Introduction
Lung cancer presents as a malignant tumor that
originates in the epithelial tissue, it is an aggressive and
prevalent disease worldwide with a high incidence rate, accounting
for 25% of all cancer-associated deaths recorded in 2019(1). Globally, according to 2020
statistics, lung cancer accounts for 12.4% of all cancer cases
worldwide and is the most common cause of cancer-associated
fatalities across all age groups (2,3),
posing a notable threat to human health and wellbeing.
Minimally invasive thoracic surgery has markedly
grown in popularity (4); this
includes video-assisted thoracic surgery (VATS), which has become a
preferred method due to its use of smaller incisions and decreased
impact on surrounding tissues, which collectively result in a
quicker healing process compared with conventional thoracotomy
(5). Despite these advantages,
VATS can lead to acute pain, which has been reported to occur in 50
to 80% of patients, with a substantial subset (30-40%) experiencing
severe intensity (6). This pain
not only slows the functional healing of the patient but also
notably compromises the overall quality of recovery (7). Poor handling of pain escalates the
risks of developing post-operative lung issues (lung parenchyma,
bronchi, pleura), can result in chronic pain conditions and may
lead to an increased reliance on pain medications following surgery
(8), therefore, ensuring pain
relief remains a primary concern for patients undergoing VATS.
Administering opioid medications systemically is the
most common method for mitigating postoperative pain following VATS
surgery, however, these elicit a range of adverse effects,
including postoperative nausea/vomiting and respiratory depression
(9,10). Cyclooxygenase-2 inhibitors have a
notable effect on postoperative analgesia in patients with lung
cancer, however, their clinical application is limited by harmful
side effects at effective drug doses, including renal impairment
and cardiovascular adverse events (11). At present, there is no set
postoperative pain management method for VATS but clinical data
indicate that nerve block procedures offer promising analgesic
effects during VATS (12,13).
Nerve block refers to the injection of local
anesthetic near peripheral nerve trunks and plexuses, cranial nerve
roots, sympathetic ganglia and other neural structures. By
temporarily blocking nerve conduction, this technique achieves
therapeutic goals such as pain relief and improved blood
circulation. Its core principle involves using anesthetic drugs
(such as lidocaine or ropivacaine) to act on nerve roots or axons,
thereby decreasing neural excitability. It can effectively control
pain, decrease perioperative analgesic/anesthetic requirements,
lower rates of postoperative nausea and vomiting, decrease chronic
pain risk, minimize respiratory complications, shorten hospital
stays and improve patient satisfaction (14). Thoracic paravertebral block (TPVB)
achieves unilateral trunk analgesia by injecting local anesthetics
into the thoracic paravertebral space to block the conduction of
corresponding spinal nerves (15).
PVB is an analgesic technique that blocks the corresponding spinal
nerve roots by injecting local anesthetic into the outer orifice of
the intervertebral foramen via a puncture needle (16). Serratus anterior plane block (SAPB)
is a technique that provides dense analgesia to the lateral chest
by blocking the thoracic intercostal nerves, which involves
ultrasound-guided injection of anesthetics into the superficial or
deep layer of the serratus anterior muscle at the level of the 5th
rib on the midaxillary line (17).
Intercostal nerve block (ICNB) via pleural cavity blocks
intercostal nerves by injecting local anesthetics into the pleural
cavity, which act on the ventral branches of the thoracic spinal
nerves running in the costal groove (18). Nerve block can be performed with or
without image guidance, traditional non-image-guided techniques
rely on anatomical landmarks, surface projections and operator
experience to determine the puncture site and depth, which may lead
to inaccurate targeting, inadequate blockade and higher risks of
complications such as vascular injury. By contrast, image-guided
nerve blocks markedly improve procedural safety and efficacy,
primary imaging modalities used for guidance include ultrasound,
fluoroscopy and computed tomography (19). A meta-analysis found that among
patients undergoing VATS for lung cancer resection, paraspinal
nerve block combined with general anesthesia decreased visual
analogue scale (VAS) scores 2-6 h after surgery (20). To the best of our knowledge,
however, there is a lack of relevant and comprehensive evaluations
of pain management methods. Therefore, the aim of the present
meta-analysis was to evaluate the efficacy and safety of nerve
block surgery for postoperative analgesia in lung cancer and
support evidence-based medicine for the clinical treatment of
postoperative pain following VATS in patients with lung cancer.
Materials and methods
Search strategy
Electronic databases, including Web of Science
(https://www.webofscience.com), Embase
(https://www.embase.com) and Cochrane (https://www.cochranelibrary.com) were
systematically searched from the establishment of the database to
April 2024, using the search terms ‘nerve block’, ‘chemical
neurolysis’, ‘chemo denervation’, ‘cancer of the lung’, ‘nerve
blockades’, ‘lung neoplasm’, ‘lung cancer’, ‘pulmonary neoplasms’,
‘pulmonary cancers’ and ‘pain’. The search strategy for Cochrane
Library, which was also applied to the other databases, is shown in
Table I.
 | Table ISearch strategy in the Cochrane
Library. |
Table I
Search strategy in the Cochrane
Library.
| Order | Search items |
|---|
| #1 |
(pain):ti,ab,kw |
| #2 | (nerve block or
nerve Blockades or chemical Neurolysis or
Chemodenervation):ti,ab,kw |
| #3 | (lung neoplasms or
pulmonary neoplasms or cancers, lung or pulmonary cancers or cancer
of the lung):ti,ab,kw |
| #4 | #1 AND #2 AND
#3 |
Study selection criteria. Types of
study
All randomized clinical trials (RCTs) of nerve block
in postoperative analgesia in patients with lung cancer, whether
single-blinded or double-blinded, were included. Both guided and
non-guided nerve block were included and the data were not
extracted separately. All patients included in the analysis were
diagnosed with lung cancer, with no exclusion based on age, sex,
ethnicity or course of disease. All the patients received lung
cancer surgery (thoracoscopic or thoracotomy). The treatment plan
was nerve block, which included TPVB, PVB, SAPB or ICNB, and the
comparators were standard analgesic therapies, which were standard
opioid-based multi-modal analgesia, including intravenous
sufentanil for intra- and post-operative pain. The search
strategies were based on the population, interventions,
comparators, outcomes and study design framework, and the findings
were reported in alignment with the protocols established by the
preferred reporting items for systematic reviews and meta-analyses
guidelines (Table II).
 | Table IISurgical information from the
included studies. |
Table II
Surgical information from the
included studies.
| First author,
year | Anesthesia | Background
analgesic modality | Type of nerve
block | Outcomes | Pain scale | ASA stage | (Refs.) |
|---|
| Kang et al,
2020 | GA | PCA | TPVB | VAS score,
incidence of postoperative adverse reactions | VAS | I-III | (21) |
| Li et al,
2018 | GA | N/A | PVB | VAS score | VAS | I-II | (22) |
| Li et al,
2017 | GA | PCA | ICNB | VAS score, number
of patients requiring additional postoperative analgesic, incidence
of postoperative adverse reactions | VAS | I-II | (23) |
| Liu et al,
2022 (A) | GA | PCA | TPVB, SAPB | VAS score, number
of administrations of patient-controlled analgesia | VAS | I-II | (24) |
| Liu et al,
2022 (B) | N/A | N/A | SAPB | Incidence of
postoperative adverse reactions | VAS | N/A | (25) |
| Shang et al,
2020 | GA | PCA | SAPB | Number of patients
requiring additional postoperative analgesic, incidence of
postoperative adverse reactions | VAS | I-III | (26) |
| Viti et al,
2022 | GA | N/A | SAPB | Number of patients
requiring additional postoperative analgesic | NRS | N/A | (27) |
| Wei et al,
2022 | GA | PCA | PVB | VAS score,
incidence of postoperative adverse reactions | VAS | I-III | (28) |
| Wu et al,
2018 | GA | PCA | PVB | VAS score, number
of patients requiring additional postoperative analgesic, incidence
of postoperative adverse reactions | VAS | N/A | (29) |
| Xu et al,
2021 | GA | PCA | ICNB | VAS score, number
of administrations of patient-controlled analgesia, incidence of
postoperative adverse reactions | VAS | I-II | (30) |
| Zhang et al,
2020 | GA | PCA | TPVB | VAS score | VAS | I-II | (31) |
| Zhao et al,
2022 | GA | PCA | PVB, ICNB | VAS score, number
of administrations of patient-controlled analgesia, incidence of
postoperative adverse reactions | VAS | I-II | (32) |
| Chen et al,
2015 | GA | PCA | PVB | VAS score, number
of patients requiring additional postoperative analgesic, number of
administrations of patient-controlled analgesia | VAS | I-II | (33) |
| Gao et al,
2022 | GA | PCA | SAPB | VAS score, number
of patients requiring additional postoperative analgesic, incidence
of postoperative adverse reactions | VAS | II-III | (34) |
Outcome measures. The primary outcome measure
was the VAS score used to assess pain intensity at 24, 48 and 72 h
following completion of surgery at rest, and the secondary outcome
indicators were the number of times the button on the
patient-controlled analgesia instrument was pressed at 24 h
following surgery, the dosage of analgesics at 48 h after surgery
and adverse reactions. In the presence of substantial
heterogeneity, subgroup analysis is warranted.
Exclusion criteria. The exclusion criteria
were as follows: i) RCTs comparing two types of nerve block
surgery, ii) non-RCTs, iii) duplicated data and iv) invalid outcome
indices.
Study selection
The literature search results were independently
assessed by two researchers according to the inclusion criteria.
All documents obtained from the databases were imported into
EndNote X9 (Clarivate) to exclude duplicate documents. The titles
and abstracts were assessed for initial screening. Of the remaining
studies, the full text was read and the final studies for inclusion
were discussed. Discrepancies were resolved by discussion with a
third examiner. Author name, publication year, anesthesia types,
outcomes, pain rating scales and American Society of
Anesthesiologists stage was collected from all the included
studies.
Statistical analysis
Stata version 16.0 (StataCorp LP) was used to
analyze the results. Dichotomous and continuous data are presented
as the relative risk and mean difference, respectively, with 95%
confidence intervals. P<0.05 was considered to indicate
statistical significance. The random-effects model was used for
meta-analysis, regardless of the I2 values.
