|
1
|
Evan AP, Lingeman JE, Worcester EM,
Bledsoe SB, Sommer AJ, Williams JC Jr, Krambeck AE, Philips CL and
Coe FL: Renal histopathology and crystal deposits in patients with
small bowel resection and calcium oxalate stone disease. Kidney
Int. 78:310–317. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Obligado SH and Goldfarb DS: The
association of nephrolithiasis with hypertension and obesity: A
review. Am J Hypertens. 21:257–264. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Borghi L, Meschi T, Guerra A, Briganti A,
Schianchi T, Allegri F and Novarini A: Essential arterial
hypertension and stone disease. Kidney Int. 55:2397–2406. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pak CY: Kidney stones. Lancet.
351:1797–1801. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Lohi H, Kujala M, Kerkelä E,
Saarialho-Kere U, Kestilä M and Kere J: Mapping of five new
putative anion transporter genes in human and characterization of
SLC26A6, a candidate gene for pancreatic anion exchanger. Genomics.
70:102–112. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kleta R: A key stone cop regulates oxalate
homeostasis. Nat Genet. 38:403–404. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Evan AP, Lingeman JE, Coe FL, Parks JH,
Bledsoe SB, Shao Y, Sommer AJ, Paterson RF, Kuo RL and Grynpas M:
Randall's plaque of patients with nephrolithiasis begins in
basement membranes of thin loops of Henle. J Clin Invest.
111:607–616. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Moe OW and Preisig PA: Dual role of
citrate in mammalian urine. Curr Opin Nephrol Hypertens.
15:419–424. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Noori N, Honarkar E, Goldfarb DS,
Kalantar-Zadeh K, Taheri M, Shakhssalim N, Parvin M and Basiri A:
Urinary lithogenic risk profile in recurrent stone formers with
hyperoxaluria: A randomized controlled trial comparing DASH
(Dietary Approaches to Stop Hypertension)-style and low-oxalate
diets. Am J Kidney Dis. 63:456–463. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Khan A: Prevalence, pathophysiological
mechanisms and factors affecting urolithiasis. Int Urol Nephrol.
