analysis
Statistical analysis was conducted using the
Statistical Package for Social Sciences (IBM SPSS Statistics for
Windows, Version 26.0; IBM Corp). Data were analyzed using the
Kruskal-Wallis test with post hoc pairwise comparisons performed
using Dunn's test, and are presented as the mean ± standard
deviation (SD). Comparisons were made between surviving and
deceased patients. Values of P<0.05 or P<0.01 were considered
to indicate statistically significant or highly statistically
significant differences with 95% or 99% confidence intervals (CIs),
respectively.
Results
Patient demographic
characteristics
Over the period of 2 years (April, 2020 to April,
2022), 3,050 data from patients who tested positive for SARS-CoV-2
and were admitted to the Erzurum Regional Training and Research
Hospital were recorded and analyzed. There were 1,550 females and
1,500 males. Of these patients, 1,450 recovered and 1,600 patients
succumbed due to COVID-19 related complications. The patient
demographic characteristics are presented in Table I.
 | Table IDemographic characteristics of the
patients with COVID-19 admitted to the ICU over the study
period. |
Table I
Demographic characteristics of the
patients with COVID-19 admitted to the ICU over the study
period.
| A, Age and sex of
the patients as regards sex |
|---|
| Characteristic | | Sex | |
|---|
| Age cohorts,
years | | Male (no. of
patients) | Female (no. of
patients) |
|
17-40 | | 895 | 905 |
|
41-70 | | 467 | 556 |
|
>70 | | 138 | 89 |
| Length of stay in
ICU, days | | | |
|
0 | | 240 | 229 |
|
1-10 | | 453 | 505 |
|
11-20 | | 363 | 358 |
|
21-30 | | 255 | 266 |
|
>30 | | 189 | 192 |
| B, Length of stay
in the ICU as per age group |
| Length of stay in
ICU, days | Patients aged 17-40
years (no. of patients) | Patients aged 41-70
years (no. of patients) | Patients aged
>70 years (no. of patients) |
| 0 | 323 | 144 | 2 |
| 1-10 | 576 | 342 | 40 |
| 11-20 | 432 | 251 | 38 |
| 21-30 | 265 | 202 | 54 |
| >30 | 204 | 84 | 93 |
The levels of blood biomarkers and disease outcomes
of the patients in the present cohort were then analyzed
considering age and sex.
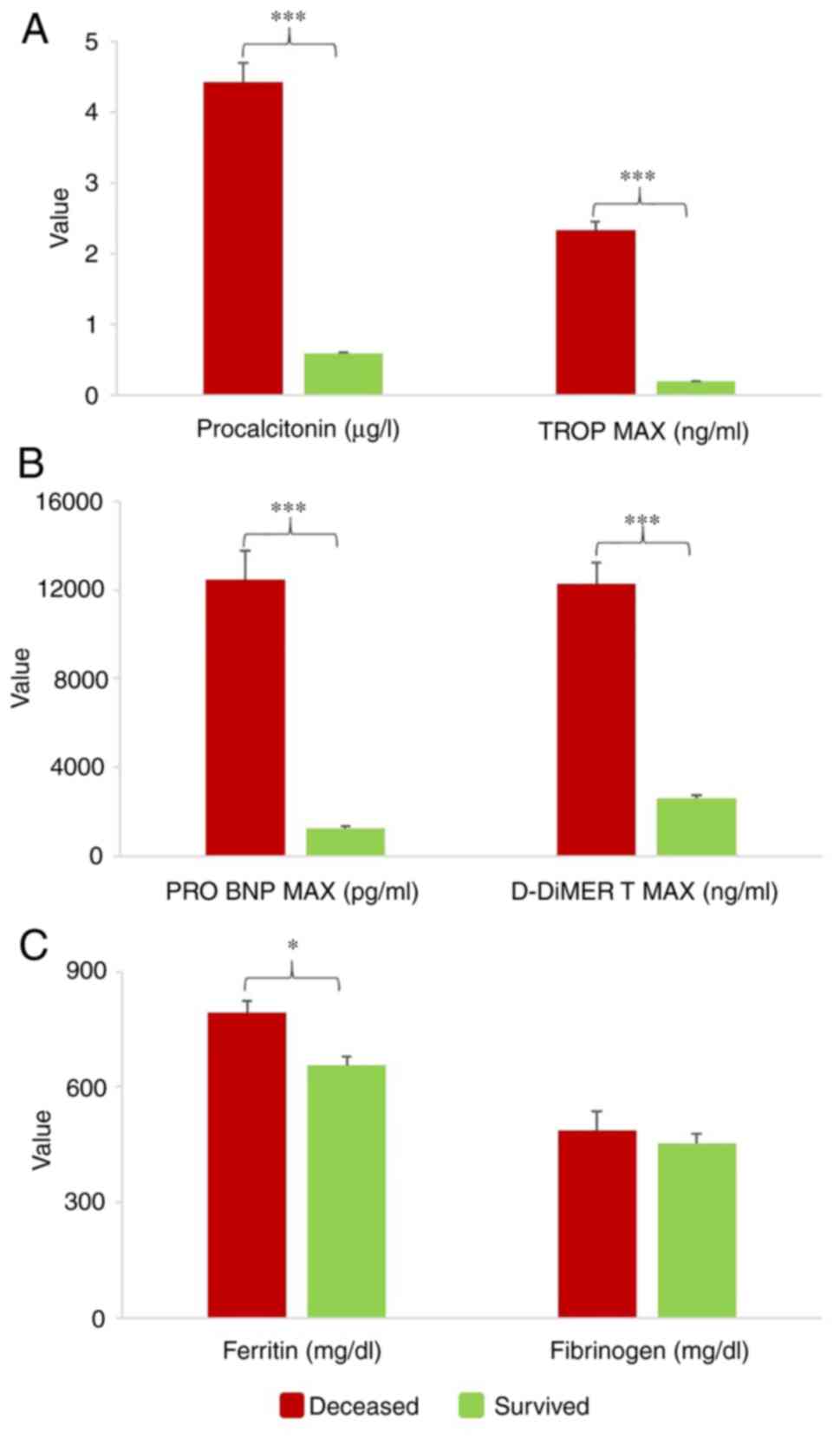
PCT, Trop max, Pro-BNP max,
fibrinogen, D-dimer and ferritin
PCT blood levels range between 0 and 0.05 µg/l under
normal conditions, and exhibit a tendency to increase in cases of
infection (37,38). In the present study, in patients
with COVID-19, the PCT levels were 9-fold higher (P<0.001, 95%
CI) in the deceased compared to the surviving patients (Fig. 1A). The average upper limit of
Pro-BNP max was determined at 300 pg/ml in patients <70 years of
age and 600 pg/ml in patients >70 years of age. The normal Trop
max level is <0.06 ng/ml; however, patients with COVID-19 and
deceased patients have been found to have higher values (mean Trop
max, 2.5 ng/ml). Herein, the Trop max values exhibited an 11-fold
increase (P<0.001, 95% CI) and Pro-BNP levels exhibited a
10-fold increase (P<0.001, 95% CI) in the deceased patients vs.
the surviving patients (Fig. 1A
and B). The D-dimer level, which
normally ranges between 200-500 ng/ml, increased up to 12,000 ng/ml
in the deceased patients, and exhibited a 4-fold increase overall
(P<0.001, 95% CI) (Fig. 1B). As
regards the ferritin levels, the reference value is 4.63-204 mg/dl
in healthy individuals, and herein, it was found to be doubled
(P<0.05, 95% CI), being higher in the deceased vs. the surviving
patients. Finally, the fibrinogen data were above the reference
value range (200-400 mg/dl), and were higher in the deceased
patients vs. the surviving patients, although with no statistically
significant difference (Fig.
1C).
