Introduction
Rheumatoid arthritis (RA) is a clinically common,
chronic, systemic autoimmune disease characterized by ‘tumor-like’
abnormal excessive proliferation of joint synovial cells,
inflammatory cell infiltration, pannus formation, and cartilage and
bone destruction (1–4). However, the precise mechanisms
associated with the pathogenesis of RA have yet to be fully
elucidated. With the deepening of research on the pathogenesis of
RA, it has been revealed that an imbalance between cell
proliferation of the joint synovial membrane and apoptosis is
closely associated with the progression of RA (5–8). The
tumor suppressor gene, p53, exerts a crucial role in the induction
of cell apoptosis, and serves as the transcription factor for some
anti- and pro-apoptotic proteins; namely, Bax,
phorbol-12-myristate-13-acetate-induced protein 1 (Noxa), p53
upregulated modulator of apoptosis (PUMA) and mouse double minute 2
homolog (MDM2) (9–14). MDM2 is an important negative
regulator of p53, which, upon combining with p53, inhibits
apoptosis and stimulates cellular inflammation via forming a
negative feedback regulatory loop, therefore functioning in a
p53-dependent capacity (15,16).
Bax, Noxa, and PUMA are pro-apoptotic proteins belonging to the
B-cell lymphoma-2 (Bcl-2) protein family, and are closely
associated with mitochondrial-dependent apoptosis, serving as major
effectors of p53-mediated cell death (17–19).
A previously published study suggested that the upregulated p53
gene in chondrocytes of patients with RA was closely associated
with the apoptosis of RA cells (20). Overexpression of the p53 gene in
the early stages of disease led to an increase in synovial
fibroblast apoptosis, thereby alleviating progression of the
disease in an adjuvant arthritis (AA) rat model (21). The expression of MDM2 in
fibroblasts of patients with RA was significantly increased and
positively correlated with the disease activity of RA, and
inhibition of MDM2 effectively inhibited the inflammatory response
of RA (16). Upregulation of Bax,
Noxa and PUMA has been observed in the apoptosis model of RA
fibroblast-like synoviocytes (22–26).
Clinical studies have confirmed that acupuncture has
the potential to be an effective therapy for patients with RA via
inhibiting the inflammatory reaction and autoimmunity (27–29).
Animal experimental studies have also confirmed that
electroacupuncture (EA) intervention may lead to a significant
inhibition of infiltration of local inflammatory cells, a decrease
in the expression of inflammatory cytokines, and the proliferation
of synovial cells, thereby effectively hindering disease
progression in an RA rat model (28,30–32).
An additional previously published study disclosed that the
regulation of apoptosis was involved in the protective effects of
acupuncture (33). It has been
demonstrated that acupuncture intervention is able to improve
memory and cognitive function by means of inhibiting neuronal
apoptosis via increases in the expression of p53 protein in the
cerebral cortex of Alzheimer's disease model mice (34). However, knockout of the p53 gene in
the midbrain dopamine neurons of Alzheimer's disease model mice was
able to eliminate the protective effect of acupuncture (35). Furthermore, previous evidence has
also suggested that EA protects rats from ischemic brain injury by
inhibiting the protein level of MDM2 (36). EA stimulation was also able to
inhibit cerebral ischemia (CI) injury-induced cell apoptosis of
cerebral and myocardial tissues in CI rats, which was discussed as
being potentially associated with the downregulation of Bax
expression, and upregulation of Bcl-2 expression, in both
myocardial and cerebral tissues (37). Furthermore, it has been revealed
that EA improves learning and memory ability, and protects
pyramidal cells from apoptosis, by blocking expression of p53 and
Noxa in the hippocampal CA1 region of vascular dementia (VD) rats.
Increasing expression levels of p53 and Noxa, therefore, have
important roles in the pathogenesis of VD (38). Considered collectively, these
results suggest that acupuncture may be able to treat certain
diseases by regulating p53, Bax, Noxa, and MDM2. However, to the
best of our knowledge, whether EA is able to suppress proliferation
by regulating the p53 signaling pathway has not been previously
investigated. In the present study, an AA rat model was
established, and the molecular mechanism was investigated via the
simultaneous EA of the acupoints ‘Zusanli’ (ST36) and ‘Xuanzhong’
(GB39).
Materials and methods
Animals and experimental design
The present study was approved by the Scientific
Investigation Board of the Chengdu University of Traditional
Chinese Medicine. All animal experiments followed the National
Institutes of Health Guide for the Care and Use of Laboratory
Animals (39). A total of 40
7-week-old male Sprague-Dawley rats (weight, 170–180 g) were
provided by Chengdu Dashuo Laboratory Animal Co., Ltd and housed
under standard conditions of temperature and humidity (12: 12 h
light: Dark cycle; indoor temperature, 23±3°C; humidity, 60±10%).
In addition, rats had ad libitum access to standard rodent
chow and water. After a 7 day period of acclimation, rats were
randomly divided into four groups, with 10 rats/group: Control; AA;
AA + EA; and AA + sham EA.
Experimental induction of AA in rats
and EA treatment
With the exception of the control rats, all rats
received an intradermal injection of 0.1 ml Complete™ Freund's
adjuvant (CFA; cat. no. F5881; Merck KGaA) into both hind paws to
induce AA. An equivalent volume of saline was administered to each
rat in the control group by intradermal injection. On day 3
following AA induction, EA stimulation was performed with sterile
metallic needles (Beijing Tianyuheng Technology Co., Ltd.) with a
width of 0.25 mm and a length of 25 mm, which synchronously entered
the ST36 (7 mm depth) and GB39 (3 mm depth) acupoints, as described
previously (31). The pattern of
stimulus frequency and duration was 2 Hz for 15 min using a
commercial electric acupuncture apparatus (SDZ-II; Suzhou Medical
Appliance Factory). EA treatment was administered every other day
for 16 days. In the AA + sham EA group, similar EA procedures were
performed; however, the needles were inserted into inappropriate
acupoints (specifically, rats in the AA + sham EA group were
treated with percutaneous electrical stimulation at a position of 5
mm away from the acupoints of ST36 and GB39).
Evaluation of development of
arthritis
The arthritic index and foot swelling (i.e.,
measurement of the hindlimb paw volume) were measured on days 0, 3,
8, 13 and 18 following AA induction, as previously described
(30,40). In brief, the polyarthritis severity
was graded on a scale of 0–4, and scored as follows: 0, no
swelling; 1, swelling of finger joints; 2, mild swelling of ankle
or wrist joints; 3, severe inflammation of the entire paws; 4, paws
with deformity or ankylosis. The foot swelling was determined by a
volume drainage method using a plethysmograph apparatus (YLS-7A;
Yiyan Sci, Ltd.).
Histopathological analysis
The rats were sacrificed on day 18 following AA
induction by intraperitoneal injection with 200 mg/kg sodium
pentobarbital. Following previous studies of histological analysis
(41,42), the ankle joints were harvested and
fixed in 4% paraformaldehyde for 48 h at 4°C, and then were
subsequently decalcified using a commercial tissue decalcification
reagent according to the manufacturer's protocol (cat. no. G1107;
Wuhan Servicebio Technology Co., Ltd.) and embedded in paraffin.
The tissues were then sliced into 4-µm thick sections. Following
washing with xylene I and II for 20 min and dehydration with 100,
95, 80 and 70% ethanol for 5 min each, the sections were stained
with hematoxylin for 30 min at 25°C, washed with water for 20 min,
stained with eosin for 5 min at 25°C. Finally, images of the
sections were captured under a light microscope (BX53; Olympus
Corporation) at magnification, ×400. The stained sections were
scored blindly by 2 investigators, as described previously
(30).
Terminal
deoxynucleotidyl-transferase-mediated dUTP nick end labeling
(TUNEL) staining
The effect of EA on apoptosis was determined using a
TUNEL assay, according to the manufacturer's protocol (cat. no.
ab15251; Roche Diagnostics). Briefly, following fixation in 4%
paraformaldehyde for 48 h at 4°C, and after deparaffinization and
dehydration, the ankle joint sections were treated with proteinase
K (20 µg/ml) for 15 min at room temperature. Subsequently,
equilibration buffer was applied for 10 sec, and the specimens were
immersed and incubated for 1 h in working strength terminal
deoxynucleotidyl transferase (TdT) enzyme solution at 37°C.