50:799–806. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shimshilashvili L, Aharon S, Moe OW and
Ohana E: Novel human polymorphisms define a key role for the
SLC26A6-STAS domain in protection from ca2+-oxalate
lithogenesis. Front Pharmacol. 11:4052020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hamm LL: Renal handling of citrate. Kidney
Int. 38:728–735. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
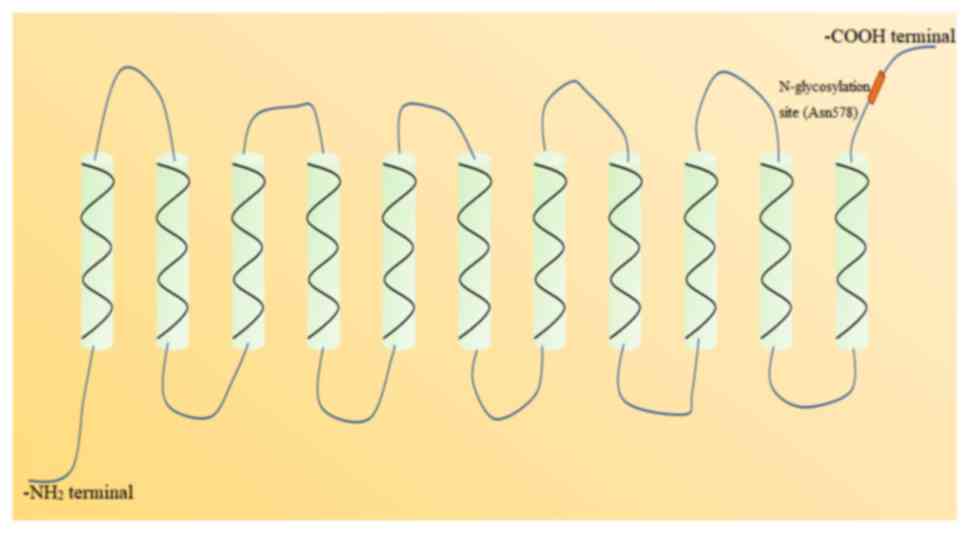
Pajor AM: Sequence and functional
characterization of a renal sodium/dicarboxylate cotransporter. J
Biol Chem. 270:5779–5785. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
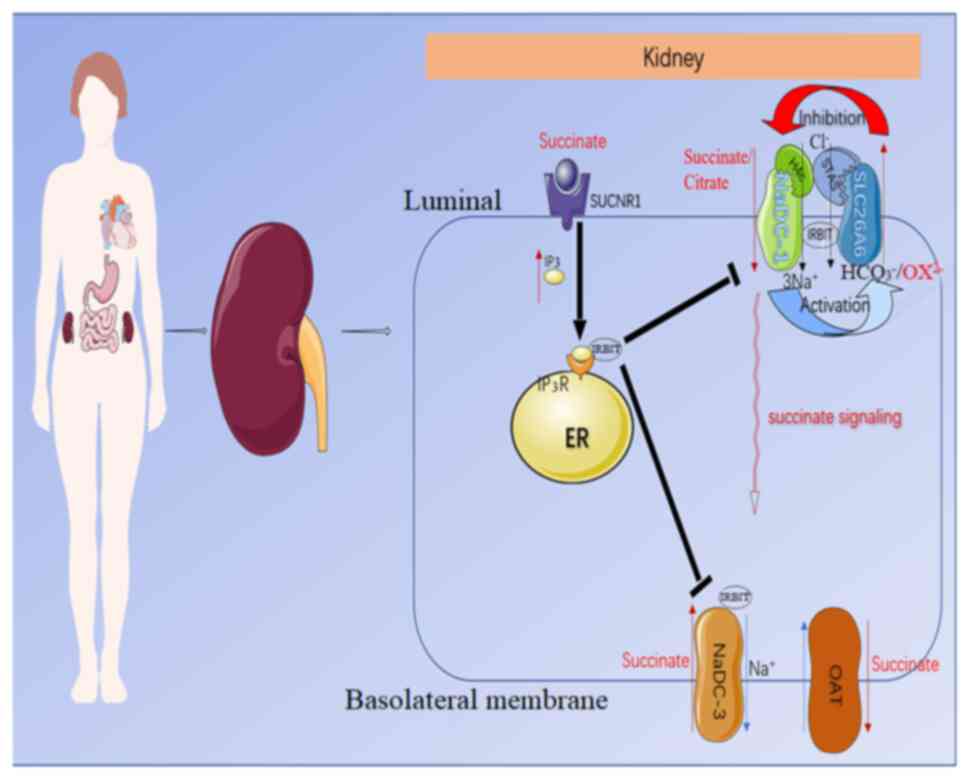
Ohana E, Shcheynikov N, Moe OW and Muallem
S: SLC26A6 and NaDC-1 transporters interact to regulate oxalate and
citrate homeostasis. J Am Soc Nephrol. 24:1617–1626. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Prakash S, Cooper G, Singhi S and Saier MH
Jr: The ion transporter superfamily. Biochim Biophys Acta.
1618:79–92. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Aguiar CJ, Andrade VL, Gomes ER, Alves MN,
Ladeira MS, Pinheiro AC, Gomes DA, Almeida AP, Goes AM, Resende RR,
et al: Succinate modulates Ca(2+) transient and cardiomyocyte
viability through PKA-dependent pathway. Cell Calcium. 47:37–46.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Vargas SL, Toma I, Kang JJ, Meer EJ and
Peti-Peterdi J: Activation of the succinate receptor GPR91 in
macula densa cells causes renin release. J Am Soc Nephrol.
20:1002–1011. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
He W, Miao FJ, Lin DC, Schwandner RT, Wang
Z, Gao J, Chen JL, Tian H and Ling L: Citric acid cycle
intermediates as ligands for orphan G-protein-coupled receptors.
Nature. 429:188–193. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Baumbach L, Leyssac PP and Skinner SL:
Studies on renin release from isolated superfused glomeruli:
Effects of temperature, urea, ouabain and ethacrynic acid. J
Physiol. 258:243–256. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Alper SL and Sharma AK: The SLC26 gene
family of anion transporters and channels. Mol Aspects Med.
