|
1
|
Choi YY, Noh SH and Cheong JH: Evolution
of gastric cancer treatment: From the golden age of surgery to an
era of precision medicine. Yonsei Med J. 56:1177–1185. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU,
Kim W, Ryu SW, Lee HJ and Song KY: Morbidity and mortality of
laparoscopic gastrectomy versus open gastrectomy for gastric
cancer: An interim report - a phase III multicenter, prospective,
randomized Trial (KLASS Trial). Ann Surg. 251:417–420. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lu J, Zheng CH, Zheng HL, Li P, Xie JW,
Wang JB, Lin JX, Chen QY, Cao LL, Lin M, et al: Randomized,
controlled trial comparing clinical outcomes of 3D and 2D
laparoscopic surgery for gastric cancer: An interim report. Surg
Endosc. 31:2939–2945. 2017. View Article : Google Scholar
|
|
4
|
Corcione F, Esposito C, Cuccurullo D,
Settembre A, Miranda N, Amato F, Pirozzi F and Caiazzo P:
Advantages and limits of robot-assisted laparoscopic surgery:
Preliminary experience. Surg Endosc. 19:117–119. 2005. View Article : Google Scholar
|
|
5
|
Hur H, Kim JY, Cho YK and Han SU:
Technical feasibility of robot-sewn anastomosis in robotic surgery
for gastric cancer. J Laparoendosc Adv Surg Tech A. 20:693–697.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Suda K, Man-I M, Ishida Y, Kawamura Y,
Satoh S and Uyama I: Potential advantages of robotic radical
gastrectomy for gastric adenocarcinoma in comparison with
conventional laparoscopic approach: A single institutional
retrospective comparative cohort study. Surg Endosc. 29:673–685.
2015. View Article : Google Scholar
|
|
7
|
Uyama I, Kanaya S, Ishida Y, Inaba K, Suda
K and Satoh S: Novel integrated robotic approach for
suprapancreatic D2 nodal dissection for treating gastric cancer:
Technique and initial experience. World J Surg. 36:331–337. 2012.
View Article : Google Scholar
|
|
8
|
Sørensen SM, Savran MM, Konge L and
Bjerrum F: Three-dimensional versus two-dimensional vision in
laparoscopy: A systematic review. Surg Endosc. 30:11–23. 2016.
View Article : Google Scholar
|
|
9
|
Kim YM, Son T, Kim HI, Noh SH and Hyung
WJ: Robotic D2 lymph node dissection during distal subtotal
gastrectomy for gastric cancer: Toward procedural standardization.
Ann Surg Oncol. 23:2409–2410. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Song J, Oh SJ, Kang WH, Hyung WJ, Choi SH
and Noh SH: Robot-assisted gastrectomy with lymph node dissection
for gastric cancer: Lessons learned from an initial 100 consecutive
procedures. Ann Surg. 249:927–932. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Son T, Lee JH, Kim YM, Kim HI, Noh SH and
Hyung WJ: Robotic spleen-preserving total gastrectomy for gastric
cancer: Comparison with conventional laparoscopic procedure. Surg
Endosc. 28:2606–2615. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lianos GD, Rausei S, Dionigi G and Boni L:
Assessing safety and feasibility of minimally invasive surgical
approaches for advanced gastric cancer. Future Oncol. 12:5–8. 2016.
