Introduction
Benign paroxysmal positional vertigo (BPPV), also
known as otolithiasis, is the most common peripheral
vertigo-associated disease (1,2). The
incidence rate of BPPV is ~2.4% (3)
with a male-to-female ratio of ~1: 2, and peak incidence among
those aged 50–60 years (4). The
primary clinical treatment options for BPPV include manual
manipulation based on the semicircular canal and otolith involved.
Vertigo symptoms can be relieved using the Epley, Semont and
Barbecue maneuvers to reposition the detached otolith from the
semicircular canal into the utriculus (5). However, these methods are only
symptomatic treatments, and can neither cure BPPV, nor prevent its
recurrence (6). Therefore, it is of
clinical significance to investigate the pathogenesis of BPPV to
provide a theoretical basis for targeted prevention and
treatment.
BPPV is classified as either primary or secondary
based on its pathogenesis. Secondary BPPV is defined as BPPV
secondary to ear surgery, trauma, use of ototoxic drugs such as
aminoglycoside, Meniere's disease, vestibular neuronitis and other
etiologies (7). Underlying
mechanisms of primary BPPV include aging, ear changes such as hair
cell loss or injury, metabolic disorders affecting the endolymph
calcium ion, decreased otolith protein secretion and greater
fragility of anchorin filaments, which results in otolith
detachment and dislocation (8,9). At
present, certain scholars consider osteoporosis to be a
predisposing factor for BPPV (10).
Other factors, such as vitamin D (VD) deficiency, hypertension,
diabetes, hyperlipemia, atherosclerosis and cerebrovascular
disease, may also contribute to BPPV (11,12).
VD is a class of lipid-soluble secosteroid
associated with human health, and is important in maintaining
calcium homeostasis in humans (13,14).
VD helps maintain normal otolith function by regulating calcium ion
homeostasis in the vestibular lymph (7). Büki et al (15) suggested that VD deficiency is
associated with BPPV and this hypothesis has been supported by
other research. For example, serum 25-hydroxy VD levels <10
ng/ml are associated with high recurrence rates of BPPV (16). VD primarily exists in the human body
as calcitriol [1,25(OH)2D3] and exerts its
biological function via the VD receptor (VDR); VDR is a member of
the ligand-activated transcription factor steroid/thyroid hormone
receptor superfamily and is found in numerous types of cell, such
as immune, neural and epithelial cells (17). Following interaction with activated
VD [1,25(OH)2D3], VDR has been shown to
induce multiple antitumor gene regulation and cell signaling
pathways, including those involved in proliferation suppression,
stimulation of cell apoptosis and autophagy, angiogenesis
inhibition and immune system regulation (18,19).
To the best of our knowledge, however, there is little information
regarding the role of VDR in BPPV.
The present study analyzed serum VD levels in
patients with BPPV, then investigated the potential role of VDR in
BPPV. The results demonstrated that VDR expression was directly
associated with the expression of otolith-associated proteins in
vivo. The association between VDR levels and the occurrence of
BPPV suggested that VDR expression levels may be an important
diagnostic marker. VDR may also be a potential target for the
prevention and control of BPPV.
Materials and methods
Patients
Patients with BPPV treated at Affiliated Hospital of
Inner Mongolia Medical University (Hohhot, China) were enrolled
from April 2017 to December 2018. Participants in the control group
had no prior history of vertigo onset. For inclusion in the
experimental group, patients were required to have met the
diagnostic criteria for BPPV (20).
Predisposing factors (position or head position change), vertigo
characteristics upon onset and positive physical examination
(Dix-Hallpike or Roll test) were used to confirm diagnosis. In
total, 48 patients were enrolled in the experimental group in
strict accordance with the inclusion and exclusion criteria, and 48
controls were recruited. The patients comprised 30 females and 18
males (ratio, 1.67:1.00) aged 50–80 years (mean age, 64.65±1.24
years). The majority (86%) of patients were evaluated within 1 week
of symptom onset. The controls comprised 28 females and 20 males
(ratio, 1.40:1.00) aged 50–80 years (mean age, 63.25±1.33
years).
Primary exclusion criteria for both the experimental
and control groups included: i) Head trauma or ear surgery history;
ii) prior medication such as calcium, VD, hormone and associated
drug substitution therapy; iii) ear disorders, such as vestibular
neuronitis, sudden deafness, otitis media or Meniere's disease; iv)
other central nervous system diseases such as transient ischemic
attack of posterior circulation, cerebral infarction, cerebral
hemorrhage or migraine; v) relevant endocrine diseases such as
hypothalamic or pituitary space-occupying lesions; vi) severe renal
insufficiency; vii) long-term anxiety or aversion to noisy
environments; and viii) unwillingness to cooperate. Written
informed consent was obtained from all participants for the use of
their blood samples. The present study was approved by the Ethics
Committee of the Affiliated Hospital of Inner Mongolia Medical
University.
Bone densitometry
Before treatment, the bone mineral density of
patients was measured via dual-energy x-ray absorptiometry using a
Hologic Discovery dual-energy x-ray absorptiometer (Hologic, Inc.).
Bone quality change was determined by T value: T≥-1.0, normal bone
mineral density; −2.5<T<-1.0, osteopenia; and T≤-2.5,
osteoporosis.
Detection of plasma
1,25(OH)2D3
The subjects were food-fasted for 12 h and
liquid-fasted for 8 h before the test. Plasma
1,25(OH)2D3 levels were measured using an
electrochemiluminescence kit (Elecsys Vitamin D total) according to
the manufacturer's directions (Roche Diagnostics). This assay has a
sensitivity of 0.83 ng/ml and a measurement range of 0.83–322.50
ng/ml.
RNA extraction and reverse
transcription-quantitative (RT-q) PCR
A total of 5 ml peripheral venous blood was
collected from all subjects and anticoagulated using citric acid.
Lymphocyte separation medium (cat. no. Corning LSM 25-072-CV;
Corning, Inc.) was used to separate lymphocytes from peripheral
blood, and total RNA was extracted using TRIzol® reagent
(cat. no. 15596026, Invitrogen; Thermo Fisher Scientific, Inc.).
