|
1
|
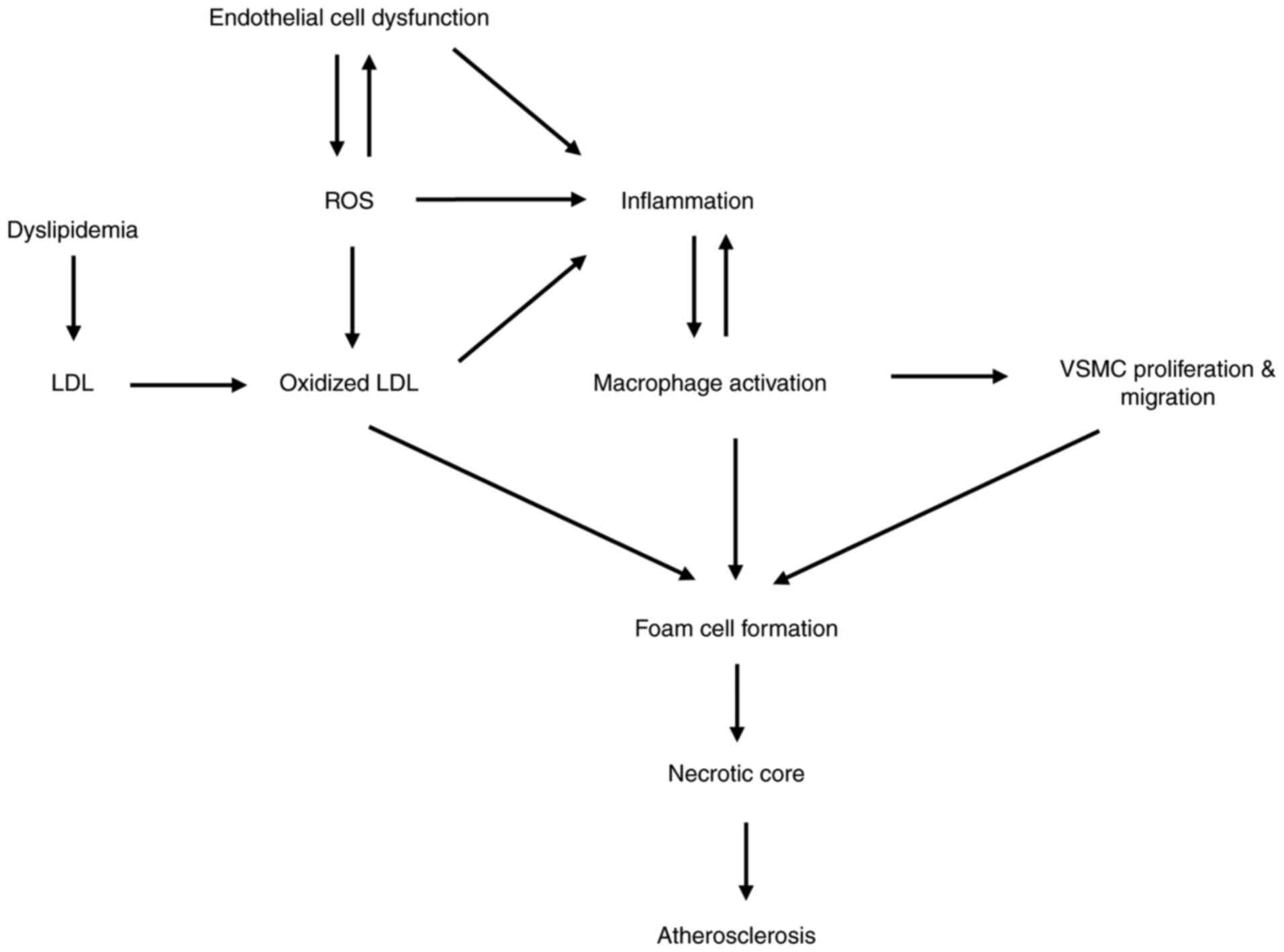
Libby P, Ridker PM and Hansson GK:
Progress and challenges in translating the biology of
atherosclerosis. Nature. 473:317–325. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gimbrone MA Jr and Garcia-Cardena G:
Endothelial cell dysfunction and the pathobiology of
atherosclerosis. Circ Res. 118:620–636. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Sena CM, Leandro A, Azul L, Seica R and
Perry G: Vascular oxidative stress: Impact and therapeutic
approaches. Front Physiol. 9:16682018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chistiakov DA, Orekhov AN and Bobryshev
YV: Effects of shear stress on endothelial cells: Go with the flow.