34:494–515. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dorwart MR, Shcheynikov N, Yang D and
Muallem S: The solute carrier 26 family of proteins in epithelial
ion transport. Physiology (Bethesda). 23:104–114. 2008.PubMed/NCBI
|
|
22
|
Price GD and Howitt SM: The cyanobacterial
bicarbonate transporter BicA: Its physiological role and the
implications of structural similarities with human SLC26
transporters. Biochem Cell Biol. 89:178–188. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
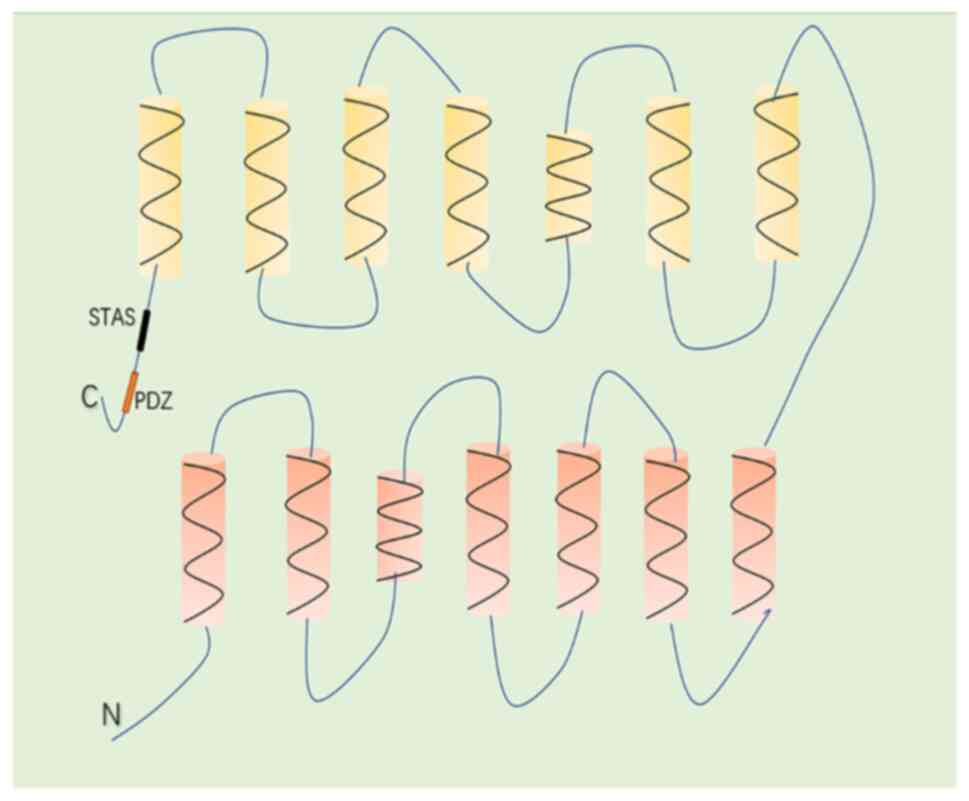
Wang J, Wang W, Wang H and Tuo B:
Physiological and pathological functions of SLC26A6. Front Med
(Lausanne). 7:6182562021. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bai X, Chen X, Feng Z, Hou K, Zhang P, Fu
B and Shi S: Identification of basolateral membrane targeting
signal of human sodium-dependent dicarboxylate transporter 3. J
Cell Physiol. 206:821–830. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Waldegger S, Moschen I, Ramirez A, Smith
RJ, Ayadi H, Lang F and Kubisch C: Cloning and characterization of
SLC26A6, a novel member of the solute carrier 26 gene family.
Genomics. 72:43–50. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Geertsma ER, Chang YN, Shaik FR, Neldner
Y, Pardon E, Steyaert J and Dutzler R: Structure of a prokaryotic
fumarate transporter reveals the architecture of the SLC26 family.
Nat Struct Mol Biol. 22:803–808. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ko SB, Zeng W, Dorwart MR, Luo X, Kim KH,
Millen L, Goto H, Naruse S, Soyombo A, Thomas PJ and Muallem S:
Gating of CFTR by the STAS domain of SLC26 transporters. Nat Cell
Biol. 6:343–350. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Malakooti J, Saksena S, Gill RK and Dudeja
PK: Transcriptional regulation of the intestinal luminal
Na+ and Cl− transporters. Biochem J.
