|
1
|
Aghajanova L, Hoffman J, Mok-Lin E and
Herndon CN: Obstetrics and gynecology residency and fertility
needs. Reprod Sci. 24:428–434. 2017. View Article : Google Scholar
|
|
2
|
Center for Disease Control and Prevention:
Assisted reproductive technology success rates: National summary
and fertility clinic reports. 2016, http://www.cdc.gov/art/pdf/2016-report/ART-2016-National-Summary-Report.pdf.
|
|
3
|
Society for Assisted Reproductive
Technology: National Summary Report. Society for Assisted
Reproductive Technology; 2016, http://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?reportingYear=2016.
|
|
4
|
Agarwal A, Mulgund A, Hamada A and Chyatte
MR: A unique view on male infertility around the globe. Reprod Biol
Endocrinol. 13:372015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Artini PG, Obino ME, Vergine F,
Sergiampietri C, Papini F and Cela V: Assisted reproductive
technique in women of advanced fertility age. Minerva Ginecol.
70:738–749. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhang WG, Zhu SY, Bai XJ, Zhao DL, Jian
SM, Li J, Li ZX, Fu B, Cai GY, Sun XF, et al: Select aging
biomarkers based on telomere length and chronological age to build
a biological age equation. Age (Dordr). 36:96392014. View Article : Google Scholar
|
|
7
|
Pfeiffer V and Lingner J: Replication of
telomeres and the regulation of telomerase. Cold Spring Harb
Perspect Biol. 5:a0104052013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jones MJ, Goodman SJ and Kobor MS: DNA
methylation and healthy human aging. Aging Cell. 14:924–932. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Rizvi S, Raza ST and Mahdi F: Telomere
length variations in aging and age-related diseases. Curr Aging
Sci. 7:161–167. 2014. View Article : Google Scholar
|
|
10
|
Tsatsakis A, Tsoukalas D, Fragkiadaki P,
Vakonaki E, Tzatzarakis M, Sarandi E, Nikitovic D, Tsilimidos G and
Alegakis AK: Developing BIOTEL: A semi-automated spreadsheet for
estimating telomere length and biological age. Front Genet.
10:842019. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Petrakis D, Vassilopoulou L, Mamoulakis C,
Psycharakis C, Anifantaki A, Sifakis S, Docea AO, Tsiaoussis J,
Makrigiannakis A and Tsatsakis AM: Endocrine disruptors leading to
obesity and related diseases. Int J Environ Res Public Health.
14:E12822017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mehrpour O, Karrari P, Zamani N, Tsatsakis
AM and Abdollahi M: Occupational exposure to pesticides and
consequences on male semen and fertility: A review. Toxicol Lett.
230:146–156. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kalliora C, Mamoulakis C, Vasilopoulos E,
Stamatiades GA, Kalafati L, Barouni R, Karakousi T, Abdollahi M and
Tsatsakis A: Association of pesticide exposure with human
congenital abnormalities. Toxicol Appl Pharmacol. 346:58–75. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sifakis S, Androutsopoulos VP, Tsatsakis
AM and Spandidos DA: Human exposure to endocrine disrupting
chemicals: Effects on the male and female reproductive systems.
Environ Toxicol Pharmacol. 51:56–70. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Katsikantami I, Sifakis S, Tzatzarakis MN,
Vakonaki E, Kalantzi OI, Tsatsakis AM and Rizos AK: A global
assessment of phthalates burden and related links to health
effects. Environ Int. 97:212–236. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yawson Emmanuel O, Obasi KK and Lawal I:
Spermatogenic and spermatotoxic effects of Telfairia occidentalis
(Ugu) aqueous leaves extract in adult male Wistar rats (Rattus
novergicus). Toxicol Rep. 5:954–958. 2018. View Article : Google Scholar :
|
|
17
|
Acosta IB, Junior ASV, E Silva EF, Cardoso
TF, Caldas JS, Jardim RD and Corcini CD: Effects of exposure to
cadmium in sperm cells of zebrafish, Danio rerio. Toxicol Rep.