Total mRNA extraction (PolyATtract® mRNA Isolation
Systems; cat. no. Z5210), first chain synthesis and PCR fluorescent
quantitation kits (GoTaq® qPCR Master Mix; cat. no.
A6001) were purchased from Promega Corporation and used according
to the manufacturer's protocols. RT-qPCR was performed using the
following thermocycling conditions: Initial denaturation at 95°C
for 30 sec, followed by 40 cycles of 5 sec at 95°C, 10 sec at 60°C
and 30 sec at 72°C. The 2−ΔΔCq method was used to
calculate the relative gene expression levels (21). The housekeeping gene β-actin was
used as an internal reference. The relative amount of the target
gene was obtained by dividing the mean copy number of the target
gene by the mean copy number of reference gene. The primer
sequences were as follows: Otoconin-90 (OC90) forward,
5′-AGTGGTTTGGATGGTGCCAA-3′ and reverse, 5′-GCACCATCATTTCCACGAGC-3′;
VDR forward, 5′-CAGGCTATCATTACGGAGTC-3′ and reverse,
5′-CTGGCATTTGTTTCTGTTCT-3′; NAPDH oxidase 3 (NOX3) forward,
5′-TTTTGGGTTCAACACTGGCT-3′ and reverse, 5′-GTCTAATTGCCTCCTCCACG-3′;
and β-actin forward, 5′-TAGTTGCGTTACACCCTTTCTTG-3′ and reverse,
5′-TGCTGTCACCTTCACCGTTC-3′.
ELISA
Protein expression levels of OC90 and NOX3 were
detected in each serum sample using ELISA kits (cat. nos.
CSB-EL016255HU and CSB-E17448h-1, respectively; both Cusabio
Technology LLC.) according to the manufacturer's instructions. The
calibration curve was plotted according to the concentration and
optical density value of the standard to calculate the
concentration of test sample.
Mouse model
A total of 12 VDR gene knockout and 12 knock-in
female C57BL/6JGpt mice (age, 6–8 weeks; weight, ~20 g) were
purchased from GemPharmatech Co., Ltd. All mice were raised in
specific pathogen free conditions with 12 h light/dark cycle and
free access to food and water at 21–24°C and 40–67% humidity. After
3 days, one group of knockout (n=6) and knock-in mice (n=6) was
sacrificed to harvest inner ear tissue for subsequent experiments.
Another group of knockout mice (n=6) was injected with
1,25(OH)2D3 100 ng/day via the caudal vein
daily for 1 week. A total of 12 control wild-type C57BL/6JGpt mice
(GemPharmatech Co., Ltd.) were injected with an equivalent dose of
normal saline daily for 1 week. The present study was approved by
the Animal Ethics Committee of Affiliated Hospital of Inner
Mongolia Medical University (approval no. QZ2017023). All
experiments were conducted in accordance with the Code for the Care
and Use of Animals for Scientific Purposes (22) and the principles of replacing,
refining, and reducing.
Western blotting
Bilateral temporal bones of mice were separated, and
the muscle and other adherent soft tissues were removed manually.
Inner ear samples were ground in liquid nitrogen and placed in PBS
buffer (cat. no. C0221A; Beyotime Institute of Biotechnology)
containing 1% protease inhibitor (cat. no. 78438; Invitrogen;
Thermo Fisher Scientific, Inc.), then placed on ice for 10 min. The
solution was centrifuged at 4°C at 12,000 × g for 10 min, and the
supernatant was reserved. Following quantification using the BCA
Protein Assay kit (cat. no. P0012S, Beyotime Institute of
Biotechnology), and electrophoresis (40 µg protein/lane separated
via 10% SDS-PAGE), proteins were transferred onto a PVDF membrane.
Then, the membrane was blocked for 1 h with 5% skimmed milk at
25°C. After washing, the membrane was incubated at 4°C overnight
with the following prediluted primary antibodies: Anti-transferrin
(1:1,000; 77 kDa; cat. no. ab109503; Abcam), anti-GAPDH (1:2,000;
36 kDa; cat. no. ab181602; Abcam), anti-VDR (1:1,000; 48 kDa;
ab109234; Abcam), anti-NOX3 (1:1,000; 65 kDa; cat. no. ab254572;
Abcam) and anti-OC90 (1:1,000; 51 kDa; cat. no. PA5-71564;
Invitrogen; Thermo Fisher Scientific, Inc.). The membrane was then
incubated with horseradish peroxidase-conjugated secondary antibody
(1:1,000; cat. no. A0208; Beyotime Institute of Biotechnology)
without agitation for 60 min at 20–25°C. Signals were visualized
using ECL reagents (EMD Millipore) and detected using an Amersham™
Imager 680 (Cytiva). ImageJ software (1.8.0; National Institutes of
Health) was used for densitometry.
Statistical analysis
Data are presented as the mean ± SD of three
independent repeats. SPSS 19.0 software (IBM Corp.) was used for
statistical analysis. Normally distributed data were analyzed via
independent sample t-tests; non-parametric Wilcoxon rank-sum tests
were used to analyze data with non-normal distributions. Receiver
operating characteristic (ROC) curve analysis was performed to
reveal the potential diagnostic value of VDR expression levels for
BPPV. Differences among multiple groups were detected via ANOVA
(one-way) with post hoc Tukey's test. χ2 test was used
for categorical data. Pearson's correlation analysis was used to
assess the correlation between VDR mRNA and 1,25(OH)2D3 levels.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Study subjects
Data was collected from patients with BPPV diagnosed
in Affiliated Hospital of Inner Mongolia Medical University. There
was no difference in the age, sex ratio, BMI, or diabetes and
hypertension rate between the patient and control groups (Table I). However, cases of decreased bone
density (particularly osteoporosis) in patients with BPPV were
significantly higher than in the control group (Table I). As shown in Table II, BPPV most commonly involved the
posterior (n=25, 52.1%), horizontal (n=16, 33.3%) and anterior
canals (n=7, 14.6%). The proportion of patients with
canalolithiasis (n=38) was 79.2% and that of cupulolithiasis (n=10)
was 20.8%.
 | Table I.Clinical characteristics of patients
and controls. |
Table I.
