Introduction
Yellow nail syndrome (YNS) is a relatively rare
syndrome consisting of a triad of yellow, slow-growing nails;
lymphedema; and respiratory lesions (1). More than half of the patients with
this syndrome have exudative pleural effusion, which may be
attributed to lymphedema (2). At
present, the etiology of this syndrome is unclear and no
fundamental treatment has been established (1,3).
Reportedly, control of the pleural effusion associated with YNS can
be achieved with repeated thoracentesis, as well as pleurodesis
(2,4,5).
However, to the best of our knowledge, no standard therapy for
pleural effusion has yet been established. Analysis of the pleural
fluid in this syndrome has shown a high proportion of lymphocytes,
suggesting that some lymphocytic abnormality may be involved in the
development of pleural effusion (6-9).
As previously shown, corticosteroids can be administered to reduce
inflammation and suppress excessive immune responses in various
lymphatic diseases, including lymphedema, lymphangitis and lymphoma
(10).
The present study describes the case of a patient
with YNS presenting with bilateral pleural effusion, whose disease
was controlled with systemic corticosteroid administration. It is
considered that this will provide useful information on the future
treatment of patients with a similar course.
Case report
A 73-year-old man (height, 167.8 cm; weight, 64.8
kg) was referred to the University of Tsukuba Hospital (Ibaraki,
Japan) in July 2017 with complaints of a cough and shortness of
breath. The patient had noticed thickening, yellowing and poor
growth of their nails ~5 years earlier, and subsequently became
aware of a cough and dyspnea, which gradually worsened, for which
the patient visited a nearby clinic. The patient had smoked 10
cigarettes/day for 60 years, but had no history of drinking
alcohol. Chest radiography taken at a previous hospital indicated
the presence of bilateral pleural effusion. Hence, the patient was
admitted to the University of Tsukuba Hospital for further
evaluation. Physical examination at admission revealed the
following: Blood pressure, 140/63 mmHg (normal range, 90/60-120/60
mmHg); pulse rate, 117 beats/min (normal range, 60-100 beats/min);
body temperature, 37.1˚C (normal range, 36.1-37.2˚C); respiratory
rate, 24 breaths/min (normal range, 12-18 breaths/min); and blood
oxygen level, 92% (normal range, 95-100%) while breathing 3 l/min
oxygen via a nasal cannula. Breath sounds were attenuated in both
lower lungs. The fingernails and toenails of the patient were
yellow and thickened (Fig. 1).
Non-pitting edema was observed in both lower extremities, with no
