Introduction
Coronavirus disease 2019 (COVID-19) induced by
severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has
caused the current global pandemic. In the quest for combatting
this pandemic, novel drugs and therapeutic approaches for difficult
cases, as well as new outlines for clinical management have come
forth at an accelerated pace. Various therapies have been tested
(1); however, among the tools that
could halt this pandemic is the achievement of herd immunity. Herd
immunity, also known as community immunity, is reached when a large
amount of the population within a community becomes immune to a
specific disease and the infectious agent subsequently stops
spreading. Thus, the immunized population as a total group would
provide protection; not every single individual is immune to the
infection as there are also non-immunized individuals alongside
naturally or artificially immunized individuals (2). Among the means used to obtain herd
immunity, the development of effective and safe vaccines is the
most operative. Acknowledging that vaccination should commence as
quickly as possible, in July 2020, the SARS-CoV-2 panel of vaccines
included 158 vaccine candidates, out of which approximately 20 were
in the advanced stages of development namely, mRNA-based vaccines,
adenoviruses-based vaccines and pathogen-specific vaccines
(3). The vaccines which, during the
summer of 2020, were in the advanced stages of clinical testing
were based upon inactivated or live attenuated viruses, protein
sub-units, virus-like particles, viral vectors (either replicating
or non-replicating), DNA, RNA, nanoparticles, each of these types
exhibiting unique advantages (4).
Of all the vaccines that were in line for approval during the
summer of 2020, only a few of these obtained FDA and subsequent EU
approval. Therefore, the first mRNA-based vaccine (Pfizer-BioNTech)
was approved by the FDA and EMA (5,6). The
approval of the Moderna vaccine on December 18, 2020 contributed to
the list of approved vaccines for COVID-19 (7). Therefore, by February 18, 2021, almost
a dozen vaccines were authorized worldwide and up to the date of
the publication of the present study, even more may be approved and
many more will be in the pipeline of development (8).
The encounter of an organisms with the actual
SARS-CoV-2 virus triggers the appearance of specific antibodies,
but the dynamics of sero-convention is still under intense studies.
It was shown that immunoglobulin (Ig)M antibodies are detectable
around the fourth day of infection, increasing until the 20th day
when peaks, and then fads away while IgG appears around the first
week of infection and peaks around the first month (9). Nevertheless, it was shown that upon
infection seroconversion (IgG or IgM antibodies) takes place
simultaneously and the concentrations of the two types of
antibodies reach a peak value that does not vary anymore (10). Moreover, in patients with mild and
severe forms it was reported that over time the IgM titer gradually
increases (11). In
oligo-symptomatic patients, lower antibodies titers were detected
compared to symptomatic individuals in a high proportion, 40.0%
compared to only 12.9% in symptomatic patients (12). In respiratory infection, IgM and IgG
isotypes were the main immune molecules that characterize humoral
immunity, while mucosal and systemic IgA-based immune responses
received much less attention (13).
Therefore the vaccination race that begun with an
unprecedent speed still has to gather data regarding the specific
immune response raised, both from the humoral and cellular immune
arms. Acquiring specific immunity upon vaccination is the key goal
of an efficient vaccine. Although over the past year, a vast number
of studies have been published on humoral and cellular immunity in
COVID-19 patients, data regarding immunity raised by a specific
vaccine are limited. Therefore, analyzing the specific response of
antibodies upon specific vaccination, the present study aimed to
investigate the humoral immune response in a homogenous group of
healthcare providers with permanent contact with infected patients
and samples with SARS-CoV-2 that were subjected to vaccination in
the first line of defense in the Romanian population.
Materials and methods
Subjects
A total of 103 subjects were followed-up between May
2020 to February 2021. The group represents healthcare workers in
contact with SARS-Cov-2-infected patients during the present
pandemic. Out of the entire group, 69 subjects received the full
vaccination protocol and were followed-up for all three
determination - 1 day prior to vaccination, 1 day before the second
dose and 24 days after the second dose. The inclusion criteria were
as follows: Vaccination with both doses on the 6th and 27th January
2021 with Pfizer-BioNTech vaccine, no positive tests for SARS-CoV-2
infection documented by RT-qPCR test, all three blood tests (1 day
prior to vaccination, 1 day before the second dose and 24 days
after the second dose), no other disease or pregnancy during
testing. The exclusion criteria of the tested group were as
follows: Lack of vaccination in the 6 January 2021 group, lack of
one of the vaccination shots, lack of one of the blood sampling
from the three-mandatory determinations, presence of active
infection documented by standard RT-qPCR in the week prior to first
blood sampling, pregnancy, any other condition (flu, inflammatory
conditions and so on). The characteristics of the enrolled
subjects, such as age and gender are presented in Table I.
 | Table I.Demographic characteristics of the
enrolled subjects. |
Table I.
Demographic characteristics of the
enrolled subjects.
| Demographic | Previously infected
subjects, n (%) | Non-infected
subjects, n (%) | Total sample,
n |
|---|
| Subjects | 16 (23) | 53 (77) | 69 |
| Female | 14 (23) | 48 (77) | 62 |
| Male | 2
(29) | 5
(71) | 7 |
| Average age of
total, years | 37.81 | 41.00 | 40.26 |
| Average age of
women, years | 39.14 | 41.48 | 40.95 |
| Average age of men,
years | 28.50 | 36.40 | 34.14 |
Associated co-morbidities of the subjects are
presented in Table SI
(supplementary material). The group of 69 subjects were vaccinated
in January 2021 and they were followed-up before and after
vaccination for measurement of the levels of serum IgG and IgA.
During this year of follow-up, the entire group was subjected to
regular testing from nasopharyngeal swabs of SARS-CoV-2 virus using
standard RT-qPCR testing approved by EMA and FDA. Subjects were
tested regularly and/or when suspicions to be infected with
AllplexTM 2019-nCoV Assay, (Seegene Inc.). At vaccination moment,
the subjects that comprised the presented group had the most recent
disease 8 weeks prior to vaccination, while the latest documented
disease was 8 months prior to the first sampling. Prior to
vaccination, out of the entire group, 23.18% of the subjects had
gone through documented COVID-19 (proved SARS-CoV-2 infection by
RT-PCR testing).
Vaccination
All the subjects received the Pfizer-BioNTech
vaccine at the specified interval according to the supplier
instructions. As all the subjects were in the first line of defense
in the current pandemic, they received their first vaccine shot on
the January 6, 2021 and the second dose on January 27, 2021.
Dynamics of sampling
All the subjects were tested for the presence of
IgA- and IgG-specific antibodies recognizing the S1 domain of the
SARS-Cov-2 spike protein beginning from May 2020 in order to follow
their immunity upon accidental infection. Following Pfizer-BioNTech
vaccination approval, all the subjects received the vaccine. All
subjects were tested 1 day prior to vaccination, 1 day before the
second dose and 24 days after the second dose.
Blood sampling
Peripheral blood samples from subjects comprising
the tested group were collected by venipuncture during the morning
hours in blood clot activator tubes (Vacutest Kima). Blood
collection was carried out at the Colentina University Hospital.
Serum samples, separated by centrifugation (1,500 × g, 10 min at
room temperature) within 4 h of blood collection, were used for
ELISA. Serum samples were stored at −80°C for concomitant
testing.
ELISA
Anti-SARS-CoV-2 ELISA (IgG and IgA) kits was used to
determine the serum levels of specific IgG and IgA (EUROIMMUN
Medizinische Labordiagnostika AG; code EI 2606-9601A for IgA kit,
code EI 2606-9601G for IgG kit). The kits are commercially
available, EMA and FDA approved for IVD testing in SARS-CoV-2
infection. The protocol used was as per the manufacturer's
instructions. Briefly, the kits are provided with ELISA plates that
are coated with the recombinant S1 domain of the spike protein of
SARS-CoV-2 expressed in the human cell line, HEK 293. All the
reagents for developing the ELISA are provided within the kit such
as: Calibrator (human IgG, IgA, respectively), Positive control
(human IgG, IgA, respectively), negative control (human IgG, IgA
respectively), enzyme conjugate peroxidase-labeled anti-human
IgG/IgA, sample buffer, wash buffer, chromogen/substrate solution
TMB/H2O2, stop solution 0.5 M sulphuric acid,
quality control certificate.
According to the manufacturer's recommendations, the
photometric measurement was performed at 450 nm with a reference
wavelength at 620 and 650 nm, using a multi-reader platform
(Varioskan Flash; Thermo Fisher Scientific). Results were
calculated as indicated, namely the Ratio between the Extinction of
the patient sample and the Extinction of the calibrator. The
manufacturer recommends the following cut-off values: ratio
<0.8; borderline ratio ≥0.8 to <1.1; positive ratio ≥1.1. The
results are presented as indexes, as recommended by the IgG and IgA
kit supplier. When appropriate, data are presented as the mean ±
standard deviation (SD) of individual data.
Statistical analysis
We have performed repeated measures ANOVA for all
the tested groups. We applied Bonferroni post hoc test to calculate
P-values according to Bonferroni-adjusted α. GraphPad Prism 8.0
(GraphPad Software, Inc.) was used for data analysis.
Results
Dynamics of IgG and IgA antibodies
prior to vaccination
Between May to September 2020 the study group was
followed-up for the serum levels of specific IgG and IgA
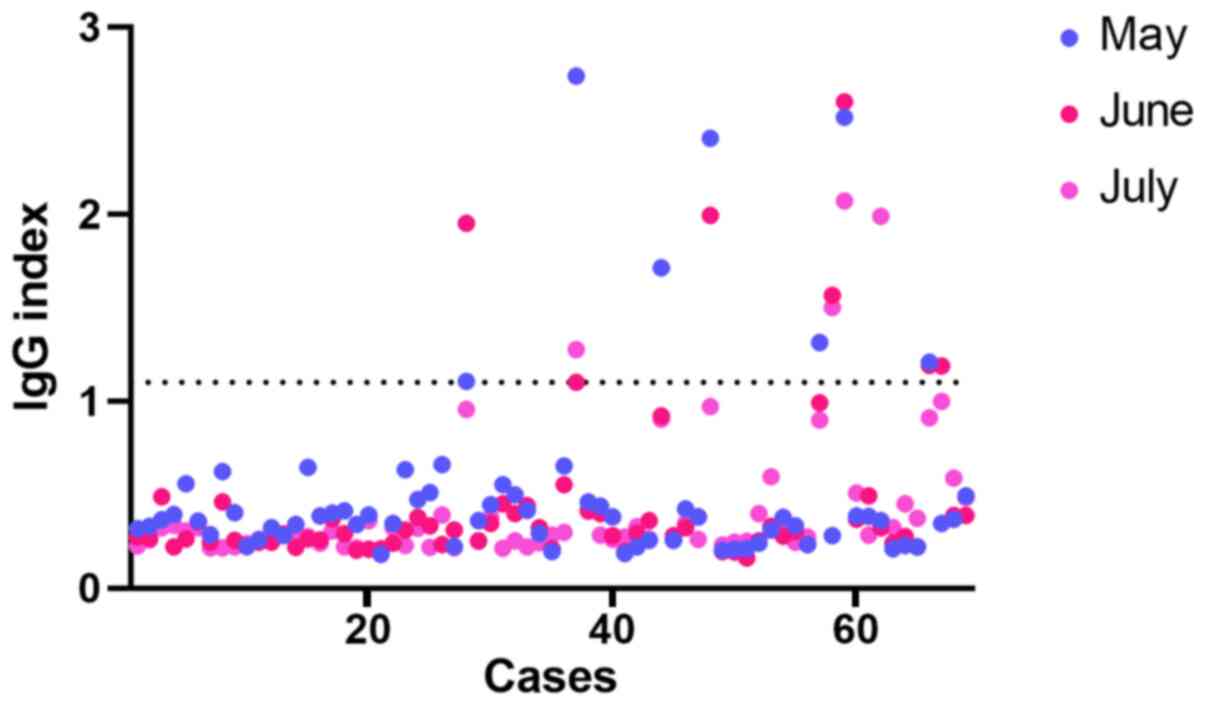
antibodies. In Fig. 1, we present
the registered dynamics for the months May-July, this snapshot
example indicates that most of the subjects had negative levels of
circulating IgG and that during the registered period, the subjects
that were infected exhibited a marked increase in the levels of
specific antibodies. The levels in convalescent healthcare workers
decreased during this time period.
