Introduction
Preterm birth (PTB) refers to delivery at <37
weeks of gestation, it is a global issue and a leading cause of
infant morbidity and mortality worldwide (1). Spontaneous preterm labor is a
syndrome involving a number of pathophysiological processes that is
primarily caused by intra-amniotic infection/inflammation (2). Compared with the normal population,
pregnant women have increased susceptibility to pathogens in the
environment, thus increasing the risk of adverse pregnancy outcomes
(3). Inflammation, or more
specifically inflammatory activation caused by infection or other
factors, plays key roles in uterine activation and delivery
(4), including promoting
inflammatory factor responses and destroying the cervical
epithelial barrier, thus inducing cervical remodeling (5). Cervical remodeling is a natural,
continually occurring process over the course of gestation, but the
mechanism of its occurrence and progression remains largely
unknown.
The production of inflammatory cytokines caused by
inflammatory activation is closely related to the maintenance of
uterine quiescence and the induction of uterine activation during
pregnancy (6,7). The increased production of
proinflammatory cytokines is related to uterine activation and the
occurrence of PTB, whereas anti-inflammatory cytokines play an
essential role in uterine quiescence during gestation (8,9).
High-mobility group box 1 protein (HMGB1) is a member of the highly
conserved non-histone DNA binding protein family, and a potent
mediator of inflammation in multiple pathological processes, such
as endotoxemia and sepsis induced by bacterial infection,
gastrointestinal inflammation, pancreatitis, ischemia-reperfusion
injury and transplantation, and intra-amniotic
inflammation-determined preterm birth (10,11).
HMGB1 is secreted by innate immune cells in response to pathogens
and is released by injured or dying cells, thus it plays a central
role in the pathogenesis of both sterile and infectious
inflammation (12). It has been
reported that HMGB1 levels are significantly increased in PTB
(11,13–15).
Toll-like receptors (TLRs) are a family of evolutionarily conserved
innate immune receptors that act as sensors of invading pathogens
and link innate and acquired immunity (11,16).
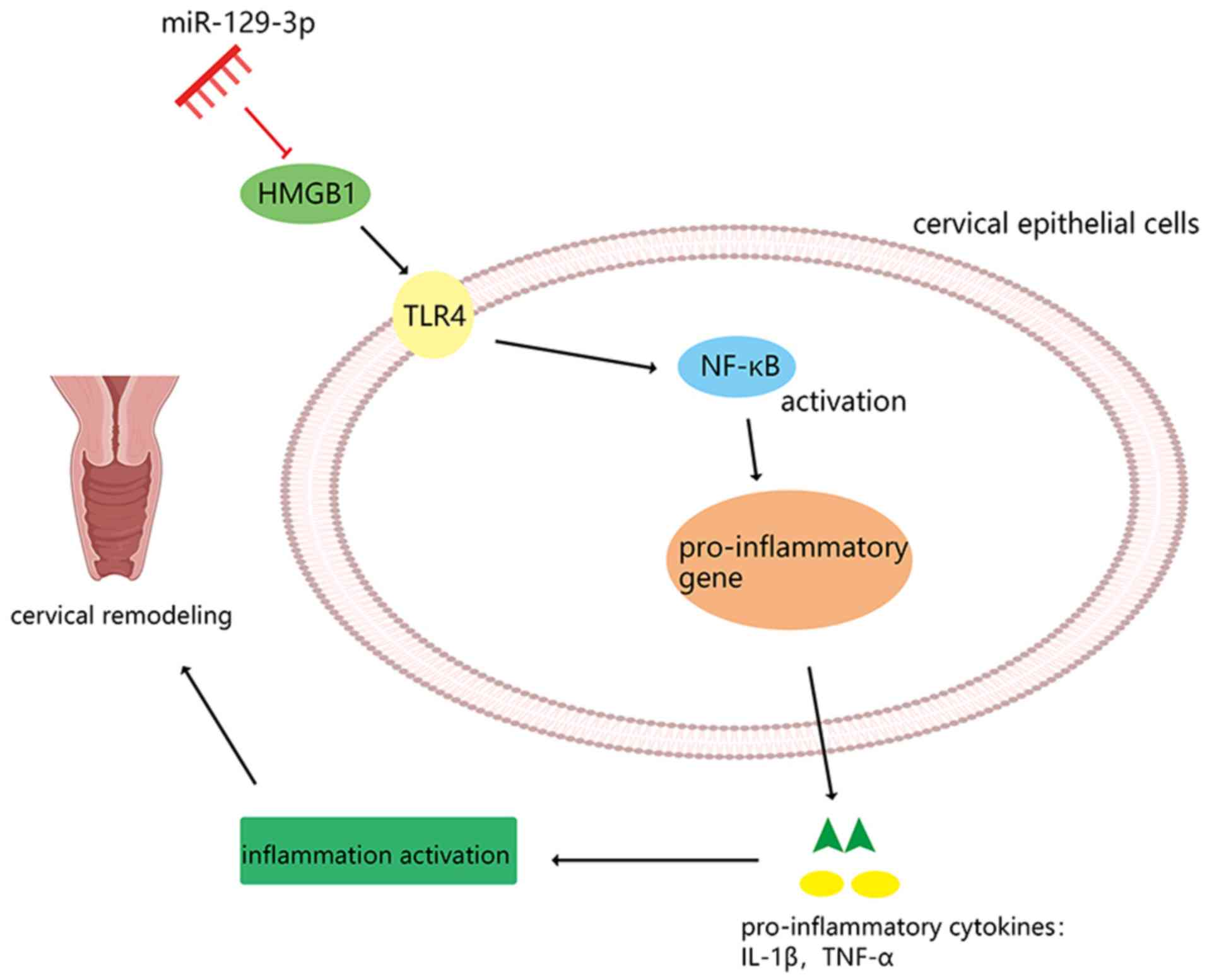
HMGB1 is a ligand that promotes TLR4 activity. TLR4 is the primary
receptor of endogenous extracellular HMGB1, which can activate
NF-κB and mediate its nuclear translocation, thus upregulating the
expression of cytokines and other inflammatory mediators (17–20).
A previous study has revealed that the TLR4/NF-кB signaling pathway
is involved in advancing gestational age, exposure to
chorioamnionitis and preterm premature rupture of membranes (PPROM)
(21). However, the regulatory
mechanism of HMGB1 and TLR4/NF-κB signaling in inflammatory
activation in PTB remains unknown.
MicroRNAs (miRNAs/miRs) are a class of small
non-coding single-stranded RNAs that are 18–22 nucleotides in
length. They negatively regulate gene expression via degradation or
posttranscriptional regulation of target mRNAs. Numerous studies
have suggested that miRNAs are involved in PTB (22–25).
Previous studies have reported that miR-199a and miR-214 are
significantly decreased in the laboring myometrium of pregnant mice
and humans, and in an inflammatory mouse model of preterm labor
(26), and they are important
regulators of myometrial contractility. It has also been reported
that miR-199a-3p plays a crucial role in regulating the process of
inflammation in multiple diseases, including cystic fibrosis
airways (27) and acute lung
injury (28). However, it is
unclear whether miR-199a-3p is involved in the regulation of
uterine activation and quiescence by regulating inflammatory
activation.
Based on previous studies, it was hypothesized that
miR-199a-3p may play an important role in PTB-related inflammatory
activation. Notably, it has been suggested that miR-199a-3p may
regulate HMGB1 expression by targeting the HMGB1 mRNA 3untranslated
region (UTR) through a bioinformatic prediction (http://www.targetscan.org/vert_72/). The present
study aimed to investigate the mechanism by which miR-199a-3p
regulates the TLR4/NF-κB-mediated inflammatory response by
targeting HMGB1 in preterm delivery. This study will provide more
evidence related to the pathogenesis of inflammatory-related PTB
and provide new insights into the targets and strategies for PTB
prevention.
Materials and methods
Human tissue preparations
All human studies were approved by the Hospital
Ethical Committee of The First Peoples Hospital of Yunnan Province
and Affiliated Hospital of Kunming University of Science and
Technology located in Kunming, China (approval no: 2016LH087), and
written informed consent was obtained from each patient before
surgery. A total of 182 females participated in this study, these
patients had been admitted to The First Peoples Hospital of Yunnan
Province between January and September 2019. The details and
baseline characteristics of the participants are shown in Table S1. Of these 182 participants, 52
were in the PTB group, 60 were in the PPROM group and 70 were in
the full-term birth (TB) group. The peripheral blood and cervical
epithelial tissues were collected from participants within 30 min
of delivery, immediately frozen and stored at −80°C for subsequent
study.
Cell culture and transfection
The ectocervical (Ecto) cell line Ect1/E6E7 (cat.
no. CRL-2614) and endocervical (Endo) cell line End1/E6E7 (cat. no.
CRL-2615) were purchased from American Type Culture Collection
(ATCC) and cultured in keratinocyte serum medium (KSM; Gibco;
Thermo Fisher Scientific, Inc.) supplemented with 0.1 ng/ml
epidermal growth factor, 50 µg/ml bovine pituitary extract
(ScienCell Research Laboratories, Inc.) and 0.1%
penicillin-streptomycin solution at 37°C in a humidified incubator
with 5% CO2. 293T cells were purchased from ATCC and
cultured in Dulbeccos modified Eagles medium (DMEM; Gibco; Thermo
Fisher Scientific, Inc.) supplemented with 10% fetal bovine serum
(FBS, Gibco; Thermo Fisher Scientific, Inc.) and 0.1%
penicillin-streptomycin solution at 37°C in a 5% CO2
humidified incubator.
For the transfection experiment, Ecto and Endo cells
were seeded into 6-well plates (Coning, Inc.) at 1.5×105
cells/well for 24 h. Then, cells were transfected with 100 nM
miR-199a-3p mimics (5-ACAGUAGUCUGCACAUUGGUUA-3) and negative miRNA
mimics (5-UAA CCAAUGUGCAGACUACUGU-3) using
Lipofectamine® 2000 (Invitrogen; Thermo Fisher
Scientific, Inc.), according to the manufacturers protocols. The
transfection efficiency was verified by reverse
transcription-quantitative (RT-q)PCR 4 h later. miR-199a-3p mimics
and negative control mimics were obtained from Shanghai GenePharma
Co., Ltd.
For HMGB1 and TLR4 overexpression experiments, 293T
cells were seeded into 24-well plates (Coning, Inc.) at
1×105 cells/well for 24 h. Clone vectors of HMGB1 and
TLR4 were purchased from Shanghai GenePharma Co., Ltd.
Subsequently, the linearized DNA, shuttle vector and pacAd vector
were co-transfected into 293T cells using Lipofectamine 2000
(Invitrogen; Thermo Fisher Scientific, Inc.). Viral lysates were
harvested and purified before infecting Ecto and Endo cells. One
day before the experiment, Ecto and Endo cells were seeded into
6-well plates (Coning, Inc.) at 1.5×105 cells/well.
Then, 50 nM adenoviruses were added to the medium to infect the
Ecto and Endo cells, the transfection efficiency was verified by
western blotting 24 h later.
LPS-induced inflammation in Ecto and
Endo cells
Ecto and Endo cells were seeded into 24-well plates
at a concentration of 1×105 cells/well for 24 h in KSM
supplemented with 0.1 ng/ml epidermal growth factor, 50 µg/ml
bovine pituitary extract (ScienCell Research Laboratories, Inc.)
and 0.1% penicillin-streptomycin solution at 37°C with 5%
CO2. Then, the medium was changed to keratinocyte
serum-free medium supplemented with 0.1% penicillin-streptomycin
solution for 24 h. Then, the cells were treated with 25 µg/ml LPS
(Sigma-Aldrich; Merck KGaA), and the control group was treated with
an equivalent of saline. The cell culture supernatant was collected
at 6 and 24 h, and the cytokines were assayed at both time points
using an enzyme-linked immunosorbent assay (ELISA) kit.
RT-qPCR
Total RNA was extracted from cervical tissues and
cells using TRIzol reagent (Invitrogen; Thermo Fisher Scientific,
Inc.) and then reverse transcribed using a PrimeScript RT regent
kit (Takara Biotechnology Co., Ltd.), following the manufacturers
instructions (with the temperature protocol of 37°C for 15 min, and
85°C for 5 sec). RT-qPCR was carried out using SYBR Real-Time PCR
Master Mix (Takara Biotechnology Co., Ltd.) on an ABI 7500
Real-Time PCR System (Applied Biosystems; Thermo Fisher Scientific,
Inc.). The thermocycling conditions were as follows: Initial
denaturation at 95°C for 10 sec, followed by 40 cycles of 95°C for
10 sec and 60°C for 30 sec. The mRNA level was normalized to GAPDH
and miRNA level was normalized to U6. The relative levels were
calculated by the 2−ΔΔCq method (29). The primer sequences used were as
follows: Human GAPDH, forward: 5-TTCCGTGTTCCTACCC-3 and reverse:
5-GTCGCAGGAGACAACC-3; human U6, forward:
5-CTCGCTTCGGCAGCACATATACT-3 and reverse:
5-ACGCTTCACGAATTTGCGTGTC-3; human HMGB1, forward:
5-CAAACCTGCCGGGAGCAGCA-3 and reverse:
5-TCTTTCATAACGAGCCTTGTCAGCC-3; human TLR4, forward:
5-TATCCAGAGCCGTTGGTGTA-3 and reverse: 5-CCCACTCGAGGTAGGTGTTT-3;
human interleukin (IL)-1β, forward: 5-TGAGCTCGCCAGTGAAATGA-3 and
reverse: 5-AACACGCAGGACAGGTACAG-3; and human tumor necrosis factor
(TNF)-α, forward: 5-CCAGACCCTCACACTCAGATCA-3 and reverse:
5-CACTTGGTGGTTTGCTACGAC-3. In addition, miRNA qPCR was carried out
using a TaqMan™ Reverse Transcription kit (Applied Biosystems;
Thermo Fisher Scientific, Inc.) and a TaqMan Universal PCR Master
Mix (Applied Biosystems; Thermo Fisher Scientific, Inc.).
