Introduction
A variety of electrical therapies applying different
signal types and treatment protocols are currently used in clinical
practice. Electrotherapy has been reported effective in the
treatment of pain, blood flow promotion, decreased tone of skeletal
striated muscle, metabolism acceleration and resorption of edema
and joint effusion (1,2). Also, some electrotherapeutic
techniques have been assayed recently for treatment of different
cancer types (3–7). The present study investigates the
cellular response to electrical stimuli currently used in
electrothermal therapies that apply the capacitive-resistive
electric transfer (CRET) technique. This non-invasive therapy is
based on localized hyperthermia induced in inner tissues when
exposed to sine wave electric currents with frequencies between
0.45 and 0.60 MHz. Such currents, which are delivered through
movable electrode pairs applied to the epidermis, induce a thermal
Joule's effect in the targeted organs due to the electric
resistivity of the tissues (8).
Preliminary assays of CRET therapy on cancer
patients showed consistent signs of slowing down the growth of the
tumor tissues, without adversely affecting the surrounding healthy
tissues (9–11). Similar effects have been reported
in response to other therapies based on capacitive hyperthermia
(12–14). Although these and other medical
effects of electro-thermal therapies have been widely described,
the cellular and molecular mechanisms involved in the biological
responses to electric currents applied by such therapies have only
recently begun to be studied (15–19).
The clinical and experimental evidence suggests that
the therapeutic action of the CRET currents within the 0.45–0.60
MHz spectrum, might be exerted not only through heating of the
treated tissues, but also by a direct, cellular or tissue response
to the electric stimuli. It is indicated by previously reported
results that exposure to 0.57–MHz currents at subthermal densities
can induce cytostasis in the human hepatocarcinoma cell line HepG2
(16). Such effect is expressed as
a decline in cell proliferation, induced by changes in expression
and activation of cell cycle control proteins, cyclins D1, A and
B1, and of the cell cycle inhibitor protein
p27Kip1(17). These
data indicate that the cytostatic action of CRET currents applied
to subthermal doses could be mediated by alterations in cell cycle
regulation.
On the other hand, preliminary data indicate that
stimulation with the above described electric parameters could
exert a partial cytotoxic action on the human neuroblastoma cell
line NB69, whose proliferation rate is higher than that of the
HepG2 line. This cytotoxic response is expressed as an increased
rate of cell death, accompanied with changes in the levels of total
proteins and DNA in the cultures (15). The aim of the present work is to
study the nature of the cytotoxic response observed in the
neuroblastoma cell line, investigating whether the electric
stimulation can deregulate the cell cycle of NB69 by inducing
changes similar to those described in the line HepG2 (16,17).
Additionally, it is important to elucidate whether subthermal
stimulation with CRET signal can induce in normal, nontumoral human
cells, cytotoxic or cytostatic responses similar to those described
in human cancer cells. In this regard, it is of particular interest
to determine whether the electric stimulation could alter the
viability of immune cells, since they can participate in cancer
control through tumor antigen recognition. Consequently, this work
further addresses characterization of the cellular response to CRET
currents by studying their potential effects on primary cultures of
peripheral blood mononuclear cells (PBMC) from healthy donors.
The obtained results support our preliminary data,
confirming that subthermal treatment with 0.57 MHz currents induces
a partial cytotoxic response in NB69 cells. Also, a cytostatic
response potentially due to alterations in cell cycle kinetics was
observed. These results, together with the previously reported
effects on the HepG2 cells, suggest that treatment with subthermal
doses of 0.57 MHz could exert antiproliferative effects on two
separate human cell lines of cancer origin. Such effects appear to
be due to interference of the electric stimulus with mechanisms
involved in the cell cycle regulation of both cell lines. By
contrast, viability of PBMC from healthy donors was not affected by
exposure to the same electric parameters. As a whole, our results
support the hypothesis that the therapeutic action of
thermoelectric treatments of the CRET type is mediated, at least in
part, by a direct cellular response to the electric stimulus, being
the proliferative lines more sensitive than the non-proliferating
PBMC. The effect at the cellular level could act in synergy with
the thermal action at the tissue level, exerted by the current when
passing through tissues with a relatively high electric
resistivity.
Materials and methods
Cell cultures
Cells of the human neuroblastoma line NB69 were
maintained in D-MEM supplemented with 15% (vol/vol) foetal bovine
serum (FBS), L-glutamine (4 mM) and penicillin-streptomycin with
Fungizone (100 U/ml) (all from Gibco, Paisley, UK). Cells were
seeded in 60 mm Ø Petri dishes (Nunc, Roskilde, Denmark), at a
5x104 cells/ml. Ten total dishes per experimental
replicate were seeded, five for treatment and five controls, and
maintained in culture for 4 days with 5% CO2 at 37°C.
The culture medium was renewed every 3 days. For BrdU assay and
immunocytochemical analysis, cells were seeded on coverslips (Ø 12
mm) placed inside the Petri dishes.
Buffy coat from whole blood obtained from healthy
donors was used as the source of PBMC. Samples from ten donors were
used. PBMC were isolated by centrifugation in Ficoll-Hypaque
density gradient (Lymphoprep, Nycomed, Zurich, Switzerland), using
the method described by Boyum in 1968 (20), and maintained in RPMI supplemented
with 10% fetal bovine serum, 1% L-glutamine, 0.1% gentamicine (all
from Gibco) and 1% penicillin-streptomycin (ICN, OH, USA). Once
isolated, the PBMC were seeded on 60 mm Ø Petri dishes (Corning NY,
USA) at a density of 2.75x106 cells/ml. Twenty total
dishes were seeded per experimental replicate, ten dishes for
treatment and ten controls. Before stimulation, cultures were
incubated for 1 h in a 5% CO2 atmosphere at 37°C.
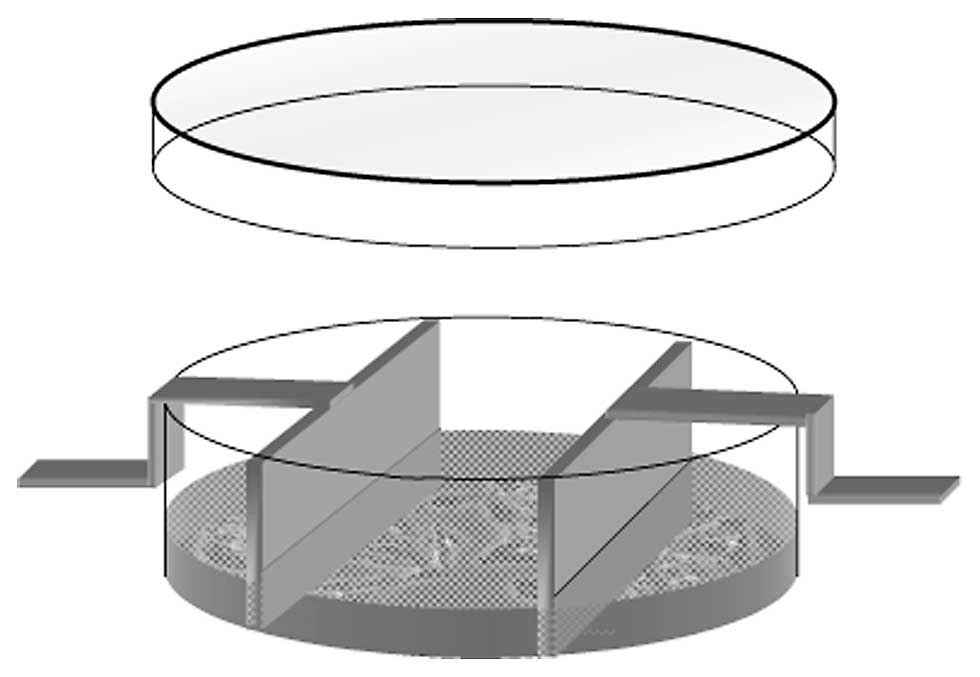
Exposure system and experimental
protocol
The exposure system has been described in detail in
previous reports (16,17). Briefly, the exposure to 0.57 MHz
electric currents was carried out through pairs of sterile
stainless steel electrodes, designed ad hoc for in
vitro stimulation, inserted inside each of the control and
exposed Petri dishes (Fig. 1). In
the experimental groups, the electrode pairs were connected in
series to a signal generator (model M-500, INDIBA S.A., Barcelona,
Spain). The stimulation pattern consisted of a 5-min pulse of 0.57
MHz, sine wave currents, delivered every 4 h along a 24-h period.