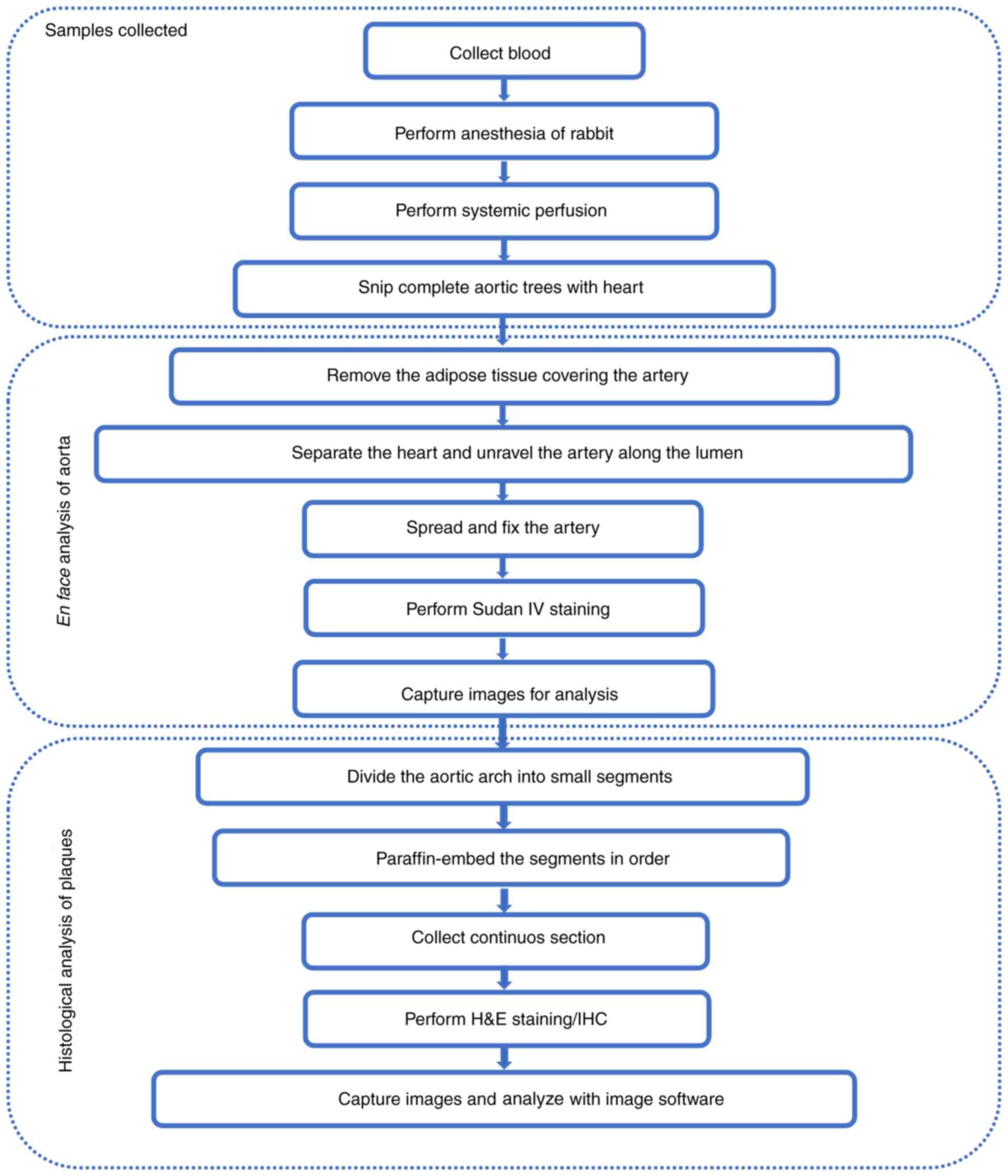
Acta Physiol (Oxf). 219:382–408. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Moore KJ, Sheedy FJ and Fisher EA:
Macrophages in atherosclerosis: A dynamic balance. Nat Rev Immunol.
13:709–721. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chistiakov DA, Melnichenko AA, Myasoedova
VA, Grechko AV and Orekhov AN: Mechanisms of foam cell formation in
atherosclerosis. J Mol Med (Berl). 95:1153–1165. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bennett MR, Sinha S and Owens GK: Vascular
smooth muscle cells in atherosclerosis. Circ Res. 118:692–702.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Davignon J and Ganz P: Role of endothelial
dysfunction in atherosclerosis. Circulation. 109 (23 Suppl
1):III27–III32. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Incalza MA, D'Oria R, Natalicchio A,
Perrini S, Laviola L and Giorgino F: Oxidative stress and reactive
oxygen species in endothelial dysfunction associated with
cardiovascular and metabolic diseases. Vascul Pharmacol. 100:1–19.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hajjar DP and Gotto AM Jr: Biological
relevance of inflammation and oxidative stress in the pathogenesis
of arterial diseases. Am J Pathol. 182:1474–1481. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rhoads JP and Major AS: How oxidized
