Introduction
Extra-nodal natural killer (NK)/T cell lymphoma,
nasal-type (ENKL), is a distinct entity according to the World
Health Organization (WHO) classification of lymphoid tissue. Though
rare in Western populations, it occurs with greater frequency among
Asians, Mexicans and South Americans of American Indian descent.
Due to its rarity and the lack of randomized controlled trials, a
definitive treatment for ENKL remains to be established. Here, we
describe our experience with a 50-year-old female patient who was
diagnosed with ENKL stage IIEA and treated by concurrent
chemoradiotherapy. Additional treatment options applied in previous
studies are also discussed, including other chemotherapy regimens
and autologous or allogenic hematopoietic stem-cell
transplantation.
Case report
A 50-year-old woman presented at the Osaka Medical
College Hospital in April 2008 with a suspected malignant white
tumor on a refractory ulcer on the right-lower gum, accompanied by
bilateral neck lymph node swelling. Levels of soluble IL-2 receptor
(716 U/ml) were increased. Genetic examination revealed no
rearrangement of T-cell receptors or immunoglobulin genes, and no
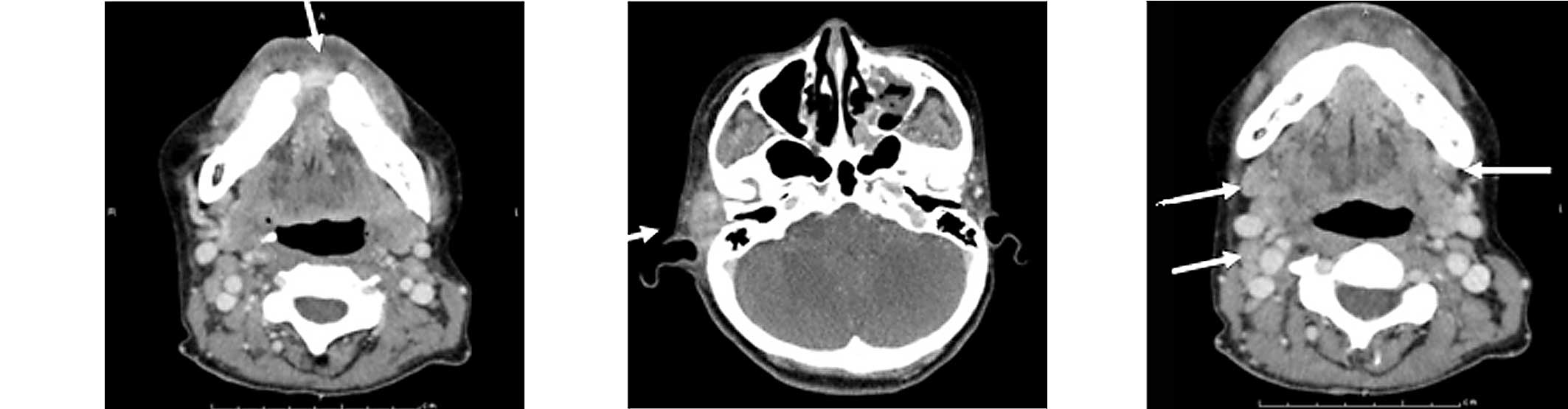
chromosomal abnormalities. CT images revealed a slightly enhanced
soft tissue mass with adjacent bone destruction and bilateral neck
lymphadenopathy (Fig. 1). No other
involved lesions were detected by garium-67 scintigraphy.
