|
1
|
Momenimovahed Z, Tiznobaik A, Taheri S and
Salehiniya H: Ovarian cancer in the world: epidemiology and risk
factors. Int J Womens Health. 11:287–299. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Siegel RL, Miller KD and Jemal A: Cancer
Statistics, 2016. CA Cancer J Clin. 66:7–30. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Luo Y, Huang J, Tang Y, Luo X, Ge L, Sheng
X, Sun X, Chen Y and Zhu D: Regional methylome profiling reveals
dynamic epigenetic heterogeneity and convergent hypomethylation of
stem cell quiescence-associated genes in breast cancer following
neoadjuvant chemotherapy. Cell Biosci. 9:162019. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sandhu R, Roll JD, Rivenbark AG and
Coleman WB: Dysregulation of the Epigenome in Human Breast Cancer':
Contributions of gene-specific DNA hypermethylation to breast
cancer pathobiology and targeting the breast cancer methylome for
improved therapy. Am J Pathol. 185:282–292. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Maire CL, Fuh MM, Kaulich K, Fita KD,
Stevic I, Heiland DH, Welsh JA, Jones JC, Görgens A, Ricklefs T, et
al: Genome-wide methylation profiling of glioblastoma cell-derived
extracellular vesicle DNA allows tumor classification. Neuro Oncol.
23:1087–1099. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang Z, Cui Y, Wang F, Xu L, Yan Y, Tong X
and Yan H: DNA methylation-regulated LINC02587 inhibits ferroptosis
and promotes the progression of glioma cells through the CoQ-FSP1
pathway. BMC Cancer. 23:9892023. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wielandt AM, Villarroel C, Hurtado C,
Simian D, Zamorano D, Martínez M, Castro M, Vial MT, Kronberg U and
López-Kostner F: Characterization of patients with sporadic
colorectal cancer following the new Consensus Molecular Subtypes
(CMS). Rev Méd Chile. 145:419–430. 2017.(In Spanish). View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Moreno-Ortiz JM, Jiménez-García J,
Gutiérrez-Angulo M, Ayala-Madrigal MD, González-Mercado A,
González-Villaseñor CO, Flores-López BA, Alvizo-Rodríguez C,
Hernández-Sandoval JA, Fernández-Galindo MA, et al: High frequency
of MLH1 promoter methylation mediated by gender and age in
colorectal tumors from Mexican patients. GMM. 157:638–644. 2021.(In
Spanish).
|
|
9
|
Del Castillo Falconi VM, Torres-Arciga K,
Matus-Ortega G, Díaz-Chávez J and Herrera LA: DNA
methyltransferases: From evolution to clinical applications. Int J
Mol Sci. 23:89942022. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li E, Bestor TH and Jaenisch R: Targeted
mutation of the DNA methyltransferase gene results in embryonic
lethality. Cell. 69:915–926. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
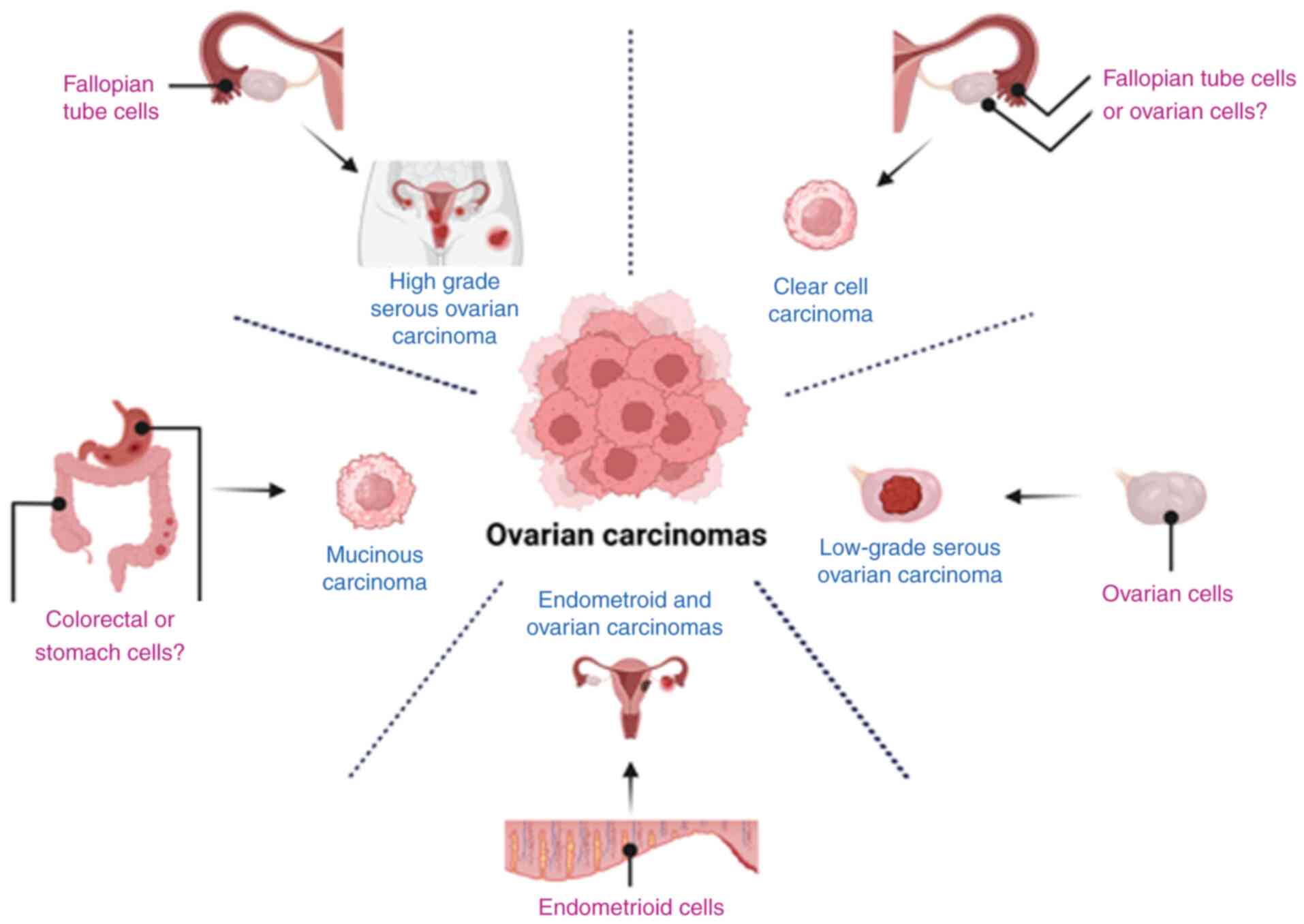
Shih IeM and Kurman RJ: Ovarian
tumorigenesis: A proposed model based on morphological and
molecular genetic analysis. Am J Pathol. 164:1511–1518. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kurman RJ and Shih IeM: Pathogenesis of
ovarian cancer: Lessons from morphology and molecular biology and
their clinical implications. Int J Gynecol Pathol. 27:151–160.