Clinical characteristics of patients
and controls.
| Characteristic | Control (n=48) | Patients with BPPV
(n=48) | P-value |
|---|
| Age, years | 63.25±1.33 | 64.65±1.24 | 0.440 |
| Male | 20 (41.2%) | 18 (37.5%) | 0.830 |
| Body mass
index | 25.44±0.12 | 25.17±0.13 | 0.120 |
| Bone mineral
density |
|
| <0.050 |
|
Normal | 25 (52.0%) | 8 (16.7%) |
|
|
Osteopenia | 15 (31.3%) | 10 (20.8%) |
|
|
Osteoporosis | 8 (16.7%) | 30 (62.5%) |
<0.001a |
| Diabetes | 6 (12.5%) | 7 (14.6%) | >0.050 |
| Hypertension | 10 (20.8%) | 11 (22.9%) | >0.050 |
 | Table II.Involvement of different sites in
patients with benign paroxysmal positional vertigo. |
Table II.
Involvement of different sites in
patients with benign paroxysmal positional vertigo.
| Site | Number of cases
(%) |
|---|
| Posterior | 25 (52.1) |
| Horizontal | 16 (33.3) |
| Anterior canal | 7 (14.6) |
|
Canalolithiasis | 38 (79.2) |
|
Cupulolithiasis | 10 (20.8) |
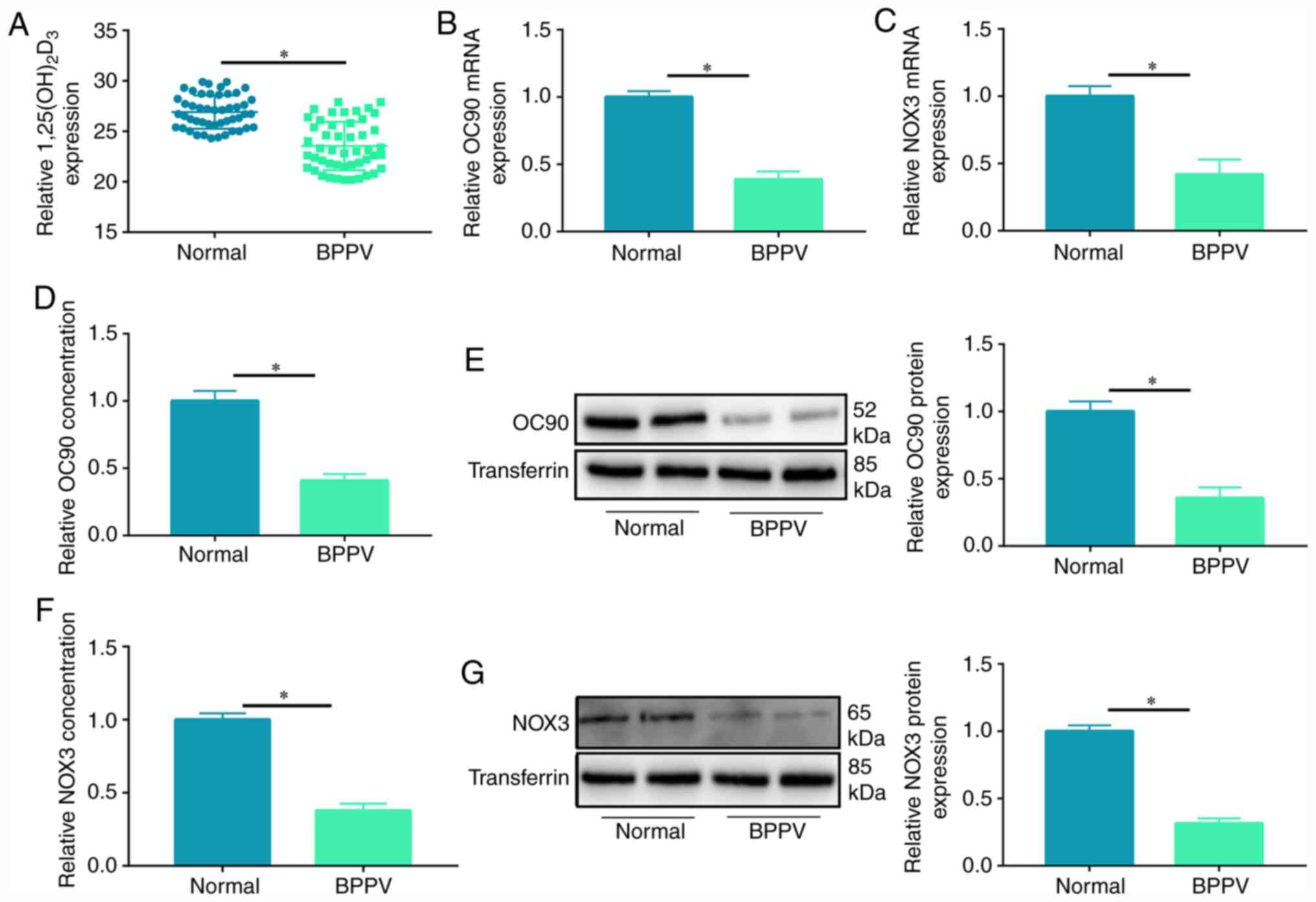
Plasma expression levels of
1,25(OH)2D3 and otolith-associated protein in
patients with BPPV
The level of 1,25(OH)2D3 was
measured in patients with BPPV; results indicated that plasma VD
levels in patients with BPPV were significantly decreased compared
with the control group (Fig. 1A).
Serum VD expression levels in patients with canalolithiasis and
cupulolithiasis exhibited no significant difference (Fig. S1). As demonstrated via RT-qPCR,
serum mRNA expression levels of otolith-associated proteins OC90
and NOX3 were notably reduced in patients with BPPV compared with
in controls (Fig. 1B and C). ELISA
indicated that protein levels of OC90 were lower in the serum of
patients with BPPV compared with in the control group; this was
supported by western blot analysis (Fig. 1D and E). Finally, NOX3 protein
levels were also significantly lower in the serum of patients with
BPPV compared with in the controls, as revealed via both ELISA and
western blotting (Fig. 1F and G).
