Introduction
Hyperthyroidism is the most common organ-specific
autoimmune disease and the most important reason for Graves'
ophthalmopathy. The predominant manifestations of the disease
include diffuse goiter, disappeared immune tolerance to thyroid
antigens and infiltration of thyroid tissues by lymphocytes. The
prevalence of hyperthyroidism accounts for 2% of people worldwide,
5–10 fold higher in females than in males (1). To date, the pathogenesis of
hyperthyroidism has not been fully established. It is known that it
may be correlated with fever, insufficient sleep, increased
psychological burden and other factors, although the pathogenesis
for the majority of patients in the clinical setting remains
unknown.
Regulatory T cells (Tregs) are a subtype of CD4 T
cells characterized by the expression of CD25, while expression of
the forkhead box P3 (FOXP3) molecule is a typical marker of Tregs
(2). Tregs account for
approximately 5–10% of peripheral blood (PB) CD4 T cells. Tregs
include two subtypes: Natural Tregs (nTregs; primarily refers to
Tregs formed in the embryo/newborn thymus, also described as thymus
Tregs or tTregs); and inducible Tregs (iTregs; predominantly
induced in vitro, also termed PB Tregs or pTregs) (3). Recent studies indicated that
CD4+CD25+ Tregs were significant in various
types of autoimmune disease (4,5), and
CD4+CD25+ Treg abnormalities may contribute
to the occurrence and progression of hyperthyroidism (6). Previous studies demonstrated that,
after CD4+CD25+ Tregs were removed from a
C57BL/6 mouse, the C57BL/6 mice were more prone to hyperthyroidism
(7,8). However, the exact action of
CD4+CD25+ Tregs in hyperthyroidism remains
unknown, and previous studies primarily focus on investigating the
changes in the percentage of CD4+CD25+ Tregs
in the PB of patients with hyperthyroidism. One study indicated
that the percentage of CD4+CD25+ Tregs in PB
was decreased in patients with hyperthyroidism (9), while another study demonstrated that
no significant percentage alterations were observed (10).
Therefore, in order to further identify the actions
of CD4+CD25+ Tregs in cases of
hyperthyroidism, the present study investigated the percentage of
CD4+CD25+ Tregs in the PB of patients with
hyperthyroidism and its influence on the proliferation of naïve CD4
T cells. In addition, the percentage of PB
CD4+CD25+ Tregs in patients with
hyperthyroidism following treatment and its influence on naïve CD4T
cells was investigated. Furthermore, in-depth analysis and
discussion were made on the action mechanism of
CD4+CD25+ Tregs in hyperthyroidism.
Materials and methods
Clinical data collection
A total of 60 patients diagnosed with
hyperthyroidism at The Fourth Clinical Medical College of Harbin
Medical University (Harbin, China) between August 2014 and December
2014 were recruited along with 60 healthy subjects at the same time
(age, 18–80 years old for controls and patients; with a 1:1
male:female). Peripheral blood (10 ml) was extracted from the
hyperthyroidism patients and healthy control subjects in the
morning for subsequent experiments. The diagnostic criteria or the
patients with hyperthyroidism were as previously described
(11). The inclusion criteria were
as follows: Patients diagnosed with hyperthyroidism who had not
received anti-thyroid medication and were aged 20–60 years-old.
Patients with recurrent hyperthyroidism, abnormal liver and renal
function, and those exhibiting complications, such as tumors or
heart disease were excluded. Written informed consent was obtained
from all participants included in the present study. The present
study was approved by the Medical Ethics committee of The Fourth
Affiliated Hospital of Harbin Medical University (Harbin,
China).
Separation method for PB mononuclear
cells (PBMCs)
Blood was samples were taken with sterile sodium
citrate as an anticoagulant (10 ml; BD Biosciences, Franklin Lakes,
NJ, USA) from the patients with hyperthyroidism and the healthy
control subjects and diluted using sterile phosphate-buffered
saline (PBS; ratio of 1:1). The diluted blood samples with sodium
citrate anticoagulant was added into a 15-ml centrifugation tube
containing lymphocyte separation medium (ratio, 2:1 of sodium
citrate anticoagulant diluted blood:lymphocyte separation medium),
and 800 × g solution was taken to be centrifuged for 18 min at 4°C.
PBMCs were collected from the buffy coat, which was added to a 15
ml centrifuge tube containing RPMI-1640 medium (Gibco; Thermo
Fisher Scientific, Inc., Waltham, MA, USA) and then 600 × g at 4°C
solution was centrifuged for 15 min at 4°C. Cell deposits were
resuspended in 10 ml RPMI-1640 medium and 400 × g solution was
centrifuged for 8 min at 4°C. Subsequently, 1 ml RPMI-1640 complete
medium containing 10% fetal bovine serum (FBS; Hyclone; GE
Healthcare Life Sciences, Logan, UT, USA) was used to resuspend the
cell deposits, and the cell suspension was prepared to reach a
concentration of 2×106 cells/ml for subsequent
experiments following 0.16% Trypan blue staining (for 3 min at room
temperature). The cells were counted by Olympus light microscope
(Olympus Corporation, Tokyo, Japan). The living cells were
stained.
Determination of the percentage of
CD4+CD25+ Tregs in PB
The Pecp5.5-CD3, PE-CD4, FITC-CD25 and APC-FOXP3
fluorescent antibody combination was used to determine the
percentage of CD4+CD25+ Tregs in the PB of
patients with hyperthyroidism and the healthy control subjects. All
antibodies were purchased from BD Biosciences. PBMCs were obtained
from hyperthyroidism patients and healthy control subjects via
sterile separation and washed twice using PBS containing 1% bovine
serum albumin (BSA; Hyclone; GE Healthcare Life Sciences). The
corresponding fluorescent antibodies were added Pecp5.5-CD3 (1:100;
cat. no. MCA463PECY5.5), PE-CD4 (1:100; cat. no. MA5-17451) and
FITC-CD25 (1:100, cat. no. 302604) and incubated at 4°C for 30 min
in the dark, and washed once with PBS containing 1% BSA. All of
antibodies were purchased from BD PharMingen; BD Biosciences.