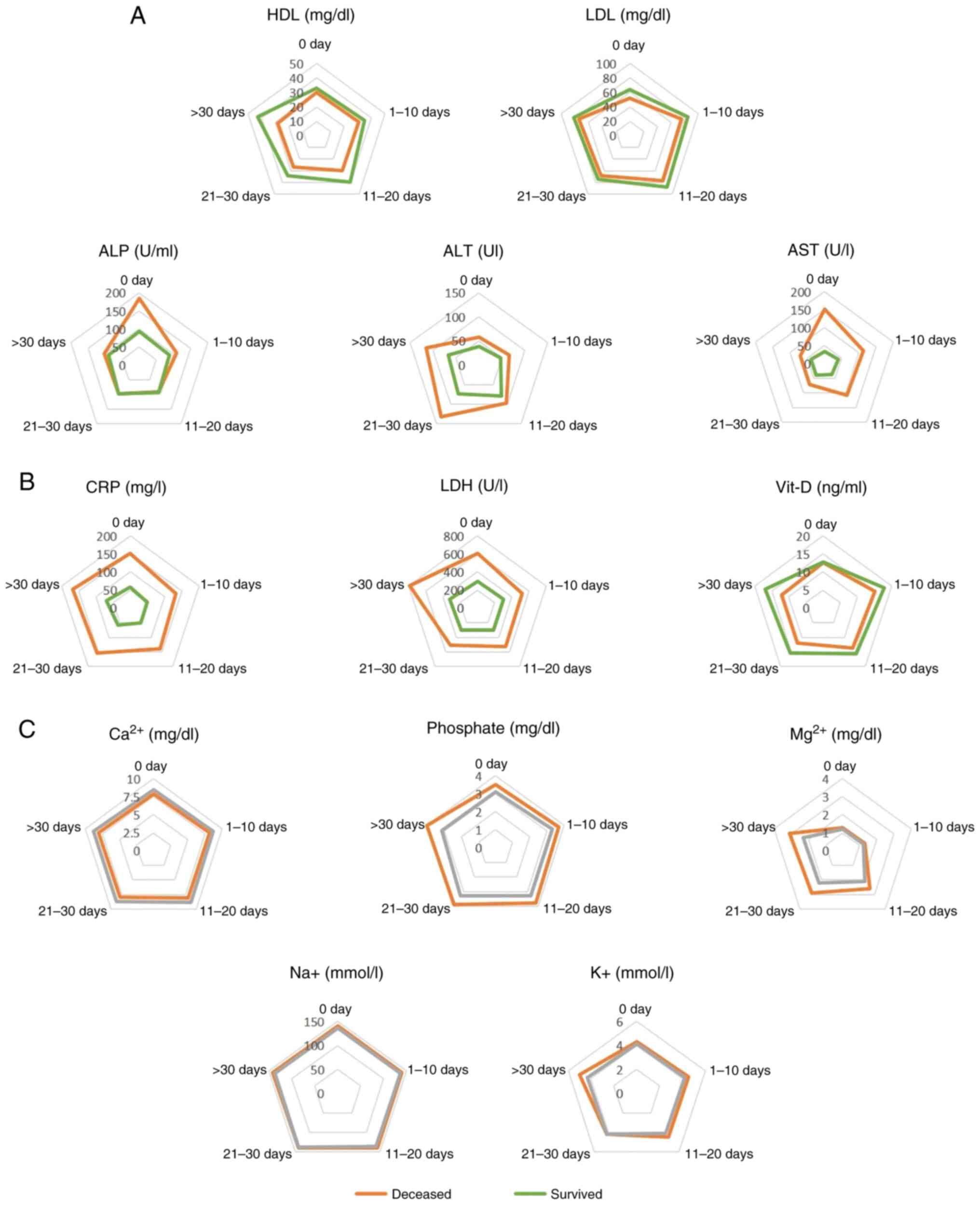
HDL and LDL
Both the HDL (reference value, 40-60 mg/dl) and LDL
(reference value, 60-130 mg/dl) levels were estimated to be ~1.5
lower in the deceased patients compared to the surviving ones
(Figs. 2A, 3A and 4A). However, no statistically significant
association was found between the HDL levels and age or sex
(Figs. 2A and 3A). The decline in HDL levels was
inversely linked with the length of stay in the ICU for the
deceased patients, and differences were observed for patients with
a prolonged (>30 days) ICU stay (Fig. 4A). As regards the LDL levels, a
statistically significant difference between the deceased and
surviving group (P<0.05, 95% CI) was observed in female patients
(Fig. 2A) of all age groups
(Fig. 3A).
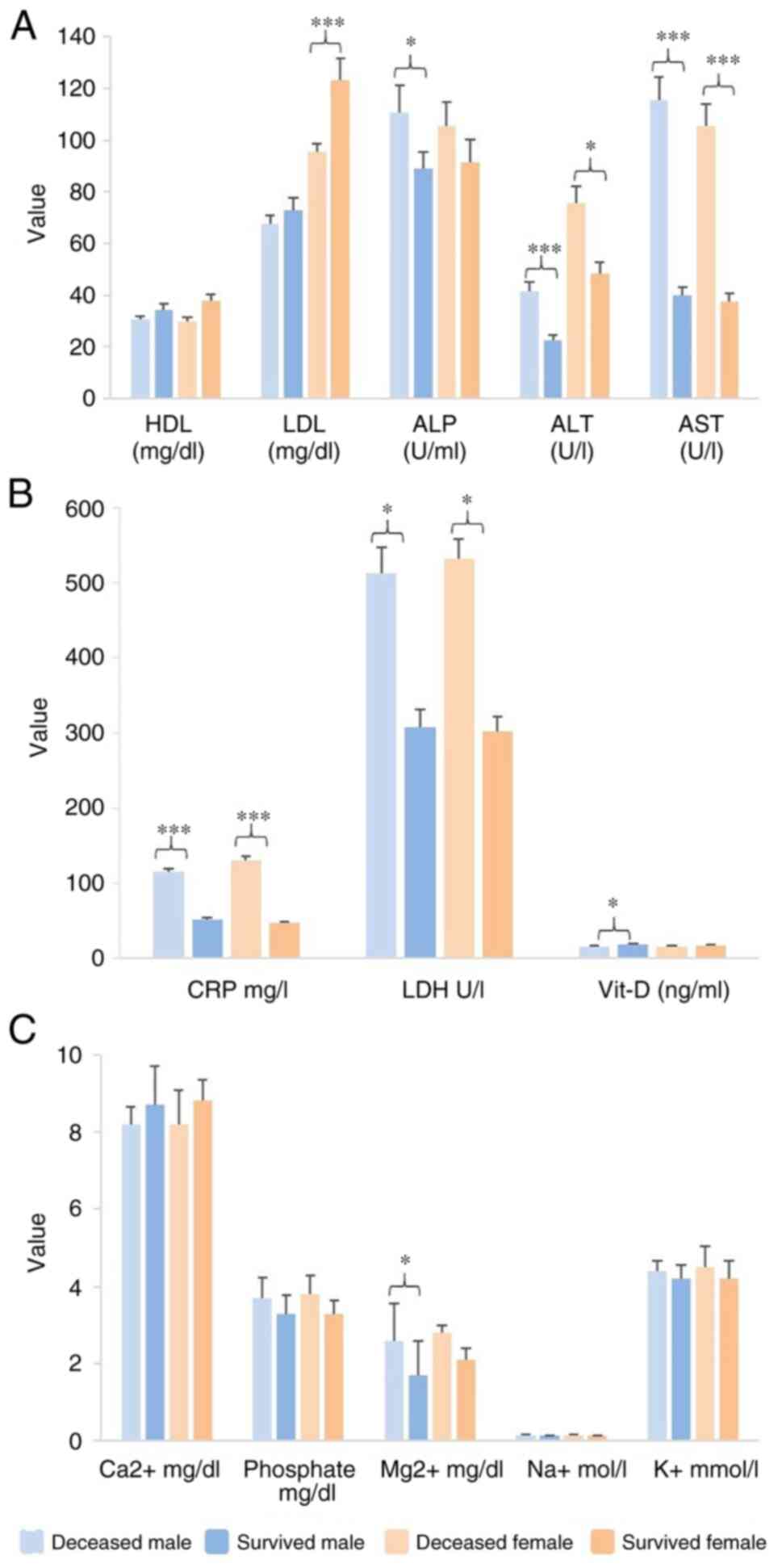
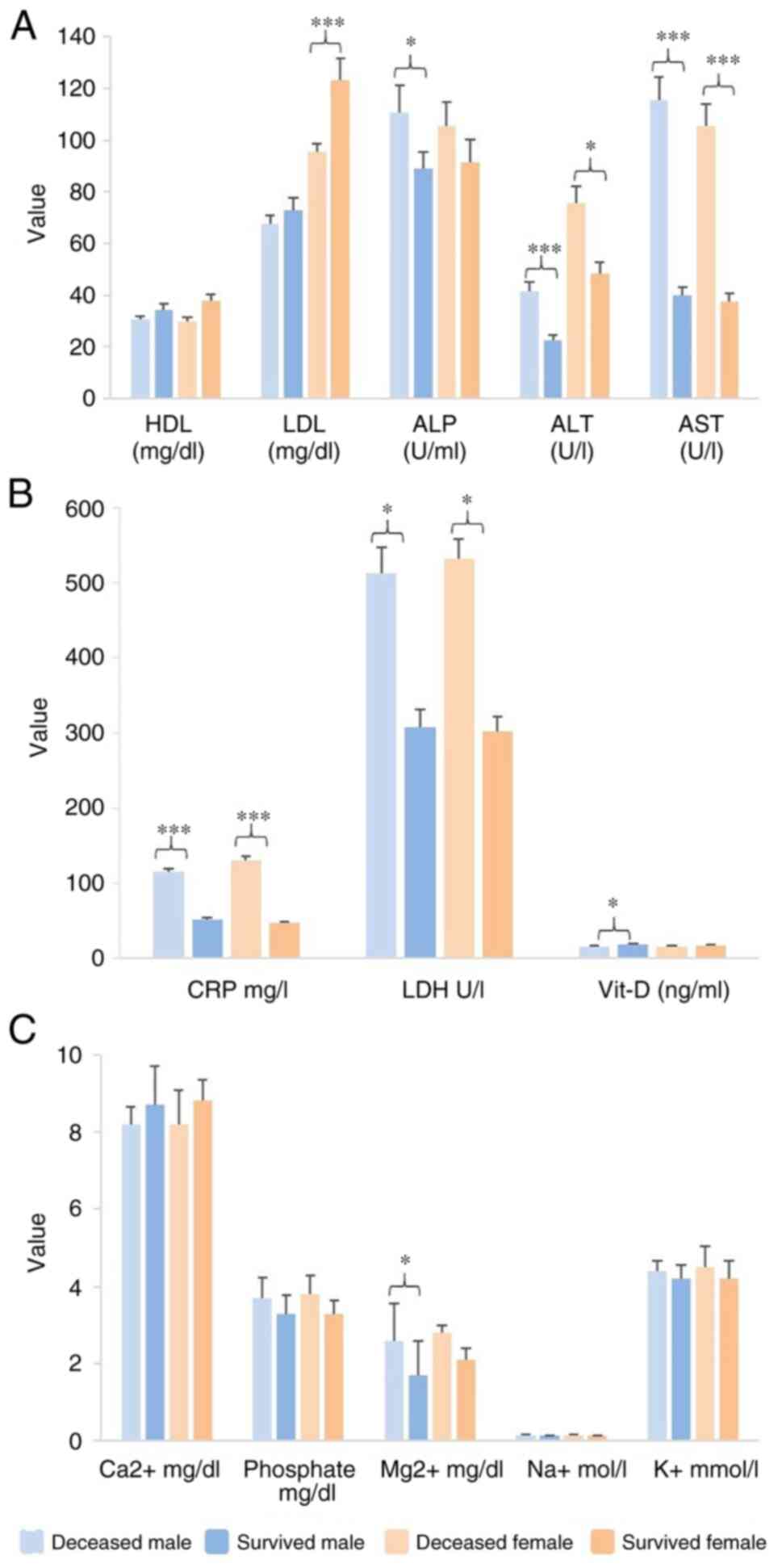 | Figure 2Sex differences as to blood biomarker
levels in the deceased and surviving patients in the present study.
(A) Lipoprotein and liver enzymes. (B) CRP, LDH and Vit-D. (C)
Ca2+, Mg2+, Na+ and K+
trace elements as to sex. *P<0.05 and
***P<0.001 (95% CI). HDL, high-density lipoprotein;
LDL, low-density lipoprotein; ALP, alkaline phosphatase; ALT,
alanine transaminase; AST, aspartate transaminase; CRP, C-reactive
protein; Vit-D, vitamin D. |
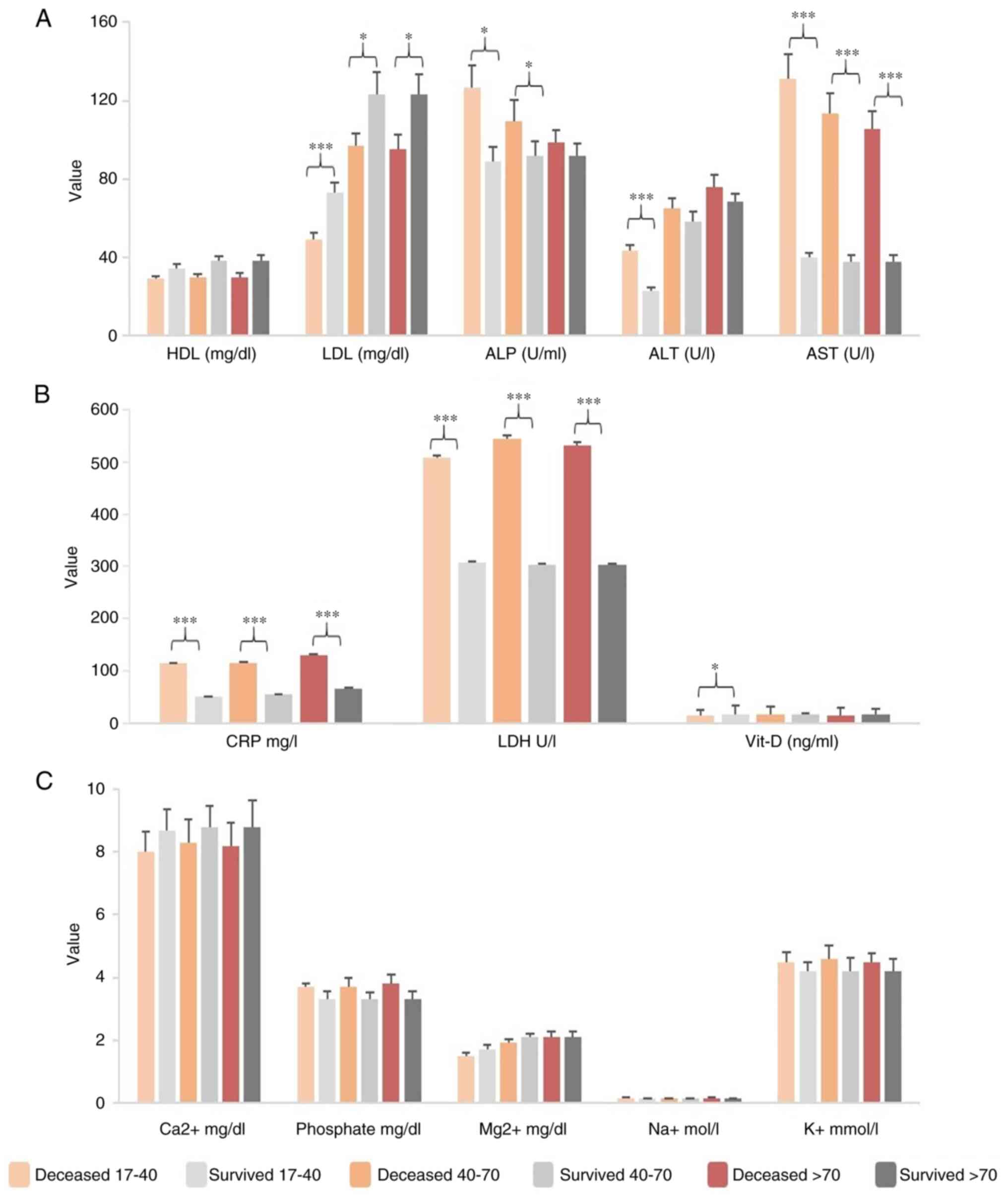
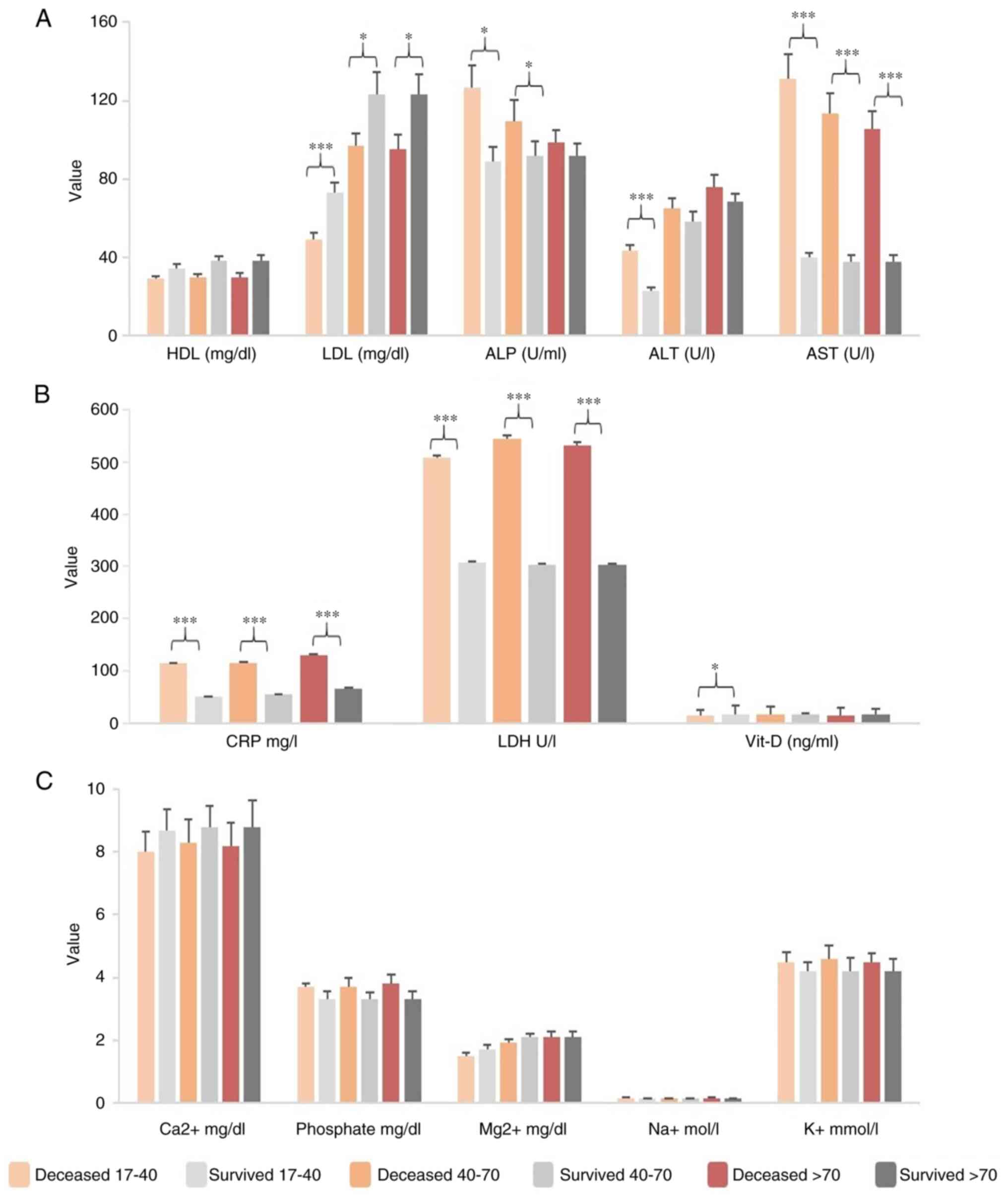 | Figure 3Age differences as regards blood
biomarkers in the deceased and surviving patients in the present
study. (A) Lipoprotein and liver enzymes. (B) CRP, LDH and Vit-Din.
(C) Ca2+, Mg2+, Na+ and