Following incubation in stop/wash buffer for 10 min to terminate
the reaction, sections were incubated for 30 min in working
strength anti-digoxigenin conjugate at room temperature in the dark
to visualize the DNA fragments. Proteinase K, equilibration buffer,
and stop/wash buffer were all included in the TUNEL assay kit.
Finally, the slides were counterstained with 0.5 µg/ml DAPI, and
mounted in fluorescence mounting medium. Sections treated only with
reaction buffer lacking the TdT enzyme were used as negative
controls. To quantify the numbers of apoptotic cells, images of 6
randomly chosen high power fields/slide at magnification, ×200,
were captured by a blinded examiner using a wide-field fluorescence
microscope (Olympus BX53; Olympus Corporation). TUNEL+
nuclei were quantified by automatic counting using ImageJ software
(v.1.47t; National Institutes of Health).
RNA isolation and reverse
transcription-quantitative polymerase chain reaction (RT-qPCR)
Total RNA was extracted from synovial tissues using
an RNA extraction kit (cat. no. G3013; Wuhan Servicebio Technology
Co., Ltd). RNA was quantified using a NanoDrop™ 2000
spectrophotometer (NanoDrop Technologies; Thermo Fisher Scientific,
Inc.), and then immediately reverse-transcribed into cDNA using a
cDNA synthesis kit (cat. no. K1622; Thermo Fisher Scientific, Inc.,
Waltham, MA, USA), according to the manufacturer's protocols.
Subsequently, qPCR was performed with SYBR® Premix EX
Taq™ II (Takara Biotechnology Co., Ltd.) on an ABI
PRISM® 7900HT Sequence Detection system (Thermo Fisher
Scientific, Inc.). The thermocycling protocol was as follows:
Initial denaturation at 95°C for 10 min, followed by 45 cycles of
15 sec at 95°C (denaturation), 60 sec at 60°C (primer annealing)
and 15 sec at 60°C (elongation), and a final extension step for 10
min at 72°C. The primer sequences used for qPCR are presented in
Table I. GAPDH was used as the
internal reference, and relative gene expression levels were
calculated using the 2−ΔΔCq method (43).
 | Table I.Primers used for reverse
transcription-quantitative polymerase chain reaction in the present
study. |
Table I.
Primers used for reverse
transcription-quantitative polymerase chain reaction in the present
study.
| Gene | Primer sequences
(5′-3′) |
|---|
| GAPDH | F:
CTGGAGAAACCTGCCAAGTATG |
|
| R:
GGTGGAAGAATGGGAGTTGCT |
| p53 | F:
GGAATCTTCTGGGACGGGA |
|
| R:
CCACGGATCTTAAGGGTGAAAT |
| MDM2 | F:
AGGCAGAAGAAGGCTTAGATGTG |
|
| R:
CGGCTGGGAATAGTCGTCAC |
Western blot analysis
As described previously (44), frozen rat ankle synovial tissues
were homogenized in cold whole cell lysis buffer (cat. no. G2002;
Wuhan Servicebio Technology Co., Ltd.) and subsequently centrifuged
at 14,000 × g for 5 min at 4°C. Protein concentration in the
supernatant was standardized using a protein concentration assay
kit (cat. no. G2026; Wuhan Servicebio Technology Co., Ltd.). A
total of 40 µg protein per lane was separated using 10% SDS-PAGE
gels, and subsequently transferred onto polyvinylidene difluoride
membranes. The membranes were blocked with 5% bovine serum albumin
(cat. no. G2013; Wuhan Servicebio Technology Co., Ltd.) for 2 h at
25°C, followed by incubation with primary antibodies against p53
(dilution, 1:1,000; cat. no. ab131442; Abcam), MDM2 (1:1,000; cat.
no. ab38618; Abcam), PUMA (1:1,000; cat. no,. bs-1573R; BIOSS), Bax
(1:500; cat. no. bs-0127M; BIOSS), NOXA (1:1,000; cat. no.
bs-19322R; BIOSS), β-actin (1:3,000; cat. no. GB12001; Wuhan
Servicebio Technology Co., Ltd.), and GAPDH [1:1,000; cat. no.
70-ab011-100; MultiSciences (Lianke) Biotech Co., Ltd.] overnight
at 4°C. The following day, membranes were incubated with
horseradish peroxidase-conjugated goat anti-rabbit immunoglobulin G
secondary antibodies (1:5,000; cat. no. 70-GAR007; MultiSciences)
for 2 h at 25°C. Finally, protein bands were developed using a
Chemidoc™ XRS Imaging system (Bio-Rad Laboratories, Inc.). The
bands of interest were quantified, and normalized against GAPDH
using Image-Pro Plus v.6.0 software (Media Cybernetics, Inc.).
Statistical analysis
The data are presented as the mean ± standard
deviation. Differences between groups were analyzed using one-way
analysis of variance, followed by Tukey multiple comparison
post-hoc tests. Statistical analyses were performed with SPSS 19.0
software (IBM Corp.). P<0.05 was considered to indicate a
statistically significant difference.
Results
EA stimulation decreases the arthritis
index scores of AA rats
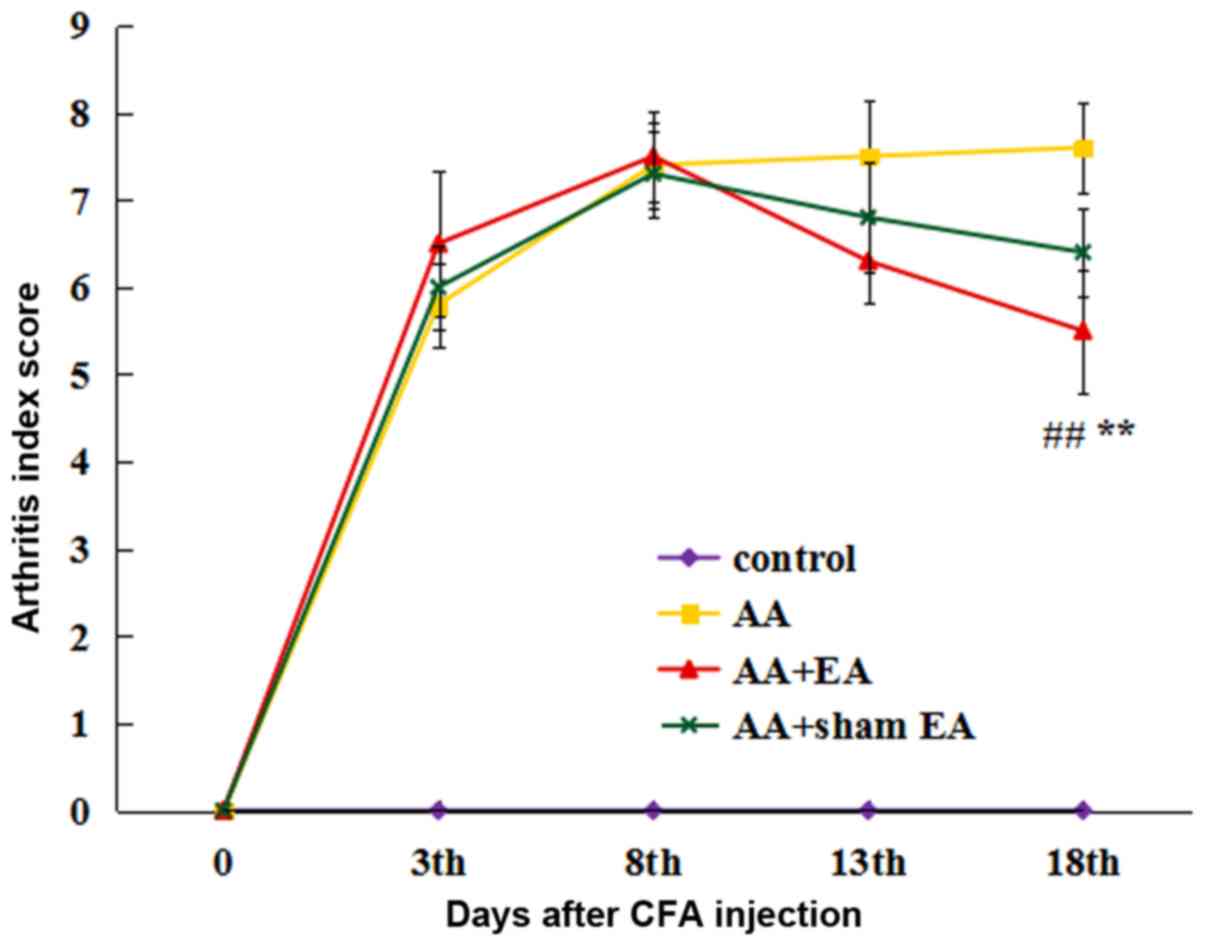
As presented in Fig.