low-density lipoprotein activates inflammatory responses. Crit Rev
Immunol. 38:333–342. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhang T, Chen J, Tang X, Luo Q, Xu D and
Yu B: Interaction between adipocytes and high-density lipoprotein:
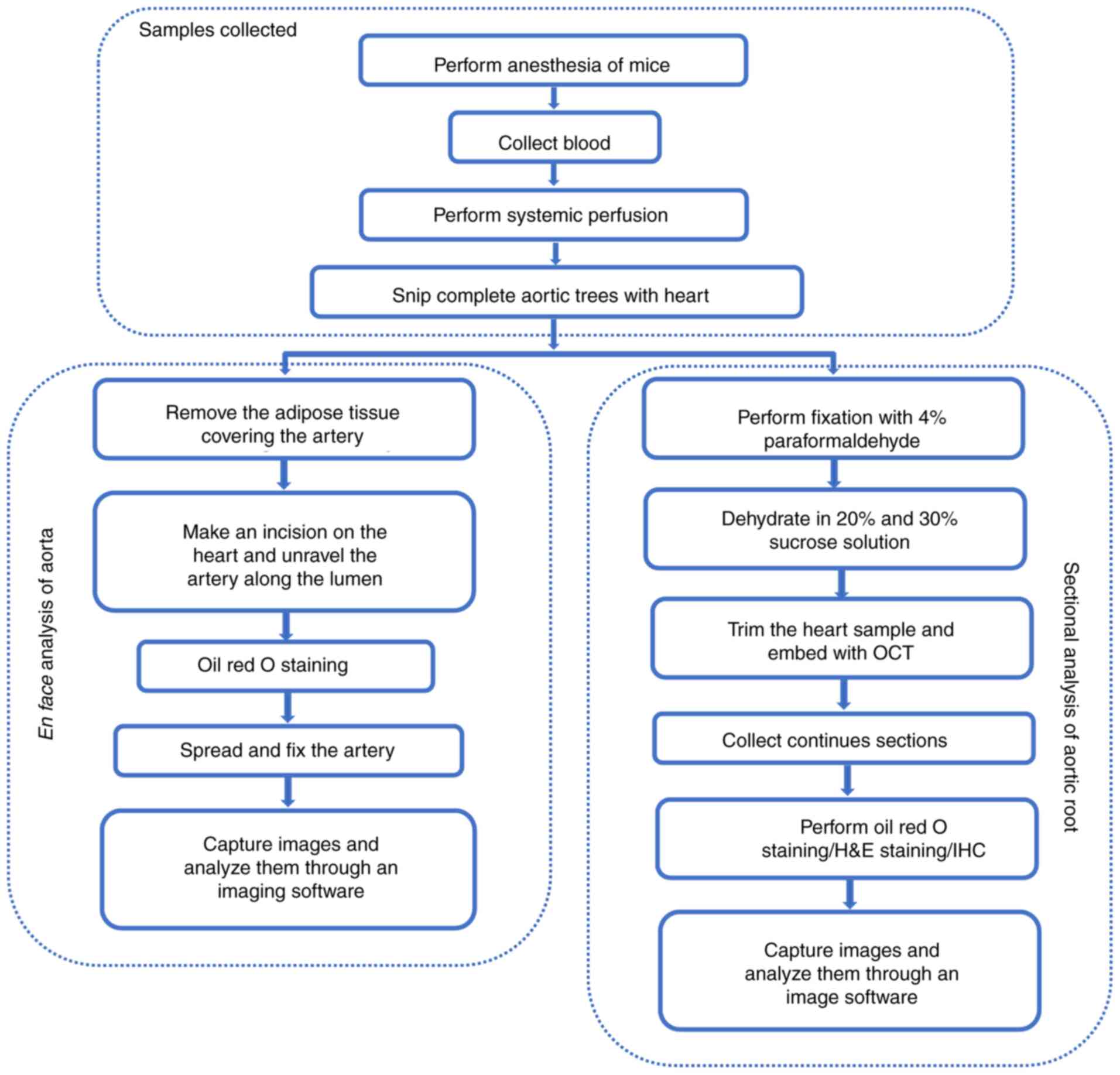
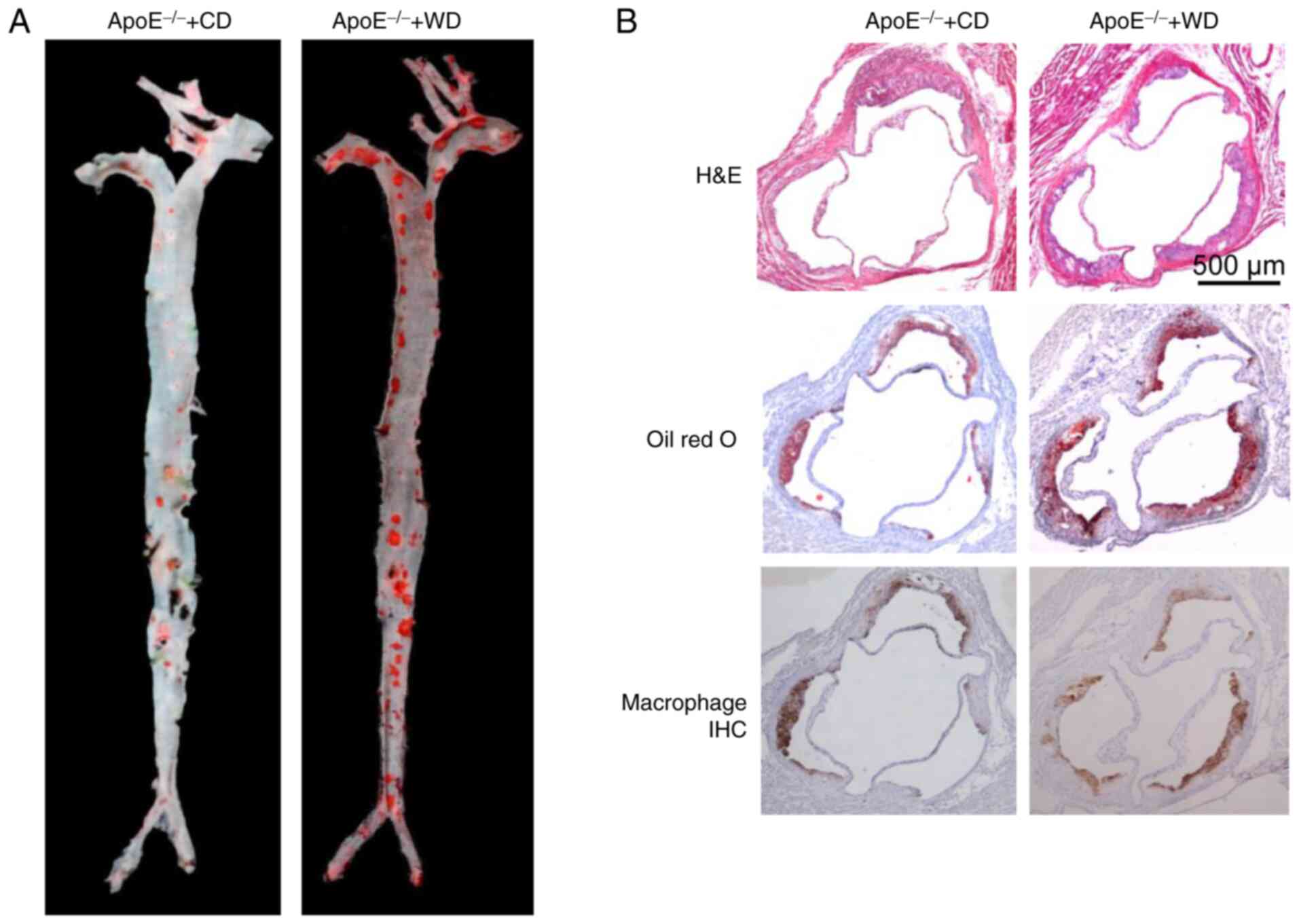
New insights into the mechanism of obesity-induced dyslipidemia and
atherosclerosis. Lipids Health Dis. 18:2232019. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ference BA, Ginsberg HN, Graham I, Ray KK,
Packard CJ, Bruckert E, Hegele RA, Krauss RM, Raal FJ, Schunkert H,
et al: Low-density lipoproteins cause atherosclerotic
cardiovascular disease. 1. Evidence from genetic, epidemiologic,
and clinical studies. A consensus statement from the European
atherosclerosis society consensus panel. Eur Heart J. 38:2459–2472.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Messner B and Bernhard D: Smoking and
cardiovascular disease: Mechanisms of endothelial dysfunction and
early atherogenesis. Arterioscler Thromb Vasc Biol. 34:509–515.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Altman R: Risk factors in coronary
atherosclerosis athero-inflammation: The meeting point. Thromb J.