palpable lymph nodes in the neck, axilla or groin. Hematological
evaluation revealed the following: White blood count (WBC) count,
8,700/µl (normal range, 3,700-9,400/µl) [neutrophils (Neu) 77%,
lymphocytes (Lym) 12% and eosinophils (Eos) 2%]; hemoglobin, 17.9
g/dl (normal range, 14-18 g/dl); total proteins, 6.4 g/dl (normal
range, 6.8-8.3 g/dl); albumin, 2.9 g/dl (normal range, 3.8-5.3
g/dl); aspartate aminotransferase, 21 U/l (normal range, 13-33
U/l); alanine transaminase, 10 U/l (normal range, 8-42 U/l);
lactate dehydrogenase (LDH), 289 U/l (normal range, 101-193 U/l);
blood urea nitrogen, 8.9 mg/dl (normal range, 8-20 mg/dl);
creatinine, 0.87 mg/dl (normal range, 0.6-1.1 mg/dl); C-reactive
protein, 1.87 mg/dl (normal range, <0.2 mg/dl);
thyroid-stimulating hormone, 1.48 µIU/ml (normal range, 0.45-4.5
µIU/ml); triiodothyronine, 1.9 pg/ml (normal range, 1.7-4.0 pg/ml);
and thyroxine, 1.2 mg/dl (normal range, 0.7-1.5 mg/dl). Rheumatoid
factor and anti-nuclear antibodies were both negative, but soluble
interleukin-2 receptor (sIL-2R) was elevated (845 U/ml; normal
range, 122-496 U/ml). Analysis of pleural fluid showed the
following: Protein, 3.9 g/dl; LDH, 120 U/l; WBC, 3,000/µl (Neu 17%,
Lym 83% and Eos 2%); adenosine deaminase level, 12.9 U/l. According
to Light's criteria, the pleural effusion was diagnosed as
exudative. Evaluation for Mycobacterium tuberculosis was
negative on smear, PCR (COBAS TaqMan 48; Roche Diagnostics) and
culture tests. The PCR was performed according to the
manufacturer's protocol and the sequences of the primers were not
disclosed. Cytological examination of the pleural fluid showed no
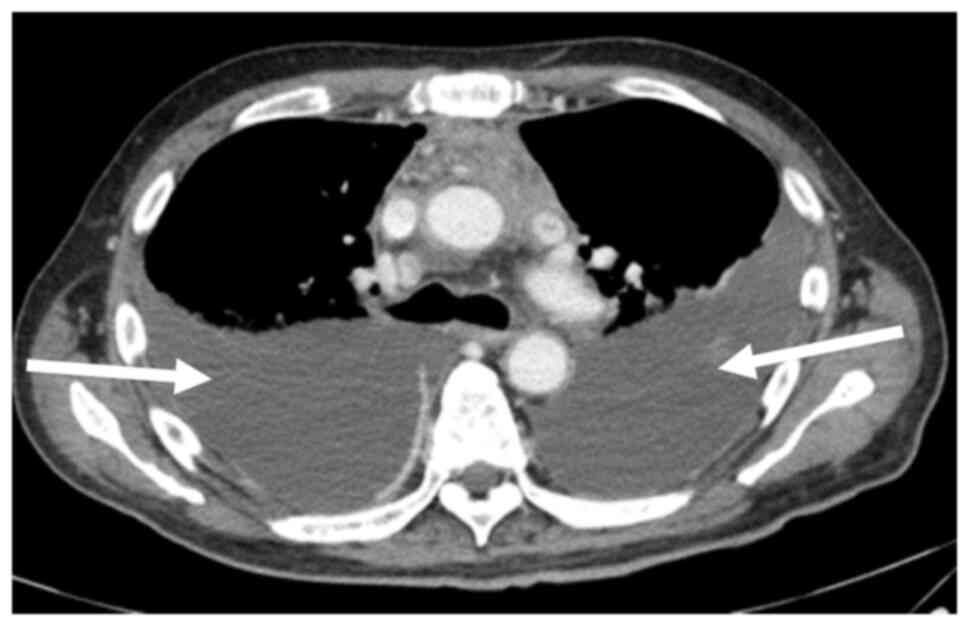
atypical cells. Chest computed tomography (CT) showed bilateral
pleural effusion, diffuse pleural thickening and mediastinal
lymphadenopathy (Fig. 2).
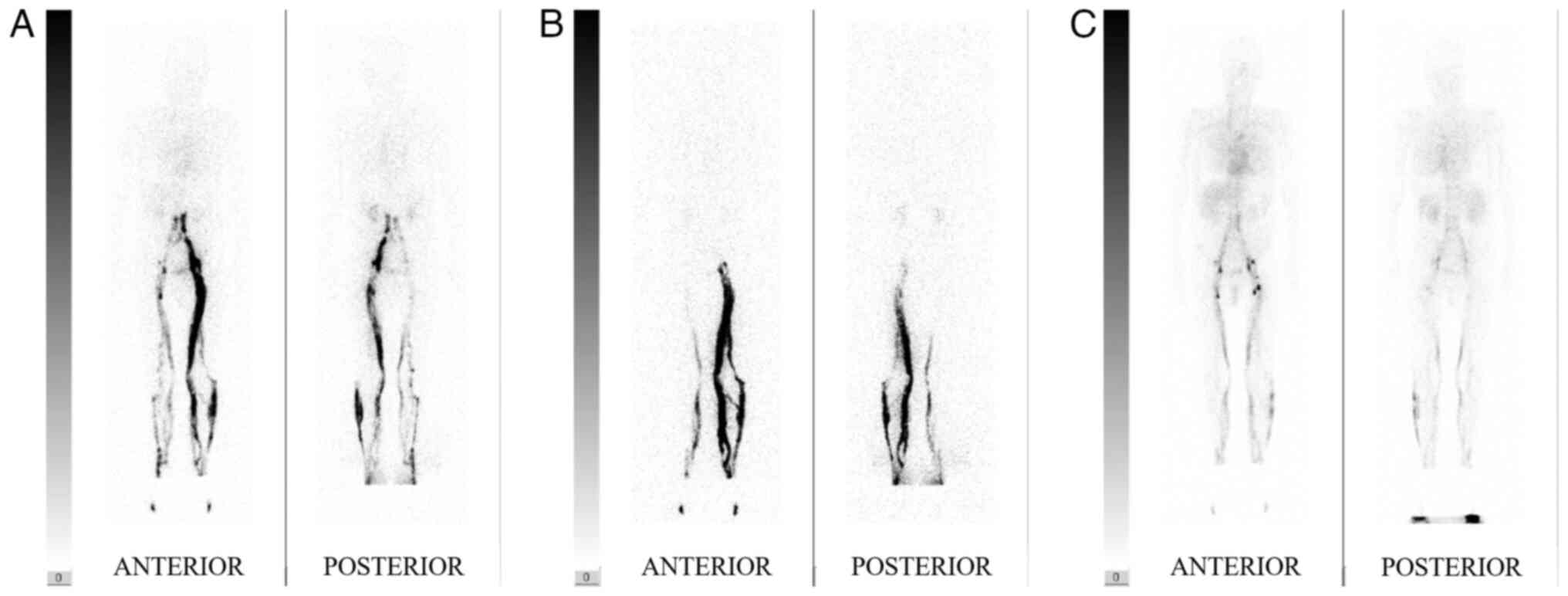
Lymphatic scintigraphy confirmed congestion of lymphatic perfusion
(Fig. 3).
To investigate the cause of the pleural effusion,
bilateral thoracentesis was performed several times. In addition,
CT-guided anterior mediastinal biopsy and thoracoscopic left
pleural biopsy were performed for histological examination.
However, all tests only showed infiltration of lymphocytes with
poor atypia and no definitive diagnosis was made. Since the
tuberculosis-specific enzyme-linked immunospot assay (T-SPOT.TB;
LSI Medience Corporation; performed according to the manufacturer's
protocol) was positive in this case, tuberculous pleurisy could not
be ruled out and it was decided that anti-tuberculosis treatment
