|
1
|
Moore KL and Dalley AF: Clinically
oriented anatomy. Lipp Williams Wilkins. 2013.
|
|
2
|
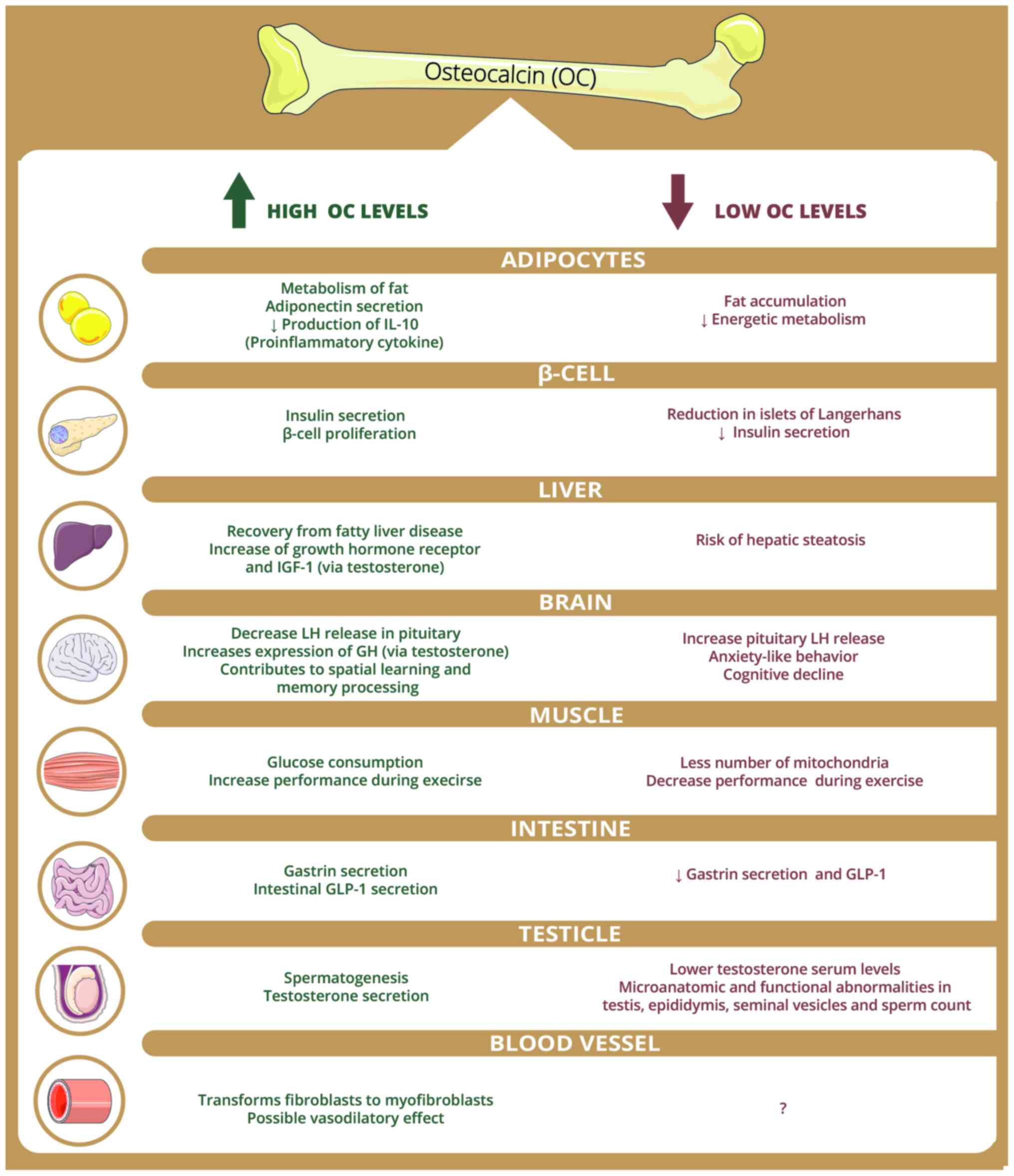
Ferron M, Hinoi E, Karsenty G and Ducy P:
Osteocalcin differentially regulates beta cell and adipocyte gene
expression and affects the development of metabolic diseases in
wild-type mice. Proc Natl Acad Sci USA. 105:5266–5270. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Villafán-Bernal JR, Sánchez-Enríquez S and
Muñoz-Valle JF: Molecular modulation of osteocalcin and its
relevance in diabetes (Review). Int J Mol Med. 28:283–293.