Luciferase reporter assays
The binding sites between miR-199a-3p and HMGB1 was
predicted with TargetScan (http://www.targetscan.org/vert_72/). Luciferase
vectors containing the 3UTR of human HMGB1 with the miR-199a-3p
binding sites and mutant miR-199a-3p binding sites, were purchased
from Shanghai GenePharma Co., Ltd. A total of 1×104 293T
cells were cultured for 24 h and then transfected with the plasmid
(wt-luc-HMGB1 or mut-luc-HMGB1) by Lipofectamine™ 2000 Transfection
Reagent (Invitrogen; Thermo Fisher Scientific, Inc.). The pRL-CMV
vector containing the CMV enhancer and early promoter elements of
Renilla luciferase (Promega Corporation) was used as an internal
control. The luciferase activity was measured using the
Dual-Luciferase® Reporter Assay System (Promega
Corporation) 24 h post transfection.
Peripheral blood specimens
Peripheral blood specimens were collected, incubated
for 15 min at room temperature and then centrifuged at 1,000 × g at
4°C for 15 min. The serum samples were stored at −20°C.
ELISA
The concentration of cytokines IL-1β (cat. no.
DLB50), IL-6 (cat. no. D6050) and TNF-α (cat. no. DTA00D; all
purchased from R&D Systems, Inc.) in serum from participants
were measured using ELISA kits following the manufacturers
instructions.
Western blotting
The Ecto and Endo cells were harvested and lysed in
RIPA buffer with protease inhibitors (Invitrogen; Thermo Fisher
Scientific, Inc.). Protein concentrations were determined using the
Pierce BCA assay (Invitrogen; Thermo Fisher Scientific, Inc.),
according to the manufacturers protocols. 40 ng of proteins were
loaded on a 12.5% SDS-PAGE and subsequently transferred to PVDF
membranes. The membranes were blocked with 5% non-fat milk for 1 h
at room temperature. Then, the cells were incubated with primary
antibodies at 4°C overnight. Expression levels of the proteins of
interest were analyzed using primary antibodies against inhibitor
of NF-κB (IκB; 1:1,000; cat. no. ab32518; Abcam), IκB kinase (IKK;
1:1,000; cat. no. ab32041; Abcam), HMGB1 (1:12,000; cat. no.
ab79823; Abcam), TLR4 (1:100; cat. no. ab22048; Abcam), cAMP
response element-binding protein (CREB; 1:500; cat. no. ab32515;
Abcam), phosphorylated (p)-CREB (1:5,000; cat. no. ab32096; Abcam),
p65 (1:1,000; cat. no. ab16502; Abcam) and p-p65 (1:16,000; cat.
no. ab6503; Abcam). Membranes were rinsed three times with 1X
Tris-buffered saline with 0.5% Tween-20 (TBST), and then incubated
with anti-rabbit IgG (1:2,000; cat. no. ab205718; Abcam)
horseradish peroxidase-conjugated secondary antibody for 1 h at
room temperature. Membranes were rinsed three times with TBST and
visualized using an ECL kit (Bio-Rad Laboratories, Inc.). The
protein bands were quantified using ImageJ software (v1.52a;
National Institutes of Health), and GAPDH was used as a loading
control. Each experiment was performed in triplicate.
Mouse model of LPS-induced preterm
labor
A total of 25 eight-week-old timed pregnant
Institute of Cancer Research (ICR) mice (28–32 g) were obtained
from Guangdong Medical Laboratory Animal Center. The mice were
housed individually with a 12-h light/dark cycle at 22°C with 50%
humidity and received ad libitum food and water. All experiments
were approved by the Animal Ethics Committee of the hospital. The
LPS-induced preterm mouse model was described in a previous study
(30). Briefly, pregnant ICR mice
(15.5 days post conception) were anesthetized by intraperitoneal
injection with 1% sodium pentobarbital (50 mg/kg) before performing
laparotomy to expose the uterus. LPS (Sigma-Aldrich; Merck KGaA) at
a dose of 1.5 µg in 50 µl or an equal volume of sterile PBS was
injected into each amniotic sac. The uterus was then carefully
reinserted into the abdominal cavity, the abdominal muscle wall and
skin were sutured, and the mouse was allowed to recuperate. The
LPS-induced mice (n=5) were sacrificed upon the PTB of one pup, and
the control mice (n=5) were sacrificed immediately afterwards.
Then, to determine the miR-199a-3p and HMGB1 in cervical epithelial
inflammation in vivo, miR-199a-3p mimics and pcDNA-HMGB1
were transfected into LPS-induced PTB mice together or alone [the
mice were divided into 3 groups: LPS only (n=5); miR-199a-3p mimics
only (n=5); and miR-199a-3p mimics and pcDNA-HMGB1 (n=5)], and the
transfection efficiency was verified by RT-qPCR or western
blotting. Subsequently, the expression of HMGB1, TLR4, p65, p-p65
and the proinflammatory cytokines, IL-1β and TNF-α, were
measured.
Statistical analysis
All data are presented as the mean ± SEM.
Differences between two or multiple groups were evaluated using a
two-tailed Students t-test or one-way ANOVA followed by Bonferroni
post hoc test. The baseline characteristics of participants were
tested by Kruskal-Wallis test and Fishers Exact test. Statistical
analyses were performed using SPSS v20.0 (IBM Corp.) and GraphPad
Prism 7.0 software (GraphPad Software, Inc.). P<0.05 was
considered to indicate a statistically significant difference.
Results
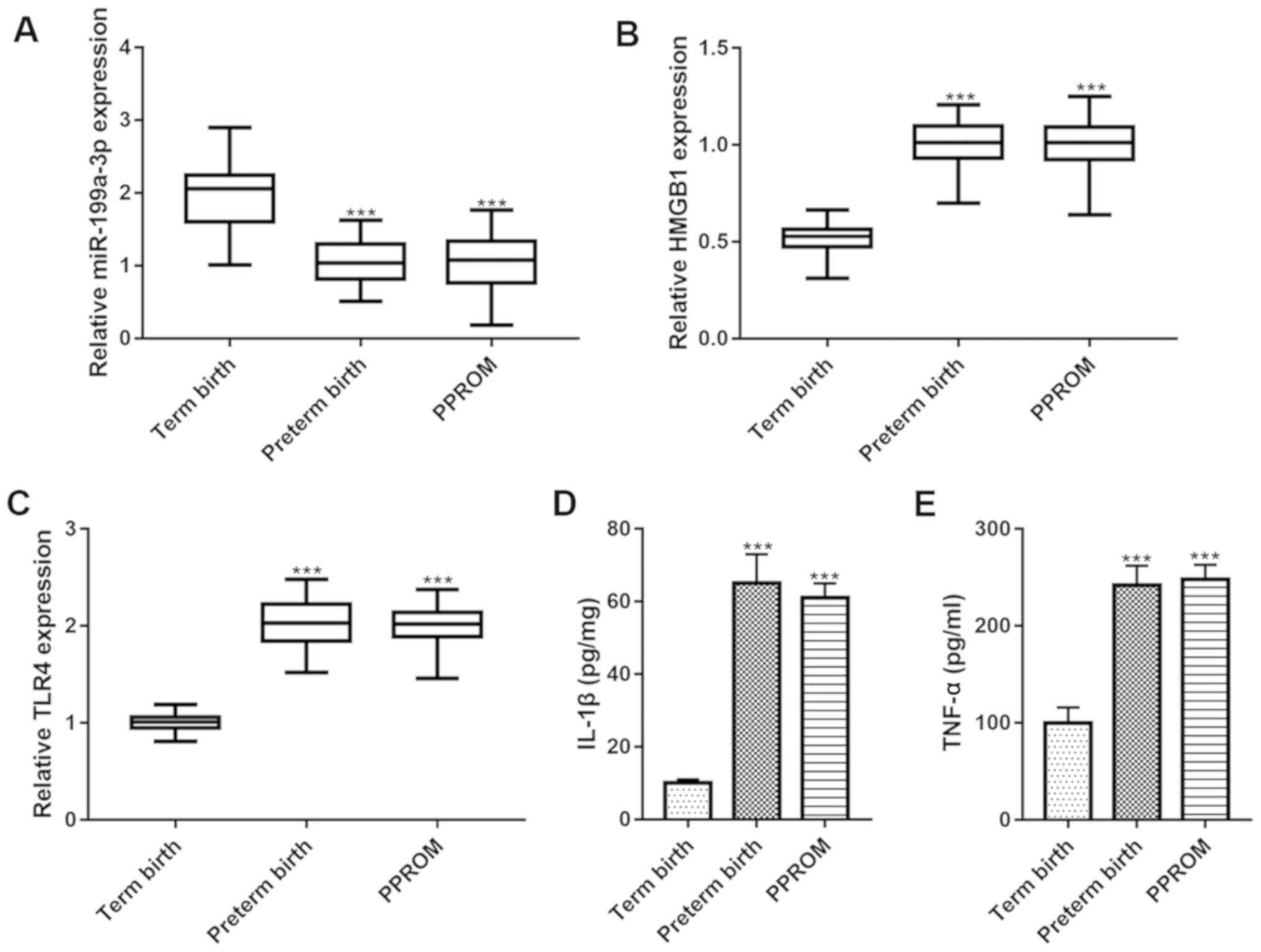
Expression of miR-199a-3p and HMGB1 in
the PTB group
A total of 182 females participated in the present
study, which included 52 patients in the PTB group, 60 in the PPROM
group and 70 in the TB group. mRNA expression of miR-199a-3p and
HMGB1 in the cervical tissues of patients in the PTB, PPROM and TB
groups were determined by RT-qPCR. The results showed that the
expression of miR-199a-3p was significantly decreased in the
cervical tissue of patients in the PTB and PPROM groups compared
with patients in the TB group (Fig.
1A). In contrast, the mRNA levels of HMGB1 and TLR4 were
significantly increased in patients in the PTB and PPROM groups
compared with in the TB group (Fig. 1B
and C). Furthermore, serum levels of proinflammatory cytokines
(IL-1β and TNF-α) were significantly increased in the PTB and PPROM
groups compared with in the TB group (Fig. 1D and E). In addition, there were no
significant differences between the PTB and PPROM groups. These
results suggested that there is a significant inflammatory response
in PTB and PPROM conditions, which may be related to the abnormal
expression of miR-129-3p, HMGB1 and TLR4.
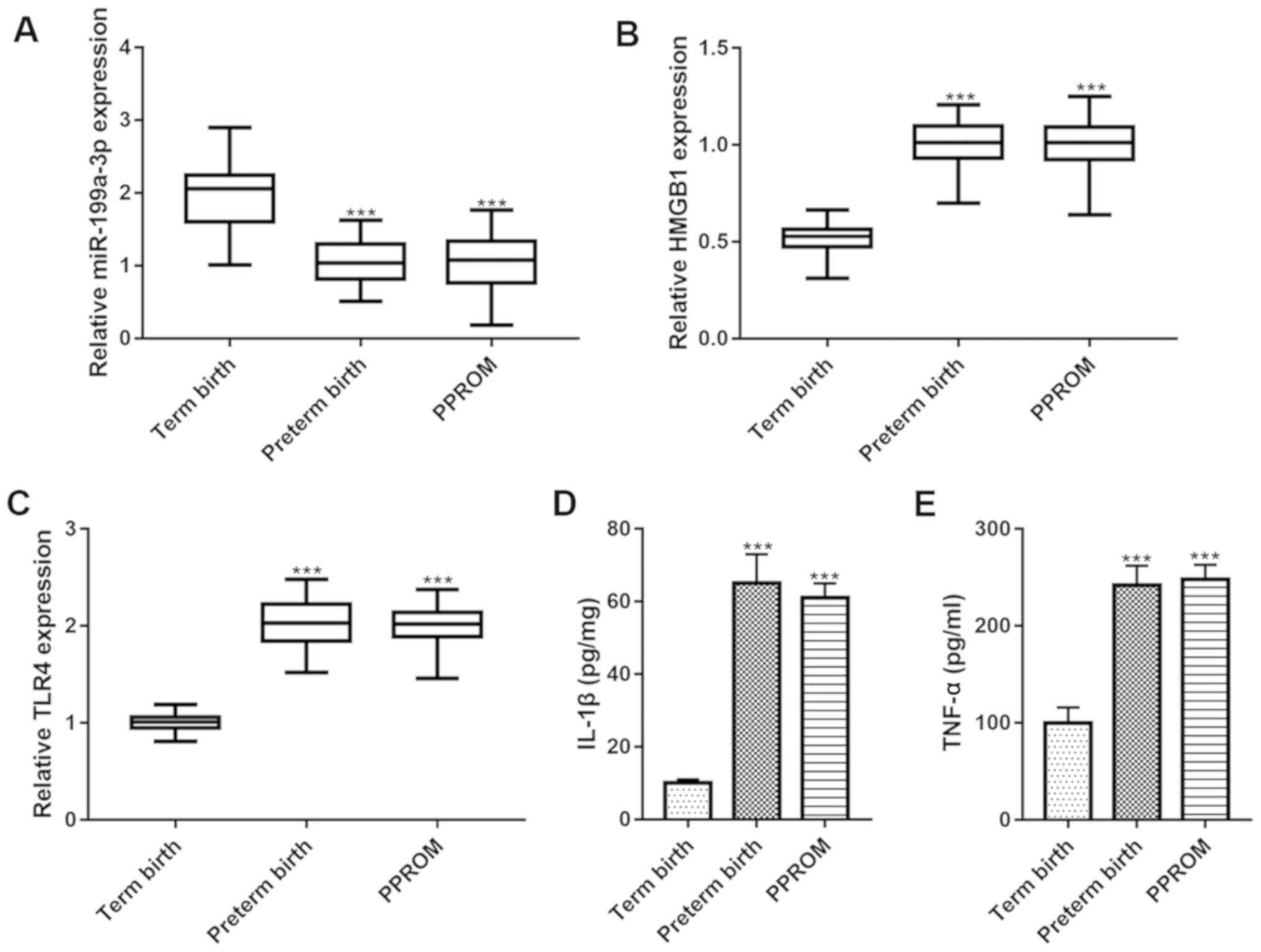 | Figure 1.Expression of miR-199a-3p and HMGB1
in cervical tissue samples from patients. The expression of (A)
miR-199a-3p, (B) HMGB1 mRNA and (C) TLR4 mRNA in cervical tissue
samples from patients in the term birth, preterm birth and PPROM
groups measured by reverse transcription-quantitative PCR. The
serum levels of (D) IL-1β and (E) TNF-α in cervical tissue samples
from patients in the term birth, preterm birth and PPROM groups,
measured using an ELISA assay. Data represents the mean ± SEM.