K+ trace elements in the different age groups.
*P<0.05 and ***P<0.001 (95% CI). HDL,
high-density lipoprotein; LDL, low-density lipoprotein; ALP,
alkaline phosphatase; ALT, alanine transaminase; AST, aspartate
transaminase; CRP, C-reactive protein; Vit-D, vitamin D. |
Liver enzymes
Data analysis revealed sex and age differences in
liver enzymes for the deceased and surviving patients in the ICU.
Male patients had higher values of AST (reference value, 0-41 U/l),
while female patients had elevated ALT values (reference value,
0-35 U/l). Higher levels of ALP, ALT and AST in male patients were
associated with a poor prognosis, and similar trends were observed
in female patients, particularly for the ALT and AST values in the
deceased patients (Fig. 2A). In
terms of age, higher levels of ALP, ALT and AST were associated
with disease severity and a poor prognosis in young adults (17-40
years of age) and middle-aged adults (40-70 years of age) (Fig. 3A). The highest ALP values were
found in cases where patients succumbed due to acute disease
complications without ICU hospitalization (Fig. 4A, ALP 0 days). For these cases, the
deceased patients regardless of age and se exhibited also a
statistically significant increase in AST values (5-fold
difference, P<0.001, 95% CI) compared to the surviving ones
(Figs. 2A and 3A). Regardless of ICU stay, the deceased
patients had significantly higher AST values (~5-fold) and there
was a trend for increased ALT levels in patients with extended ICU
stays and disease complications (Fig.
4A).
CRP
