|
1
|
Edwards DS, Kuhn KM, Potter BK and
Forsberg JA: Heterotopic ossification: A review of current
understanding, treatment, and future. J Orthop Trauma. 30 (Suppl
3):S27–S30. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Hildebrand L, Rossbach B, Kühnen P, Gossen
M, Kurtz A, Reinke P, Seemann P and Stachelscheid H: Generation of
integration free induced pluripotent stem cells from fibrodysplasia
ossificans progressiva (FOP) patients from urine samples. Stem Cell
Res. 16:54–58. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shore EM, Ahn J, Jan de Beur S, Li M, Xu
M, Gardner RJ, Zasloff MA, Whyte MP, Levine MA and Kaplan FS:
Paternally inherited inactivating mutations of the GNAS1 gene in
progressive osseous heteroplasia. N Engl J Med. 346:99–106. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Maruyama R and Yokota T:
Morpholino-mediated exon skipping targeting human ACVR1/ALK2 for
fibrodysplasia ossificans progressiva. Methods Mol Biol.
1828:497–502. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lees-Shepard JB, Yamamoto M, Biswas AA,
Stoessel SJ, Nicholas SE, Cogswell CA, Devarakonda PM, Schneider MJ
Jr, Cummins SM, Legendre NP, et al: Activin-dependent signaling in
fibro/adipogenic progenitors causes fibrodysplasia ossificans
progressiva. Nat Commun. 9:4712018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wu M, Chen G and Li YP: TGF-β and BMP
signaling in osteoblast, skeletal development, and bone formation,
homeostasis and disease. Bone Res. 4:160092016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Abula K, Muneta T, Miyatake K, Yamada J,
Matsukura Y, Inoue M, Sekiya I, Graf D, Economides AN, Rosen V and
Tsuji K: Elimination of BMP7 from the developing limb mesenchyme
leads to articular cartilage degeneration and synovial inflammation
with increased age. FEBS Lett. 589:1240–1248. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pereda A, Martos-Tello JM, Garin I,
Errea-Dorronsoro J and Perez de Nanclares G: Progressive osseous
heteroplasia caused by a mosaic GNAS mutation. Clin Endocrinol
(Oxf). 88:993–955. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Culbert AL, Chakkalakal SA, Theosmy EG,
Brennan TA, Kaplan FS and Shore EM: Alk2 regulates early
chondrogenic fate in fibrodysplasia ossificans progressiva
heterotopic endochondral ossification. Stem Cells. 32:1289–300.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Feldman G, Li M, Martin S, Urbanek M,
Urtizberea JA, Fardeau M, LeMerrer M, Connor JM, Triffitt J, Smith
R, et al: Fibrodysplasia ossificans progressiva, a heritable
disorder of severe heterotopic ossification, maps to human
chromosome 4q27-31. Am J Hum Genet. 66:128–135. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Regard JB, Malhotra D, Gvozdenovic-Jeremic
J, Josey M, Chen M, Weinstein LS, Lu J, Shore EM, Kaplan FS and
Yang Y: Activation of Hedgehog signaling by loss of GNAS causes
heterotopic ossification. Nat Med. 19:1505–1512. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Forsberg JA, Pepek JM, Wagner S, Wilson K,
Flint J, Andersen RC, Tadaki D, Gage FA, Stojadinovic A and Elster
EA: Heterotopic ossification in high-energy wartime extremity
injuries: Prevalence and risk factors. J Bone Joint Surg Am.
91:1084–1091. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kaplan FS, Le Merrer M, Glaser DL, Pignolo
RJ, Goldsby RE, Kitterman JA, Groppe J and Shore EM: Fibrodysplasia
ossificans progressiva. Best Pract Res Clin Rheumatol. 22:191–205.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kaplan FS, Xu M, Glaser DL, Collins F,
Connor M, Kitterman J, Sillence D, Zackai E, Ravitsky V, Zasloff M,
et al: Early diagnosis of fibrodysplasia ossificans progressiva.