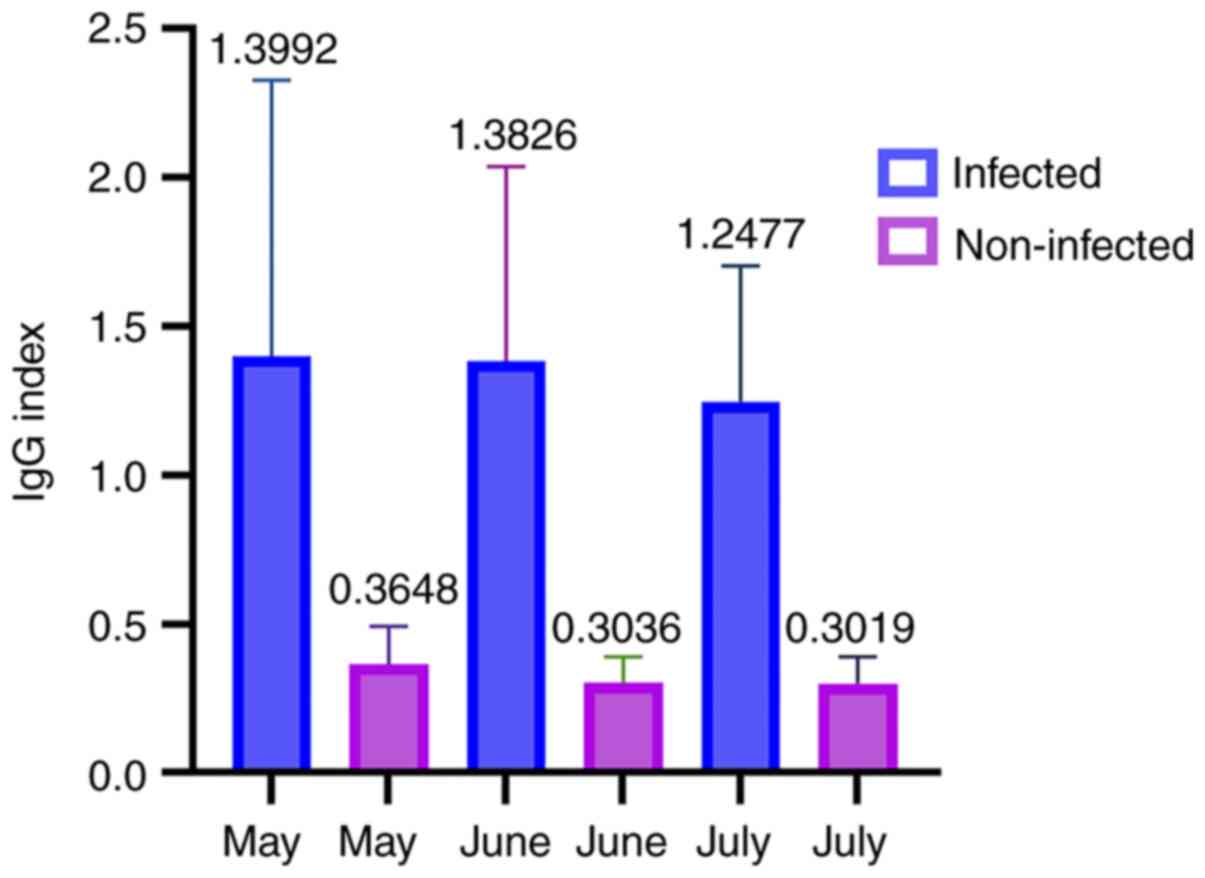
Serum IgG levels analyzed between the period of
May-September revealed the values of infected healthcare workers
during this follow-up. The mean value of the IgG index in
non-infected and infected subjects was constant during this
follow-up period and remained unaltered during these months
(Fig. 2).
Vaccination parameters
Antibodies' levels prior to
vaccination
Out of the entire study group, >23% of the
subjects were previously documented to have contracted the
SARS-CoV-2 infection during this pandemic and prior to the time of
vaccination.
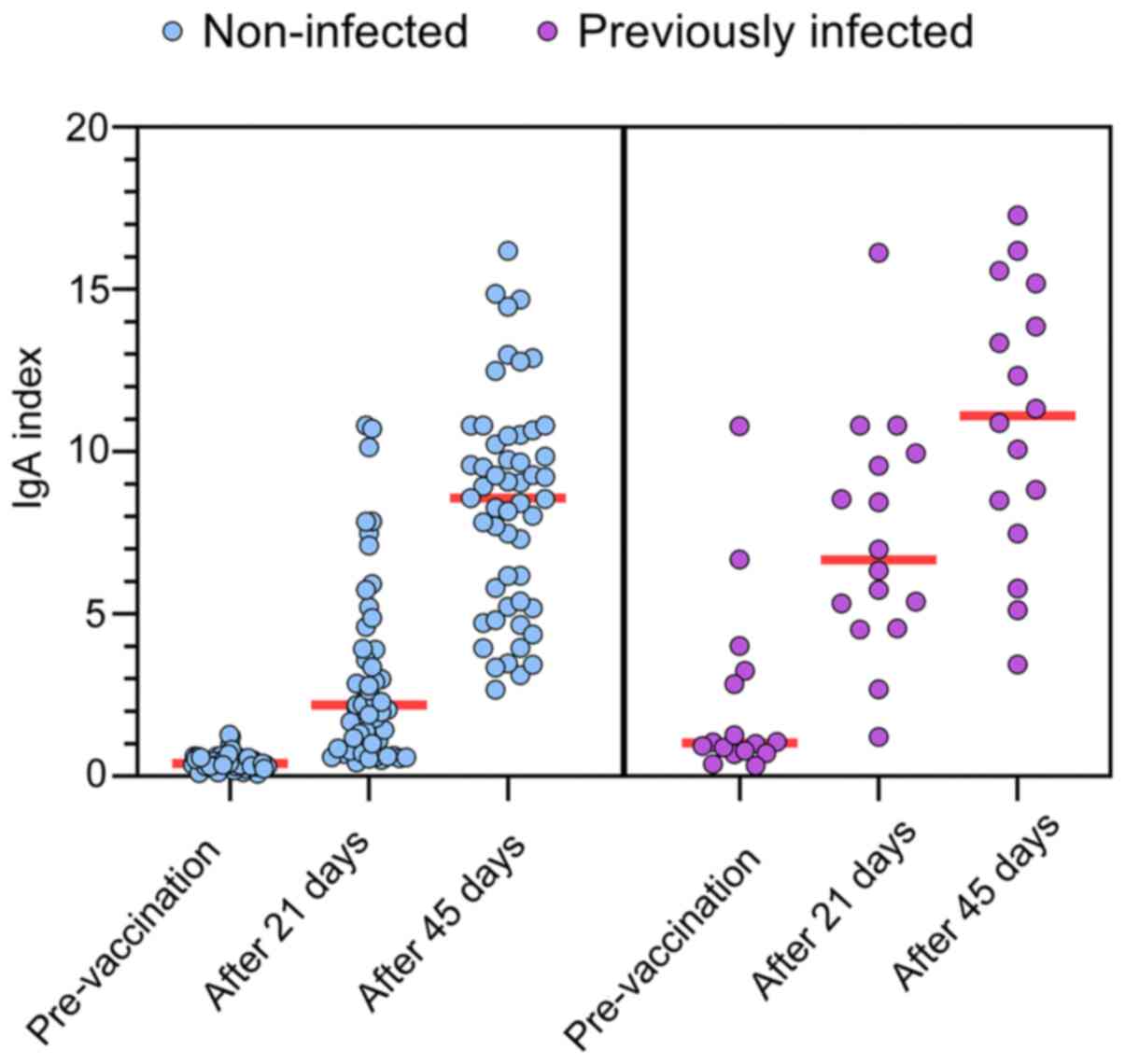
The values of both specific IgG and IgA were
significantly higher compared with the non-infected subjects prior
to vaccination (Table II). In the
non-infected subjects, the SD of the mean was low, while it was
higher in the infected subjects. The higher SD of value registered
for the antibody levels in previously infected subjects prove a
higher variability of the antibody's responses to infection due to
a specific/individual immune response and correspondingly due to
variable time from the disease onset. Owing to these statistically
significant differences, the post-vaccination dynamics are
presented separately for previously infected and non-infected
subjects.
 | Table II.IgG and IgA indexes before and after
vaccination. |
Table II.
IgG and IgA indexes before and after
vaccination.
| Index means | Non-infected
subjects, mean | Previously infected
subjects, mean | All samples,
mean |
|---|
| IgG
pre-vaccination | 0.42 |
3.02 | 1.02 |
| IgA
pre-vaccination | 0.44 |
2.29 | 0.87 |
| IgG after first
shot (21 days) | 4.03 |
6.86 | 4.69 |
| IgA after first
shot (21 days) | 3.05 |
7.31 | 4.03 |
| IgG after second
shot (45 days) | 8.13 |
9.56 | 8.46 |
| IgA after second
shot (45 days) | 8.41 | 10.95 | 9.00 |
Regardless of being in the previously infected or
non-infected group, the IgG or IgA levels prior to vaccination were
not associated with age or gender. The level of IgG was elevated
7-fold in previously infected compared with non-infected subjects,
while the IgA the level was elevated 5-fold in previously infected
compared with non-infected subjects (Table II).