Subsequently, the cell permeabilization solution (0.2 mg/ml) was
used to wash the cells once. Fixation and permeabilization buffer
(eBioscience; Thermo Fisher Scientific, Inc.; 0.5 ml) was added and
incubated at room temperature for 30 min in the dark, and
corresponding fluorescent antibodies (APC-FOXP3) were added and
incubated at room temperature for 30 min in the dark. Cell
permeabilization solution was used to wash the cells twice, and
cells were resuspended in 1% paraformaldehyde fixed solution (0.1
ml) for detection by flow cytometry. During data analysis done by
FlowJo software v10.0.6 (FlowJo LLC, Ashland, OR, USA), CD3
side-scatter was selected, and double-positive CD4 and CD25 cells
were subsequently selected in the CD3 cell door to further analyze
the expression levels of FOXP3 in the CD4 and CD25 double-positive
cells.
Sorting method for naïve CD4 T
cells
The PBMCs obtained by the above-mentioned sorting
method were separated by magnetic beads (Thermo Fisher Scientific,
Inc.) according to the manufacturer's protocol, to obtain the naïve
CD4 T cells. The specific procedure was performed as previously
described (12).
Determination on the proliferation of
naïve CD4 T cells using the carboxyfluorescein succinimidyl ester
(CFSE) method
Naïve CD4 T cells (2×106 cells/ml) were
washed once with 10 ml RPMI-1640 medium concentrate, and pre-set
CFSE dye solution (Invitrogen; Thermo Fisher Scientific, Inc.) was
added to a final concentration of 5 mmol/l, and incubated in a 5%
CO2 incubator for 10 min at 37°C in the dark.
Immediately, 5 ml pre-cooled RPMI-1640 medium containing 5% FBS was
added to the cells to terminate staining. Thereafter, 10 ml
solution was taken to be centrifuged (400 × g) at 4°C for 8 min,
and rinsed with 10 ml RPMI-1640 medium. After 2×106
cells/ml naïve CD4 T cells were resuspended using RPMI-1640
complete medium (RPMI-1640 medium containing 10% FBS), the
suspension was added to a 48-well plate coated with 1 g/ml CD3
antibody (cat. no. FR866; DAKO; Agilent Technologies, Inc., Santa
Clara, CA, USA) and 2 g/ml CD 28 antibody (cat. no. R716401-8;
DAKO; Agilent Technologies, Inc.; placed in 5% CO2
incubator at 37°C for 2 h), and incubated at 37°C for 5 days.
Subsequently, cells were collected for detection by flow cytometry.
Data were collected on a FACScan flow cytometer (BD Biosciences)
and analyzed using FlowJo software version 10.6.0 from FlowJo LLC
(Ashland, OR, USA). When inhibition of the proliferation of naïve
CD4 T cells of CD4+CD25+ Tregs was detected,
two types of cells were added to a 48-well plate coated with 1 g/ml
CD3 antibody and 2 g/ml CD 28 antibody (ratio, 1:1), and incubated
in a 5% CO2 incubator for 5 days at 37°C. The cells were
then collected for detection by flow cytometry.
Detection method for intracellular
interferon (IFN)-γ
PBMCs obtained from sterile sorting were placed into
a 48-well plate coated with 1 g/ml CD3 antibody and 2 g/ml CD 28
antibody, and incubated in a 5% CO2 incubator for 72 h
at 37°C. The PBMCs were placed in a 24-well plate, and exposed to
100 ng/ml propylene glycol monomethyl ether acetate (Sigma-Aldrich;
Merck KGaA, Darmstadt, Germany) and 1 µg/ml ionomycin for 1 h.
Golgi blockers were added for continuous incubation for 5 h at
37°C. Cells were collected and the surface molecule, CD4 of the
dead and swollen cells was stained with trypan blue at the room
temperature for 5 min, and 0.5 ml cell membrane
fixation/permeabilization buffer was added to resuspend the cells,
which were then maintained at room temperature for 30 min in the
dark. Permeabilization solution was used to rinse the cells twice,
then fluorescent antibody, IFN-γ (cat. no. ab119140; Abcam,
Cambridge, MA, USA) was added and the cells were placed at room
temperature for 30 min in the dark. Permeabilization solution was
used to rinse the cells twice, and cells were resuspended in 1%
paraformaldehyde fixed solution (0.2 ml) for detection by flow
cytometry. When inhibition of the cytokine secretion capacity of
CD4 T cells of CD4+CD25+ Tregs was detected,
two types of cells were added to a 48-well plate coated with 1 g/ml
CD3 antibody and 2 g/ml CD 28 antibody (ratio, 1:1), and incubated
in a 5% CO2 incubator for 72 h at 37°C.
Drug therapeutic strategies for
patients with hyperthyroidism
Methimazole (Merck KGaA) combined with levothyrocine
(Merck KGaA) was administered to patients with hyperthyroidism for
a treatment course of one year. Blood samples and computed
tomography scans were use to examine the three types of free
thyroid function (T3, T4 and TSH levels), thyroid antibodies (TSH
receptor antibodies, thyroid peroxidase antibody and thyroglobulin
autoantibodies) and thyroid volume, respectively to determine the
remission of the patients' conditions.
Statistical analysis
GraphPad Prism software (version 5; GraphPad
Software, Inc., La Jolla, CA, USA) was used for data analysis. Data
comparison between the two groups was performed using a paired
Student's t test. For comparisons between multiple groups, a
one-way analysis of variance test was performed and then a
Student-Newman-Keuls post-hoc test was performed. P<0.05 was
considered to indicate a statistically significant difference.