3:696–700. 2016. View Article : Google Scholar
|
|
18
|
Mello MSC, Delgado IF, Favareto APA, Lopes
CMT, Batista MM, Kempinas WD and Paumgartten FJR: Sexual maturation
and fertility of mice exposed to triphenyltin during prepubertal
and pubertal periods. Toxicol Rep. 2:405–414. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Vakonaki E, Tzatzarakis M, Tsiminikaki K,
Nathena D, Fragkiadaki P, Kalliantasi K, Kanaki K, Vaki G, Plaitis
S, Tsoukalas D, et al: Effect of chronic and heavy drug abuse on
biological aging. World Acad J Sci. 1:67–73. 2019.
|
|
20
|
Tsoukalas D, Fragkiadaki P, Docea AO,
Alegakis AK, Sarandi E, Vakonaki E, Salataj E, Kouvidi E, Nikitovic
D, Kovatsi L, et al: Association of nutraceutical supplements with
longer telomere length. Int J Mol Med. 44:218–226. 2019.PubMed/NCBI
|
|
21
|
Shammas MA: Telomeres, lifestyle, cancer,
and aging. Curr Opin Clin Nutr Metab Care. 14:28–34. 2011.
View Article : Google Scholar
|
|
22
|
Valassi E, Crespo I, Santos A and Webb SM:
Clinical consequences of Cushing's syndrome. Pituitary. 15:319–329.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Tedone E, Huang E, O'Hara R, Batten K,
Ludlow AT, Lai TP, Arosio B, Mari D, Wright WE and Shay JW:
Telomere length and telomerase activity in T cells are biomarkers
of high-performing centenarians. Aging Cell. 18:e128592019.
View Article : Google Scholar
|
|
24
|
Kordinas V, Ioannidis A and
Chatzipanagiotou S: The telomere/telomerase system in chronic
inflammatory Diseases Cause or effect? Genes (Basel). 7:E602016.
View Article : Google Scholar
|
|
25
|
Chakravarthi BV, Nepal S and Varambally S:
Genomic and epigenomic alterations in cancer. Am J Pathol.
186:1724–1735. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
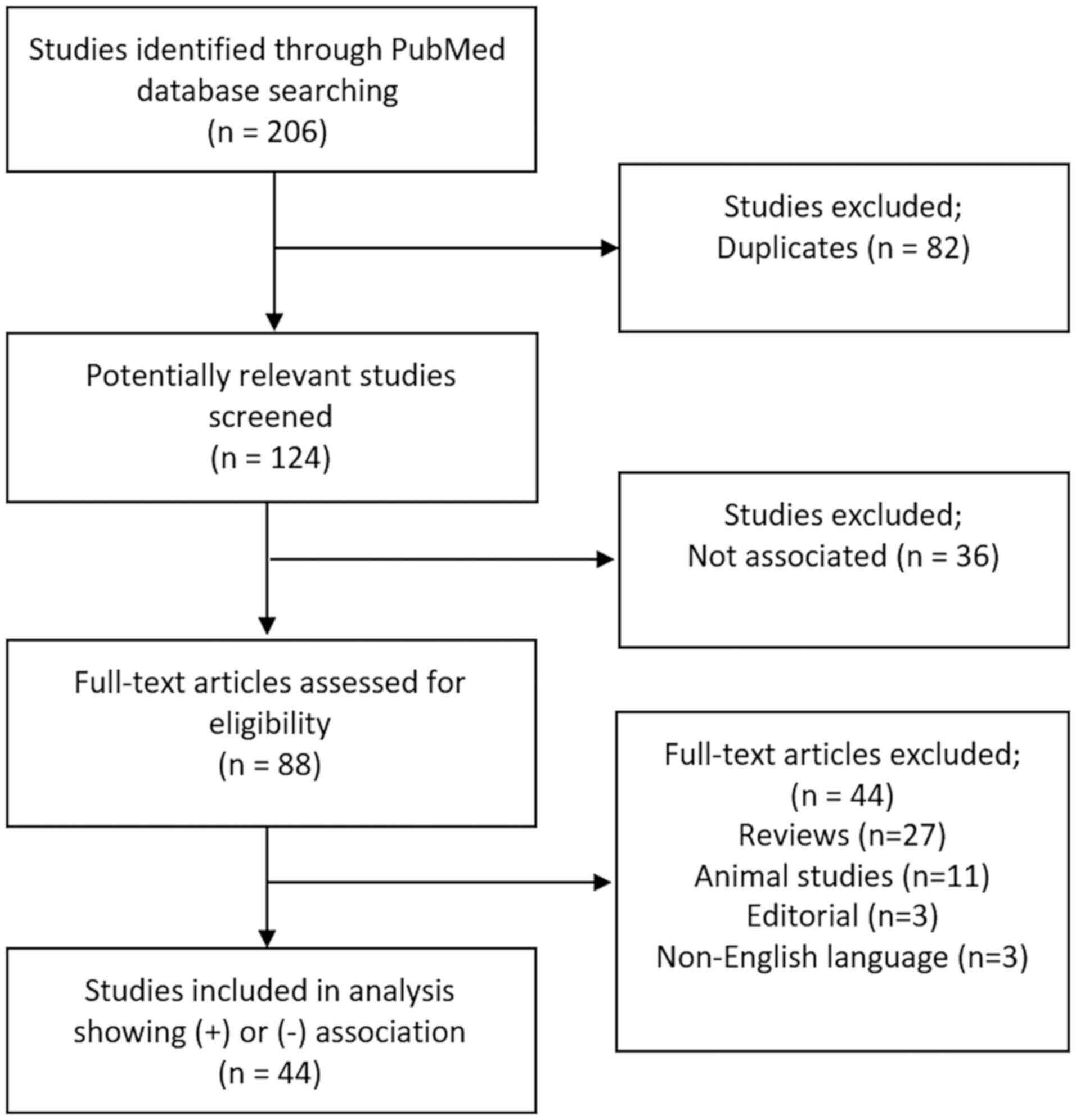
Moher D, Liberati A, Tetzlaff J and Altman
DG; Group P; PRISMA Group: Preferred reporting items for systematic