Pediatrics. 121:e1295–e1300. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Potter BK, Forsberg JA, Davis TA, Evans
KN, Hawksworth JS, Tadaki D, Brown TS, Crane NJ, Burns TC, O'Brien
FP and Elster EA: Heterotopic ossification following combat-related
trauma. J Bone Joint Surg Am. 92 (Suppl 2):S74–S89. 2010.
View Article : Google Scholar
|
|
16
|
Kan L and Kessler JA: Animal models of
typical heterotopic ossification. J Biomed Biotechnol.
2011:3092872011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Alfieri KA, Forsberg JA and Potter BK:
Blast injuries and heterotopic ossification. Bone Joint Res.
1:192–197. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Shehab D, Elgazzar AH and Collier BD:
Heterotopic ossification. J Nucl Med. 43:346–353. 2002.PubMed/NCBI
|
|
19
|
Pavey GJ, Polfer EM, Nappo KE, Tintle SM,
Forsberg JA and Potter BK: What risk factors predict recurrence of
heterotopic ossification after excision in combat-related
amputations? Clin Orthop Relat Res. 473:2814–2824. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gugala Z, Olmsted-Davis EA, Xiong Y, Davis
EL and Davis AR: Trauma-induced heterotopic ossification regulates
the blood-nerve barrier. Front Neurol. 9:4082018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Juarez JK, Wenke JC and Rivera JC:
Treatments and preventative measures for trauma-induced heterotopic
ossification: A review. Clin Transl Sci. 11:365–370. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Carroll SF, Buckley CT and Kelly DJ:
Cyclic tensile strain can play a role in directing both
intramembranous and endochondral ossification of mesenchymal stem
cells. Front Bioeng Biotechnol. 5:732017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Upadhyay J, Xie L, Huang L, Das N, Stewart
RC, Lyon MC, Palmer K, Rajamani S, Graul C, Lobo M, et al: The
expansion of heterotopic bone in fibrodysplasia ossificans
progressiva is activin A-dependent. J Bone Miner Res. 32:2489–2499.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Xu R, Hu J, Zhou X and Yang Y: Heterotopic
ossification: Mechanistic insights and clinical challenges. Bone.
109:134–142. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lounev VY, Ramachandran R, Wosczyna MN,
Yamamoto M, Maidment AD, Shore EM, Glaser DL, Goldhamer DJ and
Kaplan FS: Identification of progenitor cells that contribute to
heterotopic skeletogenesis. J Bone Joint Surg Am. 91:652–663. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Glaser DL, Economides AN, Wang L, Liu X,
Kimble RD, Fandl JP, Wilson JM, Stahl N, Kaplan FS and Shore EM: In
vivo somatic cell gene transfer of an engineered Noggin mutein
prevents BMP4-induced heterotopic ossification. J Bone Joint Surg
Am. 85:2332–2342. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kan L and Kessler JA: Evaluation of the
cellular origins of heterotopic ossification. Orthopedics.
37:329–340. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ji Y, Christopherson GT, Kluk MW, Amrani
O, Jackson WM and Nesti LJ: Heterotopic ossification following
musculoskeletal trauma: Modeling stem and progenitor cells in their
microenvironment. Adv Exp Med Biol. 720:39–50. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Medici D, Shore EM, Lounev VY, Kaplan FS,
Kalluri R and Olsen BR: Conversion of vascular endothelial cells
into multipotent stem-like cells. Nat Med. 16:1400–1406. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Olmsted-Davis E, Gannon FH, Ozen M,
Ittmann MM, Gugala Z, Hipp JA, Moran KM, Fouletier-Dilling CM,
Schumara-Martin S, Lindsey RW, et al: Hypoxic adipocytes pattern
early heterotopic bone formation. Am J Pathol. 170:620–632. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Olmsted-Davis EA, Salisbury EA, Hoang D,
Davis EL, Lazard Z, Sonnet C, Davis TA, Forsberg JA and Davis AR:
Progenitors in peripheral nerves launch heterotopic ossification.
Stem Cells Transl Med. 6:1109–1119. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Gurkan UA, Golden R, Kishore V, Riley CP,
Adamec J and Akkus O: Immune and inflammatory pathways are involved
in inherent bone marrow ossification. Clin Orthop Relat Res.