1:42003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hollander W: Role of hypertension in
atherosclerosis and cardiovascular disease. Am J Cardiol.
38:786–800. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Katakami N: Mechanism of development of
atherosclerosis and cardiovascular disease in diabetes mellitus. J
Atheroscler Thromb. 25:27–39. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Virani SS, Alonso A, Benjamin EJ,
Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR,
Cheng S, Delling FN, et al: Heart disease and stroke
statistics-2020 update: A report from the american heart
association. Circulation. 141:e139–e596. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lenfant C and Savage PJ: The early natural
history of atherosclerosis and hypertension in the young: National
institutes of health perspectives. Am J Med Sci. 310 (Suppl
1):S3–S7. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
McNamara JJ, Molot MA, Stremple JF and
Cutting RT: Coronary artery disease in combat casualties in
Vietnam. JAMA. 216:1185–1187. 1971. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Strong JP, Mcgill HC Jr, Tejada C and
Holman RL: The natural history of atherosclerosis; comparison of
the early aortic lesions in New Orleans, Guatemala, and Costa Rica.
Am J Pathol. 34:731–744. 1958.PubMed/NCBI
|
|
22
|
Enos WF, Holmes RH and Beyer J: Coronary
disease among United States soldiers killed in action in Korea;
preliminary report. J Am Med Assoc. 152:1090–1093. 1953. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Konstantinov IE and Jankovic GM: Alexander
I. Ignatowski: A pioneer in the study of atherosclerosis. Tex Heart
Inst J. 40:246–249. 2013.PubMed/NCBI
|
|
24
|
Daugherty A, Tall AR, Daemen M, Falk E,
Fisher EA, García-Cardeña G, Lusis AJ, Owens AP III, Rosenfeld ME,
Virmani R, et al: Recommendation on design, execution, and
reporting of animal atherosclerosis studies: A scientific statement
from the american heart association. Arterioscler Thromb Vasc Biol.
37:e131–e157. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wu C, Daugherty A and Lu HS: Updates on
approaches for studying atherosclerosis. Arterioscler Thromb Vasc
Biol. 39:e108–e117. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Fan J, Chen Y, Yan H, Niimi M, Wang Y and
Liang J: Principles and applications of rabbit models for
atherosclerosis research. J Atheroscler Thromb. 25:213–220. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Vesselinovitch D, Wissler RW and Doull J:
Experimental production of atherosclerosis in mice. 1. Effect of
various synthetic diets and radiation on survival time, food
consumption and body weight in mice. J Atheroscler Res. 8:483–495.
1968. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Vesselinovitch D and Wissler RW:
Experimental production of atherosclerosis in mice. 2. Effects of
atherogenic and high-fat diets on vascular changes in chronically
and acutely irradiated mice. J Atheroscler Res. 8:497–523. 1968.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Thompson JS: Atheromata in an inbred
strain of mice. J Atheroscler Res. 10:113–122. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Paigen B, Morrow A, Brandon C, Mitchell D
and Holmes P: Variation in susceptibility to atherosclerosis among
inbred strains of mice. Atherosclerosis. 57:65–73. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ishibashi S, Brown MS, Goldstein JL,
Gerard RD, Hammer RE and Herz J: Hypercholesterolemia in low
density lipoprotein receptor knockout mice and its reversal by
adenovirus-mediated gene delivery. J Clin Invest. 92:883–893. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Plump AS, Smith JD, Hayek T, Aalto-Setälä
K, Walsh A, Verstuyft JG, Rubin EM and Breslow JL: Severe
hypercholesterolemia and atherosclerosis in apolipoprotein
E-deficient mice created by homologous recombination in ES cells.
Cell. 71:343–353. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Piedrahita JA, Zhang SH, Hagaman JR,
Oliver PM and Maeda N: Generation of mice carrying a mutant
apolipoprotein E gene inactivated by gene targeting in embryonic
stem cells. Proc Natl Acad Sci USA. 89:4471–4475. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Olszanecki R and Korbut R: The effect of
montelukast on atherogenesis in apoE/LDLR-double knockout mice. J
Physiol Pharmacol. 59:633–639. 2008.PubMed/NCBI
|
|
35
|
Olszanecki R, Jawien J, Gajda M, Mateuszuk
L, Gebska A, Korabiowska M, Chłopicki S and Korbut R: Effect of
curcumin on atherosclerosis in apoE-LDLR-double knockout mice. J
Physiol Pharmacol. 4:627–635. 2005.PubMed/NCBI
|
|
36
|
Schilperoort M, van den Berg R, Bosmans
LA, van Os BW, Dollé ME, Smits NA, Guichelaar T, van Baarle D,
Koemans L, Berbée JF, et al: Disruption of circadian rhythm by
alternating light-dark cycles aggravates atherosclerosis
development in APOE* 3-leiden. CETP mice. J Pineal Res.