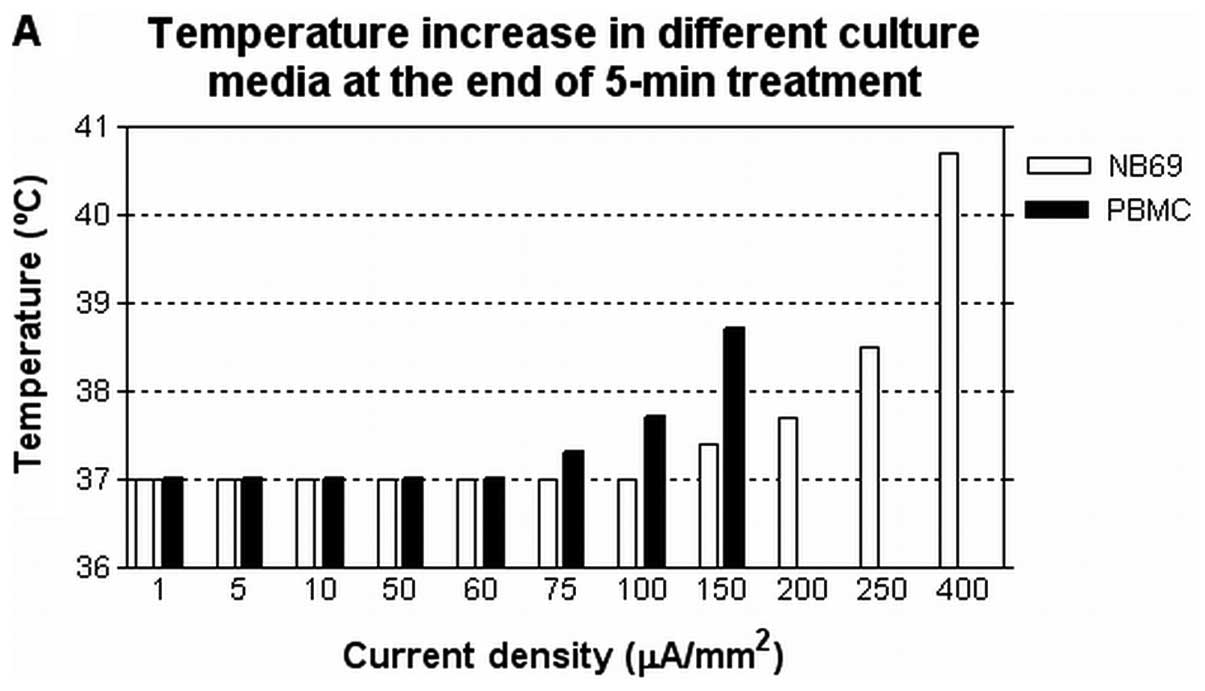
The current density values to be tested were selected from
recordings of the temperature induced by the electric current
flowing through the culture medium (Fig. 2). In the present work, we studied
the viability and proliferation of NB69 cells stimulated with
different subthermal current densities, between 1 and 100
μA/mm2, and with a thermal density of 400
μA/mm2. For PBMC assays, only the 50 μA/mm2
current density, which had proven effective in our previously
published studies, was applied. The signal parameters as well as
temperature, relative humidity and CO2 partial pressure
into incubators were monitored during experiments. In NB69 assays,
the electric treatment started at day four post-seeding, during
exponential cell growth phase, and finished 24 h after, at day five
post-seeding. To study the chronology of the NB69 response,
analyses were carried out at the beginning of exposure (0 h),
during the treatment (at 6 or 12 h), at the end of treatment (24 h)
and after two days of post-exposure incubation (72 h). For PBMC,
after 1 h of post-seeding incubation, the cell cultures were
electrically stimulated with 5-min pulses for 24 h. At the end of
treatment the cells were harvested for analysis. All experimental
procedures were carried out in blind condition for treatment.
Artifact control
To verify that the cellular responses obtained were
induced exclusively by the electric stimuli, and not by other,
uncontrolled environmental factors, assays were conducted on the
influence of the non-energized electrodes on cell viability. Also,
a number of potentially influencing factors were studied, including
the electrochemical integrity of the electrodes, electrophoretic
effects, electromagnetic fields and thermal effects. The procedures
applied have been described in previous studies (16) and the data (not shown) confirmed
that none of the studied factors changed significantly either the
physical/chemical properties of the culture medium or the cellular
behaviour.
Effects on the cell viability of NB69
cultures
The effect of 1, 5, 10, 50, 100 or 400
μA/mm2 stimuli on the cell viability of NB69 was studied
through dye exclusion with 0.4% trypan blue (Sigma, Steinheim,
Germany) at the end of the electric treatment. Three experimental
replicates were conducted for each of the assayed current
densities.