reviews and meta-analyses: The PRISMA statement. PLoS Med.
6:e10000972009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ma H, Zhou Z, Wei S, Liu Z, Pooley KA,
Dunning AM, Svenson U, Roos G, Hosgood HD III, Shen M, et al:
Shortened telomere length is associated with increased risk of
cancer: A meta-analysis. PLoS One. 6:e204662011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Haycock PC, Heydon EE, Kaptoge S,
Butterworth AS, Thompson A and Willeit P: Leucocyte telomere length
and risk of cardiovascular disease: Systematic review and
meta-analysis. BMJ. 349. pp. g42272014, View Article : Google Scholar
|
|
29
|
Willeit P, Raschenberger J, Heydon EE,
Tsimikas S, Haun M, Mayr A, Weger S, Witztum JL, Butterworth AS,
Willeit J, et al: Leucocyte telomere length and risk of type 2
diabetes mellitus: New prospective cohort study and
literature-based meta-analysis. PLoS One. 9:e1124832014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Aviv A, Kark JD and Susser E: Telomeres,
atherosclerosis, and human longevity: A causal hypothesis.
Epidemiology. 26:295–299. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhang J, Rane G, Dai X, Shanmugam MK,
Arfuso F, Samy RP, Lai MK, Kappei D, Kumar AP and Sethi G: Ageing
and the telomere connection: An intimate relationship with
inflammation. Ageing Res Rev. 25:55–69. 2016. View Article : Google Scholar
|
|
32
|
Parks CG, DeRoo LA, Miller DB, McCanlies
EC, Cawthon RM and Sandler DP: Employment and work schedule are
related to telomere length in women. Occup Environ Med. 68:582–589.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Valentijn AJ, Saretzki G, Tempest N,
Critchley HO and Hapangama DK: Human endometrial epithelial
telomerase is important for epithelial proliferation and glandular
formation with potential implications in endometriosis. Hum Reprod.
