|
1
|
Maconachie R, Mercer T, Navani N and
McVeigh G: Guideline Committee. Lung cancer: diagnosis and
management: Summary of updated NICE guidance. BMJ.
364(l1049)2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Alexander M, Kim SY and Cheng H:
Management of non-small cell lung cancer. Lung. 198:897–907.
2020.
|
|
3
|
Bray F, Laversanne M, Sung H, Ferlay J,
Siegel RL, Soerjomataram I and Jemal A: Global cancer statistics
2022: GLOBOCAN estimates of incidence and mortality worldwide for
36 cancers in 185 countries. CA Cancer J Clin. 74:229–263.
2024.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Batchelor TJP, Rasburn NJ,
Abdelnour-Berchtold E, Brunelli A, Cerfolio RJ, Gonzalez M,
Ljungqvist O, Petersen RH, Popescu WM, Slinger PD and Naidu B:
Guidelines for enhanced recovery after lung surgery:
Recommendations of the enhanced recovery after surgery
(ERAS®) Society and the European Society of Thoracic
Surgeons (ESTS). Eur J Cardiothorac Surg. 55:91–115.
2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Klapper J and D'Amico TA: VATS versus open
surgery for lung cancer resection: Moving toward a minimally
invasive approach. J Natl Compr Canc Netw. 13:162–164.
2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bendixen M, Jørgensen OD, Kronborg C,
Andersen C and Licht PB: Postoperative pain and quality of life
after lobectomy via video-assisted thoracoscopic surgery or
anterolateral thoracotomy for early-stage lung cancer: A randomised
controlled trial. Lancet Oncol. 17:836–844. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Nagahiro I, Andou A, Aoe M, Sano Y, Date H
and Shimizu N: Pulmonary function, postoperative pain, and serum
cytokine level after lobectomy: A comparison of VATS and
conventional procedure. Ann Thorac Surg. 72:362–365.
2001.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Sandeep B, Huang X, Li Y, Xiong D, Zhu B
and Xiao Z: A comparison of regional anesthesia techniques in
patients undergoing video-assisted thoracic surgery: A network
meta-analysis. Int J Surg. 105(106840)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mathew B, Lennon FE, Siegler J,
Mirzapoiazova T, Mambetsariev N, Sammani S, Gerhold LM, LaRiviere
PJ, Chen CT, Garcia JG, et al: The novel role of the mu opioid
receptor in lung cancer progression: A laboratory investigation.
Anesth Analg. 112:558–567. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Rodrigues P, Bangali H, Hammoud A, Mustafa
YF, Al-Hetty HRAK, Alkhafaji AT, Deorari MM, Al-Taee MM, Zabibah RS
and Alsalamy A: COX 2-inhibitors; a thorough and updated survey
into combinational therapies in cancers. Med Oncol.
41(41)2024.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Steegers MA, Snik DM, Verhagen AF, van der
Drift MA and Wilder-Smith OH: Only half of the chronic pain after
thoracic surgery shows a neuropathic component. J Pain. 9:955–961.
2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Fenta E, Kibret S, Hunie M, Tamire T,
Mekete G, Tiruneh A, Fentie Y, Dessalegn K and Teshome D: The
analgesic efficacy of erector spinae plane block versus
paravertebral block in thoracic surgeries: A meta-analysis. Front
Med (Lausanne). 10(1208325)2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Blanco R, Parras T, McDonnell JG and
Prats-Galino A: Serratus plane block: A novel ultrasound-guided
thoracic wall nerve block. Anaesthesia. 68:1107–1113.
2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Chen N, Qiao Q, Chen R, Xu Q, Zhang Y and
Tian Y: The effect of ultrasound-guided intercostal nerve block,
single-injection erector spinae plane block and multiple-injection
paravertebral block on postoperative analgesia in thoracoscopic
surgery: A randomized, double-blinded, clinical trial. J Clin
Anesth. 59:106–111. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Pei L, Zhou Y, Tan G, Mao F, Yang D, Guan
J, Lin Y, Wang X, Zhang Y, Zhang X, et al: Ultrasound-assisted
thoracic paravertebral block reduces intraoperative opioid
requirement and improves analgesia after breast cancer surgery: A
randomized, controlled, single-center trial. PLoS One.