1, the arthritis index scores in the AA, AA + EA and AA + sham
EA groups were significantly increased on day 3 following AA
induction (P<0.01), indicating that the AA model had been
successfully established. During the course of the experiment, the
arthritis index score in the AA group increased gradually. EA
intervention significantly decreased the arthritis index score
(P<0.01). However, no significant differences were identified
between the AA + sham EA and AA groups (P>0.05).
EA stimulation inhibits foot swelling
in AA rats
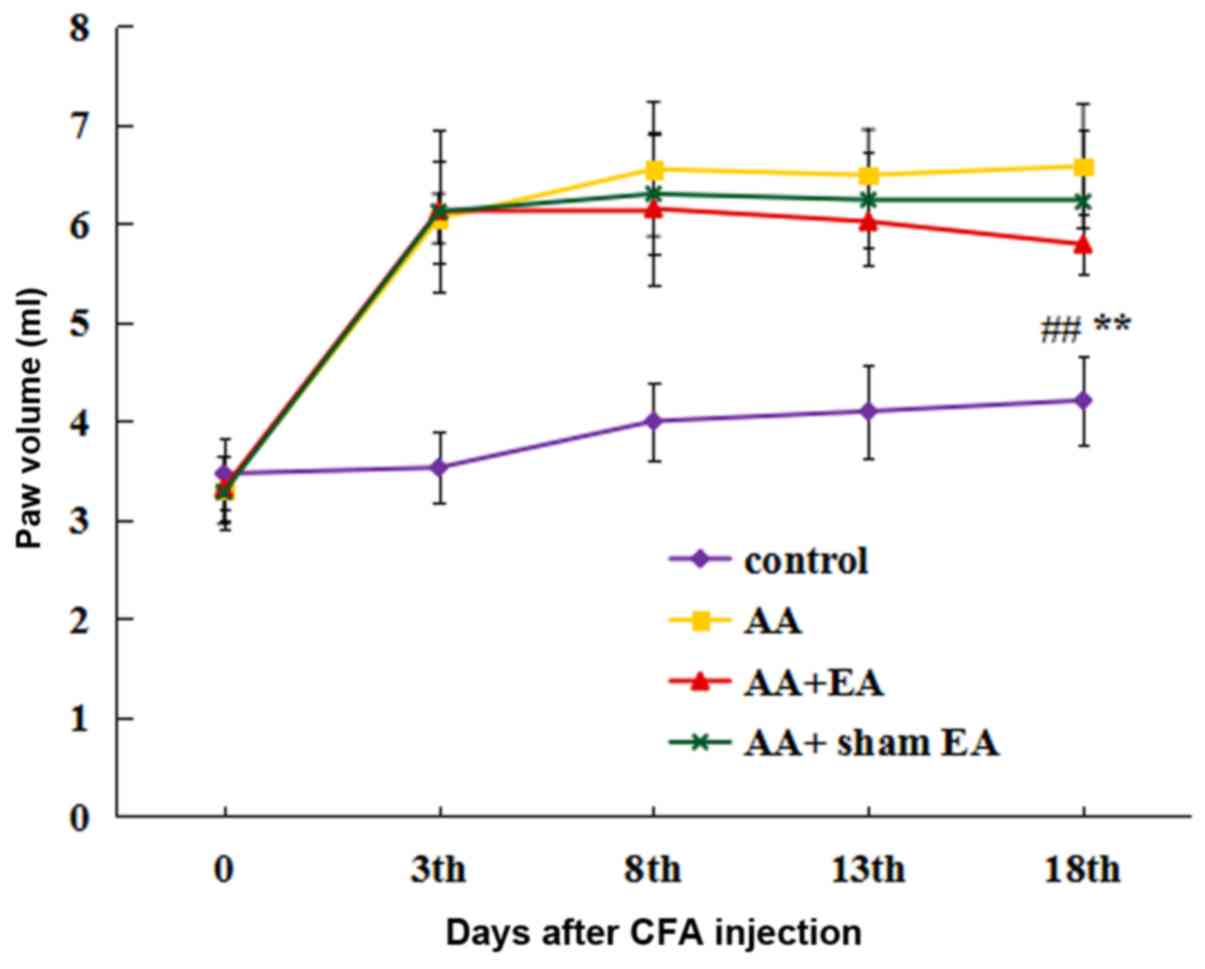
The foot swelling was measured by the volume
drainage method (Fig. 2). Prior to
initiation of the experiment, no significant differences in the
size of foot swelling were observed between the groups. At 3 days
after the injection of CFA, a significant increase in foot volume
was observed in all groups, with the exception of the control
group. After 8 sessions of EA stimulation, foot swelling in the AA
+ EA group was markedly alleviated compared with that in the AA
group (P<0.01); by contrast, foot swelling in the AA + sham EA
group was not decreased compared with that in the AA group
(P>0.05).
EA stimulation improves the
pathological morphology of synovial tissue in AA rats
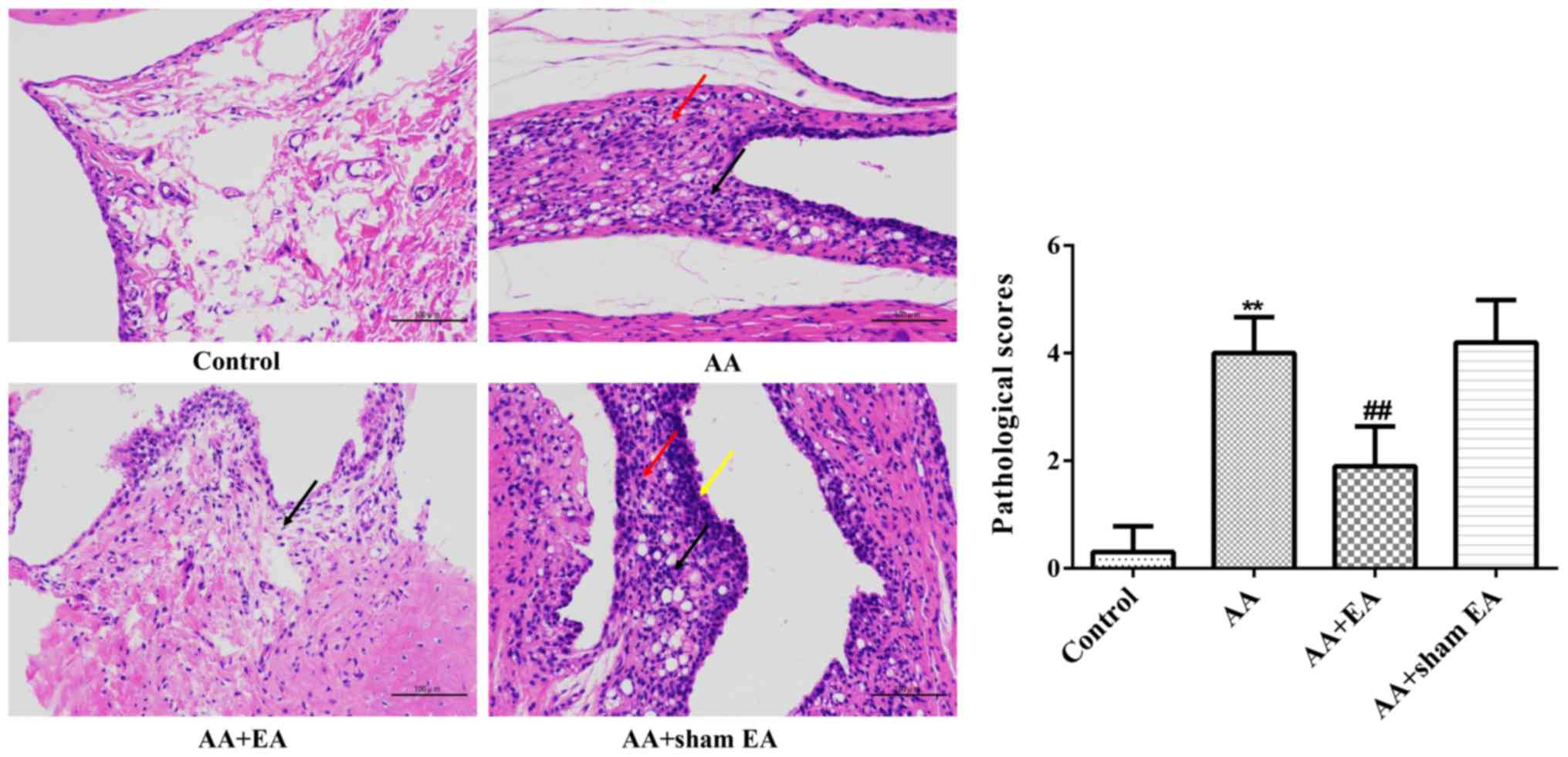
Histological analysis revealed that the
inner-surface-layer synovial cells in the ankle joint of the
control group were smooth and flat, and the cells were neatly
arranged without any indications of inflammatory cell infiltration
or synovial cell proliferation (Fig.