30:2816–2828. 2015.PubMed/NCBI
|
|
34
|
Williams CD, Boggess JF, LaMarque LR,
Meyer WR, Murray MJ, Fritz MA and Lessey BA: A prospective,
randomized study of endometrial telomerase during the menstrual
cycle. J Clin Endocrinol Metab. 86:3912–3917. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Hapangama DK, Turner MA, Drury J,
Heathcote L, Afshar Y, Mavrogianis PA and Fazleabas AT: Aberrant
expression of regulators of cell-fate found in eutopic endometrium
is found in matched ectopic endometrium among women and in a baboon
model of endometriosis. Hum Reprod. 25:2840–2850. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Kalyan S, Patel MS, Kingwell E, Côté HCF,
Liu D and Prior JC: Competing factors link to bone health in
polycystic ovary syndrome: Chronic low-grade inflammation takes a
toll. Sci Rep. 7:34322017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Miranda-Furtado CL, Ramos FK, Kogure GS,
Santana-Lemos BA, Ferriani RA, Calado RT and Dos Reis RM: A
nonrandomized trial of progressive resistance training intervention
in women with polycystic ovary syndrome and its implications in
telomere content. Reprod Sci. 23:644–654. 2016. View Article : Google Scholar
|
|
38
|
Pedroso DC, Miranda-Furtado CL, Kogure GS,
Meola J, Okuka M, Silva C, Calado RT, Ferriani RA, Keefe DL and dos
Reis RM: Inflammatory biomarkers and telomere length in women with
polycystic ovary syndrome. Fertil Steril. 103:542–547.e2. 2015.
View Article : Google Scholar
|
|
39
|
Turner S and Hartshorne GM: Telomere
lengths in human pronuclei, oocytes and spermatozoa. Mol Hum
Reprod. 19:510–518. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Pollack AZ, Rivers K and Ahrens KA: Parity
associated with telomere length among US reproductive age women.
Hum Reprod. 33:736–744. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Yu J, Berga SL, Zou W, Sun HY,
Johnston-MacAnanny E, Yalcinkaya T, Sidell N, Bagchi IC, Bagchi MK
and Taylor RN: Gap junction blockade induces apoptosis in human
endometrial stromal cells. Mol Reprod Dev. 81:666–675. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Cheng EH, Chen SU, Lee TH, Pai YP, Huang
LS, Huang CC and Lee MS: Evaluation of telomere length in cumulus
cells as a potential biomarker of oocyte and embryo quality. Hum
Reprod. 28:929–936. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Barha CK, Hanna CW, Salvante KG, Wilson
SL, Robinson WP, Altman RM and Nepomnaschy PA: Number of children
and telomere length in women: A prospective, longitudinal
evaluation. PLoS One. 11:e01464242016. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Czamanski-Cohen J, Sarid O, Cwikel J,
Douvdevani A, Levitas E, Lunenfeld E and Har-Vardi I: Cell-free DNA
and telomere length among women undergoing in vitro fertilization
treatment. J Assist Reprod Genet. 32:1697–1703. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Shalev I, Entringer S, Wadhwa PD,
Wolkowitz OM, Puterman E, Lin J and Epel ES: Stress and telomere
biology: A lifespan perspective. Psychoneuroendocrinology.