2011.PubMed/NCBI
|
|
4
|
Hauschka PV, Lian JB, Cole DE and Gundberg
CM: Osteocalcin and matrix Gla protein: Vitamin K-dependent
proteins in bone. Physiol Rev. 69:990–1047. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hernández-Gil IFT, Gracia MAA, Pingarrón
MDC and Jerez LB: Bases fisiológicas de la regeneración ósea I.
Histología y fisiología del tejido óseo. Med Oral Patol Oral Cir
Bucal. 11:47–51. 2006.
|
|
6
|
Lee NK, Sowa H, Hinoi E, Ferron M, Ahn JD,
Confavreux C, Dacquin R, Mee PJ, McKee MD, Jung DY, et al:
Endocrine regulation of energy metabolism by the skeleton. Cell.
130:456–469. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
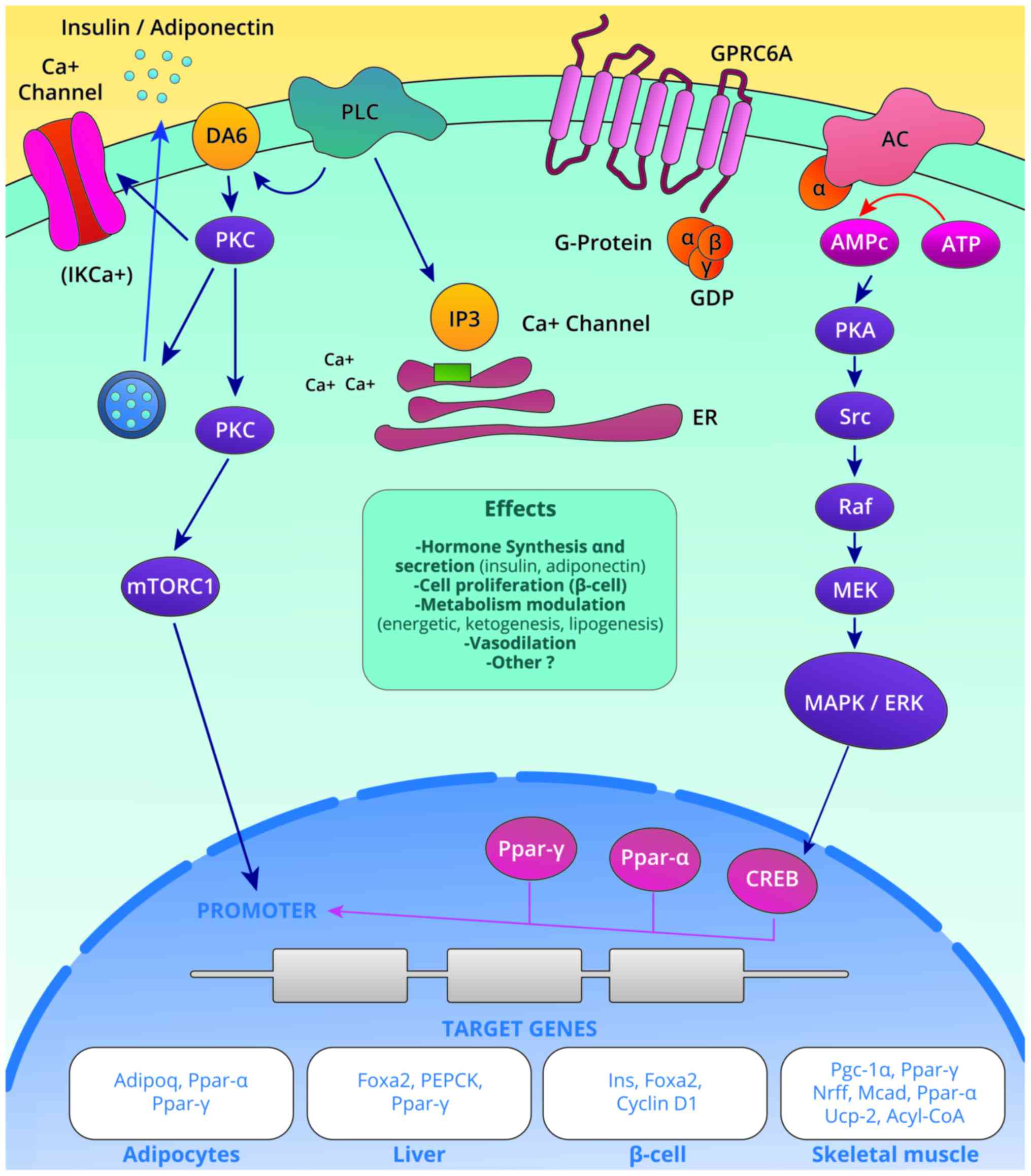
Pi M, Wu Y and Quarles LD: GPRC6A mediates
responses to osteocalcin in β-cells in vitro and pancreas in vivo.
J Bone Miner Res. 26:1680–1683. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
De Toni L, De Filippis V, Tescari S,
Ferigo M, Ferlin A, Scattolini V, Avogaro A, Vettor R and Foresta
C: Uncarboxylated osteocalcin stimulates 25-hydroxy vitamin D
production in Leydig cell line through a GPRC6a-dependent pathway.
Endocrinology. 155:4266–4274. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Clemmensen C, Smajilovic S, Wellendorph P
and Bräuner-Osborne H: The GPCR class C, group 6, subtype A
(GPRC6A) receptor: Fom cloning to physiological function. Br J
Pharmacol. 171:1129–1141. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jørgensen S, Have CT, Underwood CR,