was appropriate. However, despite attempts at anti-tuberculosis
drug therapy, consisting of isoniazid (300 mg/day), rifampicin (600
mg/day), ethambutol (750 mg/day) and pyrazinamide (1,500 mg/day)
for 6 weeks, along with antibiotics (0.5 g doripenem every 8 h for
2 weeks, followed by 4.5 g tazobactam/piperacillin every 8 h for 2
weeks), the pleural effusion showed an increasing tendency and the
general condition worsened due to inadequate dietary intake caused
as a side effect of anti-tuberculosis treatment. Finally, after
blood tests and physical examination confirmed that the patient did
not have autoimmune diseases, which can cause bilateral pleural
effusions, and was not using drugs such as bucillamine, which can
cause secondary YNS, and based on the aforementioned results and
yellowing and growth retardation of the toenails, the patient was
diagnosed with YNS. Since the general condition of the patient had
worsened, pleurodesis for bilateral pleural effusion was considered
to be dangerous due to the possibility of severe deterioration in
respiratory function and further deterioration in their ability to
perform daily activities. Hence, based on the high serum sIL-2R
level and lymphocyte-dominant exudative pleural fluid, 30 mg/day
prednisolone was initiated on the assumption that lymphatic
congestion and lymphocyte activation were involved in the
pathology. After continuing the initial prednisolone dose for 2
weeks, it was gradually tapered in 5 mg/day decrements every week
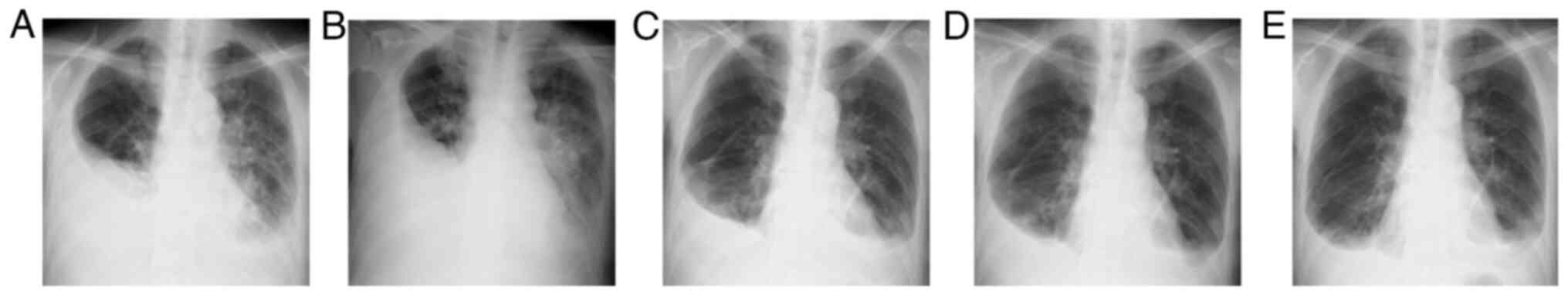
for 3 weeks, to a dose of 15 mg/day. With this treatment, the
bilateral pleural effusion, which had increased before starting
prednisolone, showed a consistent decrease (Fig. 4), with an improvement in general
condition and respiratory symptoms. The patient was subsequently
transferred to Moriya Daiichi General Hospital (Ibaraki, Japan) for
rehabilitation. The dose of prednisolone was finally reduced to 7.5
mg/day with good control of the disease with this dose. The patient
has developed no apparent adverse effects, as far as have been
observed until August 2023.
Discussion
YNS is a relatively rare syndrome proposed by Samman
and White in 1964(1).
Administration of vitamin E and topical steroid injections have
been reported to be effective for the treatment of yellowing nails
(2). Although azole antifungal
drugs (11), clarithromycin
(12) and octreotide (13) have been reported to be potentially
effective and safe systemic treatments, none of them are
established treatments. YNS is a disease diagnosed by yellow nails
with lymphedema and/or chronic respiratory findings, with no