38:1835–1842. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Fragkiadaki P, Tsoukalas D, Fragkiadoulaki
I, Psycharakis C, Nikitovic D, Spandidos DA and Tsatsakis AM:
Telomerase activity in pregnancy complications (Review). Mol Med
Rep. 14:16–21. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Perls TT, Alpert L and Fretts RC:
Middle-aged mothers live longer. Nature. 389:1331997. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Sun F, Sebastiani P, Schupf N, Bae H,
Andersen SL, McIntosh A, Abel H, Elo IT and Perls TT: Extended
maternal age at birth of last child and women's longevity in the
Long Life Family Study. Menopause. 22:26–31. 2015. View Article : Google Scholar
|
|
49
|
Fagan E, Sun F, Bae H, Elo I, Andersen SL,
Lee J, Christensen K, Thyagarajan B, Sebastiani P, Perls T, et al
Long Life Family Study: Telomere length is longer in women with
late maternal age. Menopause. 24:497–501. 2017. View Article : Google Scholar :
|
|
50
|
Gray KE, Schiff MA, Fitzpatrick AL, Kimura
M, Aviv A and Starr JR: Leukocyte telomere length and age at
menopause. Epidemiology. 25:139–146. 2014. View Article : Google Scholar :
|
|
51
|
Hapangama DK, Turner MA, Drury JA,
Martin-Ruiz C, Von Zglinicki T, Farquharson RG and Quenby S:
Endometrial telomerase shows specific expression patterns in
different types of reproductive failure. Reprod Biomed Online.
17:416–424. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Butts S, Riethman H, Ratcliffe S, Shaunik
A, Coutifaris C and Barnhart K: Correlation of telomere length and
telomerase activity with occult ovarian insufficiency. J Clin
Endocrinol Metab. 94:4835–4843. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Treff NR, Su J, Taylor D and Scott RT Jr:
Telomere DNA deficiency is associated with development of human
embryonic aneuploidy. PLoS Genet. 7:e10021612011. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Xu X, Chen X, Zhang X, Liu Y, Wang Z, Wang
P, Du Y, Qin Y and Chen ZJ: Impaired telomere length and telomerase
activity in peripheral blood leukocytes and granulosa cells in
patients with biochemical primary ovarian insufficiency. Hum
Reprod. 32:201–207. 2017.
|
|
55
|
Kuhn E, Meeker A, Wang TL, Sehdev AS,
Kurman RJ and Shih IeM: Shortened telomeres in serous tubal
intraepithelial carcinoma: An early event in ovarian high-grade
serous carcinogenesis. Am J Surg Pathol. 34:829–836. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Wei D, Xie J, Yin B, Hao H, Song X, Liu Q,
Zhang C and Sun Y: Significantly lengthened telomere in granulosa
cells from women with polycystic ovarian syndrome (PCOS). J Assist
Reprod Genet. 34:861–866. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Wang C, Shen F, Zhu Y, Fang Y and Lu S:
Telomeric repeat-containing RNA (TERRA) related to polycystic ovary
syndrome (PCOS). Clin Endocrinol (Oxf). 86:552–559. 2017.
View Article : Google Scholar
|
|
58
|
Li Q, Du J, Feng R, Xu Y, Wang H, Sang Q,
Xing Q, Zhao X, Jin L, He L, et al: A possible new mechanism in the
pathophysiology of polycystic ovary syndrome (PCOS): The discovery
that leukocyte telomere length is strongly associated with PCOS. J
Clin Endocrinol Metab. 99:E234–E240. 2014. View Article : Google Scholar
|
|
59
|
Li Y, Deng B, Ouyang N, Yuan P, Zheng L
and Wang W: Telomere length is short in PCOS and oral contraceptive
does not affect the telomerase activity in granulosa cells of
patients with PCOS. J Assist Reprod Genet. 34:849–859. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Hapangama DK, Turner MA, Drury JA, Quenby
S, Saretzki G, Martin-Ruiz C and Von Zglinicki T: Endometriosis is
associated with aberrant endometrial expression of telomerase and
increased telomere length. Hum Reprod. 23:1511–1519. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Sofiyeva N, Ekizoglu S, Gezer A, Yilmaz H,
Kolomuc Gayretli T, Buyru N and Oral E: Does telomerase activity
have an effect on infertility in patients with endometriosis? Eur J
Obstet Gynecol Reprod Biol. 213:116–122. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Valentijn AJ, Palial K, Al-Lamee H,
Tempest N, Drury J, Von Zglinicki T, Saretzki G, Murray P, Gargett
CE and Hapangama DK: SSEA-1 isolates human endometrial basal
glandular epithelial cells: Phenotypic and functional
characterization and implications in the pathogenesis of
endometriosis. Hum Reprod. 28:2695–2708. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Hanna CW, Bretherick KL, Gair JL, Fluker
MR, Stephenson MD and Robinson WP: Telomere length and reproductive
aging. Hum Reprod. 24:1206–1211. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Kuhn E, Meeker AK, Visvanathan K, Gross
AL, Wang TL, Kurman RJ and Shih IeM: Telomere length in different
histologic types of ovarian carcinoma with emphasis on clear cell
carcinoma. Mod Pathol. 24:1139–1145. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Keefe DL, Liu L and Marquard K: Telomeres
and aging-related meiotic dysfunction in women. Cell Mol Life Sci.