10(e0142249)2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Gabriel RA, Curran BP, Swisher MW, Sztain
JF, Tsuda PS, Said ET, Alexander B, Finneran JJ IV, Abramson WB,
Black JR, et al: Paravertebral versus Pectoralis-II (Interpectoral
and Pectoserratus) nerve blocks for postoperative analgesia after
nonmastectomy breast surgery: A randomized, controlled,
observer-masked noninferiority trial. Anesthesiology.
141:1039–1050. 2024.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Jackson JC, Tan KS, Pedoto A, Park BJ,
Rusch VW, Jones DR, Zhang H, Desiderio D, Fischer GW and Amar D:
Effects of serratus anterior plane block on early recovery from
thoracoscopic lung resection: A randomized, blinded,
placebo-controlled trial. Anesthesiology. 142(588)2025.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Chi Y, Su X, Liu S, Wen J, Hu M, Li H,
Huang H, Zhang Z and Xie H: Liposomal bupivacaine intercostal nerve
block for pain control in thoracoscopic surgery: A randomized
controlled trial. Front Med (Lausanne). 12(1647324)2025.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Rekatsina M and Peng PWH: The importance
of image guidance in common spine interventional procedures for
pain management: A comprehensive narrative review. Pain Ther.
14:841–863. 2025.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Zhang L, Shen J and Luo Y: The impact of
paravertebral nerve blockade on postoperative surgical site wound
pain management in patients undergoing video-assisted thoracoscopic
surgery for pulmonary carcinoma resection. Int Wound J.
21(e14608)2024.PubMed/NCBI View Article : Google Scholar
|
|
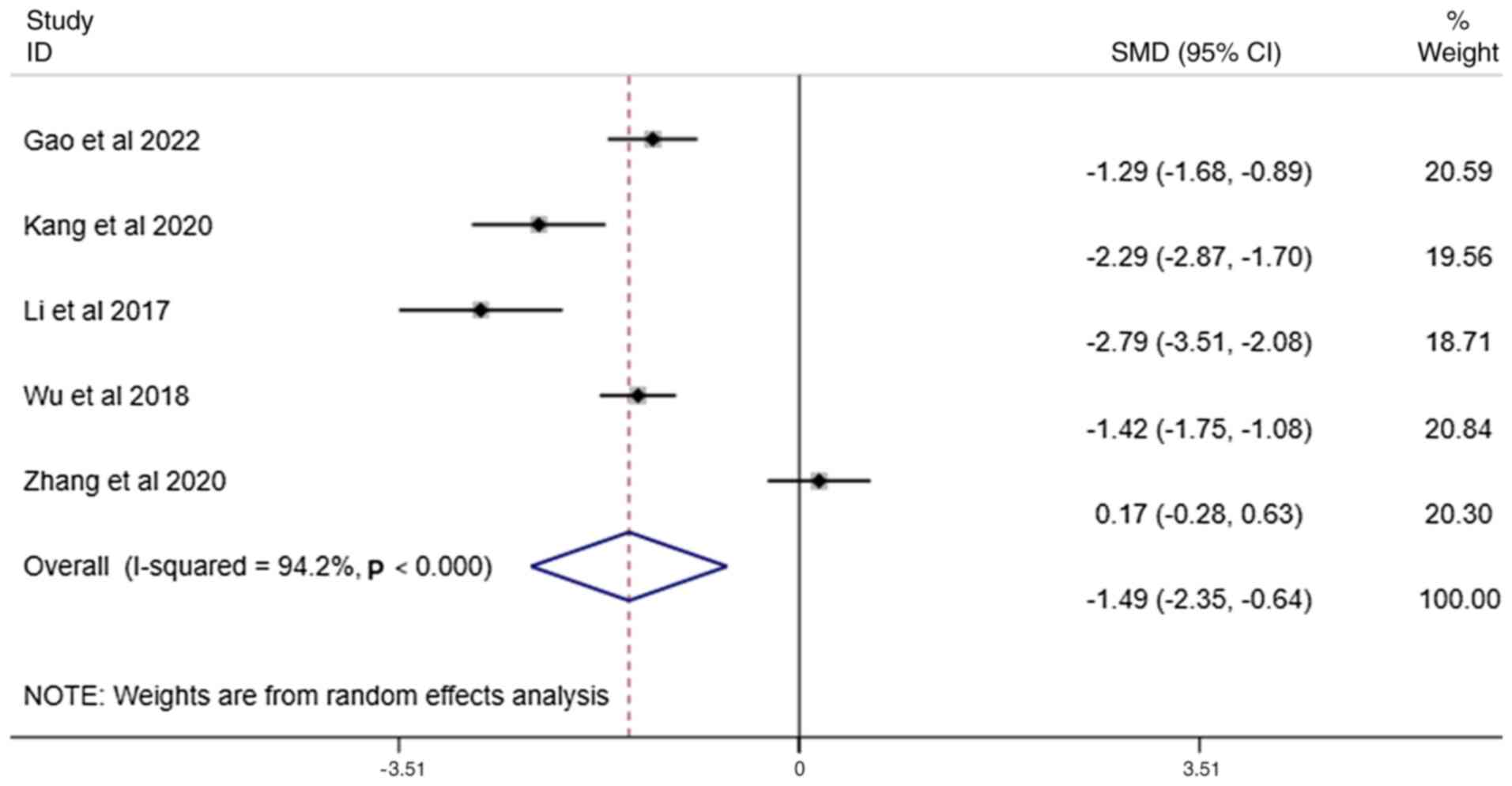
21
|
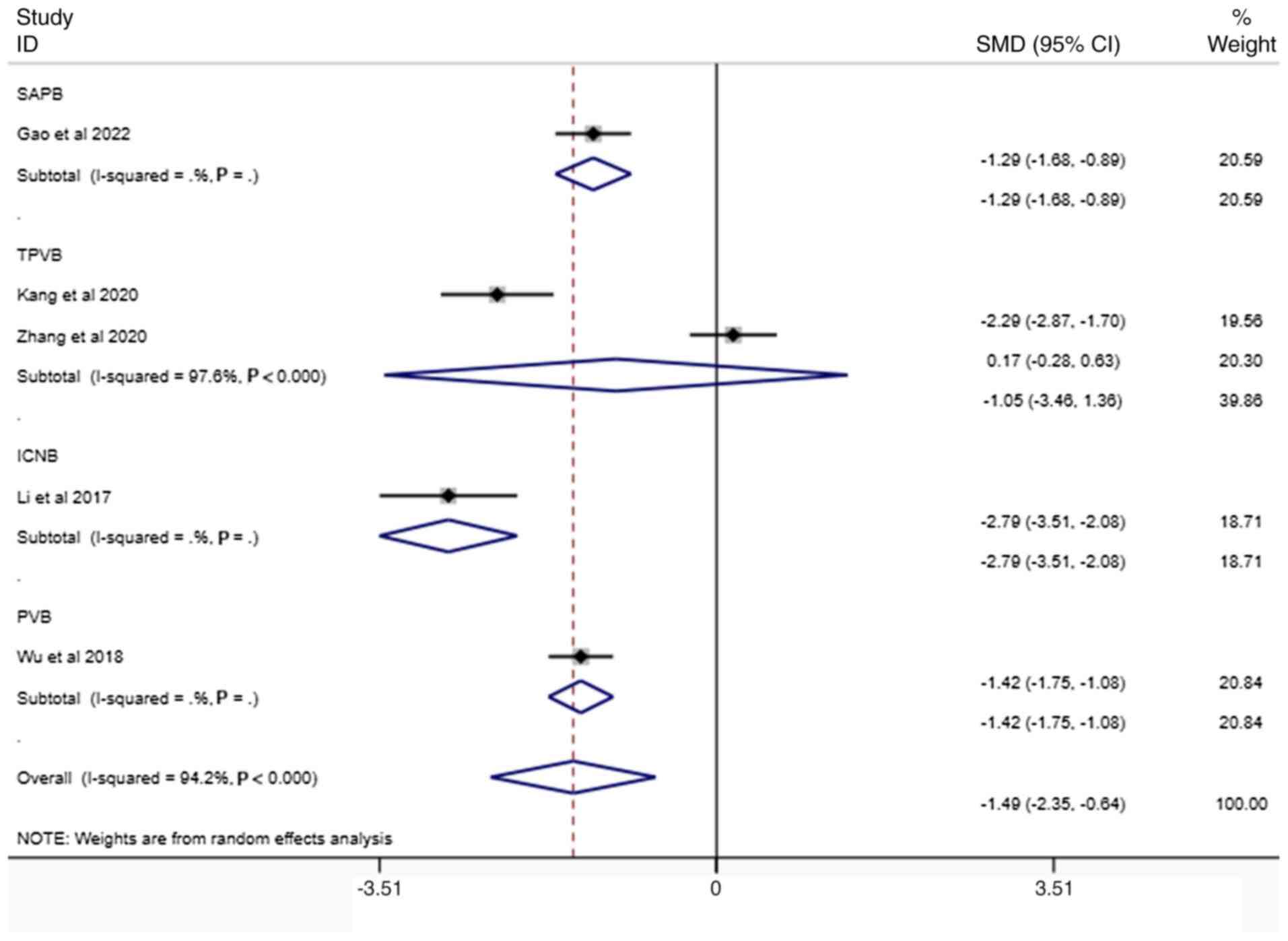
Kang K, Meng X, Li B, Yuan J, Tian E,
Zhang J and Zhang W: Effect of thoracic paravertebral nerve block
on the early postoperative rehabilitation in patients undergoing
thoracoscopic radical lung cancer surgery. World J Surg Oncol.