68:e126142020. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Berbée JF, Wong MC, Wang Y, van der Hoorn
JW, Khedoe PP, van Klinken JB, Mol IM, Hiemstra PS, Tsikas D,
Romijn JA, et al: Resveratrol protects against atherosclerosis, but
does not add to the antiatherogenic effect of atorvastatin, in
APOE* 3-leiden. CETP mice. J Nutr Biochem. 24:1423–1430. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
de Haan W, van der Hoogt CC, Westerterp M,
Hoekstra M, Dallinga-Thie GM, Princen HM, Romijn JA, Jukema JW,
Havekes LM and Rensen PC: Atorvastatin increases HDL cholesterol by
reducing CETP expression in cholesterol-fed APOE* 3-leiden. CETP
mice. Atherosclerosis. 197:57–63. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Stein EA and Raal F: Reduction of
low-density lipoprotein cholesterol by monoclonal antibody
inhibition of PCSK9. Annu Rev Med. 65:417–431. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Getz GS and Reardon CA: Apoprotein E as a
lipid transport and signaling protein in the blood, liver, and
artery wall. J Lipid Res (50 Suppl). S156–S161. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Sehayek E, Shefer S, Nguyen LB, Ono JG,
Merkel M and Breslow JL: Apolipoprotein E regulates dietary
cholesterol absorption and biliary cholesterol excretion: studies
in C57BL/6 apolipoprotein E knockout mice. Proc Natl Acad Sci USA.
97:3433–3437. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Plump AS and Breslow JL: Apolipoprotein E
and the apolipoprotein E-deficient mouse. Annu Rev Nutr.
15:495–518. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Nakashima Y, Plump AS, Raines EW, Breslow
JL and Ross R: ApoE-deficient mice develop lesions of all phases of
atherosclerosis throughout the arterial tree. Arterioscler Thromb.
14:133–140. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Rattazzi M, Bennett BJ, Bea F, Kirk EA,
Ricks JL, Speer M, Schwartz SM, Giachelli CM and Rosenfeld ME:
Calcification of advanced atherosclerotic lesions in the innominate
arteries of ApoE-deficient mice: Potential role of chondrocyte-like
cells. Arterioscler Thromb Vasc Biol. 25:1420–1425. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Meir KS and Leitersdorf E: Atherosclerosis
in the apolipoprotein-E-deficient mouse: a decade of progress.
Arterioscler Thromb Vasc Biol. 24:1006–1014. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Oppi S, Luscher TF and Stein S: Mouse
models for atherosclerosis research-which is my line? Front
Cardiovasc Med. 6:462019. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
von Scheidt M, Zhao Y, Kurt Z, Pan C, Zeng
L, Yang X, Schunkert H and Lusis AJ: Applications and limitations
of mouse models for understanding human atherosclerosis. Cell
Metab. 25:248–261. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Moore KJ, Kunjathoor VV, Koehn SL, Manning
JJ, Tseng AA, Silver JM, McKee M and Freeman MW: Loss of
receptor-mediated lipid uptake via scavenger receptor A or CD36
pathways does not ameliorate atherosclerosis in hyperlipidemic
mice. J Clin Invest. 115:2192–2201. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Go GW and Mani A: Low-density lipoprotein
receptor (LDLR) family orchestrates cholesterol homeostasis. Yale J
Biol Med. 85:19–28. 2012.PubMed/NCBI
|
|
50
|
Ishibashi S, Goldstein JL, Brown MS, Herz
J and Burns DK: Massive xanthomatosis and atherosclerosis in
cholesterol-fed low density lipoprotein receptor-negative mice. J
Clin Invest. 93:1885–1893. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Moore RE, Kawashiri MA, Kitajima K,
Secreto A, Millar JS, Pratico D and Rader DJ: Apolipoprotein A-I
deficiency results in markedly increased atherosclerosis in mice
lacking the LDL receptor. Arterioscler Thromb Vasc Biol.
23:1914–1920. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Getz GS and Reardon CA: Diet and murine
atherosclerosis. Arterioscler Thromb Vasc Biol. 26:242–249. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Boisvert WA, Spangenberg J and Curtiss LK:
Role of leukocyte-specific LDL receptors on plasma lipoprotein
cholesterol and atherosclerosis in mice. Arterioscler Thromb Vasc
Biol. 17:340–347. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Herijgers N, Van Eck M, Groot PH,
Hoogerbrugge PM and Van Berkel TJ: Effect of bone marrow
transplantation on lipoprotein metabolism and atherosclerosis in
LDL receptor-knockout mice. Arterioscler Thromb Vasc Biol.
17:1995–2003. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Linton MF, Atkinson JB and Fazio S:
Prevention of atherosclerosis in apolipoprotein E-deficient mice by
bone marrow transplantation. Science. 267:1034–1037. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Boisvert WA, Spangenberg J and Curtiss LK:
Treatment of severe hypercholesterolemia in apolipoprotein
E-deficient mice by bone marrow transplantation. J Clin Invest.
96:1118–1124. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Roche-Molina M, Sanz-Rosa D, Cruz FM,
García-Prieto J, López S, Abia R, Muriana FJ, Fuster V, Ibáñez B
and Bernal JA: Induction of sustained hypercholesterolemia by
single adeno-associated virus-mediated gene transfer of mutant
hPCSK9. Arterioscler Thromb Vasc Biol. 35:50–59. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Bjorklund MM, Hollensen AK, Hagensen MK,
Dagnaes-Hansen F, Christoffersen C, Mikkelsen JG and Bentzon JF:
Induction of atherosclerosis in mice and hamsters without germline
genetic engineering. Circ Res. 114:1684–1689. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Goettsch C, Hutcheson JD, Hagita S, Rogers
MA, Creager MD, Pham T, Choi J, Mlynarchik AK, Pieper B, Kjolby M,
et al: A single injection of gain-of-function mutant PCSK9
adeno-associated virus vector induces cardiovascular calcification
in mice with no genetic modification. Atherosclerosis. 251:109–118.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Veseli BE, Perrotta P, De Meyer GRA, Roth
L, der Donckt CV, Martinet W and De Meyer GR: Animal models of
atherosclerosis. Eur J Pharmacol. 816:3–13. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Zhang S, Picard MH, Vasile E, Zhu Y,
Raffai RL, Weisgraber KH and Krieger M: Diet-induced occlusive
coronary atherosclerosis, myocardial infarction, cardiac
dysfunction, and premature death in scavenger receptor class B type
I-deficient, hypomorphic apolipoprotein ER61 mice. Circulation.