64:139–143. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Kalmbach KH, Antunes DM, Kohlrausch F and
Keefe DL: Telomeres and female reproductive aging. Semin Reprod
Med. 33:389–395. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Keefe DL and Liu L: Telomeres and
reproductive aging. Reprod Fertil Dev. 21:10–14. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Yang Q, Zhao F, Dai S, Zhang N, Zhao W,
Bai R and Sun Y: Sperm telomere length is positively associated
with the quality of early embryonic development. Hum Reprod.
30:1876–1881. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Reig-Viader R, Capilla L, Vila-Cejudo M,
Garcia F, Anguita B, Garcia-Caldés M and Ruiz-Herrera A: Telomere
homeostasis is compromised in spermatocytes from patients with
idiopathic infertility. Fertil Steril. 102:728–738.e1. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Yan L, Wu S, Zhang S, Ji G and Gu A:
Genetic variants in telomerase reverse transcriptase (TERT) and
telomerase-associated protein 1 (TEP1) and the risk of male
infertility. Gene. 534:139–143. 2014. View Article : Google Scholar
|
|
71
|
Ferlin A, Rampazzo E, Rocca MS, Keppel S,
Frigo AC, De Rossi A and Foresta C: In young men sperm telomere
length is related to sperm number and parental age. Hum Reprod.
28:3370–3376. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Thilagavathi J, Kumar M, Mishra SS,
Venkatesh S, Kumar R and Dada R: Analysis of sperm telomere length
in men with idiopathic infertility. Arch Gynecol Obstet.
287:803–807. 2013. View Article : Google Scholar
|
|
73
|
Prescott J, Du M, Wong JY, Han J and De
Vivo I: Paternal age at birth is associated with offspring
leukocyte telomere length in the nurses' health study. Hum Reprod.
27:3622–3631. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Moskovtsev SI, Willis J, White J and
Mullen JB: Disruption of telomere-telomere interactions associated
with DNA damage in human spermatozoa. Syst Biol Reprod Med.
56:407–412. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Baird DM, Britt-Compton B, Rowson J, Amso
NN, Gregory L and Kipling D: Telomere instability in the male
germline. Hum Mol Genet. 15:45–51. 2006. View Article : Google Scholar
|
|
76
|
Biron-Shental T, Wiser A, Hershko-Klement
A, Markovitch O, Amiel A and Berkovitch A: Sub-fertile sperm cells
exemplify telomere dysfunction. J Assist Reprod Genet. 35:143–148.