18(298)2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Li X, Cui X, Zhang S and Fu Z:
Ameliorative effects of parecoxib in combination with
ultrasound-guided paravertebral block (UGPB) on stress and
inflammatory responses following thoracoscopic surgery. Trop J
Pharm Res. 17:1171–1175. 2018.
|
|
23
|
Li Y, Gong L, Xu F, Zhao H, Chen Y and
Wang C: Effects of ropivacaine as intercostal nerve blocker on
postoperative pain after video-assisted thoracic surgery of lung
cancer patients. Chin J Clin Oncol. 44:605–607. 2017.
|
|
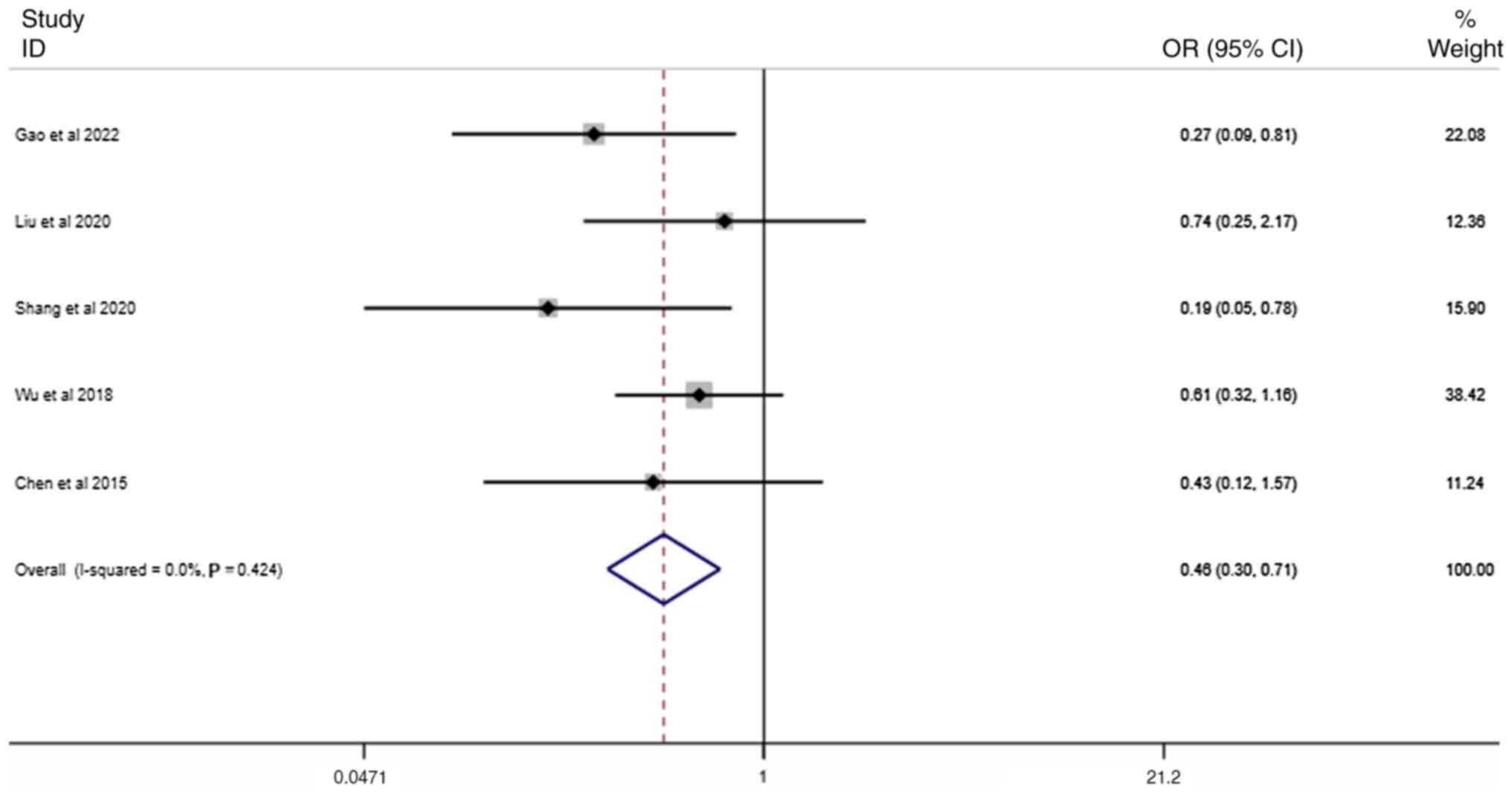
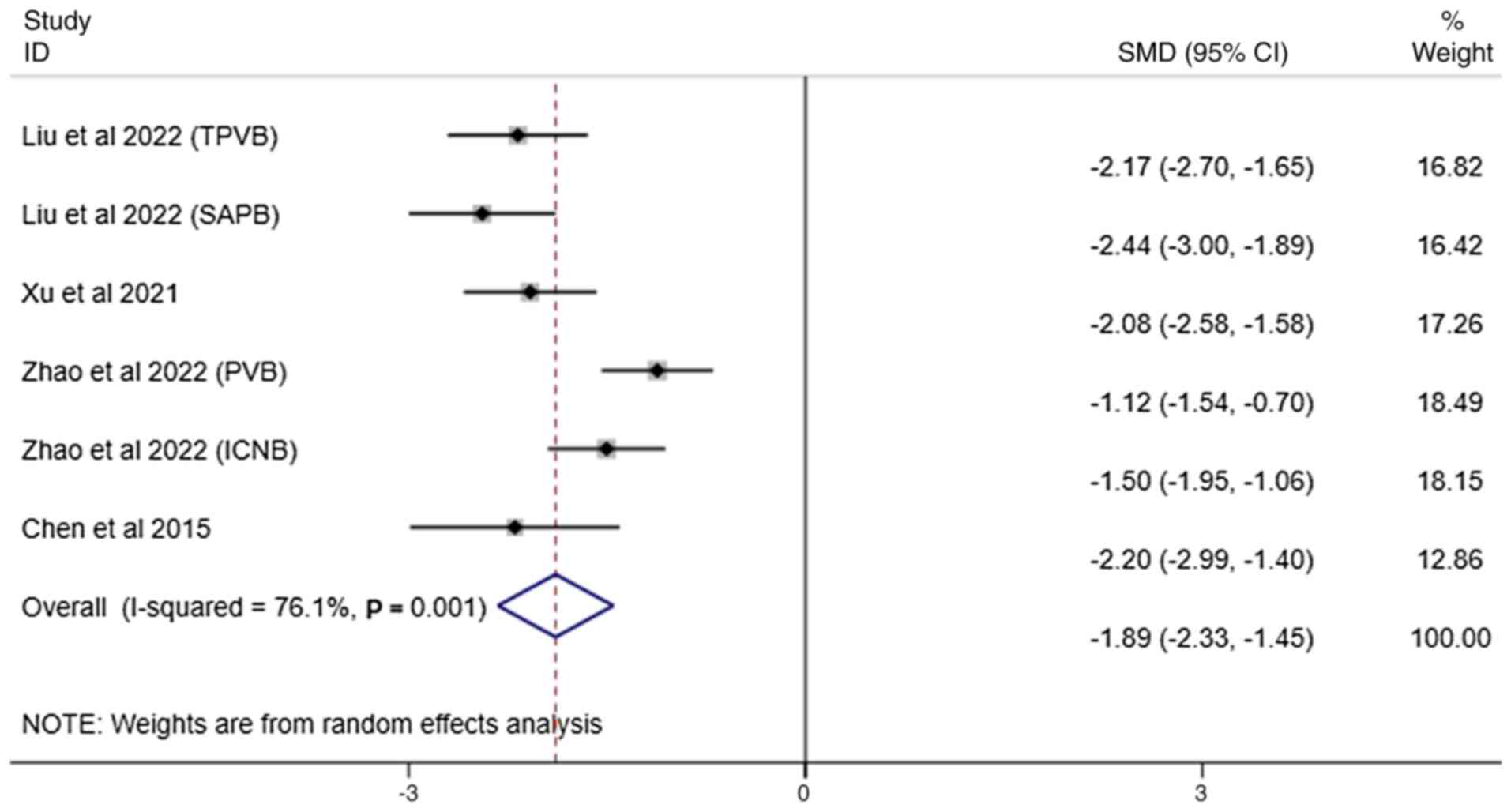
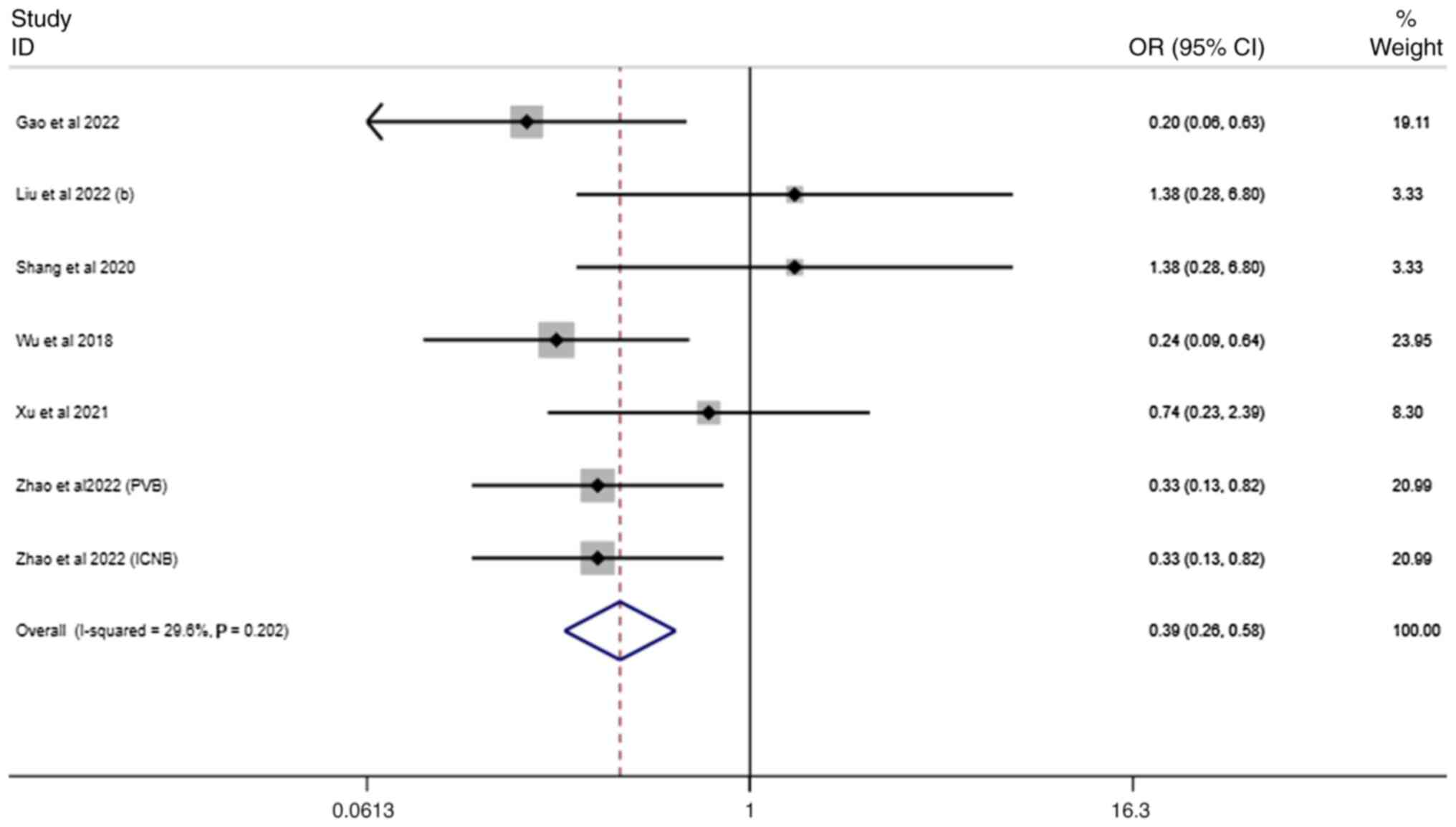
24
|
Liu X and An J: Effects of serratus
anterior plane block and thoracic paravertebral nerve block on
analgesia, immune function and serum tumor markers in patients
after thoracoscopic radical resection of lung cancer. Nagoya J Med
Sci. 84:506–515. 2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Liu Y, Li Y, Wu C and Li H: Effects of
nalbuphine combined with anterior serratus plane block in elderly
patients undergoing thoracoscopic surgery. J Healthc Eng.