Results
Search results and characteristics of
studies
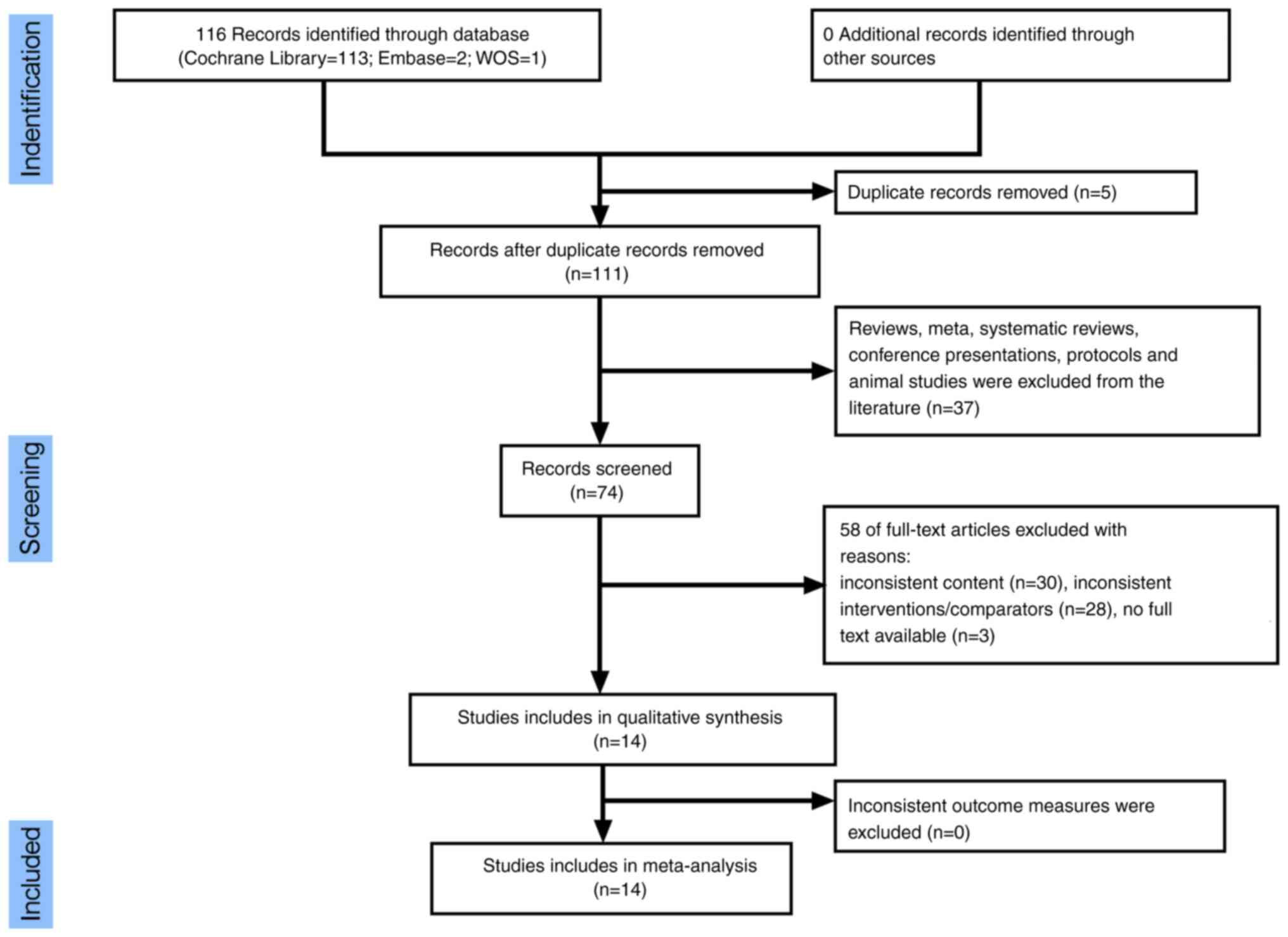
The literature search identified 116 articles, of
which five duplicates were removed. After reviewing the titles and
abstracts of the remaining articles, 37 articles were excluded
according to the inclusion and exclusion criteria, leaving 58 full
texts. After assessing the full texts, 14 studies were deemed to
meet the inclusion criteria (Fig.
1, Table III) (21-34).
 | Table IIICharacteristics of the included
studies. |
Table III
Characteristics of the included
studies.
| | Number of
patients | Age, years | Sex,
male/female | |
|---|
| First author,
year | Country | Experimental | Control | Experimental | Control | Experimental | Control | (Refs.) |
|---|
| Kang et al,
2020 | China | 41 | 34 | 51.60±11.00 | 56.10±9.80 | 21/20 | 16/18 | (21) |
| Li et al,
2018 | China | 20 | 20 | 59.40±10.77 | 54.80±13.02 | 8/12 | 9/11 | (22) |
| Li et al,
2017 | China | 30 | 30 | 23-77 | 23-77 | 35 | 25 | (23) |
| Liu et al,
2022 (A) | China | 44 (TPVB); 44
(SAPB) | 44 | 59.23±9.71;
59.16±9.68 | 58.95±9.64 | 29/15; 28/16 | 26/18 | (24) |
| Liu et al,
2022 (B) | China | 30 | 30 | 56.21±7.21 | 58.21±9.02 | 15/15 | 13/17 | (25) |