2018.PubMed/NCBI
|
|
13
|
Kurman RJ and Shih IeM: The origin and
pathogenesis of epithelial ovarian cancer: A proposed unifying
theory. Am J Surg Pathol. 34:433–443. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Samuel D, Diaz-Barbe A, Pinto A,
Schlumbrecht M and George S: Hereditary ovarian carcinoma: Cancer
pathogenesis looking beyond BRCA1 and BRCA2. Cells. 11:5392022.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ramus SJ, Harrington PA, Pye C, DiCioccio
RA, Cox MJ, Garlinghouse-Jones K, Oakley-Girvan I, Jacobs IJ, Hardy
RM, Whittemore AS, et al: Contribution of BRCA1 and BRCA2 mutations
to inherited ovarian cancer. Hum Mutat. 28:1207–1215. 2007.
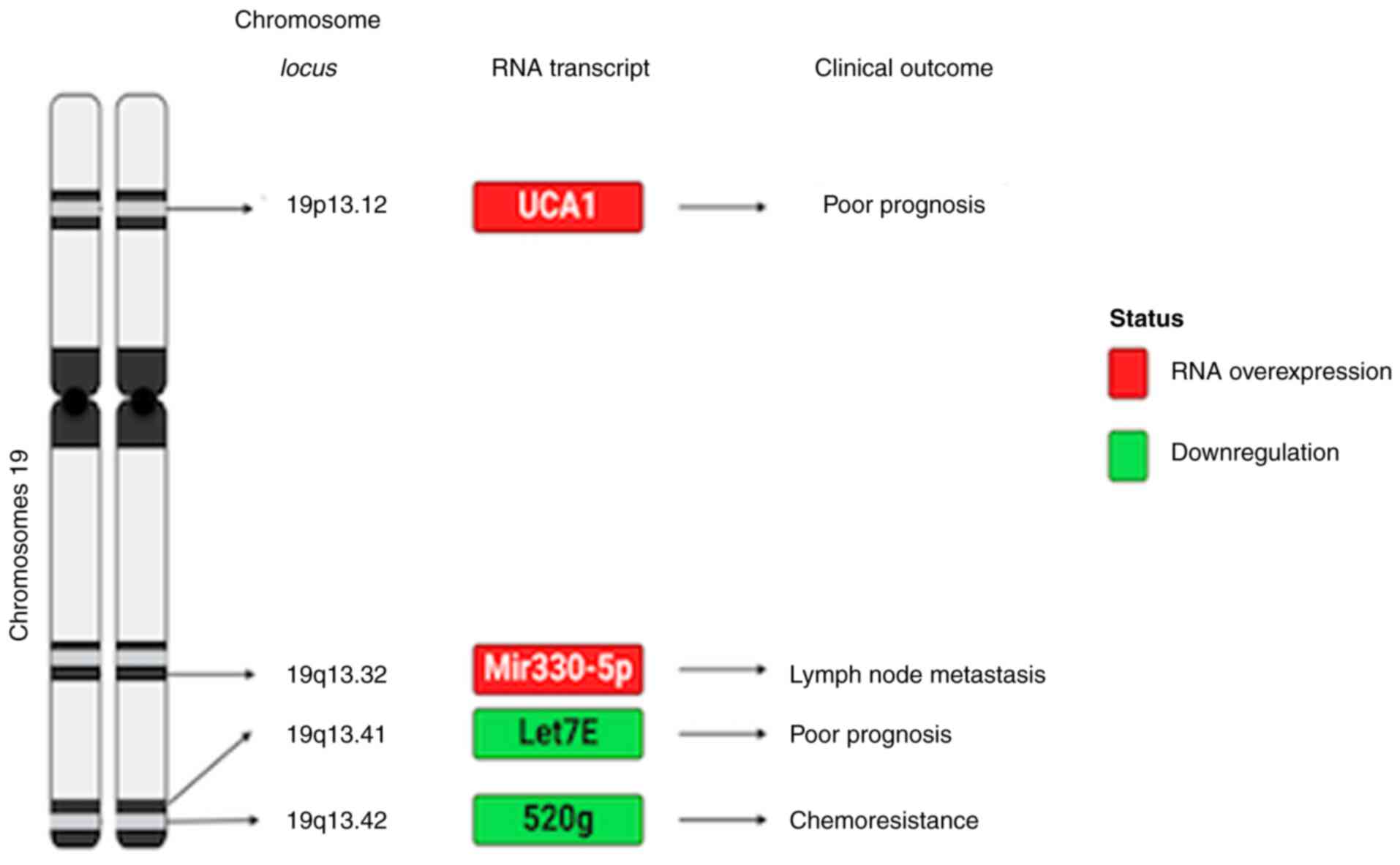
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Menon U, Karpinskyj C and Gentry-Maharaj
A: Ovarian cancer prevention and screening. Obstet Gynecol.
131:909–927. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lavoro A, Scalisi A, Candido S, Zanghì GN,
Rizzo R, Gattuso G, Caruso G, Libra M and Falzone L: Identification
of the most common BRCA alterations through analysis of germline
mutation databases: Is droplet digital PCR an additional strategy
for the assessment of such alterations in breast and ovarian cancer
families? Int J Oncol. 60:582022. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kansuttiviwat C, Lertwilaiwittaya P,
Roothumnong E, Nakthong P, Dungort P, Meesamarnpong C, Tansa-Nga W,
Pongsuktavorn K, Wiboonthanasarn S, Tititumjariya W, et al:
Germline mutations of 4567 patients with hereditary breast-ovarian
cancer spectrum in Thailand. NPJ Genom Med. 9:92024. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Andrikopoulou A, Zografos E, Apostolidou
K, Kyriazoglou A, Papatheodoridi AM, Kaparelou M, Koutsoukos K,
Liontos M, Dimopoulos MA and Zagouri F: Germline and somatic
variants in ovarian carcinoma: A next-generation sequencing (NGS)
analysis. Front Oncol. 12:10307862022. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ghose A, Bolina A, Mahajan I, Raza SA,
Clarke M, Pal A, Sanchez E, Rallis KS and Boussios S: Hereditary
ovarian cancer: Towards a cost-effective prevention strategy. Int J
Environ Res Public Health. 19:120572022. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
McCluggage WG: Morphological subtypes of
ovarian carcinoma: A review with emphasis on new developments and
pathogenesis. Pathology. 43:420–432. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Andrews L and Mutch DG: Hereditary ovarian
cancer and risk reduction. Best Pract Res Clin Obstet Gynaecol.
41:31–48. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lynch HT and Lynch JF: Hereditary
nonpolyposis colorectal cancer. Semin Surg Oncol. 18:305–313. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wu H, Shang X, Shi Y, Yang Z, Zhao J, Yang
M, Li Y and Xu S: Genetic variants of lncRNA HOTAIR and risk of
epithelial ovarian cancer among Chinese women. Oncotarget.
7:41047–41052. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bronder D, Tighe A, Wangsa D, Zong D,
Meyer TJ, Wardenaar R, Minshall P, Hirsch D, Heselmeyer-Haddad K,
Nelson L, et al: TP53 loss initiates chromosomal instability in
fallopian tube epithelial cells. Dis Model Mech. 14:dmm0490012021.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Goff BA, Mandel L, Muntz HG and Melancon
CH: Ovarian carcinoma diagnosis. Cancer. 89:2068–2075. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zeimet AG, Fiegl H, Goebel G, Kopp F,
Allasia C, Reimer D, Steppan I, Mueller-Holzner E, Ehrlich M and
Marth C: DNA ploidy, nuclear size, proliferation index and
DNA-hypomethylation in ovarian cancer. Gynecol Oncol. 121:24–31.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Widschwendter M, Jiang G, Woods C, Müller
HM, Fiegl H, Goebel G, Marth C, Müller-Holzner E, Zeimet AG, Laird
PW and Ehrlich M: DNA hypomethylation and ovarian cancer biology.