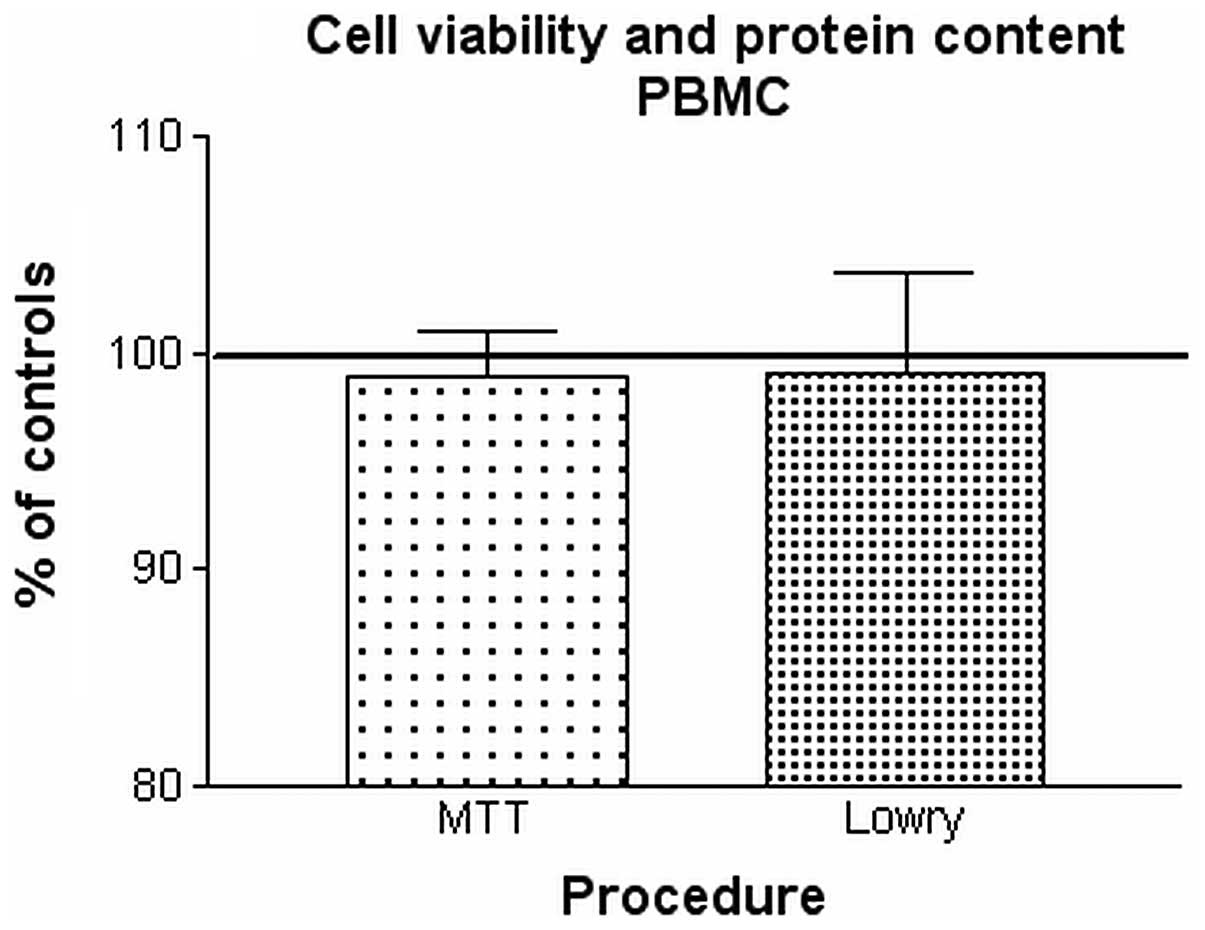
Effects on cellular viability of PBMC
culture
For PBMC, samples stimulated with 50
μA/mm2 and their respective controls were harvested at
the end of 24 h of intermittent treatment. Cell viability of the
PBMC cultures was quantified by trypan blue exclusion method,
following the same protocol as for NB69. Ten independent analysis
were carried out, one for each of the obtained blood samples. MTT
assay (Roche, Indianapolis, IN, USA) was applied following the
manufacturer's instructions, to confirm the trypan blue data. MTT
quantification was carried out on samples from two different
donors, using ELISA reader at 600 nm. As complementary assay, and
in order to study the cell density, the total protein content of
the cultures was quantified through the Lowry method, following
protocols described in previous reports (15,16).
Seven independent samples from seven different donors were
analyzed.
BrdU assay of NB69
On the basis of our previous data on the responses
electrically induced in lines NB69 and HepG2 (16,17),
a current density of 50 μA/mm2 was chosen to conduct
this assay. The effects of the exposure on cell proliferation of
NB69 were analyzed through 5-bromo-2′-deoxyuridine assay, following
the protocol described by Hernández-Bule et al(16). Briefly, just before stimulation
onset (0 h), the dishes were incubated with 5-bromo-2′-deoxyuridine
(Dako, Denmark) at a 5x10−4 M concentration. At the end
of the 24 h of exposure and/or incubation, the cells were fixed
with 4% paraformaldehyde (Merck, Darmstadt, Germany) and incubated
with monoclonal primary antibody anti-BrdU (Dako) and anti-mouse Ig
flourescein-linked whole antibody as secondary antibody (Amersham
Biosciences, Buckinghamshire, UK). The preparations were
counterstained and mounted in glycerol with Hoechst 33342
fluorescence dye (Bisbenzimide, Sigma) and studied through
fluorescence microscopy (Nikon Eclipse TE300; Melville, USA) and
Computer-Assisted Image Analysis (Analy-SIS, GMBH, Munich,
Germany). Three experimental replicates were carried out, and about
7200 cells were studied per experimental group.
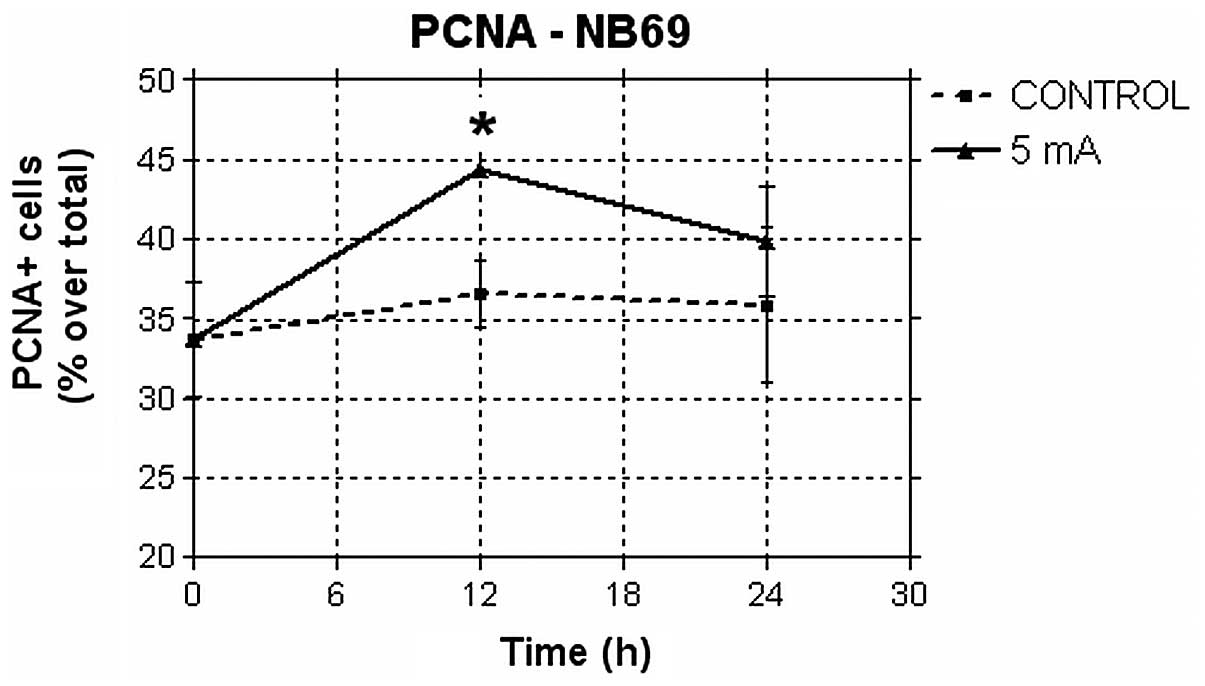
PCNA immunofluorescence of NB69
The proliferating cell nuclear antigen (PCNA) was
used to estimate potential changes induced in DNA content at
specific time intervals. Cells were grown on 12-mm Ø coverslips
placed on the bottom of the Petri dishes, on the surface between
electrodes. The samples treated with 50 μA/mm2 and their
controls were fixed with 4% paraformaldehyde (Merck). The cells
were permeabilized and incubated overnight at 4°C with primary
monoclonal antibody anti-PCNA (Santa Cruz Biotechnology, Santa
Cruz, CA, USA). After washing, the cells were incubated with
secondary antibodies conjugated to Alexa Green dye (Molecular
Probes, CA, USA), counterstained and mounted in glycerol with
Hoechst 33342 (Sigma). The samples were analyzed through
fluorescence microscopy (Nikon) and computer-assisted image
analysis (Analy-SIS, GMBH). Four experimental repeats were
conducted and two coverslips were analyzed per experimental group,
one for each of the studied time intervals (0, 12 or 24 h). The
percent of PCNA-positive cells and the total nuclei (revealed with
Hoechst 33342, Sigma) were recorded in 15 randomly selected fields
per coverslip, and a total of ∼5,000 cells per experimental group
were evaluated.