3). By contrast, the synovial tissue of the ankle joint was
highly proliferated, with irregular cell arrangement, significant
infiltration of inflammatory cells, increased new capillary
development, pannus formation, and synovitis in the AA group.
However, in the AA + EA group, the results of H&E staining
appeared to be similar to those of the control group.
EA stimulation increases the apoptotic
rate of synovial cells in AA rats
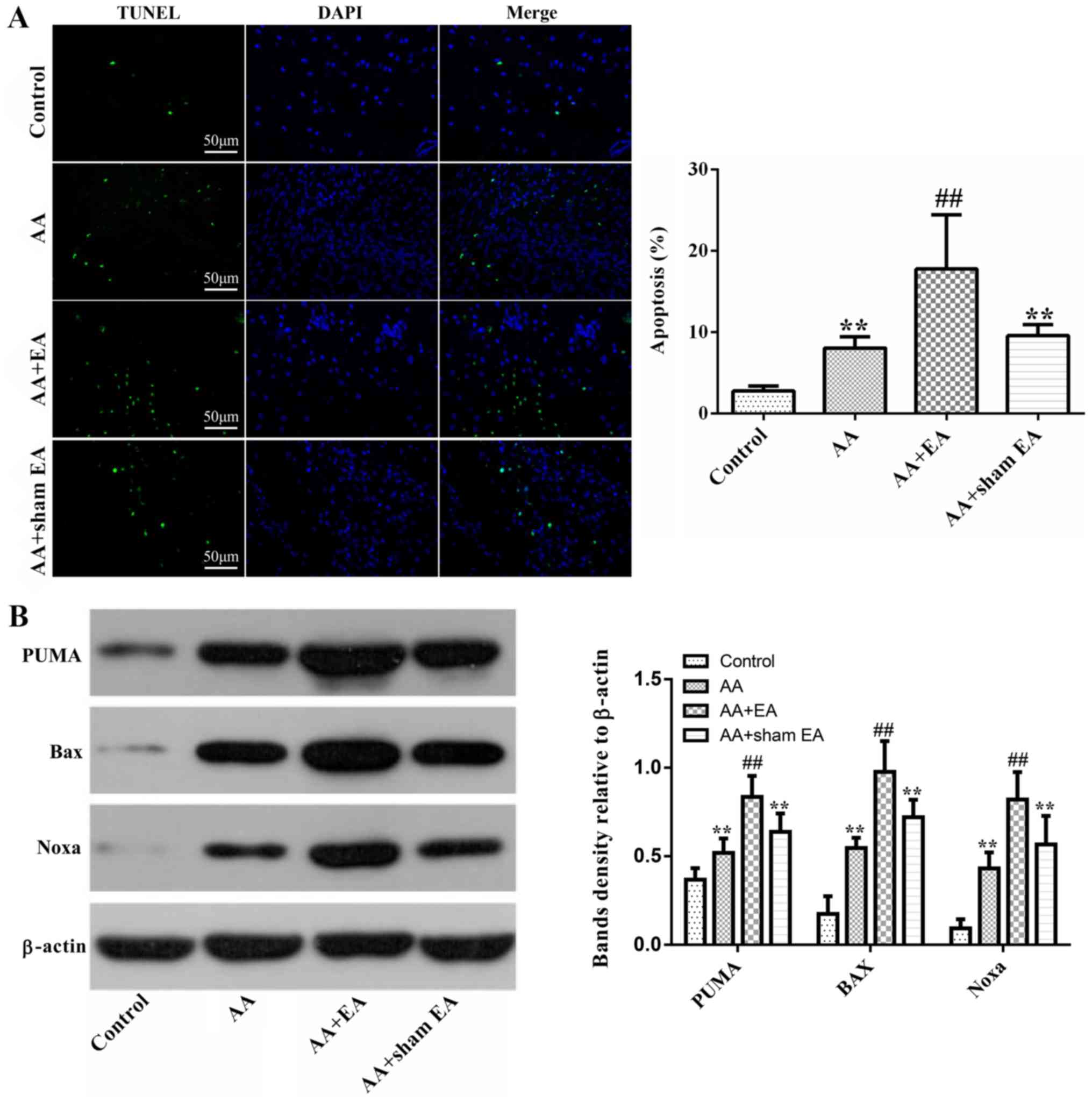
Subsequently, cell death was observed using a TUNEL
assay. Compared with the control group, the percentage of
TUNEL-positive cells increased markedly in the AA group (P<0.01;
Fig. 4A). However, compared with
the AA + sham EA and AA groups, EA stimulation led to a further,
marked increase in the number of TUNEL-positive cells (P<0.01).
Additionally, no significant difference in the apoptotic cell ratio
was observed between the AA + sham EA and AA groups
(P>0.05).
Subsequently, expression levels of the
pro-apoptosis--associated proteins, Bax, Noxa and PUMA, were
detected by western blot analysis. As demonstrated in Fig. 4B, treatment of rats with AA
resulted in increased Bax, Noxa and PUMA protein levels compared
with the control group (P<0.01). EA stimulation caused an
additional increase in Bax, Noxa and PUMA protein expression
(P<0.01). However, compared with the AA group, sham acupuncture
stimulation elicited no effect on Bax, Noxa and PUMA protein
expression (P>0.05).
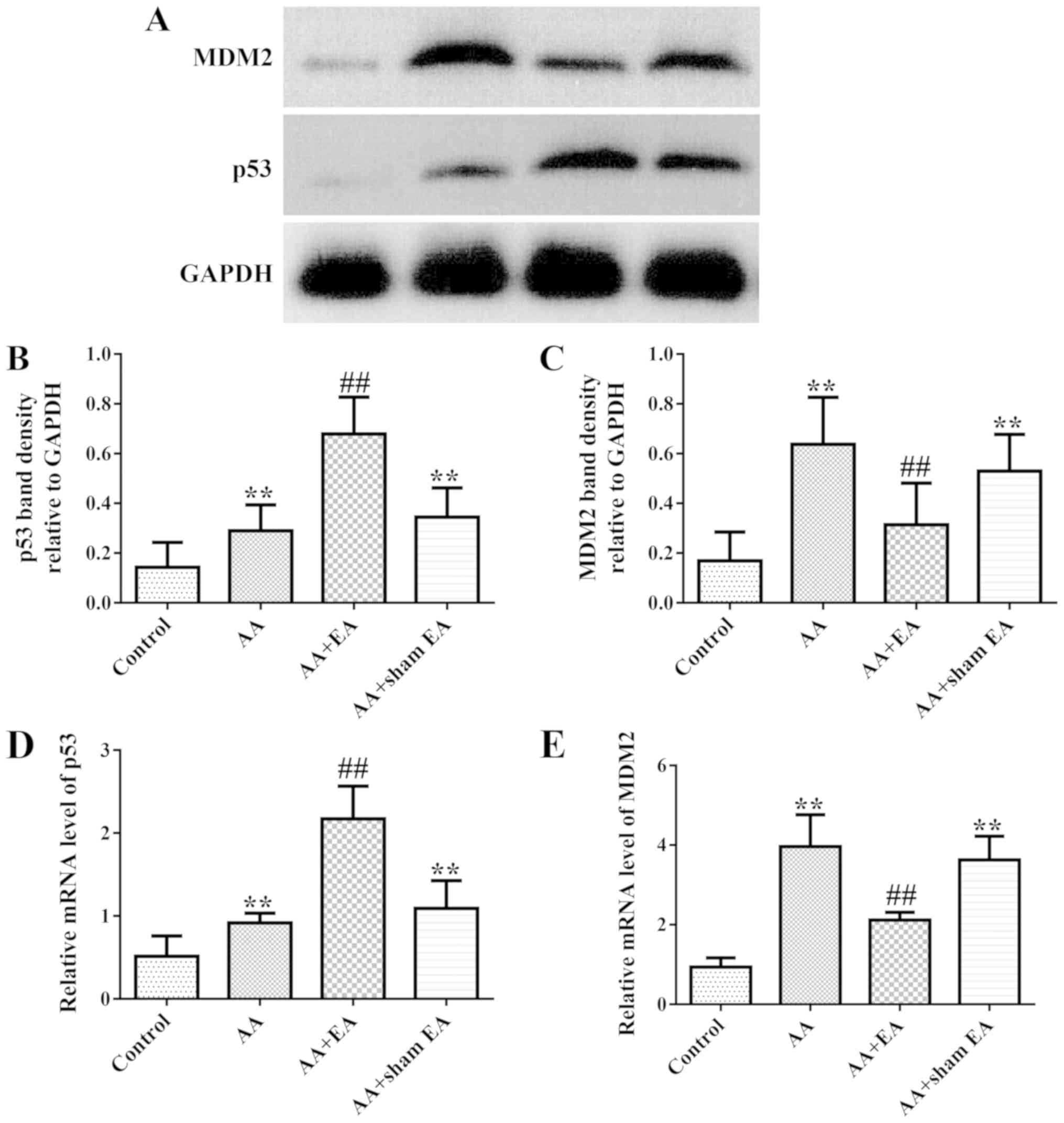
EA stimulation regulates the
expression of p53 and MDM2 in synovial tissue of AA rats
As demonstrated in Fig.