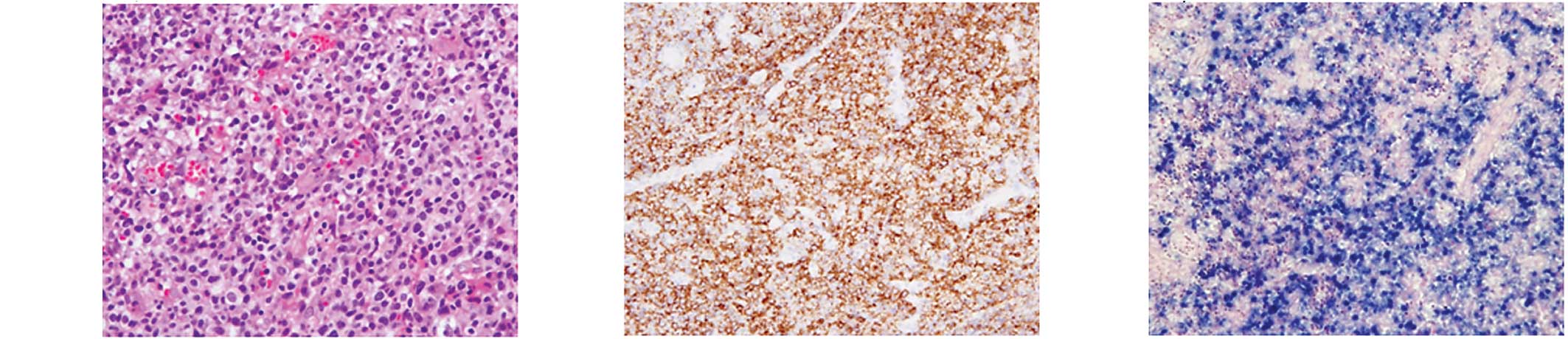
Histological examination of biopsy specimens with H&E staining
revealed diffuse infiltrate lymphoma cells. The immunophenotype was
CD56+, cytoplasmic CD3+/−, CD16+,
granzyme B+, CD20−, CD4− and
CD8−. The specimens were also positive for Epstein-Barr
virus encoded RNA (EBER) (Fig.
2).
The tumor was diagnosed as ENKL stage IIEA.
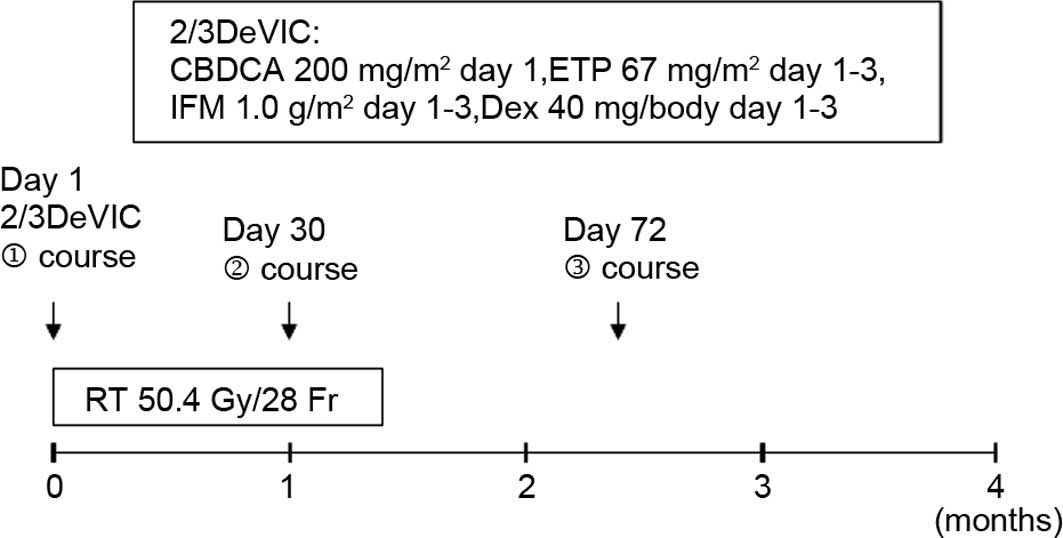
Concurrent chemoradiotherapy was administered according to the
regimen described in the Japan Clinical Oncology Group (JCOG) trial
0211-DI (Fig. 3) (1). This protocol was recommended since
ENKL is intractable and lacks a standard therapy. However, the case
was not registered with the JCOG trial, and the protocol was not
approved by an institutional review board, since it was necessary
to commence treatment immediately. The patient provided informed
written consent.