***P<0.001 vs. term birth. miR, microRNA; HMGB1, high-mobility
group box 1 protein; TLR4, toll-like receptor 4; PPROM, preterm
premature rupture of membranes; IL, interleukin; TNF, tumor
necrosis factor. |
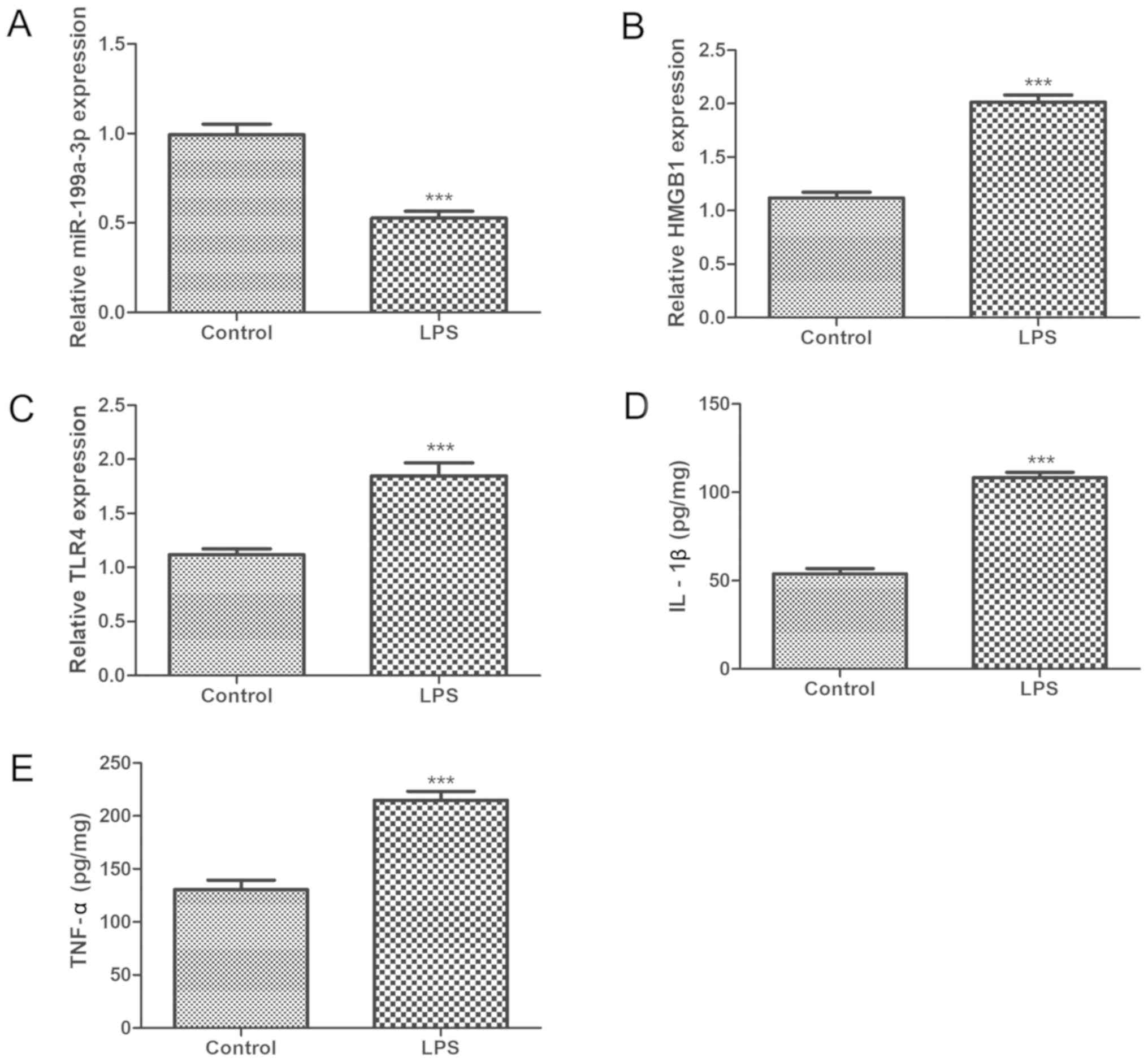
Expression of miR-199a-3p and HMGB1 in
an LPS-induced preterm mouse model
The expression levels of miR-199a-3p, HMGB1 and TLR4
in cervical tissue from PTB mice and the level of inflammation in
PTB mice were found to be similar to those observed in patients in
the PTB group. As shown in Fig. 2,
the LPS-induced preterm mouse model resulted in significant
downregulation of miR-199a-3p and upregulation of the mRNA
expression levels of HMGB1 and TLR4 compared with those in control
mice (Fig. 2A-C). Furthermore,
serum IL-1β and TNF-α showed significant increases in LPS-induced
PTB mice (Fig. 2D and E). These
results indicated that LPS-induced inflammatory preterm delivery in
pregnant mice might be achieved by regulating the expression of
miR-199a-3p, HMGB1 and TLR4.
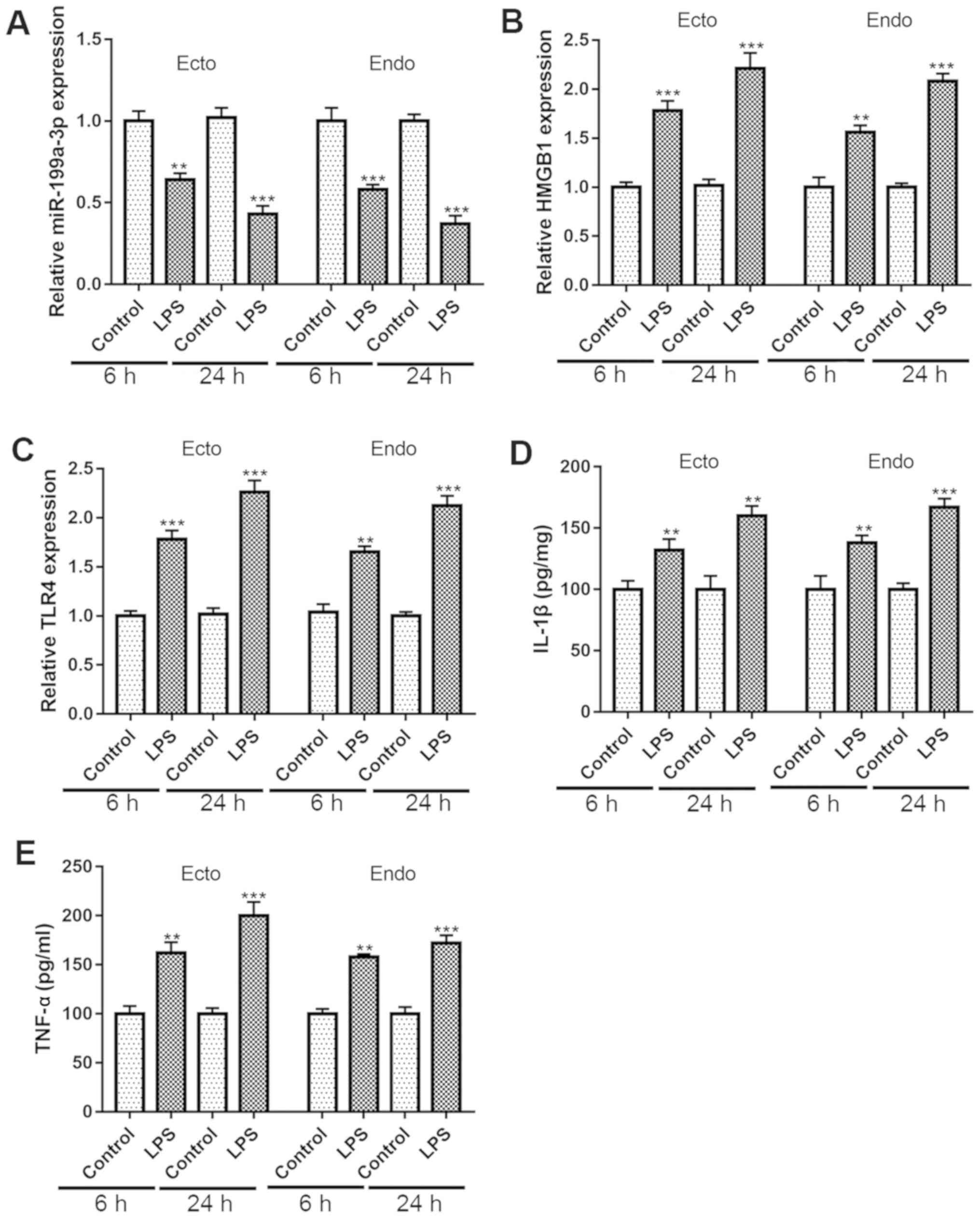
Expression of miR-199a-3p and HMGB1 in
LPS-induced cervical epithelial cells
Ecto and Endo cells were exposed to LPS, and the
expression of genes was measured at 6 and 24 h after exposure in
both cell lines. The results showed that the expression of
miR-199a-3p significantly decreased in both cell lines in a
time-dependent manner (Fig. 3A).
Similar to patients in the PTB group and LPS-induced preterm mice,
the mRNA expression of HMGB1 and TLR4 were significantly increased
in Ecto and Endo cells in a time-dependent manner (Fig. 3B and C). In addition, the L-1β and
TNF-α levels were also significantly increased in Ecto and Endo
cells in a time--dependent manner (Fig. 3D and E). These data suggested that
miR-199a-3p and HMGB1 play important roles in LPS-induced
inflammation of cervical epithelial cells in vitro.