5A-C, increased levels of p53 and MDM2 protein in synovial
tissue were observed in the AA group compared with the control
group (P<0.01). Additionally, EA stimulation resulted in an
additional increase in p53 protein expression (P<0.01). However,
by contrast, EA stimulation inhibited MDM2 protein expression
(P<0.01). Consistently, sham acupuncture stimulation exerted no
effect on p53 and MDM2 protein expression compared with the AA
group (P>0.05). In addition, treatment of rats with AA led to
significantly increased gene expression levels of the p53 and MDM2
genes (Fig. 5D and E) compared
with the control group (P<0.01). However, increased and
decreased expression mRNA levels of p53 and MDM2, respectively,
were detected following EA stimulation (P<0.01). Compared with
the AA group, sham acupuncture stimulation produced no effect on
p53 and MDM2 gene expression (P>0.05).
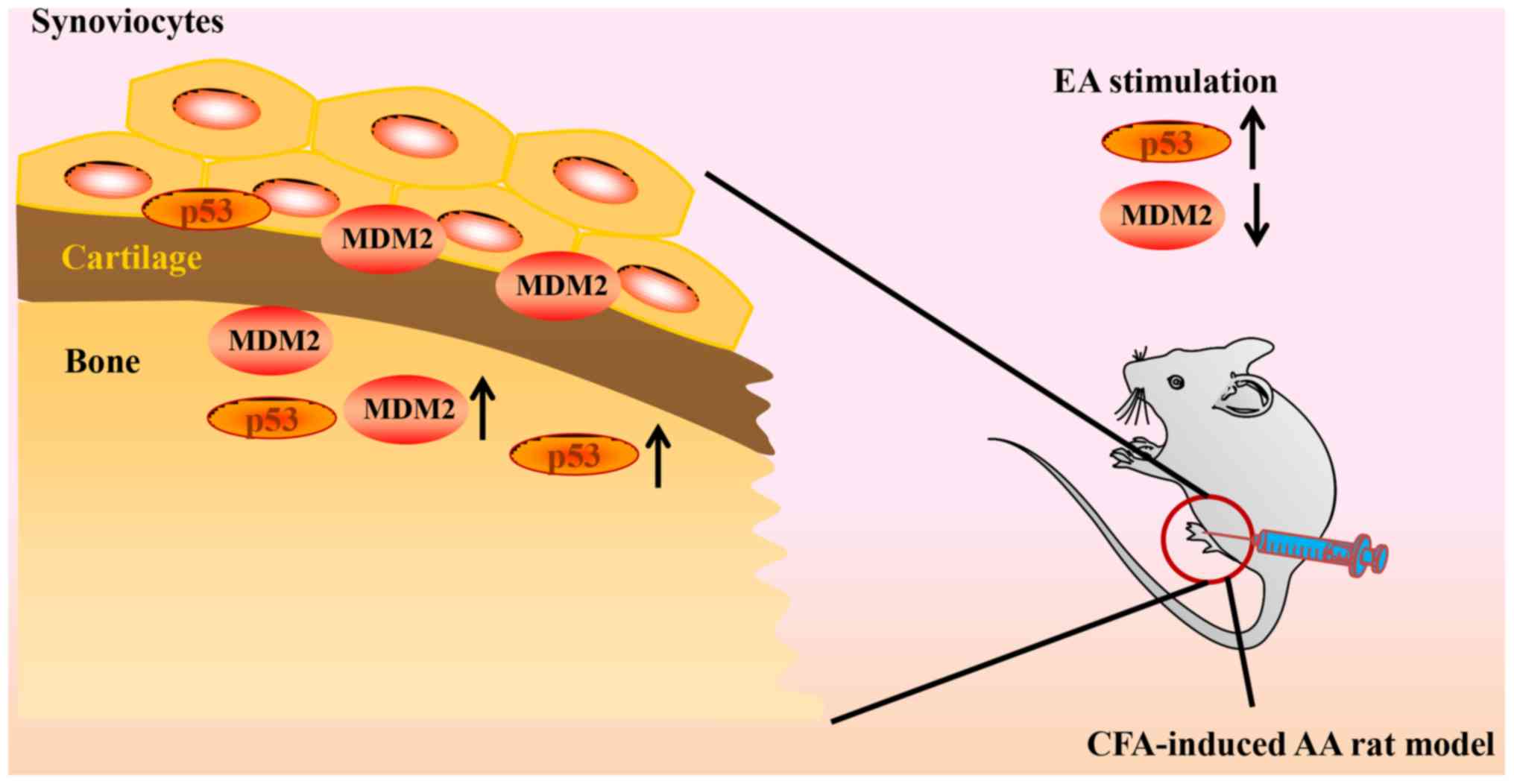
Discussion
Neovascularization and synovial cell proliferation
are two key factors in the progression of RA. Our recently
published article focused on the inhibitory effect of
electroacupuncture (EA) on synovial neovascularization in RA rats.
The results of this study suggested that EA intervention may
inhibit neovascularization by downregulating the expression of
HIF-1α and VEGF (45). The present
study aimed to investigate the effect of EA on the abnormal
proliferation of synovial cells in RA rats. The present study has
demonstrated that EA is able to effectively inhibit arthritis in AA
rats, promote synovial cell apoptosis, increase the expression
levels of p53 and its downstream factors, and decrease the
expression of MDM2, a negative regulator of p53 (Fig. 6).
Synovial cell proliferation is a hallmark pathology
of RA, which is largely due to the abnormal proliferation and
insufficient apoptosis of fibroblast-like synoviocytes of RA, which
exhibit ‘tumor-cell-like’ properties, including unlimited
proliferation, resistance to cell death, and aggressive invasion
and migration (3,7,46,47).
Previous studies have suggested that the abnormal apoptosis of
synovial cells is associated with RA, and decreased levels of
apoptosis may lead to excessive proliferation of synovial tissue,
thus promoting the deterioration of RA (5,6,48).
Previous studies have demonstrated that inducing apoptosis of
synovial cells effectively leads to an inhibition of cellular
proliferation (49,50). An additional study revealed that
acupuncture therapy may be involved in the regulation of apoptosis,
and that the underlying mechanism is predominantly governed by
regulating apoptosis-associated genes, cytokines and other
intracellular small molecules, including p53, MDM2, Bax, Noxa and
PUMA (51).