| Shang et al,
2020 | China | 30 | 30 | 56.20±7.20 | 58.23±9.03 | 15/15 | 17/13 | (26) |
| Viti et al,
2022 | Italy | 46 | 44 | 67.80±9.30 | 71.00±7.90 | 28/18 | 30/14 | (27) |
| Wei et al,
2022 | China | 170 | 168 | 76.20±6.30 | 73.50±7.10 | 83/87 | 80/88 | (28) |
| Wu et al,
2018 | China | 86 | 85 | 58.00 | 58.00 | 42/44 | 49/36 | (29) |
| Xu et al,
2021 | China | 50 | 45 | 51.28±6.39 | 50.97±7.20 | 31/19 | 30/15 | (30) |
| Zhang et al,
2020 | China | 38 | 37 | 56.00±15.00 | 50.00±13.00 | 18/24 | 19/22 | (31) |
| Zhao et al,
2022 | China | 50 (PVB); 50
(ICNB) | 50 | 52.44±9.22;
54.98±10.94 | 51.82±11.37 | 29/21, 25/25 | 28/21 | (32) |
| Chen et al,
2015 | China | 20 | 20 | 53.00±12.00 | 55.00±11.00 | 11/9 | 12/8 | (33) |
| Gao et al,
2022 | China | 60 | 60 | 55.40±11.10 | 57.20±10.30 | 33/22 | 32/21 | (34) |
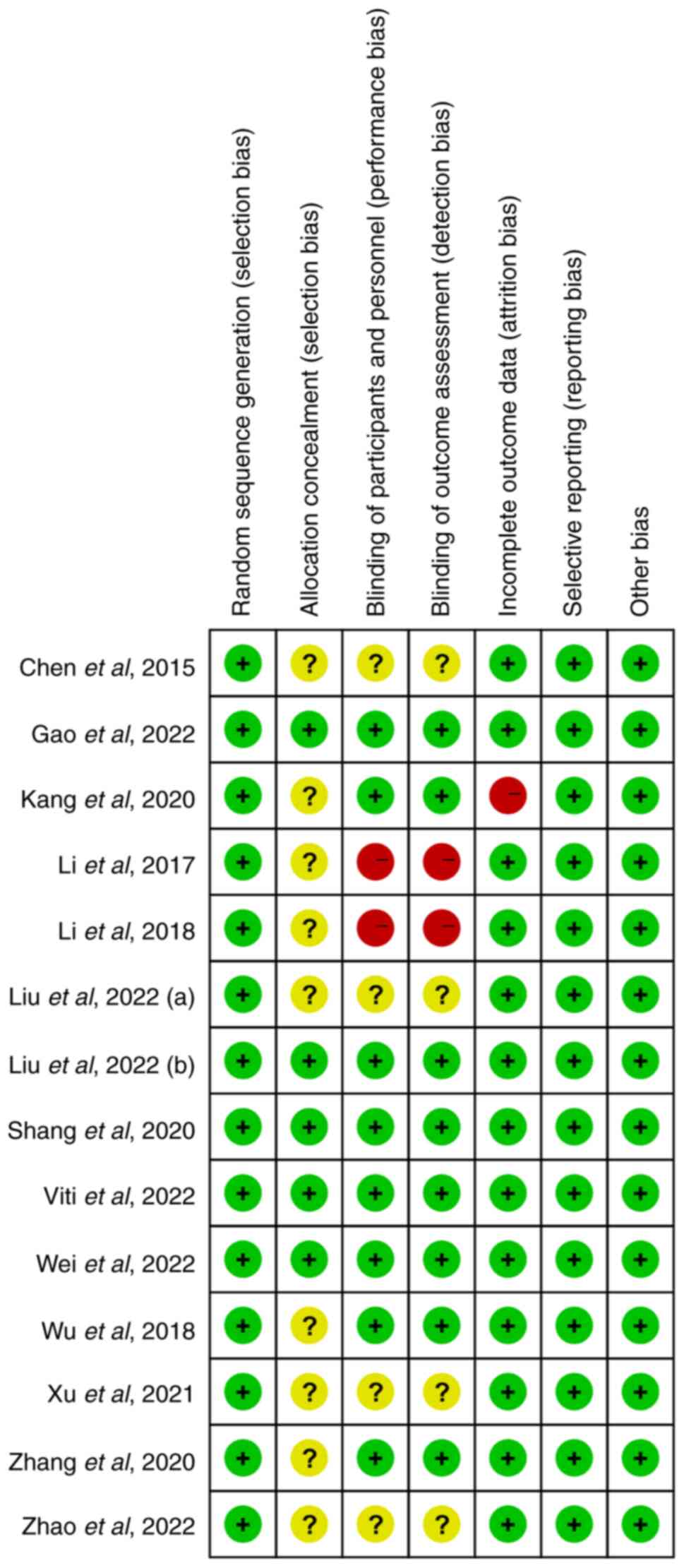
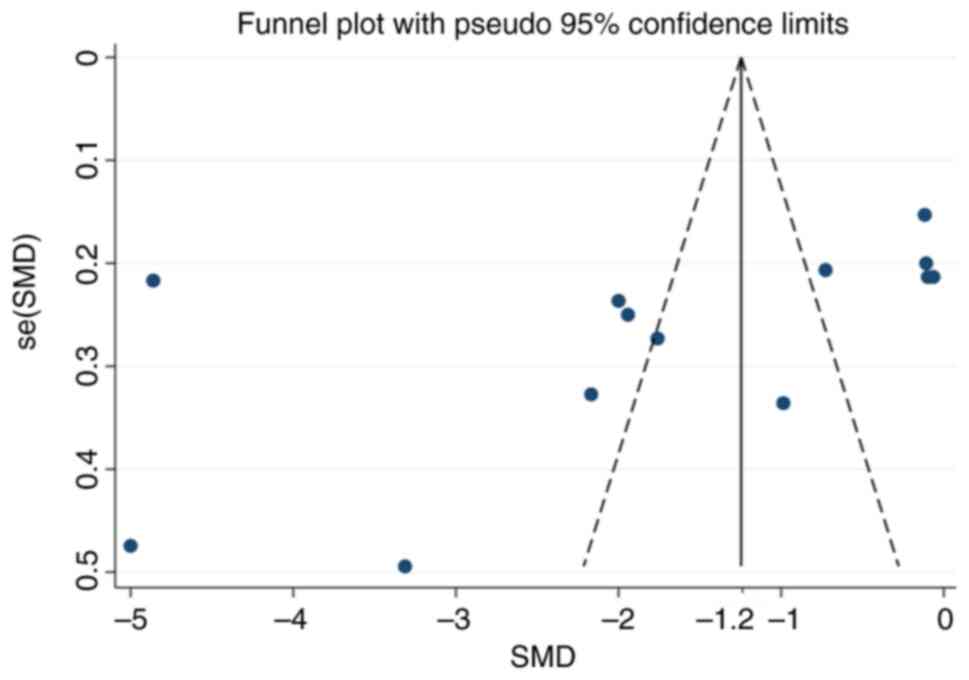
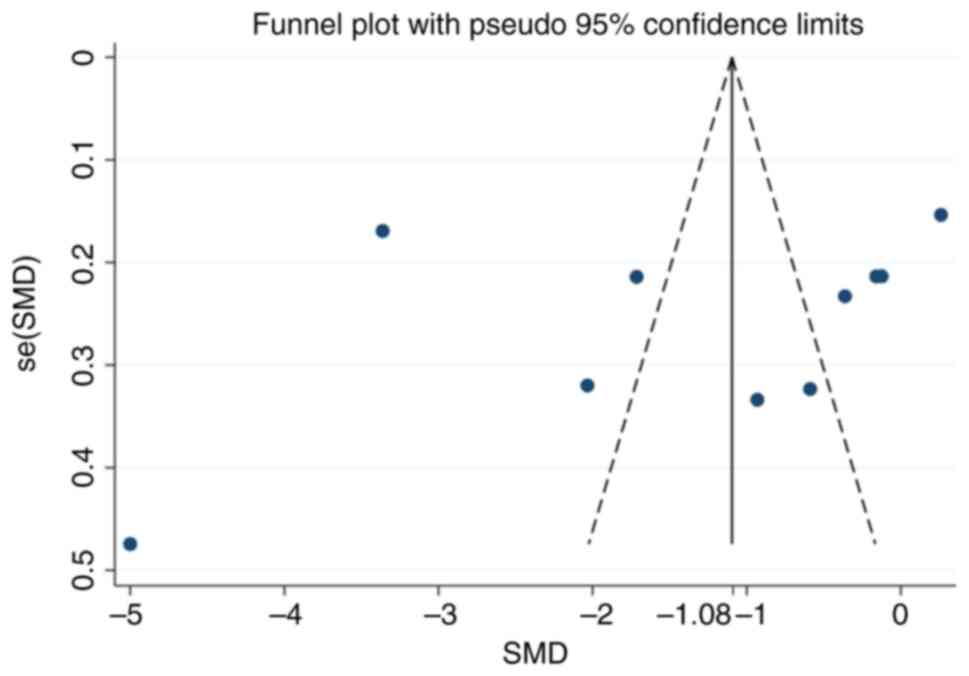
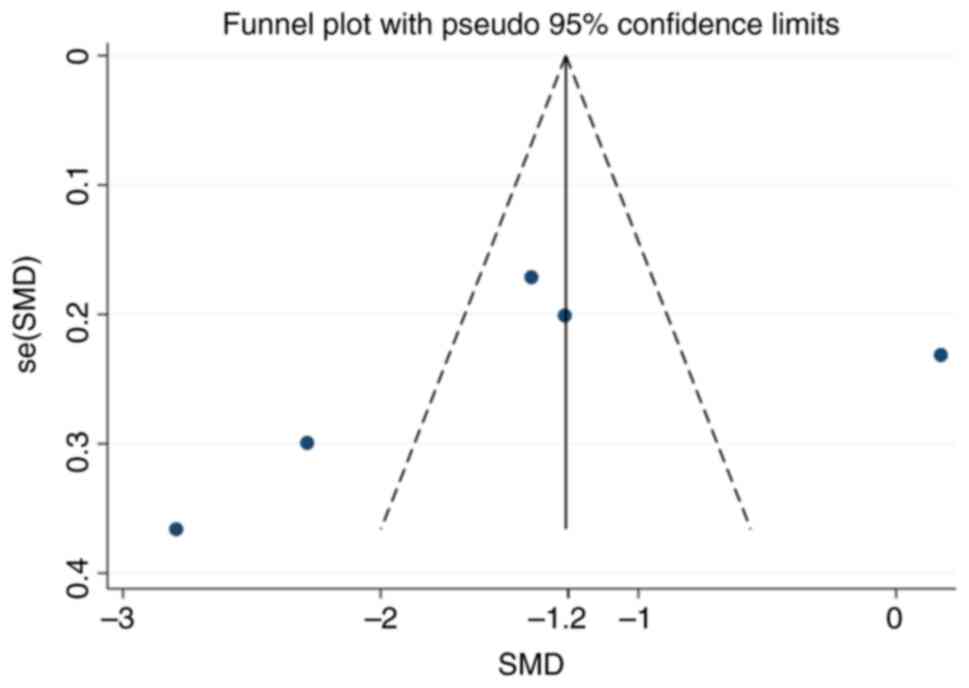
Risk of bias assessment
Using the Cochrane risk of bias tool, the risk of
bias was rated as low, unclear or high independently by two