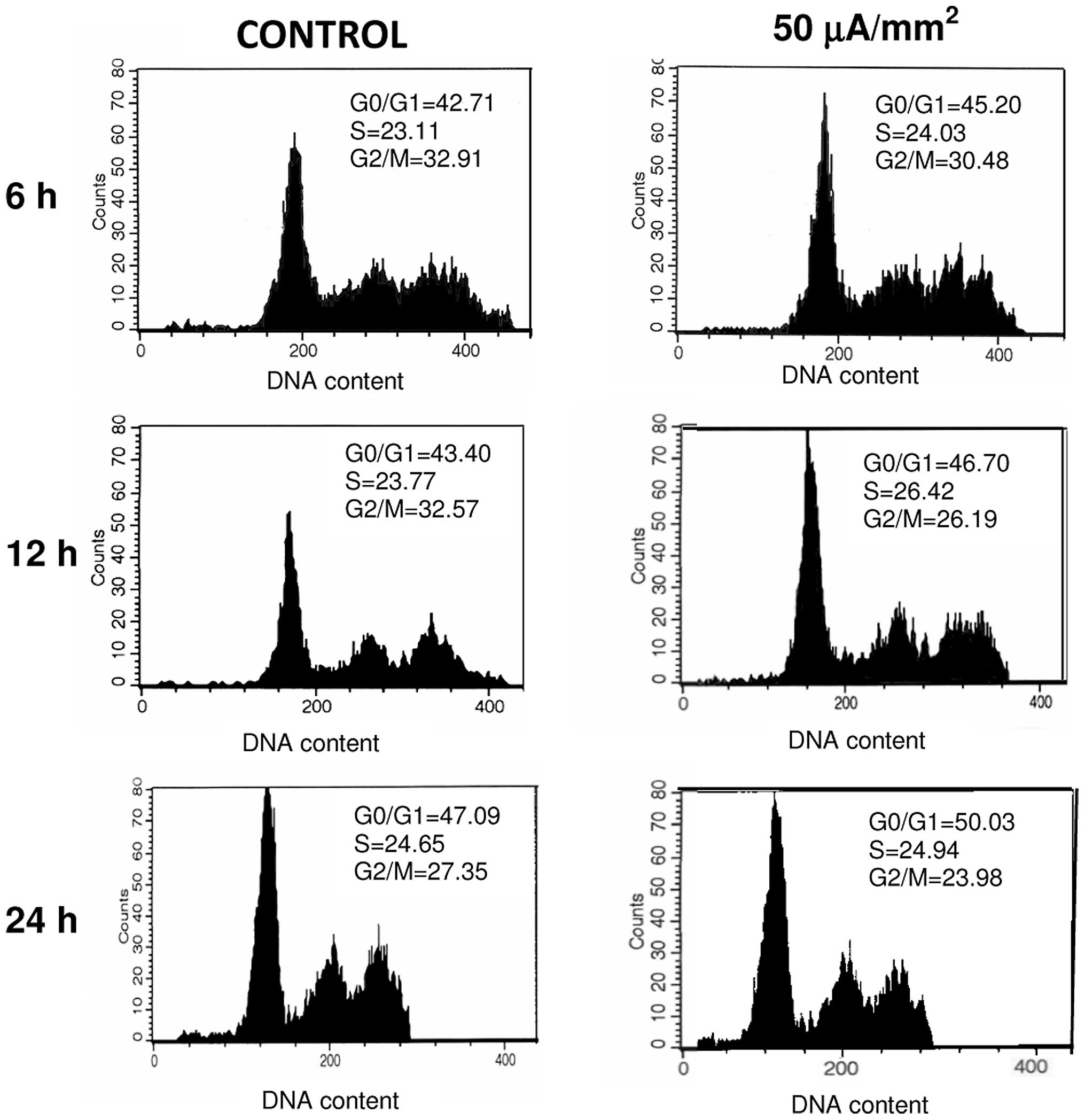
Flow cytometric analysis of effects on
apoptosis and cell cycle of NB69
After 6, 12 or 24 h of 50 μA/mm2 exposure
and/or incubation, neuroblastoma samples were fixed with 70%
ethanol as described in previous studies (16). The relative fractions of cellular
subpopulations in different phases of the cell cycle, including the
sub-G1 population (cells with less than stationary cell
complement of DNA), a qualitative indicator of apoptotic cells,
were determined. A minimum of 2 experimental replicates were
conducted for each of the three temporal intervals analyzed. The
cell cycle kinetics was determined by CellQuest 3.2 software
(Becton-Dickinson).
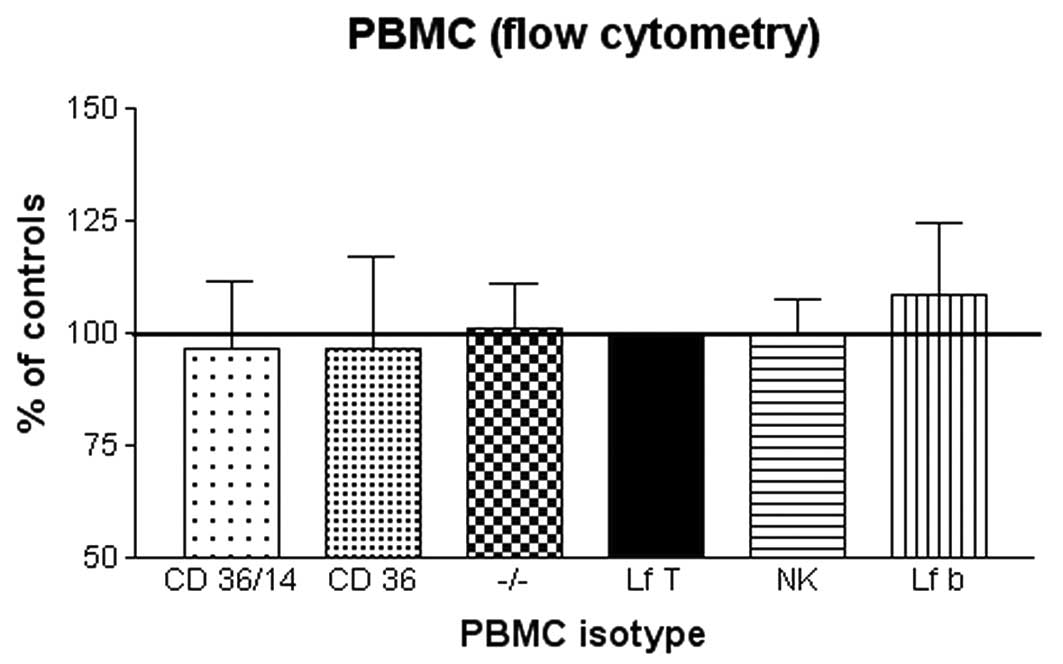
Flow cytometric analysis of PBMC
subpopulations
In order to detect potential, electrically-induced
changes in the relative rates of T lymphocytes, B lymphocytes,
natural killer cells and cells with monocytic phenotype, antibodies
anti-CD14 linked to phycoerytrin (PE), anti-CD36 linked to
fluorescein isothiocyanate (FITC), anti-CD56 linked to phycoerytrin
and anti-CD3 linked to allophycocyanin (APC) (all from
Becton-Dickinson, Franklin Lakes, NJ, USA) were used. The B
lymphocyte fraction was estimated by exclusion of the enumerated
subpopulations. Cell suspension samples (1x106 cells per
sample) were collected after 24 h of sham or intermittent
stimulation with 50 μA/mm2 and incubated with the
corresponding antibodies, in the dark and at room temperature, for
30 min. Flow cytometry of PBMC from two donors was carried out
using Becton-Dickinson FACScan (FACScalibur, Becton-Dickinson).