Results
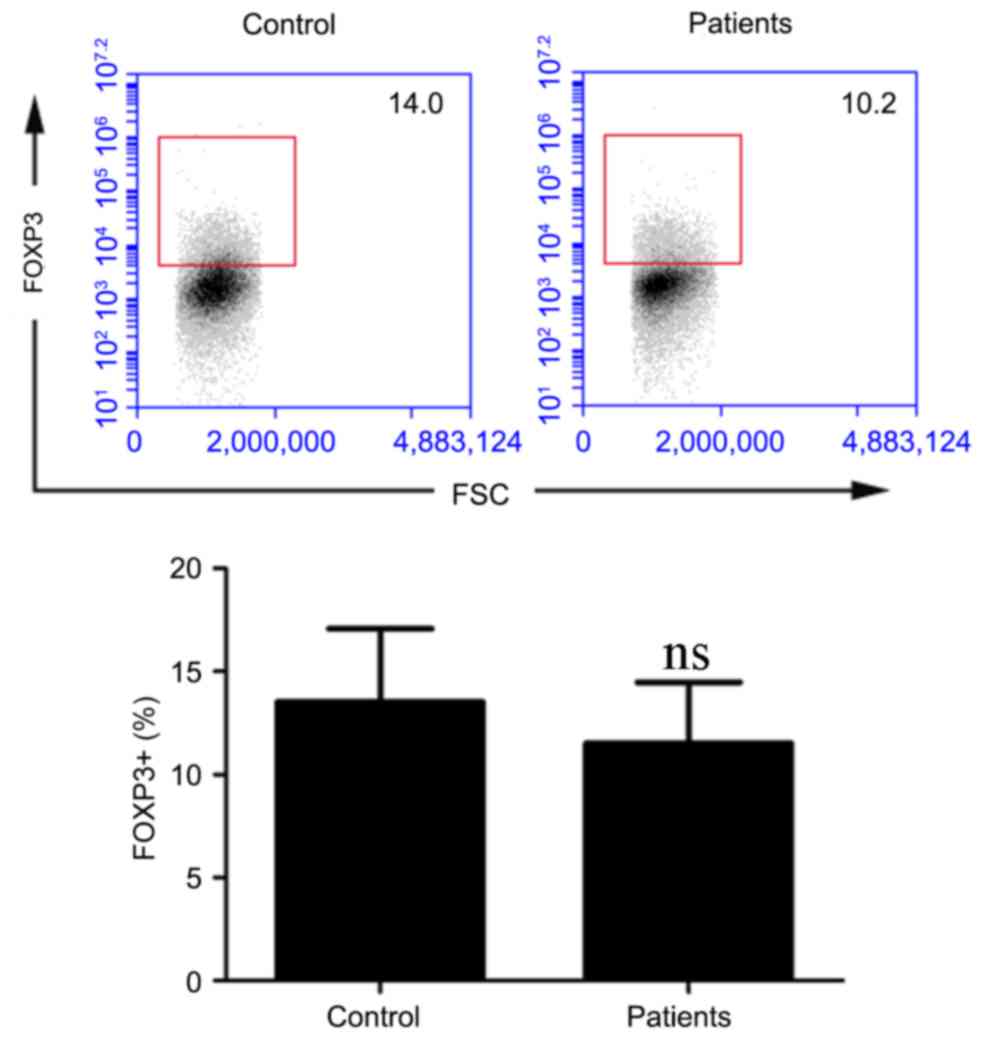
Determination on the percentage of
CD4+CD25+ Tregs in PB
As exhibited in Fig.
1, the percentage of CD4+CD25+ Tregs in
PB was 13.52±3.56% for healthy subjects, and the proportion of
CD4+CD25+ Tregs in PB was 11.53±2.94% for
patients with hyperthyroidism; the difference was not statistically
significant (P>0.05).
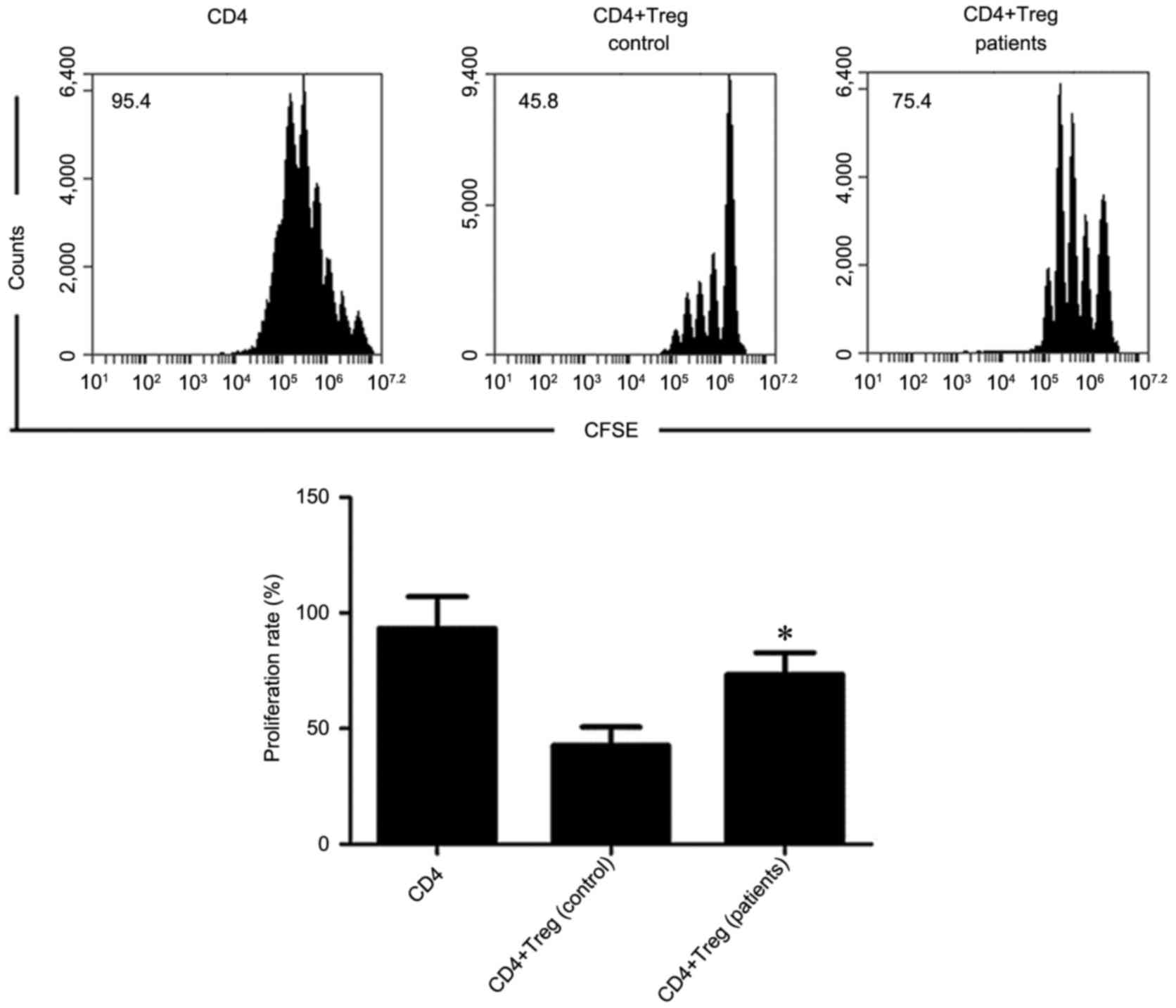
Influence of
CD4+CD25+ Tregs on the proliferation of naïve
CD4 T cells
As exhibited in Fig.
