|
1
|
Rees DC, Williams TN and Gladwin MT:
Sickle-cell disease. Lancet. 376:2018–2031. 2010.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kochhar M and McGann PT: Sickle cell
disease in India: Not just a mild condition. Br J Haematol.
206:380–381. 2025.PubMed/NCBI View Article : Google Scholar
|
|
3
|
GBD 2021 Sickle Cell Disease
Collaborators. Global, regional, and national prevalence and
mortality burden of sickle cell disease, 2000-2021: A systematic
analysis from the global burden of disease study 2021. Lancet
Haematol. 10:e585–e599. 2023.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sundd P, Gladwin MT and Novelli EM:
Pathophysiology of sickle cell disease. Annu Rev Pathol.
14:263–292. 2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Tentolouris A, Stafylidis C, Siafarikas C,
Dimopoulou MN, Makrodimitri S, Bousi S, Papalexis P, Damaskos C,
Trakas N, Sklapani P, et al: Favorable outcomes of patients with
sickle cell disease hospitalized due to COVID-19: A report of three
cases. Exp Ther Med. 23(338)2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
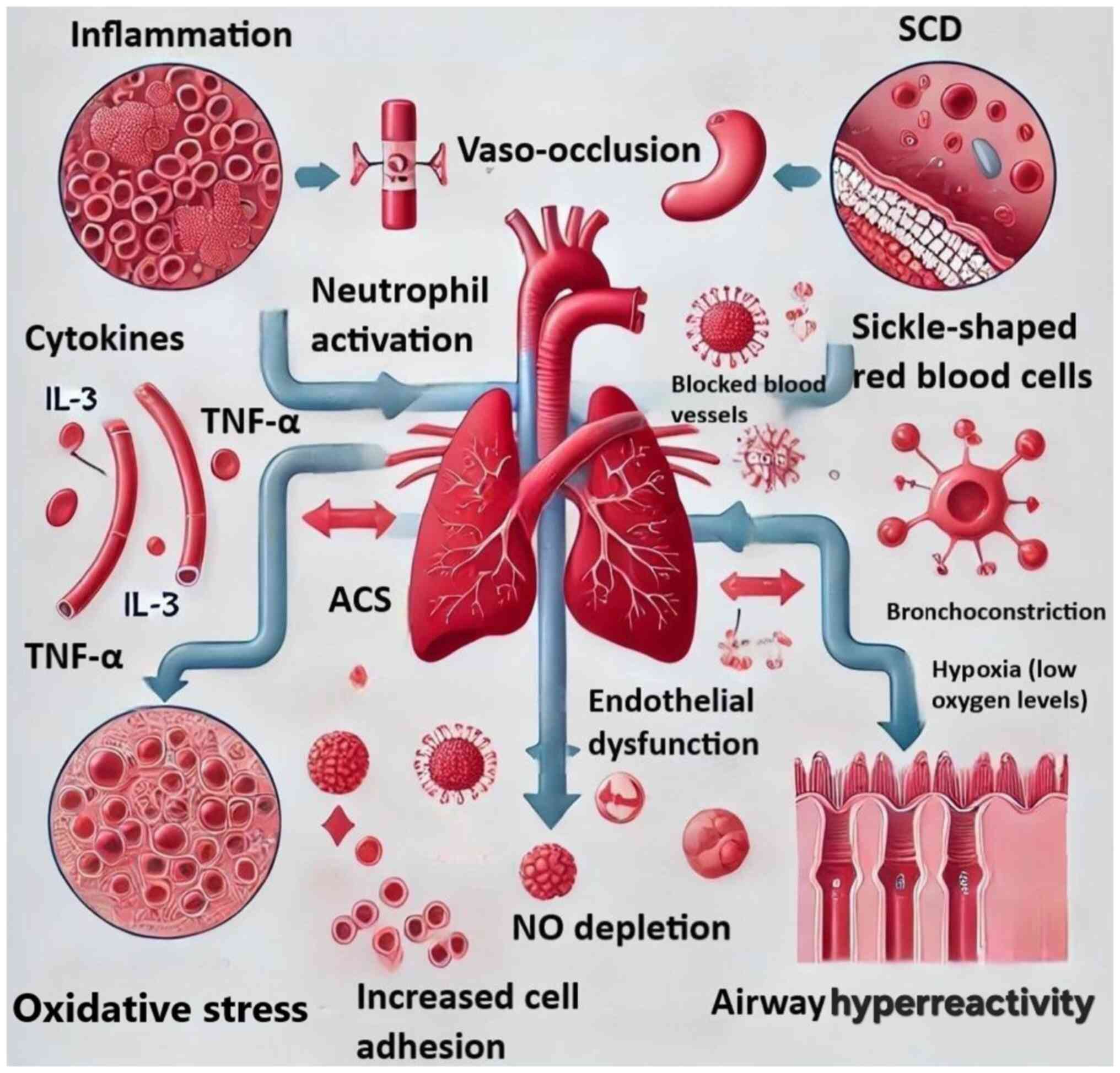
DeBaun MR and Strunk RC: The intersection
between asthma and acute chest syndrome in children with
sickle-cell anaemia. Lancet. 387:2545–2553. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Lunt A, Sturrock SS and Greenough A:
Asthma and the outcome of sickle cell disease. Expert Opin Orphan
Drugs. 6:733–740. 2018.