The expression levels of 1,25(OH)2D3 and
otolith-associated proteins were lower in patients with BPPV than
in controls. This suggested that the expression levels of VD
regulated OC90 and NOX3 expression, and were associated with the
occurrence and development of BPPV.
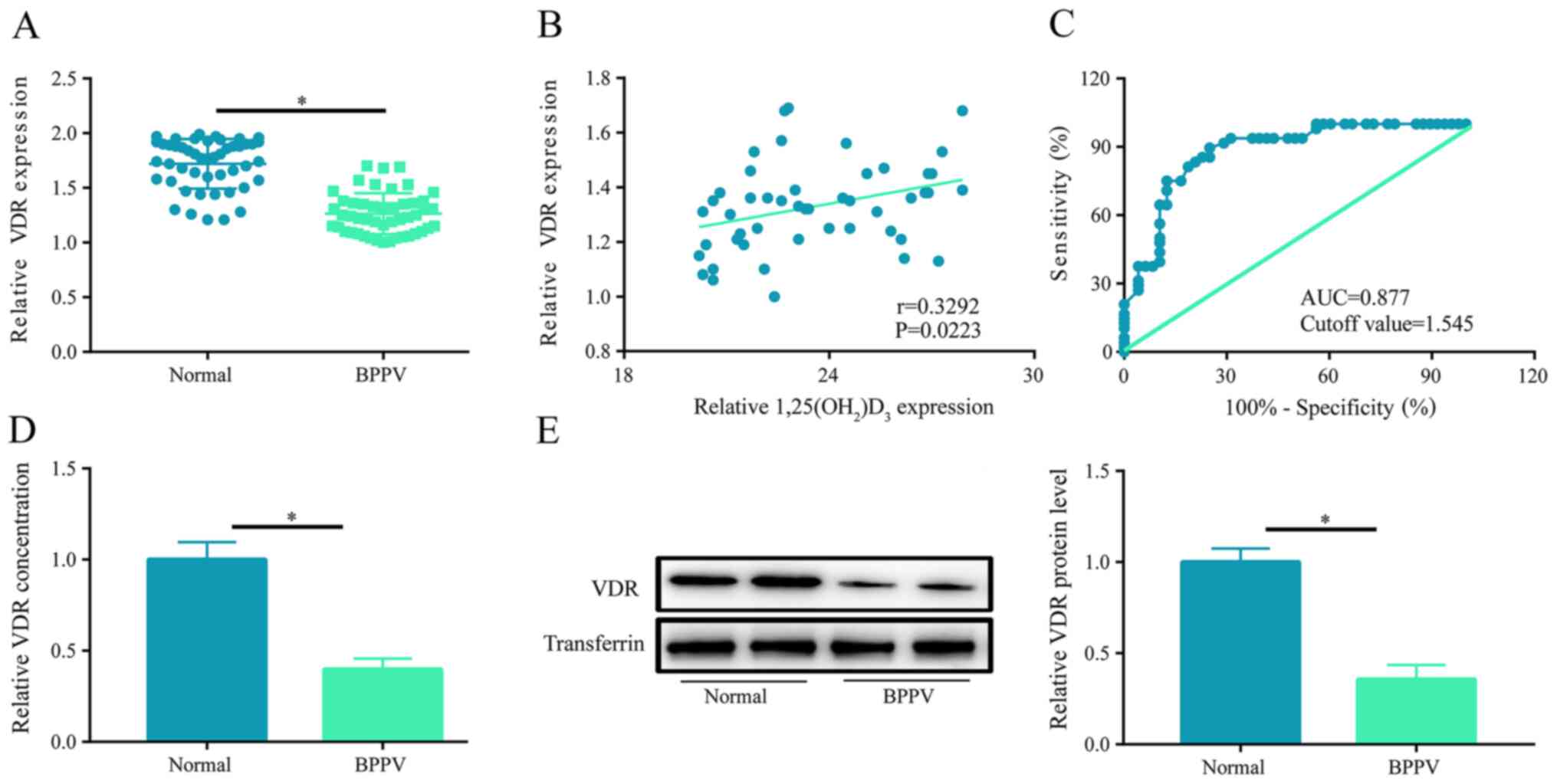
VDR is significantly underexpressed in
patients with BPPV
As VD exerts its biological role primarily via
interacting with VDR, a potential association between VDR
expression levels and BPPV was investigated. RT-qPCR was performed
to analyze VDR expression levels in the serum of patients with
BPPV: Compared with the control, VDR expression was notably
decreased (Fig. 2A), and its
expression was positively correlated with that of
1,25(OH)2D3 (r=0.3292; P=0.0223; Fig. 2B). Furthermore, ROC curve analysis
reported an area under the curve of 0.877 and cutoff value of
1.545, suggesting that VDR was a candidate diagnostic marker of
BPPV (Fig. 2C). The mRNA and
protein expression levels of VDR were also detected and shown to be
significantly lower in patients with BPPV (Fig. 2D and E).