435:313–325. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lohi H, Lamprecht G, Markovich D, Heil A,
Kujala M, Seidler U and Kere J: Isoforms of SLC26A6 mediate anion
transport and have functional PDZ interaction domains. Am J Physiol
Cell Physiol. 284:C769–C779. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Poole DF and Tyler JE: Oxalic
acid-produced surface phenomena on human enamel examined by
scanning electron microscopy. Arch Oral Biol. 15:1157–1162. 1970.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Sirish P, Ledford HA, Timofeyev V, Thai
PN, Ren L, Kim HJ, Park S, Lee JH, Dai G, Moshref M, et al: Action
potential shortening and impairment of cardiac function by ablation
of Slc26a6. Circ Arrhythm Electrophysiol. 10:e0052672017.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wang Z, Petrovic S, Mann E and Soleimani
M: Identification of an apical Cl(−)/HCO3(−) exchanger in the small
intestine. Am J Physiol Gastrointest Liver Physiol. 282:G573–G579.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Freel RW, Hatch M, Green M and Soleimani
M: Ileal oxalate absorption and urinary oxalate excretion are
enhanced in Slc26a6 null mice. Am J Physiol Gastrointest Liver
Physiol. 290:G719–G728. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ishiguro H, Yamamoto A, Nakakuki M, Yi L,
Ishiguro M, Yamaguchi M, Kondo S and Mochimaru Y: Physiology and
pathophysiology of bicarbonate secretion by pancreatic duct
epithelium. Nagoya J Med Sci. 74:1–18. 2012.PubMed/NCBI
|
|
35
|
Wang Z, Wang T, Petrovic S, Tuo B,
Riederer B, Barone S, Lorenz JN, Seidler U, Aronson PS and
Soleimani M: Renal and intestinal transport defects in Slc26a6-null
mice. Am J Physiol Cell Physiol. 288:C957–C965. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Gholami K, Muniandy S and Salleh N:
In-vivo functional study on the involvement of CFTR, SLC26A6, NHE-1
and CA isoenzymes II and XII in uterine fluid pH, volume and
electrolyte regulation in rats under different sex-steroid
influence. Int J Med Sci. 10:1121–1134. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Knauf F, Yang CL, Thomson RB, Mentone SA,
Giebisch G and Aronson PS: Identification of a chloride-formate
exchanger expressed on the brush border membrane of renal proximal
tubule cells. Proc Natl Acad Sci USA. 98:9425–9430. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Chernova MN, Jiang L, Friedman DJ, Darman
RB, Lohi H, Kere J, Vandorpe DH and Alper SL: Functional comparison
of mouse slc26a6 anion exchanger with human SLC26A6 polypeptide
variants: Differences in anion selectivity, regulation, and
electrogenicity. J Biol Chem. 280:8564–8580. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Clark JS, Vandorpe DH, Chernova MN,
Heneghan JF, Stewart AK and Alper SL: Species differences in
Cl− affinity and in electrogenicity of SLC26A6-mediated
oxalate/Cl− exchange correlate with the distinct human
and mouse susceptibilities to nephrolithiasis. J Physiol.
586:1291–1306. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Jiang Z, Grichtchenko II, Boron WF and
Aronson PS: Specificity of anion exchange mediated by mouse
Slc26a6. J Biol Chem. 277:33963–33967. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Xie Q, Welch R, Mercado A, Romero MF and
Mount DB: Molecular characterization of the murine Slc26a6 anion
exchanger: Functional comparison with Slc26a1. Am J Physiol Renal
Physiol. 283:F826–F838. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Aronson PS: Ion exchangers mediating Na+,
HCO3− and Cl− transport in the
renal proximal tubule. J Nephrol. 19 (Suppl 9):S3–S10.
2006.PubMed/NCBI
|
|
43
|
Jiang Z, Asplin JR, Evan AP, Rajendran VM,
Velazquez H, Nottoli TP, Binder HJ and Aronson PS: Calcium oxalate
urolithiasis in mice lacking anion transporter Slc26a6. Nat Genet.
38:474–478. 2006. View
Article : Google Scholar : PubMed/NCBI
|
|
44
|
Markovich D and Murer H: The SLC13 gene
family of sodium sulphate/carboxylate cotransporters. Pflugers
Arch. 447:594–602. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Markovich D, Forgo J, Stange G, Biber J
and Murer H: Expression cloning of rat renal Na+/SO4(2-)
cotransport. Proc Natl Acad Sci USA. 90:8073–8077. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Bai L and Pajor AM: Expression cloning of
NaDC-2, an intestinal Na(+)- or Li(+)-dependent dicarboxylate
transporter. Am J Physiol. 273((2 Pt 1)): G267–G274.