2, the proliferation capacity of naïve CD4 T cells
independently cultured was 93.25±13.83%. Following incubation of
CD4+CD25+ Tregs and naïve CD4 T cells from PB
of healthy control subjects; the proliferation capacity of naïve
CD4 T cells was 42.63±8.03%. Following incubation of
CD4+CD25+ Tregs and naïve CD4 T cells from PB
of patients with hyperthyroidism, the proliferation capacity of the
naïve CD4 T cells was 73.42±9.46%. The results indicated that
CD4+CD25+ Tregs from the PB of healthy
control subjects and patients with hyperthyroidism could
significantly inhibit the proliferation capacity of naïve CD4 T
cells. However, compared with the inhibitory capacity of
CD4+CD25+ Tregs in the PB of healthy control
subjects, CD4+CD25+ Tregs of patients with
hyperthyroidism exhibited a decreased inhibitory effect on the
proliferation of naïve CD4 T cells (P<0.05).
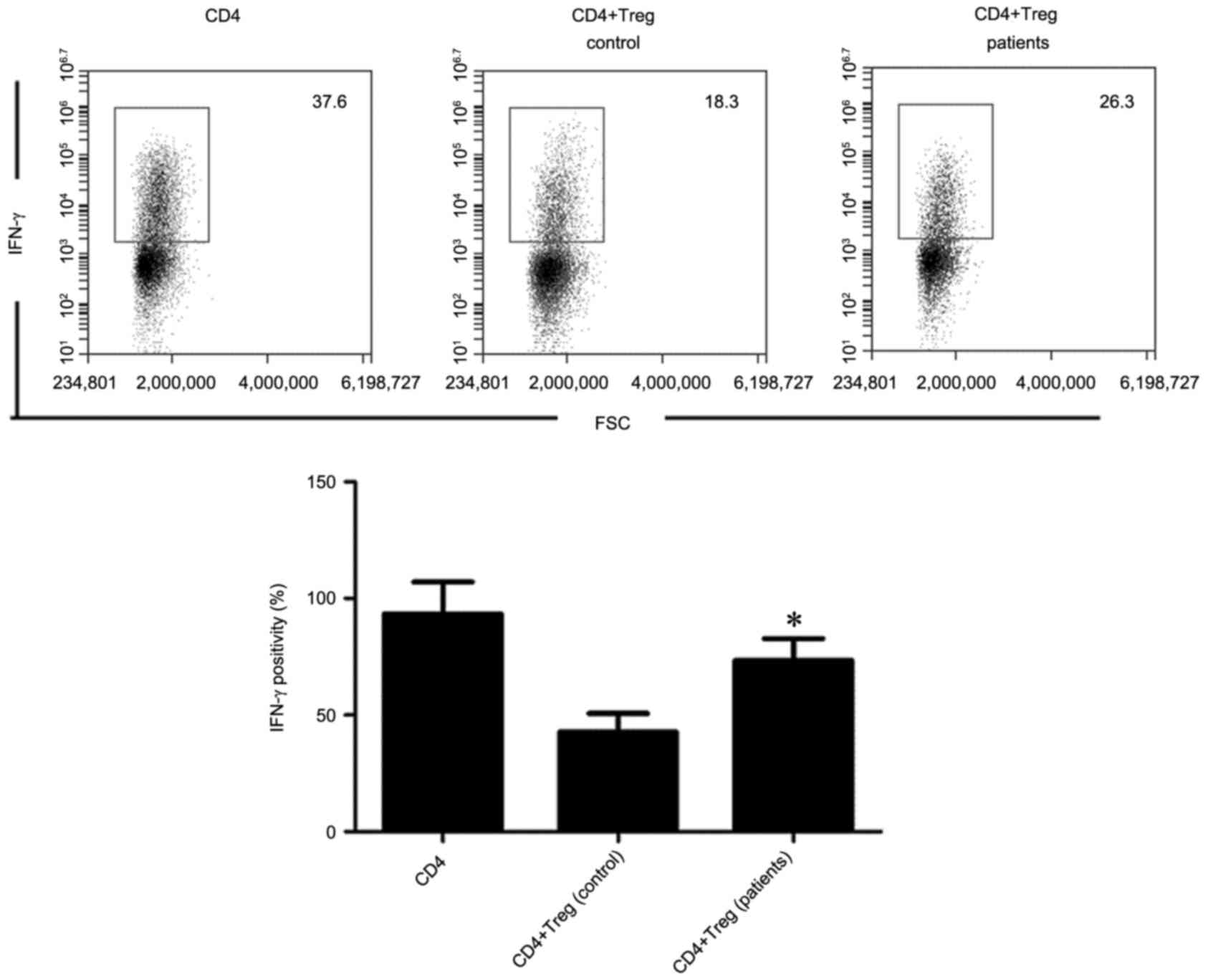
Inhibition of the secretion of
cytokines of CD4 T cells by CD4+CD25+
Tregs
As shown in Fig. 3,
after IFN-γ+ CD4 T cells in PB were co-incubated with
CD4+CD25+ Tregs for healthy control subjects,
the percentage of IFN-γ+ CD4 T cells in PB was decreased
to 17.26±5.83% from 39.46±8.93%, compared with that of patients
with hyperthyroidism, which decreased to 26.47±6.25% from
39.46±8.93%. The results indicated that
CD4+CD25+ Tregs in the PB of healthy control
subjects and patients with hyperthyroidism significantly inhibited
the cytokine secretion capacity of CD4 T cells. However, compared
with the cytokine secretion capacity of
CD4+CD25+ Tregs of CD4 T cells in the PB of
healthy control subjects, the CD4+CD25+ Tregs
of patients with hyperthyroidism exhibited a decreased inhibitory
effect on the cytokine secretion of CD4 T cells (P<0.05).
Evaluation of the curative effect of
medication
After patients with hyperthyroidism were
administered with methimazole combined with levothyrocine for 12
months, their conditions were significantly improved (Table I; P<0.05).
 | Table I.Evaluation of the curative effect of
medication on free thyroid function, thyroid antibody and thyroid
volume. |
Table I.