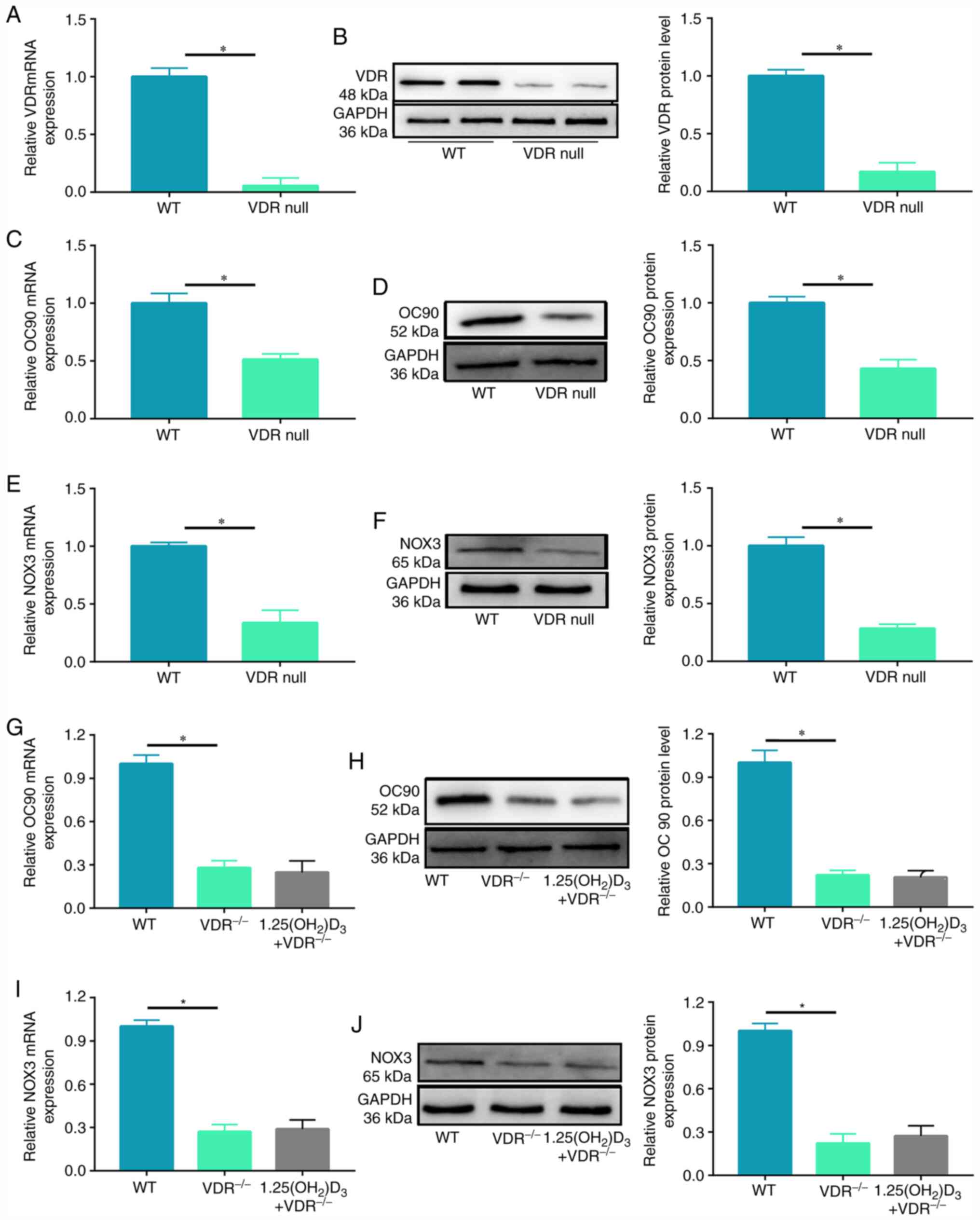
VD affects expression of OC90 and NOX3
via VDR
In order to verify the effects of VDR on the
expression levels of OC90, VDR−/− mice were purchased,
and inner ear tissue was harvested for the detection of OC90
expression levels. VDR expression levels were first verified in
knockout mice: mRNA and protein levels of VDR were significantly
decreased in VDR−/− mice compared with wild-type mice
(Fig. 3A and B). Subsequent RT-qPCR
experiments using inner ear tissue found that mRNA levels of OC90
were significantly lower in VDR−/− mice compared with
those in wild-type mice (Fig. 3C);
western blot analysis showed the same trend for OC90 protein
expression (Fig. 3D). Similarly,
NOX3 mRNA and protein expression levels were significantly
downregulated in VDR−/− mice compared with in wild-type
mice (Fig. 3E and F). This
suggested that there was an association between VDR and both OC90
and NOX3 expression levels. In order to investigate whether VD
acted via VDR to regulate expression levels of OC90 and NOX3,
activated VD or saline was injected into the caudal vein of
VDR−/− mice (wild-type injected with saline,
VDR−/− injected with saline and VDR−/−
injected with activated VD), and inner ear tissue was collected
from each group 1 week later. Injection of VD did not reverse the
inhibiting effect of the VDR−/− on otolith protein
formation (Fig. 3G-J). This
indicated that VD required VDR to exert its biological
function.
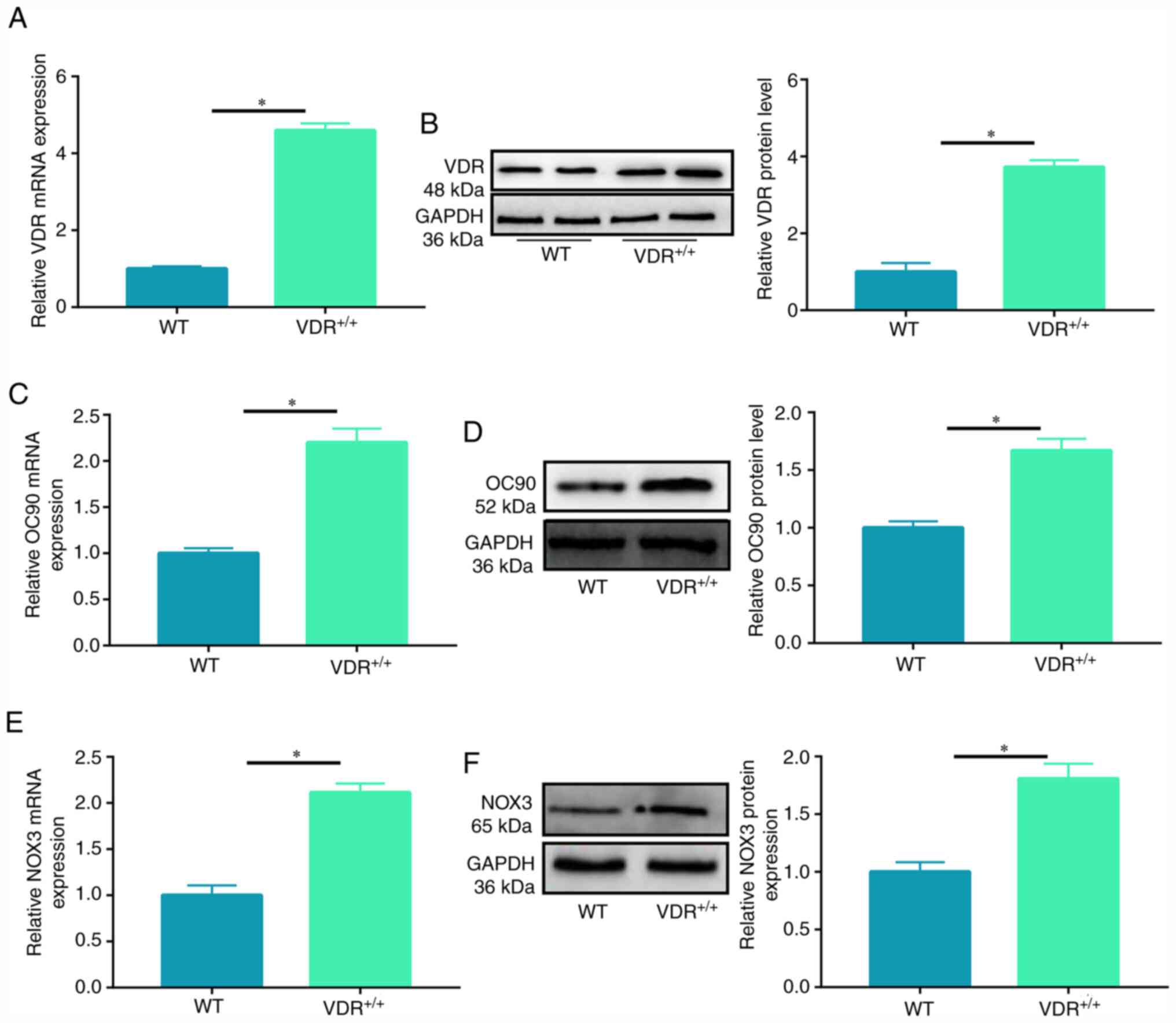
Overexpression of VDR increases
expression of OC90 and NOX3
VDR overexpression mice were constructed to further
verify the role of VDR in regulating OC90 and NOX3 expression. The
model was successful, indicated by the detection of VDR mRNA and
protein (Fig. 4A and B). RT-qPCR
and western blotting were used to detect mRNA and protein levels of
OC90 and NOX3 in inner ear tissue. mRNA and protein expression
levels of both OC90 and NOX3 were significantly increased in VDR
overexpression mice compared with in wild-type mice (Fig. 4C-F). Thus, VDR was important for
expression of the otolith-associated proteins OC90 and NOX3.
Discussion
It has previously been proposed that BPPV is caused
by numerous factors, such as aging, genetic mutation, head trauma
and ototoxic drugs, causing otolith particles on macula utriculi
and macula sacculi to detach and move into the semicircular canal
(9,23). In the present study, anterior canal
BPPV accounted for 14.6% or cases, while anterior canal BPPV was
rare, as previously reported (24).
This may be because patients of only one hospital were included and
anterior canal BPPV may have been underdiagnosed. In addition, the
number of patients in the present study was not large enough, so
anterior canal BPPV morbidity in the present study may not be
consistent with that in the population. Therefore, more clinical
samples from multiple centers are needed.
Otoliths are inlaid in the otolithic membrane
covering the macula surface and consist of an organic matrix
composed primarily of otolith proteins and deposited calcium
carbonate. These specific proteins mediate the special functions of
the inner ear. In cases of dysfunction or injury, they are released
into the circulatory system, and can be detected in the serum
(25,26). For example, otolith protein otolin-1
is specifically expressed in the inner ear (27), but can be detected in serum when it