Twenty thousand events (cells) per cell suspension were
analyzed.
Statistical analysis
Data were analyzed using unpaired, two-tailed
Student's t-test. Differences p<0.05 were considered
statistically significant.
Results
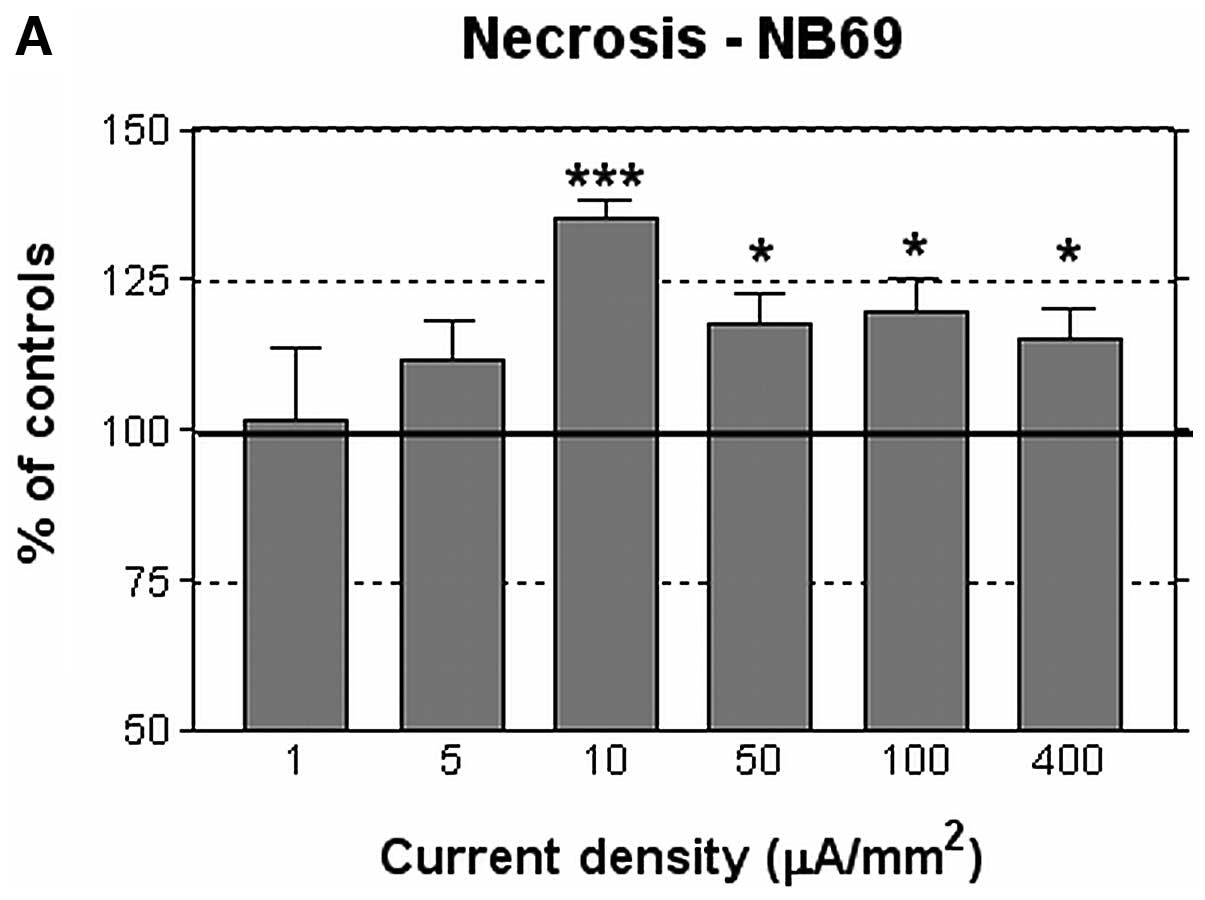
Effects on NB69 cell viability as a
function of current density
In the assayed culture conditions, the average rate
of necrosis in the control NB69 samples after 24 h of incubation in
the presence of electrode pairs was 14±1%. This survival rate
corresponds to that classically reported in the literature for NB69
cells incubated in normal, control conditions (21). At the end of the 24 h of
intermittent treatment with current densities j ≥10
μA/mm2, the rate of necrosis had increased
significantly, by 18–35% over that of the corresponding controls
samples (Fig. 3A). This cytotoxic
effect was not linearly related to the current density. In fact,
the 400 μA/mm2 current, which as shown in Fig. 2B, increased by 3.5°C the
temperature of the medium at the end of each 5-min exposure pulses,
induced cytotoxicity rates equal or below those induced by weaker
densities. Densities j ≤5 μA/mm2 did not induce
significant changes in the rate of necrosis when compared to
controls. Regarding the rate of viability of treated cultures, in
general it was slightly reduced, ∼7% below controls. The effect
reached statistical significance only for the thermal dose of 400
μA/mm2 (Fig. 3B).
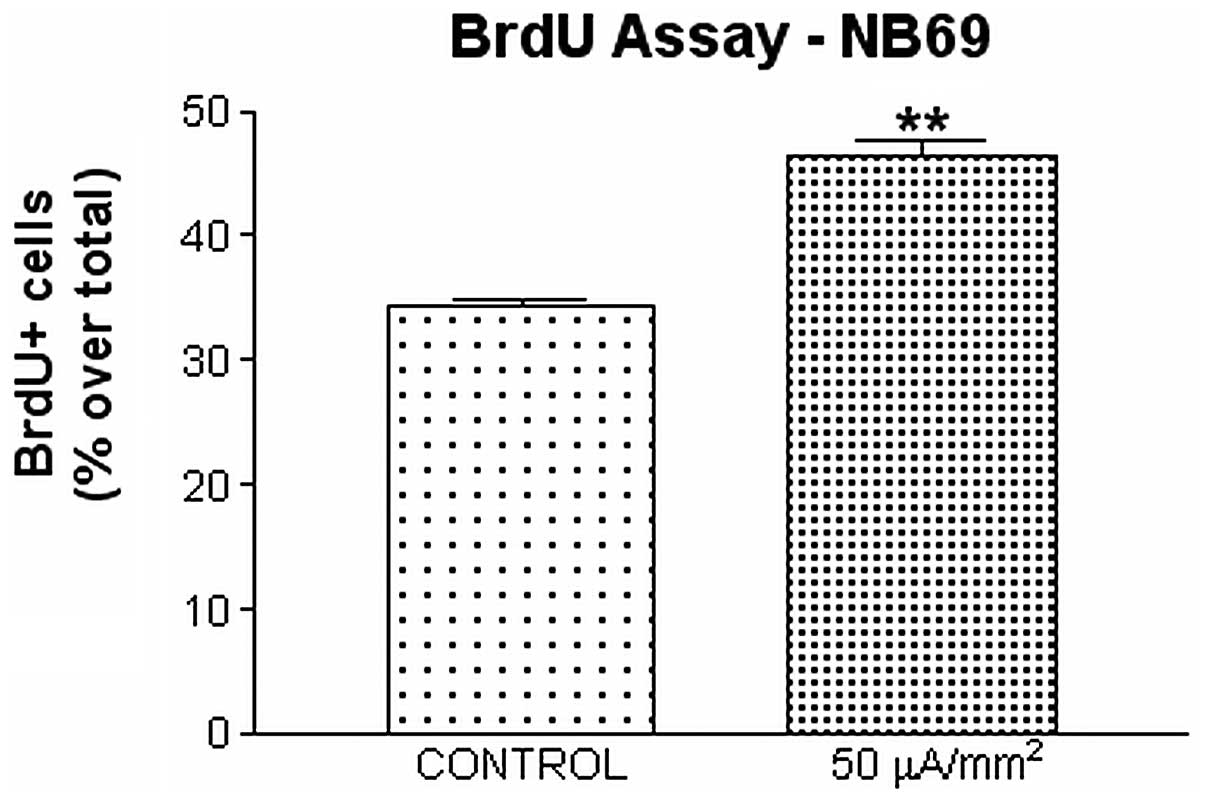
Effects of the 50 μA/mm2
electric current on DNA synthesis in NB69
Our previous studies have reported that
hepatocellular carcinoma cells are sensitive to exposure to 50
μA/mm2 CRET currents (17). From those data and from the results
described in the preceding paragraph on NB69 cell viability at the
end of the electric treatment, it was decided that all further
trials would be conducted at a current density of 50
μA/mm2. DNA synthesis was quantified through two
complementary techniques: quantification of BrdU incorporation
during the 24 h of intermittent treatment, and study of the levels
of expression of proliferating cell nuclear antigen PCNA before (0
h), during (12 h) and at the end of the exposure period (24 h). The
data showed that 24 h of treatment with the 50 μA/mm2
current significantly increased BrdU incorporation in NB69 cells
(35.08% over controls; 0.001<p<0.01; Fig. 4), which indicates that the electric
stimulus enhances DNA synthesis. The immunofluorescence assay for
PCNA reinforced this evidence by showing a significant increase
(21.49% over controls, 0.01 < p<0.05) in the percent of cells
expressing this antigen at 12 h after treatment onset. The
increased expression of PCNA seemed to last until the end of 24 h
of treatment (11.14% over controls), although at that point the
differences between the stimulated samples and their controls did
not reach statistical significance (Fig. 5).