Cancer Res. 64:4472–4480. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Feng W, Marquez RT, Lu Z, Liu J, Lu KH,
Issa JP, Fishman DM, Yu Y and Bast RC Jr: Imprinted tumor
suppressor genesARHI andPEG3 are the most frequently down-regulated
in human ovarian cancers by loss of heterozygosity and promoter
methylation. Cancer. 112:1489–1502. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Link PA, Zhang W, Odunsi K and Karpf AR:
BORIS/CTCFL mRNA isoform expression and epigenetic regulation in
epithelial ovarian cancer. Cancer Immun. 13:62013.PubMed/NCBI
|
|
31
|
Wang YQ, Yan Q, Zhang JR, Li SD, Yang YX
and Wan XP: Epigenetic inactivation of BRCA1 through promoter
hypermethylation in ovarian cancer progression. J Obstet Gynaecol
Res. 39:549–554. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Abou-Zeid AA, Azzam AZ and Kamel NA:
Methylation status of the gene promoter of cyclin-dependent kinase
inhibitor 2A (CDKN2A) in ovarian cancer. Scand J Clin Lab Invest.
71:542–547. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Bhagat R, Kumar SS, Vaderhobli S,
Premalata CS, Pallavi VR, Ramesh G and Krishnamoorthy L: Epigenetic
alteration of p16 and retinoic acid receptor beta genes in the
development of epithelial ovarian carcinoma. Tumour Biol.
35:9069–9078. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yang G, Zhang H, Liu Y, Zhou J, He W,
Quick CM, Xie D, Smoller BR and Fan CY: Epigenetic and
immunohistochemical characterization of the Clusterin gene in
ovarian tumors. Arch Gynecol Obstet. 287:989–995. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Zhang W, Barger CJ, Link PA,
Mhawech-Fauceglia P, Miller A, Akers SN, Odunsi K and Karpf AR: DNA
hypomethylation-mediated activation of Cancer/Testis Antigen 45
(CT45) genes is associated with disease progression and reduced
survival in epithelial ovarian cancer. Epigenetics. 10:736–748.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wang B, Yu L, Luo X, Huang L, Li QS, Shao
XS, Liu Y, Fan Y and Yang GZ: Detection of OPCML methylation, a
possible epigenetic marker, from free serum circulating DNA to
improve the diagnosis of early-stage ovarian epithelial cancer.
Oncol Lett. 14:217–223. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kaur M, Singh A, Singh K, Gupta S and
Sachan M: Development of a multiplex MethyLight assay for the
detection of DAPK1 and SOX1 methylation in epithelial ovarian
cancer in a north Indian population. Genes Genet Syst. 91:175–181.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Rattanapan Y, Korkiatsakul V, Kongruang A,
Chareonsirisuthigul T, Rerkamnuaychoke B, Wongkularb A and Wilailak
S: EGFL7 and RASSF1 promoter hypermethylation in epithelial ovarian
cancer. Cancer Genet. 224–225. 37–40. 2018.PubMed/NCBI
|
|
39
|
da Conceição Braga C, Silva LM, Piedade
JB, Traiman P and da Silva Filho AL: Epigenetic and expression
analysis of TRAIL-R2 and BCL2: On the TRAIL to knowledge of
apoptosis in ovarian tumors. Arch Gynecol Obstet. 289:1061–1069.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Bonito NA, Borley J, Wilhelm-Benartzi CS,
Ghaem-Maghami S and Brown R: Epigenetic regulation of the homeobox
gene MSX1 associates with platinum-resistant disease in high-grade
serous epithelial ovarian cancer. Clin Cancer Res. 22:3097–3104.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Kardum V, Karin V, Glibo M, Skrtic A,
Martic TN, Ibisevic N, Skenderi F, Vranic S and Serman L:
Methylation-associated silencing of SFRP1 gene in high-grade serous
ovarian carcinomas. Ann Diagn Pathol. 31:45–49. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Suzuki F, Akahira J, Miura I, Suzuki T,
Ito K, Hayashi S, Sasano H and Yaegashi N: Loss of estrogen
receptor beta isoform expression and its correlation with aberrant
DNA methylation of the 5′-untranslated region in human epithelial
ovarian carcinoma. Cancer Sci. 99:2365–2372. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Baranova I, Kovarikova H, Laco J, Dvorak
O, Sedlakova I, Palicka V and Chmelarova M: Aberrant methylation of
PCDH17 gene in high-grade serous ovarian carcinoma. Cancer Biomark.
23:125–133. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Ding JJ, Wang G, Shi WX, Zhou HH and Zhao
EF: Promoter hypermethylation of FANCF and susceptibility and
prognosis of epithelial ovarian cancer. Reprod Sci. 23:24–30. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Gozzi G, Chelbi ST, Manni P, Alberti L,
Fonda S, Saponaro S, Fabbiani L, Rivasi F, Benhattar J and Losi L:
Promoter methylation and downregulated expression of the TBX15 gene
in ovarian carcinoma. Oncol Lett. 12:2811–2819. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Choi YL, Kang SY, Shin YK, Choi JS, Kim
SH, Lee SJ, Bae DS and Ahn G: Aberrant hypermethylation of RASSF1A
promoter in ovarian borderline tumors and carcinomas. Virchows
Archiv. 448:331–336. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Häfner N, Steinbach D, Jansen L, Diebolder
H, Dürst M and Runnebaum IB: RUNX3 and CAMK2N1 hypermethylation as
prognostic marker for epithelial ovarian cancer. Int J Cancer.
138:217–228. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Jin P, Song Y and Yu G: The role of
abnormal methylation of Wnt5a gene promoter regions in human
epithelial ovarian cancer: A clinical and experimental study. Anal
Cell Pathol (Amst). 2018:65670812018.PubMed/NCBI
|
|
49
|
Khodadadi E, Fahmideh L, Khodadadi E, Dao
S, Yousefi M, Taghizadeh S, Asgharzadeh M, Yousefi B and Kafil HS:
Current advances in DNA methylation analysis methods. Biomed Res
Int. 2021:88275162021. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Gattuso G, Lavoro A, Caltabiano R, Madonna
G, Capone M, Ascierto PA, Falzone L, Libra M and Candido S:
Methylation-sensitive restriction enzyme-droplet digital PCR assay
for the one-step highly sensitive analysis of DNA methylation
hotspots. Int J Mol Med. 53:422024. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Falzone L, Salemi R, Travali S, Scalisi A,
McCubrey JA, Candido S and Libra M: MMP-9 overexpression is
associated with intragenic hypermethylation of MMP9 gene in
melanoma. Aging (Albany NY). 8:933–944. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Singer M, Kosti I, Pachter L and
Mandel-Gutfreund Y: A diverse epigenetic landscape at human exons
with implication for expression. Nucleic Acids Res. 43:3498–3508.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Davidson B, Tropé CG and Reich R: The
clinical and diagnostic role of microRNAs in ovarian carcinoma.
Gynecol Oncol. 133:640–646. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Sheng X and Li J, Yang L, Chen Z, Zhao Q,
Tan L, Zhou Y and Li J: Promoter hypermethylation influences the
suppressive role of maternally expressed 3, a long non-coding RNA,
in the development of epithelial ovarian cancer. Oncol Rep.