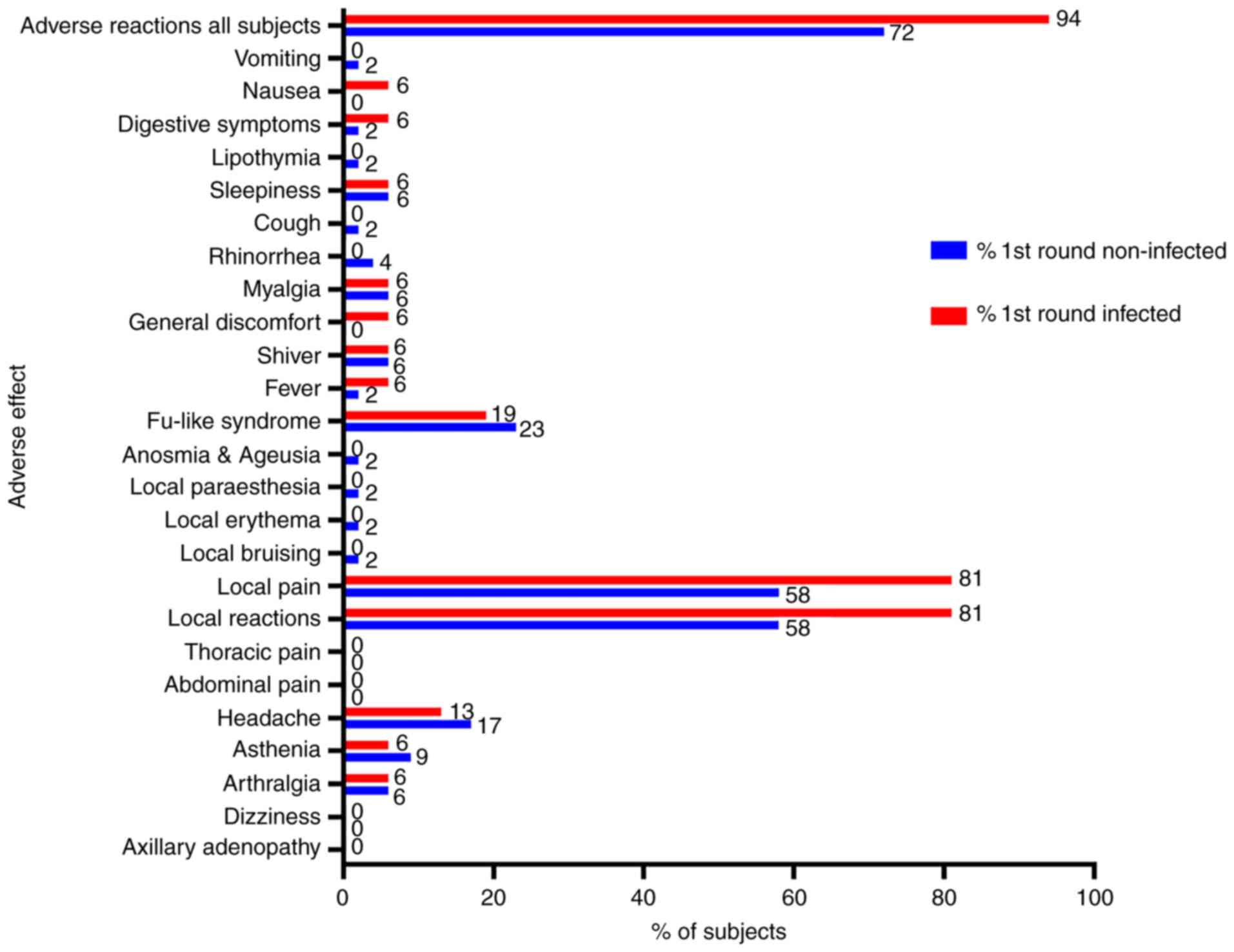
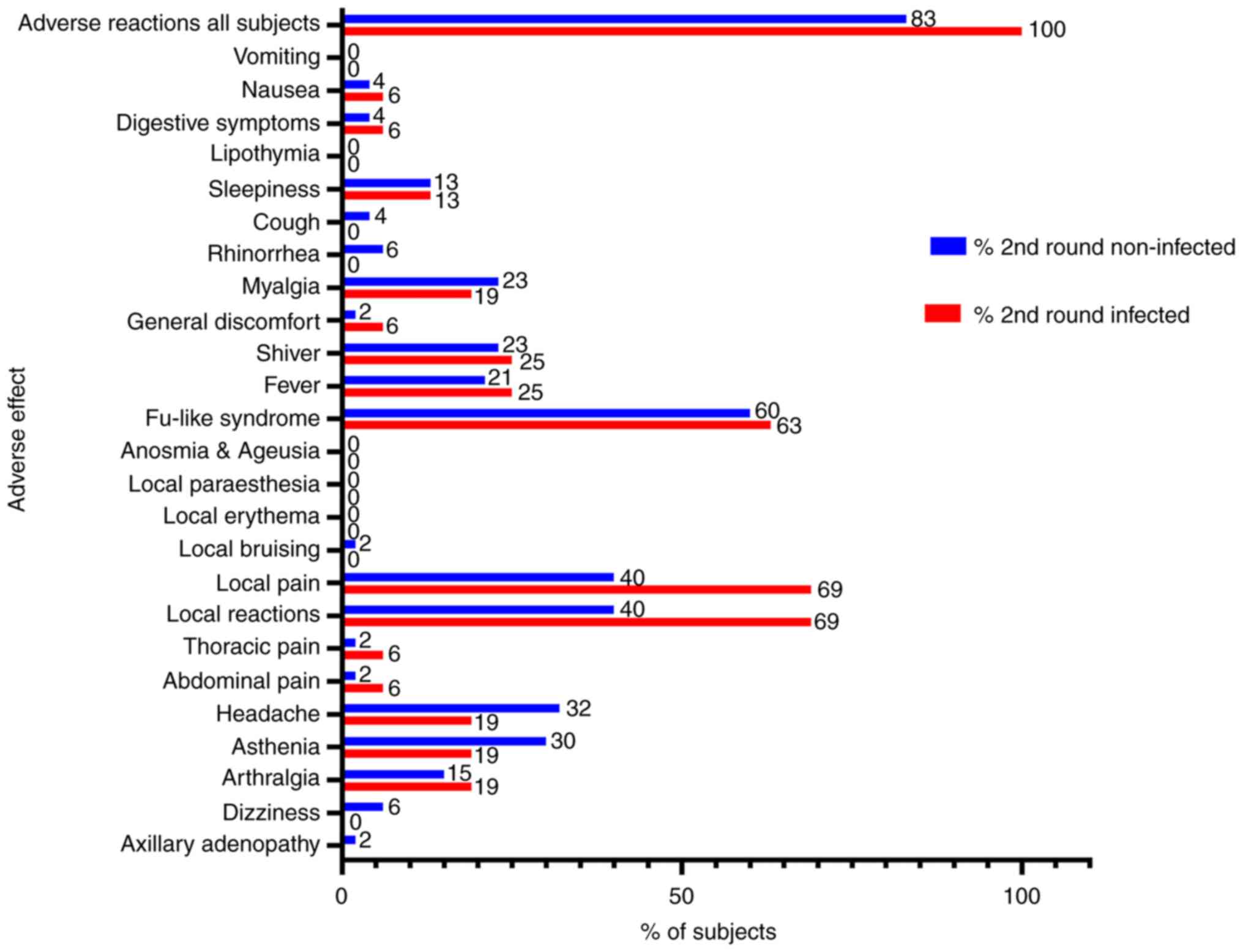
Adverse effects upon vaccination
The presence of any adverse effects was determined
upon the first and second round of vaccination for each subject.
The adverse effects and the percentage of these recorded adverse
effects within both groups is presented in Fig. 3 for the first shot and in Fig. 4 for the second one (see also
Table SII). Moreover, no
association between the presence of adverse effects with age and
gender was observed.
Of all the adverse effects, pain at the inoculation
site was present in the majority of patients in the first round
(58.49% in non-infected subjects, 81.25% of infected subjects) and
in the second round of vaccination (39.62% in non-infected
subjects, 68.75% of infected subjects). The second most common
adverse effects were flu-like symptoms reported in the first
(22.64% in non-infected subjects, 18.75% of infected subjects) and
second round of vaccination (60.38% in non-infected subjects,
62.50% of infected subjects). The rarest adverse effects recorded
were local bruising, erythema and paresthesia (one case), anosmia
and ageusia, lipothymia, cough, nausea, vomiting (one case each
after first shot), and axillary adenopathy and local bruising (one
case each after second shot). Yet, the vaccination imposed mild
adverse effects in the entire study group, with a slight increase
in the percentage of adverse effects in previously infected
subjects. The assertion was verified in both the first and second
round of vaccination. However, the adverse reactions after the
first dose of vaccination in previously infected subjects were not
similar in frequency with those noted after the second dose of
vaccination in non-infected subjects, as one would expect (i.e.,
the first dose of vaccination in subjects previously infected with
COVID-19 did not act as a ‘booster’ in SARS-Cov2 naïve subjects
considering the occurrence of adverse reactions).