2022(7408951)2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Shang LH, Xiao ZN, Zhao YL and Long B:
Analgesic effect of serratus anterior plane block after
thoracoscopic surgery: A randomized controlled double-blinded
study. Ther Clin Risk Manag. 16:1257–1265. 2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Viti A, Bertoglio P, Zamperini M, Tubaro
A, Menestrina N, Bonadiman S, Avesani R, Guerriero M and Terzi A:
Serratus plane block for video-assisted thoracoscopic surgery major
lung resection: A randomized controlled trial. Interact Cardiovasc
Thorac Surg. 30:366–372. 2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Wei W, Zheng X, Gu Y, Fu W, Tang C and Yao
Y: Effect of general anesthesia with thoracic paravertebral block
on postoperative delirium in elderly patients undergoing
thoracoscopic lobectomy: A randomized-controlled trial. BMC
Anesthesiol. 22(1)2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Wu Z, Fang S, Wang Q, Wu C, Zhan T and Wu
M: Patient-controlled paravertebral block for video-assisted
thoracic surgery: A randomized trial. Ann Thorac Surg. 106:888–894.
2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Xu J, Pu M, Xu X, Xiang J and Rong X: The
postoperative analgesic effect of intercostal nerve block and
intravenous patient-controlled analgesia on patients undergoing
lung cancer surgery. Am J Transl Res. 13:9790–9795. 2021.PubMed/NCBI
|
|
31
|
Zhang W, Cong X, Zhang L, Sun M, Li B,
Geng H, Gu J and Zhang J: Effects of thoracic nerve block on
perioperative lung injury, immune function, and recovery after
thoracic surgery. Clin Transl Med. 10(e38)2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Zhao X, Li X, Wang Y, Xiao W, Zhang B,
Meng X and Sun X: Efficacy of intrathoracic intercostal nerve block
on postoperative acute and chronic pains of patients undergoing
video-assisted thoracoscopic surgery. J Pain Res. 15:2273–2281.
2022.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Chen J, Zhang Y, Huang C, Chen K, Fan M
and Fan Z: Effects of thoracic paravertebral block on postoperative
analgesia and serum level of tumor marker in lung cancer patients
undergoing video-assisted thoracoscopic surgery. Zhongguo Fei Ai Za
Zhi. 18:104–109. 2015.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
34
|
Gao W, Yang XL, Hu JC, Gu H, Wu XN, Hu SS,
Wang S, Chai XQ and Wang D: Continuous serratus anterior plane
block improved early pulmonary function after lung cancer surgical
procedure. Ann Thorac Surg. 113:436–443. 2022.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Cumpston M, Li T, Page MJ, Chandler J,
Welch VA, Higgins JP and Thomas J: Updated guidance for trusted
systematic reviews: A new edition of the cochrane handbook for
systematic reviews of interventions. Cochrane Database Syst Rev.