111:3457–3464. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Westerterp M, van der Hoogt CC, de Haan W,
Offerman EH, Dallinga-Thie GM, Jukema JW, Havekes LM and Rensen PC:
Cholesteryl ester transfer protein decreases high-density
lipoprotein and severely aggravates atherosclerosis in
APOE*3-leiden mice. Arterioscler Thromb Vasc Biol. 26:2552–2559.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
van den Maagdenberg AM, Hofker MH,
Krimpenfort PJ, de Bruijn I, van Vlijmen B, van der Boom H, Havekes
LM and Frants RR: Transgenic mice carrying the apolipoprotein
E3-Leiden gene exhibit hyperlipoproteinemia. J Biol Chem.
268:10540–10545. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Berbee JF, Boon MR, Khedoe PP, Bartelt A,
Schlein C, Worthmann A, Kooijman S, Hoeke G, Mol IM, John C, et al:
Brown fat activation reduces hypercholesterolaemia and protects
from atherosclerosis development. Nat Commun. 6:63562015.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Van der Donckt C, Van Herck JL, Schrijvers
DM, Vanhoutte G, Verhoye M, Blockx I, Van Der Linden A, Bauters D,
Lijnen HR, Sluimer JC, et al: Elastin fragmentation in
atherosclerotic mice leads to intraplaque neovascularization,
plaque rupture, myocardial infarction, stroke, and sudden death.
Eur Heart J. 36:1049–1058. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Roth L, Rombouts M, Schrijvers DM, Lemmens
K, De Keulenaer GW, Martinet W and De Meyer GR: Chronic
intermittent mental stress promotes atherosclerotic plaque
vulnerability, myocardial infarction and sudden death in mice.
Atherosclerosis. 242:288–294. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Steinberg D: In celebration of the 100th
anniversary of the lipid hypothesis of atherosclerosis. J Lipid
Res. 54:2946–2949. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Fan J and Watanabe T: Cholesterol-fed and
transgenic rabbit models for the study of atherosclerosis. J
Atheroscler Thromb. 7:26–32. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Fan J, Kitajima S, Watanabe T, Xu J, Zhang
J, Liu E and Chen YE: Rabbit models for the study of human
atherosclerosis: From pathophysiological mechanisms to
translational medicine. Pharmacol Ther. 146:104–119. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Niimi M, Yang D, Kitajima S, Ning B, Wang
C, Li S, Liu E, Zhang J, Chen YE and Fan J: ApoE knockout rabbits:
A novel model for the study of human hyperlipidemia.
Atherosclerosis. 245:187–193. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Matsuhisa F, Kitajima S, Nishijima K,
Akiyoshi T, Morimoto M and Fan J: Transgenic rabbit models: Now and
the future. Applied Sciences. 10:74162020. View Article : Google Scholar
|
|
72
|
Yu QQ, Cheng DX, Xu LR, Li YK, Zheng XY,
Liu Y, Li YF, Liu HL, Bai L, Wang R, et al: Urotensin II and
urantide exert opposite effects on the cellular components of
atherosclerotic plaque in hypercholesterolemic rabbits. Acta
Pharmacol Sin. 41:546–553. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Chen Y, Waqar AB, Nishijima K, Ning B,
Kitajima S, Matsuhisa F, Chen L, Liu E, Koike T, Yu Y, et al:
Macrophage-derived MMP-9 enhances the progression of
atherosclerotic lesions and vascular calcification in transgenic
rabbits. J Cell Mol Med. 24:4261–4274. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Gao S, Wang X, Cheng D, Li J, Li L, Ran L,
Zhao S, Fan J and Liu E: Overexpression of cholesteryl ester
transfer protein increases macrophage-derived foam cell
accumulation in atherosclerotic lesions of transgenic rabbits.
Mediators Inflamm. 2017:38242762017. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Ding Y, Wang Y, Zhu H, Fan J, Yu L, Liu G
and Liu E: Hypertriglyceridemia and delayed clearance of fat load
in transgenic rabbits expressing human apolipoprotein CIII.
Transgenic Res. 20:867–875. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Koike T, Kitajima S, Yu Y, Li Y, Nishijima
K, Liu E, Sun H, Waqar AB, Shibata N, Inoue T, et al: Expression of
human apoAII in transgenic rabbits leads to dyslipidemia: A new
model for combined hyperlipidemia. Arterioscler Thromb Vasc Biol.
29:2047–2053. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Wang C, Nishijima K, Kitajima S, Niimi M,
Yan H, Chen Y, Ning B, Matsuhisa F, Liu E, Zhang J, et al:
Increased hepatic expression of endothelial lipase inhibits
cholesterol diet-induced hypercholesterolemia and atherosclerosis
in transgenic rabbits. Arterioscler Thromb Vasc Biol. 37:1282–1289.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Watanabe Y: Serial inbreeding of rabbits
with hereditary hyperlipidemia (WHHL-rabbit). Atherosclerosis.
36:261–268. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Shiomi M and Ito T: The Watanabe heritable
hyperlipidemic (WHHL) rabbit, its characteristics and history of
development: A tribute to the late Dr. Yoshio Watanabe.