470:2528–2540. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Luu HH, Song WX, Luo X, Manning D, Luo J,
Deng ZL, Montag AG, Haydon RC and He TC: Distinct roles of bone
morphogenetic proteins in osteogenic differentiation of mesenchymal
stem cells. J Orthop Res. 25:665–677. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Chen D, Zhao M and Mundy GR: Bone
morphogenetic proteins. Growth Factors. 22:233–241. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Rahman MS, Akhtar N, Jamil HM, Banik RS
and Asaduzzaman SM: TGF-β/BMP signaling and other molecular events:
Regulation of osteoblastogenesis and bone formation. Bone Res.
15005015.
|
|
36
|
Sánchez-Duffhues G, Hiepen C, Knaus P and
Ten Dijke P: Bone morphogenetic protein signaling in bone
homeostasis. Bone. 80:43–59. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Shore EM and Kaplan FS: Role of altered
signal transduction in heterotopic ossification and fibrodysplasia
ossificans progressiva. Curr Osteoporos Rep. 9:83–88. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Bouvard B, Masson C, Legrand E and Audran
M: Fibrodysplasia ossificans progressiva. A case report and focus
on the BMP signaling pathway. Morphologie. 100:250–255. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kan C, Chen L, Hu Y, Ding N, Lu H, Li Y,
Kessler JA and Kan L: Conserved signaling pathways underlying