One previous study identified that fibroblast-like
synoviocytes (FLS) obtained from AA rats significantly proliferated
and exhibited increased levels of pro-inflammatory cytokines TNF-α
and IL-β compared with the control group. Concomitantly, the
apoptotic rate of FLS was significantly decreased, the expression
level of anti-apoptotic protein Bcl-2 was upregulated, and the
relative expression of Bax was decreased. A potential mechanism is
that the mitochondrial apoptotic pathway of AA-FLS is inhibited and
exhibits anti-apoptotic properties, while arthritic symptoms are
manifested (52). A second study
indicated that increasing the apoptotic rate of synovial cells in
AA rats may significantly improve the symptoms of arthritis. Its
mechanism may be associated with decreases in Bcl-2 and increases
in Bax expression levels, and increases in caspase-3 activity
(53).
In the present study, AA rats were selected as a
model of RA, which is the most commonly used animal model (54,55).
The results indicated that, compared with the control group, after
72 h, the toes and ankles of RA rats possessed different degrees of
swelling, deformity and increased arthritis index scores. The
results of the H&E staining of synovial tissue revealed
abnormal proliferation of synovial cells, connective tissue and
blood capillaries. Furthermore, a large number of inflammatory
cells had infiltrated the synovium. Concomitantly, the proportion
of TUNEL-positive cells increased markedly in the AA group. These
pathological changes in the AA rat model were consistent both with
the symptoms of patients with clinical RA and with pathological
lesions in previously described experimental animal models
(32,56).
Previous studies have suggested that p53, a tumor
suppressor factor, fulfills a crucial role in
mitochondrial-dependent apoptosis (12,13).
MDM2 is a key negative regulator of p53, affecting the
transcriptional activity and stability of p53, and thereby forms a
negative feedback pathway with p53 (15,16).
Previous studies have indicated that in wild-type cells, p53
expression is maintained at a very low level under normal
physiological conditions. However, in the state of cellular stress
including hypoxia and DNA damage, p53 is stabilized and
accumulated. In addition, enhanced transcriptional activity of p53
may increase the expression of MDM2, a downstream regulator of p53
(57–59). In accordance with previous studies
(31,60), in the present study, EA performed
on the ST36 and GB39 acupoints resulted in an inhibition of the
proliferation of synovial cells and joint inflammation in rats.
Notably, the results of the present study also indicated that EA
stimulation led to a marked increase in synovial cell apoptosis, as
evidenced by intensive TUNEL-positive staining. Furthermore,
compared with the AA group, the protein and gene expression levels
of p53 were demonstrated to increase in the synovial cells of AA
rats, whereas the protein and gene expression levels of MDM2 were
inhibited.
Previous data have suggested that increased levels
of p53-induced apoptosis occur in fibroblasts of AA rat synovial
tissue during increasing and chronic arthritis (16,21,31,61–65).
Additionally, inhibited expression of the p53 gene in synovial
fibroblasts may lead to upregulation of inflammatory factors in
CD4+ T lymphocytes of patients with RA, including
interleukin-17 and interferon-γ (66). Taken together, an accumulation of
the p53 gene product may alleviate RA via inhibiting the
inflammatory factor-induced subsequent spread of inflammatory
reactions, and inducing apoptosis in synovial tissue. Zhang et
al (16) demonstrated that the
expression of MDM2 protein was significantly increased in
fibroblast-like synovial cells of patients with RA, and that this
was positively correlated with the disease activity of RA. In
addition, inhibition of MDM2 protein expression may serve an
anti-inflammatory role by regulating the mitogen-activated protein
kinase and NF-κB signaling pathways in collagen-induced arthritic
mice (67).
Previous studies have indicated that local hypoxia
of synovial joints caused by RA may activate the p53-mediated
mitochondrial apoptotic pathway (18,19).
It has been suggested that, as a downstream effector of the Bcl-2
protein family, p53 fulfills a crucial role in
mitochondrial-dependent apoptosis, a process that results in
abnormal expression of Bax, Noxa and PUMA (12–14).
Noxa may inhibit the expression of anti-apoptotic Bcl-2 family
members, while PUMA increases the expression and conformational
changes of Bax, which in turn contributes to pore formation
(13,17,68–70).
The results of the present study indicated that compared with the
AA group, EA intervention may increase the expression of Bax, Noxa
and PUMA proteins in the downstream regulatory genes of p53.
The aforementioned results of the present study
suggested that EA was able to effectively treat RA disease by
regulating the expression of p53 and MDM2, and promoting further
expression of the proapoptotic proteins, Bax, Noxa and PUMA, data
that were consistent with previous studies (16,20,21).
Prior clinical studies have suggested that the
effects of acupuncture or EA intervention at acupoints are markedly
improved compared with those of sham acupuncture intervention at
non-acupoints near to acupoints (71–73).
In an animal experiment on the anti-inflammatory effects of EA,
pretreatment of the Hegu acupoint led to an improvement in the
survival rate of rats with lethal endotoxemia, whereas acupuncture
at non-acupoints, located on the ulna side of the metacarpus,
failed to elicit a similar effect (74). These results also suggested that
the anti-inflammatory effects of EA on acupoints is markedly
improved compared with that of non-acupoints. The results of the
present study also confirmed that sham EA stimulation exerted no
effect on the arthritis scores, pathological lesions of synovial
joints, apoptosis, or gene or protein expression of p53 and its
downstream factors including Bax, Noxa, PUMA, or MDM2, compared
with the AA group; these data were consistent with previous studies
(6,21,26).
In conclusion, the results from the present study
have demonstrated that EA stimulation of the ST36 and GB39
acupoints exhibited potential therapeutic effects on AA rats.
Furthermore, the underlying mechanisms may be associated with
increases in the expression of the p53 signaling pathway, thereby
inducing apoptosis in synovial tissue. However, further
investigations are required to determine the precise mechanisms
underlying activation of the p53 signaling pathway by EA.
Acknowledgements
Not applicable.
Funding
The current study was supported by the National
Natural Science Foundation of China (grant nos. 81704152 and
81503599) and the project of the Science and Technology Department
in Sichuan province (grant no. 2019YJ0491).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JZ designed and performed the experiments, and
evaluated the data and reviewed the manuscript. CS performed the
experiments and wrote the manuscript. YuzC, QL, HL and XL also
performed the experiments. YZ, YunC and LL analyzed the data. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Scientific
Investigation Board of the Chengdu University of Traditional
Chinese Medicine. All animal experiments followed the National
Institutes of Health Guide for the Care and Use of Laboratory
Animals.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Firestein GS: Evolving concepts of
rheumatoid arthritis. Nature. 423:356–361. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Matsui T, Nakata N, Nagai S, Nakatani A,
Takahashi M, Momose T, Ohtomo K and Koyasu S: Inflammatory
cytokines and hypoxia contribute to 18F-FDG uptake by cells
involved in pannus formation in rheumatoid arthritis. J Nucl Med.
50:920–926. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bartok B and Firestein GS: Fibroblast-like
synoviocytes: Key effector cells in rheumatoid arthritis. Immunol
Rev. 233:233–255. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ma J, Wang X, Lv T, Liu J, Ren Y, Zhang J
and Zhang Y: Effects of fhrelin on the apoptosis of rheumatoid
arthritis fibroblast-like synoviocyte MH7A cells. Biol Pharm Bull.
42:158–163. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mahoney JA and Rosen A: Apoptosis and
autoimmunity. Curr Opin Immunol. 17:583–588. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chou CT, Yang JS and Lee MR: Apoptosis in
rheumatoid arthritis-expression of Fas, Fas-L, p53, and Bcl-2 in
rheumatoid synovial tissues. J Pathol. 193:110–116. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hou YN and Guo LH: Role of synovial
fibroblasts in the pathogenesis of rheumatoid arthritis. Chin J
Cell Biol. 31:157e1622009.
|
|
8
|
Li R, Cai L, Tang WJ, Lei C, Hu CM and Yu
F: Apoptotic effect of geniposide on fibroblast-like synoviocytes
in rats with adjuvant-induced arthritis via inhibiting ERK signal
pathway in vitro. Inflflammation. 39:30–38. 2016. View Article : Google Scholar
|
|
9
|
Aupperle KR, Boyle DL, Hendrix M, Seftor
EA, Zvaifler NJ, Barbosa M and Firestein GS: Regulation of
synoviocyte proliferation, apoptosis, and invasion by the p53 tumor
suppressor gene. Am J Pathol. 152:1091–1098. 1998.PubMed/NCBI
|
|
10
|
Tak PP, Zvaifler NJ, Green DR and
Firestein GS: Rheumatoid arthritis and p53: How oxidative stress,
might alter the course of inflammatory diseases. Immunol Today.