Evaluation of the curative effect of
medication on free thyroid function, thyroid antibody and thyroid
volume.
| Index | Prior to
treatment | Following
treatment | P-value |
|---|
| TSH (mIU/l) |
1.75±0.83 |
1.05±1.34 | >0.05 |
| FT3 (pmol/l) |
22.45±9.63 |
8.45±1.41 | <0.05 |
| FT4 (pmol/l) |
53.74±21.85 |
22.62±8.35 | <0.05 |
| TSH receptor
antibodies (mIU/l) |
33.67±24.63 |
8.46±4.25 | <0.05 |
| Thyroid peroxidase
antibody (IU/ml) |
256.36±84.72 |
184.25±49.05 | <0.05 |
| Thyroglobulin
autoantibodies (IU/ml) |
535.33±203.24 |
438.94±135.36 | <0.05 |
| Thyroid volume
(ml) |
34.24±7.63 |
21.45±4.93 | <0.05 |
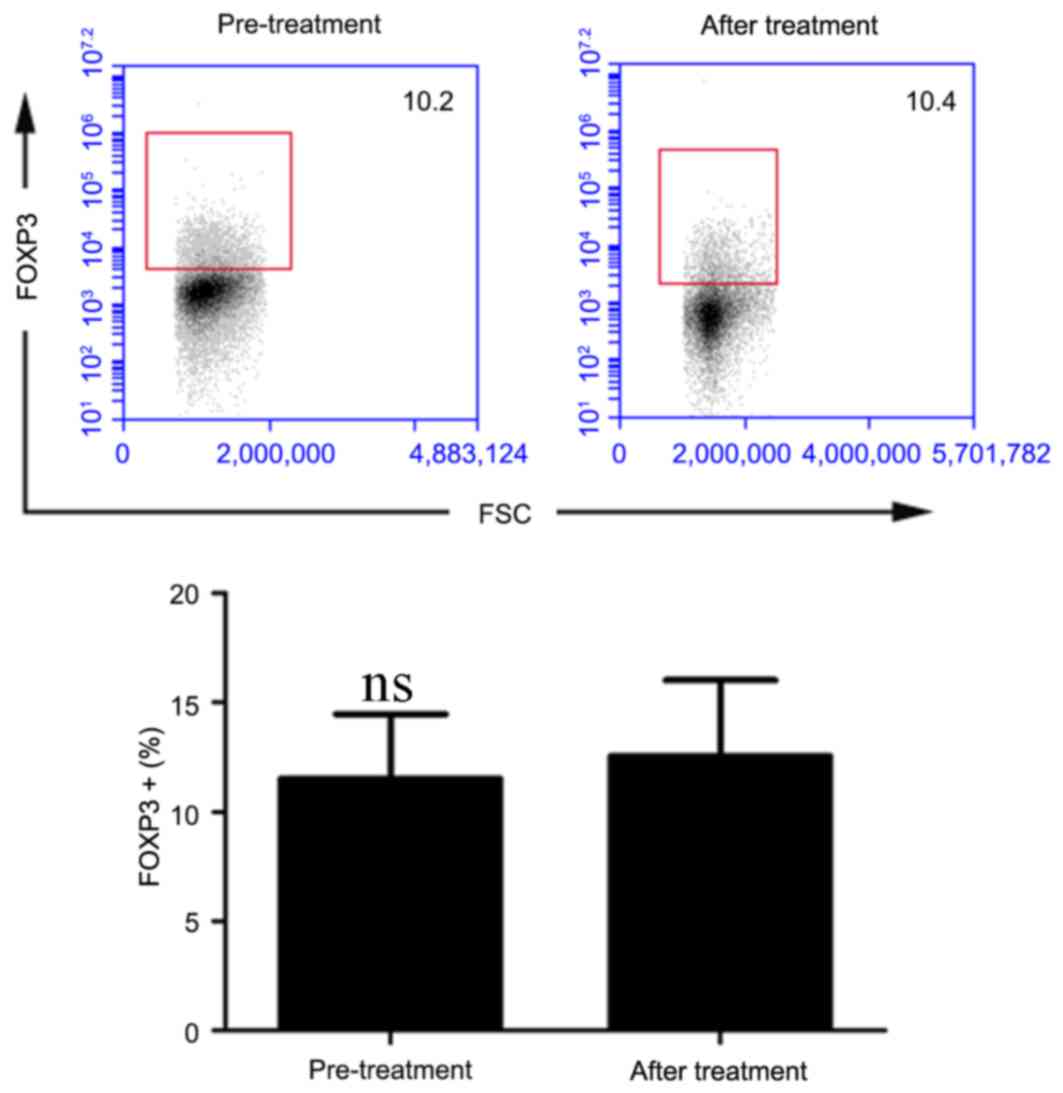
Determination of the percentage of
CD4+CD25+ Tregs in the PB of hyperthyroidism
patients that underwent treatment
As shown in Fig. 4,
the percentage of CD4+CD25+ Tregs in the PB
of patients with hyperthyroidism prior to treatment was
11.53±2.94%, compared with 12.56±3.46% following treatment. The
difference was not statistically significant (P>0.05).