Johansen LD, Wellendorph P, Gjesing AP, Jørgensen CV, Quan S, Rui
G, Inoue A, et al: Genetic variations in the human G
protein-coupled receptor class C, group 6, member A (GPRC6A)
control cell surface expression and function. J Biol Chem.
292:1524–1534. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Arnold KA, Eichelbaum M and Burk O:
Alternative splicing affects the function and tissue-specific
expression of the human constitutive androstane receptor. Nucl
Recept. 2:12004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wellendorph P and Bräuner-Osborne H:
Molecular cloning, expression, and sequence analysis of GPRC6A, a
novel family C G-protein-coupled receptor. Gene. 335:37–46. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ozaki KI, Awazu M, Tamiya M, Iwasaki Y,
Harada A, Kugisaki S, Tanimura S and Kohno M: Targeting the ERK
signaling pathway as a potential treatment for insulin resistance
and type 2 diabetes. Am J Physiol Endocrinol Metab. 310:E643–E651.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mera P, Laue K, Wei J, Berger JM and
Karsenty G: Osteocalcin is necessary and sufficient to maintain
muscle mass in older mice. Mol Metab. 5:1042–1047. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Du J, Zhang M, Lu J, Zhang X, Xiong Q, Xu
Y, Bao Y and Jia W: Osteocalcin improves nonalcoholic fatty liver
disease in mice through activation of Nrf2 and inhibition of JNK.