Effects of the 50 μA/mm2
electric current on the cell cycle of NB69
As described above, the rate of cell death in NB69
was significantly increased at the end of the 24-h intermittent
stimulation (Fig. 3A). On the
other hand, the treatment also induced an increase in DNA synthesis
through BrdU incorporation (Fig.
4) as well as increased rate of PCNA-positive cells (Fig. 5), which could be indicative of a
cytoproliferative response. To elucidate the causes of such
apparent contradiction, we studied the cell cycle through flow
cytometry, during the treatment (6 and 12 h after the exposure
onset) and at the end of the treatment (24 h). The results of the
analysis showed a modest increase, non-significant statistically,
of cells in S phase after 6 h of exposure, when compared to the
corresponding sham samples (Fig. 6
and Table I). After six additional
hours of treatment, the fraction of the cellular population in S
phase did not differ from that of the control samples, but a
statistically significant decrease in the rate of cells in
G2/M (17.9% below controls, 0.01< p<0.05) was
detected in the exposed group. At the end of 24 h of treatment no
significant differences were detected with respect to controls.
These results may indicate that the electric stimulation induced
either a blocking of the cell cycle in S phase, or a prolongation
of S phase and, hence, of the time necessary to complete a cycle.
This is consistent with the peak of DNA synthesis observed at 12
and 24 h of treatment, as revealed both by PCNA immunofluorescence
and BrdU incorporation (Figs. 4
and 5).
 | Table ITreatment-induced changes in the cell
cycle of NB69. |
Table I
Treatment-induced changes in the cell
cycle of NB69.
| Time (h) | No. of experimental
replicates | %
G0/G1 phase | % S phase | % G2/M
phase |
|---|
| 6 | 2 | 108.9±4.4 | 115.2±15.9 | 111.9±27.3 |
| 12 | 2 | 103.7±5.5 | 101.0±14.4 | 82.1±2.3a |
| 24 | 3 | 97.6±9.8 | 111.1±17.0 | 107.1±24.5 |
Besides, the graphs in Fig. 6 revealed absence of the DNA
sub-G1 peak, a qualitative indicator of apoptosis. This
suggests that the electric treatment does not induce apoptosis
during the studied intervals. Additional, more specific tests and a
study of apoptosis after the treatment would be needed to confirm
these indications.
Effects of the 50 μA/mm2
electric current on the viability of PBMC
In contrast to the response of neuroblastoma cells,
exposure to 50 μA/mm2 did not change significantly the
survival and necrosis rates in PBMC, as revealed by trypan blue
exclusion technique (Table II).
The supplementary analysis by MTT assay also showed no significant
changes with respect to controls in the viability of treated PBMC
samples. As for the cell density, determined through quantitative
analysis of protein levels, no significant differences were
detected between exposed samples and their respective controls
(Fig. 7).
 | Table IIPBMC viability before and after
treatment. |
Table II
PBMC viability before and after
treatment.
| Time after seeding
(h) | Electrodes
present | Current density
(μA/mm2) | Viable cells per
dish (n) | Necrotic cells per
dish (n) |
|---|
| 0 | No | 0 |
11.0x106±0.0 | 1.0x103
±0.0 |
| 1 | No | 0 |
10.9x106±0.0 |
30.0x103±3.0x103 |
| 24 | Yes | 0 |
7.2x106±0.4x106 |
254.2x103±70.2x103 |
| 24 | Yes | 50 |
7.9x106±0.6x106 |
302.1x103±17.8x103 |
Flow cytometric analysis of the response
of PBMC subpopulations to the 50 μA/mm2 current
PBMC populations are composed of cellular
subpopulations of different isotypes of monocytes and lymphocytes.
In order to study potential treatment-induced alterations in
specific cell subpopulations, different cell samples from two
healthy donors were analyze by flow cytometry. At the end of the 24
h of intermittent treatment no significant changes were found in
the distribution or the relative rate of any of the cell
subpopulations (Fig. 8). These
results are consistent with those on viability and cell density,
and reinforce the indications that PBMC from healthy donors do not
respond to subthermal levels of 0.57 MHz electric currents.
Discussion
Electrothermal CRET therapies induce hyperthermia in
deep tissues by transdermal application of electric currents within
the 0.45–0.6 MHz frequency range. Pilot trials on patients with
glioblastoma multiforme have reported that CRET treatment can
reduce peritumoral edema and intratumoral vascularization, and
induce extensive necrosis in the tumor core and significant tumor
growth reduction, without affecting the surrounding healthy brain
tissue (9). More recently, Kato
et al(22) have shown that
CRET treatment administered at thermal doses can significantly
potentiate the anticancer effect of 6-O-palmitoyl-ascorbate on
human tongue squamous carcinoma cells. Moreover, recent
experimental studies by our group have shown that in vitro
stimulation with subthermal doses of 0.57 MHz, CRET electric
currents, induces partial cytostasis in the human hepatocarcinoma
cell line HepG2 (16). This
cytostasis would be mediated by alterations, also induced by the
CRET treatment, in the expression and activation of cell cycle
control proteins (cyclins D1, A, B1 and p27), and such alterations
lead to a blockage or slowing down of the G1 and S
phases of the cell cycle of HepG2 (17). Prior, preliminary studies by
Hernández-Bule et al(15)
had reported that the same 0.57 MHz signal administered at
non-thermal or subthermal doses, could exert cytotoxic effects in
neuroblastoma cells. The results of the present study confirm such
cytotoxic response in a fraction of the NB69 population. The effect
manifests as significant increases in the rate of necrosis, which
at least within the tested density range, are not linearly
dependent on the applied current density (Fig. 3A). This reinforces the hypothesis
that the cellular response to the electric stimulus is different,
and at some extent independent, of the thermal effects attributed
to electrothermal therapies.