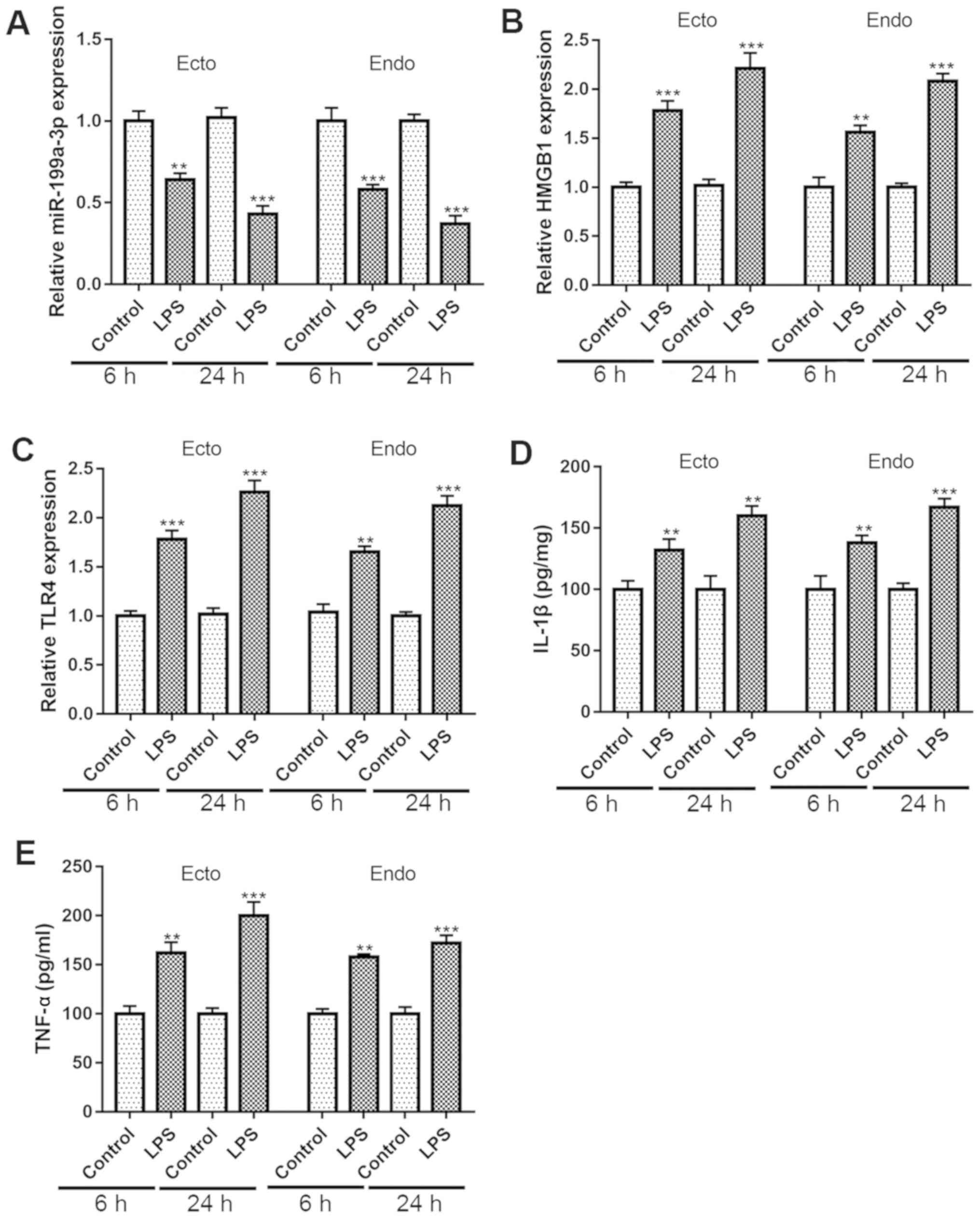 | Figure 3.Expression of miR-199a-3p and HMGB1
in LPS-induced cervical epithelial cells. The expression of (A)
miR-199a-3p, (B) HMGB1 mRNA and (C) TLR4 mRNA in Ecto and Endo
cells at 6 and 24 h after LPS (25 µg/ml) treatment, as determined
by reverse transcription-quantitative PCR. The levels of (D) IL-1β
and (E) TNF-α in the cell culture medium of Ecto and Endo cells at
6 and 24 h after LPS (25 µg/ml) treatment, as detected using an
ELISA assay. Data represents the mean ± SEM. **P<0.01,
***P<0.001 vs. control. miR, microRNA; HMGB1, high-mobility
group box 1 protein; TLR4, toll-like receptor 4; IL, interleukin;
TNF, tumor necrosis factor; LPS, lipopolysaccharide; Ecto,
ectocervical; Endo, endocervical. |
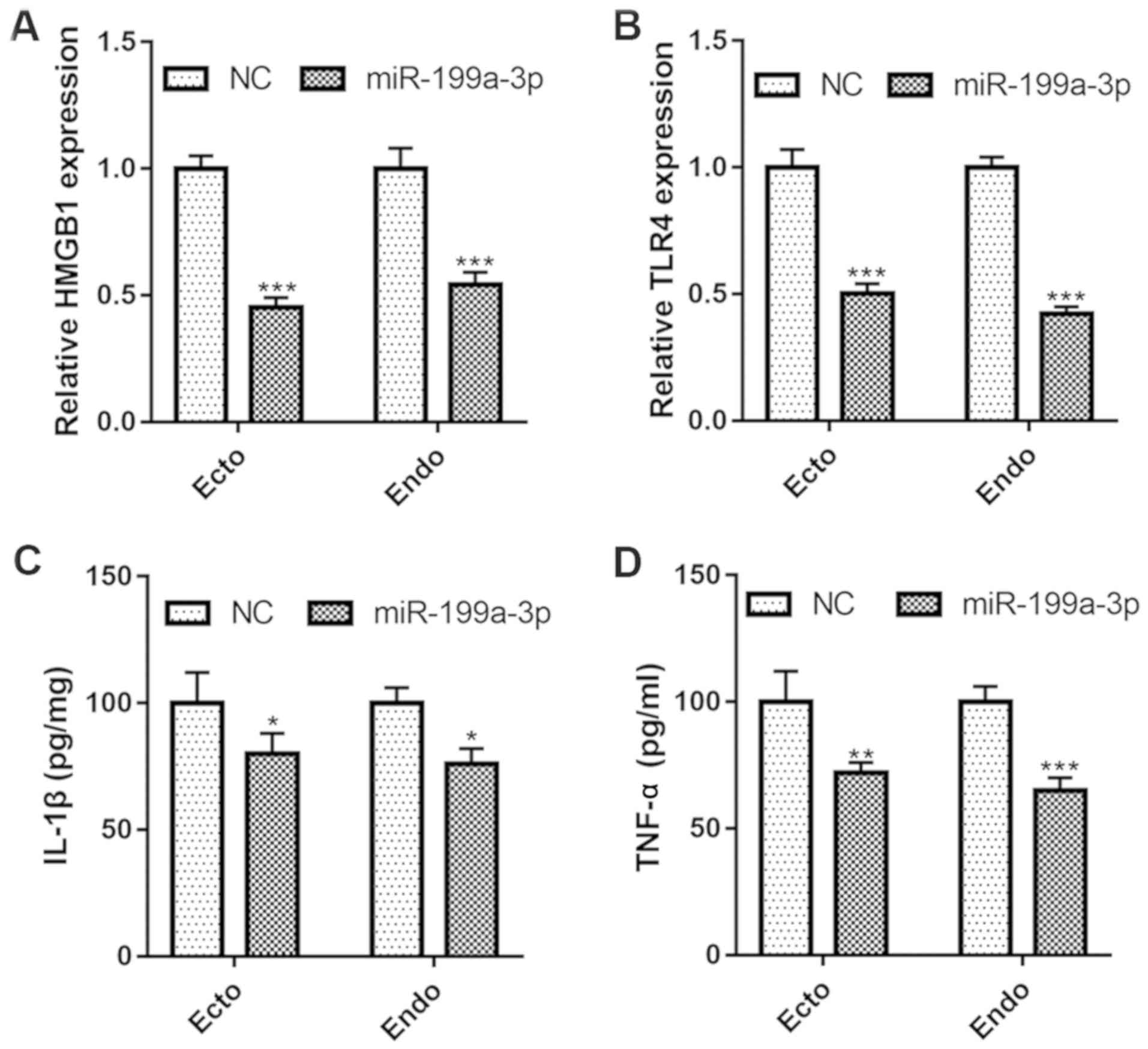
Overexpression of miR-199a-3p inhibits
the inflammatory phenotype in vitro
To investigate the effect of miR-199a-3p on cervical
epithelial cell inflammation, Ecto and Endo cells were transfected
with miR-199a-3p mimics (transfection efficiency presented in
Fig. S1A), which significantly
decreased the mRNA expression of HMGB1 and TLR4 (Fig. 4A and B). Concurrently, transfection
of miR-129-3p mimics inhibited the proinflammatory cytokine
production in both Ecto and Endo cells. As shown in Fig. 4C and D, the levels of IL-1β and
TNF-α were significantly decreased after miR-129-3p overexpression.
These results suggested that upregulation of the expression of
miR-199a-3p could inhibit the expression of HMGB1 and TLR4, and
contribute to anti-inflammation in cervical epithelial cells in
vitro.
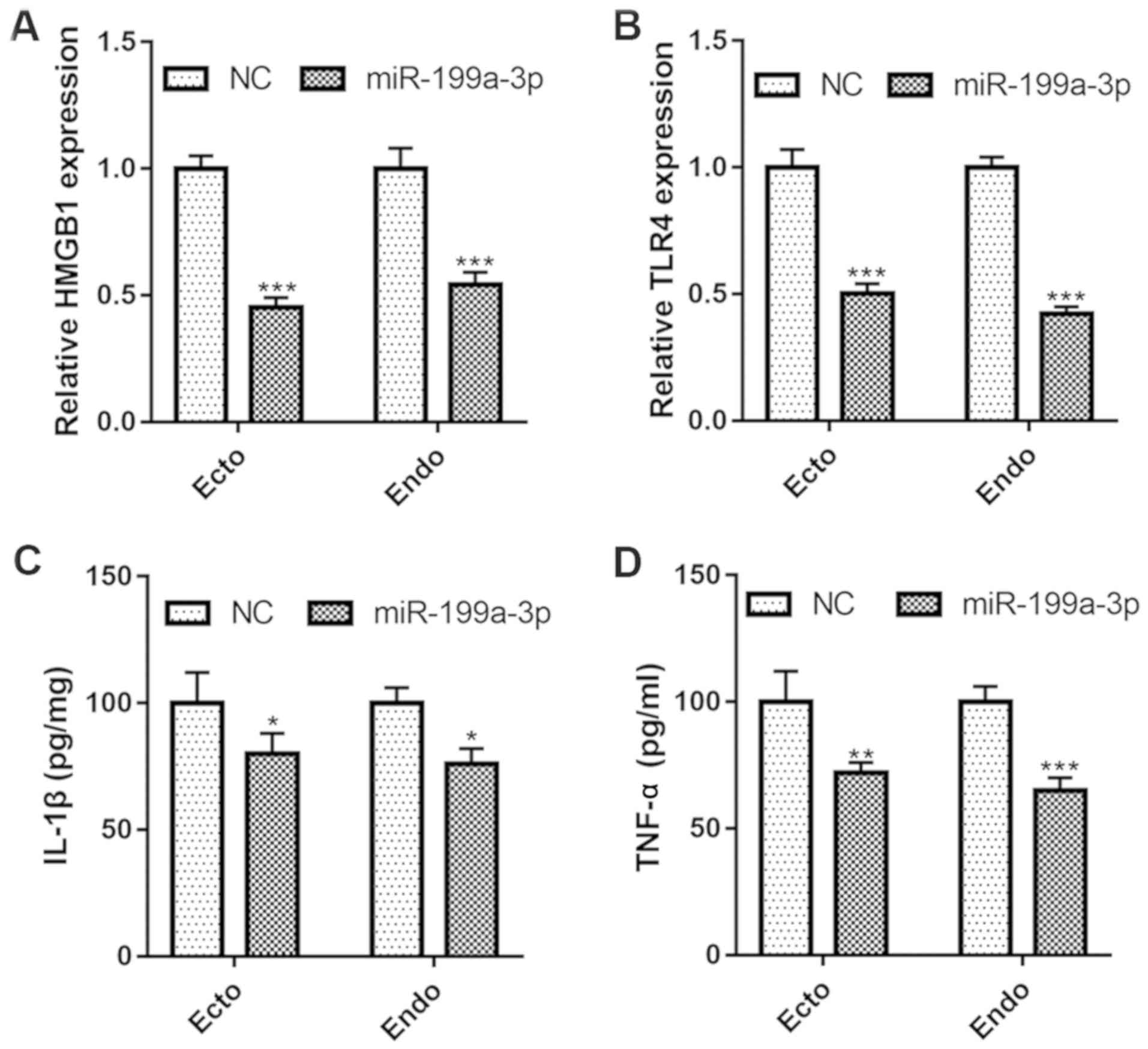 | Figure 4.Overexpression of miR-199a-3p
inhibits inflammatory phenotype in vitro. The mRNA expression of
(A) HMGB1 and (B) TLR4 in Ecto and Endo cells after miR-199a-3p
overexpression, as determined by reverse transcription-quantitative
PCR. The levels of (C) IL-1β and (D) TNF-α in the cell culture
medium of Ecto and Endo cells after miR-199a-3p overexpression, as
measured by ELISA assay. Data represents the mean ± SEM.
*P<0.05, **P<0.01, ***P<0.001 vs. NC. miR, microRNA;
HMGB1, high-mobility group box 1 protein; TLR4, toll-like receptor
4; IL, interleukin; TNF, tumor necrosis factor; LPS,
lipopolysaccharide; Ecto, ectocervical; Endo, endocervical; NC,
negative control. |
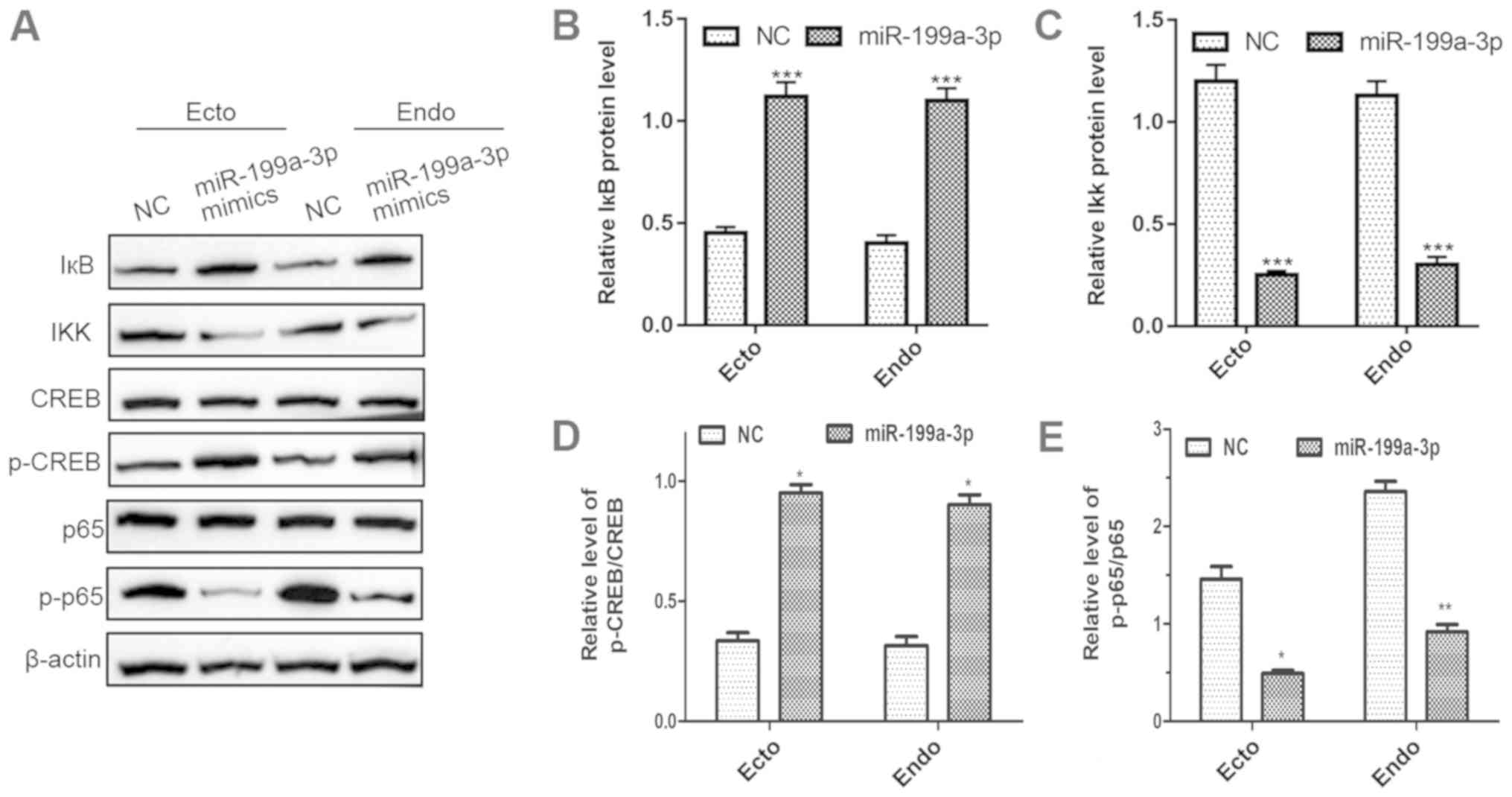
Overexpression of miR-199a-3p
suppresses the NF-кB pathway in cervical epithelial cells
To explore whether miR-199a-3p influences
inflammatory responses by regulating the NF-κB pathway, Ecto and
Endo cells were transfected with miR-199a-3p mimics, and the
proteins involved in the NF-κB pathway were detected by western
blotting. As shown in Fig. 5,
there was a significant increase in the protein expression of IκB
and activated p-CREB (Fig. 5A, B and
D). In contrast, the protein expression levels of IKK and p-p65
were significantly decreased (Fig. 5A,
C and E). Notably, the expression of total CREB and p65 showed
no obvious change (Fig. 5A). These
data demonstrated that overexpression of miR-129-3p could inhibit
the activation of NF-κB signaling, which indicated that the NF-κB
pathway participates in the regulation of the inflammatory response
by miR-129-3p.