heterotopic ossification. Bone. 109:43–48. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
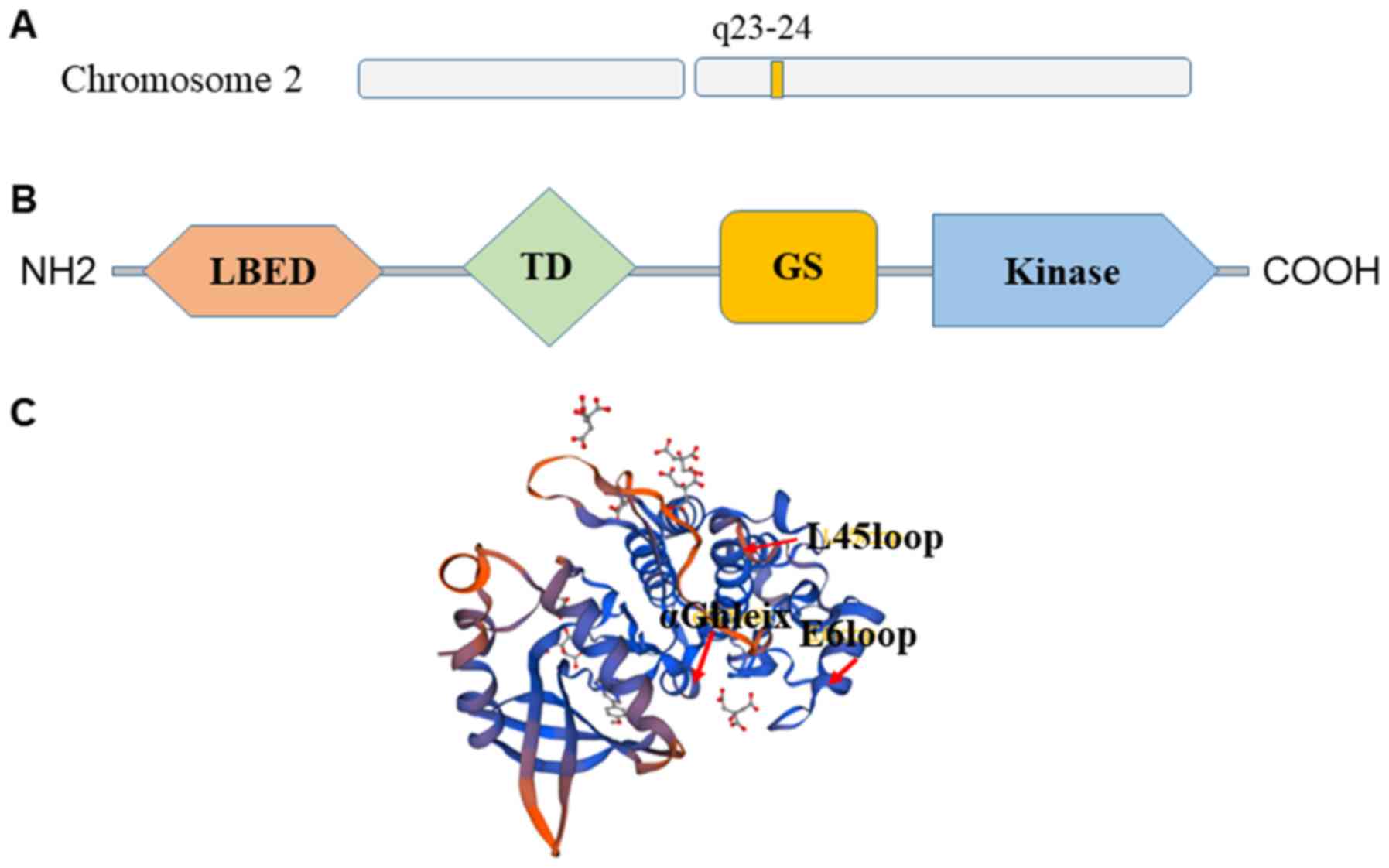
Chaikuad A, Alfano I, Kerr G, Sanvitale
CE, Boergermann JH, Triffitt JT, von Delft F, Knapp S, Knaus P and
Bullock AN: Structure of the bone morphogenetic protein receptor
ALK2 and implications for fibrodysplasia ossificans progressiva. J
Biol Chem. 287:36990–36998. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Dudas M, Sridurongrit S, Nagy A, Okazaki K
and Kaartinen V: Craniofacial defects in mice lacking BMP type I
receptor Alk2 in neural crest cells. Mech Dev. 121:173–182. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Lin H, Ying Y, Wang YY, Wang G, Jiang SS,
Huang D, Luo L, Chen YG, Gerstenfeld LC and Luo Z: AMPK
downregulates ALK2 via increasing the interaction between Smurf1
and Smad6, leading to inhibition of osteogenic differentiation.
Biochim Biophys Acta Mol Cell Res. 1864:2369–2377. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Engers DW, Frist AY, Lindsley CW, Hong CC
and Hopkins CR: Synthesis and structure-activity relationships of a
novel and selective bone morphogenetic protein receptor (BMP)
inhibitor derived from the pyrazolo[1.5-a]pyrimidine scaffold of
dorsomorphin: The discovery of ML347 as an ALK2 versus ALK3
selective MLPCN probe. Bioorg Med Chem Lett. 23:3248–3252. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Machiya A, Tsukamoto S, Ohte S, Kuratani