32:277–285. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Loginov VI, Pronina IV, Burdennyy AM,
Filippova EA, Kazubskaya TP, Kushlinsky DN, Utkin DO, Khodyrev DS,
Kushlinskii NE, Dmitriev AA and Braga EA: Novel miRNA genes
deregulated by aberrant methylation in ovarian carcinoma are
involved in metastasis. Gene. 662:28–36. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Filippov-Levy N, Cohen-Schussheim H, Tropé
CG, Hetland Falkenthal TE, Smith Y, Davidson B and Reich R:
Expression and clinical role of long non-coding RNA in high-grade
serous carcinoma. Gynecol Oncol. 148:559–566. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Liu X, Dai C, Jia G, Xu S, Fu Z, Xu J, Li
Q, Ruan H and Xu P: Microarray analysis reveals differentially
expressed lncRNAs in benign epithelial ovarian cysts and normal
ovaries. Oncol Rep. 38:799–808. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Lu YM, Wang Y, Liu SQ, Zhou MY and Guo YR:
Profile and validation of dysregulated long non-coding RNAs and
mRNAs in ovarian cancer. Oncol Rep. 40:2964–2976. 2018.PubMed/NCBI
|
|
59
|
Wang H, Fu Z, Dai C, Cao J, Liu X, Xu J,
Lv M, Gu Y, Zhang J, Hua X, et al: LncRNAs expression profiling in
normal ovary, benign ovarian cyst and malignant epithelial ovarian
cancer. Sci Rep. 6:389832016. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Boyd C and McCluggage WG: Low-grade
ovarian serous neoplasms (low-grade serous carcinoma and serous
borderline tumor) associated with high-grade serous carcinoma or
undifferentiated carcinoma: Report of a series of cases of an
unusual phenomenon. Am J Surg Pathol. 36:368–375. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Pisanic TR II, Cope LM, Lin SF, Yen TT,
Athamanolap P, Asaka R, Nakayama K, Fader AN, Wang TH, Shih IM and
Wang TL: Methylomic analysis of ovarian cancers identifies
tumor-specific alterations readily detectable in early precursor
lesions. Clin Cancer Res. 24:6536–6547. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Klinkebiel D, Zhang W, Akers SN, Odunsi K
and Karpf AR: DNA Methylome analyses implicate fallopian tube
epithelia as the origin for high-grade serous ovarian cancer. Mol
Cancer Res. 14:787–794. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Givel AM, Kieffer Y, Scholer-Dahirel A,
Sirven P, Cardon M, Pelon F, Magagna I, Gentric G, Costa A, Bonneau
C, Mieulet V, et al: miR200-regulated CXCL12β promotes fibroblast
heterogeneity and immunosuppression in ovarian cancers. Nat Commun.
9:10562018. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Wang Y, Qiu C, Lu N, Liu Z, Jin C, Sun C,
Bu H, Yu H, Dongol S and Kong B: FOXD1 is targeted by miR-30a-5p
and miR-200a-5p and suppresses the proliferation of human ovarian
carcinoma cells by promoting p21 expression in a p53-independent
manner. Int J Oncol. 52:2130–2142. 2018.PubMed/NCBI
|
|
65
|
Ma H, Tian T, Liang S, Liu X, Shen H, Xia
M, Liu X, Zhang W, Wang L, Chen S and Yu L: Estrogen
receptor-mediated miR-486-5p regulation of OLFM4 expression in
ovarian cancer. Oncotarget. 7:10594–1605. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Nymoen DA, Slipicevic A, Holth A, Emilsen
E, Hetland Falkenthal TE, Tropé CG, Reich R, Flørenes VA and
Davidson B: MiR-29a is a candidate biomarker of better survival in
metastatic high-grade serous carcinoma. Hum Pathol. 54:74–81. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Arts FA, Keogh L, Smyth P, O'Toole S, Ta
R, Gleeson N, O'Leary JJ, Flavin R and Sheils O: miR-223
potentially targets SWI/SNF complex protein SMARCD1 in atypical
proliferative serous tumor and high-grade ovarian serous carcinoma.
Hum Pathol. 70:98–104. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Chaluvally-Raghavan P, Jeong KJ, Pradeep
S, Silva AM, Yu S, Liu W, Moss T, Rodriguez-Aguayo C, Zhang D, Ram
P, et al: Direct upregulation of STAT3 by MicroRNA-551b-3p
deregulates growth and metastasis of ovarian cancer. Cell Rep.
15:1493–1504. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Zhao H, Liu S, Wang G, Wu X, Ding Y, Guo
G, Jiang J and Cui S: Expression of miR-136 is associated with the
primary cisplatin resistance of human epithelial ovarian cancer.
Oncol Rep. 33:591–598. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Kuznetsov VA, Tang Z and Ivshina AV:
Identification of common oncogenic and early developmental pathways
in the ovarian carcinomas controlling by distinct prognostically
significant microRNA subsets. BMC Genomics. 18 (Suppl 6):6922017.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Zhang X, Guo G, Wang G, Zhao J, Wang B, Yu
X and Ding Y: Profile of differentially expressed miRNAs in
high-grade serous carcinoma and clear cell ovarian carcinoma, and
the expression of miR-510 in ovarian carcinoma. Mol Med Rep.
12:8021–8031. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Yanaihara N, Noguchi Y, Saito M, Takenaka
M, Takakura S, Yamada K and Okamoto A: MicroRNA gene expression
signature driven by miR-9 overexpression in ovarian clear cell
carcinoma. PLoS One. 11:e01625842016. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Furlan D, Carnevali I, Marcomini B,
Cerutti R, Dainese E, Capella C and Riva C: The high frequency of
de novo promoter methylation in synchronous primary endometrial and
ovarian carcinomas. Clin Cancer Res. 12:3329–3336. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Niskakoski A, Pasanen A, Porkka N, Eldfors
S, Lassus H, Renkonen-Sinisalo L, Kaur S, Mecklin JP, Bützow R and
Peltomäki P: Converging endometrial and ovarian tumorigenesis in
Lynch syndrome: Shared origin of synchronous carcinomas. Gynecol
Oncol. 150:92–98. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Kolbe DL, DeLoia JA, Porter-Gill P,
Strange M, Petrykowska HM, Guirguis A, Krivak TC, Brody LC and
Elnitski L: Differential analysis of ovarian and endometrial
cancers identifies a methylator phenotype. PLoS One. 7:e329412012.
View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Guo C, Ren F, Wang D, Li Y, Liu K, Liu S
and Chen P: RUNX3 is inactivated by promoter hypermethylation in
malignant transformation of ovarian endometriosis. Oncol Rep.
32:2580–2588. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Liew PL, Huang RL, Weng YC, Fang CL,
Hui-Ming Huang T and Lai HC: Distinct methylation profile of
mucinous ovarian carcinoma reveals susceptibility to proteasome
inhibitors: Methylation profile of MuOC and PSMB8. Int J Cancer.
143:355–367. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Agostini A, Brunetti M, Davidson B, Tropé
CG, Eriksson AGZ, Heim S, Panagopoulos I and Micci F: The microRNA
miR-192/215 family is upregulated in mucinous ovarian carcinomas.