Endocrine. 53:701–709. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pi M, Kapoor K, Ye R, Nishimoto SK, Smith
JC, Baudry J and Quarles LD: Evidence for osteocalcin binding and
activation of GPRC6A in β-cells. Endocrinology. 157:1866–1880.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wei J, Hanna T, Suda N, Karsenty G and
Ducy P: Osteocalcin promotes β-cell proliferation during
development and adulthood through Gprc6a. Diabetes. 63:1021–1031.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Otani T, Mizokami A, Hayashi Y, Gao J,
Mori Y, Nakamura S, Takeuchi H and Hirata M: Signaling pathway for
adiponectin expression in adipocytes by osteocalcin. Cell Signal.
27:532–544. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mera P, Laue K, Ferron M, Confavreux C,
Wei J, Galán-Díez M, Lacampagne A, Mitchell SJ, Mattison JA, Chen
Y, et al: Osteocalcin signaling in myofibers is necessary and
sufficient for optimum adaptation to exercise. Cell Metab.
23:1078–1092. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ferron M, McKee MD, Levine RL, Ducy P and
Karsenty G: Intermittent injections of osteocalcin improve glucose
metabolism and prevent type 2 diabetes in mice. Bone. 50:568–575.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Karsenty G and Oury F: Regulation of male
fertility by the bone-derived hormone osteocalcin. Mol Cell
Endocrinol. 382:521–526. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Le B, Chen H, Zirkin B and Burnett A: New
targets for increasing endogenous testosterone production: Clinical
implications and review of the literature. Andrology. 2:484–490.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Oury F, Ferron M, Huizhen W, Confavreux C,
Wei J, Galán-Díez M, Lacampagne A, Mitchell SJ, Mattison JA, Chen
Y, et al: Osteocalcin regulates murine and human fertility through
a pancreas-bone-testis axis. J Clin Invest. 123:2421–2433. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Smith LB and Saunders PT: The skeleton:
The new controller of male fertility? Cell. 144:642–643. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mizokami A, Yasutake Y, Higashi S,
Kawakubo-Yasukochi T, Chishaki S, Takahashi I, Takeuchi H and
Hirata M: Oral administration of osteocalcin improves glucose
utilization by stimulating glucagon-like peptide-1 secretion. Bone.
69:68–79. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Mizokami A, Yasutake Y, Gao J, Matsuda M,
Takahashi I, Takeuchi H and Hirata M: Osteocalcin induces release
of glucagon-like peptide-1 and thereby stimulates insulin secretion
in mice. PLoS One. 8:e573752013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhao C, Liang J, Yang Y, Yu M and Qu X:
The impact of glucagon-like peptide-1 on bone metabolism and its
possible mechanisms. Front Endocrinol (Lausanne). 8:982017.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ducy P, Desbois C, Boyce B, Pinero G,
Story B, Dunstan C, Smith E, Bonadio J, Goldstein S, Gundberg C, et
al: Increased bone formation in osteocalcin-deficient mice. Nature.
382:448–452. 1996. View
Article : Google Scholar : PubMed/NCBI
|
|
29
|
Li Y and Li K: Osteocalcin induces growth
hormone/insulin-like growth factor-1 system by promoting
testosterone synthesis in male mice. Horm Metab Res. 46:768–773.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Khrimian L, Obri A and Karsenty G:
Modulation of cognition and anxiety-like behavior by bone
remodeling. Mol Metab. 6:1610–1615. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Khrimian L, Obri A, Ramos-Brossier M,
Rousseaud A, Moriceau S, Nicot AS, Mera P, Kosmidis S, Karnavas T,
Saudou F, et al: Gpr158 mediates osteocalcin's regulation of
cognition. J Exp Med. 214:2859–2873. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Obri A, Khrimian L, Karsenty G and Oury F:
Osteocalcin in the brain: From embryonic development to age-related
decline in cognition. Nat Rev Endocrinol. 14:174–182. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Di Nisio A, Rocca MS, Fadini GP, De Toni
L, Marcuzzo G, Marescotti MC, Sanna M, Plebani M, Vettor R, Avogaro
A and Foresta C: The rs2274911 polymorphism in GPRC6A gene is
associated with insulin resistance in normal weight and obese
subjects. Clin Endocrinol (Oxf). 86:185–191. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Pietschmann P and Schernthaner G: The
effect of pirenzepine on growth hormone and blood glucose levels in
type I diabetes mellitus. A controlled study in patients on basal
bolus insulin treatment. Acta Endocrinol (Copenh). 117:315–319.