researchers. This included random sequence generation, allocation
concealment, blinding of participants and personnel, blinding of
outcome assessments, incomplete outcome data, selective reporting
and other sources of bias. Discrepancies were resolved by a third
reviewer. The symmetry of the funnel plot demonstrated that there
was no publication bias. The risk of bias assessment is summarized
in Fig. 2, which indicated that
the included studies exhibited the lowest risk of bias in random
sequence generation and completeness of outcome data, while
demonstrating the highest risk of bias in blinding of investigators
and participants (performance bias). Other domains, such as
allocation concealment and selective reporting, showed overall
lower risk of bias. This meta-analysis included 14 studies, of
which 3 had at least one study with a risk of partial bias. The
remaining 11 studies did not explicitly report details regarding
the implementation of randomization and blinding.
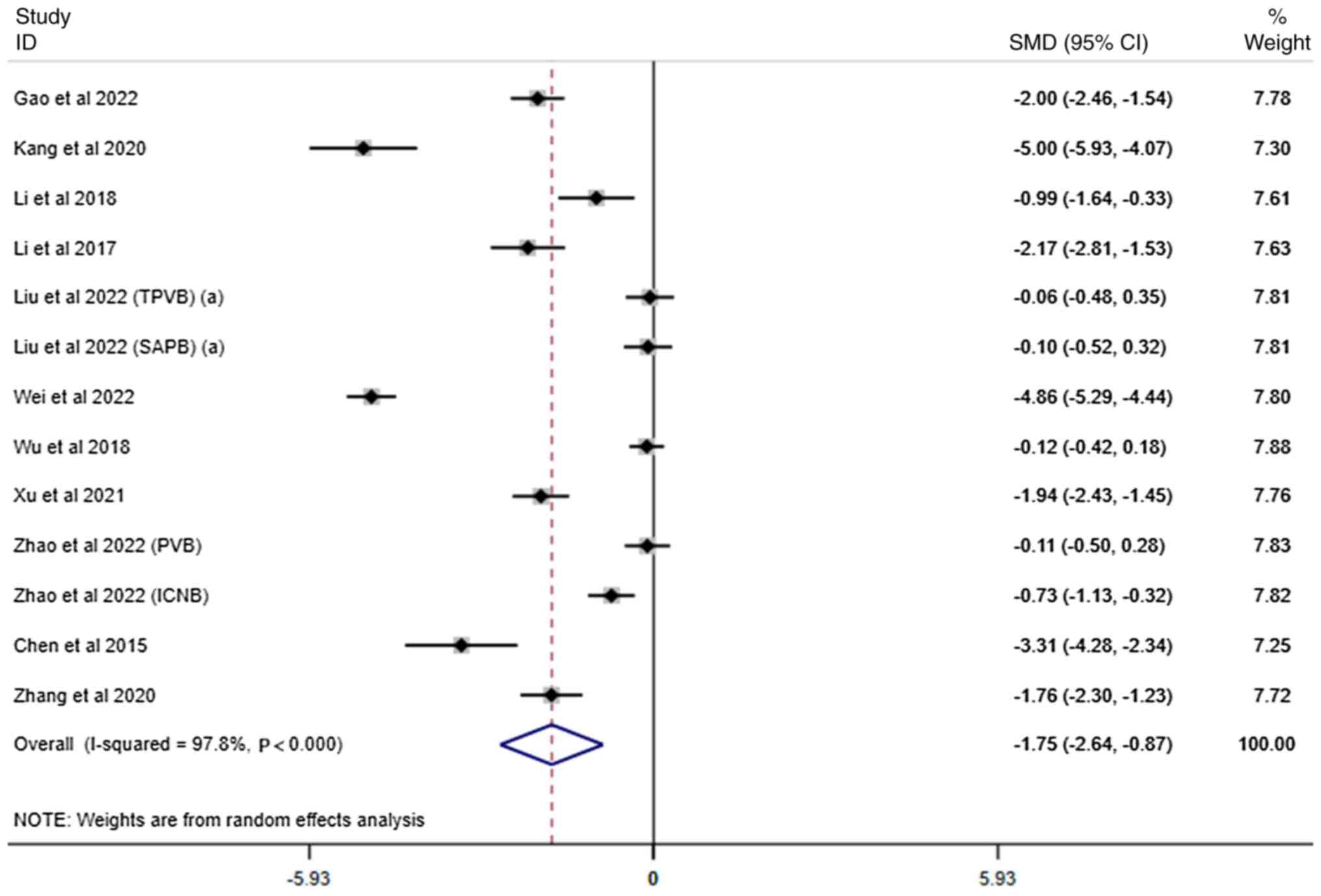
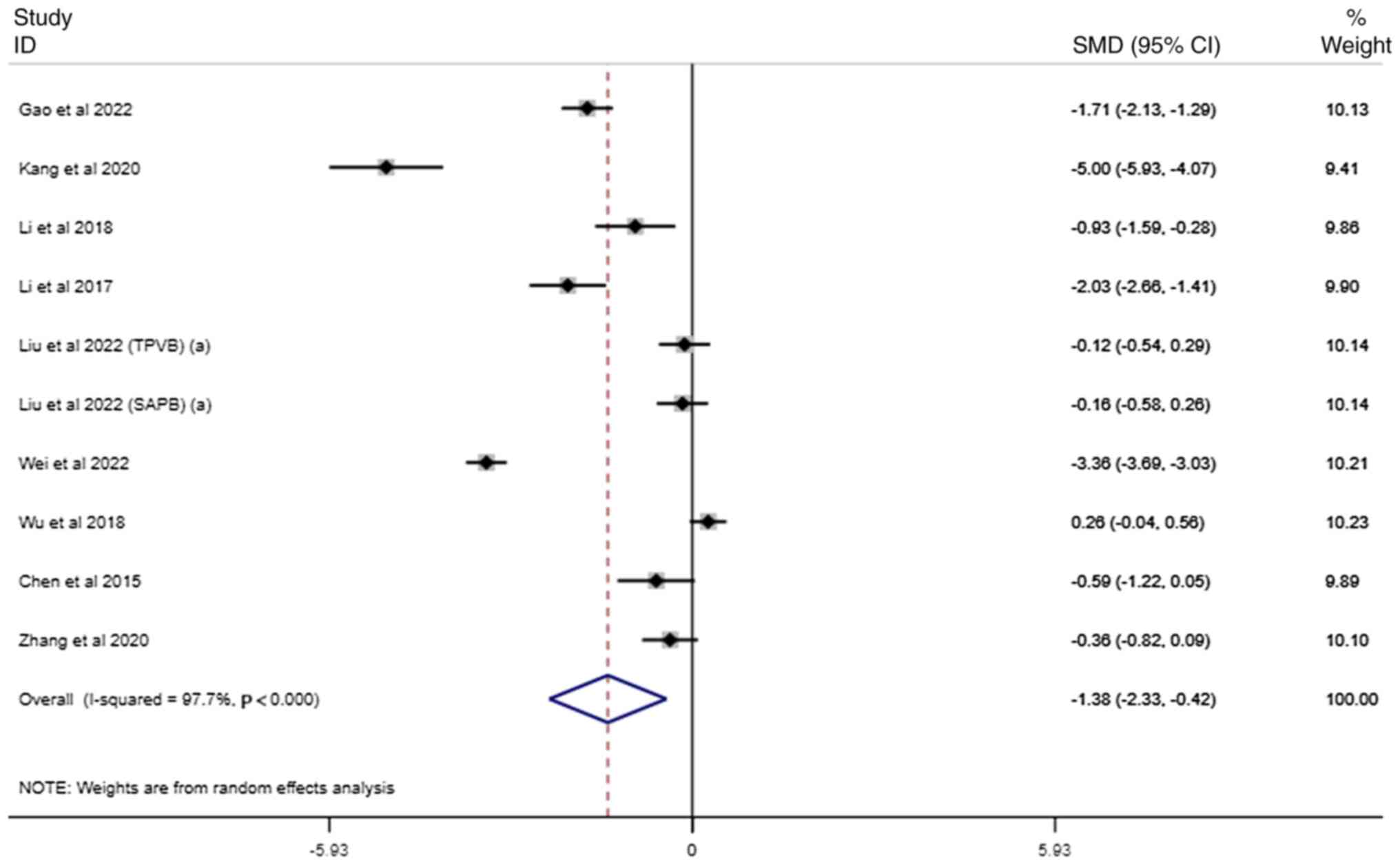
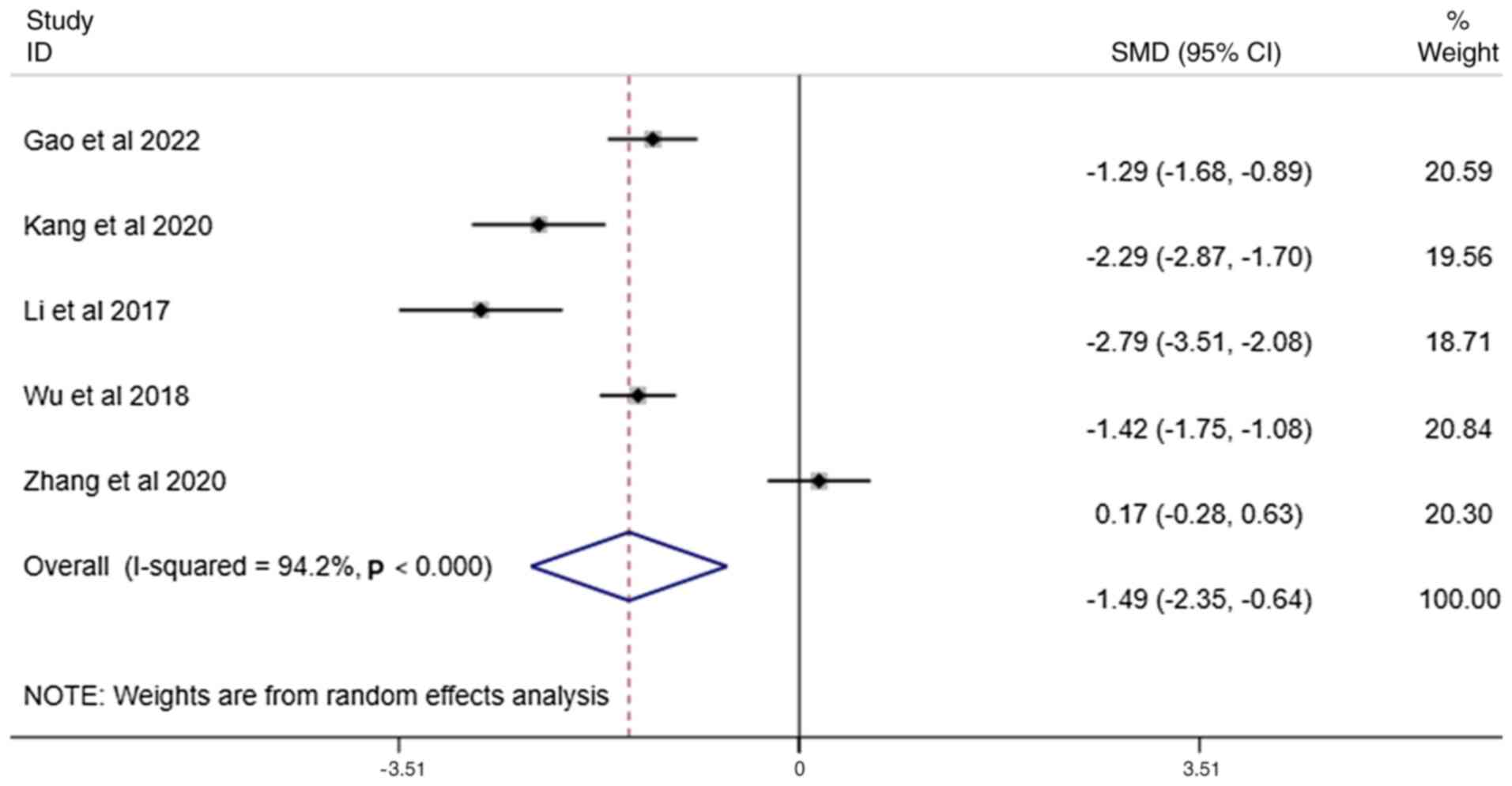
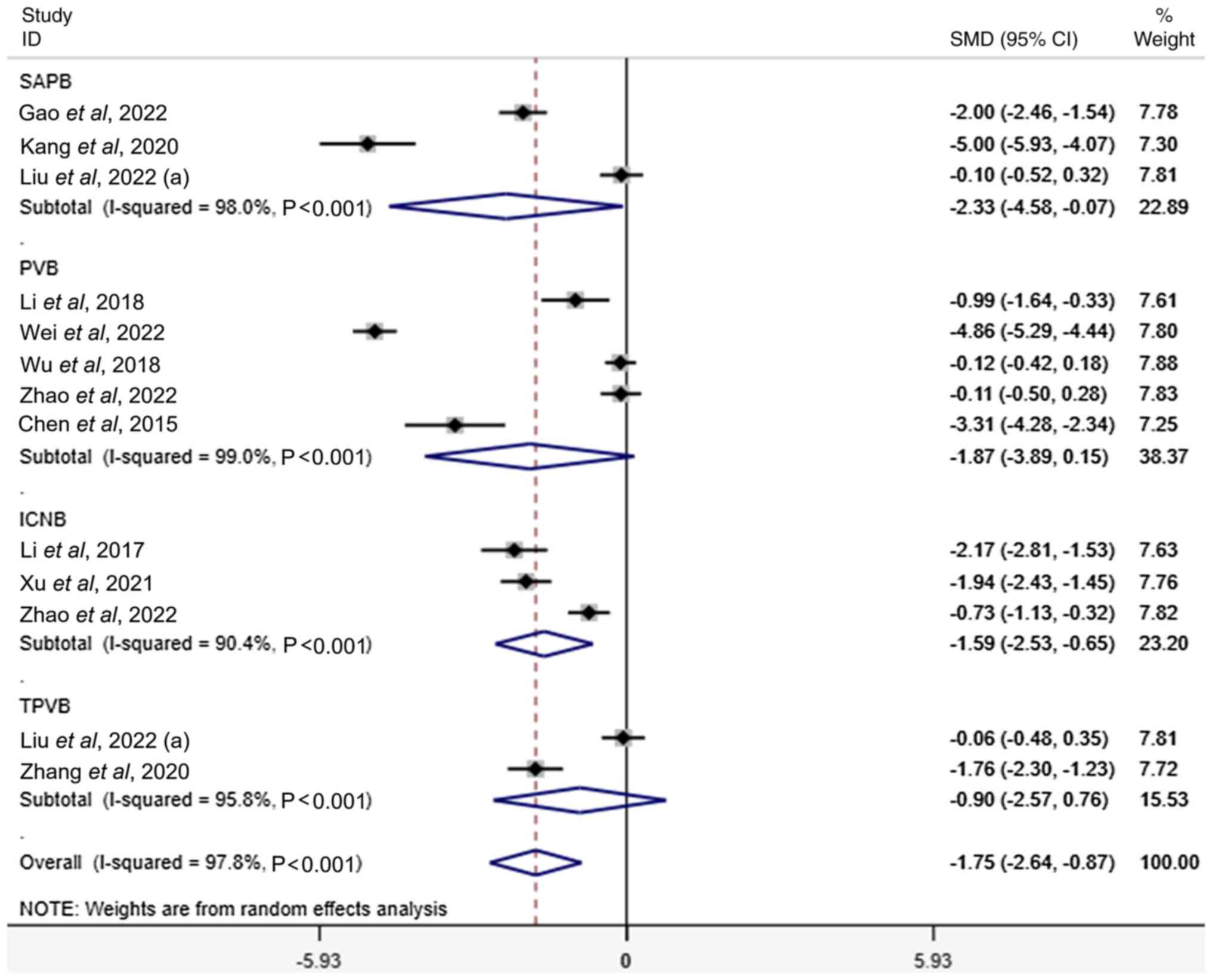
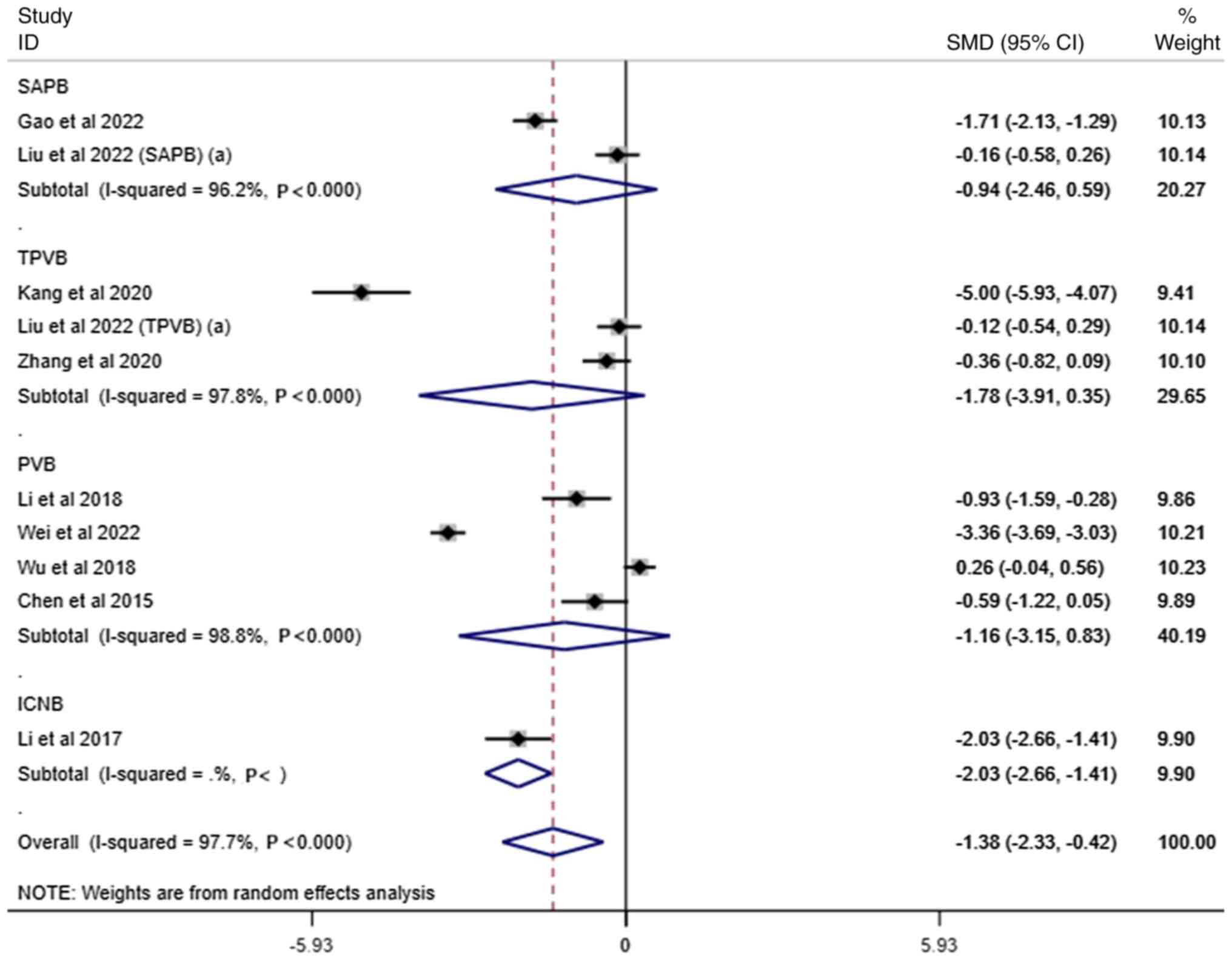
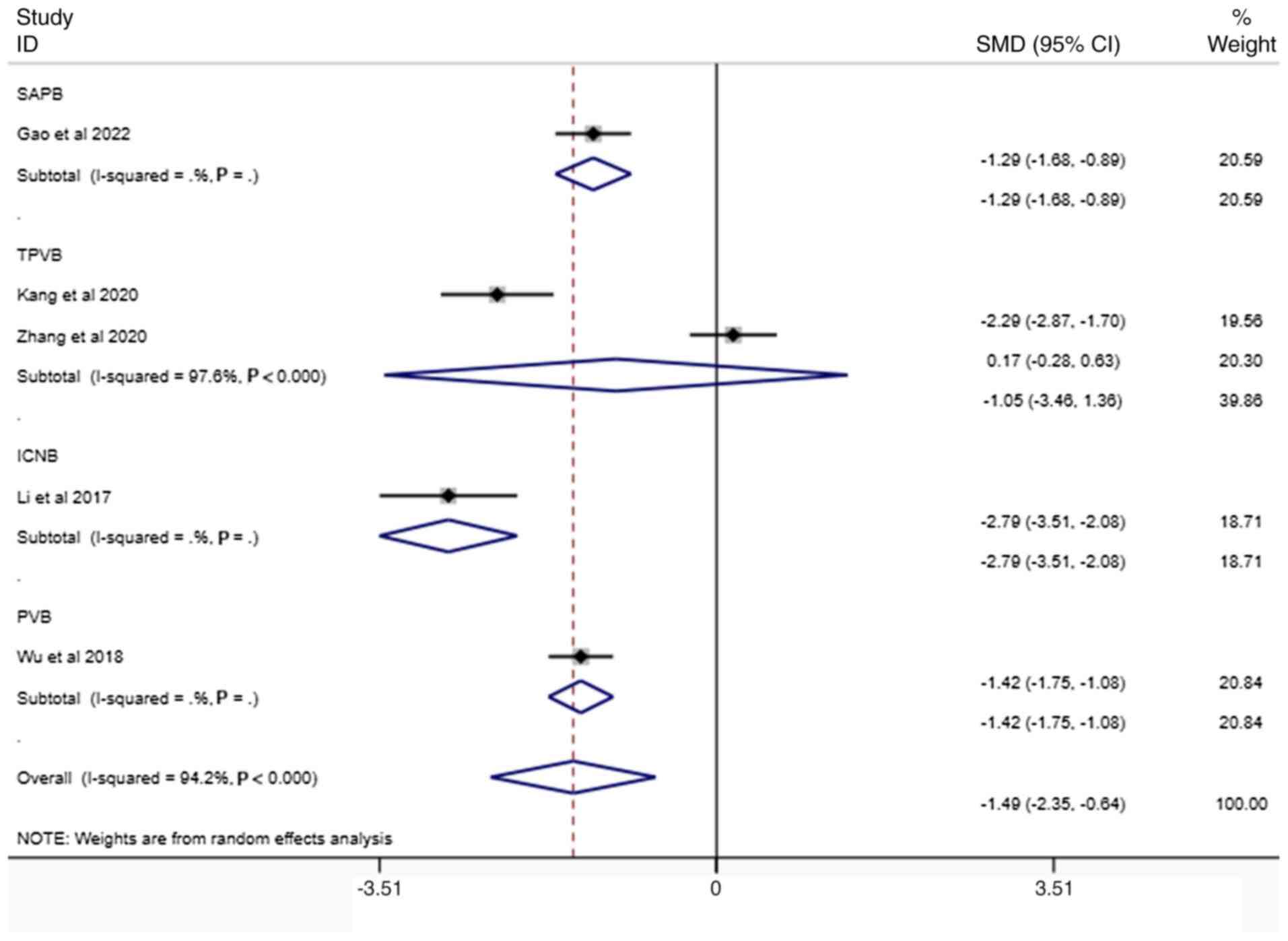