specific findings on hematologic examination. The present case
exhibited mild hypoalbuminemia, but this is not necessarily a
specific finding. Maldonado et al (14) reported that 97% of patients with
YNS have normal albumin levels. In addition, bilateral pleural
effusion has been observed in 68.3% of patients with YNS, with most
being exudative pleural fluid with a predominant lymphocyte
fraction (2). Although its exact
etiology is unknown, lymphatic congestion is presumed to be the
cause of the pleural effusion (2),
and the lymphoscintigraphy performed in the present study showed
delayed drainage of contrast media. However, similar findings are
also seen in other diseases, such as lymphangiogenic dysplasia,
impaired lymphatic transport and lymphatic disorders in congenital
heart diseases (15).
Elevated serum sIL-2R levels are well known to be
present in patients with malignant lymphoma and this test is used
for the auxiliary diagnosis of malignant lymphoma (16). The mechanism by which the serum
level of sIL-2R increases is supposedly derived from the
extracellular release of sIL-2R and release of the α-chain of its
soluble component when antigen-activated T cells express
IL-2(17). Therefore, an increase
in serum sIL-2R is not specific for malignant lymphoma and it has
been suggested to reflect activation of the immune defense
mechanism in diseases involving T-cell activation (17). Elevated serum sIL-2R levels in
association with T-cell activation have been reported in diseases
such as sarcoidosis, rheumatoid arthritis, systemic lupus
erythematosus and tuberculosis (6-8,18,19).
In order to investigate the state of T-cell activation in the
present patient, the serum sIL-2R levels were evaluated and their
elevation was confirmed. To the best of our knowledge, there is
only one previous report that investigated serum sIL-2R levels in a
patient with YNS. Watanabe et al (9) detected elevated serum sIL-2R
measurements (877 IU/ml) in a patient with YNS and pleural
effusion. This previous study suggested that the mechanism of
pleural fluid retention in YNS may involve activation of pleural
fluid and blood lymphocytes, in addition to congestion of lymphatic
perfusion. The serum sIL-2R level in the present patient was 845
U/ml. Considering the results of the previous study (9) and the course of the present patient,
an increase in serum sIL-2R may be noteworthy from the viewpoint of
the involvement of T cells and activation of the immune defense
mechanism, although its disease specificity is low. In future,
further research on the correlation between elevated serum sIL-2R
and the etiology of YNS may be useful.