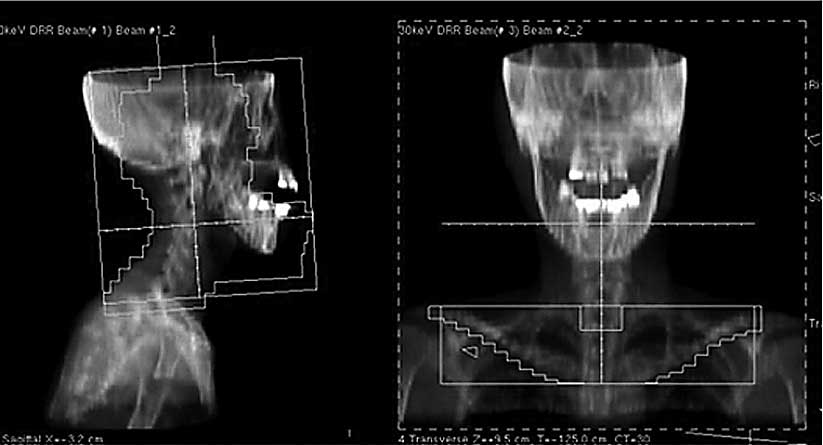
All extra-nodal lesions identified in the CT images
as well as the bilateral neck and supraclavicular lymph node
regions were included within the radiation portals. Using a 4-MV
photon beam, 41.4 Gy in 23 fractions over 4.6 weeks was delivered
to the extra-nodal site and to the neck and supraclavicular lymph
node regions (Fig. 4A).
Subsequently, the radiation portals were modified to avoid the
spinal cord, and 9.0 Gy in 5 fractions over a week was delivered to
the lesions with 4- and 10-MV photon beams (Fig. 4B). A 10-MeV electron beam was
employed to adequately cover the mandibular tumor area. The patient
suffered from grade 3 neutropenia and grade 3 acute oral mucositis,
which required temporary intravenous hyperalimentation.
On CT images captured 7 days after the completion of
the radiation therapy, the therapeutic effect was determined to be
a partial response. Five months after the final diagnosis, both
in-field and distant tumor recurrences were observed on PET/CT
images. Salvage chemotherapy (JALSG ALL202 protocol) was performed,
but the patient succumbed 1 month after recurrence.
Discussion
ENKL is characterized histologically by angiocentric
and polymorphous lymphoreticular infiltrates, and clinically by
progressive necrotic lesions occurring mainly in the nasal cavity
and a poor prognosis caused by rapid progression of the lesion into
distinct organs. This lymphoma is very rare in Western populations,
but occurs with greater frequency among Asians, Mexicans and South
Americans of American Indian descent. It has been reported that
NK/T cell lymphoma accounts for approximately 2.6% of all malignant
lymphomas in Japan (2). ENKL is
subcategorized into ‘nasal’ and ‘nasal-type’ ENKL according to the
anatomic sites of the primary disease. In previous reports, nasal
ENKL has been observed in the nasal cavity and upper aerodigestive
area, while nasal-type ENKL has been noted in other sites (4,5). The
nose and paranasal area, including the upper aerodigestive tract,
is the origin of more than 80% of ENKL occurences. The skin is the
second most frequent organ of origin, accounting for approximately
10% of occurrences, followed by the liver and/or spleen at 5% and,
more rarely, the lungs, gastrointestinal tract, kidney, pancreas,
testis and brain (7). Clinical
characteristics differ between nasal and nasal-type ENKL:
nasal-type ENKL is more advanced at diagnosis, and therefore, has a
poorer prognosis than nasal ENKL (4).
As ENKL is very sensitive to radiation therapy (RT),
RT plays a crucial role in its treatment, especially during the
limited stages of the disease (stages I/II). Previous reports have
suggested that RT as an initial treatment improves the local
control probability (LCP) and overall survival (OS) of patients
(5). Isobe et al reported
that patients who received over 50 Gy with an RT field that
included potential contiguous areas (the paranasal sinuses, palate
and nasopharynx) with an adequate margin had a higher LCP. These
results were statistically significant (5). Koom et al analyzed the
dose-response relationships for local control, which showed a
sigmoidal shape and reached a plateau at doses in excess of 54 Gy.
However, the authors also found that dose escalation in patients
who do not attain a complete response after the planned RT dose may
improve the LCP (9). Therefore,
doses over 50 Gy and an extended RT field are considered to confer
a favorable prognosis (8).
Currently, combined chemotherapy is performed in
many cases of ENKL, (3–7,9).
However, ENKL is often resistant to the anthracycline-based
chemotherapy used for malignant lymphomas (3,7). One
possible explanation for this resistance is that ENKL commonly
expresses P-glycoprotein, which is a product of the multidrug
resistance-1 gene (11) and has an
effect on anthracycline. Several reports have concluded that the
addition of current chemotherapy regimes to radiation therapy for
the treatment of ENKL may not improve the OS of the patients
(4,6). Therefore, the development of
effective chemotherapy regimens is an important step towards
improving the prognosis of both limited and advanced stage ENKL.