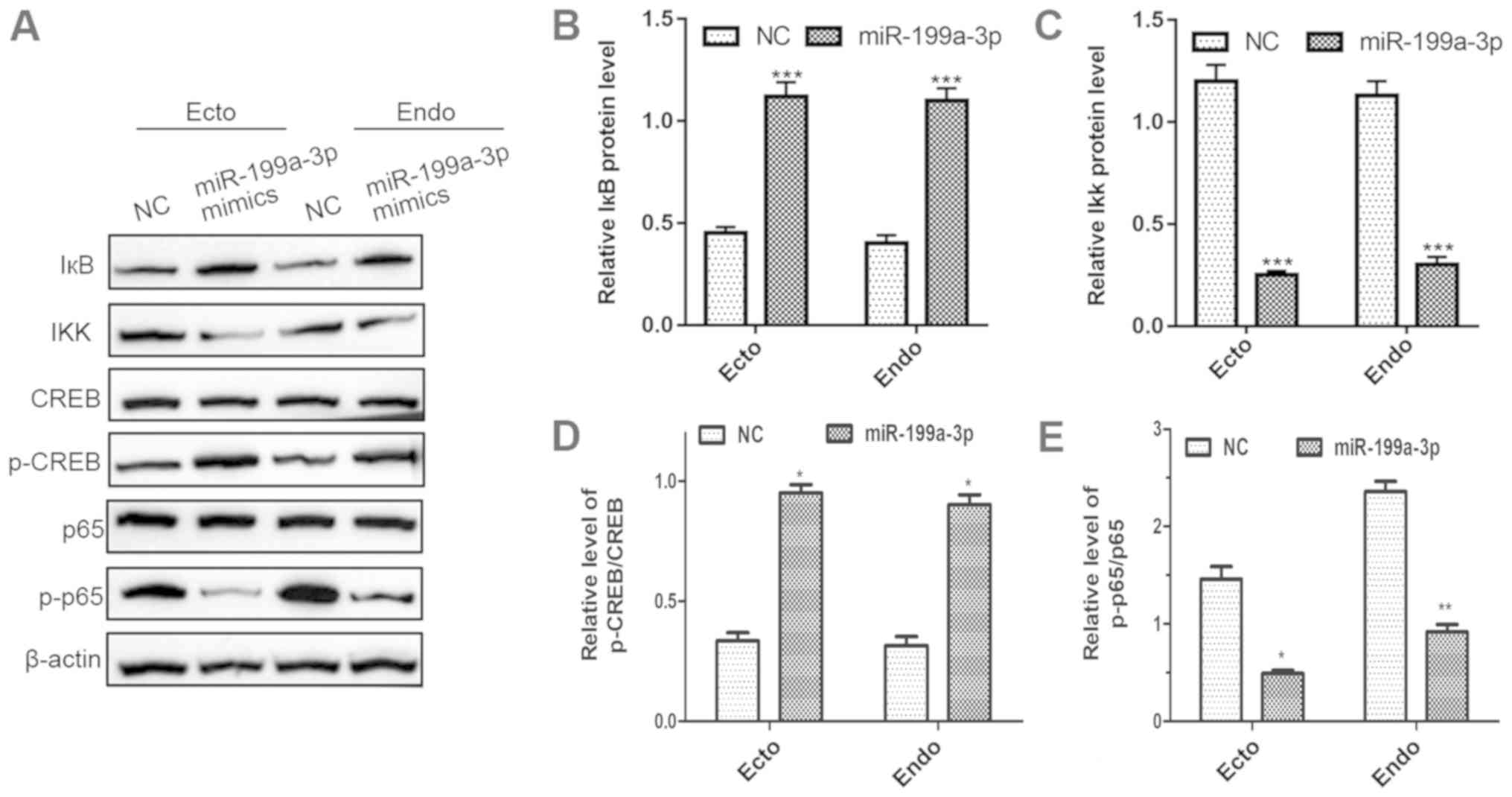 | Figure 5.Overexpression of miR-199a-3p
suppresses NF-кB signaling in cervical epithelial cells. (A) The
protein expression levels of IκB, IKK, p-CREB and p-p65 in Ecto and
Endo cells after miR-199a-3p overexpression were analyzed by
western blotting. (B-E) The quantification of these western blots.
Data represents the mean ± SEM. *P<0.05, **P<0.01,
***P<0.001 vs. NC. miR, microRNA; p-, phosphorylated; Ecto,
ectocervical; Endo, endocervical; NC, negative control; IκB,
inhibitor of NF-κB; IKK, IκB kinase; CREB, cAMP response
element-binding protein. |
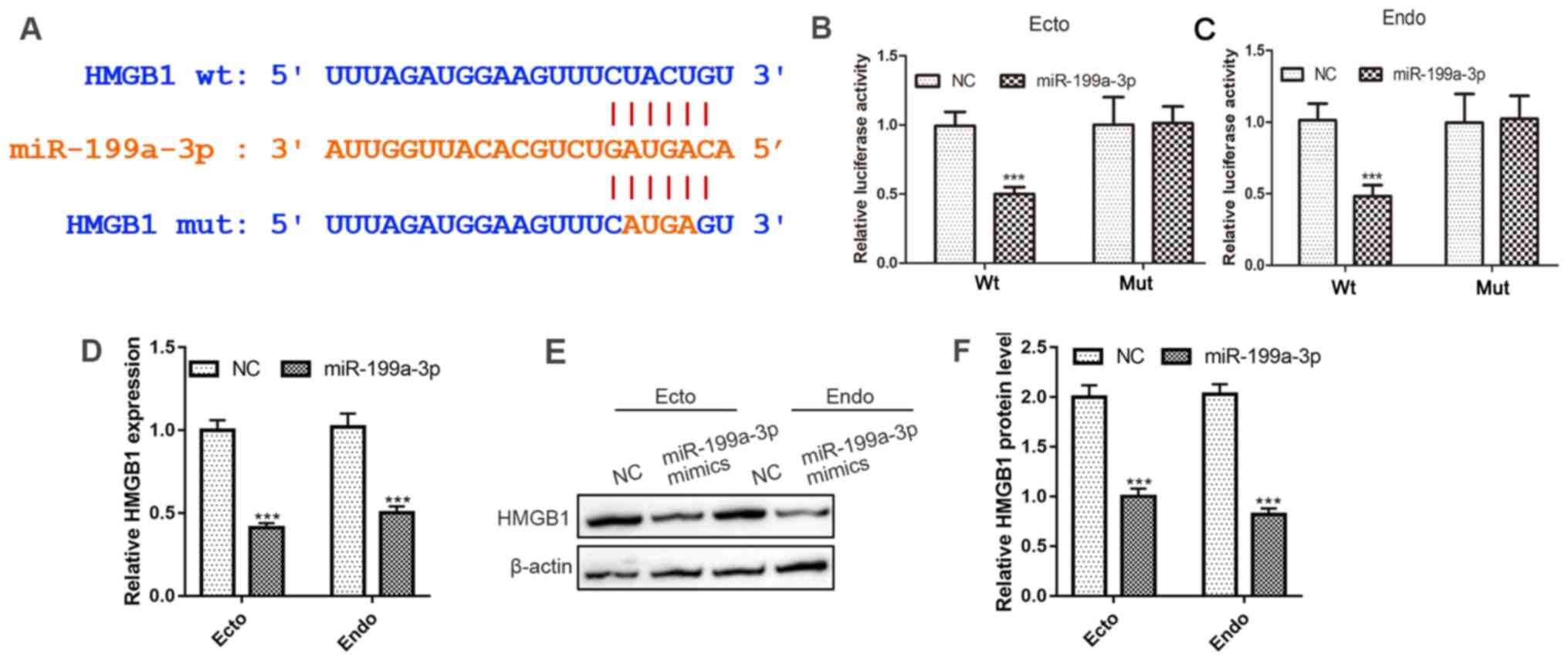
miR-199a-3p targets HMGB1
To explore the underlying targets of miR-199a-3p in
Ecto and Endo cells, the targets of miR-129-3p were predicted by
the bioinformatics software TargetScan. As shown in Fig. 6A, HMGB1 was found to be one of the
targets of miR-129-3p, and a binding site for miR-199a-3p was found
on the HMGB1 mRNA 3UTR. To verify the targeting relationship
between miR-129-3p and HMGB1, a luciferase reporter assay was
performed. The results showed that luciferase activity was
significantly suppressed in Ecto and Endo cells co-transfected with
miR-199a-3p mimics and the luciferase reporter vector of wild-type
HMGB1 containing the miR-199a-3p binding site sequence, but there
was no significant difference in luciferase activity between the
negative control- and miR-129-3p mimic-transfected group when the
cells were co-transfected with the binding site mutant HMGB1
luciferase reporter vector (Fig. 6B
and C). Moreover, Ecto and Endo cells transfected with
miR-199a-3p mimics significantly suppressed both the mRNA and
protein expression of HMGB1 (Fig.
6D-F). These results suggested that miR-199a-3p could suppress
the expression of HMGB1 at both the mRNA and protein levels by
directly targeting the 3UTR of HMGB1 mRNA.
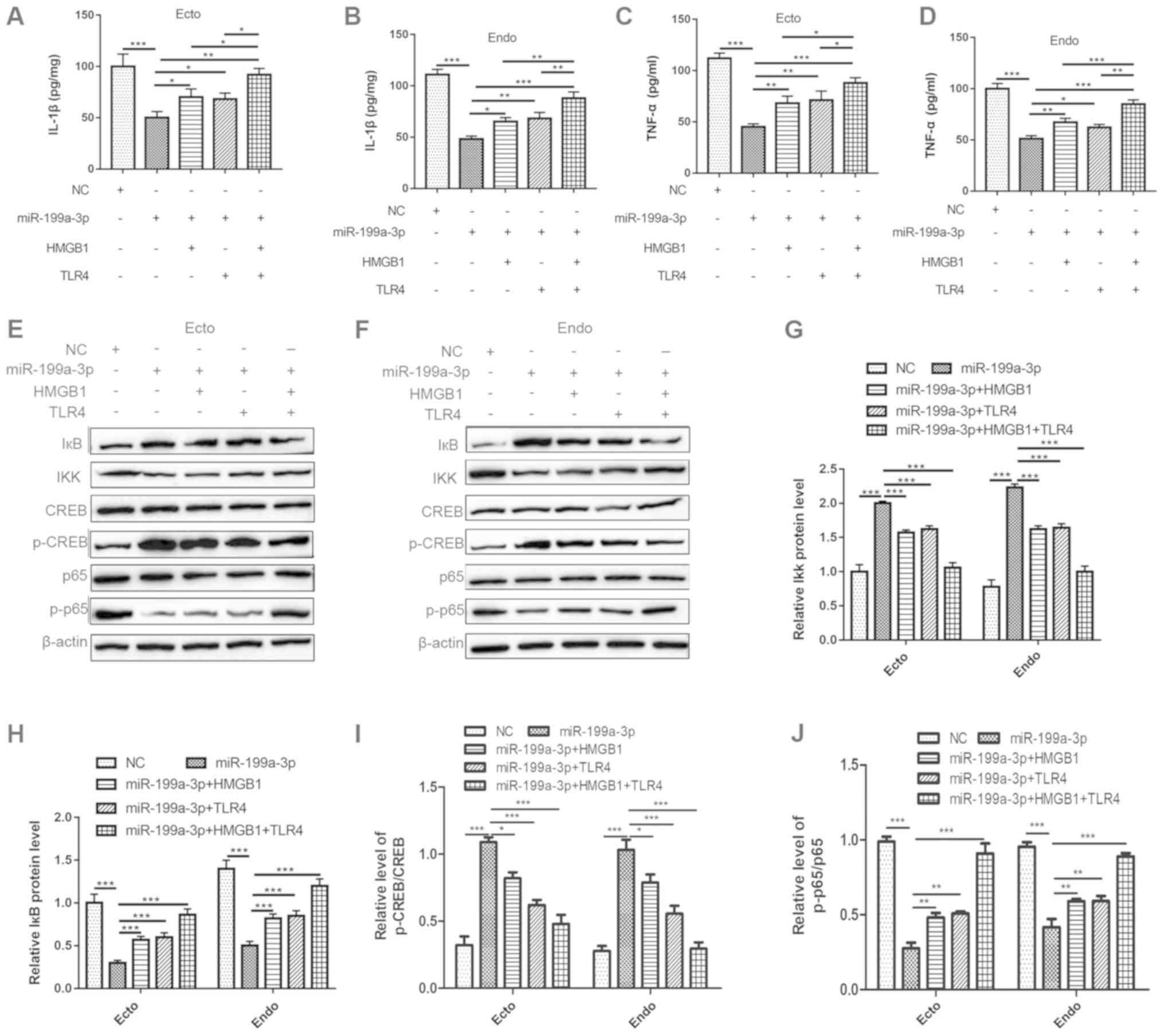
miR-199a-3p regulates inflammation via
the HMGB1/TLR4/NF-κB pathway
To investigate the mechanism by which miR-199a-3p
regulates inflammation, adenovirus vectors containing HMGB1 and
TLR4 were transfected into both Ecto and Endo cells (the
transfection efficiency of pcDNA-HMGB1 and pcDNA-TLR4 in Ecto and
Endo cells is presented in Fig. S1B
and D), and then the levels of inflammatory cytokines and
expression levels of proteins in the NF-κB pathway were analyzed.