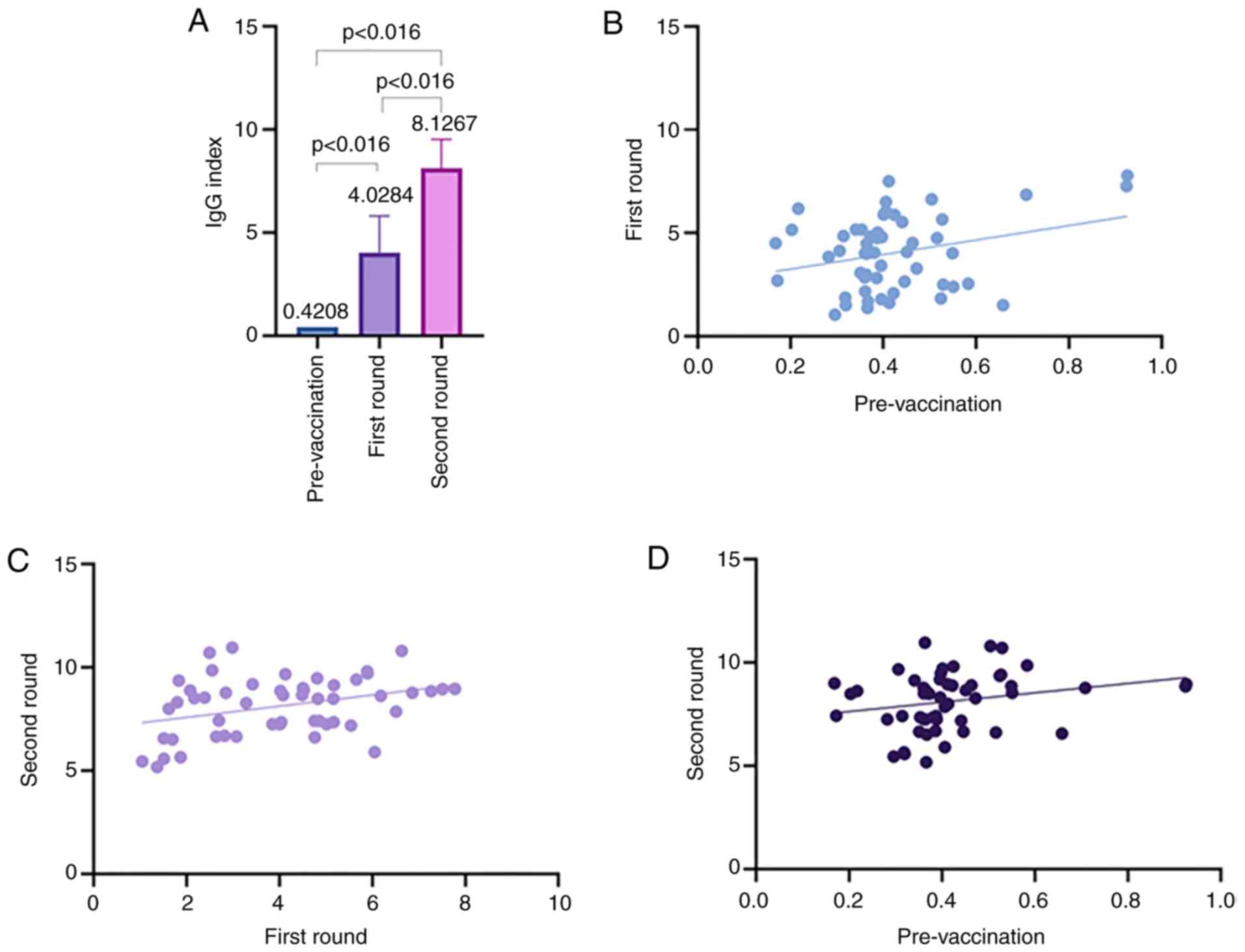
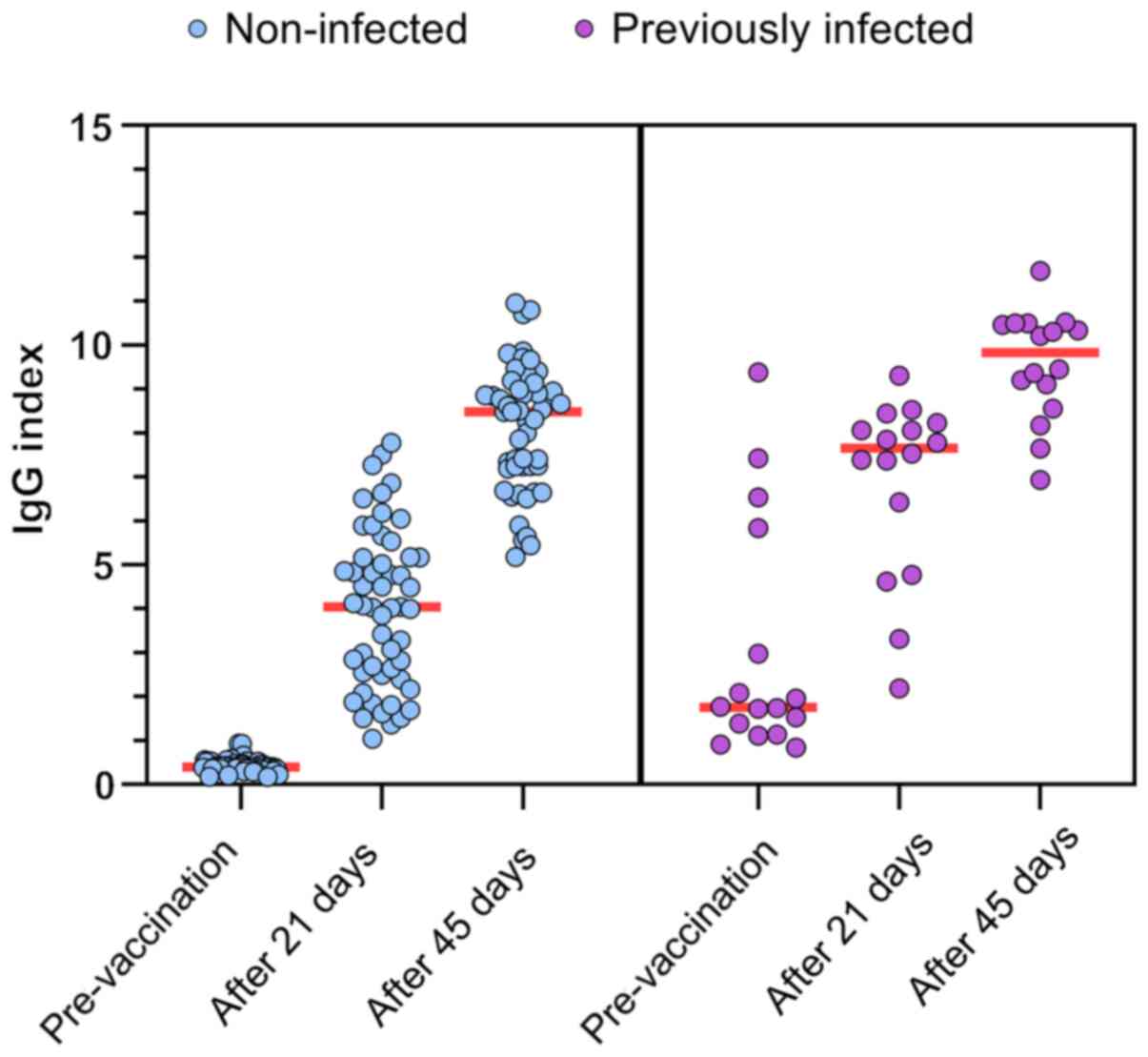
Specific IgG levels upon
vaccination
The basal level of IgG was differed significantly
between the two analyzed groups (Table
II) and the levels were elevated >7-fold in previously
infected subjects compared with non-infected ones. This clear
positive level detected in previously infected subjects (mean index
>3) indicated that upon vaccination, this group developed IgG
antibodies through disease and that vaccination led to increased
levels (Fig. 5). After the first
vaccination dose, the IgG levels in non-infected subjects exhibited
an increase of almost 12-fold increase in males and almost 11-fold
increase in females. After the second round of vaccination, the IgG
levels increased 1.33-fold in males and 2.11-fold in females, when
compared to the first dose. Although in males it seemed that the
IgG response at 21 days was higher compared with that in females,
after the second round of vaccination, the IgG serum seemed to
homogenize in both groups, proving that the generated immune
response has a plateau that is reached by all subjects. The
increase registered upon vaccination in the IgG level is
statistically different when assessed pre-vaccination versus 21
days and data after 21 days compared to registered levels after 45
days (Tables III and IV). Applying repeated measures ANOVA in
the group of naïve subjects has emphasized the results showing that
the vaccine led to statistically significant differences in IgG
level [F(2,104)=570.6139, P<0.05]. We applied Bonferroni post
hoc test and the results showed that all p-values are less than the
Bonferroni-adjusted alpha level (Table
IV).
 | Table III.Statistical out lines of repeated
measures ANOVA. |
Table III.
Statistical out lines of repeated
measures ANOVA.
| A, IgG index in the
naïve subject group |
|---|
|
|---|
| Source of
variation | SS | df | MS | F | P-value | F crit |
|---|
| Rows |
123.111261 | 52 | 2.367524 | 1.714723 | 0.010171 | 1.46636 |
| Columns |
1,575.69727 | 2 | 787.8486 | 570.6139 | 8.57E-57 |
3.083706 |
| Error |
143.5931642 | 104 | 1.380704 |
|
|
|
| Total | 1,842.401696 | 158 |
|
|
|
|
|
| B, IgG index in
the previously infected subjects group |
|
| Source of
variation | SS | df | MS | F | P-value | F crit |
|
| Rows | 57.19408843 | 15 | 3.812939 | 1.966985 | 0.100866 | 2.403447 |
| Columns | 57.99053419 | 1 | 57.99053 | 29.91563 | 6.46E-05 | 4.543077 |
| Error | 29.07703675 | 15 | 1.938469 |
|
|
|
| Total | 144.2616594 | 31 |
|
|
|
|
|
| C, IgA index in
the naïve subject group |
|
| Source of
variation | SS | df | MS | F | P-value | F crit |
|
| Rows |
448.4025381 | 52 | 8.623126 | 1.702135 | 0.011067 | 1.46636 |
| Columns | 1,748.404978 | 2 | 874.2025 | 172.5605 | 9.18E-34 |
3.083706 |
| Error |
526.8706159 | 104 | 5.066064 |
|
|
|
| Total | 2,723.678132 | 158 |
|
|
|
|
|
| D, IgA index in
the previously infected subjects group |
|
| Source of
variation | SS | df | MS | F | P-value | F crit |
|
| Rows |
393.3714199 | 15 | 26.22476 | 5.42375 | 0.001118 | 2.403447 |
| Columns |
105.9619832 | 1 | 105.962 | 21.91483 | 0.000295 | 4.543077 |
| Error |
72.52757384 | 15 | 4.835172 |
|
|
|
| Total |
571.860977 | 31 |
|
|
|
|
 | Table IV.Bonferroni post hoc test (Bonferroni
corrected) 0.0166667 analysis of the repeated measures ANOVA
results. |
Table IV.
Bonferroni post hoc test (Bonferroni
corrected) 0.0166667 analysis of the repeated measures ANOVA
results.
| A, IgG index in the
naïve subject group |
|---|
|
|---|
| Group | P-value
(t-test) | Significant |
|---|
| Pre-vaccination vs.
After 21 days | 4.11859E-27 | Yes |
| After 21 days vs.
After 45 days | 5.80142E-24 | Yes |
| Pre-vaccination vs.
After 45 days | 3.97412E-65 | Yes |
|
| B, IgG in the
previously infected subjects group |
|
| Group | P-value
(t-test) |
Significant |
|
| Pre-vaccination vs.
After 21 days | 8.16202E-05 | Yes |
| After 21 days vs.
After 45 days | 9.77281E-05 | Yes |
| Pre-vaccination vs.
After 45 days | 7.73566E-10 | Yes |
|
| C, IgA index in
the naïve subject group |
|
| Group | P-value
(t-test) |
Significant |
|
| Pre-vaccination vs.
After 21 days | 4.15878E-10 | Yes |
| After 21 days vs.
After 45 days | 1.00589E-14 | Yes |
| Pre-vaccination vs.
After 45 days | 2.4916E-32 | Yes |
|
| D, IgA index in
the previously infected subjects group |
|
| Group | P-value
(t-test) |
Significant |
|
| Pre-vaccination vs.
After 21 days | 0.000151896 | Yes |
| After 21 days vs.
After 45 days | 0.013922345 | Yes |
| Pre-vaccination vs.