moves into systemic circulation via the blood-labyrinth barrier
(28). OC90 is the most common
otolith protein in humans, mice and other mammals: It accounts for
>90% of the otolith organic matrix, and is considered to be a
necessary factor for otolith growth and maintenance (29). Although the organic matrix accounts
for a smaller percentage of the otolith, it is now considered to be
vital in the development of the otolith (25).
OC90 is generated by non-sensory cells outside the
macula and transferred to the macula sacculi and macula utriculi
post-synthesis, where it recruits calcium deposits to promote the
formation of the original otolith body (30,31).
In addition, OC90 may also regulate otolith growth and promote the
transformation of otoliths from their original form to their mature
hexagonal form (27). Zhao et
al (31) demonstrated that OC90
gene knockout mice do not effectively recruit Ca2+ to
the macula from the bloodstream during development. In these mice,
significantly fewer otoliths, with a notably larger volume and
loose arrangement, were observed compared with wild-type mice. The
knockout mice also exhibited etiological posture disorders
(26). Multiple non-intra-otolith
proteins participate in the regulation of the growth and
development of otoliths: One protein that regulates otolith growth
is NOX3 (32–34). NOX3 controls otolith growth by
regulating of the secretion or function of otolith proteins, as
well as the spatial and temporal distribution of calcium and other
ions. Therefore, OC90 and NOX3 were selected as detection indices
to assess the effects of VD and VDR on BPPV onset in the present
study.
VD is known for its role in the homeostasis of
calcium and phosphorus (35). VDR
is present in cells throughout the body, and is involved in cell
proliferation and differentiation as well as immunomodulation
(36). The functions of VD are
mediated by nuclear VDR. Studies have shown that increased VDR
expression levels are associated with decreased mortality rates and
improved prognosis in numerous types of cancer, including breast
and prostate cancer (37,38). Wen et al (39) reported that VDR expression levels
are significantly decreased in gastric cancer tissue but are high
in well- and moderately differentiated tissue and small tumors.
This indicates that VDR may be a prognostic factor of gastric
cancer.
To the best of our knowledge, there are few studies
on the role of VDR in BPPV. The present study investigated the
potential role of VDR in the occurrence and development of BPPV. It
was first verified that patients with BPPV had lower serum levels
of VD. Additionally, patients with BPPV had notably lower plasma
expressions levels of OC90 and NOX3, indicating an association
between VD levels and BPPV occurrence. VDR expression levels were
significantly lower in the serum of patients with BPPV than in that
of the controls. VDR expression levels were positively associated
with serum VD levels, indicating that VD deficiency and VDR
expression may serve a role in BPPV. However, the present study was
relatively small, and the association between VDR and VD in
patients with BPPV should be further verified using a larger sample
group. ROC curve analysis showed that VDR may be used as a
diagnostic marker of BPPV, providing a new theoretical foundation
for clinical, auxiliary or early diagnosis of BPPV.