VAS scores
A total of 11 studies (21-24,28-34)
reported pain scores at rest, with 11 reporting scores after 24 h
(I2=97.8%, Fig. 3), 9
(21-24,28,29,31,33,34)
reporting scores after 48 h (I2=97.7%, Fig. 4) and 5 (21,23,29,31,34)
extending at 72 h post-intervention (I2 =94.2%, Fig. 5). The forest plot showed a high
degree of heterogeneity, sensitivity analyses were conducted, yet
significant heterogeneity persisted. The pooled data indicated that
compared against the conventional anesthesia groups, nerve block
techniques yielded comparable levels of discomfort. At each time
interval, the severity of pain measured by standardized scales
failed to demonstrate any significant difference between treatment
modalities.
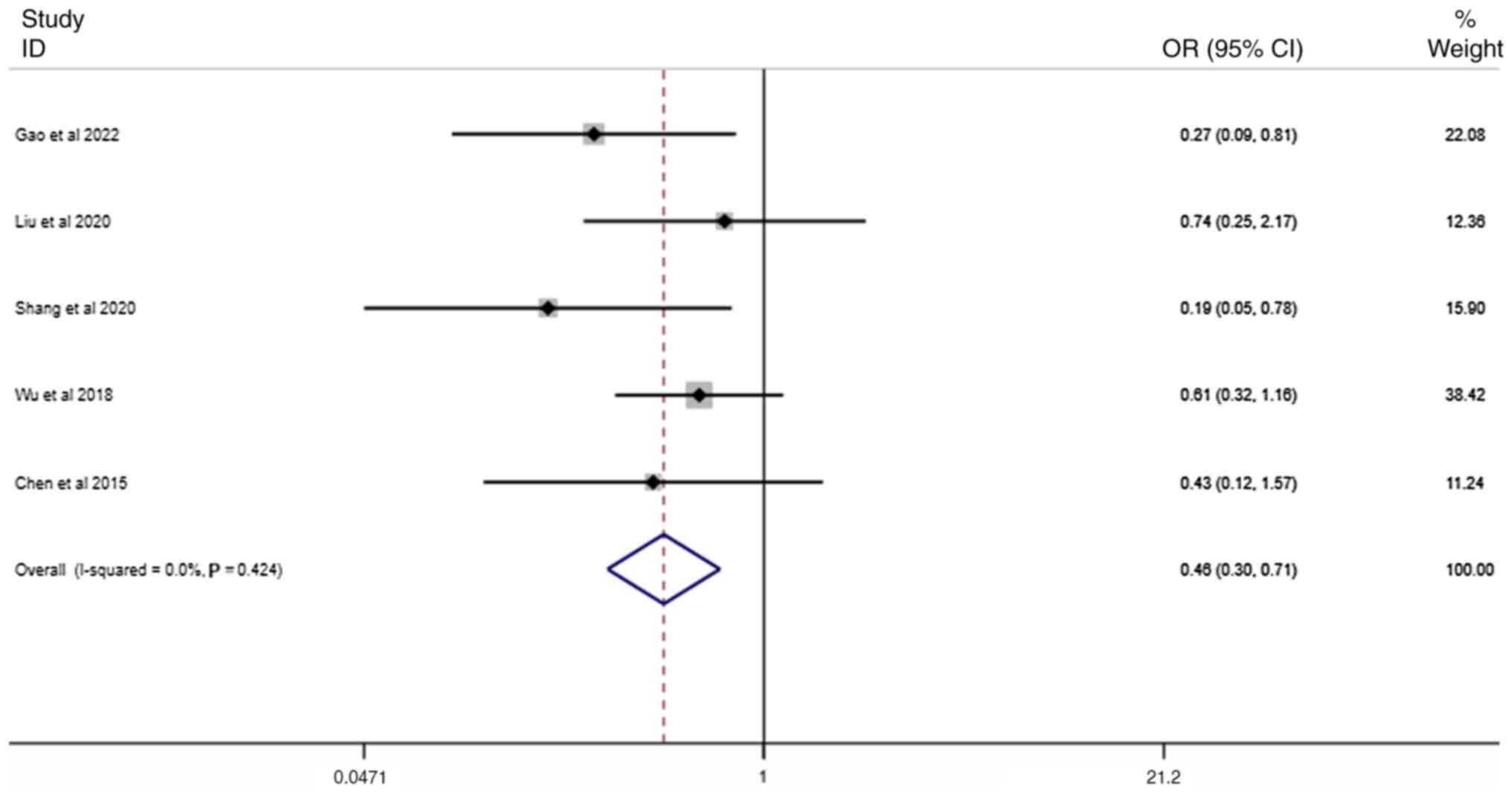
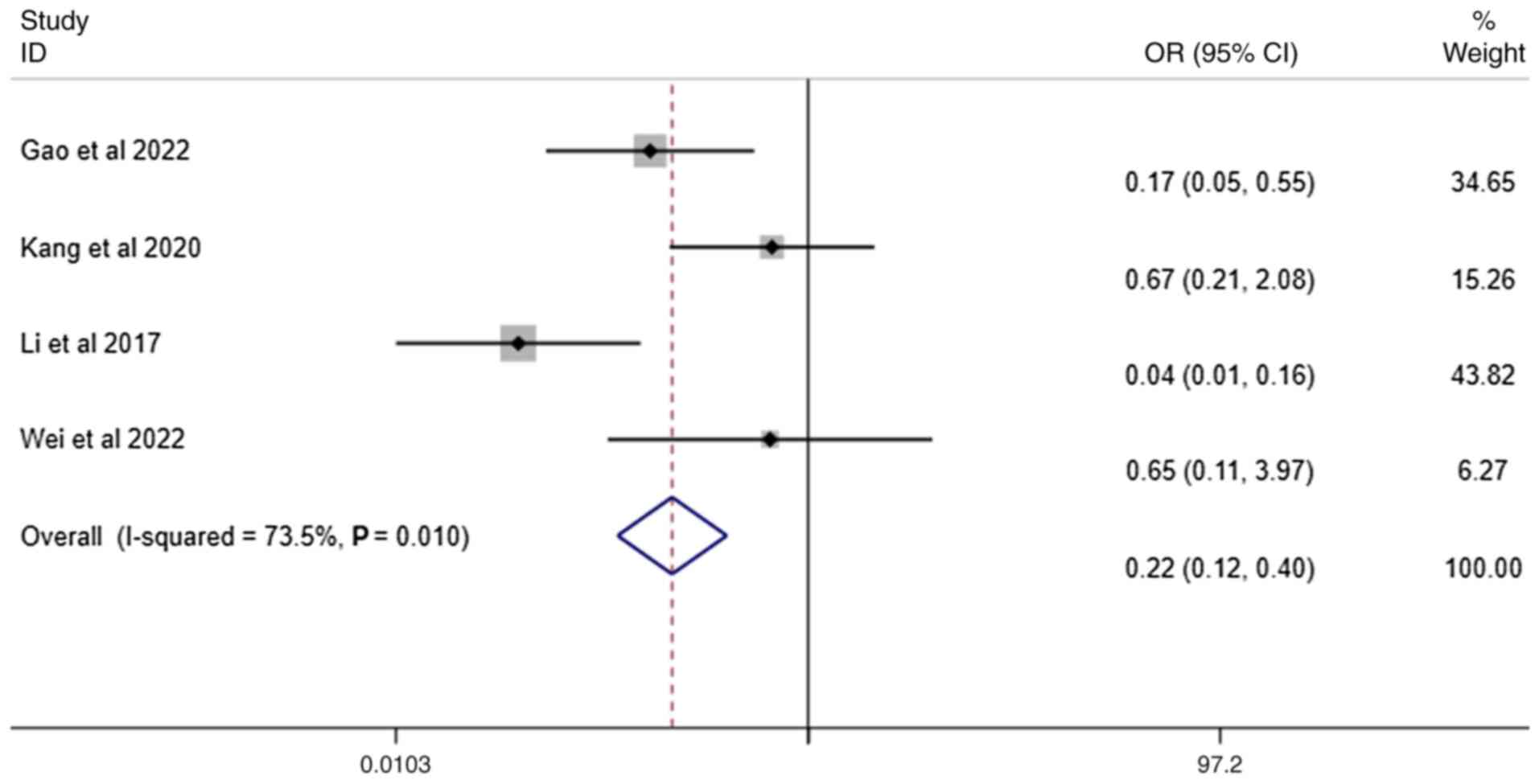
Number of individuals requiring
additional postoperative analgesic
A total of 5 studies (25,26,29,33,34)
studies reported the use of additional postoperative analgesics and
included interventions. In the group receiving neural blockade,
there was a significant decrease in the number of patients who
required additional pain medication postoperatively
(I2=0.0%, Fig. 6).