After 45 days | 1.33505E-07 | Yes |
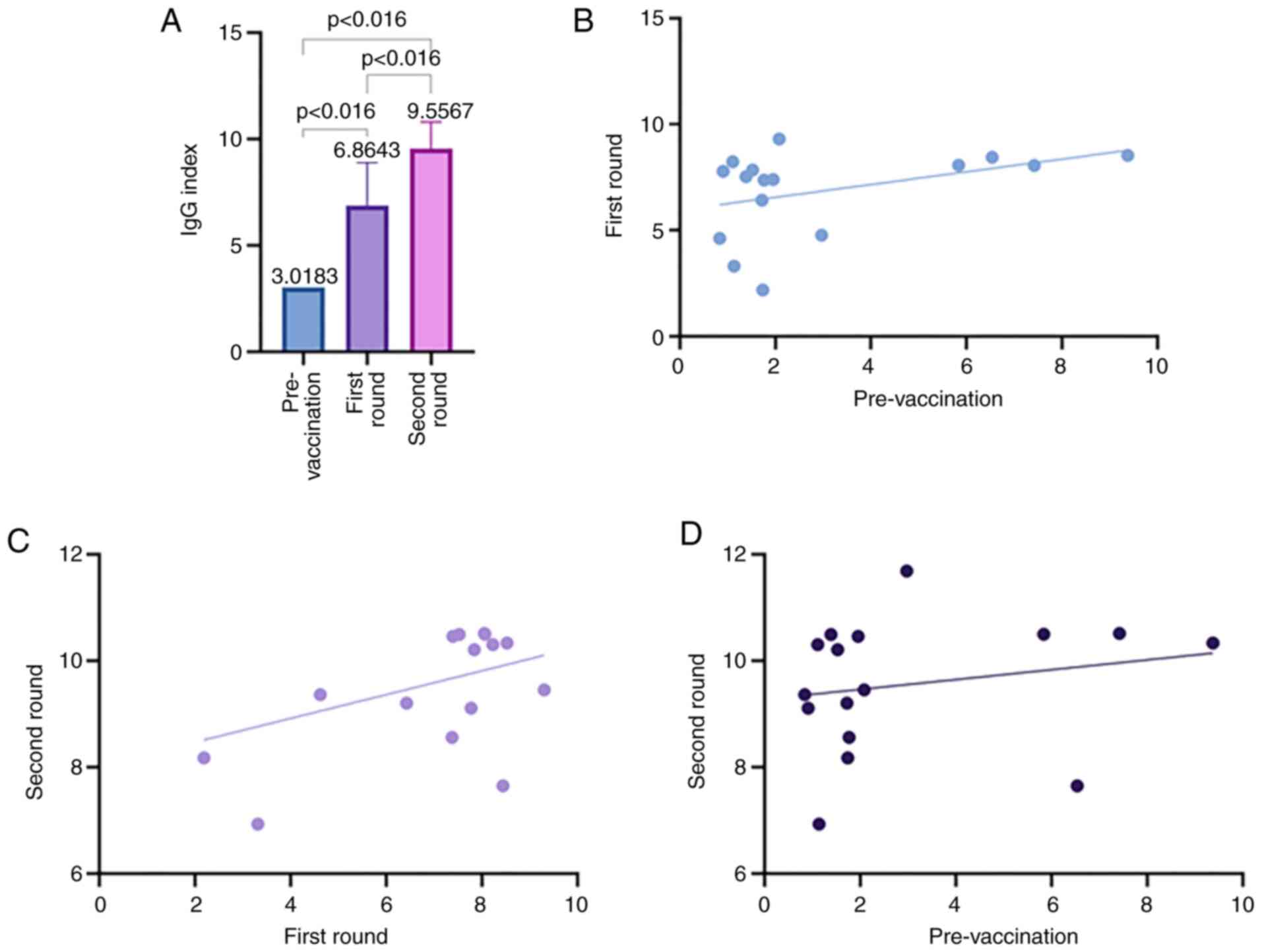
In previously infected subjects subjected to
vaccination (Fig. 6) we have
registered after the first vaccination dose, an increase of
2.47-fold in males and 2.25-fold in females. After the second dose,
an increase of 1.82-fold was observed in males and one of 1.33-fold
in females. The overall vaccination procedure seemed to increase
the levels of IgG in both males and females in previously infected
subjects in comparison with uninfected subjects. The increase
registered upon vaccination in the prior infected subjects in the
IgG level is statistically different when assessed pre-vaccination
versus levels after 21 days and IgG levels after 21 days compared
to the 45 days registered levels (Fig.
6). The data of the groups come from the same individuals
followed as indicated above and the dispersion of individual IgG
indexes for each subject at moments of pre-vaccination, after 21
days and 45 days is presented in Fig.
7. In infected group, applying repeated measures ANOVA has
shown that the vaccine induced statistically significant
differences in IgG level [F(1,15)=29.91563, P<0.05] and
Bonferroni post hoc test emphasized all p-values as less than the
Bonferroni-adjusted alpha level (Table
IV).
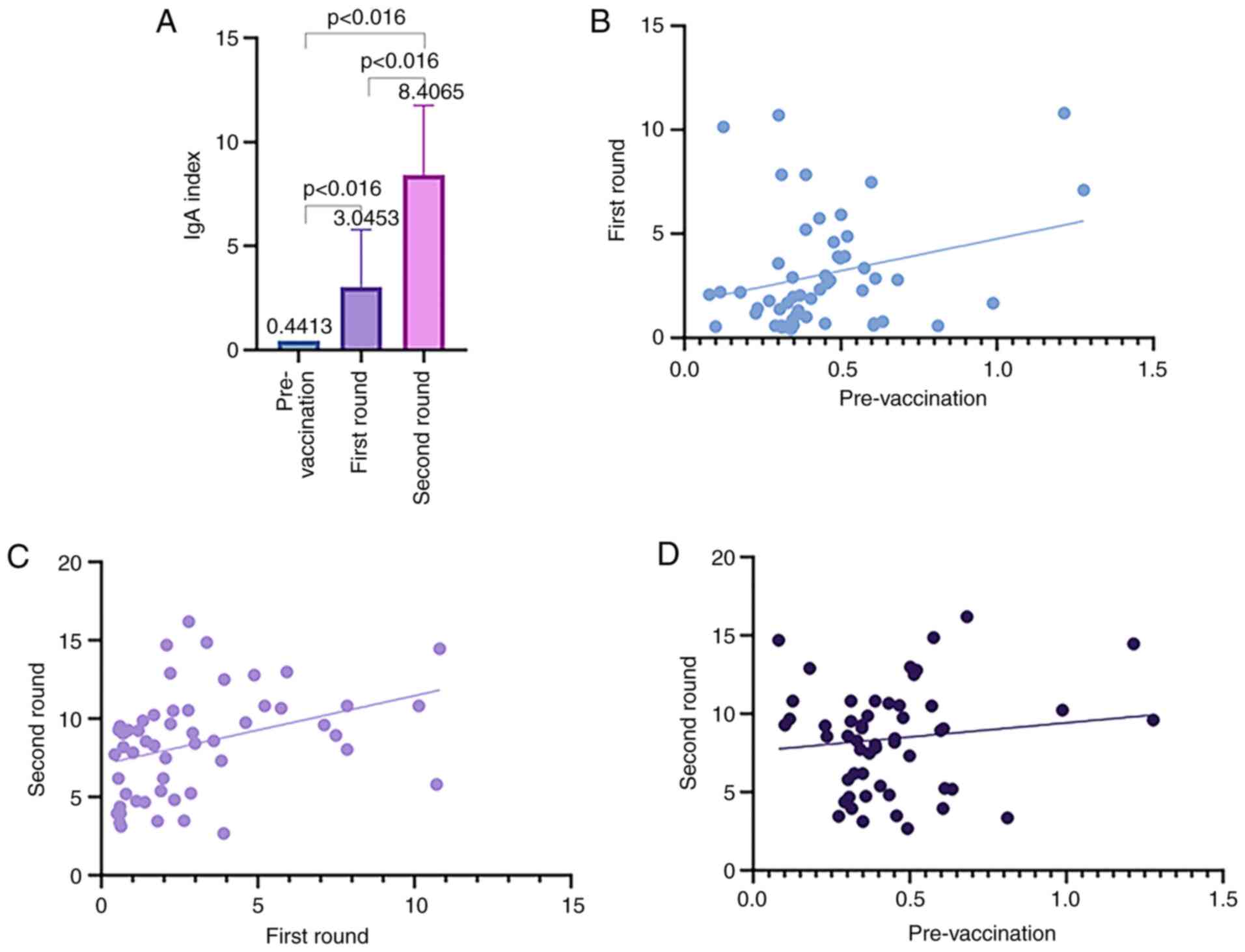
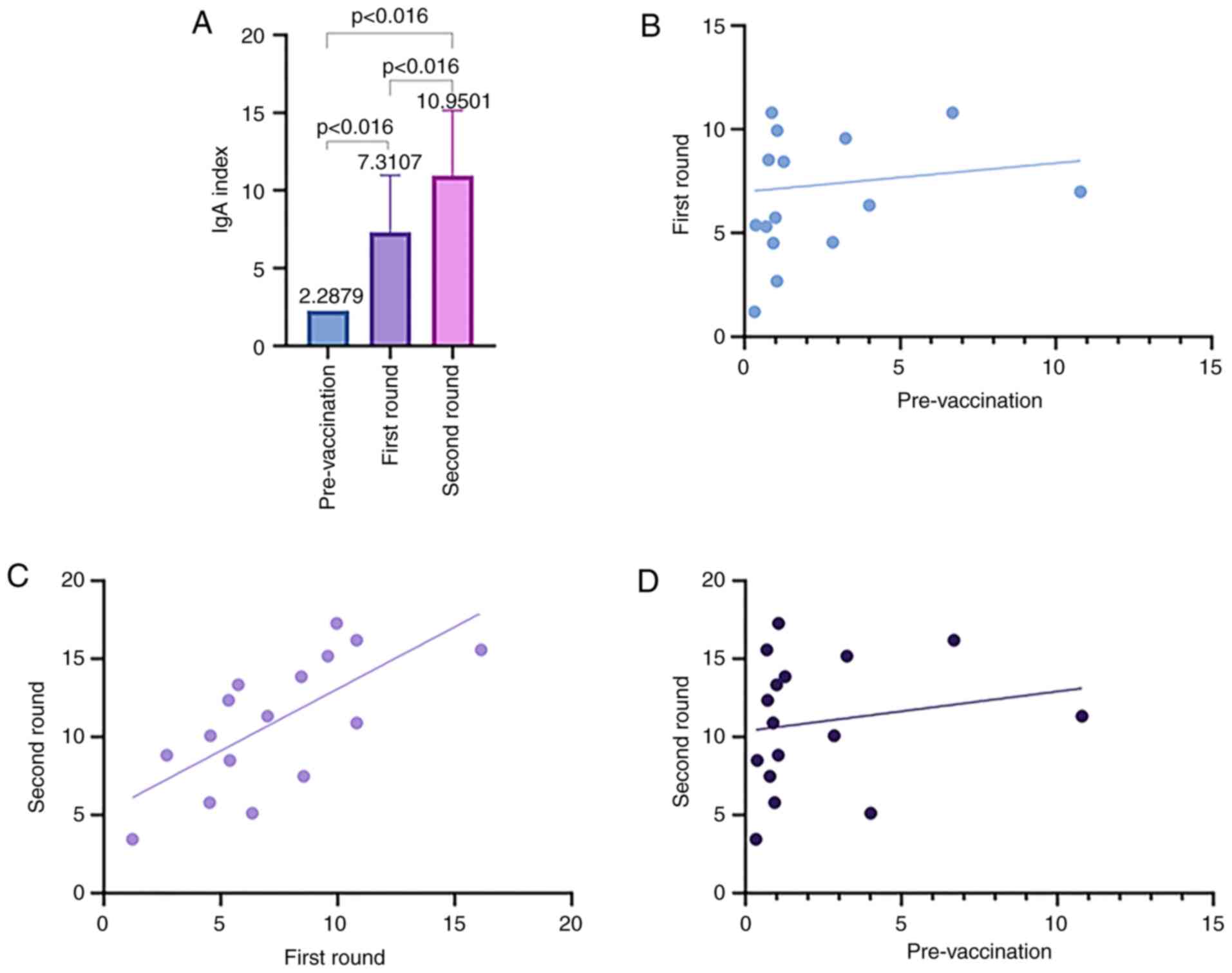
Specific IgA levels upon
vaccination
Similar to the serum levels registered for IgG, the
levels registered for IgA differed between the two groups. These
levels were elevated >5-fold in previously infected subjects
compared with naïve ones (Table
II). In the non-infected (naïve) subjects, upon the first
vaccination dose, the level of IgA (Fig. 8) seemed to be lower compared with
the level of IgG in the same subjects. When applying statistics in
naïve subjects for IgA levels, similar differences were found in
comparison to IgG levels. Therefore, repeated measures ANOVA has
shown that the vaccine induced statistically significant
differences in IgA level [F(2,104)=172.5605, P<0.05] and
Bonferroni post hoc test emphasized all p-values as less than the
Bonferroni-adjusted alpha level (Tables III and IV).