Sci Rep. 8:110692018. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Vang R, Shih IeM and Kurman RJ: Ovarian
low-grade and high-grade serous carcinoma: Pathogenesis,
clinicopathologic and molecular biologic features, and diagnostic
problems. Adv Anat Pathol. 16:267–282. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Bowtell DD: The genesis and evolution of
high-grade serous ovarian cancer. Nat Rev Cancer. 10:803–808. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
81
|
O'Shea AS: Clinical staging of ovarian
cancer. Methods Mol Biol. 2424:3–10. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Richards EJ, Permuth-Wey J, Li Y, Chen YA,
Coppola D, Reid BM, Lin HY, Teer JK, Berchuck A, Birrer MJ, et al:
A functional variant in HOXA11-AS, a novel long non-coding RNA,
inhibits the oncogenic phenotype of epithelial ovarian cancer.
Oncotarget. 6:34745–34757. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Zhang T, Wu D, Deng S, Han R, Liu T, Li J
and Xu Y: Integrated analysis reveals that long non-coding RNA
TUBA4B can be used as a prognostic biomarker in various cancers.
Cell Physiol Biochem. 49:530–544. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Meryet-Figuière M, Lambert B, Gauduchon P,
Vigneron N, Brotin E, Poulain L and Denoyelle C: An overview of
long non-coding RNAs in ovarian cancers. Oncotarget. 7:44719–44734.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Zhong Y, Gao D, He S, Shuai C and Peng S:
Dysregulated expression of long noncoding RNAs in ovarian cancer.
Int J Gynecol Cancer. 26:1564–1570. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Ma Y, Lu Y and Lu B: MicroRNA and Long
Non-Coding RNA in ovarian carcinoma: Translational insights and
potential clinical applications. Cancer Invest. 34:465–476. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Lin X, Qiu J and Hua K: Long non-coding
RNAs as emerging regulators of epithelial to mesenchymal transition
in gynecologic cancers. Biosci Trends. 12:342–353. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Micheel J, Safrastyan A and Wollny D:
Advances in non-coding RNA sequencing. Noncoding RNA.
7:702021.PubMed/NCBI
|
|
89
|
Zhang N, Hu G, Myers TG and Williamson PR:
Protocols for the analysis of microRNA expression, biogenesis, and
function in immune cells. Curr Protoc Immunol. 126:e782019.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Zhang S, Leng T, Zhang Q, Zhao Q, Nie X
and Yang L: Sanguinarine inhibits epithelial ovarian cancer
development via regulating long non-coding RNA CASC2-EIF4A3 axis
and/or inhibiting NF-κB signaling or PI3K/AKT/mTOR pathway. Biomed
Pharmacother. 102:302–308. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Qiu JJ, Lin YY, Ye LC, Ding JX, Feng WW,
Jin HY, Zhang Y, Li Q and Hua KQ: Overexpression of long non-coding
RNA HOTAIR predicts poor patient prognosis and promotes tumor
metastasis in epithelial ovarian cancer. Gynecol Oncol.
134:121–128. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Xi J, Feng J and Zeng S: Long noncoding
RNA lncBRM facilitates the proliferation, migration and invasion of
ovarian cancer cells via upregulation of Sox4. Am J Cancer Res.
7:2180–2189. 2017.PubMed/NCBI
|
|
93
|
Zhang Y, Dun Y, Zhou S and Huang XH:
LncRNA HOXD-AS1 promotes epithelial ovarian cancer cells
proliferation and invasion by targeting miR-133a-3p and activating
Wnt/β-catenin signaling pathway. Biomed Pharmacother. 96:1216–1221.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Liu Y, Wang Y, Yao D and Cui D: LncSOX4
serves an oncogenic role in the tumorigenesis of epithelial ovarian
cancer by promoting cell proliferation and inhibiting apoptosis.
Mol Med Rep. 17:8282–8288. 2018.PubMed/NCBI
|
|
95
|
Yan H, Li H, Li P, Li X, Lin J, Zhu L,
Silva MA, Wang X, Wang P and Zhang Z: Long noncoding RNA MLK7-AS1
promotes ovarian cancer cells progression by modulating
miR-375/YAP1 axis. J Exp Clin Cancer Res. 37:2372018. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Li T, Chen Y, Zhang J and Liu S: LncRNA
TUG1 promotes cells proliferation and inhibits cells apoptosis
through regulating AURKA in epithelial ovarian cancer cells.
Medicine (Baltimore). 97:e121312018. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Wang YS, Ma LN, Sun JX, Liu N and Wang H:
Long non-coding CPS1-IT1 is a positive prognostic factor and
inhibits epithelial ovarian cancer tumorigenesis. Eur Rev Med
Pharmacol Sci. 21:3169–3175. 2017.PubMed/NCBI
|
|
98
|
Zhu FF, Zheng FY, Wang HO, Zheng JJ and
Zhang Q: Downregulation of lncRNA TUBA4B is associated with poor
prognosis for epithelial ovarian cancer. Pathol Oncol Res.
24:419–425. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Ying X, Wei K, Lin Z, Cui Y, Ding J, Chen
Y and Xu B: MicroRNA-125b suppresses ovarian cancer progression via
suppression of the epithelial-mesenchymal transition pathway by
targeting the SET protein. Cell Physiol Biochem. 39:501–510. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Zhu T, Gao W, Chen X, Zhang Y, Wu M, Zhang
P and Wang S: A pilot study of circulating MicroRNA-125b as a
diagnostic and prognostic biomarker for epithelial ovarian cancer.
Int J Gynecol Cancer. 27:3–10. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Teng Y, Zhang Y, Qu K, Yang X, Fu J, Chen
W and Li X: MicroRNA-29B (mir-29b) regulates the Warburg effect in
ovarian cancer by targeting AKT2 and AKT3. Oncotarget.
6:40799–40814. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Cao Q, Lu K, Dai S, Hu Y and Fan W:
Clinicopathological and prognostic implications of the miR-200
family in patients with epithelial ovarian cancer. Int J Clin Exp
Pathol. 7:2392–2401. 2014.PubMed/NCBI
|
|
103
|
Kapetanakis NI, Uzan C, Jimenez-Pailhes
AS, Gouy S, Bentivegna E, Morice P, Caron O, Gourzones-Dmitriev C,
Le Teuff G and Busson P: Plasma miR-200b in ovarian carcinoma
patients: Distinct pattern of pre/post-treatment variation compared
to CA-125 and potential for prediction of progression-free
survival. Oncotarget. 6:36815–36824. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Meng X, Müller V, Milde-Langosch K,
Trillsch F, Pantel K and Schwarzenbach H: Diagnostic and prognostic
relevance of circulating exosomal miR-373, miR-200a, miR-200b and
miR-200c in patients with epithelial ovarian cancer. Oncotarget.