The results showed that overexpression of HMGB1 and TLR4
significantly reversed the proinflammatory effects of miR-199a-3p
in Ecto and Endo cells. The expression levels of TNF-α and IL-1β
were upregulated when miR-129-3p was co-transfected with HMGB1 or
TLR4 adenovirus vectors compared with those in cells transfected
with miR-129-3p mimics alone (Fig.
7A-D). In addition, overexpression of miR-199a-3p significantly
suppressed the activation of the proteins in the NF-κB pathway, but
this effect was reversed by overexpression of HMGB1 and TLR4. As
shown in Fig. 7E-J, overexpression
of miR-129-3p upregulated the expression of IKK and p-CREB, but
this effect was reversed by HMGB1 and/or TLR4 overexpression, and
the downregulation of IκB and p-p65 was also reversed upon
co-transfection with HMGB1 and/or TLR4 adenovirus vectors. These
results indicated that the inhibition of NF-κB signaling by
miR-129-3p occurred through targeting HMGB1 and partly depended on
the participation of TLR4. Specifically, miR-129-3p could regulate
TLR4/NF-κB signaling by targeting HMGB1, thus influencing the
production of NF-κB-dependent proinflammatory cytokines.
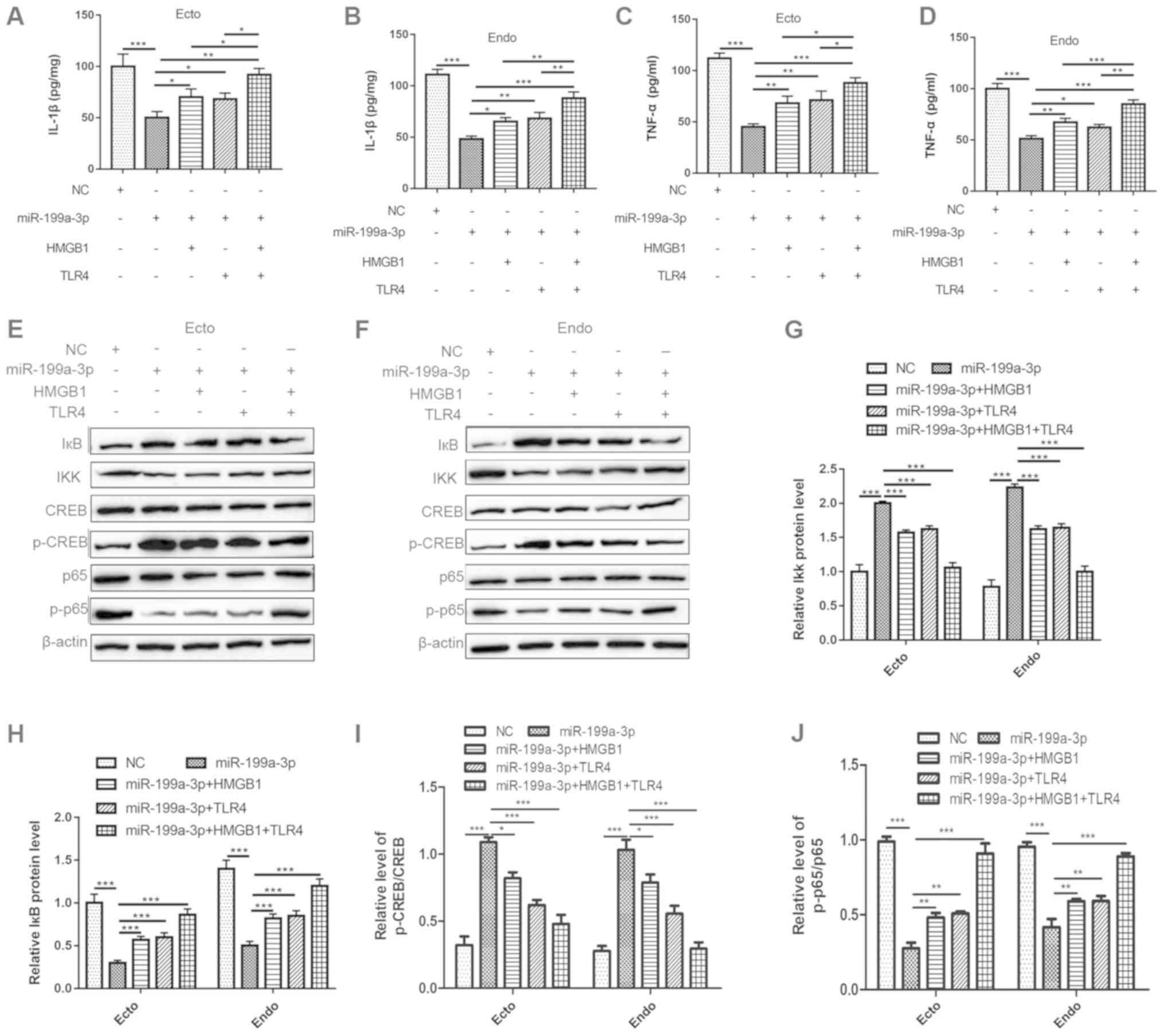 | Figure 7.miR-199a-3p regulates inflammation
via the HMGB1/TLR4/NF-кB pathway. The Ecto and Endo cells were
divided into 5 groups: i) NC group; ii) miR-199a-3p mimics group;
iii) miR-199a-3p mimics + pcDNA-HMGB1 group; iv) miR-199a-3p mimics
+ pcDNA-TLR4 group; v) miR-199a-3p mimics + pcDNA-HMGB1 +
pcDNA-TLR4 group. (A-D) The levels of IL-1β and TNF-α in the cell
culture medium were measured using an ELISA assay. (E-J) The
protein expression levels of IκB, IKK, p-CREB and p-p65 in Ecto and
Endo cells were determined by western blotting. Data represents the
mean ± SEM. *P<0.05, **P<0.01, ***P<0.001. miR, microRNA;
HMGB1, high-mobility group box 1 protein; Ecto, ectocervical; Endo,
endocervical; NC, negative control; TLR4, toll-like receptor 4; IL,
interleukin; TNF, tumor necrosis factor; p-, phosphorylated; IκB,
inhibitor of NF-κB; IKK, IκB kinase; CREB, cAMP response
element-binding protein. |
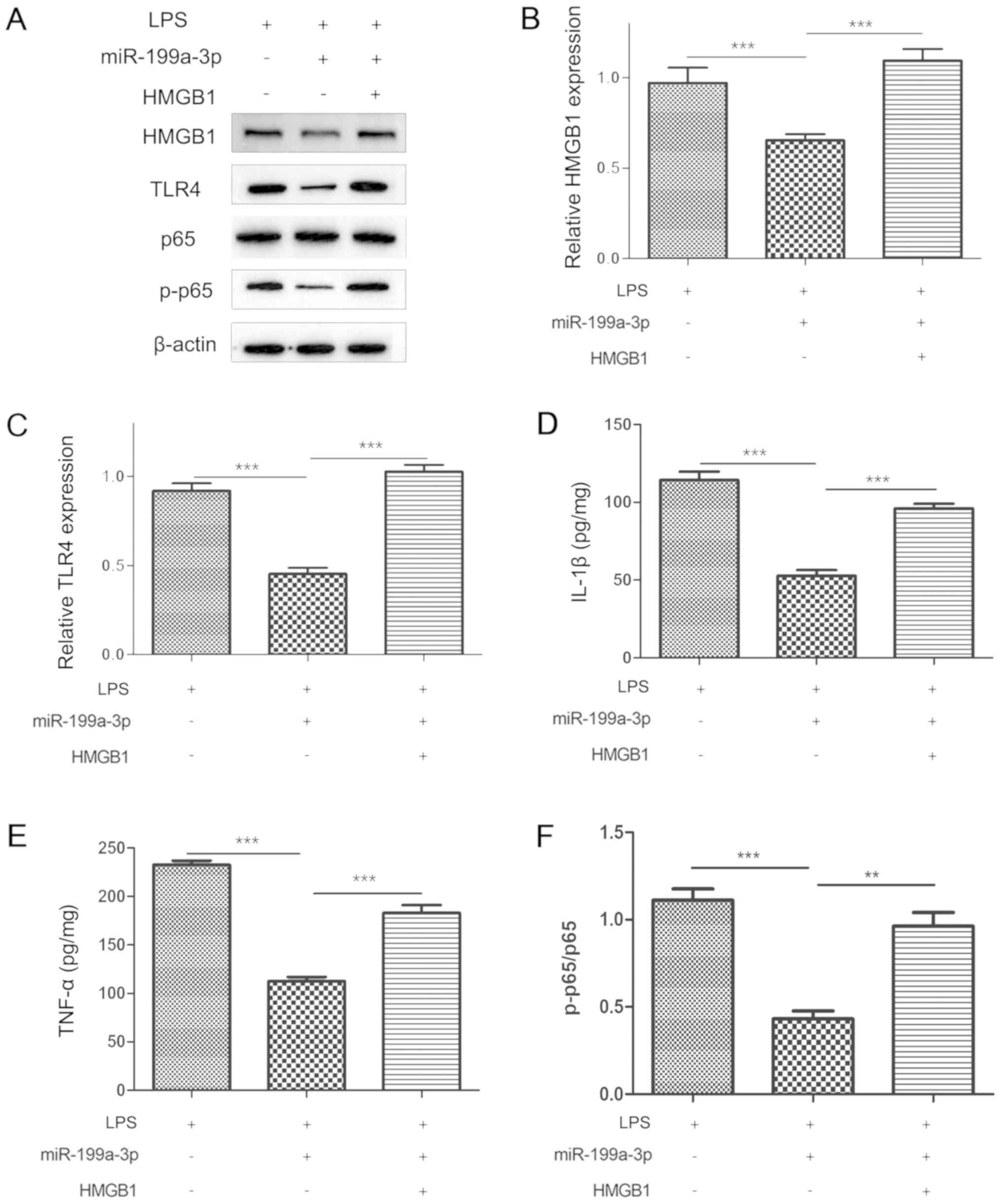
miR-199a-3p regulates inflammation
during PTB in vivo by targeting HMGB1
To determine the role of miR-199a-3p and HMGB1 in
inflammation during preterm labor in vivo, miR-199a-3p
mimics and/or pcDNA-HMGB1 were transfected into the LPS-induced
mouse PTB model (the transfection efficiency of miR-199a-3p mimics
and pcDNA-HMGB1 are presented in Fig.
S1C and E, respectively). The overexpression of miR-129-3p
significantly attenuated the expression of HMGB1 and TLR4 (Fig. 8A-C), and the release of IL-1β and
TNF-α was inhibited in the cervical tissues of LPS-induced PTB mice
(Fig. 8D and E). However, the
effects of overexpressing miR-129-3p were significantly reversed by
the HMGB1 adenovirus vector. After upregulating HMGB1, the
expression of TLR4 was also upregulated, and the levels of
proinflammatory cytokines IL-1β and TNF-α were concurrently
increased in cervical tissues (Fig.
8A-E). Furthermore, NF-κB signaling participated in this
process. Overexpression of miR-129-3p inhibited the activation of
p65, and the level of p-p65 in cervical tissues was decreased
compared with that in LPS-induced PTB mice. However, when
miR-129-3p mimics and pcDNA-HMGB1 were co-transfected into
LPS-induced PTB mice, the expression of p-p65 was upregulated
compared with that in the miR-129-3p-overexpression group (Fig. 8A and F). These data showed that
miR-129-3p suppressed cervical inflammation in vivo by
targeting HMGB1 in order to regulate the TLR4/NF-κB pathway.