A previous study detected VDRs in the nuclei of the
epithelium lining the crista ampullaris, membranous semicircular
canal and surrounding osteocytes in mice (40). Furthermore, VDR mutant mice showed
decreased balance function using the accelerating rotarod, tilting
platform, rotating tube and swim tests, which suggested that
decreased VD causes vestibular dysfunction (40). The present study investigated the
formation of inner ear-associated protein using VDR gene knockout
and knock-in mice. The results revealed that expression levels of
the inner ear-associated proteins OC90 and NOX3 were significantly
lower in VDR knockout mice than in wild-type mice. Conversely,
expression levels of OC90 and NOX3 in the inner ear tissue of VDR
overexpression mice were notably higher than those in wild-type
mice. This suggested that VDR was vital for the expression of
otolith proteins. Following injection of VD into the caudal vein of
VDR knockout mice, expression levels the OC90 and NOX3 in the inner
ear tissue were not notably increased. This indicated that VDR was
crucial for the expression of inner ear-associated proteins.
Taken together, the results of the present study
indicated that VDR expression levels are significantly decreased in
patients with BPPV. In vivo experiments demonstrated that
VDR was associated with the expression of inner ear-associated
proteins OC90 and NOX3, and that VDR expression may have diagnostic
potential, with the protein potentially serving an important role
in BPPV pathogenesis. This not only enriches knowledge of BPPV, but
may also provide a new theoretical basis for clinical diagnosis and
treatment of BPPV. However, the present study has certain
limitations. It is unknown whether the downregulation of VDR in
patients with BPPV is a universal phenomenon. Additional samples
and multicenter cooperation will be needed for further validation.
In addition, only two inner ear-associated proteins, OC90 and NOX3,
were investigated. Further investigation is required to determine
how VDR affects the expression of other inner ear-associated
proteins; additionally, the underlying mechanisms concerning how
VDR modulates the synthesis of inner ear-associated proteins
remains unclear.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SZ and JX performed the experiments and generated
data. SZ and PL made substantial contributions to the conception
and design of the study. YG, BW and LX conducted data analysis and
interpretation. All authors contributed to the drafting and
revision of the manuscript and agreed to be accountable for all
aspects of the research. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present animal study was approved by The
Affiliated Hospital of Inner Mongolia Medical University (approval
no. QZ2017023). Human experiments were approved by the Ethics
Committee of the Affiliated Hospital of Inner Mongolia Medical
University. Written informed consent was provided by all
subjects.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Froehling DA, Silverstein MD, Mohr DN,
Beatty CW, Offord KP and Ballard DJ: Benign positional vertigo:
Incidence and prognosis in a population-based study in Olmsted
County, Minnesota. Mayo Clin Proc. 66:596–601. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Imai T, Higashi-Shingai K, Takimoto Y,
Masumura C, Hattori K and Inohara H: New scoring system of an
interview for the diagnosis of benign paroxysmal positional
vertigo. Acta Otolaryngol. 136:283–288. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fife TD, Iverson DJ, Lempert T, Furman JM,
Baloh RW, Tusa RJ, Hain TC, Herdman S, Morrow MJ and Gronseth GS;
Quality Standards Subcommittee, American Academy of Neurology, :
Practice parameter: Therapies for benign paroxysmal positional
vertigo (an evidence-based review): Report of the quality standards
subcommittee of the American academy of neurology. Neurology.
70:2067–2074. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bhattacharyya N, Gubbels SP, Schwartz SR,
Edlow JA, El-Kashlan H, Fife T, Holmberg JM, Mahoney K,
Hollingsworth DB, Roberts R, et al: Clinical practice guideline:
Benign paroxysmal positional vertigo (Update). Otolaryngol Head
Neck Surg. 156 (3 Suppl):S1–S47. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ogun OA, Büki B, Cohn ES, Janky KL and
Lundberg YW: Menopause and benign paroxysmal positional vertigo.
Menopause. 21:886–889. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Imai T, Takeda N, Ikezono T, Shigeno K,
Asai M, Watanabe Y and Suzuki M; Committee for Standards in
Diagnosis of Japan Society for Equilibrium Research, :
Classification, diagnostic criteria and management of benign
paroxysmal positional vertigo. Auris Nasus Larynx. 44:1–6. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Jeong SH, Kim JS, Shin JW, Kim S, Lee H,
Lee AY, Kim JM, Jo H, Song J and Ghim Y: Decreased serum vitamin D
in idiopathic benign paroxysmal positional vertigo. J Neurol.
260:832–838. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Baloh RW, Honrubia V and Jacobson K:
Benign positional vertigo: Clinical and oculographic features in
240 cases. Neurology. 37:371–378. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lundberg YW, Xu Y, Thiessen KD and Kramer
KL: Mechanisms of otoconia and otolith development. Dev Dyn.
244:239–253. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wu Y, Gu C, Han W, Lu X, Chen C and Fan Z:
Reduction of bone mineral density in native Chinese female
idiopathic benign paroxysmal positional vertigo patients. Am J
Otolaryngol. 39:31–33. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yoda S, Cureoglu S, Yildirim-Baylan M,
Morita N, Fukushima H, Harada T and Paparella MM: Association
between type 1 diabetes mellitus and deposits in the semicircular
canals. Otolaryngol Head Neck Surg. 145:458–462. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Xu J and Zhang J: LncRNA TP73-AS1 is a
novel regulator in cervical cancer via miR-329-3p/ARF1 axis. J Cell
Biochem. 121:344–352. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Holick MF: Resurrection of vitamin D
deficiency and rickets. J Clin Invest. 116:2062–2072. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Christakos S, Dhawan P, Verstuyf A,
Verlinden L and Carmeliet G: Vitamin D: Metabolism, molecular
mechanism of action, and pleiotropic effects. Physiol Rev.