1997.PubMed/NCBI
|
|
47
|
Steffgen J, Burckhardt BC, Langenberg C,
Kühne L, Müller GA, Burckhardt G and Wolff NA: Expression cloning
and characterization of a novel sodium-dicarboxylate cotransporter
from winter flounder kidney. J Biol Chem. 274:20191–20196. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Pajor AM: Molecular cloning and functional
expression of a sodium-dicarboxylate cotransporter from human
kidney. Am J Physiol. 270((4 Pt 2)): F642–F648. 1996.PubMed/NCBI
|
|
49
|
Pajor AM and Sun NN: Molecular cloning,
chromosomal organization, and functional characterization of a
sodium-dicarboxylate cotransporter from mouse kidney. Am J Physiol
Renal Physiol. 279:F482–F490. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Khatri IA, Kovacs SV and Forstner JF:
Cloning of the cDNA for a rat intestinal Na+/dicarboxylate
cotransporter reveals partial sequence homology with a rat
intestinal mucin. Biochim Biophys Acta. 1309:58–62. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Sekine T, Cha SH, Hosoyamada M, Kanai Y,
Watanabe N, Furuta Y, Fukuda K, Igarashi T and Endou H: Cloning,
functional characterization, and localization of a rat renal
Na+-dicarboxylate transporter. Am J Physiol. 275:F298–F305.
1998.PubMed/NCBI
|
|
52
|
Chen XZ, Shayakul C, Berger UV, Tian W and
Hediger MA: Characterization of a rat Na+-dicarboxylate
cotransporter. J Biol Chem. 273:20972–20981. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Mann SS, Hart T, Pettenati MJ, von
Kap-herr C and Holmes RP: Assignment of the sodium-dependent
dicarboxylate transporter gene (SLC13A2 alias NaDC-1) to human
chromosome region 17p11.1->q11.1 by radiation hybrid mapping and
fluorescence in situ hybridization. Cytogenet Cell Genet. 84:89–90.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Pajor AM: Molecular properties of
sodium/dicarboxylate cotransporters. J Membr Biol. 175:1–8. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Pajor AM: Sodium-coupled transporters for
Krebs cycle intermediates. Annu Rev Physiol. 61:663–682. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Hamm LL: Renal handling of citrate. Kidney
Int. 38:728–735. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Aronson PS: Essential roles of
CFEX-mediated Cl(−)-oxalate exchange in proximal tubule NaCl
transport and prevention of urolithiasis. Kidney Int. 70:1207–1213.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Brennan TS, Klahr S and Hamm LL: Citrate
transport in rabbit nephron. Am J Physiol. 251((4 Pt 2)):
F683–F689. 1986.PubMed/NCBI
|
|
59
|
Shcheynikov N, Wang Y, Park M, Ko SB,
Dorwart M, Naruse S, Thomas PJ and Muallem S: Coupling modes and
stoichiometry of Cl-/HCO3− exchange by
slc26a3 and slc26a6. J Gen Physiol. 127:511–524. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Khamaysi A, Anbtawee-Jomaa S, Fremder M,
Eini-Rider H, Shimshilashvili L, Aharon S, Aizenshtein E, Shlomi T,
Noguchi A, Springer D, et al: Systemic succinate homeostasis and
local succinate signaling affect blood pressure and modify risks
for calcium oxalate lithogenesis. J Am Soc Nephrol. 30:381–392.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Mancusso R, Gregorio GG, Liu Q and Wang
DN: Structure and mechanism of a bacterial sodium-dependent
dicarboxylate transporter. Nature. 491:622–626. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Robben JH, Fenton RA, Vargas SL, Schweer
H, Peti-Peterdi J, Deen PM and Milligan G: Localization of the
succinate receptor in the distal nephron and its signaling in
polarized MDCK cells. Kidney Int. 76:1258–1267. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Sundstrom L, Greasley PJ, Engberg S,
Wallander M and Ryberg E: Succinate receptor GPR91, a Gaα(i)
coupled receptor that increases intracellular calcium
concentrations through PLCβ. FEBS Lett. 587:2399–2404. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Ando H, Mizutani A, Matsu-ura T and
Mikoshiba K: IRBIT, a novel inositol 1,4,5-trisphosphate (IP3)
receptor-binding protein, is released from the IP3 receptor upon
IP3 binding to the receptor. J Biol Chem. 278:10602–10612. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Park S, Shcheynikov N, Hong JH, Zheng C,
Suh SH, Kawaai K, Ando H, Mizutani A, Abe T, Kiyonari H, et al:
Irbit mediates synergy between ca(2+) and cAMP signaling pathways
during epithelial transport in mice. Gastroenterology. 145:232–241.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Lungkaphin A, Lewchalermwongse B and
Chatsudthipong V: Relative contribution of OAT1 and OAT3 transport
activities in isolated perfused rabbit renal proximal tubules.