Multiple cellular pathways leading to cell death
have been described, including perturbation of ion homeostasis,
activation of proteases and phospholipases, degradation of DNA and
generation of reactive oxygen intermediates (23). The molecular basis of the cytotoxic
action exerted by CRET currents remain to be elucidated. However,
it might be related with electrically-induced alterations in the
expression or activation of one or more proteins involved in the
cell cycle regulation, as described by Hernández-Bule et al
and Wang et al(17,18).
In addition to the described effects on cell
viability, the present results show that intermittent treatment
with the 0.57 MHz currents significantly increases DNA levels in
NB69, since a significant increase in BrdU incorporation into the
DNA was detected at the end of the 24 h of treatment. Additionally,
we found a significant increase in the expression of proliferating
cell nuclear antigen after 12-h exposure, which appears to last
until the end of treatment, even if at 24 h the difference with
respect to controls did not reach statistical significance. PCNA is
an auxiliary protein of DNA polymerase-δ, which is synthesized
during the late G1 and S phases of the cell cycle. PCNA
expression is correlated with the cell proliferative state and is
involved in DNA replication and repair (24–26).
In the present study the upregulated expression of PCNA,
accompanied with changes in the BrdU staining pattern, indicates
that the observed effect in PCNA was proliferative, rather than due
to DNA damage. Besides, the amount of energy delivered to the cells
by the electric treatment is far too low as to break chemical bonds
or cause thermal effects, thus, other alternative mechanisms would
be involved in the observed biological responses.
This dual, cytotoxic and cytoproliferative response
could be due to alterations in cell cycle progression similar to
those reported previously in HepG2 hepatocarcinoma cells exposed to
the same electric stimulus (16,17).
In fact, the present flow cytometry data reinforce this
interpretation. At 6 h of the stimulation onset, modest,
non-significant statistical increases were detected in the
proportions of NB69 cells in G0/G1 and,
mainly, in S phase. After the first 12 h of intermittent exposure,
these increases were followed by a significant decrease, of ∼20%
below controls, in the fraction of the cellular population
distributed in G2 and M phases. At the end of the 24 h
of treatment a modest increase in the proportion of cells in S
phase was detected, which was similar to that observed at 6 h.
Taken together, these results could be indicative of a slowdown or
a transient blocking of the S phase in a fraction of the cell
population, which would cause cycle elongation and, therefore, the
decline in the cell density of the culture, as observed after
treatment.
The analysis of the evolution of NB69 cultures
showed that the treatment-induced decrease in cell population
persisted two days after the end of the electric stimulation (72 h
after the exposure onset). Indeed, at that time a 7.59% decrease in
the number of living cells and a 17.18% increase in the rate of
necrosis, were observed in the exposed samples when compared to
controls. Such an effect could result from the combination of a
cytotoxic action, exerted on a particularly sensitive cellular
subpopulation, plus a transient slowing or blocking of the cell
cycle in another subpopulation of the same samples. In fact, it has
been reported that the NB69 line integrates two predominant cell
subtypes, a subpopulation with 45 chromosomes and another with 48
chromosomes, which show a marked tendency to undergo cytogenetic
changes (27). These
subpopulations could respond differently to the electric stimulus.
In this context it must be underlined that at the end of the 24 h
of intermittent stimulation with current densities j <400
μA/mm2, the cell death rates were significantly
increased with respect to controls, whereas the number of living
cells did not change significantly (Fig. 3B). This could be attributable to
the existence of a third cell subtype, recently described by Acosta
et al(28). This
subpopulation could either be insensitive to the electric
stimulation or respond to it by slightly increasing its
proliferation, which would partly compensate the decline in the
viability rate due to the treatment-induced necrosis in the
vulnerable subpopulation. However, since in general the samples
treated with j ≤400 μA/mm2 tend to show a decrease in
the total number of viable cells (Fig.
3B), it is conceivable that in our cultures the relative size
of the third subpopulation would have little relevance.
Within the context of the existing evidence on the
cellular response to subthermal, 0.57 MHz electric currents
(16,17), the analysis of the present data
indicates that at least a fraction or subpopulation of the NB69
cell line, would be more responsive to the electric stimulus than
the HepG2 cells. Such differential sensitivity could be related to
the proliferation rate, which is higher in NB69 (doubling time = 12
h in our experimental conditions) than in HepG2 (doubling time = 42
h). This hypothesis would be supported by the lack of
responsiveness of PBMC cultures, which are virtually quiescent
unless activated by exogenous mitogenic agents. Indeed, our data
show that the same electric stimulus that elicits significant
changes in the cell cycle, cell proliferation and the viability of
two human tumor lines, does not affect any of the studied processes
in PBMC. Collectively, these results are consistent with those
reported by other authors showing that dividing cells are
particularly, if not exclusively, sensitive to the effects of
electric stimuli of frequencies ranging from 100 KHz to 1 MHz
(4,19).
In conclusion, our results show that human
neuroblastoma cells NB69 are sensitive to the in vitro
exposure to short pulses of 0.57 MHz subthermal currents applied
over a period of 24 h. This response is similar in nature to that
reported in the line HepG2 when exposed to the same electric
stimulus. This reinforces the evidence that at least certain types
of tumor cells are sensitive to 0.57 MHz currents, and that the
cellular response involves mechanisms other than those triggered by
conventional thermal stimuli. In connection with electro-thermal
CRET treatments applied to cancer patients, it has been proposed
that the partial cytotoxic response observed in vitro in
NB69, or the cytostatic effect reported in HepG2, could act in
synergy with the potential oncostatic action exerted by the
hyperthermia induced in the tumor tissue by Joule's effect
(15). The fact that PBMC from
healthy donors have been revealed irresponsive to the electric
stimulus, strengthens the hypothesis that non-proliferating cells,
or cells with low proliferation rates, do not respond to the
electric treatment. This could be envisioned as an endorsement to
the current medical evidence on safety of therapies based on the
application of the tested stimulus. Thus, the available
experimental evidence on human cellular models is supportive of the
claim that CRET could be effective as a potential adjuvant in the
treatment of some cancer related processes. However, a deeper
understanding of the cellular and molecular mechanisms of response
to electrical stimuli in the intermediate frequency and
radiofrequency ranges, is crucial to the potential applications of
electro-thermal therapies like CRET in oncology.
Acknowledgements
M.L. Hernández-Bule was supported by
an INDIBA, S.A. grant for Ph.D. students. This study was performed
under assignment and supervision of the Spanish Ministry of
Health.
References
|
1
|
Ottawa Panel: Ottawa panel evidence based
clinical practice guidelines for electrotherapy and thermotherapy
interventions in the management of rheumatoid arthritis in adults.
Phys Ther. 84:1016–1043. 2004.
|
|
2
|
Ricci NA, Dias CN and Driusso P: The use
of electrothermal and phototherapeutic methods for the treatment of
fibromyalgia syndrome: a systematic review. Rev Bras Fisioter.
14:1–9. 2010.PubMed/NCBI
|
|
3
|
Sersa G, Jarm T, Kotnit T, Koer A,
Podkrajsek M, Sentjurc M, Miklavcic D, Kadivec M, Kranic S, Secerov
A and Cemazar M: Vascular disrupting action of electroporation and
electrochemotherapy with bleomycin in murine sarcoma. Br J Cancer.