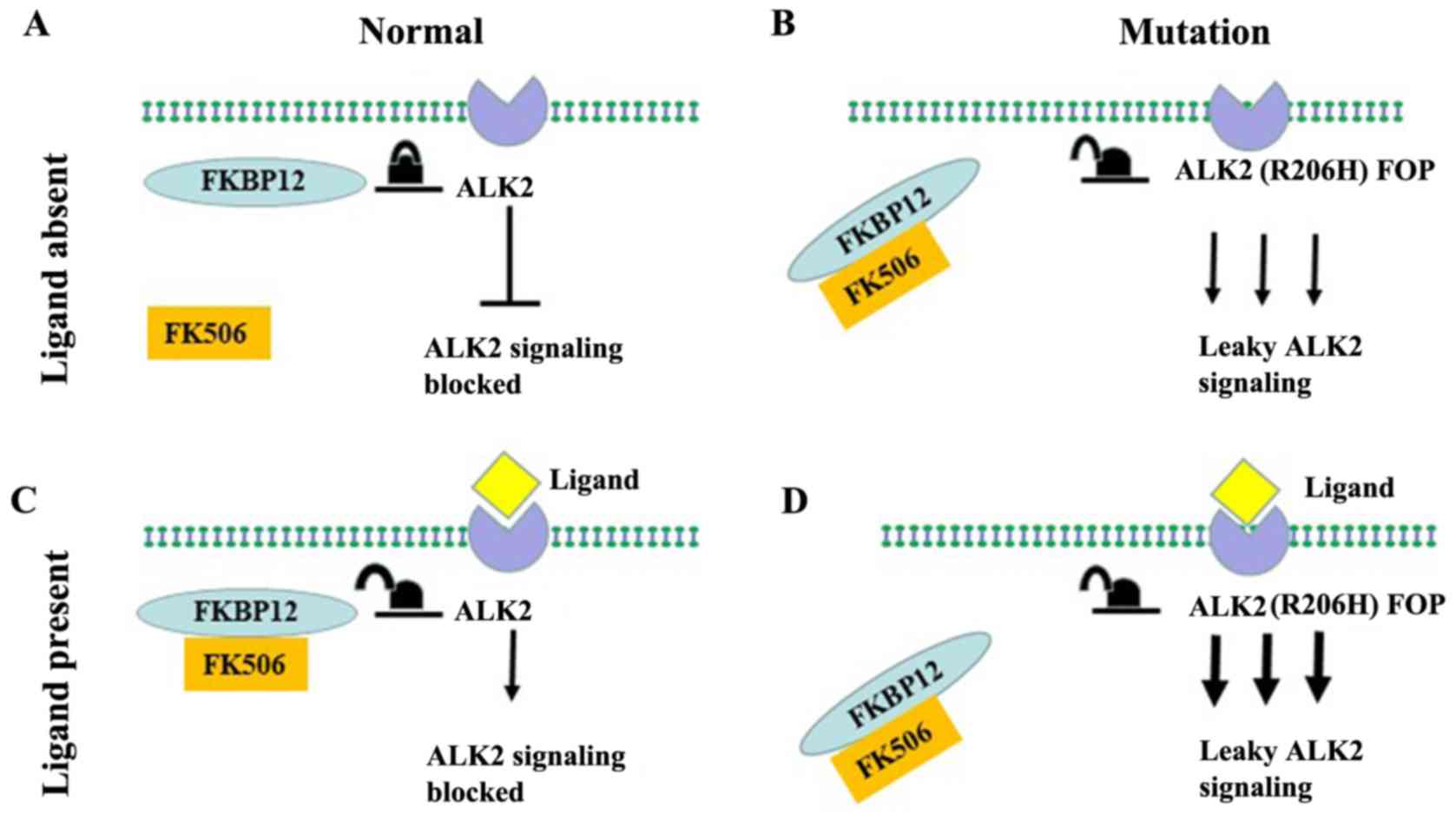
M, Fujimoto M, Kumagai K, Osawa K, Suda N, Bullock AN and Katagiri
T: Effects of FKBP12 and type II BMP receptors on signal
transduction by ALK2 activating mutations associated with genetic
disorders. Bone. 111:101–108. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
van Dinther M, Visser N, de Gorter DJ,
Doorn J, Goumans MJ, de Boer J and ten Dijke P: ALK2 R206H mutation
linked to fibrodysplasia ossificans progressiva confers
constitutive activity to the BMP type I receptor and sensitizes
mesenchymal cells to BMP-induced osteoblast differentiation and
bone formation. J Bone Miner Res. 25:1208–1215. 2010.PubMed/NCBI
|
|
46
|
Chakkalakal SA, Zhang D, Culbert AL,
Convente MR, Caron RJ, Wright AC, Maidment AD, Kaplan FS and Shore
EM: An Acvr1 R206H knock-in mouse has fibrodysplasia ossificans
progressiva. J Bone Miner Res. 27:1746–1756. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Hatsell SJ, Idone V, Wolken DM, Huang L,
Kim HJ, Wang L, Wen X, Nannuru KC, Jimenez J, Xie L, et al:
ACVR1R206H receptor mutation causes fibrodysplasia ossificans
progressiva by imparting responsiveness to activin A. Sci Transl
Med. 7:303ra1372015. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Katagiri T: A door opens for
fibrodysplasia ossificans progressiva. Trends Biochem Sci.