1988. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Rosato MT, Schneider SH and Shapses SA:
Bone turnover and insulin-like growth factor I levels increase
after improved glycemic control in noninsulin-dependent diabetes
mellitus. Calcif Tissue Int. 63:107–111. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Akin O, Göl K, Aktürk M and Erkaya S:
Evaluation of bone turnover in postmenopausal patients with type 2
diabetes mellitus using biochemical markers and bone mineral
density measurements. Gynecol Endocrinol. 17:19–29. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Achemlal L, Tellal S, Rkiouak F, Nouijai
A, Bezza A, Derouiche el M, Ghafir D and El Maghraoui A: Bone
metabolism in male patients with type 2 diabetes. Clin Rheumatol.
24:493–496. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Sanchez-Enriquez S, Ballesteros-Gonzalez
IT, Villafán-Bernal JR, Pascoe-Gonzalez S, Rivera-Leon EA,
Bastidas-Ramirez BE, Rivas-Carrillo JD, Alcala-Zermeno JL,
Armendariz-Borunda J, Llamas-Covarrubias IM and Zepeda-Moreno A:
Serum levels of undercarboxylated osteocalcin are related to
cardiovascular risk factors in patients with type 2 diabetes
mellitus and healthy subjects. World J Diabetes. 8:11–17. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Díaz-López A, Bulló M, Juanola-Falgarona
M, Martínez-González MA, Estruch R, Covas MI, Arós F and
Salas-Salvadó J: Reduced serum concentrations of carboxylated and
undercarboxylated osteocalcin are associated with risk of
developing type 2 diabetes mellitus in a high cardiovascular risk
population: A nested case-control study. J Clin Endocrinol Metab.
98:4524–4531. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Razny U, Fedak D, Kiec-Wilk B, Goralska J,
Gruca A, Zdzienicka A, Kiec-Klimczak M, Solnica B,
Hubalewska-Dydejczyk A and Malczewska-Malec M: Carboxylated and
undercarboxylated osteocalcin in metabolic complications of human
obesity and prediabetes. Diabetes Metab Res Rev. 33:2017.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Liu C, Wo J, Zhao Q, Wang Y, Wang B and
Zhao W: Association between serum total osteocalcin level and type
2 diabetes mellitus: A systematic review and meta-analysis. Horm
Metab Res. 47:813–819. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Kunutsor SK, Apekey TA and Laukkanen JA:
Association of serum total osteocalcin with type 2 diabetes and
intermediate metabolic phenotypes: Systematic review and
meta-analysis of observational evidence. Eur J Epidemiol.
30:599–614. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Luo Y, Ma X, Hao Y, Xiong Q, Xu Y, Pan X,
Bao Y and Jia W: Relationship between serum osteocalcin level and
carotid intima-media thickness in a metabolically healthy Chinese
population. Cardiovasc Diabetol. 14:822015. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Sheng L, Cao W, Cha B, Chen Z, Wang F and
Liu J: Serum osteocalcin level and its association with carotid
atherosclerosis in patients with type 2 diabetes. Cardiovasc
Diabetol. 12:222013. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Pirilä S, Taskinen M, Turanlahti M,
Kajosaari M, Mäkitie O, Saarinen-Pihkala UM and Viljakainen H: Bone
health and risk factors of cardiovascular disease-a cross-sectional
study in healthy young adults. PLoS One. 9:e1080402014. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Maser RE, Lenhard MJ, Sneider MB and
Pohlig RT: Osteoprotegerin is a better serum biomarker of coronary
artery calcification than osteocalcin in type 2 diabetes. Endocr
Pract. 21:14–22. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Giudici KV PhD, Fisberg RM, Marchioni DML,
Peters BSE and Martini LA: Crosstalk between bone and fat tissue:
Associations between vitamin D, osteocalcin, adipokines, and
markers of glucose metabolism among adolescents. J Am Coll Nutr.