|
|
8
|
De A, Williams S, Yao Y, Jin Z, Brittenham
GM, Kattan M, Lovinsky-Desir S and Lee MT: Acute chest syndrome,
airway inflammation and lung function in sickle cell disease. PLoS
One. 18(e0283349)2023.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Samarasinghe AE and Rosch JW: Convergence
of inflammatory pathways in allergic asthma and sickle cell
disease. Front Immunol. 10(3058)2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
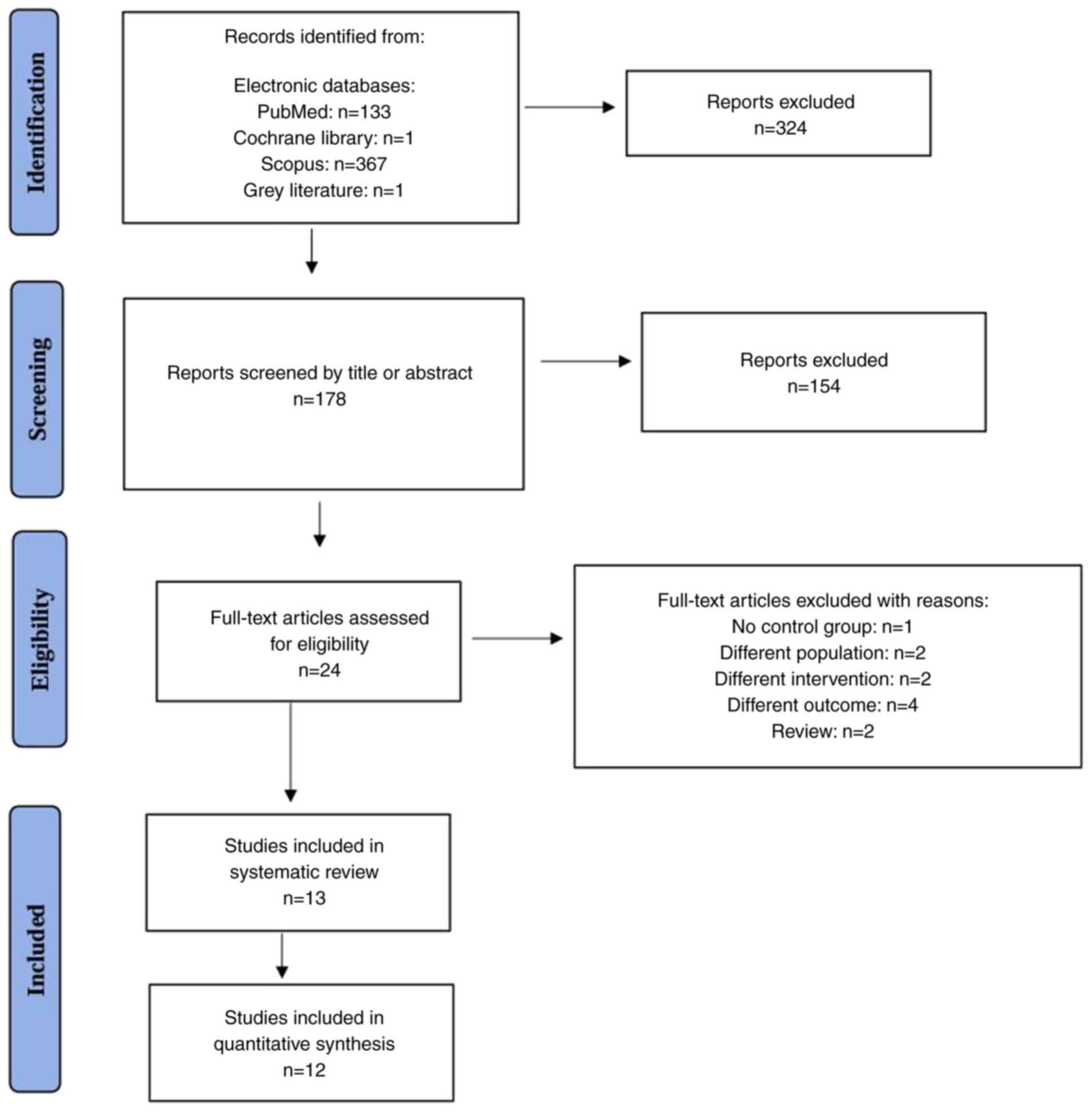
Page MJ, McKenzie JE, Bossuyt PM, Boutron
I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan
SE, et al: The PRISMA 2020 statement: an updated guideline for
reporting systematic reviews. BMJ. 372(n71)2021.PubMed/NCBI View
Article : Google Scholar
|
|
11
|
Stroup DF, Berlin JA, Morton SC, Olkin I,
Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA and Thacker
SB: Meta-analysis of observational studies in epidemiology: A
proposal for reporting. Meta-analysis of observational studies in
epidemiology (MOOSE) group. JAMA. 283:2008–2012. 2000.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wells GA, Shea B, O'Connell D, O'Connell
D, Peterson J, Welch Losos M, Tugwell P, Ga SW, Zello G and
Petersen J: The Newcastle-Ottawa Scale (NOS) for assessing the
quality of nonrandomized studies in meta-analyses. American Academy
of General Practice, Kansas City, MO, 2000.