Statistically significant differences for CRP
(reference value, <0.5 mg/l) were observed regardless of sex,
age and ICU stay, with increased levels related to disease severity
and a poor prognosis. The CRP values were higher in deceased males
compared to surviving males, and were found to be doubled in
elderly patients (>70 years of age). They were also found to be
associated with a prolonged ICU stay and a poor prognosis, since
the values were almost 2-fold higher (P<0.001, 95% CI) between
the deceased and surviving patients (Figs. 2B, 3B and 4B).
LDH
There was a statistically significant difference
(P<0.05, 95% CI) with a 300% increase in LDH levels between the
deceased and surviving patients (Fig.
2B). There was a significant increase in LDH levels (reference
value, 90-240 U/l), particularly in patients >70 years of age
and with prolonged hospitalization (>30 days) (Figs. 3B and 4B).
Vit-D
All groups, regardless of sex, age, or ICU stay, had
Vit-D levels below the normal reference value (20-50 ng/ml).
Younger adults with a Vit-D deficiency had worse outcomes than
those without one (Fig. 3B). It
was observed that the COVID-19 mortality rate of individuals
hospitalized in ICU, especially at a younger age (17-40 years), was
inversely proportional to the decrease in Vit-D levels.
Additionally, it was found that the Vit-D levels did not differ in
males compared to females. In addition, Vit-D levels in patients
who completed ICU treatment and were discharged (16.9±0.12 ng/ml in
females and 17.5±0.43 ng/ml in males) did not exhibit a significant
difference (P>0.05) (Fig.
2B).