96:365–408. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Büki B, Ecker M, Jünger H and Lundberg YW:
Vitamin D deficiency and benign paroxysmal positioning vertigo. Med
Hypotheses. 80:201–204. 2013. View Article : Google Scholar
|
|
16
|
Talaat HS, Kabel AM, Khaliel LH, Abuhadied
G, El-Naga HA and Talaat AS: Reduction of recurrence rate of benign
paroxysmal positional vertigo by treatment of severe vitamin D
deficiency. Auris Nasus Larynx. 43:237–241. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Haussler MR, Whitfield GK, Haussler CA,
Hsieh JC, Thompson PD, Selznick SH, Dominguez CE and Jurutka PW:
The nuclear vitamin D receptor: Biological and molecular regulatory
properties revealed. J Bone Miner Res. 13:325–349. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Feldman D, Krishnan AV, Swami S,
Giovannucci E and Feldman BJ: The role of vitamin D in reducing
cancer risk and progression. Nat Rev Cancer. 14:342–357. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Dovnik A and Dovnik NF: Vitamin D and
ovarian cancer: Systematic review of the literature with a focus on
molecular mechanisms. Cells. 9:3352020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Editorial Board of Chinese Journal of
Otorhinolaryngology Head and Neck Surgery; Society of
Otorhinolaryngology Head and Neck Surgery Chinese Medical:
Association, . Guideline of diagnosis and treatment of benign
paroxysmal positional vertigo (2017). Zhonghua Er Bi Yan Hou Tou
Jing Wai Ke Za Zhi. 52:173–177. 2017.(In Chinese). PubMed/NCBI
|
|
21
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Code of practice for the care and use of
animals for experimental purposes in Australia. Med J Aust.
141:871–876. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Jang YS, Hwang CH, Shin JY, Bae WY and Kim
LS: Age-related changes on the morphology of the otoconia.
Laryngoscope. 116:996–1001. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yang X, Ling X, Shen B, Hong Y, Li K, Si L
and Kim JS: Diagnosis strategy and Yacovino maneuver for anterior
canal-benign paroxysmal positional vertigo. J Neurol.
266:1674–1684. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Thalmann R, Ignatova E, Kachar B, Ornitz
DM and Thalmann I: Development and maintenance of otoconia:
Biochemical considerations. Ann N Y Acad Sci. 942:162–178. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhao X, Jones SM, Yamoah EN and Lundberg
YW: Otoconin-90 deletion leads to imbalance but normal hearing: A
comparison with other otoconia mutants. Neuroscience. 153:289–299.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Deans MR, Peterson JM and Wong GW:
Mammalian otolin: A multimeric glycoprotein specific to the inner
ear that interacts with otoconial matrix protein otoconin-90 and
Cerebellin-1. PLoS One. 5:e127652010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Parham K, Sacks D, Bixby C and Fall P:
Inner ear protein as a biomarker in circulation? Otolaryngol Head
Neck Surg. 151:1038–1040. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lundberg YW, Zhao X and Yamoah EN:
Assembly of the otoconia complex to the macular sensory epithelium
of the vestibule. Brain Res. 1091:47–57. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hughes I, Thalmann I, Thalmann R and
Ornitz DM: Mixing model systems: Using zebrafish and mouse inner
ear mutants and other organ systems to unravel the mystery of
otoconial development. Brain Res. 1091:58–74. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhao X, Yang H, Yamoah EN and Lundberg YW:
Gene targeting reveals the role of Oc90 as the essential organizer
of the otoconial organic matrix. Dev Biol. 304:508–524. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kim E, Hyrc KL, Speck J, Salles FT,
Lundberg YW, Goldberg MP, Kachar B, Warchol ME and Ornitz DM:
Missense mutations in otopetrin 1 affect subcellular localization
and inhibition of purinergic signaling in vestibular supporting
cells. Mol Cell Neurosci. 46:655–661. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kim E, Hyrc KL, Speck J, Lundberg YW,
Salles FT, Kachar B, Goldberg MP, Warchol ME and Ornitz DM:
Regulation of cellular calcium in vestibular supporting cells by
otopetrin 1. J Neurophysiol. 104:3439–3450. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Paffenholz R, Bergstrom RA, Pasutto F,
Wabnitz P, Munroe RJ, Jagla W, Heinzmann U, Marquardt A, Bareiss A,
Laufs J, et al: Vestibular defects in head-tilt mice result from
mutations in Nox3, encoding an NADPH oxidase. Genes Dev.
18:486–491. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Prosser DE and Jones G: Enzymes involved
in the activation and inactivation of vitamin D. Trends Biochem
Sci. 29:664–673. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Nagpal S, Na S and Rathnachalam R:
Noncalcemic actions of vitamin D receptor ligands. Endocr Rev.
26:662–687. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Hendrickson WK, Flavin R, Kasperzyk JL,
Fiorentino M, Fang F, Lis R, Fiore C, Penney KL, Ma J, Kantoff PW,
et al: Vitamin D receptor protein expression in tumor tissue and
prostate cancer progression. J Clin Oncol. 29:2378–2385. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Berger U, McClelland RA, Wilson P, Greene
GL, Haussler MR, Pike JW, Colston K, Easton D and Coombes RC:
Immunocytochemical determination of estrogen receptor, progesterone
receptor, and 1,25-dihydroxyvitamin D3 receptor in breast cancer
and relationship to prognosis. Cancer Res. 51:239–244.
1991.PubMed/NCBI
|
|
39
|
Wen Y, Da M, Zhang Y, Peng L, Yao J and
Duan Y: Alterations in vitamin D signaling pathway in gastric
cancer progression: A study of vitamin D receptor expression in
human normal, premalignant, and malignant gastric tissue. Int J
Clin Exp Pathol. 8:13176–13184. 2015.PubMed/NCBI
|
|
40
|
Minasyan A, Keisala T, Zou J, Zhang Y,
Toppila E, Syvälä H, Lou YR, Kalueff AV, Pyykkö I and Tuohimaa P:
Vestibular dysfunction in vitamin D receptor mutant mice. J Steroid
Biochem Mol Biol. 114:161–166. 2009. View Article : Google Scholar : PubMed/NCBI
|