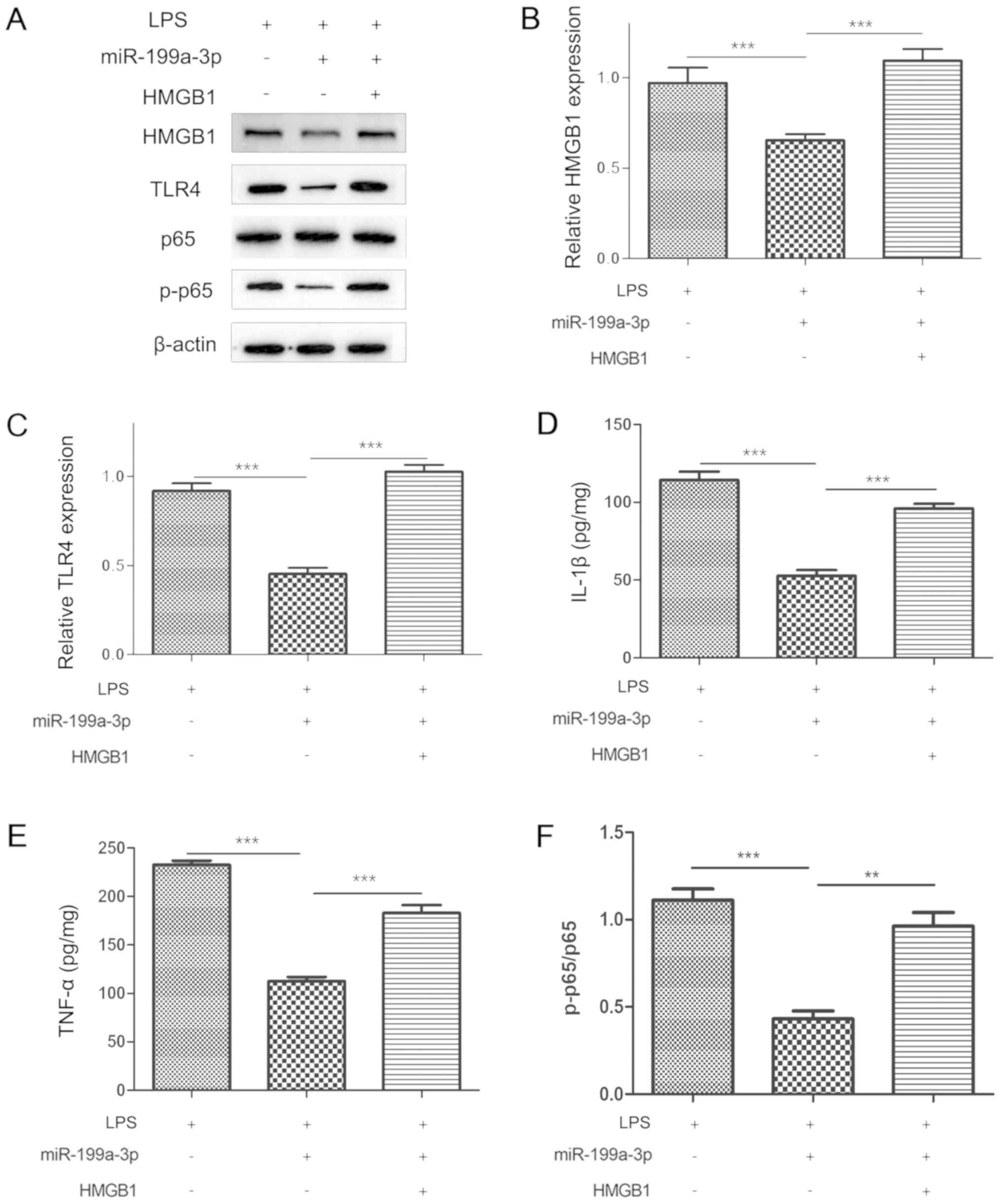 | Figure 8.Inflammatory role of miR-199a-3p and
HMGB1 during PTB in vivo. The LPS-induced PTB mice were used
to determine the protective effect of miR-199a-3p. The miR-199a-3p
mimics were transfected into LPS-induced PTB mice with or without
co-transfection of pcDNA-HMGB1. (A-C) The protein levels of HMGB1
and TLR4 in cervical epithelial tissues were measured by western
blotting. The levels of proinflammatory cytokines (D) IL-1β and (E)
TNF-α were measured by ELISA. (A and F) The activation of NF-κB
signaling was determined by the level of p-p65, as measured by
western blotting. Data represents the mean ± SEM. **P<0.01,
***P<0.001. miR, microRNA; HMGB1, high-mobility group box 1
protein; PTB, preterm birth; LPS, lipopolysaccharide; TLR4,
toll-like receptor 4; IL, interleukin; TNF, tumor necrosis factor;
p-, phosphorylated. |
Discussion
The present study explored a novel pathway that
regulates the molecular mechanism contributing to cervical
inflammation activation, which induces cervical epithelial barrier
injury and cervical remodeling. In the present study, the function
of miR-199a-3p and its target gene HMGB1 were investigated in
inflammatory-related PTB. The results showed that miR-199a-3p was
significantly downregulated in patients in the PTB and PPROM
groups, as well as in an LPS-induced preterm mouse model and
LPS-treated Ecto and Endo cells. In contrast, the expression of
HMGB1 and its primary membrane receptor TLR4 were both
significantly increased, which was accompanied by the increased
release of the proinflammatory factors IL-1β and TNF-α. Moreover,
the results demonstrated that miR-199a-3p participated in the
inflammatory activation of cervical remodeling during pregnancy by
inhibiting the activation of the TLR4/NF-κB proinflammatory signal
by targeting the 3UTR of HMGB1 (Fig.
9).
PTB is defined as delivery before 37 completed weeks
of gestation by the World Health Organization and can be subdivided
into extremely preterm (<28 weeks), very preterm (28–32 weeks)
and moderate to late PTB (32–36 weeks) (31). Currently, PTB is the primary cause
of perinatal morbidity and mortality (32), and the second cause of childhood
death below the age of 5 years (33). Spontaneous preterm labor is a
syndrome caused by multiple pathological processes and causes 70%
of PTBs (34). The increase in
uterine contractility, cervical dilatation and rupture of
chorioamniotic membranes are the ‘common pathways’ of delivery,
both in full term delivery and premature delivery (35). More specifically, the common
pathway is activated physiologically in the case of full-term
labor, whereas several disease processes activate one or more of
the components of the common pathway in the case of preterm labor.
Accumulating evidence suggests that preterm labor is a syndrome
attributable to multiple pathologic processes (35), including infection (36), vascular disorders (37), decidual senescence, uterine
overdistension (38–40), cervical disease (41), breakdown of maternal-fetal
tolerance and stress (42). Of
these, only intra-amniotic infection/inflammation has been causally
linked to spontaneous preterm delivery (43–45).
The innate immune system activated by endogenous danger signals
causes an inflammatory process in sterile inflammation (46), followed by the release of
proinflammatory cytokines, including IL-1β, IL-18, IFN-γ and TNF-α
(4, 47). In the present study, it was determined that the levels of
IL-1β and TNF-α were significantly increased in PTB, which
suggested that the differential regulation of molecules during
inflammation in PTB may be novel markers for the diagnosis of
PTB.
Stimulating uterine contraction is the first step of
preterm delivery, followed by cervical remodeling and early
delivery, and studies have shown that premature cervical remodeling
may be the main step of spontaneous preterm delivery (48–51).
Previous studies have suggested that infection- or
inflammatory-mediated destruction of the cervical epithelial
barrier promotes cervical remodeling and plays an important role in
the pathogenesis of preterm delivery (52–54).
However, the pathogenesis of cervical epithelial inflammation needs
further study. It is known that miR-199a-3p plays an important role
in inflammatory responses (55),
and it also plays a negative regulatory role in the NF-кB signaling
pathway to modulate inflammatory processes in cystic fibrosis
airways (27). Moreover,
miR-199a-3p is a crucial regulator of myometrial contractility and
prevention of PTB (26). The
present study focused on the role of miR-199a-3p in cervical
epithelial inflammation. First, it was found that the expression of
miR-199a-3p was significantly reduced in the cervical epithelial
tissues of patients in the PTB group, in an LPS-induced preterm
mouse model and LPS-induced Ecto and Endo cells. Furthermore,
overexpression of miR-199a-3p significantly suppressed the
expression of HMGB1, TLR4, p-p65, IL-1β and TNF-α in vitro
and in vivo. These results indicated that miR-199a-3p plays
an important role in the inflammation of cervical epithelial cells
during the process of preterm labor and may regulate HMGB1 and
TLR4/NF-κB signaling.
HMGB1 is a highly evolutionarily conserved protein
that promotes gene transcription when it is localized to the
nucleus and acts as an alarmin when released extracellularly
(56). HMGB1 is a late mediator of
several inflammatory diseases that signal through several
receptors, including advanced glycation end products (RAGE), TLR2
and TLR4 (57,58). Furthermore, HMGB1 binds to
receptors that stimulate immune cells to produce various
proinflammatory cytokines such as TNF-α, IL-1β, IL-1α and IL-8
(59,60). Proinflammatory cytokines can induce
excessive cellular or tissue damage to inflammatory lesions
(61,62). As the major receptor of endogenous
extracellular HMGB1, TLR4 can activate the proinflammatory
signaling of the NF-κB pathway and thus promote the expression of
proinflammatory mediators (17–20).
Previous reports have revealed that HMGB1 is involved in the
occurrence of PTB and plays an important role in the pathogenesis
of the inflammatory process in spontaneous PTB (63). The TLR4/NF-κB pathway also plays a
critical role in inflammation, and reports have confirmed that the
expression and activation of TLR4/NF-κB signaling are involved in
gestational inflammation (64). In
the present study, the role of HMGB1, its downstream TLR4/NF-κB
signaling in preterm cervical epithelial inflammation and its
upstream regulatory mechanism were explored. The results showed
that HMGB1 was increased in the cervical epithelial tissues from
the patients in the PTB group and the LPS-induced preterm mouse
model, and also in LPS-induced Ecto and Endo cells. Notably, the
expression of HMGB1 was negatively regulated by miR-199a-3p, which
directly targeted the 3UTR of HMGB1 mRNA. Overexpression of HMGB1
significantly reversed the anti-inflammatory effects of miR-199a-3p
mimics in vitro and in vivo. Concurrently, the
expression of the TLR4/NF-κB pathway and proinflammatory cytokines
were also upregulated after HMGB1 was overexpressed in LPS-induced
preterm labor mice. These results indicated that HMGB1 promotes
cervical epithelial inflammation in preterm delivery via the
TLR4/NF-κB pathway, and this molecular axis can be negatively
regulated by miR-199a-3p.
Overall, this study suggested that miR-199a-3p plays
a negative regulatory role in the cervical epithelial inflammatory
process during PTB. Furthermore, miR-199a-3p regulates the
inflammatory process by targeting HMGB1 in order to modulate the
TLR4/NF-κB pathway (Fig. 9). This
study provides new insights into the mechanism of cervical
remodeling in spontaneous preterm delivery and suggests that
cervical epithelial inflammation is involved in the occurrence of
cervical remodeling to promote the development of preterm labor. In
addition, the present study provides a new approach and potential
biological target molecules for the prevention of
inflammatory-induced spontaneous PTB.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
This study was supported by grants from the Yunnan
Applied Basic Research Project-Kunming Medical University Union
Foundation (grant no. 2017FE468-117); the Health Science and
Technology Program of Yunnan Province (grant number 2016NS199); the
Science and Technology Talents and Platform Plan of Yunnan Province
(grant no. 2017HC008 and S2016IC027).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author upon reasonable
request.
Authors contributions
All authors contributed substantially to this
manuscript. JP and JJ contributed equally to this manuscript, they
performed all experiments and were the major contributors in
writing the manuscript. HW participated primarily in the in vitro
tests; XF contributed primarily to the animal experiments; and XD
contributed to conception and design this study and guided the
writing of manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent for
publication
All human tissues were obtained with the approval of
the Hospital Ethical Committee. Informed consent was provided by
each participant before surgery. All experimental mouse protocols
were approved by the Animal Ethics Committee of the Hospital, and
the animals were handled according to the management requirements
of the Animal Management Association of the Hospital.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
McCall EM, Alderdice F, Halliday HL, Vohra
S and Johnston L: Interventions to prevent hypothermia at birth in
preterm and/or low birth weight infants. Cochrane Database Syst
Rev. 2:CD0042102018.PubMed/NCBI
|
|
2
|
Son M and Miller ES: Predicting preterm
birth: Cervical length and fetal fibronectin. Semin Perinatol.
41:445–451. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gomez-Lopez N, Romero R, Xu Y, Plazyo O,
Unkel R, Leng Y, Than NG, Chaiworapongsa T, Panaitescu B, Dong Z,
et al: A role for the inflammasome in spontaneous preterm labor
with acute histologic chorioamnionitis. Reprod Sci. 24:1382–1401.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Boyle AK, Rinaldi SF, Norman JE and Stock
SJ: Preterm birth: Inflammation, fetal injury and treatment
strategies. J Reprod Immunol. 119:62–66. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Vink J and Mourad M: The pathophysiology
of human premature cervical remodeling resulting in spontaneous
preterm birth: Where are we now? Semin Perinatol. 41:427–437. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Carter Moylan HE, Caitlyn Nguyen-Ngo C,
Ratana Lim R and Lappas M: The short chain fatty acids butyrate and
propionate protect against inflammation induced activation of
mediators involved in active labor: implications for preterm birth.
Mol Hum Reprod. April 1–2020.(Epub ahead of print).
|
|
7
|
Canan Unal C, Esra Karatas E, Fadıloglu E,
Portakal O and Beksac MS: Comparison of term and preterm labor
procalcitonin and leukocyte cell volume, conductivity and light
scatter (VCS) parameters in order to demonstrate the impact of
inflammation on the triggering mechanisms of preterm uterin
contractions. J Obstet Gynaecol Res. 46:694–698. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Challis JR, Lockwood CJ, Myatt L, Norman
JE, Strauss JF III and Petraglia F: Inflammation and pregnancy.