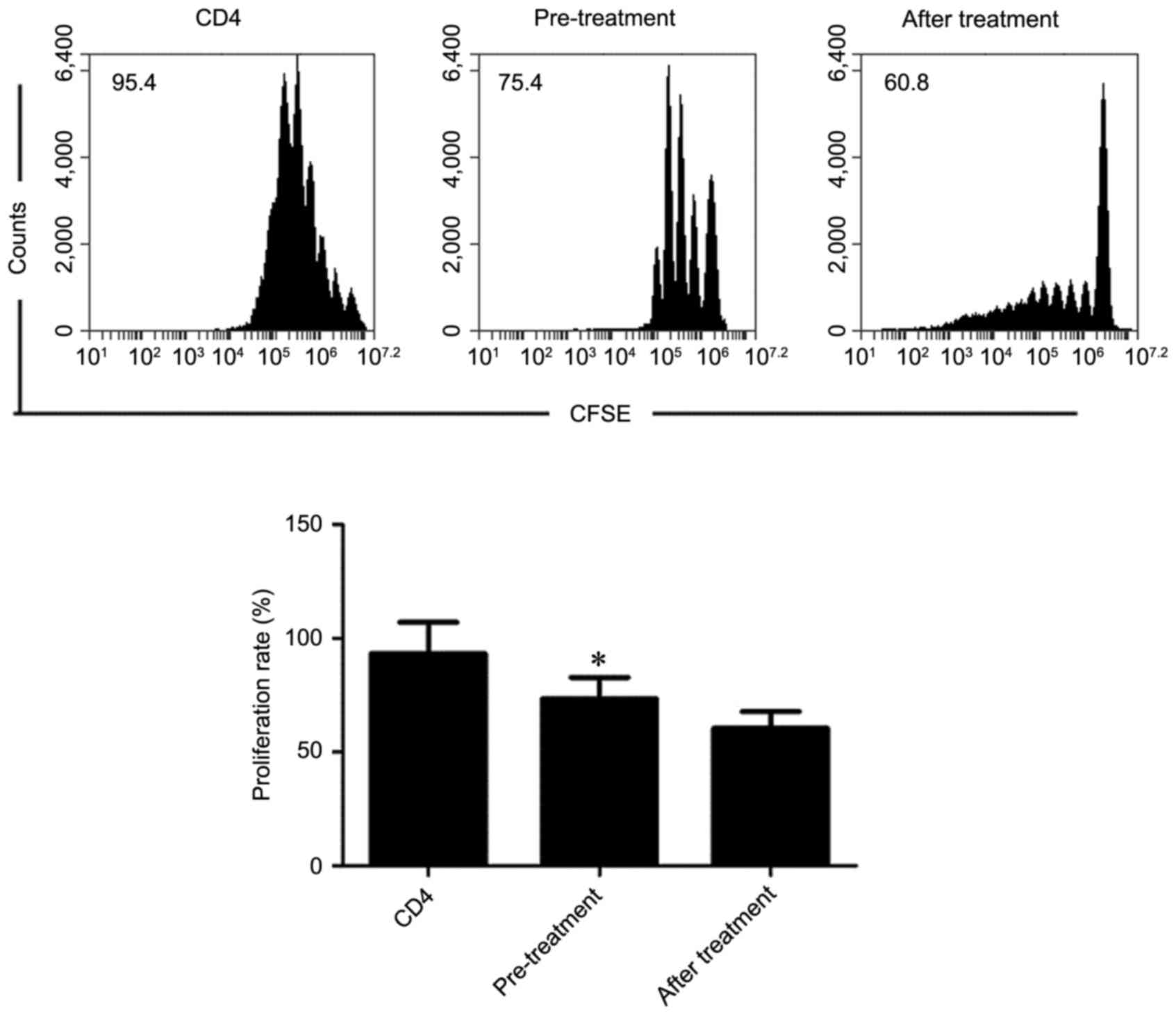
Influence of
CD4+CD25+ Tregs in the PB of treated
hyperthyroidism patients on the proliferation of naïve CD4 T
cells
As exhibited in Fig.
5, following PB CD4+CD25+ Tregs were
co-incubated with naïve CD4 T cells from patients with
hyperthyroidism before treatment, the proliferation capacity of
naïve CD4 T cells was 73.42±9.46%, compared with 60.45±7.42%
following treatment. The results indicated that
CD4+CD25+ Tregs in PB of healthy control
subjects and patients with hyperthyroidism significantly inhibited
the proliferation capacity of naïve CD4 T cells. However, compared
with the inhibitory capacity of CD4+CD25+
Tregs in the PB of healthy control subjects,
CD4+CD25+ Tregs of patients with
hyperthyroidism exhibited increased inhibition on the proliferation
of naïve CD4 T cells (P<0.05).
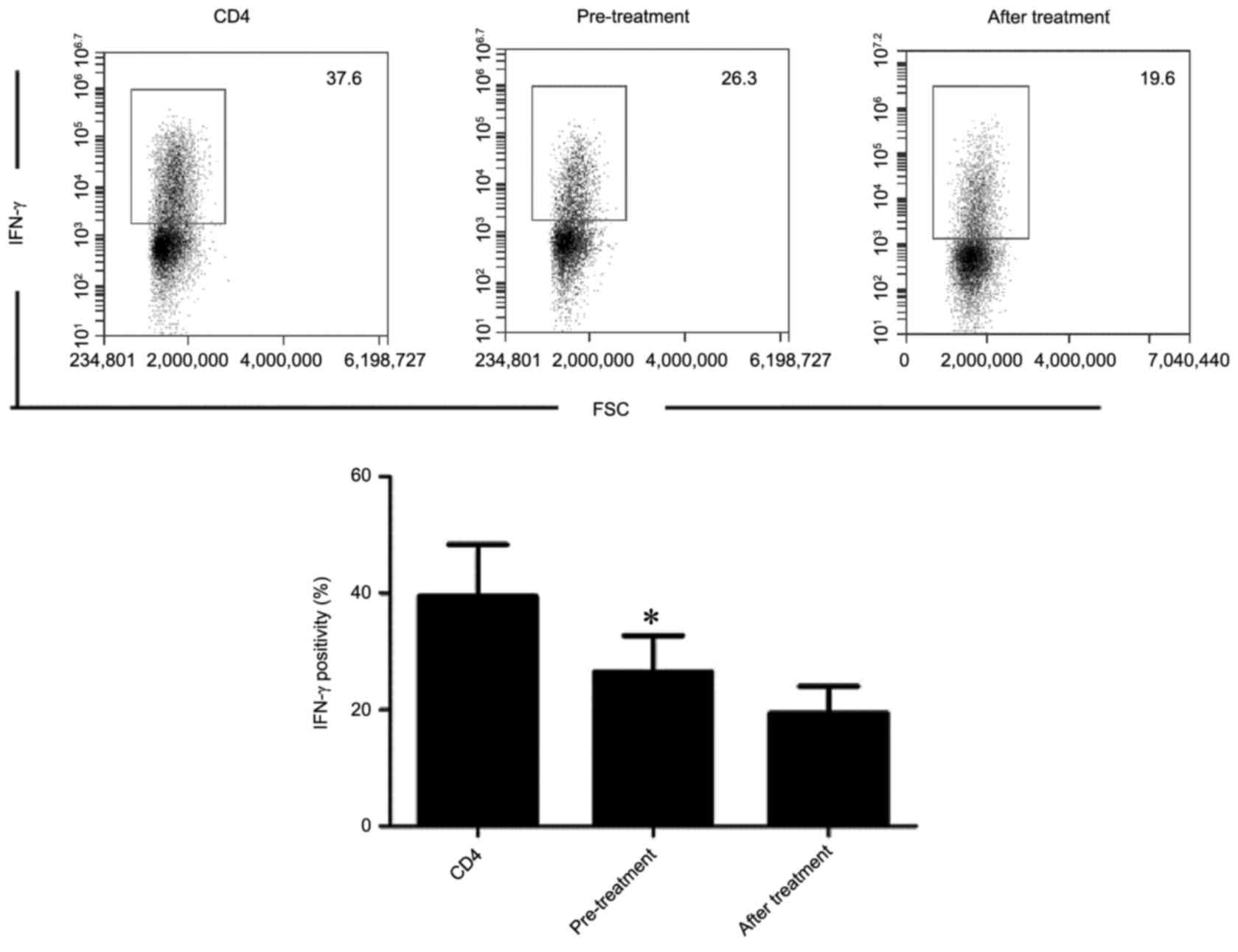
Inhibition of the secretion of
cytokines of CD4 T cells by PB CD4+CD25+
Tregs of patients with hyperthyroidism following treatment
As exhibited in Fig.