36:273–280. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Tan A, Gao Y, Yang X, Zhang H, Qin X, Mo
L, Peng T, Xia N and Mo Z: Low serum osteocalcin level is a
potential marker for metabolic syndrome: Results from a Chinese
male population survey. Metabolism. 60:1186–1192. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Wang JW, Tang QY, Ruan HJ and Cai W:
Relation between serum osteocalcin levels and body composition in
obese children. J Pediatr Gastroenterol Nutr. 58:729–732.
2014.PubMed/NCBI
|
|
50
|
Alfadda AA, Masood A, Shaik SA, Dekhil H
and Goran M: Association between osteocalcin, metabolic syndrome,
and cardiovascular risk factors: Role of total and
undercarboxylated osteocalcin in patients with type 2 diabetes. Int
J Endocrinol. 2013:1975192013. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Magni P, Macchi C, Sirtori CR and Corsi
Romanelli MM: Osteocalcin as a potential risk biomarker for
cardiovascular and metabolic diseases. Clin Chem Lab Med.
54:1579–1587. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Ma H, Lin H, Hu Y, Li X, He W, Jin X, Gao
J, Zhao N and Gao X: Serum levels of osteocalcin in relation to
glucose metabolism and carotid atherosclerosis in Chinese
middle-aged and elderly male adults: The Shanghai Changfeng Study.
Eur J Intern Med. 25:259–264. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Yang R, Ma X, Dou J, Wang F, Luo Y, Li D,
Zhu J, Bao Y and Jia W: Relationship between serum osteocalcin
levels and carotid intima-media thickness in Chinese postmenopausal
women. Menopause. 20:1194–1199. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Reyes G, arcía R, Rozas Moreno P and
Muñoz-Torres M: Osteocalcin and atherosclerosis: A complex
relationship. Diabetes Res Clin Pract. 92:405–406. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Kanazawa I, Yamaguchi T, Yamamoto M,
Yamauchi M, Kurioka S, Yano S and Sugimoto T: Serum osteocalcin
level is associated with glucose metabolism and atherosclerosis
parameters in type 2 diabetes mellitus. J Clin Endocrinol Metab.
94:45–49. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Bradburn S, McPhee JS, Bagley L, Sipila S,
Stenroth L, Narici MV, Pääsuke M, Gapeyeva H, Osborne G, Sassano L,
et al: Association between osteocalcin and cognitive performance in
healthy older adults. Age Ageing. 45:844–849. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Amin S, El Amrousy D, Elrifaey S, Gamal R
and Hodeib H: Serum osteocalcin levels in children with
nonalcoholic fatty liver disease. J Pediatr Gastroenterol Nutr.
66:117–121. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Abd-Allah Ebrahim HT and El-Behery EG:
Osteocalcin: A new biomarker for non alcoholic fatty liver disease
(NAFLD) in children and adolescents. Clin Med Biochem.
3:1332017.
|
|
59
|
Zhang Q, Riddle RC and Clemens TL: Bone
and the regulation of global energy balance. J Intern Med.
277:681–689. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Iki M, Tamaki J, Fujita Y, et al: Serum
undercarboxylated osteocalcin levels are inversely associated with
glycemic status and insulin resistance in an elderly Japanese male
population: Fujiwara-kyo Osteoporosis Risk in Men (FORMEN) Study.
Osteoporos Int. 23:761–770. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Villafán-Bernal JR, Llamas-Covarrubias MA,
Muñoz-Valle JF, et al: A cut-point value of uncarboxylated to
carboxylated index is associated with glycemic status markers in
type 2 diabetes. J Investig Med. 62:33–36. 2014. View Article : Google Scholar : PubMed/NCBI
|