Several clinical studies of potential regimens are ongoing. For
limited stage ENKL, Yamaguchi et al reported a favorable
treatment outcome with concurrent chemoradiotherapy according to a
DeVIC regimen (3), which consists
of carboplatin, ifosphamide, etoposide and dexamethasone.
Carboplatin and ifosphamide are not affected by P-glycoprotein, and
etoposide is a key drug for the treatment of Epstein-Bar
virus-related hemophagocytic syndrome. For advanced stage or
relapsed ENKL, SMILE chemotherapy (consisting of L-asparaginase,
methotrexate, ifosphamide, etoposide and dexamethasone) (10) and autologous or allogenic
hematopoietic stem-cell transplantation have been reported to be
effective, though these studies have only been conducted in a small
patient sample.
In the current case, a complete response was not
achieved after the completion of treatment, and no therapeutic
effects of treatment were observed after recurrence. According to
previous reports, the survival curves decrease abruptly within 1-2
years of treatment and later increase very slowly (4–9).
Patients with a complete response and good local control tend to
achieve a longer survival time (3,9).
These studies and our current report indicate that additional boost
irradiation may improve patient outcome. Furthermore, intensive
follow-up and speedy induction salvage chemoradiotherapy should be
performed.
References
|
1.
|
Yamaguchi M, Tobinai K, Oguchi M, et al:
Phase I/II Study of Concurrent Chemoradiotherapy for Localized
Nasal Natural Killer/T-Cell Lymphoma: Japan Clinical Oncology Group
Study JCOG0211. J Clin Oncol. 27:5594–6001. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Lymphoma Study Group of Japanese
Pathologists: The World Health Organization classification of
malignant lymphomas in Japan: incidence of recently recognized
entities. Pathol Int. 50:696–702. 2000. View Article : Google Scholar
|
|
3.
|
Yamaguchi M, Ogawa S, Nomoto Y, et al:
Treatment outcome of nasal NK-T cell lymphoma: a report of 12
consecutively-diagnosed cases and a review of the literature. J
Clin Exp Hematopathol. 41:93–99. 2001. View Article : Google Scholar
|
|
4.
|
Cheung MMC, Chan JKC, Lau WH, Ngan RKC and
Foo WWL: Early stage nasal T/NK-cell lymphoma: clinical outcome,
prognostic factors, and the effect of treatment modality. Int J
Radiat Oncol Biol Phys. 54:182–190. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Isobe K, Uno T, Tamaru J, et al:
Extranodal natural killer/T-cell lymphoma, nasal type. Cancer.
106:609–615. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Kim K, Chie EK, Kim CW, Kim IH and Park
CI: Treatment outcome of angiocentric T-cell and NK/T-cell
lymphoma, nasal type: radiotherapy versus chemoradiotherapy. Jpn J
Clin Oncol. 35:1–5. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Suzuki R, Takeuchi K, Ohshima K and
Nakamura S: Extranodal NK/T-cell lymphoma: diagnosis and treatment
cues. Hematol Oncol. 26:66–72. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
8.
|
Shikama N, Ikeda H, Nakamura S, et al:
Localized aggressive non-Hodgkin’s lymphoma of the nasal cavity: a
survey by the Japan Lymphoma Radiation Therapy Group. Int J Radiat
Oncol Biol Phys. 51:1228–1233. 2001.
|
|
9.
|
Koom W, Chung E, Yang W, et al:
Angiocentric T-cell and NK/T-cell lymphomas: radiotherapeutic
viewpoints. Int J Radiat Oncol Biol Phys. 59:1127–1137. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Yamaguchi M, Suzuki R, Kwong YL, et al:
Phase I study of dexamethasone, methotrexate, ifosfamide,
L-asparaginase, and etoposide (SMILE) chemotherapy for
advanced-stage, relapsed or refractory extranodal natural killer
(NK)/T-cell lymphoma and leukemia. Cancer Sci. 99:1016–1020. 2008.
View Article : Google Scholar
|
|
11.
|
Egashira M, Kawamata N, Sugimoto K, Kaneko
T and Oshimi K: P-glycoprotein expression on normal and abnormally
expanded natural killer and inhibition of P-glycoprotein function
by cyclosporine A and its analogue, P SC83. Blood. 93:599–606.
1999.PubMed/NCBI
|