Trace elements
The calcium (Ca2+) levels (reference
value, 8.8-10.6 mg/dl) were similar in all patients, regardless of
the disease outcome, sex, age and ICU stay (Figs. 2C, 3C and 4C). However, the phosphate levels were
increased in patients with a prolonged hospitalization in the ICU.
In addition, the deceased patients had higher levels of phosphate
compared to the survivors (~0.71-fold increase, P<0.05, 95% CI).
Hypermagnesemia was frequently observed and could be associated
with disease severity and mortality. Hypermagnesemia was more
pronounced in males than females, with Mg2+ levels being
~2-fold higher in the deceased compared with the surviving male
patients (P<0.05, 95% CI). By contrast, the increase in
Mg2+ levels in females was not statistically
significant. Moreover, increased Mg2+ levels were
observed in cases with a prolonged hospitalization (Figs. 2C, 3C and 4C). As regards potassium (K+;
reference value, 3.5-5.2 mmol/l) and sodium (Na+) levels
(reference value, 135-146 mmol/l), a prolonged hospitalization
resulted in increased levels of K+, although they were
within the normal expected values. Similarly, no significant
differences were observed in Na+ levels.
Discussion
Severe COVID-19 can cause various respiratory
manifestations ranging from a persistent dry cough and dyspnea to
more severe complications, such as pneumonia with a high fever,
dyspnea, ARDS and pulmonary infiltrates (4,39).
In addition, depending on the comorbidities, it may be associated
with organ failure and hemodynamic distress. Therefore, patient
stratification is required to analyze potential confounding factors
that play a role in inflammation, hemodynamic stress, coagulopathy,
pulmonary embolism, kidney or liver dysfunction and heart failure.
This will assist clinicians to identify patients who are at risk of
being admitted to the ICU and those who may develop severe disease.
Previous studies have reported organ dysfunction (11.0%) (40) and coagulopathy (14.6%) (24), which have resulted in high
mortality rates (4.3%). Although these studies cover different
number of patients and consider factors such as region, age and
length of hospital stay, the essential findings are consistent
(12,13,17,41).
The present study compared the blood parameters of deceased
patients with COVID-19 (n=1,600) with those (n=1.450) who were
discharged from the ICU. The aim of the present study was to
identify statistically significant differences in biomarkers that
are commonly used to assess organ dysfunction, coagulation
disorders, pulmonary embolism risk, inflammation and general blood
biomarkers, and trace elements. Additionally, the present study
investigated whether age and sex differences should be considered
with certain biomarkers.
The role of PCT in COVID-19 pathogenesis has been
proposed, and previous studies have reported that high PCT levels
are associated with the severity of COVID-19 (12-14).
A recent meta-analysis reported a 5-fold increase in PCT values
(42). In the present study, a
9-fold increase was estimated in deceased individuals compared to
the survivors, suggesting that elevated PCT levels may be
associated with severe disease progression. Pro-BNP levels, which
help to assess the risk for heart failure risk and pulmonary
embolism, are often elevated in COVID-19 and have been strongly and
independently associated with mortality (41). Comparable results were observed in
the present study, with a 10-fold increase observed in deceased
patients with COVID-19. This increase was consistent regardless of
age and sex differences. Fibrinogen, an acute phase protein
synthesized in excessive amounts by the liver is involved in fibrin
formation, the final step of coagulation process. Previous research
has suggested that changes in fibrinogen levels need to be
addressed in COVID-19 patients (8). Although changes in fibrinogen levels
are considered clinically relevant to disease severity, herein, no
statistically significant differences were observed regarding
disease outcomes in ICU patients and fibrinogen levels, even when
age and sex differences were taken into account. This suggests that
fibrinogen may potentially serve as a biomarker for COVID-19 at an
early stage prior to ICU admission. Another coagulation factor,
D-dimer, which is formed due to fibrin degradation, is known to
increase thrombotic events and indicates fibrinolysis. Elevated
D-dimer values have previously been associated with a poor
prognosis and high mortality rates in COVID-19(43). These increased values may be
attributed to the activation of the coagulation cascade secondary
to the systemic inflammatory response syndrome in patients with
COVID-19(44). In the present
study, D-dimer levels were found to be ~4-fold higher in deceased
patients compared to those who recovered. Another inflammatory
biomarker associated with COVID-19 is ferritin (45). Changes in ferritin levels were
examined, and an increase was observed, suggesting a potential
association between elevated ferritin levels with disease
progression and overall survival. Similarly, statistically
significant differences in Trop max values were found between the
deceased and surviving cohorts. Trop max has been proposed as a
potential biomarker for disease progression and worse prognosis in
patients with COVID-19(46).
In addition to specific biomarkers related to
infection, inflammation, embolism and coagulopathy, the present
study also examined whether differences could be observed in
general blood biomarkers when accounting for age and sex
differences. For example, previous reports suggest a possible link
between Vit-D levels and the prognosis of patients with COVID-19.
Vit-D levels tend to be decreased in patients admitted to the ICU,
particularly in those who do not survive. The mechanism behind the
association between Vit-D and viral infection is not yet fully
understood; thus, the role of Vit-D deficiency in disease prognosis
warrants further investigation and monitoring. This effect is
considered to be due to the immunomodulatory effect of Vit-D.
However, the results obtained thus far have been inconclusive, with
other studies not showing any positive impact on death rate,
intubation or length of stay with high Vit-D supplementation in the
ICU (47). In the present study,
Vit-D deficiency was also related to a poor outcomes of patients
with COVID-19, although the results varied considering age and sex
(48).
In contrast to Vit-D, the LDH and CRP levels
exhibited a clear association. LDH levels are elevated in acute
hypoxia thus, these levels are expected to be elevated in patients
with COVID-19 (49,50). LDH levels also increase with
advancing age and the length of stay in the ICU due to the body's
tolerance to oxidative stress. This is further exacerbated by
multiple organ damage, particularly to the liver and lungs
(51). In the present study, the
LDH levels were found to be related to disease progression, with a
300% higher value recorded in the deceased compared to the
surviving patients, particularly in elderly patients with a
prolonged hospitalization period. The rise in LDH levels is also
associated an increase in liver enzyme levels and is associated
with an increase in CRP levels (51). CRP levels have been reported to be
higher in patients with COVID-19 with a poor prognosis (52). Previous research has demonstrated
that CRP levels in patients who have succumbed due toCOVID-19 are
10-fold higher than in those who survived (53). The present study observed that the
serum CRP levels increased from 60 mg/l in surviving patients to
120 mg/l in the deceased patients, particularly in those >70
years of age. In addition to its association with LDH levels, CRP
has also been reported to function in conjunction with increased
cytokine levels (IL-1 and IL-6) (51).
In addition to the inflammatory biomarkers, the
present study also analyzed enzyme activities in patients with
COVID-19. The liver is a potential target for SARS-CoV-2, given the
higher expression of ACE2 receptors which the virus exploits.
Previous research has indicated that increased ALT and/or AST
levels and the AST/ALT ratio >1 are associated with disease
progression and an increased mortality rate in hospitalized
patients with COVID-19(54).
Similar findings were observed in the present study, with increased
AST values associated with male patients and increased ALT values
with female patients, while no differences based on age were not
recorded.
Furthermore, the analysis of trace elements was
conducted to identify potential relevance for patients with
COVID-19. Ca2+ is responsible for a number of
physiological functions, such as blood coagulation, the regulation
of muscle contractions, the secretion of hormones and enzymes, and
the regulation of the immune system (54,55).
Previous studies have reported a significant prevalence of
hypocalcemia in patients with COVID-19, with lower levels being
associated with Vit-D deficiency (55-57).
The results of the present study also demonstrated an association,
particularly in cases of disease progression resulting in mortality
and extended hospital stays, which may be attributed to the role of
the liver in Vit-D metabolism. Phosphate is essential for energy
metabolism and abnormal serum phosphate levels have been previously
reported in patients hospitalized in ICUs due to COVID-19 (27,28).