Reprod Sci. 16:206–215. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mendelson CR: Minireview: Fetal-maternal
hormonal signaling in pregnancy and labor. Mol Endocrinol.
23:947–954. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lu HY, Ma JL, Shan JY, Zhang J, Wang QX
and Zhang Q: High-mobility group box-1 and receptor for advanced
glycation end products in preterm infants with brain injury. World
J Pediatr. 13:228–235. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Splichalova A, Slavikova V, Splichalova Z
and Splichal I: Preterm life in sterile conditions: A study on
preterm, germ-free piglets. Front Immunol. 9:2202018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Andersson U and Tracey KJ: HMGB1 is a
therapeutic target for sterile inflammation and infection. Annu Rev
Immunol. 29:139–162. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Baumbusch MA, Buhimschi CS, Oliver EA,
Zhao G, Thung S, Rood K and Buhimschi IA: High Mobility Group-Box 1
(HMGB1) levels are increased in amniotic fluid of women with
intra-amniotic inflammation-determined preterm birth, and the
source may be the damaged fetal membranes. Cytokine. 81:82–87.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Plazyo O, Romero R, Unkel R, Balancio A,
Mial TN, Xu Y, Dong Z, Hassan SS and Gomez-Lopez N: HMGB1 induces
an inflammatory response in the chorioamniotic membranes that is
partially mediated by the inflammasome. Biol Reprod. 95:1302016.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Menon R, Behnia F, Polettini J, Saade GR,
Campisi J and Velarde M: Placental membrane aging and HMGB1
signaling associated with human parturition. Aging (Albany NY).
8:216–230. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mukherjee S, Huda S and Sinha Babu SP:
Toll-like receptor polymorphism in host immune response to
infectious diseases: A review. Scand J Immunol. 90:e127712019.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tsung A, Klune JR, Zhang X, Jeyabalan G,
Cao Z, Peng X, Stolz DB, Geller DA, Rosengart MR and Billiar TR:
HMGB1 release induced by liver ischemia involves Toll-like receptor
4-dependent reactive oxygen species production and calcium-mediated
signaling. J Exp Med. 204((12)): 2913–2923. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Park JS, Svetkauskaite D, He Q, Kim JY,
Strassheim D, Ishizaka A and Abraham E: Involvement of toll-like
receptors 2 and 4 in cellular activation by high mobility group box
1 protein. J Biol Chem. 279:7370–7377. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tsung A, Zheng N, Jeyabalan G, Izuishi K,
Klune JR, Geller DA, Lotze MT, Lu L and Billiar TR: Increasing
numbers of hepatic dendritic cells promote HMGB1-mediated
ischemia-reperfusion injury. J Leukoc Biol. 81:119–128. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Fan J, Li Y, Levy RM, Fan JJ, Hackam DJ,
Vodovotz Y, Yang H, Tracey KJ, Billiar TR and Wilson MA:
Hemorrhagic shock induces NAD(P)H oxidase activation in
neutrophils: Role of HMGB1-TLR4 signaling. J Immunol.
178:6573–6580. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kumar N, Nandula P, Menden H, Jarzembowski
J and Sampath V: Placental TLR/NLR expression signatures are
altered with gestational age and inflammation. J Matern Fetal
Neonatal Med. 30:1588–1595. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhong X, Jiang YZ, Liu P, He W, Xiong Z,
Chang W, Zhu J and Cui Q: Toll-like 4 receptor /NFκB
inflammatory/miR-146a pathway contributes to the ART-correlated
preterm birth outcome. Oncotarget. 7:72475–72485. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Elovitz MA, Anton L, Bastek J and Brown
AG: Can microRNA profiling in maternal blood identify women at risk
for preterm birth? Am J Obstet Gynecol. 212:782.e1–782.e5. 2015.
View Article : Google Scholar
|
|
24
|
Elovitz MA, Brown AG, Anton L, Gilstrop M,
Heiser L and Bastek J: Distinct cervical microRNA profiles are
present in women destined to have a preterm birth. Am J Obstet
Gynecol. 210:221.e1–11. 2014. View Article : Google Scholar
|
|
25
|
Wommack JC, Trzeciakowski JP, Miranda RC,
Stowe RP and Ruiz RJ: Micro RNA clusters in maternal plasma are
associated with preterm birth and infant outcomes. PLoS One.
13:e01990292018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Williams KC, Renthal NE, Gerard RD and
Mendelson CR: The microRNA (miR)-199a/214 cluster mediates opposing
effects of progesterone and estrogen on uterine contractility
during pregnancy and labor. Mol Endocrinol. 26:1857–1867. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Bardin P, Marchal-Duval E, Sonneville F,
Blouquit-Laye S, Rousselet N, Le Rouzic P, Corvol H and Tabary O:
Small RNA and transcriptome sequencing reveal the role of
miR-199a-3p in inflammatory processes in cystic fibrosis airways. J
Pathol. 245:410–420. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Chen Z, Dong WH, Chen Q, Li QG and Qiu ZM:
NLRP1Downregulation of miR-199a-3p mediated by the
CtBP2-HDAC1-FOXP3 transcriptional complex contributes to acute lung
injury by targeting. Int J Biol Sci. 15:2627–2640. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Δ Δ C(T)) Method. Methods. 25:402–408. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Renthal NE, Chen CC, Williams KC, Gerard
RD, Prange-Kiel J and Mendelson CR: miR-200 family and targets,
ZEB1 and ZEB2, modulate uterine quiescence and contractility during
pregnancy and labor. Proc Natl Acad Sci USA. 107:20828–20833. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Organization WH: WHO: Recommended
definitions, terminology and format for statistical tables related
to the perinatal period and use of a new certificate for cause of
perinatal deaths. Modifications recommended by FIGO as amended
October 14, 1976. Acta Obstet Gynecol Scand. 56:247–253.
1977.PubMed/NCBI
|
|
32
|
Goldenberg RL, Culhane JF, Iams JD and
Romero R: Epidemiology and causes of preterm birth. Lancet.
371:75–84. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Liu L, Johnson HL, Cousens S, Perin J,
Scott S, Lawn JE, Rudan I, Campbell H, Cibulskis R, Li M, et al
Child Health Epidemiology Reference Group of WHO and UNICEF, :
Global, regional, and national causes of child mortality: An
updated systematic analysis for 2010 with time trends since 2000.
Lancet. 379:2151–2161. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Paquette AG, Shynlova O, Kibschull M,
Price ND and Lye SJ; Global Alliance to Prevent Prematurity and
Stillbirth Systems Biology of Preterm Birth Team, : Comparative
analysis of gene expression in maternal peripheral blood and
monocytes during spontaneous preterm labor. Am J Obstet Gynecol.
218:345.e341–345.e330. 2018. View Article : Google Scholar
|
|
35
|
Romero R, Espinoza J, Kusanovic JP, Gotsch
F, Hassan S, Erez O, Chaiworapongsa T and Mazor M: The preterm
parturition syndrome. BJOG. 113 (Suppl 3):17–42. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Gonçalves LF, Chaiworapongsa T and Romero
R: Intrauterine infection and prematurity. Ment Retard Dev Disabil
Res Rev. 8:3–13. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
The Preterm Labor Syndrome, . Biochemical,
Cytologic, Immunologic, Pathologic, Microbiologic, and Clinical
Evidence That Preterm Labor Is a Heterogeneous Disease. Am J Obstet
Gynecol. 168:2881993. View Article : Google Scholar
|
|
38
|
Ludmir J, Samuels P, Brooks S and Mennuti
MT: Pregnancy outcome of patients with uncorrected uterine
anomalies managed in a high-risk obstetric setting. Obstet Gynecol.
75:906–910. 1990.PubMed/NCBI
|
|
39
|
Lallar M and Nandal R and Nandal R; Anam
Ul Haq, : Perinatal outcome in idiopathic polyhydramnios. J Obstet
Gynaecol India. 65:310–314. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Colditz P: Multiple Pregnancy:
Epidemiology, Gestation, and Perinatal Outcome. Twin Res Hum Genet.
9:183–184. 2006. View Article : Google Scholar
|
|
41
|
Choi J, Park JW, Kim BJ, Choi YJ, Hwang JH
and Lee SM: Funisitis is more common in cervical insufficiency than
in preterm labor and preterm premature rupture of membranes. J
Perinat Med. 44:523–529. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Hobel CJ: Stress and preterm birth. Clin
Obstet Gynecol. 47:856–880, discussion 881–882. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Romero R, Dey SK and Fisher SJ: Preterm
labor: One syndrome, many causes. Science. 345:760–765. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Romero R, Gómez R, Chaiworapongsa T,
Conoscenti G, Kim JC and Kim YM: The role of infection in preterm
labour and delivery. Paediatr Perinat Epidemiol. 15 (Suppl
2):41–56. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Gilman-Sachs A, Dambaeva S, Salazar Garcia
MD, Hussein Y, Kwak-Kim J and Beaman K: Inflammation induced
preterm labor and birth. J Reprod Immunol. 129:53–58. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Chen GY and Nuñez G: Sterile inflammation:
Sensing and reacting to damage. Nat Rev Immunol. 10:826–837. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Cappelletti M, Della Bella S, Ferrazzi E,
Mavilio D and Divanovic S: Inflammation and preterm birth. J Leukoc
Biol. 99:67–78. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Timmons BC, Mitchell SM, Gilpin C and
Mahendroo MS: Dynamic changes in the cervical epithelial tight
junction complex and differentiation occur during cervical ripening
and parturition. Endocrinology. 148:1278–1287. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Gonzalez JM, Xu H, Chai J, Ofori E and
Elovitz MA: Preterm and term cervical ripening in CD1 Mice (Mus
musculus): Similar or divergent molecular mechanisms? Biol Reprod.
81:1226–1232. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Timmons B, Akins M and Mahendroo M:
Cervical remodeling during pregnancy and parturition. Trends
Endocrinol Metab. 21:353–361. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Read CP, Word RA, Ruscheinsky MA, Timmons
BC and Mahendroo MS: Cervical remodeling during pregnancy and
parturition: Molecular characterization of the softening phase in
mice. Reproduction. 134:327–340. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Nold C, Anton L, Brown A and Elovitz M:
Inflammation promotes a cytokine response and disrupts the cervical
epithelial barrier: a possible mechanism of premature cervical
remodeling and preterm birth. Am J Obstet Gynecol 206: 208.e1-7,
2012.
|
|
53
|
Akgul Y, Word RA, Ensign LM, Yamaguchi Y,
Lydon J, Hanes J and Mahendroo M: Hyaluronan in cervical epithelia
protects against infection-mediated preterm birth. J Clin Invest.
124:5481–5489. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Timmons BC and Mahendroo M: Processes
regulating cervical ripening differ from cervical dilation and
postpartum repair: Insights from gene expression studies. Reprod
Sci. 14 (Suppl):53–62. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Gu N, You L, Shi C, Yang L, Pang L, Cui X,
Ji C, Zheng W and Guo X: Expression of miR-199a-3p in human
adipocytes is regulated by free fatty acids and adipokines. Mol Med
Rep. 14:1180–1186. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Lotze MT and Tracey KJ: High-mobility
group box 1 protein (HMGB1): Nuclear weapon in the immune arsenal.
Nat Rev Immunol. 5:331–342. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Bellussi LM, Iosif C, Sarafoleanu C, Jianu
E, Duda R, Panaitescu E, Passali FM and Passali D: Are HMGB1
protein expression and secretion markers of upper airways
inflammatory diseases? J Biol Regul Homeost Agents. 27:791–804.
2013.PubMed/NCBI
|
|
58
|
Tian J, Avalos AM, Mao SY, Chen B, Senthil
K, Wu H, Parroche P, Drabic S, Golenbock D, Sirois C, et al:
Toll-like receptor 9-dependent activation by DNA-containing immune
complexes is mediated by HMGB1 and RAGE. Nat Immunol. 8:487–496.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Dong W, Zhu Q, Yang B, Qin Q, Wang Y, Xia
X, Zhu X, Liu Z, Song E and Song Y: Polychlorinated biphenyl
quinone induces caspase 1-mediated pyroptosis through induction of
pro-inflammatory HMGB1-TLR4-NLRP3-GSDMD signal axis. Chem Res
Toxicol. 32:1051–1057. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Thankam FG, Roesch ZK, Dilisio MF, Radwan
MM, Kovilam A, Gross RM and Agrawal DK: Association of inflammatory
responses and ECM disorganization with HMGB1 upregulation and NLRP3
inflammasome activation in the injured rotator cuff tendon. Sci
Rep. 8:89182018. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Kim EJ, Park SY, Baek SE, Jang MA, Lee WS,
Bae SS, Kim K and Kim CD: HMGB1 increases IL-1β production in
vascular smooth muscle cells via NLRP3 inflammasome. Front Physiol.
9:3132018. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Subramanian S, Pallati PK, Sharma P,
Agrawal DK and Nandipati KC: Significant association of TREM-1 with
HMGB1, TLRs and RAGE in the pathogenesis of insulin resistance in
obese diabetic populations. Am J Transl Res. 9:3224–3244.
2017.PubMed/NCBI
|
|
63
|
Son GH, Kim Y, Lee JJ, Lee KY, Ham H, Song
JE, Park ST and Kim YH: MicroRNA-548 regulates high mobility group
box 1 expression in patients with preterm birth and
chorioamnionitis. Sci Rep. 9:197462019. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Kumar N, Nandula P, Menden H, Jarzembowski
J and Sampath V: Placental TLR/NLR expression signatures are
altered with gestational age and inflammation. J Matern Fetal
Neonatal Med. 30:1588–1595. 2017. View Article : Google Scholar : PubMed/NCBI
|