41:119–121. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Yu PB, Deng DY, Lai CS, Hong CC, Cuny GD,
Bouxsein ML, Hong DW, McManus PM, Katagiri T, Sachidanandan C, et
al: BMP type I receptor inhibition reduces heterotopic [corrected]
ossification. Nat Med. 14:1363–1369. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Hino K, Ikeya M, Horigome K, Matsumoto Y,
Ebise H, Nishio M, Sekiguchi K, Shibata M, Nagata S, Matsuda S and
Toguchida J: Neofunction of ACVR1 in fibrodysplasia ossificans
progressiva. Proc Natl Acad Sci USA. 112:15438–15443. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Olsen OE, Wader KF, Hella H, Mylin AK,
Turesson I, Nesthus I, Waage A, Sundan A and Holien T: Activin A
inhibits BMP-signaling by binding ACVR2A and ACVR2B. Cell Commun
Signal. 13:272015. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Wang H, Lindborg C, Lounev V, Kim JH,
McCarrick-Walmsley R, Xu M, Mangiavini L, Groppe JC, Shore EM,
Schipani E, et al: Cellular hypoxia promotes heterotopic
ossification by amplifying BMP signaling. J Bone Miner Res.
31:1652–1665. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Kent WT, Shelton TJ and Eastman J:
Heterotopic ossification around the knee after tibial nailing and
ipsilateral antegrade and retrograde femoral nailing in the
treatment of floating knee injuries. Int Orthop. 42:1379–1385.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Wang YK, Sun WF, Liu XG, Deng J, Yan BE,
Jiang WY and Lin XB: Comparative study of serum levels of BMP-2 and
heterotopic ossification in traumatic brain injury and fractures
patients. Zhongguo Gu Shang. 24:399–403. 2011.(In Chinese).
PubMed/NCBI
|
|
55
|
Peterson JR, De La Rosa S, Eboda O, Cilwa
KE, Agarwal S, Buchman SR, Cederna PS, Xi C, Morris MD, Herndon DN,
et al: Treatment of heterotopic ossification through remote ATP
hydrolysis. Sci Transl Med. 6:255ra1322014. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Kang H, Dang AB, Joshi SK, Halloran B,
Nissenson R, Zhang X, Li J, Kim HT and Liu X: Novel mouse model of
spinal cord injury-induced heterotopic ossification. J Rehabil Res
Dev. 51:1109–1118. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Lengner CJ, Lepper C, van Wijnen AJ, Stein
JL, Stein GS and Lian JB: Primary mouse embryonic fibroblasts: A
model of mesenchymal cartilage formation. J Cell Physiol.
200:327–333. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Sun E and Hanyu-Deutmeyer AA: Heterotopic
Ossification. StatPearlsTreasure Island (FL): StatPearls Publishing
StatPearls Publishing LLC; 2018
|
|
59
|
Beckmann JT, Wylie JD, Potter MQ, Maak TG,
Greene TH and Aoki SK: Effect of naproxen prophylaxis on
heterotopic ossification following hip arthroscopy: A double-blind
randomized placebo-controlled trial. J Bone Joint Surg Am.
97:2032–2037. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Rivera JC, Hsu JR, Noel SP, Wenke JC and
Rathbone CR: Locally delivered nonsteroidal antiinflammatory drug:
A potential option for heterotopic ossification prevention. Clin
Transl Sci. 8:591–593. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Rath E, Warschawski Y, Maman E, Dolkart O,
Sharfman ZT, Salai M and Amar E: Selective COX-2 inhibitors
significantly reduce the occurrence of heterotopic ossification
after Hip arthroscopic surgery. Am J Sports Med. 44:677–681. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Beckmann JT, Wylie JD, Kapron AL, Hanson
JA, Maak TG and Aoki SK: The effect of NSAID prophylaxis and
operative variables on heterotopic ossification after Hip
arthroscopy. Am J Sports Med. 42:1359–1364. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Haran M, Bhuta T and Lee B:
Pharmacological interventions for treating acute heterotopic
ossification. Cochrane Database Syst Rev. CD0033212004.PubMed/NCBI
|
|
64
|
Salazar D, Golz A, Israel H and Marra G:
Heterotopic ossification of the elbow treated with surgical
resection: Risk factors, bony ankylosis, and complications. Clin
Orthop Relat Res. 472:2269–2275. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Sheybani A, TenNapel MJ, Lack WD, Clerkin
P, Hyer DE, Sun W and Jacobson GM: Risk of radiation-induced
malignancy with heterotopic ossification prophylaxis: A
case-control analysis. Int J Radiat Oncol Biol Phys. 89:584–589.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Kaplan FS, Pignolo RJ, Al Mukaddam MM and
Shore EM: Hard targets for a second skeleton: Therapeutic horizons
for fibrodysplasia ossificans progressiva (FOP). Expert Opin Orphan
Drugs. 5:291–294. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Cappato S, Tonachini L, Giacopelli F,
Tirone M, Galietta LJ, Sormani M, Giovenzana A, Spinelli AE,
Canciani B, Brunelli S, et al: High-throughput screening for
modulators of ACVR1 transcription: Discovery of potential
therapeutics for fibrodysplasia ossificans progressiva. Dis Model
Mech. 9:685–696. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Glister C, Regan SL, Samir M and Knight P:
Gremlin, Noggin, Chordin and follistatin differentially modulate
BMP induced suppression of androgen secretion by bovine ovarian
theca cells. J Mol Endocrinol. Oct 1–2018.(Epub ahead of print).