21:78–82. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yamanishi Y, Boyle DL, Rosengren S, Green
DR, Zvaifler NJ and Firestein GS: Regional analysis of p53
mutations in rheumatoid arthritis synovium. Proc Natl Acad Sci USA.
99:10025–10030. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Doroshevskaya AY, Kondratovskii PM,
Dubikov AI and Eliseikina MG: Apoptosis regulator proteins: Basis
for the development of innovation strategies for the treatment of
rheumatoid arthritis in patients of different age. Bull Exp Biol
Med. 156:377–380. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Nakano K and Vousden KH: PUMA, a novel
proapoptotic gene, is induced by p53. Mol Cell. 7:683–694. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Villunger A, Michalak EM, Coultas L,
Müllauer F, Böck G, Ausserlechner MJ, Adams JM and Strasser A: p53-
and drug-induced apoptotic responses mediated by BH3-only proteins
puma and Noxa. Science. 302:1036–1038. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Thomasova D, Mulay SR, Bruns H and Anders
HJ: p53-Independent roles of MDM2 in NF-κB signaling: Implications
for cancer therapy, wound healing, and autoimmune diseases.
Neoplasia. 14:1097–1101. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang L, Luo J, Wen H, Zhang T, Zuo X and
Li X: MDM2 promotes rheumatoid arthritis via activation of MAPK and
NF-κB. Int Immunopharmacol. 30:69–73. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cory S and Adams JM: The Bcl2 family:
Regulators of the cellular life-or-death switch. Nat Rev Cancer.
2:647–656. 2002. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bouvard V, Zaitchouk T, Vacher M, Duthu A,
Canivet M, Choisy-Rossi C, Nieruchalski M and May E: Tissue and
cell-specific expression of the p53-target genes: Bax, Fas, MDM2
and Waf1/p21, before and following ionising irradiation in mice.
Oncogene. 19:649–660. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ohtsuka T, Ryu H, Minamishima YA, Macip S,
Sagara J, Nakayama KI, Aaronson SA and Lee SW: ASC is a Bax adaptor
and regulates the p53-Bax mitochondrial apoptosis pathway. Nat Cell
Biol. 6:121–128. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
20
|
Itoh K, Hase H, Kojima H, Saotome K,
Nishioka K and Kobata T: Central role of mitochondria and p53 in
Fas-mediated apoptosis of rheumatoid synovial fibroblasts.
Rheumatology (Oxford). 43:277–285. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tak PP, Klapwijk MS, Broersen SF, van de
Geest DA, Overbeek M and Firestein GS: Apoptosis and 53 expression
in rat adjuvant arthritis. Arthritis Res. 2:229–235. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Li Y, He N, Shen L and Liu M: Apoptotic
effect of Aralia echinocaulis extract on fibroblast-like
synoviocytes in rats with adjuvant-induced arthritis via inhibiting
the Akt/Hif-1α signaling pathway in vitro. J Pharmacol Sci.
139:340–345. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cha HS, Rosengren S, Boyle DL and
Firestein GS: PUMA regulation and proapoptotic effects in
fibroblast-like synoviocytes. Arthritis Rheum. 54:587–592. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mazumder S, Choudhary GS, Al-Harbi S and
Almasan A: Mcl-1 phosphorylation defines ABT-737 resistance that
can be overcome by increased NOXA expression in leukemic B cells.
Cancer Res. 72:3069–3079. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Idrus E, Nakashima T, Wang L, Hayashi M,
Okamoto K, Kodama T, Tanaka N, Taniguchi T and Takayanagi H: The
role of the BH3-only protein Noxa in bone homeostasis. Biochem
Biophys Res Commun. 410:620–625. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Cottier KE, Fogle EM, Fox DA and Ahmed S:
Noxa in rheumatic diseases: Present understanding and future
impact. Rheumatology (Oxford). 53:1539–1546. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
He G, Wu Z, Wang Q, et al: Therapeutic
observation of electroacupuncture plus electromagnetic therapy for
rheumatoid arthritis. Shanghai J Acupuncture Moxibustion.
33:247–250. 2014.(In Chinese).
|
|
28
|
Ouyang BS, Gao J, Che JL, Zhang Y, Li J,
Yang HZ, Hu TY, Yang M, Wu YJ and Ji LL: Effect of
Electro-acupuncture on tumor necrosis Factor-α and vascular
endothelial growth factor in peripheral blood and Joint synovia of
patients with rheumatoid arthritis. Chin J Integr Med. 17:505–509.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chou PC and Chu HY: Clinical efficacy of
acupuncture on rheumatoid arthritis and associated mechanisms: A
systemic review. Evid Based Complement Alternat Med.
2018:85969182018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
He TF, Yang WJ, Zhang SH, Zhang CY, Li LB
and Chen YF: Electroacupuncture inhibits inflammation reaction by
upregulating vasoactive intestinal peptide in rats with
adjuvant-induced arthritis. Evid Based Complement Alternat Med.
2011:1–8. 2011. View Article : Google Scholar
|
|
31
|
Zhu J, Chen XY, Li LB, Yu XT, Zhou Y, Yang
WJ, Liu Z, Zhao N, Fu C, Zhang SH and Chen YF: Electroacupuncture
attenuates collagen-induced arthritis in rats through vasoactive
intestinal peptide signalling-dependent re-establishment of the
regulatory T cell/T-helper 17 cell balance. Acupunct Med.
33:305–311. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Dong ZQ, Zhu J, Lu DZ, Chen Q and Xu YL:
Effect of electroacupuncture in ‘Zusanli’ and ‘Kunlun’ acupoints on
TLR4 signaling pathway of adjuvant arthritis rats. Am J Ther.
25:e314–e319. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Chen L, Wu Q, Yang M, Deng S, Bai L, Chen
L and Liang L: Research review of the action mechanism of
acupuncture based on cell apoptosis. Shanghai J Acupuncture
Moxibustion. 35:1143–1146. 2016.(In Chinese).
|
|
34
|
Liu J, Zhang Y, Sun J, Xu S and Zhang X:
Effect of acupuncture on the p53 Protein expression of mice with
Alzheimer's disease. Chin J Integrated Traditional Western Med.
33:1367–1371. 2013.(In Chinese).
|
|
35
|
Park JY, Choi H, Baek S, Jang J, Lee A,
Jeon S, Kim J and Park HJ: p53 signalling mediates
acupuncture-induced neuroprotection in Parkinson's disease. Biochem
Biophys Res Commun. 460:772–779. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
An N, Xu T, Sun Q and Zhang H: Research on
effect of electroacupuncture on MDM2 expression in hypoxic-ischemic
encephalopathy rat model. Chin Arch Traditional Chin Med.
34:289–292. 2016.(In Chinese).
|
|
37
|
Shi WY, Yan J, Chang XR, Lou BD, Li JX,
Huang J, Lin H, Wang C and Zhang W: Observation of
electroacupuncture intervention on cell apoptosis and Bax and Bcl-2
expression in cerebral and myocardial tissues in cerebral ischemia
rats based on ‘heart-brain correlation’ theory. Zhen Ci Yan Jiu.
44:107–112. 2019.(In Chinese). PubMed/NCBI
|
|
38
|
Zhu Y and Zeng Y: Electroacupuncture
protected pyramidal cells in hippocampal CA1 region of vascular
dementia rats by inhibiting the expression of P53 and Noxa. CNS
Neurosci Ther. 17:599–604. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Shalev M: APHIS, FDA, and NIH issue
memorandum of understanding on laboratory animal welfare. Lab Anim
(NY). 15:132006. View Article : Google Scholar
|
|
40
|
Li P, Xie G, Song S, Huang P, Wu Y, Wang
Q, Chang Y, Zhang Y, Zhou A, Liu L, et al: Clinical manifestations
and the main evaluation method on adjuvant-induced arthritis model
in rats. Chin J Immunol. 28:453–457. 2012.(In Chinese).
|
|
41
|
Ai X, Hou Y, Wang X, Wang X, Liang Y, Zhu
Z, Wang P, Zeng Y, Li X, Lai X, et al: Amelioration of dry eye
syndrome in db/db mice with diabetes mellitus by treatment with
Tibetan Medicine Formula Jikan mingmu drops. J Ethnopharmacol.