In the previously infected group, the first
vaccination dose induced a higher level of IgA compared with the
level of IgG in the same subjects. In the non-infected group, after
the second vaccination dose, the IgA levels increased compared with
the IgG levels.
While in non-infected subjects' females and males
seem to have a similar increase of IgA, after the second round of
vaccination, the mean value obtained in male subjects is increased
compared to females. In the prior infected group, the first dose
increases the IgA level similar in females and males (3.19 times in
females and 3.21 times in males, respectively). The second dose
induces the highest registered levels in both males and females at
similar levels (Fig. 9). Similar to
the IgG levels, in the IgA case the dispersion of individual
distribution of IgA indexes for each subject at moments of
pre-vaccination, after 21 days and 45 days is presented in Fig. 10. In previously infected subjects
repeated measures ANOVA has shown that the vaccine induced
statistically significant differences in IgA level
[F(1,15)=21.91483, P<0.05] and Bonferroni post hoc test
emphasized all P-values as less than the Bonferroni-adjusted alpha
level (Tables III and IV).
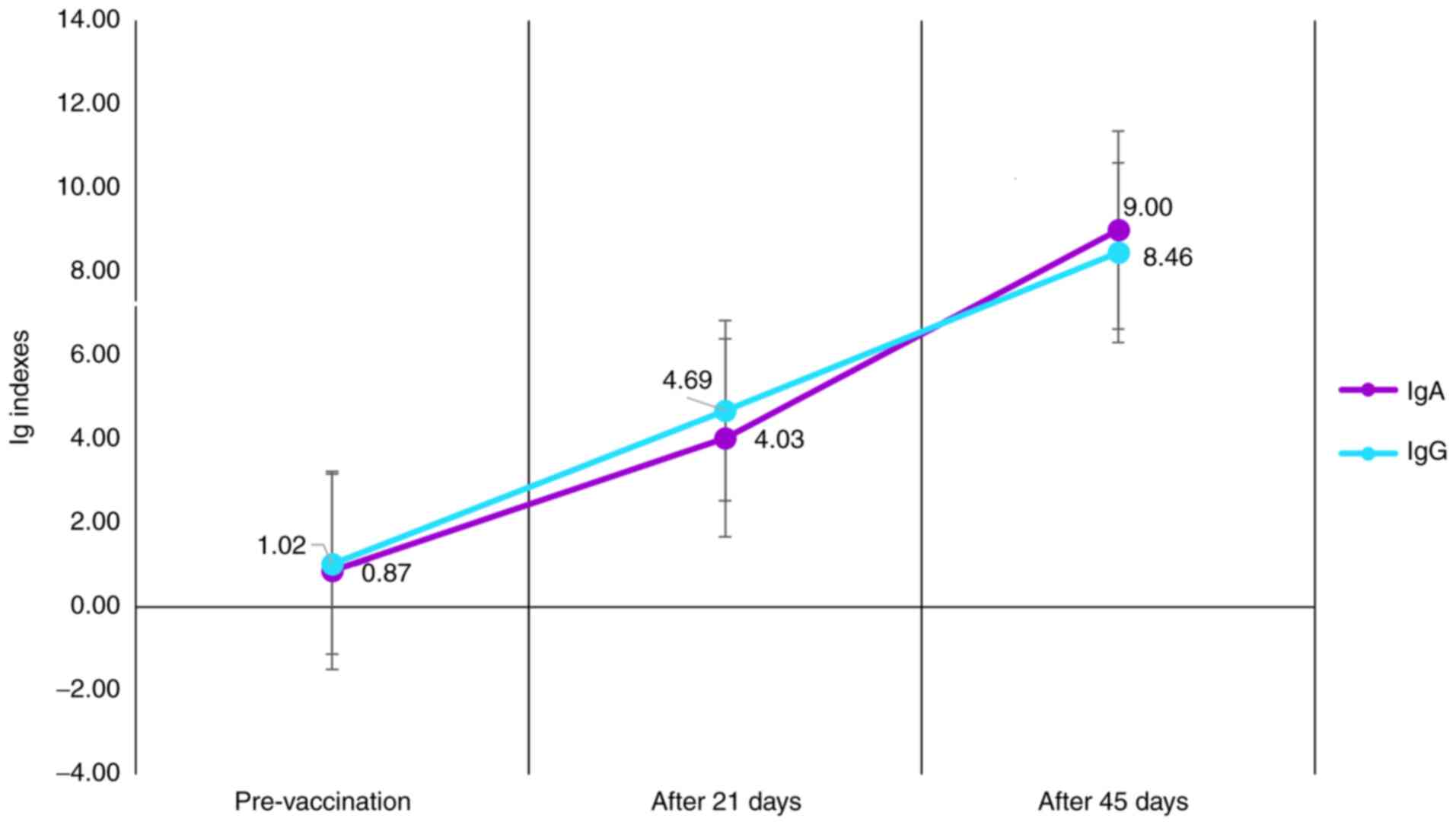
The associations between the IgG and IgA levels upon
the first and second dose of vaccination indicated that in the
entire vaccination group, regardless of prior exposure to the
infectious agent, the increment and levels of IgG and IgA were
similar (Fig. 11). Therefore, the
levels upon vaccination were statistically similar regardless of
the starting baseline prior to vaccination (Tables III and IV).
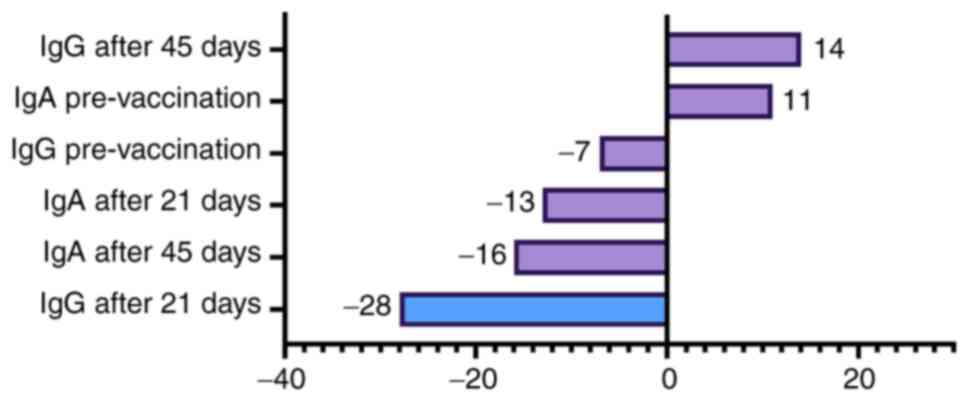
When analyzing all possible associations, the most
significant one was the IgG index after the first dose that induced
an antibody response in naïve (non-infected) subjects <28% in
females compared with males (Fig.
12). A possible explanation for this difference, as previously
demonstrated by us (14) and other
groups (15), is the
hormone-dependent immune response that induces different antibody
dynamics. Moreover, even the clinical outcome of COVID-19 was
recently reported as correlated with gender (16).
In the present study, seroconversion was achieved in
98.5% of subjects after the first dose for IgG and 81% for IgA, and
in 100% of the entire group after the second dose with highly
similar antibody levels.
Discussion
Up to date there are several approved vaccines that
are already applied into the vaccination protocols along with the
one that was analyzed herein. Another mRNA-based vaccine developed
by Moderna has shown in the NCT04470427 trial tests that is capable
to develop specific antibodies (17,18).
Another type of vaccine that is as well applied on a large scale
(AZD1222) has a different design than the mRNA-based vaccines.
AZD1222 is based on the replication-deficient simian adenovirus
vector ChAdOx1, containing the gene of S glycoprotein. This vaccine
was shown to induce antibodies in vaccinated subjects (19). Therefore, the COVID-19 vaccines that
are on large scale application around the world seem to induce the
intended specific immune response. Questions still remain to be
answered regarding how long this immunity will offer protection and
if the new variants that are appearing would be neutralized by the
antibodies raised to these vaccination platforms. It seems that, at
least for the time being, data indicate that these vaccines induce
a significant increase in binding antibodies to spike protein of
SARS-CoV-1, MERS, and to the four common coronaviruses, currently
circulating in the UK. Therefore, there are good news in terms of
the specific immune response that can fight also other viral
variants and possibly the newly emergent ones (20).
Over the past year, almost 300 studies have become
available in the PubMed database focusing on humoral and cellular
immunity in COVID-19 patients; however, to the best of our
knowledge, there are a handful of reports focusing on the real-case
scenario upon vaccination. We have learned some lessons from
investigating the immunity of infected patients. Therefore, upon
disease high titers of specific IgG levels with serum-neutralizing
viral potency in a pseudo-type entry assay were reported (21). Moreover, a strong correlation was
found between antibody titers and the percentage of virus-specific
T cells (22). Research on
seroprevalence has revealed that seropositive samples were found as
early as mid-February, and our results obtained during the summer
of 2020 have shown that seroprevalence is stable, suggesting
lasting antibody serum levels in subjects as obtained by another
group (23). We have chosen ELISA
testing because most serological studies embrace the quantitative
ELISA platform (24). The ELISA
test that we have used (EUROIMMUN Anti-SARS-CoV-2 ELISA Assay) was
evaluated, validated and it is comprised in the FDA recommended
lists of immunoassays to be used in current pandemia. This type of
analysis has proven to have good sensitivity for the detection of
IgA and excellent sensitivity for the detection of IgG, as early as
≥4 days after the diagnosis of COVID-19 by RT-PCR, with no
cross-reactivity to common human coronaviruses infection, types
NL63 and OC43 (25). In the present
study, seroconversion was achieved in 98.5% of subjects after the
first dose for IgG and 81% for IgA, and in 100% of the group after
the second dose, with highly similar antibody levels; these results
were similar to those of a recent report on a small, vaccinated
group of oncological patients (26).