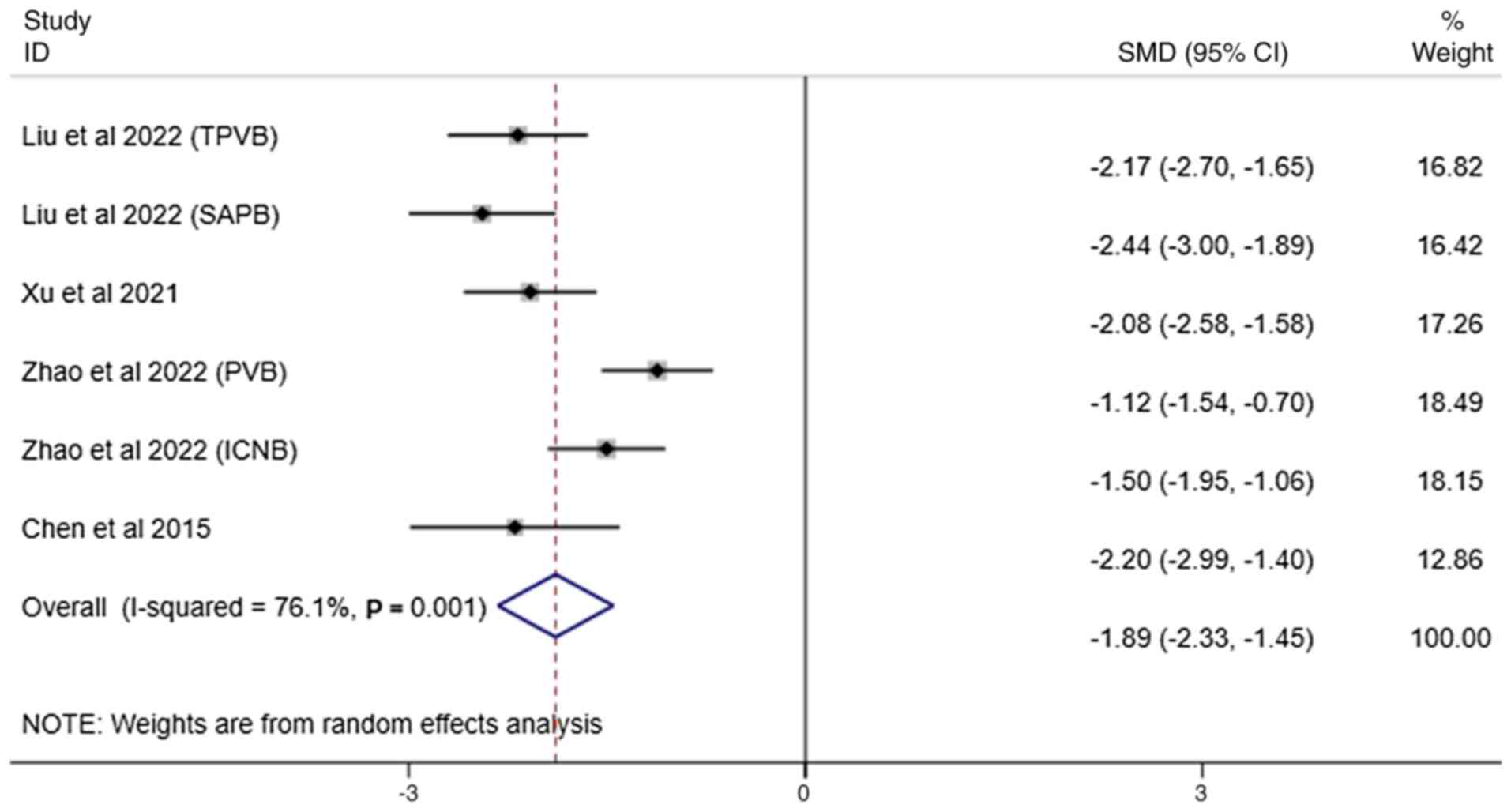
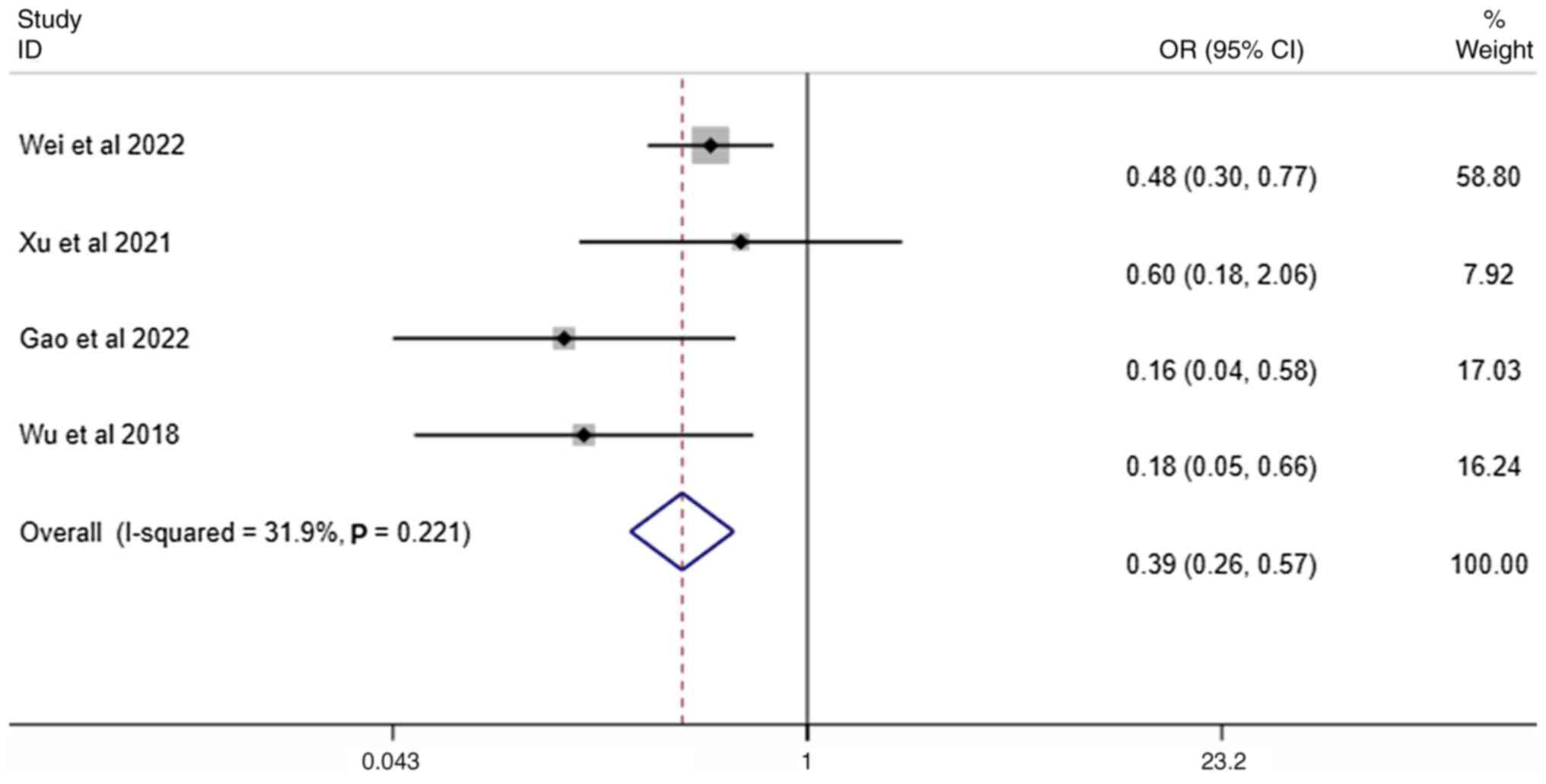
Administration of patient-controlled
analgesia
A total of 4 studies (24,30,32,34)
reported the administration of patient-controlled analgesia and
included interventions. The nerve block cohort required
significantly fewer patient-controlled analgesia interventions
compared with the control (I2=72.5%, Fig. 7).
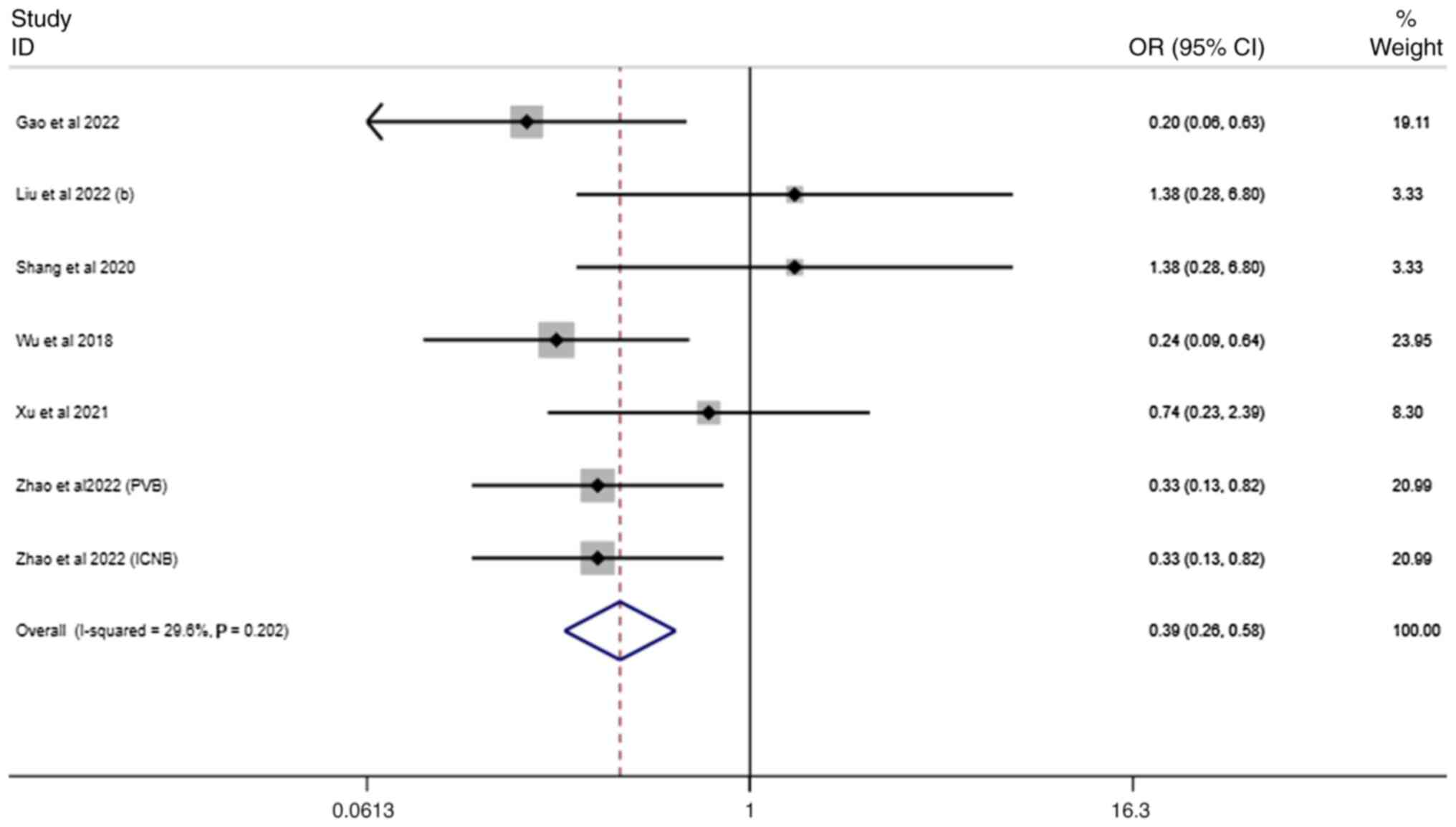
Incidence of postoperative adverse
reactions. Nausea and vomiting
A total of 6 studies (25,26,29,30,32,34)
reported nausea and vomiting, including interventions. The pooled
outcome indicated that, compared with control group, subjects who
received regional numbing techniques exhibited fewer instances of
nausea and emesis following surgery (I2=29.5%, Fig. 8).