98:388–398. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kirson ED, Dbaly V, Tovarys F, Vymazal J,
Soustiel JF, Itzhaki A, Mordechovich D, Steinberg-Shapira S,
Gurvich Z, Shneiderman R, et al: Alternating electric fields arrest
cell proliferation in animal tumor models and human brain tumors.
Proc Natl Acad Sci USA. 107:10152–10157. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Garon EB, Sawcer D, Vernier PT, Tang T,
Sun Y, Marcu L, Gundersen MA and Koeffler HP: In vitro and in vivo
evaluation and a case report of intense nanosecond pulsed electric
field as a local therapy for human malignancies. Int J Cancer.
121:675–682. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fiorentini G, Giovanis P, Rossi S, Dentico
P, Paola R, Turrisi G and Bernardeschi P: A phase II clinical study
on relapsed malignant gliomas treated with electro-hyperthermia. In
Vivo. 20:721–724. 2006.PubMed/NCBI
|
|
7
|
Kamisawa T, Tu Y, Egawa N, Karasawa K,
Matsuda T, Tsuruta K and Okamoto A: Thermo-chemo-radiotherapy for
advanced bile duct carcinoma. World J Gastroenterol. 11:4206–4209.
2005.PubMed/NCBI
|
|
8
|
Grimnes S and Martinsen ØG: Joule effect
and temperature rise. Bioimpedance and Bioelectricity Basics.
Academic Press: Harcourt and Technology Co.; London: pp. 71–73.
2000
|
|
9
|
Ley A, Cladellas M, Colet P, de las Heras
P, Florensa J, Prim J, Roussos J, Ariza A and Calbet J:
Transferencia eléctrica capacitiva (TEC): Técnica no invasiva de
hipertermia profunda en el tratamiento de los gliomas cerebrales.
Resultados preliminares. Neurocirugía. 3:118–123. 1992.(In
Spanish).
|
|
10
|
Ley A, Ariza A and Rosell R: Tratamiento
quirúrgico de los gliomas malignos. Hipertermia. Tumores del
Sistema Nervioso Central. Epidemiologia, Nosología y Terapéutica,
Doyma: Barcelona: pp. 55–64. 1993, (In Spanish).
|
|
11
|
Ley A: Hipertermia intracraneal no
invasiva mediante la técnica de Transferencia Eléctrica Capacitiva
(TEC). Resultados de la termometría cerebral e intratumoral.
Neurocirugía. 14:41–45. 2003.(In Spanish).
|
|
12
|
Sakamoto T, Katoh H, Shimizu T, Yamashita
I, Takemori S, Tazawa K and Fujimaki M: Clinical results of
treatment of advanced carcinoma with hyperthermia in combination
with chemoradiotherapy. Chest. 112:1487–1493. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Matsui Y, Nakagana A, Kamiyama Y, Yamamoto
K, Kubo N and Nakase Y: Selective thermocoagulation of unresectable
pancreatic cancers by using radiofrequency capacitive heating.
Pancreas. 20:14–20. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ohguri T, Imada H, Yahara K, Kakeda S,
Tomimatsu A, Kato F, Nomoto S, Terashima H and Korogi Y: Effect of
8-MHz radiofrequency-capacitive regional hyperthermia with strong
superficial cooling for unresectable or recurrent colorectal
cancer. Int J Hyperthermia. 20:465–475. 2004. View Article : Google Scholar
|
|
15
|
Hernández-Bule ML, Trillo MA, Bazán E,
Martínez-Pascual MA, Leal J and Úbeda A: Niveles atérmicos de
corrientes eléctricas usadas en terapia por transferencia eléctrica
capacitiva inducen efectos citotóxicos parciales en cultivos de
neuroblastoma humano. Neurocirugía. 15:366–371. 2004.(In
Spanish).
|
|
16
|
Hernández-Bule ML, Trillo MA, Cid MA, Leal
J and Ubeda A: In vitro exposure to 0.57 MHz electric
currents exerts cytostatic effects in HepG2 human hepatocarcinoma
cells. Int J Oncol. 30:583–592. 2007.
|
|
17
|
Hernández-Bule ML, Cid MA, Trillo MA, Leal
J and Ubeda A: Cytostatic response of HepG2 to 0.57 MHz electric
currents mediated by changes in cell cycle control proteins. Int J
Oncol. 37:1399–1405. 2010.PubMed/NCBI
|
|
18
|
Wang E, Yin Y, Zhao M, Forrester JV and
McCaig CD: Physiological electric fields control the G1/S phase
cell cycle checkpoint to inhibit endothelial cell proliferation.
FASEB J. 17:458–460. 2003.PubMed/NCBI
|
|
19
|
Kirson ED, Gurvich Z, Shneiderman R, Dekel
E, Itzhaki A, Wasserman Y, Schatzberger R and Palti Y: Disruption
of cancer cell replication by alternating electric fields. Cancer
Res. 64:3288–3295. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Boyum A: Isolation of leucocytes from
human blood. A two-phase system for removal of red cells with
methylcellulose as erythrocyte-aggregating agent. Scand J Clin Lab
Invest (Suppl). 97:9–29. 1968.PubMed/NCBI
|
|
21
|
Rodríguez-Martín E, Canals S, Casarejos
MJ, de Bernardo S, Handler A and Mena MA: L-DOPA and
glia-conditioned medium have additive effects on tyrosine
hydroxylase expression in human catecholamine-rich neuroblastoma
NB69 cells. J Neurochem. 78:535–545. 2001.PubMed/NCBI
|
|
22
|
Kato S, Asada R, Kageyama K, Saitoh Y and
Miwa N: Anticancer effects of 6-O-palmitoyl-ascorbate combined with
a capacitive-resistive electric transfer hyperthermic apparatus as
compared with ascorbate in relation to ascorbyl radical generation.
Cytotechnology. 63:425–435. 2011. View Article : Google Scholar
|
|
23
|
Aslan JE and Thomas G: Death by committee:
organellar trafficking and communication in apoptosis. Traffic.
10:1390–1404. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Woods AL, Hall PA, Shepherd NA, Hanby AM,
Waseem NH, Lane DP and Levison DA: The assessment of proliferating
cell nuclear antigen (PCNA) immunostaining in primary
gastrointestinal lymphomas and its relationship to histological
grade, S+G2+M phase fraction (flow cytometric analysis) and
prognosis. Histophatology. 19:21–27. 1991.
|
|
25
|
Connolly KM and Bogdanffy MS: Evaluation
of proliferating cell nuclear antigen (PCNA) as an endogenous
marker of cell proliferation in rat liver: a dual-stain comparison
with 5-bromo-2′-deoxyuridine. J Histochem Cytochem. 41:1–6.
1993.PubMed/NCBI
|
|
26
|
Nakano A, Norihito W, Yasuhiro N,
Takashimizu S and Matsuzaki S: Immunohistochemical studies on the
expression of P-glycoprotein and p53 in relation to histological
differentiation and cell proliferation in hepatocellular carcinoma.
Hepatol Res. 25:158–165. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Feder MK and Gilbert F: Clonal evolution
in a human neuroblastoma. J Natl Cancer Inst. 70:1051–1056.
1983.PubMed/NCBI
|
|
28
|
Acosta S, Lavarino C, Paris R, García I,
de Torres C, Rodríguez E, Beleta H and Mora J: Comprehensive
characterization of neuroblastoma cell line subtypes reveals
bilineage potential similar to neural crest stem cells. BMC Dev
Biol. 12:9–12. 2009.PubMed/NCBI
|