The fact that the specific IgG level followed the
level of IgA is proof that the generated immune response upon
vaccination stimulates multiple B lymphocyte clones. Moreover,
previously infected subjects exhibited both IgG and IgA levels,
detectable even after 8 months post-infection, as we evidenced in
the present study group with one case exhibiting positive antibody
levels after 8 months. Our results are in accordance with the
reported humoral immune response to SARS-CoV-2 infection that shows
an early response of IgA, instead of IgM (27).
Gender association with the post-vaccination level
revealed no association, as no associations were observed with the
degree of adverse effects and prior encounters with the viral
agent. Even though the presence of adverse effects seemed a bit
higher in the subjects that experienced the disease in comparison
to naïve subjects. We do not rule out that a larger group of
subjects would have unveiled statistical differences associated
with age and gender. Similar results showed that in a cohort of the
same vaccine recipients post-vaccine symptoms were more prominent
for prior infected subjects after the first dose, but overall
symptomology was similar between groups after the second dose
(28).
For subjects that still had positive levels of IgG
and IgA occurring after infection, the levels at the first dose and
second dose were slightly increased compared with the ones
registered in uninfected subjects. Results reported in April 2021
have shown that specific IgG antibody levels elicited by a single
vaccine dose in prior SARS-CoV-2 infected subjects were similar to
those seen after two doses of vaccine in individuals without prior
infection (28). In a nested
case-control analysis within COVIDsortium (51 participants),
a study performed in health-care workers showed that after the
first dose of the Pfizer-BioNTech vaccine, the prior infected
subjects vaccination increased total antibodies more than 140-fold
in comparison to their pre-vaccine levels (29).
Although the most tested antibodies panel in
COVID-19 disease is represented by the IgG and IgM pair, assessing
circulating IgA levels could provide useful insight into the
humoral immunity course developed in both patients who were
previously infected and those who were vaccinated. IgA represents
the most abundant antibody class produced in humans, being critical
in the first line of antimicrobial defense, by neutralizing
pathogens targeting the mucosal boundary (30). IgA comprises different subclasses
(IgA1/IgA2) and/or isoforms (monomeric, dimeric/secretory). While
the IgA circulating form is predominantly monomeric IgA1 (85%) and
considered as an anti-inflammatory isotype, the dimeric/secretory
IgA exhibits both pro- and anti-inflammatory actions (31).
Both circulating and secretory IgA levels present
certain distinct features; thus, IgA from serum/plasma originates
mainly from bone marrow-derived plasma cells and typically includes
the monomeric form, namely IgA1. By contrast, IgA located in mucosa
comprises both isoforms, IgA1 and IgA2 being produced by plasma
cells located in the lamina propria of mucosal surfaces (32).
Even though IgA delineates the humoral immunity
profile at the mucosal level, it is insufficiently exploited to
wholly outline the immune response in the COVID-19 disease context
and is almost ignored in post-vaccination studies. Testing serum
IgA-specific antibodies in both infected and therefore, in
vaccinated subjects is of particular interest since the role and
function of IgA in SARS-Cov-2 infection remains uncertain. In
addition, both serum and salivary IgA antibody responses have been
registered to SARS-CoV-2 spike antigens (33).
The assessment of circulating IgA antibodies in
COVID-19 is of equal importance as IgG testing, in order to clarify
mostly the asymptomatic and mild cases that typically represent
COVID-19 infections (32).
To date, to the best of our knowledge, no data are
available regarding IgA circulating levels in vaccinated subjects,
and very few in different COVID-19 forms (27). Experience obtained from one year of
the COVID-19 pandemic has revealed that SARS-CoV-2-blood IgA
occurrence requires an average seroconversion period of 2–5 days
following symptom onset (34), and
it is attributed to an early action in SARS-CoV-2 infection, being
even more potent than IgG in neutralizing SARS-CoV-2 (35). Regarding the remanence of IgA in
blood, a recent study suggested that the durability of the
circulating anti-spike IgA was even up to 8 months following
SARS-CoV-2 infection (36). The
authors also observed, in the oldest infected subject, that the
levels of IgG and circulatory IgA maintained their positivity.
The potency of serum IgA versus IgG in SARS-Cov-2
infection was recently reported to be associated with the
monomeric/dimeric state of IgA. Namely, the serum monomeric IgA is
typically two-fold less effective than IgG, while the dimeric IgA
from the mucosal level is significantly more potent than monomer
IgA in neutralizing SARS-CoV-2 (37).
When analyzing the data of IgG indexes in subjects
with a previous SARS-Cov-2 infection versus subjects without COVID,
several hypotheses have emerged. Vaccination induces higher levels
of IgG after the first dose of vaccination in not infected subjects
(IgG mean index, 4.03) in comparison to the basic levels obtained
by subjects through natural immunization (IgG mean index, 3.02).
The vaccination of individuals with COVID-19 prior to immunization
must be recommended, since the increase in IgG levels is 33% higher
in ‘non-COVID’ subjects compared to the IgG levels obtained by
natural immunization. The vaccination of previously infected
subjects with the first dose induces antibody responses slightly
lower (IgG mean index, 6.86) than those recorded after the second
dose of vaccine in ‘non-COVID’ subjects (IgG mean index, 8.13).
Non-infected subjects have IgG indexes with 21.13% higher after the
second shot compared to previously infected subjects after the
first shot. The vaccination of subjects that have experienced the
disease with the second dose further increases their IgG levels
(IgG mean index, 9.56) by up to 40% (39.35% compared with the IgG
levels after first dose) and by 17.58% compared with the IgG levels
after the second dose in naïve subjects. Based on this finding, the
need for a second shot of the vaccine can be debated in subjects
infected with COVID-19 prior to vaccination. The humoral immune
response with the capacity to protect against disease obtained
after the first vaccination shot in these subjects is excellent,
however, a second shot has the capacity to augment it. Perhaps,
considering these findings, in the context of the lack of a
sufficient vaccine doses worldwide, one might consider an extension
of the time period between the first and second dose of the vaccine
for subjects with previously SARS-CoV-2 infection.
Similarly, as in the case of the discussions
regarding the IgG levels, the findings for the IgA levels can have
some original points that should be outlined. Since IgA is involved
mainly in local protection, its levels may be associated with
capacity of transmission. Vaccination also induced higher levels of
IgA after the first dose in naïve subjects (IgA mean index, 3.05)
than basal levels obtained in previously infected subjects (IgA
mean index 2.29). To be pointed out that the IgA basal levels of
previously infected subjects is high, although, as mentioned, in
this sub-group of subjects we have individuals that recovered from
the disease even as old as 8 months ago. The increase in the IgA
levels in non-infected subjects was 33.18% higher than the levels
obtained by natural immunization. Vaccination with the first dose
in previously infected subjects induced an IgA response slightly
lower (IgA mean index, 7.31) than those recorded after the second
dose of vaccination in naïve subjects for IgG (IgG mean index,
8.41). However, the increase in IgA levels in non-infected subjects
after the second shot versus subjects with previous infection after
first shot was lower than that of IgG (with 15.04%). The
vaccination of previously infected subjects with the second dose
markedly increased the IgA levels (IgA mean index, 10.95) by almost
half (increase with 49.79%) compared with the IgA levels after the
first dose and by 30.20% compared with the IgA levels in naïve
subjects after the second dose. Considering the risk of developing
COVID-19 after complete vaccination with two shots and implicitly
the risk of further dissemination of infection, the second
vaccination shot in previously infected subjects induced a potent
IgA response that may provide supplementary protection against
transmission.
We are pointing out that serology testing is
important prior to vaccination to analyze quickly the humoral
immune status of the subject, so that the following vaccination
protocol could be adapted. The same conclusion was published in
March 2021 by Manisty et al, stating that this testing can
induce a prioritization use of the Pfizer booster doses for
individuals that did not experience the disease. This approach
could accelerate vaccination and, facing new virus variants (UK,
South Africa, Brazil), achieving herd immunity quickly, stopping
the spreading and hindering new variants emergence (38).
The present study has some limitations regarding the
monitored specific response. Although antibody-mediated immunity
was followed, the understanding of cellular immunity upon
vaccination in this group could have revealed additional aspects.
Studies published at the end of 2020 have shown that in the phase
I/II trial in healthy adults receiving this type of vaccine after
two doses elicited robust CD4+ and CD8+ T
cell responses in correlation with strong IgG responses, levels
that were found increased in comparison to individuals
post-COVID-19 (39). Thus, in our
study, a focus on cellular immunity, namely memory B and T cells
would have broadened the investigation regarding the vaccination
outcome. Another limitation of our study is that direct
neutralizing antibodies would have pin-pointed the actual efficacy
of vaccination. Of note, during the follow-up period in the present
study, immunized subjects did not become re-infected, although in
some cases, close un-vaccinated family members developed the
infection. In a preliminary study published in March 2021 regarding
neutralizing antibodies induced by the same vaccine has shown that
neutralizing antibodies concentrations post-vaccination are
superior from those observed among COVID-19 human convalescent
serum (40). Another limitation of
the study is the low number of participants. This limitation is
surmounted by the fact that the group is thoroughly investigated
and monitored through-out this pandemic regarding co-morbidities,
side effects of vaccination and the overall evolution of their
health during a possible infection and post-infection. All these
clinical data are somewhat difficult to be obtained from large data
bases.
The present study aimed to analyze the profiles and
dynamics of immunization raised through vaccination between a
homogenous group of healthcare workers, and thus to create a
clear-cut tool which may be used to assess the intensity and
duration of humoral immunity comprising specific antibodies (IgG
and IgA) to key proteins from SARS-CoV-2 (e.g., Spike protein). The
authors aim to perform further studies, analyzing antibody
persistence and the presence of memory immune cell populations.
Indeed, the whole picture of anti-SARS-Cov-2 immunity, and the
post-vaccination status in particular, should encompass both
humoral and cellular immunity corroborated parameters. However, the
methods through which these humoral immunity figures could be
extrapolated to evaluate the infection ‘mimicked’ by vaccination
remain to be determined.
In conclusion, far from being an exhaustive study on
vaccination, the present study has evaluated, in a homogenous
healthcare workers group, the antibody levels prior and
post-vaccination. It was demonstrated that the vaccine induced high
levels of specific IgG and IgA in all the tested subjects. The
vaccine induced levels of antibodies that were statistically
equivalent regardless of the prior infection. In the present study,
seroconversion was achieved in 100% of the group for both tested
antibodies after vaccination protocol completion with highly
similar antibody levels.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was supported by the Executive
Agency for Higher Education, Research, Development and Innovation
(UEFISCDI; grant no. PN-III-P1-1.2-PCCDI-2017-341/2018) and the
Core Program, with the support of NASR, project PN no.
19/29.01.01.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SZ, LN, CM, CC and MN contributed to the study
design, data collection, statistical analysis, data interpretation
and manuscript preparation. MC and CP contributed to data
collection and statistical analysis. AB, BM and CS contributed to
data collection, statistical analysis and manuscript preparation.