Pulmonary adverse reactions. A total of 4
studies (21,23,28,34)
reported the pulmonary adverse reactions (I2=44.8%;
Fig. 9). In comparison with the
control group, patients in the experimental cohort exhibited a
notable improvement in lung function.
Other adverse reactions. A total of 4 studies
(28-30,34)
reported other adverse reactions, which included delirium,
hypersomnia, venous thrombosis and intestinal obstruction. Compared
with the control group, individuals within the experimental cohort
experienced fewer instances of other side effects
(I2=31.3%, Fig.
10).
Summary and analysis of results
Of 14 studies included in the present meta-analysis,
there was no significant disparity in the VAS score between the
nerve block group and the control group. Sensitivity analyses was
implemented by excluding studies with a high risk of bias. Wei
et al (28)'s study
population consisted entirely of elderly patients (>65 years
old), the control group in Wu et al (29) used the potent opioid sufentanil and
all patients uniformly received non-steroidal anti-inflammatory
drugs as background analgesia, resulting in a high intensity of
analgesia in the control group. Furthermore, these two studies had
large sample sizes and marked weight in the analysis. Their
exclusion was performed to test the robustness of the overall
meta-analysis results. Marked heterogeneity persisted after
excluding Wei et al (28)
(I2=95.3%, Fig. S1),
and this persisted after excluding Wu et al (29) (I2=97.7%, Fig. S2). In addition, after excluding
both Wei et al (28) and Wu
et al (29), no notable
changes in the level of heterogeneity were observed
(I2=95.1%, Fig. S3).
Subgroup analysis based on different nerve block areas for
heterogeneity testing was then performed (Fig. 11, Fig. 12, Fig. 13, Fig. 14, Fig. 15 and Fig. 16), the heterogeneity among groups
could not be clearly explained. Meta-regression was not performed
in due to the limited number of included studies. With only 14
RCTs, the statistical power for a meta-regression would be low,
increasing the risk of false-negative findings and model
instability (35). Key potential
effect modifiers, such as the specific type and concentration of
local anesthetic, technical nuances of the nerve blocks and
patient-specific factors such as baseline pain tolerance, were
reported inconsistently across studies, precluding their systematic
extraction and synthesis. The considerable heterogeneity observed,
particularly in pain score outcomes, may arise from a combination
of clinical and methodological diversity. In the absence of
comprehensive and uniformly reported covariate data,
meta-regression would be unlikely to explain the sources of this
heterogeneity and could lead to spurious conclusions (36). Due to inconsistent drug
concentrations and technical details, it was not possible to
identify the cause of heterogeneity. Nevertheless, nerve block
demonstrated notable efficacy in decreasing the number of patients
requiring additional analgesics post-surgery and the frequency of
patient-initiated pain relief button presses. Overall, nerve block
alleviated postoperative pain in patients and they lowered the
incidence of postoperative adverse reactions, effectively
facilitating a quicker recovery.
Discussion
Life expectancy of patients with cancer is affected
by a variety of factors (37).
Pain is a key factor that not only enhances the stress response of
the body but also triggers the release of inflammatory factors,
which can trigger intense stress responses, leading to massive
catecholamine release and increasing the risk of myocardial
ischemia in high-risk patients, and exacerbates postoperative lung
injury (38). Therefore, improving
postoperative pain management methods is key for improving the
quality of life and extending the life expectancy of patients with
cancer. Pain relief allows patients to breathe more freely and
cough up sputum effectively, helping to keep the airways open, as
well as keeping blood pressure and heart rate relatively stable and
allowing for smoother urination. This decreases the risk of
respiratory complications such as atelectasis and pneumonia,
cardiovascular complications, urinary tract infection and urinary
retention (39).
Hade et al (40) showed that a significant proportion
of patients experienced moderate to severe rebound pain following
neurosurgical procedures, with marked discomfort during surgery and
intense pain in the recovery room. This may explain the substantial
variation in VAS score observed between nerve block and general
anesthesia in the present study. The patients with lung cancer
included in the present meta-analysis covered multiple stages, and
patients at stage II-III required adjuvant therapy following
surgery. Adjuvant chemotherapeutic drugs often cause adverse
reactions such as nausea, vomiting and fatigue (41), which may interfere with the
perception and expression of pain; joint pain caused by targeted
therapies may also affect the accurate assessment of the effect of
nerve blocking techniques. Therefore, the advantages of nerve block
technology in postoperative pain management of patients with lung
cancer are difficult to evaluate accurately.
Mitigating postoperative side effects can markedly
improve the quality of life of patients and serves a vital role in
the recovery process (42).
Reduced nausea and vomiting can reduce the stress response of the
gastrointestinal tract and maintain normal peristalsis and
digestive function of the gastrointestinal tract (43). To allow the gastrointestinal tract
to resume normal emptying and absorption functions faster, allowing
patients to resume consumption of their normal diet sooner,
clinicians should ensure effective intake of nutrients, provide
sufficient energy and nutritional support for physical recovery and
promote wound healing and recovery of the body functions. When
severe pain and frequent nausea and vomiting are relieved, the
psychological pressure is decreased, thus improving the quality of
life at the psychological level (44). Guerra-Londono et al
(45) indicated that intercostal
nerve block analgesia is associated with a decreased risk of nausea
and vomiting when compared with systemic analgesia, in agreement
with the results of the present study. Cancer rehabilitation is a
critical process that helps patients restore physical function and
improve quality of life through several methods (46), therefore, quality of life is a key
outcome indicator for cancer rehabilitation. The present study did
not include direct quality of life data. Although secondary
outcomes (such as reduced analgesic requirements and fewer
complications) suggest potential quality of life benefits, it was
not possible to perform a quantitative synthesis as the original
studies did not use a standardized quality of life scale (47,48).
Given the potential for related bias in the
meta-analysis, there is a critical need for more robustly designed,
large-scale RCTs, coupled with extensive long-term follow-up, to
provide more definitive findings. Future studies should emphasize
larger, multi-center trials to validate the present results and
investigate the long-term impacts of nerve block across various
populations.
Among 16 RCTs in the present meta-analysis, 15
(93.8%) originated from China, with only one (21) from Italy. Variations in genetics,
pain tolerance, anesthesia technique, drug choices (such as
ropivacaine concentration) and postoperative management across
populations restrict generalizability. Addressing this geographical
bias requires future studies to include diverse cohorts such as
American and African cohorts.
The present study has several limitations, firstly,
the meta-analysis included 3 studies, at least 1 of which had a
high risk of bias in certain areas, whereas the other 11 studies
failed to provide clear explanations regarding randomization and
blinding procedures. Secondly, high heterogeneity was observed in
the VAS score, possibly due to inconsistencies in drug
concentration and technical details. The time points for measuring
pain scores were not always represented by accurate values (the
actual timing of pain score measurements may vary and is not always
entirely accurate). The present study did not separately analyze
image-guided and non-guided nerve block. Patients have different
tolerance standards for pain. In addition, the research regions
were limited, with the majority coming from China. Furthermore,
there was a lack of direct quality of life evidence. Finally, due
to the limited number of studies and total sample size, subgroup
analysis did not identify causes for heterogeneity.
In conclusion, the present meta-analysis compared
the efficacy of regional analgesic techniques in enhancing
postoperative pain control in VATS. Compared with other
meta-analyses (45,49,50),
the patients included in the present study all had lung cancer and
underwent VATS surgery. All the studies included in the analysis
compared VATS with conventional anesthetic techniques. Nerve block
demonstrated clear advantages in postoperative pain management and
concurrently exhibited lower incidences of associated complications
following surgery. Further research comparing nerve block
technology with conventional anesthetic techniques for thoracic
procedures will clarify differences between the two approaches in
terms of analgesic efficacy, medical costs, and patient tolerance,
thereby guiding precise clinical implementation.
Supplementary Material
Visual analogue scale score after 24
h, excluding Wei et al (28). Weights calculated from random
effects analysis. CI, confidence interval; SMD, standardized mean
difference; PVB, paravertebral block; TPVB, thoracic paravertebral
space to block; SAPB, serratus anterior plane block; ICNB,
intercostal nerve block.
Visual analogue scale score after 24
h, omitting Wu et al (29).
Weights calculated from random effects analysis. CI, confidence
interval; SMD, standardized mean difference; PVB, paravertebral
block; TPVB, thoracic paravertebral space to block; SAPB, serratus
anterior plane block; ICNB, intercostal nerve block.
Visual analogue scale score after 24
h, omitting Wei et al (28)
and Wu et al (29). Weights
calculated from random effects analysis. CI, confidence interval.
SMD, standardized mean difference. PVB, paravertebral block. TPVB,
thoracic paravertebral space to block; SAPB, serratus anterior
plane block; ICNB, intercostal nerve block.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by the Chengdu
University of Traditional Chinese Medicine ‘Xinglin Scholars’
Discipline Talent Scientific Research Enhancement Plan Public
Science Project (grant no. KPZX2023001).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
JW performed data extraction in duplicate and
contributed to manuscript drafting and critical revision. YXL
analyzed and interpreted data. SZ conducted database searches and
initial screening, assisted in data synthesis and interpretation.
BA acted as senior reviewer, resolving discrepancies in screening,
data extraction, and risk of bias assessment; provided senior
supervision throughout the study; and critically revised and
approved the final manuscript. JW and YXL confirm the authenticity
of all the raw data. All authors have read and approved the final
version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Maconachie R, Mercer T, Navani N and
McVeigh G: Guideline Committee. Lung cancer: diagnosis and
management: Summary of updated NICE guidance. BMJ.
364(l1049)2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Alexander M, Kim SY and Cheng H:
Management of non-small cell lung cancer. Lung. 198:897–907.
2020.
|
|
3
|
Bray F, Laversanne M, Sung H, Ferlay J,
Siegel RL, Soerjomataram I and Jemal A: Global cancer statistics
2022: GLOBOCAN estimates of incidence and mortality worldwide for
36 cancers in 185 countries. CA Cancer J Clin. 74:229–263.
2024.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Batchelor TJP, Rasburn NJ,
Abdelnour-Berchtold E, Brunelli A, Cerfolio RJ, Gonzalez M,
Ljungqvist O, Petersen RH, Popescu WM, Slinger PD and Naidu B:
Guidelines for enhanced recovery after lung surgery:
Recommendations of the enhanced recovery after surgery
(ERAS®) Society and the European Society of Thoracic
Surgeons (ESTS). Eur J Cardiothorac Surg. 55:91–115.
2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Klapper J and D'Amico TA: VATS versus open
surgery for lung cancer resection: Moving toward a minimally
invasive approach. J Natl Compr Canc Netw. 13:162–164.
2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bendixen M, Jørgensen OD, Kronborg C,
Andersen C and Licht PB: Postoperative pain and quality of life
after lobectomy via video-assisted thoracoscopic surgery or
anterolateral thoracotomy for early-stage lung cancer: A randomised
controlled trial. Lancet Oncol. 17:836–844. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Nagahiro I, Andou A, Aoe M, Sano Y, Date H
and Shimizu N: Pulmonary function, postoperative pain, and serum
cytokine level after lobectomy: A comparison of VATS and
conventional procedure. Ann Thorac Surg. 72:362–365.
2001.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Sandeep B, Huang X, Li Y, Xiong D, Zhu B
and Xiao Z: A comparison of regional anesthesia techniques in
patients undergoing video-assisted thoracic surgery: A network
meta-analysis. Int J Surg. 105(106840)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mathew B, Lennon FE, Siegler J,
Mirzapoiazova T, Mambetsariev N, Sammani S, Gerhold LM, LaRiviere
PJ, Chen CT, Garcia JG, et al: The novel role of the mu opioid
receptor in lung cancer progression: A laboratory investigation.