PubMed/NCBI
|
|
69
|
Yu PB, Hong CC, Sachidanandan C, Babitt
JL, Deng DY, Hoyng SA, Lin HY, Bloch KD and Peterson RT:
Dorsomorphin inhibits BMP signals required for embryogenesis and
iron metabolism. Nat Chem Biol. 4:33–41. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Cuny GD, Yu PB, Laha JK, Xing X, Liu JF,
Lai CS, Deng DY, Sachidanandan C, Bloch KD and Peterson RT:
Structure-activity relationship study of bone morphogenetic protein
(BMP) signaling inhibitors. Bioorg Med Chem Lett. 18:4388–4392.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Mohedas AH, Xing X, Armstrong KA, Bullock
AN, Cuny GD and Yu PB: Development of an ALK2-biased BMP type I
receptor kinase inhibitor. ACS Chem Biol. 8:1291–1302. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Hao J, Ho JN, Lewis JA, Karim KA, Daniels
RN, Gentry PR, Hopkins CR, Lindsley CW and Hong CC: In vivo
structure-activity relationship study of dorsomorphin analogues
identifies selective VEGF and BMP inhibitors. ACS Chem Biol.
5:245–253. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Tsugawa D, Oya Y, Masuzaki R, Ray K,
Engers DW, Dib M, Do N, Kuramitsu K, Ho K, Frist A, et al: Specific
activin receptor-like kinase 3 inhibitors enhance liver
regeneration. J Pharmacol Exp Ther. 351:549–558. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Mohedas AH, Wang Y, Sanvitale CE, Canning
P, Choi S, Xing X, Bullock AN, Cuny GD and Yu PB:
Structure-activity relationship of 3,5-diaryl-2-aminopyridine ALK2
inhibitors reveals unaltered binding affinity for fibrodysplasia
ossificans progressiva causing mutants. J Med Chem. 57:7900–7915.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Williams E and Bullock AN: Structural
basis for the potent and selective binding of LDN-212854 to the BMP
receptor kinase ALK2. Bone. 109:251–258. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Dey D, Bagarova J, Hatsell SJ, Armstrong
KA, Huang L, Ermann J, Vonner AJ, Shen Y, Mohedas AH, Lee A, et al:
Two tissue-resident progenitor lineages drive distinct phenotypes
of heterotopic ossification. Sci Transl Med. 8:366ra1632016.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Giacopelli F, Cappato S, Tonachini L, Mura
M, Di Lascio S, Fornasari D, Ravazzolo R and Bocciardi R:
Identification and characterization of regulatory elements in the
promoter of ACVR1, the gene mutated in Fibrodysplasia Ossificans
Progressiva. Orphanet J Rare Dis. 8:1452013. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Li L, Liu Y, Guo Y, Liu B, Zhao Y, Li P,
Song F, Zheng H, Yu J, Song T, et al: Regulatory MiR-148a-ACVR1/BMP
circuit defines a cancer stem cell-like aggressive subtype of
hepatocellular carcinoma. Hepatology. 61:574–584. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Zumbrennen-Bullough KB, Wu Q, Core AB,
Canali S, Chen W, Theurl I, Meynard D and Babitt JL: MicroRNA-130a
is up-regulated in mouse liver by iron deficiency and targets the
bone morphogenetic protein (BMP) receptor ALK2 to attenuate BMP
signaling and hepcidin transcription. J Biol Chem. 289:23796–23808.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Song H, Wang Q, Wen J, Liu S, Gao X, Cheng
J and Zhang D: ACVR1, a therapeutic target of fibrodysplasia
ossificans progressiva, is negatively regulated by miR-148a. Int J