Although the increase in phosphate levels has not yet been fully
explained, the Ca/P ratio holds physiological significance.
However, phosphate metabolism is impaired in COVID-19, along with
the rise in Ca2+.
This increase in association with the mortality rate
may be due to multiple organ damage caused by factors such as
hypoxia, viral infection energy need and blood rate (58). Abnormal electrolyte levels,
particularly hypermagnesemia, are often associated with decreased
renal function, since the kidneys maintain
calcium-magnesium-phosphate homeostasis (59,60).
Mg2+ has been shown to exert anti-inflammatory effects
independently and by activating Vit-D (61). Given that the level of
Mg2+ was higher in the present study in deceased
patients with COVID-19, a poor prognosis associated with
hypermagnesemia may be considered (62). Although there was a slight increase
in Na+ and K+ levels, the results were not
statistically significant.
No significant differences were found between the
cohorts regarding the total protein content and serum albumin. A
low albumin level usually reflects liver and kidney dysfunction
(63). In patients with COVID-19,
albumin is an independent risk factor associated with no
improvement during follow-up. Furthermore, the activity of the
virus is higher in elderly individuals and those with immune system
disorders, which supports the theory of low albumin.
The present study has certain limitations which
should be mentioned. The findings are specific to a single
peripheral hospital in Turkey and may not be extrapolated to other
regions or populations due to possible deviations in patient
characteristics, healthcare practices, environmental
characteristics and other local features (64). Moreover, it is necessary to
consider other factors, such as exposure to environmental
pollutants and other xenobiotics, which could affect immune
response or contribute to the pathogenesis of SARS-CoV-2 and its
immunopathology (65-68).
Therefore, these factors need to be considered when interpreting
the study findings and conducting further research in different
settings. As an observational study, there is also a possibility of
unmeasured confounders that could affect the outcomes and limit the
comprehensive understanding of patient outcomes in critical care
settings. Chronic conditions such as diabetes, heart failure,
chronic obstructive pulmonary disease (COPD), etc., may influence
some of the estimated values in this study prior to the onset of
any COVID-19-related conditions. Additionally, COVID-19 may further
affect values related to these diseases. Addressing this properly
would necessitate creating an extensive dataset and conducting
analyses for each of these diseases and multimorbidity conditions
(e.g., heart disease, heart disease and diabetes, heart disease and
COPD, diabetes and COPD, etc.) and comparing them with COVID-19
cases to extract the specific impact of COVID-19. Furthermore, for
thorough evaluation and to further mitigate the impact of
underlying diseases, several other indicators such as IL-6, renal
function, and white blood cell counts could be employed. However,
this would require a different study design that falls outside the
scope of the present study. Initially, the present study obtained
data on 5,500 patients; however, after excluding chronic and
serious diseases (e.g., bacterial infections), the study cohort was
narrowed down to 3,050 patients. Future research should take into
consideration the aforementioned confounders and indicators, as
well as differences in treatment protocols during various pandemic
waves, variations among SARS-CoV-2 variants, disparities in the
quality of care across different healthcare systems worldwide, and
outcomes in ICU patients both with and without COVID-19.
In conclusion, although pandemic waves appear to be
receding and the post-pandemic era, it is essential to gain a
comprehensive understanding of the clinical outcomes that have
transpired. COVID-19 has undeniably demonstrated the urgent
necessity to formulate effective strategies that can promptly
stratify patients into risk groups, thereby equipping clinicians in
ICU wards with important predictive information regarding the
potential progression of COVID-19. The analysis of clinical data
from the current observational study revealed that PCT, Trop max,
ferritin, D-dimer, CRP and LDH levels are often increased in
patients with disease progression, resulting in prolonged
hospitalization and fatal COVID-19 related complications. In
addition, certain discrepancies related to age and sex have also
been documented in specific cases. These parameters could be
further monitored in the context of patient monitoring and
prediction of disease progression in ICUs toward risk analysis.
Future studies may uncover whether interventions aimed at
regulating the levels of these markers can significantly affect
treatment outcomes.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
ATa, DAS and ATs conceptualized and designed the
study. SG, MEN, OG, CC and AA engaged in the acquisition, analysis
and interpretation of the data. MS, TKN, AOD, AID, RM and EH
contributed to the interpretation of the data, along with
manuscript drafting and finalization. EH and DAS were involved in
the interpretation of the data and on critical revisions on the
intellectual content. ATa and ATs confirm the authenticity of all
the raw data. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study complied with the guidelines of
the 1975 Declaration of Helsinki, as revised in 2013, and was
approved by the Erzurum City hospital's Ethics Committee (Erzurum
Regional Training and Research Hospital) and the Turkish Ministry
of Health, General Directorate of Health Services (approval no.
2020-12-22T15_29_35). Written informed consent was obtained for
data analysis and publication. All data were collected anonymously,
contained non-identifiable information, and analyzed accordingly.
No individual data is presented.
Patient consent for publication
Not applicable.
Competing interests
DAS is the Editor-in-Chief for the journal, but had
no personal involvement in the reviewing process, or any influence
in terms of adjudicating on the final decision, for this article.
The other authors declare that they have no competing
interests.
References
|
1
|
Fernandes Q, Inchakalody VP, Merhi M,
Mestiri S, Taib N, Moustafa Abo El-Ella D, Bedhiafi T, Raza A,
Al-Zaidan L, Mohsen MO, et al: Emerging COVID-19 variants and their
impact on SARS-CoV-2 diagnosis, therapeutics and vaccines. Ann Med.
54:524–540. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kostoff RN, Briggs MB, Kanduc D, Dewanjee
S, Kandimalla R, Shoenfeld Y, Porter AL and Tsatsakis A: Modifiable
contributing factors to COVID-19: A comprehensive review. Food Chem
Toxicol. 171(113511)2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rasmussen SA, Khoury MJ and Del Rio C:
Precision public health as a key tool in the COVID-19 Response.
JAMA. 324:933–934. 2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Du P, Li D, Wang A, Shen S, Ma Z and Li X:
A systematic review and meta-analysis of risk factors associated
with severity and death in COVID-19 Patients. Can J Infect Dis Med
Microbiol. 2021(6660930)2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Scavone C, Mascolo A, Rafaniello C,
Sportiello L, Trama U, Zoccoli A, Bernardi FF, Racagni G, Berrino
L, Castaldo G, et al: Therapeutic strategies to fight COVID-19:
Which is the status artis ? Br J Pharmacol. 179:2128–2148.
2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kostoff RN, Briggs MB, Kanduc D, Shores
DR, Kovatsi L, Drakoulis N, Porter AL, Tsatsakis A and Spandidos
DA: Contributing factors common to COVID-19 and gastrointestinal
cancer. Oncol Rep. 47(16)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Sorrentino S, Cacia M, Leo I, Polimeni A,
Sabatino J, Spaccarotella CAM, Mongiardo A, De Rosa S and Indolfi
C: B-Type Natriuretic Peptide as Biomarker of COVID-19 Disease
Severity-A Meta-Analysis. J Clin Med. 9(2957)2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Osawa I, Okamoto K, Ikeda M, Otani A,
Wakimoto Y, Yamashita M, Shinohara T, Kanno Y, Jubishi D, Kurano M,
et al: Dynamic changes in fibrinogen and D-dimer levels in COVID-19
patients on nafamostat mesylate. J Thromb Thrombolysis. 51:649–656.
2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Düz ME, Balcı A and Menekşe E: D-dimer
levels and COVID-19 severity: systematic review and meta-analysis.
Tuberk Toraks. 68:353–360. 2020.PubMed/NCBI View
Article : Google Scholar
|
|
10
|
Gungor B, Atici A, Baycan OF, Alici G,
Ozturk F, Tugrul S, Asoglu R, Cevik E, Sahin I and Barman HA:
Elevated D-dimer levels on admission are associated with severity
and increased risk of mortality in COVID-19: A systematic review
and meta-analysis. Am J Emerg Med. 39:173–179. 2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Wibowo A, Pranata R, Akbar MR, Purnomowati
A and Martha JW: Prognostic performance of troponin in COVID-19: A
diagnostic meta-analysis and meta-regression. Int J Infect Dis.