7:16923–16935. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Du Z and Sha X: Demethoxycurcumin
inhibited human epithelia ovarian cancer cells' growth via
up-regulating miR-551a. Tumour Biol. 39:10104283176943022017.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Chen S, Chen X, Xiu YL, Sun KX and Zhao Y:
MicroRNA-490-3P targets CDK1 and inhibits ovarian epithelial
carcinoma tumorigenesis and progression. Cancer Lett. 362:122–130.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Shuang T, Wang M, Shi C, Zhou Y and Wang
D: Down-regulated expression of miR-134 contributes to paclitaxel
resistance in human ovarian cancer cells. FEBS Lett. 589:3154–3164.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Zou YT, Gao JY, Wang HL, Wang Y, Wang H
and Li PL: Downregulation of microRNA-630 inhibits cell
proliferation and invasion and enhances chemosensitivity in human
ovarian carcinoma. Genet Mol Res. 14:8766–8777. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Zhang H and Li W: Dysregulation of
micro-143-3p and BALBP1 contributes to the pathogenesis of the
development of ovarian carcinoma. Oncol Rep. 36:3605–3610. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Zhang W, Zeng Q, Ban Z, Cao J, Chu T, Lei
D, Liu C, Guo W and Zeng X: Effects of let-7c on the proliferation
of ovarian carcinoma cells by targeted regulation of CDC25a gene
expression. Oncol Lett. 16:5543–5550. 2018.PubMed/NCBI
|
|
111
|
Liu MX, Siu MK, Liu SS, Yam JW, Ngan HY
and Chan DW: Epigenetic silencing of microRNA-199b-5p is associated
with acquired chemoresistance via activation of JAG1-Notch1
signaling in ovarian cancer. Oncotarget. 5:944–958. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Kobayashi M, Sawada K, Nakamura K,
Yoshimura A, Miyamoto M, Shimizu A, Ishida K, Nakatsuka E, Kodama
M, Hashimoto K, et al: Exosomal miR-1290 is a potential biomarker
of high-grade serous ovarian carcinoma and can discriminate
patients from those with malignancies of other histological types.
J Ovarian Res. 11:812018. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Zhao H, Bi T, Qu Z, Jiang J, Cui S and
Wang Y: Expression of miR-224-5p is associated with the original
cisplatin resistance of ovarian papillary serous carcinoma. Oncol
Rep. 32:1003–1012. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Chen Y, Chen Q, Liu Q and Gao F: Human
epididymis protein 4 expression positively correlated with miR-21
and served as a prognostic indicator in ovarian cancer. Tumour
Biol. 37:8359–8365. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Li L, Huang K, You Y, Fu X, Hu L, Song L
and Meng Y: Hypoxia-induced miR-210 in epithelial ovarian cancer
enhances cancer cell viability via promoting proliferation and
inhibiting apoptosis. Int J Oncol. 44:2111–2120. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Zhu X, Shen H, Yin X, Long L, Chen X, Feng
F, Liu Y, Zhao P, Xu Y, Li M, et al: IL-6R/STAT3/miR-204 feedback
loop contributes to cisplatin resistance of epithelial ovarian
cancer cells. Oncotarget. 8:39154–39166. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Fan Y, Fan J, Huang L, Ye M, Huang Z, Wang
Y, Li Q and Huang J: Increased expression of microRNA-196a predicts
poor prognosis in human ovarian carcinoma. Int J Clin Exp Pathol.
8:4132–4137. 2015.PubMed/NCBI
|
|
118
|
Koukourakis MI, Kontomanolis E,
Sotiropoulou M, Mitrakas A, Dafa E, Pouliliou S, Sivridis E and
Giatromanolaki A: Increased soluble PD-L1 levels in the plasma of
patients with epithelial ovarian cancer correlate with plasma
levels of miR34a and miR200. Anticancer Res. 38:5739–5745. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Liu J, Dou Y and Sheng M: Inhibition of
microRNA-383 has tumor suppressive effect in human epithelial
ovarian cancer through the action on caspase-2 gene. Biomed
Pharmacother. 83:1286–1294. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Dai F, Zhang Y and Chen Y: Involvement of
miR-29b signaling in the sensitivity to chemotherapy in patients
with ovarian carcinoma. Hum Pathol. 45:1285–1293. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Xiao M, Cai J, Cai L, Jia J, Xie L, Zhu Y,
Huang B, Jin D and Wang Z: Let-7e sensitizes epithelial ovarian
cancer to cisplatin through repressing DNA double strand break
repair. J Ovarian Res. 10:242017. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Li X, Pan Q, Wan X, Mao Y, Lu W, Xie X and
Cheng X: Methylation-associated Has-miR-9 deregulation in
paclitaxel-resistant epithelial ovarian carcinoma. BMC Cancer.
15:5092015. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Paudel D, Zhou W, Ouyang Y, Dong S, Huang
Q, Giri R, Wang J and Tong X: MicroRNA-130b functions as a tumor
suppressor by regulating RUNX3 in epithelial ovarian cancer. Gene.
586:48–55. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Duan S, Dong X, Hai J, Jiang J, Wang W,
Yang J, Zhang W and Chen C: MicroRNA-135a-3p is downregulated and
serves as a tumour suppressor in ovarian cancer by targeting CCR2.
Biomed Pharmacother. 107:712–720. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Chen X, Dong C, Law PT, Chan MT, Su Z,
Wang S, Wu WK and Xu H: MicroRNA-145 targets TRIM2 and exerts
tumor-suppressing functions in epithelial ovarian cancer. Gynecol
Oncol. 139:513–519. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Qin CZ, Lou XY, Lv QL, Cheng L, Wu NY, Hu
L and Zhou HH: MicroRNA-184 acts as a potential diagnostic and
prognostic marker in epithelial ovarian cancer and regualtes cell
proliferation, apoptosis and inflammation. Pharmazie. 70:668–673.
2015.PubMed/NCBI
|
|
127
|
Liang T, Li L, Cheng Y, Ren C and Zhang G:
MicroRNA-194 promotes the growth, migration, and invasion of
ovarian carcinoma cells by targeting protein tyrosine phosphatase
nonreceptor type 12. Onco Targets Ther. 9:4307–4315. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Wei C, Zhang X, He S, Liu B, Han H and Sun
X: MicroRNA-219-5p inhibits the proliferation, migration, and
invasion of epithelial ovarian cancer cells by targeting the
Twist/Wnt/β-catenin signaling pathway. Gene. 637:25–32. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Fu X, Li Y, Alvero A, Li J, Wu Q, Xiao Q,
Peng Y, Hu Y, Li X, Yan W, et al: MicroRNA-222-3p/GNAI2/AKT axis
inhibits epithelial ovarian cancer cell growth and associates with
good overall survival. Oncotarget. 7:80633–80654. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Wu X, Ruan Y, Jiang H and Xu C:
MicroRNA-424 inhibits cell migration, invasion, and epithelial
mesenchymal transition by downregulating doublecortin-like kinase 1
in ovarian clear cell carcinoma. Int J Biochem Cell Biol. 85:66–74.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Zhang J, Liu L, Sun Y, Xiang J, Zhou D,
Wang L, Xu H, Yang X, Du N, Zhang M, et al: MicroRNA-520g promotes
epithelial ovarian cancer progression and chemoresistance via DAPK2
repression. Oncotarget. 7:26516–26534. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Zhang L, Li Z, Gai F and Wang Y:
MicroRNA-137 suppresses tumor growth in epithelial ovarian cancer
in vitro and in vivo. Mol Med Rep. 12:3107–3114. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Liu J, Jin S and Wang R: MicroRNA-139
suppressed tumor cell proliferation, migration and invasion by
directly targeting HDGF in epithelial ovarian cancer. Mol Med Rep.
16:3379–3386. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Xu L, Li H, Su L, Lu Q and Liu Z:
MicroRNA-455 inhibits cell proliferation and invasion of epithelial
ovarian cancer by directly targeting Notch1. Mol Med Rep.
16:9777–9785. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Yan J, Jiang J, Meng XN, Xiu YL and Zong
ZH: MiR-23b targets cyclin G1 and suppresses ovarian cancer
tumorigenesis and progression. J Exp Clin Cancer Res. 35:312016.