View Article : Google Scholar
|
|
13
|
Junfeng Z, Yan S, Bo T, Yingxue H, Dongzhu
Z, Yongliang Z, Feng Q and Peiwu Y: Robotic gastrectomy versus
laparoscopic gastrectomy for gastric cancer: Comparison of surgical
performance and short-term outcomes. Surg Endosc. 28:1779–1787.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shen W, Xi H, Wei B, Cui J, Bian S, Zhang
K, Wang N, Huang X and Chen L: Robotic versus laparoscopic
gastrectomy for gastric cancer: Comparison of short-term surgical
outcomes. Surg Endosc. 30:574–580. 2016. View Article : Google Scholar
|
|
15
|
Nakauchi M, Suda K, Susumu S, Kadoya S,
Inaba K, Ishida Y and Uyama I: Comparison of the long-term outcomes
of robotic radical gastrectomy for gastric cancer and conventional
lapa-roscopic approach: A single institutional retrospective cohort
study. Surg Endosc. 30:5444–5452. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Obama K, Kim YM, Kang DR, Son T, Kim HI,
Noh SH and Hyung WJ: Long-term oncologic outcomes of robotic
gastrectomy for gastric cancer compared with laparoscopic
gastrectomy. Gastric Cancer. 21:285–295. 2018. View Article : Google Scholar
|
|
17
|
Coratti A, Fernandes E, Lombardi A, Di
Marino M, Annecchiarico M, Felicioni L and Giulianotti PC:
Robot-assisted surgery for gastric carcinoma: Five years follow-up
and beyond: A single western center experience and long-term
oncological outcomes. Eur J Surg Oncol. 41:1106–1113. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Rozner MA: The American Society of
Anesthesiologists physical status score and risk of perioperative
infection. JAMA. 275:15441996. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Borrmann R: Geschwulste des Magens und des
Duodenums. Handbuch Spez Pathol Anat und Histo. Henke F and