Mol Sci. 13:2063–2077. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Mura M, Cappato S, Giacopelli F, Ravazzolo
R and Bocciardi R: The role of the 3′UTR region in the regulation
of the ACVR1/Alk-2 gene expression. PLoS One. 7:e509582012.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Karbiener M, Neuhold C, Opriessnig P,
Prokesch A, Bogner-Strauss JG and Scheideler M: MicroRNA-30c
promotes human adipocyte differentiation and co-represses PAI-1 and
ALK2. RNA Biol. 8:850–860. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Shi S, Cai J, de Gorter DJ,
Sanchez-Duffhues G, Kemaladewi DU, Hoogaars WM, Aartsma-Rus A, 't
Hoen PA and ten Dijke P: Antisense-oligonucleotide mediated exon
skipping in activin-receptor-like kinase 2: Inhibiting the receptor
that is overactive in fibrodysplasia ossificans progressiva. PLoS
One. 8:e690962013. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Takahashi M, Katagiri T, Furuya H and
Hohjoh H: Disease-causing allele-specific silencing against the
ALK2 mutants, R206H and G356D, in fibrodysplasia ossificans
progressiva. Gene Ther. 19:781–785. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Kaplan J, Kaplan FS and Shore EM:
Restoration of normal BMP signaling levels and osteogenic
differentiation in FOP mesenchymal progenitor cells by mutant
allele-specific targeting. Gene Ther. 19:786–790. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Aartsma-Rus A, Fokkema I, Verschuuren J,
Ginjaar I, van Deutekom J, van Ommen GJ and den Dunnen JT:
Theoretic applicability of antisense-mediated exon skipping for
Duchenne muscular dystrophy mutations. Hum Mutat. 30:293–299. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Miki Y, Morioka T, Shioi A, Fujimoto K,
Sakura T, Uedono H, Kakutani Y, Ochi A, Mori K, Shoji T, et al:
Oncostatin M induces C2C12 myotube atrophy by modulating muscle
differentiation and degradation. Biochem Biophys Res Commun.
516:951–956. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Yamamoto R, Matsushita M, Kitoh H, Masuda
A, Ito M, Katagiri T, Kawai T, Ishiguro N and Ohno K: Clinically
applicable antianginal agents suppress osteoblastic transformation
of myogenic cells and heterotopic ossifications in mice. J Bone
Miner Metab. 31:26–33. 2013.PubMed/NCBI
|
|
89
|
Kitoh H, Achiwa M, Kaneko H, Mishima K,
Matsushita M, Kadono I, Horowitz JD, Sallustio BC, Ohno K and
Ishiguro N: Perhexiline maleate in the treatment of fibrodysplasia
ossificans progressiva: An open-labeled clinical trial. Orphanet J
Rare Dis. 8:1632013. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Kaplan FS, Pignolo RJ and Shore EM: From
mysteries to medicines: Drug development for fibrodysplasia
ossificans progressive. Expert Opin Orphan Drugs. 1:637–649. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Cappato S, Giacopelli F, Ravazzolo R and
Bocciardi R: The horizon of a therapy for rare genetic diseases: A
‘Druggable’ future for fibrodysplasia ossificans progressiva. Int J
Mol Sci. 19(pii): E9892018. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Pang J, Zuo Y, Chen Y, Song L, Zhu Q, Yu
J, Shan C, Cai Z, Hao J, Kaplan FS, et al: ACVR1-Fc suppresses BMP
signaling and chondro-osseous differentiation in an in vitro model
of Fibrodysplasia ossificans progressiva. Bone. 92:29–36. 2016.
View Article : Google Scholar : PubMed/NCBI
|