Biochim Biophys Acta. 1758:789–795. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Okamoto N, Aruga S, Tomita K, Takeuchi T
and Kitamura T: Chronic acid ingestion promotes renal stone
formation in rats treated with vitamin D3. Int J Urol. 14:60–66.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Monico CG, Weinstein A, Jiang Z, Jiang Z,
Rohlinger AL, Cogal AG, Bjornson BB, Olson JB, Bergstralh EJ,
Milliner DS and Aronson PS: Phenotypic and functional analysis of
human SLC26A6 variants in patients with familial hyperoxaluria and
calcium oxalate nephrolithiasis. Am J Kidney Dis. 52:1096–1103.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Jiang H, Pokhrel G, Chen Y, Wang T, Yin C,
Liu J, Wang S and Liu Z: High expression of SLC26A6 in the kidney
may contribute to renal calcification via an SLC26A6-dependent
mechanism. PeerJ. 6:e51922018. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Khan SR, Khan A and Byer KJ: Temporal
changes in the expression of mRNA of NADPH oxidase subunits in
renal epithelial cells exposed to oxalate or calcium oxalate
crystals. Nephrol Dial Transplant. 26:1778–1785. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Jiang H, Gao X, Gong J, Yang Q, Lan R,
Wang T, Liu J, Yin C, Wang S and Liu Z: Downregulated expression of
solute carrier family 26 member 6 in NRK-52E cells attenuates
oxalate-induced intracellular oxidative stress. Oxid Med Cell
Longev. 2018:17246482018. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Lu X, Sun D, Xu B, Pan J, Wei Y, Mao X, Yu
D, Liu H and Gao B: In silico screening and molecular dynamic study
of nonsynonymous single nucleotide polymorphisms associated with
kidney stones in the SLC26A6 gene. J Urol. 196:118–123. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Corbetta S, Eller-Vainicher C, Frigerio M,
Valaperta R, Costa E, Vicentini L, Baccarelli A, Beck-Peccoz P and
Spada A: Analysis of the 206M polymorphic variant of the SLC26A6
gene encoding a Cl− oxalate transporter in patients with
primary hyperparathyroidism. Eur J Endocrinol. 160:283–288. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Udomsilp P, Saepoo S, Ittiwut R,
Shotelersuk V, Dissayabutra T, Boonla C and Tosukhowong P:
rs11567842 SNP in SLC13A2 gene associates with hypocitraturia in
Thai patients with nephrolithiasis. Genes Genomics. 40:965–972.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Bosch B and De Boeck K: Searching for a
cure for cystic fibrosis. A 25-year quest in a nutshell. Eur J
Pediatr. 175:1–8. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Bissig M, Hagenbuch B, Stieger B, Koller T
and Meier PJ: Functional expression cloning of the canalicular
sulfate transport system of rat hepatocytes. J Biol Chem.
269:3017–21. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Regeer RR and Markovich D: A dileucine
motif targets the sulfate anion transporter sat-1 to the
basolateral membrane in renal cell lines. Am. J. Physiol. 287((2)):
C365–C372. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Hästbacka J, de la Chapelle A, Mahtani MM,
Clines G, Reeve-Daly MP, Daly M, Hamilton BA, Kusumi K, Trivedi B,
et al: The diastrophic dysplasia gene encodes a novel sulfate
transporter: positional cloning by fine-structure linkage
disequilibrium mapping. Cell. 78((6)): 1073–1087. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Heneghan JF, Akhavein A, Salas MJ,
Shmukler BE, Karniski LP, Vandorpe DH and Alper SL: Regulated
transport of sulfate and oxalate by SLC26A2/DTDST. Am J Physiol
Cell Physiol. 298((6)): C1363-75. doi: 10.1152/ajpcell.00004.2010.