10(ED000142)2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Stogiannis D, Siannis F and Androulakis E:
Heterogeneity in meta-analysis: A comprehensive overview. Int J
Biostat. 20:169–199. 2023.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Planchard D, Popat S, Kerr K, Novello S,
Smit EF, Faivre-Finn C, Mok TS, Reck M, Van Schil PE, Hellmann MD,
et al: Metastatic non-small cell lung cancer: ESMO clinical
practice guidelines for diagnosis, treatment and follow-up. Ann
Oncol. 29:iv192–iv237. 2018.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Polański J, Tański W, Dudek K and
Jankowska-Polańska B: Pain and coping strategies as determinants of
malnutrition risk in lung cancer patients: A cross-sectional study.
Nutrients. 16(2193)2024.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Chou R, Gordon DB, de Leon-Casasola OA,
Rosenberg JM, Bickler S, Brennan T, Carter T, Cassidy CL,
Chittenden EH, Degenhardt E, et al: Management of postoperative
pain: A clinical practice guideline from the American Pain Society,
the American Society of Regional Anesthesia and Pain Medicine, and
the American Society of Anesthesiologists' Committee on Regional
Anesthesia, Executive Committee, and Administrative Council. J
Pain. 17:131–157. 2016.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Hade AD, Okano S, Pelecanos A and Chin A:
. Factors associated with low levels of patient satisfaction
following peripheral nerve block. Anaesth Intensive Care.
49:125–132. 2021.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Chen YK, Boden KA and Schreiber KL: The
role of regional anaesthesia and multimodal analgesia in the
prevention of chronic postoperative pain: A narrative review.
Anaesthesia. 76 (Suppl 1):S8–S17. 2021.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Gouez M, Delrieu L, Bouleuc C, Girard N,
Raynard B and Marchal T: Association between nutritional status and
treatment response and survival in patients treated with
immunotherapy for lung cancer: A retrospective french study.
Cancers (Basel). 14(3439)2022.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Lan T, Chen L and Wei X: Inflammatory
cytokines in cancer: Comprehensive understanding and clinical
progress in gene therapy. Cells. 10(100)2021.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Morrison EJ, Novotny PJ, Sloan JA, Yang P,
Patten CA, Ruddy KJ and Clark MM: Emotional problems, quality of
life, and symptom burden in patients with lung cancer. Clin Lung
Cancer. 18:497–503. 2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Guerra-Londono CE, Privorotskiy A,
Cozowicz C, Hicklen RS, Memtsoudis SG, Mariano ER and Cata JP:
Assessment of intercostal nerve block analgesia for thoracic
surgery: A systematic review and meta-analysis. JAMA Netw Open.
4(e2133394)2021.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Li D, Sun CL, Kim H, Soto-Perez-de-Celis
E, Chung V, Koczywas M, Fakih M, Chao J, Cabrera Chien L, Charles
K, et al: Geriatric assessment-driven intervention (GAIN) on
chemotherapy-related toxic effects in older adults with cancer: A
randomized clinical trial. JAMA Oncol. 7(e214158)2021.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Wolf AMD, Oeffinger KC, Shih TY, Walter
LC, Church TR, Fontham ETH, Elkin EB, Etzioni RD, Guerra CE,
Perkins RB, et al: Screening for lung cancer: 2023 guideline update
from the American Cancer Society. CA Cancer J Clin. 74:50–81.
2024.PubMed/NCBI View Article : Google Scholar
|
|
48
|
de Rooij BH, van den Hurk C, Smaardijk V,
Fernandez-Ortega P, Navarro-Martin A, Barberio L, Guckenberger M,
Schmid S, Walraven I, Vallow S, et al: Development of an updated,
standardized, patient-centered outcome set for lung cancer. Lung
Cancer. 173:5–13. 2022.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Capuano P, Hileman BA, Martucci G, Raffa
GM, Toscano A, Burgio G, Arcadipane A and Kowalewski M: Erector
spinae plane block versus paravertebral block for postoperative
pain management in thoracic surgery: A systematic review and
meta-analysis. Minerva Anestesiol. 89:1042–1050. 2023.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Gonçalves JPF, Duran ML, Barreto ESR,
Antunes Júnior CR, Albuquerque LG, Lins-Kusterer LEF, Azi LMTA and
Kraychete DC: Efficacy of erector spinae plane block for
postoperative pain management: A meta-analysis and trial sequential
analysis of randomized controlled trials.
|