No standard therapy has been established for the
treatment of pleural effusion associated with YNS. Although
thoracentesis and pleurodesis have been performed (2,4,5,20,21),
they are not curative and are known to have a number of possible
complications. In particular, since there are patients who develop
serious complications with pleurodesis (22), it is necessary to carefully
consider the indications for this procedure. In the present case,
it was decided that corticosteroids would be administered to the
patient due to their poor physical condition and the possibility
that pleurodesis would result in restrictive ventilatory impairment
that would make discharge difficult. To the best of our knowledge,
there is only one previous report of administration of
corticosteroids to control bilateral pleural effusion in a patient
with YNS, lymphatic congestion and activation of immune defense
mechanisms (23). That patient had
bucillamine-induced YNS (23).
Since there was no improvement despite discontinuation of
bucillamine administration, based on the histopathological findings
showing a similarity to rheumatoid pleurisy, the patient was
administered corticosteroid treatment, resulting in improvement in
both pleurisy and lymphedema (23). The present patient was first
treated with anti-tuberculosis drugs, but they were ineffective and
were discontinued due to side effects. Thereafter, prednisolone was
administered to the patient with caution, based on the evidence of
bilateral lymphocyte-predominant exudative pleural effusion,
pleural biopsy showing lymphocytic infiltration with poor atypia
and high serum levels of sIL-2R. Taking these factors into
consideration, it was concluded that the expected efficacy of
steroid therapy well outweighed the risk of side effects. In the
present patient, the bilateral pleural effusion decreased with
corticosteroid therapy. It was thus hypothesized that steroid
administration might have improved lymphatic congestion and
suppressed lymphocyte activation.
There are several limitations to the present report.
First, a single case study is not sufficient to establish the
efficacy and safety of prednisolone as a treatment for the pleural
pathology of YNS, since it is not representative of the entire
population of patients with YNS and may not consider other factors
that could affect the outcome. Second, it is possible that during
longer term follow-up, patients may develop adverse effects due to
systemic steroid administration. For these reasons, further studies
are needed to validate the efficacy of prednisolone as a treatment
option for YNS.
It is clear that corticosteroids are not a treatment
that should be selected lightly, considering the risk of
exacerbation of infectious diseases caused by a number of pathogens
due to the resultant immunosuppression. Therefore, if appropriate
evaluation of the differential diagnosis is performed, and relief
of lymphatic congestion and inhibition of activation of immune
defense mechanisms are considered beneficial for the patient,
steroids might be an option for the treatment of pleural fluid
associated with YNS. The present study might provide useful
information for physicians who encounter similar patients such us
that described in the present case report.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Author's contributions
NH was responsible for treatment, scans and blood
testing. MT, HM, KK, TY, YK, RS, KY, CT, HS and NH contributed to
the planning, acquisition of data and drafting the manuscript. MT
and HM confirm the authenticity of all the raw data. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report and all accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Samman PD and White WF: The ‘Yellow Nail’
Syndrome. Br J Dermatol. 76:153–157. 1964.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Valdés L, Huggins JT, Gude F, Ferreiro L,
Alvarez-Dobaño JM, Golpe A, Toubes ME, González-Barcala FJ, José ES
and Sahn SA: Characteristics of patients with yellow nail syndrome
and pleural effusion. Respirology. 19:985–992. 2014.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Vignes S and Baran R: Yellow nail
syndrome: A review. Orphanet J Rare Dis. 12(42)2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hillerdal G: Yellow nail syndrome:
Treatment with octreotide. Clin Respir J. 1:120–121.
2007.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Glazer M, Berkman N, Lafair JS and Kramer
MR: Successful talc slurry pleurodesis in patients with
nonmalignant pleural effusion. Chest. 117:1404–1409.
2000.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Symons JA, Wood NC, Di Giovine FS and Duff
GW: Soluble IL-2 receptor in rheumatoid arthritis. Correlation with
disease activity, IL-1 and IL-2 inhibition. J Immunol.