Lubarsch O: Springer Verlag; Berlin: pp. 812–1054. 1926
|
|
20
|
Ajani JA, D'Amico TA, Almhanna K, Bentrem
DJ, Chao J, Das P, Denlinger CS, Fanta P, Farjah F, Fuchs CS, et
al: Gastric cancer, version 3.2016, NCCN clinical practice
guidelines in oncology. J Natl Compr Canc Netw. 14:1286–1312. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dindo D, Demartines N and Clavien PA:
Classification of surgical complications: A new proposal with
evaluation in a cohort of 6336 patients and results of a survey.
Ann Surg. 240:205–213. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yang SY, Roh KH, Kim YN, Cho M, Lim SH,
Son T, Hyung WJ and Kim HI: Surgical Outcomes After Open,
Laparoscopic, and Robotic Gastrectomy for Gastric Cancer. Ann Surg
Oncol. 24:1770–1777. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
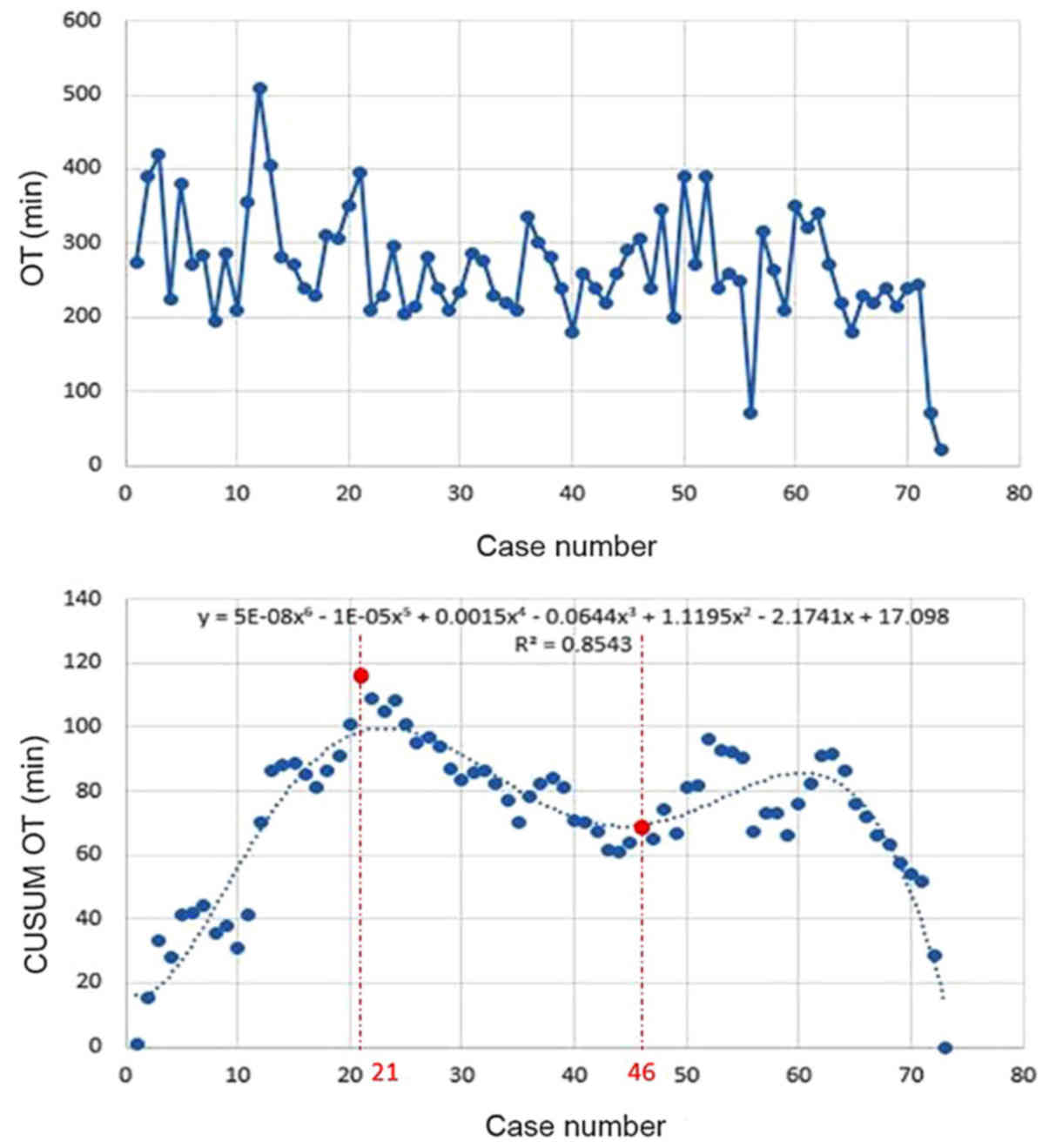
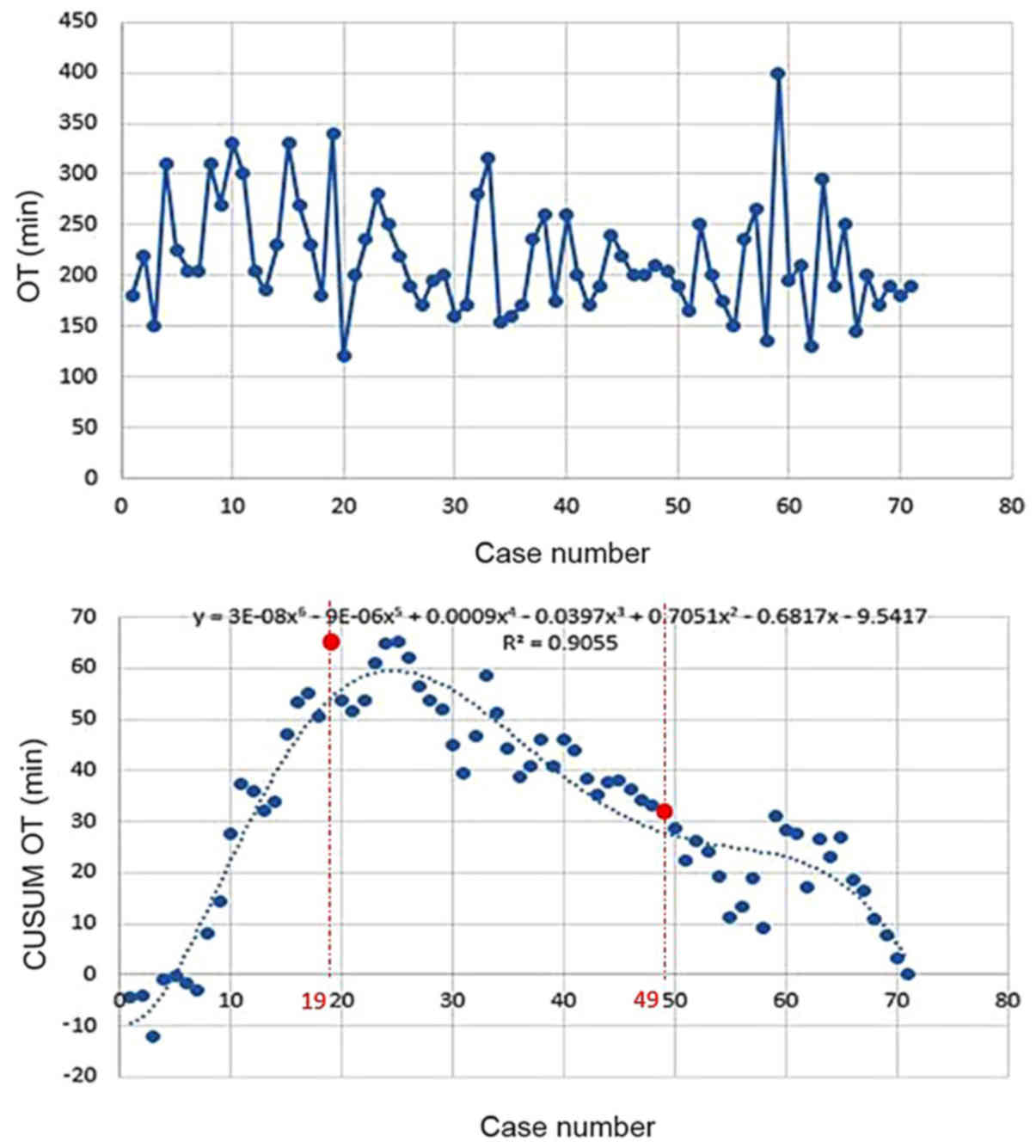
Maguire T, Mayne CJ, Terry T and Tincello
DG: Analysis of the surgical learning curve using the cumulative
sum (CUSUM) method. Neurourol Urodyn. 32:964–967. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zhou J, Shi Y, Qian F, Tang B, Hao Y, Zhao
Y and Yu P: Cumulative summation analysis of learning curve for
robot-assisted gastrectomy in gastric cancer. J Surg Oncol.
111:760–767. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Biswas P and Kalbfleisch JD: A
risk-adjusted CUSUM in continuous time based on the Cox model. Stat
Med. 27:3382–3406. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
26
|
Pendlimari R, Holubar SD, Dozois EJ,
Larson DW, Pemberton JH and Cima RR: Technical proficiency in
hand-assisted laparoscopic colon and rectal surgery: Determining
how many cases are required to achieve mastery. Arch Surg.
147:317–322. 2012. View Article : Google Scholar