View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Lin J, Zhang L, Huang H, Huang Y, Huang L,
Wang J, Huang S, He L, Zhou Y, Jia W, et al: MiR-26b/KPNA2 axis
inhibits epithelial ovarian carcinoma proliferation and metastasis
through downregulating OCT4. Oncotarget. 6:23793–23806. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Xu J, Jiang N, Shi H, Zhao S, Yao S and
Shen H: miR-28-5p promotes the development and progression of
ovarian cancer through inhibition of N4BP1. Int J Oncol.
50:1383–1391. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Wang Y, Zhang X, Tang W, Lin Z, Xu L, Dong
R, Li Y, Li J, Zhang Z, Li X, et al: miR-130a upregulates mTOR
pathway by targeting TSC1 and is transactivated by NF-κB in
high-grade serous ovarian carcinoma. Cell Death Differ.
24:2089–2100. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Wang L, He J, Xu H, Xu L and Li N: MiR-143
targets CTGF and exerts tumor-suppressing functions in epithelial
ovarian cancer. Am J Transl Res. 8:2716–2726. 2016.PubMed/NCBI
|
|
140
|
Dong M, Yang P and Hua F: miR-191
modulates malignant transformation of endometriosis through
regulating TIMP3. Med Sci Monit. 21:915–920. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Niu K, Shen W, Zhang Y, Zhao Y and Lu Y:
MiR-205 promotes motility of ovarian cancer cells via targeting
ZEB1. Gene. 574:330–336. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Dai C, Xie Y, Zhuang X and Yuan Z: MiR-206
inhibits epithelial ovarian cancer cells growth and invasion via
blocking c-Met/AKT/mTOR signaling pathway. Biomed Pharmacother.
104:763–770. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Xia B, Yang S, Liu T and Lou G: miR-211
suppresses epithelial ovarian cancer proliferation and cell-cycle
progression by targeting Cyclin D1 and CDK6. Mol Cancer. 14:572015.
View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Wu Q, Ren X, Zhang Y, Fu X, Li Y, Peng Y,
Xiao Q, Li T, Ouyang C, Hu Y, et al: MiR-221-3p targets ARF4 and
inhibits the proliferation and migration of epithelial ovarian
cancer cells. Biochem Biophys Res Commun. 497:1162–1170. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Cao L, Wan Q, Li F and Tang C: MiR-363
inhibits cisplatin chemoresistance of epithelial ovarian cancer by
regulating snail-induced epithelial-mesenchymal transition. BMB
Rep. 51:456–461. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Xia B, Li H, Yang S, Liu T and Lou G:
MiR-381 inhibits epithelial ovarian cancer malignancy via YY1
suppression. Tumour Biol. 37:9157–9167. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Yuan J, Wang K and Xi M: MiR-494 inhibits
epithelial ovarian cancer growth by targeting c-Myc. Med Sci Monit.
22:617–624. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Li N, Zhao X, Wang L, Zhang S, Cui M and
He J: miR-494 suppresses tumor growth of epithelial ovarian
carcinoma by targeting IGF1R. Tumour Biol. 37:7767–7776. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Zhou QH, Zhao YM, JIA LL and Zhang Y:
Mir-595 is a significant indicator of poor patient prognosis in
epithelial ovarian cancer. Eur Rev Med Pharmacol Sci. 21:4278–4282.
2017.PubMed/NCBI
|
|
150
|
Zhang S, Zhang JY, Lu LJ, Wang CH and Wang
LH: MiR-630 promotes epithelial ovarian cancer proliferation and
invasion via targeting KLF6. Eur Rev Med Pharmacol Sci.
21:4542–4547. 217.PubMed/NCBI
|
|
151
|
Shi C and Zhang Z: miR-761 inhibits tumor
progression by targeting MSI1 in ovarian carcinoma. Tumour Biol.
37:5437–5443. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Xie X, Huang Y, Chen L and Wang J: miR-221
regulates proliferation and apoptosis of ovarian cancer cells by
targeting BMF. Oncol Lett. 16:6697–6704. 2018.PubMed/NCBI
|
|
153
|
Wen C, Liu X, Ma H, Zhang W and Li H:
miR-338-3p suppresses tumor growth of ovarian epithelial carcinoma
by targeting Runx2. Int J Oncol. 46:2277–2285. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Salem M, O'Brien JA, Bernaudo S, Shawer H,
Ye G, Brkić J, Amleh A, Vanderhyden BC, Refky B, Yang BB, et al:
miR-590-3p promotes ovarian cancer growth and metastasis via a
Novel FOXA2-versican pathway. Cancer Res. 78:4175–4190. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Lin Z, Zhao J, Wang X, Zhu X and Gong L:
Overexpression of microRNA-497 suppresses cell proliferation and
induces apoptosis through targeting paired box 2 in human ovarian
cancer. Oncol Rep. 36:2101–2107. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Lin M, Xia B, Qin L, Chen H and Lou G:
S100A7 regulates ovarian cancer cell metastasis and chemoresistance
through MAPK signaling and is targeted by miR-330-5p. DNA Cell
Biol. 37:491–500. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Chen JL, Chen F, Zhang TT and Liu NF:
Suppression of SIK1 by miR-141 in human ovarian cancer cell lines
and tissues. Int J Mol Med. 37:1601–1610. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Zuberi M, Khan I, Gandhi G, Ray PC and
Saxena A: The conglomeration of diagnostic, prognostic and
therapeutic potential of serum miR-199a and its association with
clinicopathological features in epithelial ovarian cancer. Tumour
Biol. 37:11259–11266. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Guan X, Zong ZH, Chen S, Sang XB, Wu DD,
Wang LL, Liu Y and Zhao Y: The role of miR-372 in ovarian carcinoma
cell proliferation. Gene. 624:14–20. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Li J, Li D and Zhang W: Tumor suppressor
role of miR-217 in human epithelial ovarian cancer by targeting
IGF1R. Oncol Rep. 35:1671–1679. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Zhang X, Liu J, Zang D, Wu S, Liu A, Zhu
J, Wu G, Li J and Jiang L: Upregulation of miR-572
transcriptionally suppresses SOCS1 and p21 and contributes to human
ovarian cancer progression. Oncotarget. 6:15180–15193. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Zhou J, Gong G, Tan H, Dai F, Zhu X, Chen
Y, Wang J, Liu Y, Chen P, Wu X and Wen J: Urinary microRNA-30a-5p
is a potential biomarker for ovarian serous adenocarcinoma. Oncol
Rep. 33:2915–2923. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Zhang X, Li S, Dong C, Xie X and Zhang Y:
Knockdown of long noncoding RNA NR_026689 inhibits proliferation
and invasion and increases apoptosis in ovarian carcinoma HO-8910PM
cells. Oncol Res. 25:259–265. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Zhu L, Guo Q, Lu X, Zhao J, Shi J, Wang Z
and Zhou X: CTD-2020K17.1, a novel long non-coding RNA, promotes
migration, invasion, and proliferation of serous ovarian cancer
cells in vitro. Med Sci Monit. 24:1329–1339. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Qiu JJ, Zhang XD, Tang XY, Zheng TT, Zhang
Y and Hua KQ: ElncRNA1, a long non-coding RNA that is
transcriptionally induced by oestrogen, promotes epithelial ovarian