105:312–318. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zhang JJ, Dong X, Cao YY, Yuan YD, Yang
YB, Yan YQ, Akdis CA and Gao YD: Clinical characteristics of 140
patients infected with SARS-CoV-2 in Wuhan, China. Allergy.
75:1730–1741. 2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Chen P, Zhang Y, Wen Y, Guo J, Bai W, Jia
J, Ma Y and Xu Y: Clinical and demographic characteristics of
cluster cases and sporadic cases of coronavirus disease 2019
(COVID-19) in 141 patients in the main district of Chongqing,
China, between january and february 2020. Med Sci Monit.
26(e923985)2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Guo F, Xie J, Wu W, Li S, Hu M, Li J,
Jiang L, Du B, Tong Z and Qiu H: Clinical characteristics and
outcomes of critically ill patients with coronavirus disease 2019
with hypotension in China: A retrospective cohort study. Ann
Palliat Med. 10:8536–8546. 2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Warusevitane A, Karunatilake D, Sim J,
Smith C and Roffe C: early diagnosis of pneumonia in severe stroke:
Clinical features and the diagnostic role of C-Reactive Protein.
PLoS One. 11(e0150269)2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Wang G, Wu C, Zhang Q, Wu F, Yu B, Lv J,
Li Y, Li T, Zhang S, Wu C, et al: C-Reactive protein level may
predict the risk of COVID-19 Aggravation. Open Forum Infect Dis.
7(ofaa153)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Liu F, Li L, Xu M, Wu J, Luo D, Zhu Y, Li
B, Song X and Zhou X: Prognostic value of interleukin-6, C-reactive
protein, and procalcitonin in patients with COVID-19. J Clin Virol.
127(104370)2020.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Chen X, Yang Y, Huang M, Liu L, Zhang X,
Xu J, Geng S, Han B, Xiao J and Wan Y: Differences between COVID-19
and suspected then confirmed SARS-CoV-2-negative pneumonia: A
retrospective study from a single center. J Med Virol.
92:1572–1579. 2020.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Sharifpour M, Rangaraju S, Liu M, Alabyad
D, Nahab FB, Creel-Bulos CM and Jabaley CS: Emory COVID-19 Quality
& Clinical Research Collaborative. C-Reactive protein as a
prognostic indicator in hospitalized patients with COVID-19. PLoS
One. 15(e0242400)2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Pousa PA, Mendonça TSC, Oliveira EA and
Simões-E-Silva AC: Extrapulmonary manifestations of COVID-19 in
children: A comprehensive review and pathophysiological
considerations. J Pediatr (Rio J). 97:116–139. 2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Peerschke EI, Valentino A, So RJ, Shulman
S and Ravinder : Thromboinflammation supports complement
activation in cancer patients with COVID-19. Front Immunol.
12(716361)2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Batatinha HAP, Krüger K and Rosa Neto JC:
Thromboinflammation and COVID-19: The role of exercise in the
prevention and treatment. Front Cardiovasc Med.
7(582824)2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Carvalho T: Extrapulmonary SARS-CoV-2
manifestations. Nat Med. 26(1806)2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Goshua G, Pine AB, Meizlish ML, Chang CH,
Zhang H, Bahel P, Baluha A, Bar N, Bona RD, Burns AJ, et al:
Endotheliopathy in COVID-19-associated coagulopathy: Evidence from
a single-centre, cross-sectional study. Lancet Haematol.
7:e575–e582. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Maier JA: Endothelial cells and magnesium:
Implications in atherosclerosis. Clin Sci (Lond). 122:397–407.
2011.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Mazilu L, Katsiki N, Nikolouzakis TK,
Aslanidis MI, Lazopoulos G, Kouretas D, Tsatsakis A, Suceveanu AI,
Stoian AP, Parepa IR, et al: Thrombosis and Haemostasis challenges
in COVID-19-Therapeutic perspectives of heparin and tissue-type
plasminogen activator and potential toxicological reactions-a mini
review. Food Chem Toxicol. 148(111974)2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Broman M, Wilsson AMJ, Hansson F and
Klarin B: Analysis of Hypo- and Hyperphosphatemia in an Intensive
Care Unit Cohort. Anesth Analg. 124:1897–1905. 2017.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Fakhrolmobasheri M, Vakhshoori M,
Heidarpour M, Najimi A, Mozafari AM and Rezvanian H:
Hypophosphatemia in coronavirus disease 2019 (COVID-19),
complications, and considerations: A systematic review. Biomed Res
Int. 2022(1468786)2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Bego T, Meseldžić N, Prnjavorac B,
Prnjavorac L, Marjanović D, Azevedo R, Pinto E, Duro M, Couto C and
Almeida A: Association of trace element status in COVID-19 patients
with disease severity. J Trace Elem Med Biol.
74(127055)2022.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Docea AO, Tsatsakis A, Albulescu D,
Cristea O, Zlatian O, Vinceti M, Moschos SA, Tsoukalas D, Goumenou
M, Drakoulis N, et al: A new threat from an old enemy: Re-emergence
of coronavirus (Review). Int J Mol Med. 45:1631–1643.
2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Stancioiu F, Papadakis GZ, Kteniadakis S,
Izotov BN, Coleman MD, Spandidos DA and Tsatsakis A: A dissection
of SARS-CoV2 with clinical implications (Review). Int J Mol Med.
46:489–508. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Marginean CM, Popescu M, Vasile CM,
Cioboata R, Mitrut P, Popescu IAS, Biciusca V, Docea AO, Mitrut R,
Marginean IC, et al: Challenges in the differential diagnosis of
COVID-19 Pneumonia: A pictorial review. Diagnostics (Basel).
12(2823)2022.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Skalny AV, Rink L, Ajsuvakova OP, Aschner
M, Gritsenko VA, Alekseenko SI, Svistunov AA, Petrakis D, Spandidos
DA, Aaseth J, et al: Zinc and respiratory tract infections:
Perspectives for COVID-19 (Review). Int J Mol Med. 46:17–26.
2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Neagu M, Calina D, Docea AO, Constantin C,
Filippini T, Vinceti M, Drakoulis N, Poulas K, Nikolouzakis TK,
Spandidos DA and Tsatsakis A: Back to basics in COVID-19: Antigens
and antibodies-Completing the puzzl. J Cell Mol Med. 25:4523–4533.
2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Calina D, Hernández AF, Hartung T, Egorov
AM, Izotov BN, Nikolouzakis TK, Tsatsakis A, Vlachoyiannopoulos PG
and Docea AO: Challenges and scientific prospects of the newest
generation of mRNA-Based vaccines against SARS-CoV-2. Life (Basel).
11(907)2021.PubMed/NCBI View Article : Google Scholar
|
|
36
|
WHO: Clinical management of COVID-19:
Living guideline, 13 January 2023. Clin Manag COVID-19 LIVING
Guidel Sept 2022 2023, 2023.
|
|
37
|
Tello-Montoliu A, Marín F, Roldán V,
Mainar L, López MT, Sogorb F, Vicente V and Lip GY: A multimarker
risk stratification approach to non-ST elevation acute coronary
syndrome: Implications of troponin T, CRP, NT pro-BNP and fibrin
D-dimer levels. J Intern Med. 262:651–658. 2007.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Covington EW, Roberts MZ and Dong J:
Procalcitonin monitoring as a guide for antimicrobial therapy: A
review of current literature. Pharmacotherapy. 38:569–581.
2018.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Aslan A, Aslan C, Zolbanin NM and Jafari
R: Acute respiratory distress syndrome in COVID-19: possible
mechanisms and therapeutic management. Pneumonia (Nathan).