6, for healthy control subjects, the percentage of PB
IFN-γ+ CD4 T cells was 39.46±8.93%. For patients with
hyperthyroidism, the percentage of PB IFN-γ+ CD4 T cells
was 26.47±6.25% before treatment. After PB IFN-γ+ CD4 T
cells were co-incubated with CD4+CD25+ Tregs,
the percentage of PB IFN-γ+ CD4 T cells was 19.43±4.61%.
The results indicated that CD4+CD25+ Tregs in
the PB of patients with hyperthyroidism before and after treatment
significantly inhibited the secretion of CD4 T cell cytokines.
Compared with the inhibition of cytokine secretion of CD4 T cells
by CD4+CD25+ Tregs in the PB of patients with
hyperthyroidism prior to treatment, CD4+CD25+
Tregs in the PB of patients with hyperthyroidism exhibited
increased inhibition of CD4 T cell cytokine secretion following
treatment (P<0.05).
Discussion
Hyperthyroidism is the most common organ-specific
autoimmune disease and the most important reason for Graves'
ophthalmopathy (13–15). Although the pathogenesis of
hyperthyroidism has not been completely elucidated, recent studies
indicated that the change of immunologic function may be closely
correlated with the occurrence of hyperthyroidism (16,17).
The maintenance of immune function is closely associated with
immunosuppressive cells existing in the body. Major cells with
immunosuppressive functions in the body include CD4 Treg,
regulatory B cells, regulatory DC cells and V1 T cells (18–20).
The present study investigated the percentage of
CD4+CD25+ Tregs in the PB of patients with
hyperthyroidism and changes of CD4+CD25+ Treg
function. The results demonstrated that compared with the
percentage of PB CD4+CD25+ Tregs in healthy
control subjects, no significant percentage changes were observed
for PB CD4+CD25+ Tregs in patients with
hyperthyroidism (P>0.05). Such results were consistent with
results of a previous study (10).
However, compared with the percentage of
CD4+CD25+ Tregs in the PB of healthy control
subjects, there are certain studies that report a decreased
percentage of PB CD4+CD25+ Tregs in patients
with hyperthyroidism (10). It is
proposed that the differing study results are caused by various
detection methods and staining technologies. The current study
further detected CD4+CD25+ Treg cell
functions in the PB of patients with hyperthyroidism, and the
result indicated that the immunosuppressive functions of PB
CD4+CD25+ Tregs were decreased in the
patients with hyperthyroidism. PB CD4+CD25+
Tregs inhibited the proliferation of naïve CD4 T cells and
significantly decreased the secretion of CD4 T cell cytokines in
patients with hyperthyroidism (P<0.05). This result indicated
that the PB CD4+CD25+ Treg immunosuppression
function was decreased in patients with hyperthyroidism and the
non-proportional decrease may be closely associated with the
occurrence and progression of hyperthyroidism. Although it remains
unknown as to whether there is a decrease in the immunosuppressive
functions of PB CD4+CD25+ Tregs in patients
with hyperthyroidism, previous studies demonstrated that C57BL/6
mice were more prone to hyperthyroidism after
CD4+CD25+ Tregs were removed from the C57BL/6
mice (7,8). This further indicates that
CD4+CD25+ Tregs are important in the
occurrence and progression of hyperthyroidism.
Although factors causing a decrease in
immunosuppressive functions of PB CD4+CD25+
Tregs remain unknown in patients with hyperthyroidism, the results
of the present study and associated studies indicate that the
decrease in the immunosuppressive functions of PB
CD4+CD25+ Tregs may be closely correlated
with the occurrence and progression of hyperthyroidism. Therefore,
improving the immunosuppressive functions of PB
CD4+CD25+ Tregs via surgery may be an
effective therapeutic strategy to treat hyperthyroidism. Hu et
al (6) reported that
dexamethasone exerted positive effects in hyperthyroidism (6) and may improve the immunosuppressive
function of CD4+CD25+ Tregs (21). In addition, Klatka et al
(3) reported that methimazole may
be administered to pediatric patients with hyperthyroidism and acts
by regulating the function of Tregs. In the present study,
methimazole combined with levothyrocine was administered to
patients with hyperthyroidism over the course of one year. It was
found that conditions of patients with hyperthyroidism were
significantly improved (P<0.05) subsequent to this drug therapy.
Compared with the percentage of PB CD4+CD25+
Tregs in the patients with hyperthyroidism before treatment, no
significant changes were observed in the percentage of PB
CD4+CD25+ Tregs cells following treatment
(P>0.05). For patients with hyperthyroidism subsequent to
treatment, CD4+CD25+ Tregs exhibited
significantly reduced inhibition of naïve CD4T cell proliferation
and increased secretion capacity of CD4 T cell cytokines, compared
with those of the patients with hyperthyroidism before treatment
(P<0.05). Such results further demonstrate that improving the
immunosuppressive function of PB CD4+CD25+
Tregs is an effective method for treating patients with
hyperthyroidism.
There are several limitations in the present study.
First, the sample size was limited and the results need to be
confirmed. Second, the present study was only conducted using
patient samples; further work with animal model is likely to be the
most effective approach for understanding the mechanisms.