141:2612–2618. 1988.PubMed/NCBI
|
|
7
|
Takahashi S, Setoguchi Y, Nukiwa T and
Kira S: Soluble interleukin-2 receptor in sera of patients with
pulmonary tuberculosis. Chest. 99:310–314. 1991.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Dik WA and Heron M: Clinical significance
of soluble interleukin-2 receptor measurement in immune-mediated
diseases. Neth J Med. 78:220–231. 2020.PubMed/NCBI
|
|
9
|
Watanabe E, Mochiduki Y, Nakahara Y,
Kawamura T and Sasaki S: A case of yellow nail syndrome with
bilateral pleural effusion. Nihon Kokyuki Gakkai Zasshi.
48:458–462. 2010.PubMed/NCBI(In Japanese).
|
|
10
|
Hokari R and Tomioka A: The role of
lymphatics in intestinal inflammation. Inflamm Regen.
41(25)2021.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Baran R and Thomas L: Combination of
fluconazole and alpha-tocopherol in the treatment of yellow nail
syndrome. J Drugs Dermatol. 8:276–278. 2009.PubMed/NCBI
|
|
12
|
Suzuki M, Yoshizawa A, Sugiyama H,
Ichimura Y, Morita A, Takasaki J, Naka G, Hirano S, Izumi S, Takeda
Y, et al: A case of yellow nail syndrome with dramatically improved
nail discoloration by oral clarithromycin. Case Rep Dermatol.
3:251–258. 2011.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Lotfollahi L, Abedini A, Alavi Darazam I,
Kiani A and Fadaii A: Yellow Nail Syndrome: Report of a case
successfully treated with octreotide. Tanaffos. 14:67–71.
2015.PubMed/NCBI
|
|
14
|
Maldonado F, Tazelaar HD, Wang CW and Ryu
JH: Yellow nail syndrome: Analysis of 41 consecutive patients.
Chest. 134:375–381. 2008.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Gaber Y: Diseases of Lymphatics. In:
Braun-Falco´s Dermatology. Plewig G, French L, Ruzicka T, Kaufmann
R, Hertl M (eds). Springer, Berlin, Heidelberg, 2020.
|
|
16
|
Chrobák L: Clinical significance of
soluble interleukin-2 receptor. Acta Medica (Hradec Kralove).
39:3–6. 1996.PubMed/NCBI
|
|
17
|
Caruso C, Candore G, Cigna D, Colucci AT
and Modica MA: Biological significance of soluble IL-2 receptor.
Mediators Inflamm. 2:3–21. 1993.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ina Y, Takada K, Sato T, Yamamoto M, Noda
M and Morishita M: Soluble interleukin 2 receptors in patients with
sarcoidosis. Possible origin. Chest. 102:1128–1133. 1992.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Rubin LA and Nelson DL: The soluble
interleukin-2 receptor: Biology, function and clinical application.
Ann Intern Med. 113:619–627. 1990.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Yamagishi T, Hatanaka N, Kamemura H,
Nakazawa I, Hirano Y, Kodaka N, Miura A, Kitahara A, Sawata T,
Hosaka K and Sanno K: Idiopathic yellow nail syndrome successfully
treated with OK-432. Internal Med. 46:1127–1130. 2007.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Katsura H, Nakagawa K, Iwasaki T, Tamura M
and Nakane S: Thoracoscopic assisted pleuro-peritoneal shunt
placement procedure for patient having refractory pleural effusion:
A case report of ‘yellow-nail syndrome’. Jpn J Chest Surg.
21:565–570. 2007.(in Japanese).
|
|
22
|
Mohs Z, DeVillers M, Ziegler S, Basson MD
and Newman W: Management of malignant pleural effusions in U.S.
Veterans: A retrospective review. Ann Thorac Cardiovasc Surg.
28:420–428. 2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Hase I, Kurasawa K, Takizawa H, Yamaguchi
B, Sakuma H and Ishii Y: Hyperplasia of Lymphoid follicles and
lymphangiectasia in the parietal pleura in bucillamine-induced
yellow nail syndrome. Intern Med. 57:1887–1892. 2018.PubMed/NCBI View Article : Google Scholar
|