Atherosclerosis. 207:1–7. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Masashi S and Takashi I: The Watanabe
heritable hyperlipidemic (WHHL) rabbit, its characteristics and
history of development: A tribute to the late Dr. Yoshio Watanabe.
Atherosclerosis. 207:1–7. 2009. View Article : Google Scholar
|
|
81
|
Ning B, Wang X, Yu Y, Waqar AB, Yu Q,
Koike T, Shiomi M, Liu E, Wang Y and Fan J: High-fructose and
high-fat diet-induced insulin resistance enhances atherosclerosis
in Watanabe heritable hyperlipidemic rabbits. Nutr Metab (Lond).
12:302015. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Lichtman AH, Clinton SK, Iiyama K,
Connelly PW, Libby P and Cybulsky MI: Hyperlipidemia and
atherosclerotic lesion development in LDL receptor-deficient mice
fed defined semipurified diets with and without cholate.
Arterioscler Thromb Vasc Biol. 19:1938–1944. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Reardon CA, Blachowicz L, Lukens J,
Nissenbaum M and Getz GS: Genetic background selectively influences
innominate artery atherosclerosis: Immune system deficiency as a
probe. Arterioscler Thromb Vasc Biol. 23:1449–1454. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Lin Y, Bai L, Chen Y, Zhu N, Bai Y, Li Q,
Zhao S, Fan J and Liu E: Practical assessment of the quantification
of atherosclerotic lesions in apoE(−)/(−) mice. Mol Med Rep.
12:5298–5306. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Centa M, Ketelhuth DFJ, Malin S and
Gisterå A: Quantification of atherosclerosis in mice. J Vis Exp.
12:doi: 10.3791/59828. 2019.PubMed/NCBI
|
|
86
|
Bai L, Li Z, Li Q, Guan H, Zhao S, Liu R,
Wang R, Zhang J, Jia Y, Fan J, et al: Mediator 1 is atherosclerosis
protective by regulating macrophage polarization. Arterioscler
Thromb Vasc Biol. 37:1470–1481. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Wang R, Zhang Y, Xu L, Lin Y, Yang X, Bai
L, Chen Y, Zhao S, Fan J, Cheng X and Liu E: Protein inhibitor of
activated STAT3 suppresses oxidized LDL-induced cell responses
during atherosclerosis in apolipoprotein E-deficient mice. Sci Rep.
6:367902016. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Guan H, Lin Y, Bai L, An Y, Shang J, Wang
Z, Zhao S, Fan J and Liu E: Dietary cocoa powder improves
hyperlipidemia and reduces atherosclerosis in apoE deficient mice
through the inhibition of hepatic endoplasmic reticulum stress.
Mediators Inflamm. 2016:19375722016. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Li S, Wang YN, Niimi M, Ning B, Chen Y,
Kang D, Wang Z, Yu Q, Waqar AB, Liu E, et al: Angiotensin II
destabilizes coronary plaques in watanabe heritable hyperlipidemic
rabbits. Arterioscler Thromb Vasc Biol. 36:810–816. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Yan H, Niimi M, Matsuhisa F, Zhou H,
Kitajima S, Chen Y, Wang C, Yang X, Yao J, Yang D, et al:
Apolipoprotein CIII deficiency protects against atherosclerosis in
knockout rabbits. Arterioscler Thromb Vasc Biol. 40:2095–2107.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Dweck MR, Aikawa E, Newby DE, Tarkin JM,
Rudd JH, Narula J and Fayad ZA: Noninvasive molecular imaging of
disease activity in atherosclerosis. Circ Res. 119:330–340. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Chen Q, Yu J, Lukashova L, Latoche JD, Zhu
J, Lavery L, Verdelis K, Anderson CJ and Kim K: validation of
ultrasound super-resolution imaging of vasa vasorum in rabbit
atherosclerotic plaques. IEEE Trans Ultrason Ferroelectr Freq
Control. 67:1725–1729. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Zhang X, Ha S, Wei W, Duan S, Shi Y and
Yang Y: Noninvasive imaging of aortic atherosclerosis by ultrasound
biomicroscopy in a mouse model. J Ultrasound Med. 34:111–116. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Punjabi M, Xu L, Ochoa-Espinosa A,
Kosareva A, Wolff T, Murtaja A, Broisat A, Devoogdt N and Kaufmann
BA: Ultrasound molecular imaging of atherosclerosis with
nanobodies: Translatable microbubble targeting murine and human
VCAM (Vascular Cell Adhesion Molecule) 1. Arterioscler Thromb Vasc
Biol. 39:2520–2530. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Borland SJ, Behnsen J, Ashton N, Francis
SE, Brennan K, Sherratt MJ, Withers PJ and Canfield AE: X-ray
micro-computed tomography: An emerging technology to analyze
vascular calcification in animal models. Int J Mol Sci.
21:45382020. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Magnoni M, Ammirati E and Camici PG:
Non-invasive molecular imaging of vulnerable atherosclerotic
plaques. J Cardiol. 65:261–269. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Choudhury RP, Fuster V, Badimon JJ, Fisher
EA and Fayad ZA: MRI and characterization of atherosclerotic
plaque: Emerging applications and molecular imaging. Arterioscler
Thromb Vasc Biol. 22:1065–1074. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Evans NR, Tarkin JM, Chowdhury MM,
Warburton EA and Rudd JH: PET imaging of atherosclerotic disease:
Advancing plaque assessment from anatomy to pathophysiology. Curr
Atheroscler Rep. 18:302016. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Calcagno C, Lairez O, Hawkins J, Kerr SW,
Dugas MS, Simpson T, Epskamp J, Robson PM, Eldib M, Bander I, et
al: Combined PET/DCE-MRI in a rabbit model of atherosclerosis:
Integrated quantification of plaque inflammation, permeability, and
burden during treatment with a leukotriene A4 hydrolase inhibitor.