In conclusion, the current study indicates that
CD4+CD25+ Treg function was decreased in
patients with hyperthyroidism, and the non-proportional decrease
may be closely associated with the occurrence and progression of
hyperthyroidism.
References
|
1
|
Vanderpump MPJ: The epidemiology of
thyroid disease. Br Med Bull. 99:39–51. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mao C, Wang S, Xiao Y, Xu J, Jiang Q, Jin
M, Jiang X, Guo H, Ning G and Zhang Y: Impairment of regulatory
capacity of CD4+CD25+ regulatory T cells mediated by dendritic cell
polarization and hyperthyroidism in Graves' disease. J Immunol.
186:4734–4743. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Klatka M, Kaszubowska L, Grywalska E,
Wasiak M, Szewczyk L, Foerster J, Cyman M and Rolinski J: Treatment
of Graves' disease with methimazole in children alters the
proliferation of Treg cells and CD3+ T lymphocytes. Folia Histochem
Cytobiol. 52:69–77. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hamari S, Kirveskoski T, Glumoff V,
Kulmala P, Simell O, Knip M and Veijola R: Analyses of regulatory
CD4+ CD25+ FOXP3+ T cells and observations from peripheral T cell
subpopulation markers during the development of type 1 diabetes in
children. Scand J Immunol. 83:279–287. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Legorreta-Haquet MV, Chávez-Rueda K,
Chávez-Sánchez L, Cervera-Castillo H, Zenteno-Galindo E,
Barile-Fabris L, Burgos-Vargas R, Álvarez-Hernández E and
Blanco-Favela F: Function of treg cells decreased in patients with
systemic lupus erythematosus due to the effect of prolactin.
Medicine (Baltimore). 95:e23842016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hu Y, Tian W, Zhang LL, Liu H, Yin GP, He
BS and Mao XM: Function of regulatory T-cells improved by
dexamethasone in Graves' disease. Eur J Endocrinol. 166:641–646.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Saitoh O and Nagayama Y: Regulation of
Graves' hyperthyroidism with naturally occurring CD4+CD25+
regulatory T cells in a mouse model. Endocrinology. 147:2417–2422.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nagayama Y, Horie I, Saitoh O, Nakahara M
and Abiru N: CD4+CD25+ naturally occurring regulatory T cells and
not lymphopenia play a role in the pathogenesis of iodide-induced
autoimmune thyroiditis in NOD-H2h4 mice. J Autoimmun. 29:195–202.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mao C, Wang S, Xiao Y, Xu J, Jiang Q, Jin
M, Jiang X, Guo H, Ning G and Zhang Y: Impairment of regulatory
capacity of CD4+ CD25+ regulatory T cells mediated by dendritic
cell polarization and hyperthyroidism in Graves' disease. J
Immunol. 186:4734–4743. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
He K, Hu Y and Mao X: Abnormal proportions
of immune regulatory cells and their subsets in peripheral blood of
patients with Graves' disease. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi.
30:1190–1193. 2014.(In Chinese). PubMed/NCBI
|
|
11
|
Lantz M, Calissendorff J, Träisk F,
Tallstedt L, Planck T, Törring O, Hallengren B and Åsman P:
Adjuvant treatment of graves' disease with diclofenac: Safety,
effects on ophthalmopathy and antibody concentrations. Eur Thyroid
J. 5:50–56. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chen JF, Gao J, Zhang D, Wang ZH and Zhu
JY: CD4+Foxp3+ regulatory T cells converted by rapamycin from
peripheral CD4+CD25(−) naive T cells display more potent regulatory
ability in vitro. Chin Med J (Engl). 123:942–948. 2010.PubMed/NCBI
|
|
13
|
Singhal N, Praveen VP, Bhavani N, Menon
AS, Menon U, Abraham N, Kumar H, JayKunmar RV, Nair V, Sundaram S
and Sundaram P: Technetium uptake predicts remission and relapse in
Grave's disease patients on antithyroid drugs for at least 1 year
in South Indian subjects. Indian J Endocrinol Metab. 20:157–161.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Allencherril J and Birnbaum I: Heart
failure in thyrotoxic cardiomopathy: Extracorporeal membrane
oxygenation treatment for graves' disease. J Extra Corpor Technol.
47:231–232. 2015.PubMed/NCBI
|
|
15
|
Kaaroud H, Oueslati I, Harzallah A, Ben
Nacef I, Khiari K and Ben Hamida F: Benzylthiouracil induced ANCA
associated glomerulonephritis in patients with graves' disease.
Tunis Med. 93:696–701. 2015.PubMed/NCBI
|
|
16
|
Sasazuki T, Inoko H, Morishima S and
Morishima Y: Gene map of the HLA region, graves' disease and
hshimoto thyroiditis, and hematopoietic stem cell transplantation.
Adv Immunol. 129:175–249. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Côté-Bigras S, Tran V, Turcotte S,
Rola-Pleszczynski M, Verrerult J and Rottembourg D: Impaired immune
regulation after radioiodine therapy for Graves' disease and the
protective effect of Methimazole. Endocrine. 52:587–596. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wei Y, Zheng D, Li X, Zhou W, Qian Y, Ming
C and Shi B: Infusion of dendritic cells carrying donor lymphocytes
treated with 8-methoxypsoralen and ultraviolet A light induces
CD19+IL-10+ regulatory B cells and promotes skin allograft
survival. Transplant Proc. 46:pp. 3641–3646. 2014; View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li Q, Guo Z, Xu X, Xia X and Cao X:
Pulmonary stromal cells induce the generation of regulatory DC
attenuating T-cell-mediated lung inflammation. Eur J Immunol.
38:2751–2761. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Peng G, Wang HY, Peng W, Kiniwa Y, Seo KH
and Wang RF: Tumor-infiltrating gammadelta T cells suppress T and
dendritic cell function via mechanisms controlled by a unique
toll-like receptor signaling pathway. Immunity. 27:334–348. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mao XM, Li HQ, Li Q, Li DM, Xie XJ, Yin
GP, Zhang P, Xu XH, Wu JD, Chen SW and Wang SK: Prevention of
relapse of Graves' disease by treatment with an intrathyroid
injection of dexamethasone. J Clin Endocrinol Metab. 94:4984–4991.
2009. View Article : Google Scholar : PubMed/NCBI
|