|
|
13
|
Deeks JJ, Higgins JPT and Altman DG:
Analyzing data and undertaking meta-analyses. Chapter 9: In:
Cochrane Handbook for Systematic Reviews of Interventions. Higgins
JPT and Green S (eds). The Cochrane Collaboration, London,
2011.
|
|
14
|
Meta-Mar. Meta Mar: A tool for
meta-analysis. Available from https://www.meta-mar.com/.
|
|
15
|
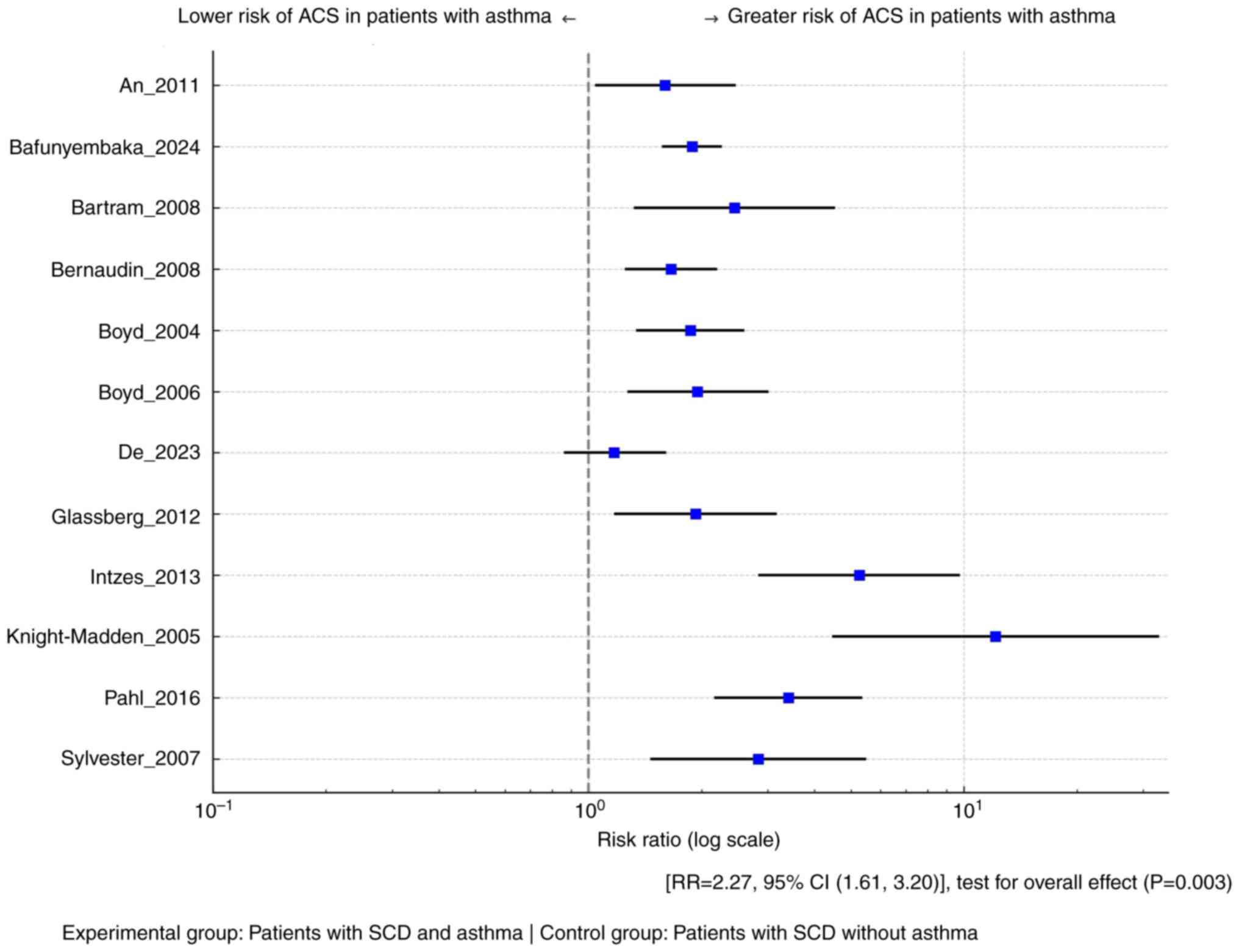
Boyd JH, Moinuddin A, Strunk RC and DeBaun
MR: Asthma and acute chest in sickle-cell disease. Pediatr
Pulmonol. 38:229–232. 2004.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Knight-Madden JM, Forrester TS, Lewis NA
and Greenough A: Asthma in children with sickle cell disease and
its association with acute chest syndrome. Thorax. 60:206–210.