JACC Cardiovasc Imaging. 11:291–301. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Calcagno C, Perez-Medina C, Mulder WJM and
Fayad ZA: Whole-Body atherosclerosis imaging by positron emission
tomography/magnetic resonance imaging: From mice to nonhuman
primates. Arterioscler Thromb Vasc Biol. 40:1123–1134. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Luehmann HP, Detering L, Fors BP, Pressly
ED, Woodard PK, Randolph GJ, Gropler RJ, Hawker CJ and Liu Y:
PET/CT imaging of chemokine receptors in inflammatory
atherosclerosis using targeted nanoparticles. J Nucl Med.
57:1124–1129. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Cheng D, Li X, Zhang C, Tan H, Wang C,
Pang L and Shi H: Detection of vulnerable atherosclerosis plaques
with a dual-modal single-photon-emission computed
tomography/magnetic resonance imaging probe targeting apoptotic
macrophages. ACS Appl Mater Interfaces. 7:2847–2855. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Rahaman SO, Lennon DJ, Febbraio M, Podrez
EA, Hazen SL and Silverstein RL: A CD36-dependent signaling cascade
is necessary for macrophage foam cell formation. Cell Metab.
4:211–221. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Versari D, Daghini E, Virdis A, Ghiadoni L
and Taddei S: Endothelial dysfunction as a target for prevention of
cardiovascular disease. Diabetes Care. 32 (Suppl 2):S314–S321.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Medina-Leyte DJ, Domínguez-Pérez M,
Mercado I, Villarreal-Molina MT and Jacobo-Albavera L: Use of human
umbilical vein endothelial cells (HUVEC) as a model to study
cardiovascular disease: A review. Applied Sciences. 10:9382020.
View Article : Google Scholar
|
|
106
|
Yang Q, Xu J, Ma Q, Liu Z, Sudhahar V, Cao
Y, Wang L, Zeng X, Zhou Y, Zhang M, et al: PRKAA1/AMPKα1-driven
glycolysis in endothelial cells exposed to disturbed flow protects
against atherosclerosis. Nat Commun. 9:46672018. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Chen Y, Liu R, Zhang G, Yu Q, Jia M, Zheng
C, Wang Y, Xu C, Zhang Y and Liu E: Hypercysteinemia promotes
atherosclerosis by reducing protein S-nitrosylation. Biomed
Pharmacother. 70:253–259. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
O'Donnell J, Mille-Baker B and Laffan M:
Human umbilical vein endothelial cells differ from other
endothelial cells in failing to express ABO blood group antigens. J
Vasc Res. 37:540–547. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Addis R, Campesi I, Fois M, Capobianco G,
Dessole S, Fenu G, Montella A, Cattaneo MG, Vicentini LM and
Franconi F: Human umbilical endothelial cells (HUVECs) have a sex:
Characterisation of the phenotype of male and female cells. Biol
Sex Differ. 5:182014. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Crampton SP, Davis J and Hughes CC:
Isolation of human umbilical vein endothelial cells (HUVEC). J Vis
Exp. 183:doi: 10.3791/183. 2007.PubMed/NCBI
|
|
111
|
Jaffe EA, Nachman RL, Becker CG and Minick
CR: Culture of human endothelial cells derived from umbilical
veins. Identification by morphologic and immunologic criteria. J
Clin Invest. 52:2745–2756. 1973. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Baudin B, Bruneel A, Bosselut N and
Vaubourdolle M: A protocol for isolation and culture of human
umbilical vein endothelial cells. Nat Protoc. 2:481–485. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Liu L and Shi GP: CD31: Beyond a marker
for endothelial cells. Cardiovasc Res. 94:3–5. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Tabas I and Bornfeldt KE: Macrophage
phenotype and function in different stages of atherosclerosis. Circ
Res. 118:653–667. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Li AC and Glass CK: The macrophage foam
cell as a target for therapeutic intervention. Nat Med.
8:1235–1242. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Zimmerman MA, Selzman CH, Reznikov LL,
Miller SA, Raeburn CD, Emmick J, Meng X and Harken AH: Lack of
TNF-alpha attenuates intimal hyperplasia after mouse carotid artery
injury. Am J Physiol Regul Integr Comp Physiol. 283:R505–R512.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Zhang X, Goncalves R and Mosser DM: The
isolation and characterization of murine macrophages. Curr Protoc
Immunol Chapter. 14:Unit 14 11. 2008.PubMed/NCBI
|
|
118
|
Austyn JM and Gordon S: F4/80, a
monoclonal antibody directed specifically against the mouse
macrophage. Eur J Immunol. 11:805–815. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Bennett MR and Boyle JJ: Apoptosis of
vascular smooth muscle cells in atherosclerosis. Atherosclerosis.
138:3–9. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Gao S, Xu L, Zhang Y, Yu Q, Li J, Guan H,
Wang X, Cheng D, Liu Y, Bai L, et al: Salusin-alpha inhibits
proliferation and migration of vascular smooth muscle cell via
Akt/mTOR signaling. Cell Physiol Biochem. 50:1740–1753. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Feng C, Wang X, Shi H, Yan Q, Zheng M, Li
J, Zhang Q, Qin Y, Zhong Y, Mi J and Lai L: Generation of ApoE
deficient dogs via combination of embryo injection of CRISPR/Cas9
with somatic cell nuclear transfer. J Genet Genomics. 45:47–50.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Fang B, Ren X, Wang Y, Li Z, Zhao L, Zhang
M, Li C, Zhang Z, Chen L, Li X, et al: Apolipoprotein E deficiency
accelerates atherosclerosis development in miniature pigs. Dis
Model Mech. 11:dmm0366322018. View Article : Google Scholar : PubMed/NCBI
|