13(14)2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Wu T, Zuo Z, Kang S, Jiang L, Luo X, Xia
Z, Liu J, Xiao X, Ye M and Deng M: Multi-organ Dysfunction in
Patients with COVID-19: A systematic review and meta-analysis.
Aging Dis. 11:874–894. 2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J,
Wang B, Xiang H, Cheng Z, Xiong Y, et al: Clinical Characteristics
of 138 Hospitalized Patients With 2019 novel coronavirus-infected
pneumonia in Wuhan, China. JAMA. 323:1061–1069. 2020.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Lippi G and Plebani M: Procalcitonin in
patients with severe coronavirus disease 2019 (COVID-19): A
meta-analysis. Clin Chim Acta. 505:190–191. 2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Giannis D, Ziogas IA and Gianni P:
Coagulation disorders in coronavirus infected patients: COVID-19,
SARS-CoV-1, MERS-CoV and lessons from the past. J Clin Virol.
127(104362)2020.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Léonard-Lorant I, Delabranche X, Séverac
F, Helms J, Pauzet C, Collange O, Schneider F, Labani A, Bilbault
P, Molière S, et al: Acute Pulmonary Embolism in Patients with
COVID-19 at CT Angiography and Relationship to d-Dimer Levels.
Radiology. 296:E189–E191. 2020.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Cheng L, Li H, Li L, Liu C, Yan S, Chen H
and Li Y: Ferritin in the coronavirus disease 2019 (COVID-19): A
systematic review and meta-analysis. J Clin Lab Anal.
34(e23618)2020.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Salvatici M, Barbieri B, Cioffi SMG,
Morenghi E, Leone FP, Maura F, Moriello G and Sandri MT:
Association between cardiac troponin I and mortality in patients
with COVID-19. Biomarkers. 25:634–640. 2020.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Orchard L, Baldry M, Nasim-Mohi M, Monck
C, Saeed K, Grocott MPW and Ahilanandan D: Vitamin-D levels and
intensive care unit outcomes of a cohort of critically ill COVID-19
patients. Clin Chem Lab Med. 59:1155–1163. 2021.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Güven M and Gültekin H: The effect of
high-dose parenteral vitamin D(3) on COVID-19-related inhospital
mortality in critical COVID-19 patients during intensive care unit
admission: An observational cohort study. Eur J Clin Nutr.
75:1383–1388. 2021.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Lukacova S, Sørensen BS, Alsner J,
Overgaard J and Horsman MR: The impact of hypoxia on the activity
of lactate dehydrogenase in two different pre-clinical tumour
models. Acta Oncol. 47:941–947. 2008.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Fialek B, Pruc M, Smereka J, Jas R,
Rahnama-Hezavah M, Denegri A, Szarpak A, Jaguszewski MJ, Peacock FW
and Szarpak L: Diagnostic value of lactate dehydrogenase in
COVID-19: A systematic review and meta-analysis. Cardiol J.
29:751–758. 2022.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Poggiali E, Zaino D, Immovilli P, Rovero
L, Losi G, Dacrema A, Nuccetelli M, Vadacca GB, Guidetti D,
Vercelli A, et al: Lactate dehydrogenase and C-reactive protein as
predictors of respiratory failure in CoVID-19 patients. Clin Chim
Acta. 509:135–138. 2020.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Ali N: Elevated level of C-reactive
protein may be an early marker to predict risk for severity of
COVID-19. J Med Virol. 92:2409–2411. 2020.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Smilowitz NR, Kunichoff D, Garshick M,
Shah B, Pillinger M, Hochman JS and Berger JS: C-reactive protein
and clinical outcomes in patients with COVID-19. Eur Heart J.
42:2270–2279. 2021.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Medetalibeyoglu A, Catma Y, Senkal N,
Ormeci A, Cavus B, Kose M, Bayramlar OF, Yildiz G, Akyuz F,
Kaymakoglu S and Tukek T: The effect of liver test abnormalities on
the prognosis of COVID-19. Ann Hepatol. 19:614–621. 2020.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Osman W, Al Fahdi F, Al Salmi I, Al
Khalili H, Gokhale A and Khamis F: serum calcium and vitamin D
levels: Correlation with severity of COVID-19 in hospitalized
patients in Royal Hospital, Oman. Int J Infect Dis. 107:153–163.
2021.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Sun JK, Zhang WH, Zou L, Liu Y, Li JJ, Kan
XH, Dai L, Shi QK, Yuan ST, Yu WK, et al: Serum calcium as a
biomarker of clinical severity and prognosis in patients with
coronavirus disease 2019. Aging (Albany NY). 12:11287–11295.
2020.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Alemzadeh E, Alemzadeh E, Ziaee M, Abedi A
and Salehiniya H: The effect of low serum calcium level on the
severity and mortality of Covid patients: A systematic review and
meta-analysis. Immunity, Inflamm Dis. 9:1219–1228. 2021.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Malinowska J, Małecka-Giełdowska M,
Bańkowska D, Borecka K and Ciepiela O: Hypermagnesemia and
hyperphosphatemia are highly prevalent in patients with COVID-19
and increase the risk of death. Int J Infect Dis. 122:543–549.
2022.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Bailey RL, Gahche JJ, Lentino CV, Dwyer
JT, Engel JS, Thomas PR, Betz JM, Sempos CT and Picciano MF:
Dietary supplement use in the United States, 2003-2006. J Nutr.
141:261–266. 2011.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Blaine J, Chonchol M and Levi M: Renal
control of calcium, phosphate, and magnesium homeostasis. Clin J Am
Soc Nephrol. 10:1257–1272. 2015.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Uwitonze AM and Razzaque MS: Role of
Magnesium in Vitamin D Activation and Function. J Am Osteopath
Assoc. 118:181–189. 2018.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Stevens JS, Moses AA, Nickolas TL, Husain
SA and Mohan S: Increased mortality associated with hypermagnesemia
in severe COVID-19 Illness. Kidney360. 2:1087–1094. 2021.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Ko JH, Park GE, Lee JY, Lee JY, Cho SY, Ha
YE, Kang CI, Kang JM, Kim YJ, Huh HJ, et al: Predictive factors for
pneumonia development and progression to respiratory failure in
MERS-CoV infected patients. J Infect. 73:468–475. 2016.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Thakur B, Dubey P, Benitez J, Torres JP,
Reddy S, Shokar N, Aung K, Mukherjee D and Dwivedi AK: A systematic
review and meta-analysis of geographic differences in comorbidities
and associated severity and mortality among individuals with
COVID-19. Sci Rep. 11(8562)2021.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Petrakis D, Nikolouzakis TK, Karzi V,
Vardavas AI, Vardavas CI and Tsatsakis A: The growing anthropogenic
immune deficit and the COVID-19 pandemic. Public Heal Toxicol.
1(1)2021.
|
|
66
|
Tsatsakis A, Petrakis D, Nikolouzakis TK,
Docea AO, Calina D, Vinceti M, Goumenou M, Kostoff RN, Mamoulakis
C, Aschner M and Hernández AF: COVID-19, an opportunity to
reevaluate the correlation between long-term effects of
anthropogenic pollutants on viral epidemic/pandemic events and
prevalence. Food Chem Toxicol. 141(111418)2020.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Skalny AV, Timashev PS, Aschner M, Aaseth
J, Chernova LN, Belyaev VE, Grabeklis AR, Notova SV, Lobinski R,
Tsatsakis A, et al: Serum zinc, copper, and other biometals are
associated with COVID-19 severity markers. Metabolites.
11(244)2021.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Agathokleous E, Barceló D, Iavicoli I,
Tsatsakis A and Calabrese EJ: Disinfectant-induced hormesis: An
unknown environmental threat of the application of disinfectants to
prevent SARS-CoV-2 infection during the COVID-19 pandemic? Environ
Pollut. 292(Pt B)(118429)2022.PubMed/NCBI View Article : Google Scholar
|