Epub 2010 Mar 10. Erratum in: Am J Physiol Cell Physiol. 2011 Feb;
300(2): C383. PMID: 20219950; PMCID: PMC2889644. PubMed/NCBI
|
|
80
|
Haila S, Hästbacka J, Böhling T,
Karjalainen-Lindsberg ML, Kere J and Saarialho-Kere U: SLC26A2
(diastrophic dysplasia sulfate transporter) is expressed in
developing and mature cartilage but also in other tissues and cell
types. J Histochem. Cytochem. 49((8)): 973–982. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Hoglund P, Haila S, Socha J, Tomaszewski
L, Saarialho-Kere U, Karjalainen-Lindsberg ML, Airola K, Holmberg
C, de la Chapelle A and Kere J: Mutations of the Down-regulated in
adenoma (DRA) gene cause congenital chloride diarrhoea. Nat Genet.
14:316–319. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Chernova MN, Jiang L, Shmukler BE,
Schweinfest CW, Blanco P, Freedman SD, Stewart AK and Alper SL:
Acute regulation of the SLC26A3 congenital chloride diarrhoea anion
exchanger (DRA) expressed in Xenopus oocytes. J Physiol. 549((Pt
1)): 3–19. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Sheffield VC, Kraiem Z, Beck JC, Nishimura
D, Stone EM, Salameh M, Sadeh O and Glaser B: Pendred syndrome maps
to chromosome 7q21-34 and is caused by an intrinsic defect in
thyroid iodine organification. Nat Genet. 12:424–426. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Shcheynikov N, Yang D, Wang Y, Zeng W,
Karniski LP, So I, Wall SM and Muallem S: The Slc26a4 transporter
functions as an electroneutral Cl-/I-/HCO3−
exchanger: Role of Slc26a4 and Slc26a6 in I- and
HCO3− secretion and in regulation of CFTR in
the parotid duct. J Physiol. 586:3813–3824. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Liu XZ, Ouyang XM, Xia XJ, Zheng J, Pandya
A, Li F, Du LL, Welch KO, Petit C, Smith RJ, et al: Prestin, a
cochlear motor protein, is defective in non-syndromic hearing loss.
Hum Mol Genet. 12:1155–1162. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Alvarez BV, Kieller DM, Quon AL, Markovich
D and Casey JR: Slc26a6: A cardiac chloride-hydroxyl exchanger and
predominant chloride-bicarbonate exchanger of the mouse heart. J
Physiol. 561((Pt 3)): 721–734. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Petrovic S, Amlal H, Sun X, Karet F,
Barone S and Soleimani M: Vasopressin induces expression of the
Cl-/HCO3− exchanger SLC26A7 in kidney
medullary collecting ducts of Brattleboro rats. Am J Physiol Renal
Physiol. 290:F1194–F1201. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Dudas PL, Mentone S, Greineder CF,
Biemesderfer D and Aronson PS: Immunolocalization of anion
transporter Slc26a7 in mouse kidney. Am J Physiol Renal Physiol.
290:F937–F945. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Toure A, Morin L, Pineau C, Becq F,
Dorseuil O and Gacon G: Tat1, a novel sulfate transporter
specifically expressed in human male germ cells and potentially
linked to rhogtpase signaling. J Biol Chem. 276:20309–20315. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Lohi H, Kujala M, Makela S, Lehtonen E,
Kestila M, Saarialho-Kere U, Markovich D and Kere J: Functional
characterization of three novel tissue-specific anion exchangers
SLC26A7, -A8, and -A9. J Biol Chem. 277:14246–14254. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Loriol C, Dulong S, Avella M, Gabillat N,
Boulukos K, Borgese F and Ehrenfeld J: Characterization of SLC26A9,
facilitation of Cl (−) transport by bicarbonate. Cell Physiol
Biochem. 22:15–30. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Wang J, Chen X, Liu B and Zhu Z:
Suppression of PTP1B in gastric cancer cells in vitro induces a
change in the genome-wide expression profile and inhibits gastric
cancer cell growth. Cell Biol Int. 34:747–753. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Stewart AK, Shmukler BE, Vandorpe DH,
Reimold F, Heneghan JF, Nakakuki M, Akhavein A, Ko S, Ishiguro H
and Alper SL: SLC26 anion exchangers of guinea pig pancreatic duct:
Molecular cloning and functional characterization. Am J Physiol
Cell Physiol. 301:C289–C303. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Ouesleti S, Brunel V, Ben Turkia H,
Dranguet H, Miled A, Miladi N, Ben Dridi MF, Lavoinne A,
Saugier-Veber P and Bekri S: Molecular characterization of MPS
IIIA, MPS IIIB and MPS IIIC in Tunisian patients. Clin Chim Acta.
412:2326–2331. 2011. View Article : Google Scholar : PubMed/NCBI
|