Anesth Analg. 112:558–567. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Rodrigues P, Bangali H, Hammoud A, Mustafa
YF, Al-Hetty HRAK, Alkhafaji AT, Deorari MM, Al-Taee MM, Zabibah RS
and Alsalamy A: COX 2-inhibitors; a thorough and updated survey
into combinational therapies in cancers. Med Oncol.
41(41)2024.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Steegers MA, Snik DM, Verhagen AF, van der
Drift MA and Wilder-Smith OH: Only half of the chronic pain after
thoracic surgery shows a neuropathic component. J Pain. 9:955–961.
2008.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Fenta E, Kibret S, Hunie M, Tamire T,
Mekete G, Tiruneh A, Fentie Y, Dessalegn K and Teshome D: The
analgesic efficacy of erector spinae plane block versus
paravertebral block in thoracic surgeries: A meta-analysis. Front
Med (Lausanne). 10(1208325)2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Blanco R, Parras T, McDonnell JG and
Prats-Galino A: Serratus plane block: A novel ultrasound-guided
thoracic wall nerve block. Anaesthesia. 68:1107–1113.
2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Chen N, Qiao Q, Chen R, Xu Q, Zhang Y and
Tian Y: The effect of ultrasound-guided intercostal nerve block,
single-injection erector spinae plane block and multiple-injection
paravertebral block on postoperative analgesia in thoracoscopic
surgery: A randomized, double-blinded, clinical trial. J Clin
Anesth. 59:106–111. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Pei L, Zhou Y, Tan G, Mao F, Yang D, Guan
J, Lin Y, Wang X, Zhang Y, Zhang X, et al: Ultrasound-assisted
thoracic paravertebral block reduces intraoperative opioid
requirement and improves analgesia after breast cancer surgery: A
randomized, controlled, single-center trial. PLoS One.
10(e0142249)2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Gabriel RA, Curran BP, Swisher MW, Sztain
JF, Tsuda PS, Said ET, Alexander B, Finneran JJ IV, Abramson WB,
Black JR, et al: Paravertebral versus Pectoralis-II (Interpectoral
and Pectoserratus) nerve blocks for postoperative analgesia after
nonmastectomy breast surgery: A randomized, controlled,
observer-masked noninferiority trial. Anesthesiology.
141:1039–1050. 2024.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Jackson JC, Tan KS, Pedoto A, Park BJ,
Rusch VW, Jones DR, Zhang H, Desiderio D, Fischer GW and Amar D:
Effects of serratus anterior plane block on early recovery from
thoracoscopic lung resection: A randomized, blinded,
placebo-controlled trial. Anesthesiology. 142(588)2025.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Chi Y, Su X, Liu S, Wen J, Hu M, Li H,
Huang H, Zhang Z and Xie H: Liposomal bupivacaine intercostal nerve
block for pain control in thoracoscopic surgery: A randomized
controlled trial. Front Med (Lausanne). 12(1647324)2025.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Rekatsina M and Peng PWH: The importance
of image guidance in common spine interventional procedures for
pain management: A comprehensive narrative review. Pain Ther.
14:841–863. 2025.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Zhang L, Shen J and Luo Y: The impact of
paravertebral nerve blockade on postoperative surgical site wound
pain management in patients undergoing video-assisted thoracoscopic
surgery for pulmonary carcinoma resection. Int Wound J.
21(e14608)2024.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kang K, Meng X, Li B, Yuan J, Tian E,
Zhang J and Zhang W: Effect of thoracic paravertebral nerve block
on the early postoperative rehabilitation in patients undergoing
thoracoscopic radical lung cancer surgery. World J Surg Oncol.
18(298)2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Li X, Cui X, Zhang S and Fu Z:
Ameliorative effects of parecoxib in combination with
ultrasound-guided paravertebral block (UGPB) on stress and
inflammatory responses following thoracoscopic surgery. Trop J
Pharm Res. 17:1171–1175. 2018.
|
|
23
|
Li Y, Gong L, Xu F, Zhao H, Chen Y and
Wang C: Effects of ropivacaine as intercostal nerve blocker on
postoperative pain after video-assisted thoracic surgery of lung
cancer patients. Chin J Clin Oncol. 44:605–607. 2017.
|
|
24
|
Liu X and An J: Effects of serratus
anterior plane block and thoracic paravertebral nerve block on
analgesia, immune function and serum tumor markers in patients
after thoracoscopic radical resection of lung cancer. Nagoya J Med
Sci. 84:506–515. 2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Liu Y, Li Y, Wu C and Li H: Effects of
nalbuphine combined with anterior serratus plane block in elderly
patients undergoing thoracoscopic surgery. J Healthc Eng.
2022(7408951)2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Shang LH, Xiao ZN, Zhao YL and Long B:
Analgesic effect of serratus anterior plane block after
thoracoscopic surgery: A randomized controlled double-blinded
study. Ther Clin Risk Manag. 16:1257–1265. 2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Viti A, Bertoglio P, Zamperini M, Tubaro
A, Menestrina N, Bonadiman S, Avesani R, Guerriero M and Terzi A:
Serratus plane block for video-assisted thoracoscopic surgery major
lung resection: A randomized controlled trial. Interact Cardiovasc
Thorac Surg. 30:366–372. 2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Wei W, Zheng X, Gu Y, Fu W, Tang C and Yao
Y: Effect of general anesthesia with thoracic paravertebral block
on postoperative delirium in elderly patients undergoing
thoracoscopic lobectomy: A randomized-controlled trial. BMC
Anesthesiol. 22(1)2022.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Wu Z, Fang S, Wang Q, Wu C, Zhan T and Wu
M: Patient-controlled paravertebral block for video-assisted
thoracic surgery: A randomized trial. Ann Thorac Surg. 106:888–894.
2018.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Xu J, Pu M, Xu X, Xiang J and Rong X: The
postoperative analgesic effect of intercostal nerve block and
intravenous patient-controlled analgesia on patients undergoing
lung cancer surgery. Am J Transl Res. 13:9790–9795. 2021.PubMed/NCBI
|
|
31
|
Zhang W, Cong X, Zhang L, Sun M, Li B,
Geng H, Gu J and Zhang J: Effects of thoracic nerve block on
perioperative lung injury, immune function, and recovery after
thoracic surgery. Clin Transl Med. 10(e38)2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Zhao X, Li X, Wang Y, Xiao W, Zhang B,
Meng X and Sun X: Efficacy of intrathoracic intercostal nerve block
on postoperative acute and chronic pains of patients undergoing
video-assisted thoracoscopic surgery. J Pain Res. 15:2273–2281.
2022.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Chen J, Zhang Y, Huang C, Chen K, Fan M
and Fan Z: Effects of thoracic paravertebral block on postoperative
analgesia and serum level of tumor marker in lung cancer patients
undergoing video-assisted thoracoscopic surgery. Zhongguo Fei Ai Za
Zhi. 18:104–109. 2015.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
34
|
Gao W, Yang XL, Hu JC, Gu H, Wu XN, Hu SS,
Wang S, Chai XQ and Wang D: Continuous serratus anterior plane
block improved early pulmonary function after lung cancer surgical
procedure. Ann Thorac Surg. 113:436–443. 2022.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Cumpston M, Li T, Page MJ, Chandler J,
Welch VA, Higgins JP and Thomas J: Updated guidance for trusted
systematic reviews: A new edition of the cochrane handbook for
systematic reviews of interventions. Cochrane Database Syst Rev.
10(ED000142)2019.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Stogiannis D, Siannis F and Androulakis E:
Heterogeneity in meta-analysis: A comprehensive overview. Int J
Biostat. 20:169–199. 2023.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Planchard D, Popat S, Kerr K, Novello S,
Smit EF, Faivre-Finn C, Mok TS, Reck M, Van Schil PE, Hellmann MD,
et al: Metastatic non-small cell lung cancer: ESMO clinical
practice guidelines for diagnosis, treatment and follow-up. Ann
Oncol. 29:iv192–iv237. 2018.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Polański J, Tański W, Dudek K and
Jankowska-Polańska B: Pain and coping strategies as determinants of
malnutrition risk in lung cancer patients: A cross-sectional study.
Nutrients. 16(2193)2024.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Chou R, Gordon DB, de Leon-Casasola OA,
Rosenberg JM, Bickler S, Brennan T, Carter T, Cassidy CL,
Chittenden EH, Degenhardt E, et al: Management of postoperative
pain: A clinical practice guideline from the American Pain Society,
the American Society of Regional Anesthesia and Pain Medicine, and
the American Society of Anesthesiologists' Committee on Regional
Anesthesia, Executive Committee, and Administrative Council. J
Pain. 17:131–157. 2016.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Hade AD, Okano S, Pelecanos A and Chin A:
. Factors associated with low levels of patient satisfaction
following peripheral nerve block. Anaesth Intensive Care.
49:125–132. 2021.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Chen YK, Boden KA and Schreiber KL: The
role of regional anaesthesia and multimodal analgesia in the
prevention of chronic postoperative pain: A narrative review.
Anaesthesia. 76 (Suppl 1):S8–S17. 2021.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Gouez M, Delrieu L, Bouleuc C, Girard N,
Raynard B and Marchal T: Association between nutritional status and
treatment response and survival in patients treated with
immunotherapy for lung cancer: A retrospective french study.
Cancers (Basel). 14(3439)2022.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Lan T, Chen L and Wei X: Inflammatory
cytokines in cancer: Comprehensive understanding and clinical
progress in gene therapy. Cells. 10(100)2021.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Morrison EJ, Novotny PJ, Sloan JA, Yang P,
Patten CA, Ruddy KJ and Clark MM: Emotional problems, quality of
life, and symptom burden in patients with lung cancer. Clin Lung
Cancer. 18:497–503. 2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Guerra-Londono CE, Privorotskiy A,
Cozowicz C, Hicklen RS, Memtsoudis SG, Mariano ER and Cata JP:
Assessment of intercostal nerve block analgesia for thoracic
surgery: A systematic review and meta-analysis. JAMA Netw Open.
4(e2133394)2021.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Li D, Sun CL, Kim H, Soto-Perez-de-Celis
E, Chung V, Koczywas M, Fakih M, Chao J, Cabrera Chien L, Charles
K, et al: Geriatric assessment-driven intervention (GAIN) on
chemotherapy-related toxic effects in older adults with cancer: A
randomized clinical trial. JAMA Oncol. 7(e214158)2021.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Wolf AMD, Oeffinger KC, Shih TY, Walter
LC, Church TR, Fontham ETH, Elkin EB, Etzioni RD, Guerra CE,
Perkins RB, et al: Screening for lung cancer: 2023 guideline update
from the American Cancer Society. CA Cancer J Clin. 74:50–81.
2024.PubMed/NCBI View Article : Google Scholar
|
|
48
|
de Rooij BH, van den Hurk C, Smaardijk V,
Fernandez-Ortega P, Navarro-Martin A, Barberio L, Guckenberger M,
Schmid S, Walraven I, Vallow S, et al: Development of an updated,
standardized, patient-centered outcome set for lung cancer. Lung
Cancer. 173:5–13. 2022.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Capuano P, Hileman BA, Martucci G, Raffa
GM, Toscano A, Burgio G, Arcadipane A and Kowalewski M: Erector
spinae plane block versus paravertebral block for postoperative
pain management in thoracic surgery: A systematic review and
meta-analysis. Minerva Anestesiol. 89:1042–1050. 2023.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Gonçalves JPF, Duran ML, Barreto ESR,
Antunes Júnior CR, Albuquerque LG, Lins-Kusterer LEF, Azi LMTA and
Kraychete DC: Efficacy of erector spinae plane block for
postoperative pain management: A meta-analysis and trial sequential
analysis of randomized controlled trials.
|