2018. View Article : Google Scholar :
|
|
77
|
Vecoli C, Montano L, Borghini A, Notari T,
Guglielmino A, Mercuri A, Turchi S and Andreassi MG: Effects of
highly polluted environment on sperm telomere length: A Pilot
Study. Int J Mol Sci. 18:E17032017. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Lafuente R, Bosch-Rue E, Ribas-Maynou J,
Alvarez J, Brassesco C, Amengual MJ, Benet J, Garcia-Peiró A and
Brassesco M: Sperm telomere length in motile sperm selection
techniques: A qFISH approach. Andrologia. 50:e128402018. View Article : Google Scholar
|
|
79
|
Cariati F, Jaroudi S, Alfarawati S, Raberi
A, Alviggi C, Pivonello R and Wells D: Investigation of sperm
telomere length as a potential marker of paternal genome integrity
and semen quality. Reprod Biomed Online. 33:404–411. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Mishra S, Kumar R, Malhotra N, Singh N and
Dada R: Mild oxidative stress is beneficial for sperm telomere
length maintenance. World J Methodol. 6:163–170. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Rocca MS, Speltra E, Menegazzo M, Garolla
A, Foresta C and Ferlin A: Sperm telomere length as a parameter of
sperm quality in normozoospermic men. Hum Reprod. 31:1158–1163.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Liu SY, Zhang CJ, Peng HY, Huang XQ, Sun
H, Lin KQ, Huang K, Chu JY and Yang ZQ: Association study of
telomere length with idiopathic male infertility. Yi Chuan.
37:1137–1142. 2015.In Chinese. PubMed/NCBI
|
|
83
|
Antunes DM, Kalmbach KH, Wang F, Dracxler
RC, Seth-Smith ML, Kramer Y, Buldo-Licciardi J, Kohlrausch FB and
Keefe DL: A single-cell assay for telomere DNA content shows
increasing telomere length heterogeneity, as well as increasing
mean telomere length in human spermatozoa with advancing age. J
Assist Reprod Genet. 32:1685–1690. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Yang Q, Zhang N, Zhao F, Zhao W, Dai S,
Liu J, Bukhari I, Xin H, Niu W and Sun Y: Processing of semen by
density gradient centrifugation selects spermatozoa with longer
telomeres for assisted reproduction techniques. Reprod Biomed
Online. 31:44–50. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Yang Q, Luo X, Bai R, Zhao F, Dai S, Li F,
Zhu J, Liu J, Niu W and Sun Y: Shorter leukocyte telomere length is
associated with risk of nonobstructive azoospermia. Fertil Steril.
110:648–654.e1. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Heidary H, Pouresmaeili F, Mirfakhraie R,
Omrani MD, Ghaedi H, Fazeli Z, Sayban S, Ghafouri-Fard S, Azargashb
E and Shokri F: An association study between longitudinal changes
of leukocyte telomere and the risk of azoospermia in a population
of Iranian infertile men. Iran Biomed J. 22:231–236. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Jørgensen PB, Fedder J, Koelvraa S and
Graakjaer J: Age-dependence of relative telomere length profiles
during spermatogenesis in man. Maturitas. 75:380–385. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Pech MF, Garbuzov A, Hasegawa K, Sukhwani
M, Zhang RJ, Benayoun BA, Brockman SA, Lin S, Brunet A, Orwig KE,
et al: High telomerase is a hallmark of undifferentiated
spermatogonia and is required for maintenance of male germline stem
cells. Genes Dev. 29:2420–2434. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Ling X, Zhang G, Chen Q, Yang H, Sun L,
Zhou N, Wang Z, Zou P, Wang X, Cui Z, et al: Shorter sperm telomere
length in association with exposure to polycyclic aromatic
hydrocarbons: Results from the MARHCS cohort study in Chongqing,
China and in vivo animal experiments. Environ Int. 95:79–85. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Liu M, Hales BF and Robaire B: Effects of
four chemotherapeutic agents, bleomycin, etoposide, cisplatin, and
cyclophosphamide, on DNA damage and telomeres in a mouse
spermatogonial cell line. Biol Reprod. 90:722014. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Dracxler RC, Oh C, Kalmbach K, Wang F, Liu
L, Kallas EG, Giret MT, Seth-Smith ML, Antunes D, Keefe DL, et al:
Peripheral blood telomere content is greater in patients with
endometriosis than in controls. Reprod Sci. 21:1465–1471. 2014.
View Article : Google Scholar : PubMed/NCBI
|