241:1119922019. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Hou Y, Wang X, Chen X, Zhang J, Ai X,
Liang Y, Yu Y, Zhang Y, Meng X, Kuang T and Hu Y: Establishment and
evaluation of a simulated high-altitude hypoxic brain injury model
in SD rats. Mol Med Rep. 19:2758–2766. 2019.PubMed/NCBI
|
|
43
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Wang X, Hou Y, Li Q, Li X, Wang W, Ai X,
Kuang T, Chen X, Zhang Y, Zhang J, et al: Rhodiola crenulata
attenuates apoptosis and mitochondrial energy metabolism disorder
in rats with hypobaric hypoxia-induced brain injury by regulating
the HIF-1α/microRNA 210/ISCU1/2(COX10) signaling pathway. J
Ethnopharmacol. 241:1118012019. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Zhu J, Su CG, Chen YZ, Hao XY and Jiang
JZ: Electroacupuncture on ST36 and GB39 acupoints inhibits synovial
angiogenesis via downregulating HIF-1α/VEGF expression in a rat
model of adjuvant arthritis. Evid Based Complement Alternat Med.
2019:57419312019. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Müller-Ladner U and Pap T: Pathogenesis of
RA: More than just immune cells. Z Rheumatol. 64:396–401. 2005.(In
German). View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Bottini N and Firestein GS: Duality of
fibroblast-like synoviocytes in RA: Passive responders and
imprinted aggressors. Nat Rev Rheumatol. 9:24–33. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Baier A, Meineckel I, Gay S and Pap T:
Apoptosis in rheumatoid arthritis. Curr Opin Rheumatol. 15:274–279.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Peng C, Luo L, Hu L, Wu Z, Cai R, Hao F,
Hu W and Hong J: Study on the effect of moxibustion in treating
rhreumatoid arthritis rats and its mechanism. J Acupuncture Tuina
Sci. 10:336–341. 2012.(In Chinese). View Article : Google Scholar
|
|
50
|
Zhang C, Cai R and Tang Z: Influences of
moxibustion on inflammatory factors and synoviocytes in rats with
rheumatoid arthritis. J Beijing Univ Traditional Chin Med.
37:190–194. 2014.(In Chinese).
|
|
51
|
Chen L, Wu QF, Yang MX, et al: Research
review of the action mechanism of acupuncture based on cell
apoptosis. Shanghai J Acupuncture Moxibustion. 35:1143–1146.
2016.(In Chinese).
|
|
52
|
Gao W, Deng Q, Bai S and Tong L:
Establishment and characteristic analysis of fibroblast-like
synoviocytes in rats with adjuvant arthritis. Chin Pharmacol
Bulletin. 12:1693–1698. 2015.
|
|
53
|
Meng Q, Du X, Wang H, Gu H, Zhan J and
Zhou Z: Astragalus polysaccharides inhibits cell growth and
pro-inflammatory response in IL-1β-stimulated fibroblast-like
synoviocytes by enhancement of autophagy via PI3K/AKT/mTOR
inhibition. Apoptosis. 22:1138–1146. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Dekkers JS, Schoones JW, Huizinga TW, Toes
RE and van der Helm-van Mil AH: Possibilities for preventive
treatment in rheumatoid arthritis? Lessons from experimental animal
models of arthritis: A systematic literature review and
meta-analysis. Ann Rheum Dis. 76:458–467. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Taşçi Bozbaş G, Yilmaz M, Paşaoğlu E,
Gürer G, Ivgin R and Demirci B: Effect of ozone in Freund's
complete adjuvant-induced arthritis. Arch Rheumatol. 33:137–142.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Smolen JS, Aletaha D and McInnes IB:
Rheumatoid arthritis. Lancet. 388:2023–2038. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Ren XY, Liu QX and Wang HY: p53 and cell
death. Chin J Bioch Mol Biol. 34:588–594. 2018.
|
|
58
|
Zhen D, Zhao F and Song H: Progress of
polysaccharides regulating p53 signal network. Chin J Cell Biol.
39:1234–1242. 2017.
|
|
59
|
Peng L, Liu J, Xie X, et al: The research
progress of p53 regulating the balance of tumor and aging. Chem
Life. 37:515–520. 2017.(In Chinese).
|
|
60
|
Zhu J, Chen X, Li L, Zhou Y, Bing X and
Chen Y: Experimental study on vasoactive intestinal peptide
mediated by electroacupuncture for the treatment of
collagen-induced arthritis in rats. Shanghai J Traditional Chin
Med. 49:72–76. 2015.(In Chinese).
|
|
61
|
Lassus P, Bertrand C, Zugasti O, Chambon
JP, Soussi T, Mathieu-Mahul D and Hibner U: Anti-apoptotic activity
of p53 maps to the COOH-terminal domain and is retained in a highly
oncogenic natural mutant. Oncogene. 18:4699–4709. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Nakajima T, Aono H, Hasunuma T, Yamamoto
K, Shirai T, Hirohata K and Nishioka K: Apoptosis and functional
Fas antigen in rheumatoid arthritis synoviocytes. Arthritis Rheum.
38:485–491. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Firestein GS, Yeo M and Zvaifler NJ:
Apoptosis in rheumatoid arthritis synovium. J Clin Invest.
96:1631–1638. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Kobayashi T, Okamoto K, Kobata T, Hasunuma
T and Nishioka K: Apomodulation as a novel therapeutic concept for
the regulation of apoptosis in rheumatoid synoviocytes. Curr Opin
Rheumatol. 11:188–193. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Yao Q, Wang S, Glorioso JC, Evans CH,
Robbins PD, Ghivizzani SC and Oligino TJ: Gene transfer of p53 to
arthritic joints stimulates synovial apoptosis and inhibits
inflammation. Mol Ther. 3:901–910. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Tang B, You X, Zhao L, Zhang T, Zhang L,
Zhang X and Tang F: The effect of p53 expression in fibroblast-like
synoviocytes on CD4+ T lymphocytes in patients with
rheumatoid arthritis. Chin J Rheumatol. 13:587–591. 2009.(In
Chinese).
|
|
67
|
Vassilev LT, Vu BT, Graves B, Carvajal D,
Podlaski F, Filipovic Z, Kong N, Kammlott U, Lukacs C, Klein C, et
al: In vivo activation of the p53 pathway by small-molecule
antagonists of MDM2. Science. 303:844–848. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Yang E, Zha J, Jockel J, Boise LH,
Thompson CB and Korsmeyer SJ: Bad, a heterodimeric partner for
Bcl-XL and Bcl-2, displaces Bax and promotes cell death. Cell.
80:285–291. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Oda E, Ohki R, Murasawa H, Nemoto J,
Shibue T, Yamashita T, Tokino T, Taniguchi T and Tanaka N: Noxa, a
BH3-only member of the Bcl-2 family and candidate mediator of
p53induced apoptosis. Science. 288:1053–1058. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Liu FT, Newland AC and Jia L: Bax
conformational change is a crucial step for PUMA-mediated apoptosis
in human leukemia. Biochem Biophys Res Commun. 310:956–962. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Seca S, Patrício M, Kirch S, Franconi G,
Cabrita AS and Greten HJ: Effectiveness of acupuncture on pain,
functional disability, and quality of life in rheumatoid arthritis
of the hand: Results of a double-blind randomized clinical trial. J
Altern Complement Med. 25:86–97. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Liu Z, Liu Y, Xu H, He L, Chen Y, Fu L, Li
N, Lu Y, Su T, Sun J, et al: Effect of electroacupuncture on
urinary leakage among women with stress urinary incontinence: A
randomized clinical trial. JAMA. 317:2493–2501. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Liu Z, Yan S, Wu J, He L, Li N, Dong G,
Fang J, Fu W, Fu L, Sun J, et al: Acupuncture for chronic severe
functional constipation: A randomized trial. Ann Intern Med.
165:761–769. 2016.PubMed/NCBI
|
|
74
|
Song JG, Li HH, Cao YF, Lv X, Zhang P, Li
YS, Zheng YJ, Li Q, Yin PH, Song SL, et al: Electroacupuncture
improves survival in rats with lethal endotoxemia via the autonomic
nervous system. Anesthesiology. 116:406–414. 2012. View Article : Google Scholar : PubMed/NCBI
|