2005.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Boyd JH, Macklin EA, Strunk RC and DeBaun
MR: Asthma is associated with acute chest syndrome and pain in
children with sickle cell anemia. Blood. 108:2923–2927.
2006.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sylvester KP, Patey RA, Broughton S,
Rafferty GF, Rees D, Thein SL and Greenough A: Temporal
relationship of asthma to acute chest syndrome in sickle cell
disease. Pediatr Pulmonol. 42:103–106. 2007.PubMed/NCBI View Article : Google Scholar
|
|
19
|
An P, Barron-Casella EA, Strunk RC,
Hamilton RG, Casella JF and DeBaun MR: Elevation of IgE in children
with sickle cell disease is associated with doctor diagnosis of
asthma and increased morbidity. J Allergy Clin Immunol.
127:1440–1446. 2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Glassberg JA, Chow A, Wisnivesky J,
Hoffman R, Debaun MR and Richardson LD: Wheezing and asthma are
independent risk factors for increased sickle cell disease
morbidity. Br J Haematol. 159:472–479. 2012.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Intzes S, Kalpatthi RV, Short R and Imran
H: Pulmonary function abnormalities and asthma are prevalent in
children with sickle cell disease and are associated with acute
chest syndrome. Pediatr Hematol Oncol. 30:726–732. 2013.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Strunk RC, Cohen RT, Cooper BP, Rodeghier
M, Kirkham FJ, Warner JO, Stocks J, Kirkby J, Roberts I, Rosen CL,
et al: Wheezing symptoms and parental asthma are associated with a
physician diagnosis of asthma in children with sickle cell anemia.
J Pediatr. 164:821–826.e1. 2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Bafunyembaka G, Nacher M, Maniassom C,
Birindwa AM and Elenga N: Asthma is an independent risk factor for
acute chest syndrome in children with sickle cell disease in French
Guiana. Children (Basel). 11(1541)2024.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Bartram JL, Fine-Goulden MR, Green D,
Ahmad R and Inusa BP: Asthma in pediatric sickle cell acute chest
syndrome: In an inner City London hospital. Blood.
112(2481)2008.
|
|
25
|
Bernaudin F, Strunk RC, Kamdem A, Arnaud
C, An P, Torres M, Delacourt C and DeBaun MR: Asthma is associated
with acute chest syndrome, but not with an increased rate of
hospitalization for pain among children in France with sickle cell
anemia: A retrospective cohort study. Haematologica. 93:1917–1918.
2008.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Pahl K and Mullen CA: Original research:
Acute chest syndrome in sickle cell disease: Effect of genotype and
asthma. Exp Biol Med (Maywood). 241:745–758. 2016.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Willen SM, Rodeghier M and DeBaun MR:
Asthma in children with sickle cell disease. Curr Opin Pediatr.
31:349–356. 2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Habib N, Pasha MA and Tang DD: Current
understanding of asthma pathogenesis and biomarkers. Cells.
11(2764)2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Gomez E and Morris CR: Asthma management
in sickle cell disease. Biomed Res Int. 2013(604140)2013.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Miller AC and Gladwin MT: Pulmonary
complications of sickle cell disease. Am J Respir Crit Care Med.
185:1154–1165. 2012.PubMed/NCBI View Article : Google Scholar
|