|
|
27
|
Biau DJ, Resche-Rigon M, Godiris-Petit G,
Nizard RS and Porcher R: Quality control of surgical and
interventional procedures: A review of the CUSUM. Qual Saf Health
Care. 16:203–207. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Son T, Hyung WJ, Lee JH, Kim YM, Kim HI,
An JY, Cheong JH and Noh SH: Clinical implication of an
insufficient number of examined lymph nodes after curative
resection for gastric cancer. Cancer. 118:4687–4693. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hyun MH, Lee CH, Kwon YJ, Cho SI, Jang YJ,
Kim DH, Kim JH, Park SH, Mok YJ and Park SS: Robot versus
lapa-roscopic gastrectomy for cancer by an experienced surgeon:
Comparisons of surgery, complications, and surgical stress. Ann
Surg Oncol. 20:1258–1265. 2013. View Article : Google Scholar
|
|
30
|
Kim HI, Han SU, Yang HK, Kim YW, Lee HJ,
Ryu KW, Park JM, An JY, Kim MC, Park S, et al: Multicenter
Prospective Comparative Study of Robotic Versus Laparoscopic
Gastrectomy for Gastric Adenocarcinoma. Ann Surg. 263:103–109.
2016. View Article : Google Scholar
|
|
31
|
Lanfranco AR, Castellanos AE, Desai JP and
Meyers WC: Robotic surgery: A current perspective. Ann Surg.
239:14–21. 2004. View Article : Google Scholar
|
|
32
|
Kim HI, Park MS, Song KJ, Woo Y and Hyung
WJ: Rapid and safe learning of robotic gastrectomy for gastric
cancer: Multidimensional analysis in a comparison with laparoscopic
gastrectomy. Eur J Surg Oncol. 40:1346–1354. 2014. View Article : Google Scholar
|
|
33
|
Jeong O, Ryu SY, Choi WY, Piao Z and Park
YK: Risk factors and learning curve associated with postoperative
morbidity of laparoscopic total gastrectomy for gastric carcinoma.
Ann Surg Oncol. 21:2994–3001. 2014. View Article : Google Scholar : PubMed/NCBI
|