SZ, LN, BM, CS and MN confirmed the authenticity of all the raw
data. All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Colentina University Hospital (approval no. 25/2017)
and performed according to the Declaration of Helsinki. Written
informed consent was provided by all patients prior to the study
start.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Constantin C, Neagu M, Diana Supeanu T,
Chiurciu V and A Spandidos D: IgY - turning the page toward passive
immunization in COVID-19 infection (Review). Exp Ther Med.
20:151–158. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Neagu M: The bumpy road to achieve herd
immunity in COVID-19. J Immunoassay Immunochem. 41:928–945. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
World Health Organization (WHO), .
COVID-19 vaccine tracker and landscape. WHO; Geneva: 2020,
https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccinesJune
8–2021
|
|
4
|
Kaur SP and Gupta V: COVID-19 vaccine: A
comprehensive status report. Virus Res. 288:1981142020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tauzin A, Nayrac M, Benlarbi M, Gong SY,
Gasser R, Beaudoin-Bussières G, Brassard N, Laumaea A, Vézina D,
Prévost J, et al: A single BNT162b2 mRNA dose elicits antibodies
with Fc-mediated effector functions and boost pre-existing humoral
and T cell responses. bioRxiv. doi: 10.1101/2021.03.18.435972
(Preprint).
|
|
6
|
Oliver SE, Gargano JW, Marin M, Wallace M,
Curran KG, Chamberland M, McClung N, Campos-Outcalt D, Morgan RL,
Mbaeyi S, et al: The Advisory Committee on Immunization Practices'
Interim Recommendation for Use of Pfizer-BioNTech COVID-19 Vaccine
- United States, December 2020. MMWR Morb Mortal Wkly Rep.
69:1922–1924. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Deva Priya SA, Kavitha S, Venugopal P,
Sriram DK and George M: Can mRNA vaccines turn the tables during
the COVID-19 pandemic? Current status and challenges. Clin Drug
Investig. Mar 23–2021.(Epub ahead of print).
|
|
8
|
Meo SA, Bukhari IA, Akram J, Meo AS and
Klonoff DC: COVID-19 vaccines: Comparison of biological,
pharmacological characteristics and adverse effects of
Pfizer/BioNTech and Moderna Vaccines. Eur Rev Med Pharmacol Sci.
25:1663–1669. 2021.PubMed/NCBI
|
|
9
|
Liu X, Wang J, Xu X, Liao G, Chen Y and Hu
CH: Patterns of IgG and IgM antibody response in COVID-19 patients.
Emerg Microbes Infect. 9:1269–1274. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Long QX, Liu BZ, Deng HJ, Wu GC, Deng K,
Chen YK, Liao P, Qiu JF, Lin Y, Cai XF, et al: Antibody responses
to SARS-CoV-2 in patients with COVID-19. Nat Med. 26:845–848. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shen L, Wang C, Zhao J, Tang X, Shen Y, Lu
M, Ding Z, Huang C, Zhang J, Li S, et al: Delayed specific IgM
antibody responses observed among COVID-19 patients with severe
progression. Emerg Microbes Infect. 9:1096–1101. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Long QX, Tang XJ, Shi QL, Li Q, Deng HJ,
Yuan J, Hu JL, Xu W, Zhang Y, Lv FJ, et al: Clinical and
immunological assessment of asymptomatic SARS-CoV-2 infections. Nat
Med. 26:1200–1204. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lou B, Li TD, Zheng SF, Su YY, Li ZY, Liu
W, Yu F, Ge SX, Zou QD, Yuan Q, et al: Serology characteristics of
SARS-CoV-2 infection after exposure and post-symptom onset. Eur
Respir J. 56:20007632020. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Surcel M, Constantin C, Caruntu C, Zurac S
and Neagu M: Inflammatory cytokine pattern is sex-dependent in
mouse cutaneous melanoma experimental model. J Immunol Res.
2017:92121342017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bellenghi M, Puglisi R, Pontecorvi G, De
Feo A, Carè A and Mattia G: Sex and gender disparities in melanoma.
Cancers (Basel). 12:18192020. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gebhard C, Regitz-Zagrosek V, Neuhauser
HK, Morgan R and Klein SL: Impact of sex and gender on COVID-19
outcomes in Europe. Biol Sex Differ. 11:292020. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ledford H: Moderna COVID vaccine becomes
second to get US authorization. Nature. Dec 18–2020.(Epub ahead of
print). View Article : Google Scholar
|
|
18
|
Prüβ BM: Current state of the first
COVID-19 vaccines. Vaccines (Basel). 9:302021. View Article : Google Scholar
|
|
19
|
Khani E, Khiali S and Entezari-Maleki T:
Potential COVID-19 therapeutic agents and vaccines: an
evidence-based review. J Clin Pharmacol. 61:429–460. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Skelly DT, Harding AC, Gilbert-Jaramillo
J, Knight ML, Longet S, Brown A, Adele S, Adland E, Brown H;
Medawar Laboratory Team, ; Tipton T, Stafford L, Johnson SA, Amini
A; OPTIC Clinical Group, ; Tan TK, Schimanski L, Huang KYA, Rijal
P, et al: Vaccine-induced immunity provides more robust heterotypic
immunity than natural infection to emerging SARS-CoV-2 variants of
concern. Research Square. doi: 10.21203/rs.3.rs-226857/v1
(Preprint).
|
|
21
|
Hyseni I, Molesti E, Benincasa L, Piu P,
Casa E, Temperton NJ, Manenti A and Montomoli E: Characterisation
of SARS-CoV-2 lentiviral pseudotypes and correlation between
pseudotype-based neutralisation assays and live virus-based micro
neutralisation assays. Viruses. 12:10112020. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ni L, Ye F, Cheng M-L, Feng Y, Deng YQ,
Zhao H, Wei P, Ge J, Gou M, Li X, et al: Detection of
SARS-CoV-2-specific humoral and cellular immunity in COVID-19
convalescent individuals. Immunity. 52:971–977.e3. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Stadlbauer D, Tan J, Jiang K, Hernandez
MM, Fabre S, Amanat F, Teo C, Arunkumar GA, McMahon M, Capuano C,
et al: Repeated cross-sectional sero-monitoring of SARS-CoV-2 in
New York City. Nature. 590:146–150. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Neagu M, Calina D, Docea AO, Constantin C,
Filippini T, Vinceti M, Drakoulis N, Poulas K, Nikolouzakis TK,
Spandidos DA, et al: Back to basics in COVID-19: Antigens and
antibodies-Completing the puzzle. J Cell Mol Med. 25:4523–4533.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Beavis KG, Matushek SM, Abeleda APF,
Bethel C, Hunt C, Gillen S, Moran A and Tesic V: Evaluation of the
EUROIMMUN Anti-SARS-CoV-2 ELISA Assay for detection of IgA and IgG
antibodies. J Clin Virol. 129:1044682020. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Thakkar A, Pradhan K, Jindal S, Cui Z,
Rockwell B, Shah AP, Packer SR, Sica RA, Sparano JD, Goldstein DY,
et al: Patterns of seroconversion for SARS-CoV-2 IgG in patients
with malignant disease and association with anticancer therapy. Nat
Cancer. 2:392–399. 2021. View Article : Google Scholar
|
|
27
|
Yu HQ, Sun BQ, Fang ZF, Zhao JC, Liu XY,
Li YM, Sun XZ, Liang HF, Zhong B, Huang ZF, et al: Distinct
features of SARS-CoV-2-specific IgA response in COVID-19 patients.
Eur Respir J. 56:20015262020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ebinger JE, Fert-Bober J, Printsev I, Wu
M, Sun N, Prostko JC, Frias EC, Stewart JL, Van Eyk JE, Braun JG,
et al: Antibody responses to the BNT162b2 mRNA vaccine in
individuals previously infected with SARS-CoV-2. Nat Med. Apr
1–2021.(Epub ahead of print). View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Walsh EE, Frenck RW Jr, Falsey AR, Kitchin
N, Absalon J, Gurtman A, Lockhart S, Neuzil K, Mulligan MJ, Bailey
R, et al: Safety and immunogenicity of two RNA-based COVID-19
vaccine candidates. N Engl J Med. 383:2439–2450. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Mkaddem SB, Christou I, Rossato E,
Berthelot L, Lehuen A and Monteiro RC: IgA, IgA receptors, and
their anti-inflammatory properties. Curr Top Microbiol Immunol.
382:221–235. 2014.PubMed/NCBI
|
|
31
|
Gayet R, Michaud E, Nicoli F, Chanut B,
Paul M, Rochereau N, Guillon C, He Z, Papagno L, Bioley G, et al:
Impact of IgA isoforms on their ability to activate dendritic cells
and to prime T cells. Eur J Immunol. 50:1295–1306. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Russell MW, Moldoveanu Z, Ogra PL and
Mestecky J: Mucosal immunity in COVID-19: a neglected but critical
aspect of SARS-CoV-2 infection. Front Immunol. 11:6113372020.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Isho B, Abe KT, Zuo M, Jamal AJ, Rathod B,
Wang JH, Li Z, Chao G, Rojas OL, Bang YM, et al: Persistence of
serum and saliva antibody responses to SARS-CoV-2 spike antigens in
COVID-19 patients. Sci Immunol. 5:eabe55112020.PubMed/NCBI
|
|
34
|
Lu L, Zhang H, Zhan M, Jiang J, Yin H,
Dauphars DJ, Li SY, Li Y and He YW: Antibody response and therapy
in COVID-19 patients: What can be learned for vaccine development?
Sci China Life Sci. 63:1833–1849. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Sterlin D, Mathian A, Miyara M, Mohr A,
Anna F, Claër L, Quentric P, Fadlallah J, Devilliers H, Ghillani P,
et al: IgA dominates the early neutralizing antibody response to
SARS-CoV-2. Sci Transl Med. 13:eabd22232021. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Dan JM, Mateus J, Kato Y, Hastie KM, Yu
ED, Faliti CE, Grifoni A, Ramirez SI, Haupt S, Frazier A, et al:
Immunological memory to SARS-CoV-2 assessed for up to 8 months
after infection. Science. 371:eabf40632021. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wang Z, Lorenzi JCC, Muecksch F, Finkin S,
Viant C, Gaebler C, Cipolla M, Hoffmann HH, Oliveira TY, Oren DA,
et al: Enhanced SARS-CoV-2 neutralization by dimeric IgA. Sci
Transl Med. 13:eabf15552021. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Manisty C, Otter AD, Treibel TA, McKnight
Á, Altmann DM, Brooks T, Noursadeghi M, Boyton RJ, Semper A and
Moon JC: Antibody response to first BNT162b2 dose in previously
SARS-CoV-2-infected individuals. Lancet. 397:1057–1058. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Sahin U, Muik A, Derhovanessian E, Vogler
I, Kranz LM, Vormehr M, Baum A, Pascal K, Quandt J, Maurus D, et
al: COVID-19 vaccine BNT162b1 elicits human antibody and TH1 T cell
responses. Nature. 586:594–599. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Lombardi A, Bozzi G, Ungaro R, Villa S,
Castelli V, Mangioni D, Muscatello A, Gori A and Bandera A: Mini
review immunological consequences of immunization with COVID-19
mRNA vaccines: preliminary results. Front Immunol. 12:6577112021.
View Article : Google Scholar : PubMed/NCBI
|