cancer cell proliferation. Int J Oncol. 51:507–514. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Gao Y, Meng H, Liu S, Hu J, Zhang Y, Jiao
T, Liu Y, Ou J, Wang D, Yao L, et al: LncRNA-HOST2 regulates cell
biological behaviors in epithelial ovarian cancer through a
mechanism involving microRNA let-7b. Hum Mol Genet. 24:841–852.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Wang Y, Wang H, Song T, Zou Y, Jiang J,
Fang L and Li P: HOTAIR is a potential target for the treatment of
cisplatin-resistant ovarian cancer. Mol Med Rep. 12:2211–2216.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Lu CW, Zhou DD, Xie T, Hao JL, Pant OP, Lu
CB and Liu XF: HOXA11 antisense long noncoding RNA (HOXA11-AS): A
promising lncRNA in human cancers. Cancer Med. 7:3792–3799. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Du W, Feng Z and Sun Q: LncRNA LINC00319
accelerates ovarian cancer progression through miR-423-5p/NACC1
pathway. Biochem Biophys Res Commun. 507:198–202. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Shu C, Yan D, Mo Y, Gu J, Shah N and He J:
Long noncoding RNA lncARSR promotes epithelial ovarian cancer cell
proliferation and invasion by association with HuR and miR-200
family. Am J Cancer Res. 8:981–992. 2018.PubMed/NCBI
|
|
171
|
Chen S, Wu DD, Sang XB, Wang LL, Zong ZH,
Sun KX, Liu BL and Zhao Y: The lncRNA HULC functions as an oncogene
by targeting ATG7 and ITGB1 in epithelial ovarian carcinoma. Cell
Death Dis. 8:e31182017. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Qnbo L, Guan W, Ren W, Zhang L, Zhang J
and Xu G: MALAT1 affects ovarian cancer cell behavior and patient
survival. Oncol Rep. 39:2644–2652. 2018.PubMed/NCBI
|
|
173
|
Lin Q, Guan W, Ren W, Zhang L, Zhang J and
Xu G: MALAT1 affects ovarian cancer cell behavior and patient
survival. Oncol Rep. 39:2644–2652. 2018.PubMed/NCBI
|
|
174
|
Yan C, Jiang Y, Wan Y, Zhang L, Liu J,
Zhou S and Cheng W: Long noncoding RNA NBAT-1 suppresses
tumorigenesis and predicts favorable prognosis in ovarian cancer.
Onco Targets Ther. 10:1993–2002. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Liu Y, Wang Y, Fu X and Lu Z: Long
non-coding RNA NEAT1 promoted ovarian cancer cells' metastasis
through regulation of miR-382-3p/ROCK1 axial. Cancer Sci.
109:2188–2198. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Chen S, Wang LL, Sun KX, Liu Y, Guan X,
Zong ZH and Zhao Y: LncRNA PCGEM1 induces ovarian carcinoma
tumorigenesis and progression through RhoA pathway. Cell Physiol
Biochem. 47:1578–1588. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
177
|
Huang K, Geng J and Wang J: Long
non-coding RNA RP11-552M11.4 promotes cells proliferation,
migration and invasion by targeting BRCA2 in ovarian cancer. Cancer
Sci. 109:1428–1446. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
178
|
Li H, Liu C, Lu Z, Chen L, Wang J, Li Y
and Ma H: Upregulation of the long non-coding RNA SPRY4-IT1
indicates a poor prognosis and promotes tumorigenesis in ovarian
cancer. Biomed Pharmacother. 88:529–534. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
179
|
Li TH, Zhang JJ, Liu SX and Chen Y: Long
non-coding RNA taurine-upregulated gene 1 predicts unfavorable
prognosis, promotes cells proliferation, and inhibits cells
apoptosis in epithelial ovarian cancer. Medicine (Baltimore).
97:e05752018. View Article : Google Scholar : PubMed/NCBI
|
|
180
|
Hong HH, Hou LK, Pan X, Wu CY, Huang H, Li
B and Nie W: Long non-coding RNA UCA1 is a predictive biomarker of
cancer. Oncotarget. 7:44442–44447. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
181
|
Zhang L, Cao X, Zhang L, Zhang X, Sheng H
and Tao K: UCA1 overexpression predicts clinical outcome of
patients with ovarian cancer receiving adjuvant chemotherapy.
Cancer Chemother Pharmacol. 77:629–634. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
182
|
Qiu JJ, Wang Y, Liu YL, Zhang Y, Ding JX
and Hua KQ: The long non-coding RNA ANRIL promotes proliferation
and cell cycle progression and inhibits apoptosis and senescence in
epithelial ovarian cancer. Oncotarget. 7:32478–32492. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
183
|
Cao Y, Shi H, Ren F, Jia Y and Zhang R:
Long non-coding RNA CCAT1 promotes metastasis and poor prognosis in
epithelial ovarian cancer. Exp Cell Res. 359:185–194. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
184
|
Hua F, Li CH, Chen XG and Liu XP: Long
Noncoding RNA CCAT2 knockdown suppresses tumorous progression by
sponging miR-424 in epithelial ovarian cancer. Oncol Res.
26:241–247. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
185
|
Yim GW, Kim HJ, Kim LK, Kim SW, Kim S, Nam
EJ and Kim YT: Long Non-coding RNA HOXA11 antisense promotes cell
proliferation and invasion and predicts patient prognosis in serous
ovarian cancer. Cancer Res Treat. 49:656–668. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
186
|
Koutsaki M, Spandidos DA and Zaravinos A:
Epithelial-mesenchymal transition-associated miRNAs in ovarian
carcinoma, with highlight on the miR-200 family: Prognostic value
and prospective role in ovarian cancer therapeutics. Cancer Lett.
351:173–181. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
187
|
Sulaiman SA, Ab Mutalib NS and Jamal R:
miR-200c regulation of metastases in ovarian cancer: Potential role
in epithelial and mesenchymal transition. Front Pharmacol.
7:2712016. View Article : Google Scholar : PubMed/NCBI
|
|
188
|
Teng Y, Su X, Zhang X, Zhang Y, Li C, Niu
W, Liu C and Qu K: miRNA-200a/c as potential biomarker in
epithelial ovarian cancer (EOC): Evidence based on miRNA
meta-signature and clinical investigations. Oncotarget.
7:81621–81633. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
189
|
Muralidhar G and Barbolina M: The miR-200
Family: Versatile players in epithelial ovarian cancer. Int J Mol
Sci. 16:16833–16847. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
190
|
Zuberi M, Khan I, Mir R, Gandhi G, Ray PC
and Saxena A: Utility of serum miR-125b as a diagnostic and
prognostic indicator and its alliance with a panel of tumor
suppressor genes in epithelial ovarian cancer. PLoS One.
11:e01539022016. View Article : Google Scholar : PubMed/NCBI
|
|
191
|
Faul C, Gerszten K, Edwards R, Land S,
D'Angelo G, Kelley J III and Price F: A phase I/II study of
hypofractionated whole abdominal radiation therapy in patients with
chemoresistant ovarian carcinoma: Karnofsky score determines
treatment outcome. Int J Radiat Oncol Biol Phys. 47:749–754. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
192
|
Iorio GC, Martini S, Arcadipane F, Ricardi
U and Franco P: The role of radiotherapy in epithelial ovarian
cancer: A literature overview. Med Oncol. 36:642019. View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Sorbe B: Consolidation treatment of
advanced ovarian carcinoma with radiotherapy after induction
chemotherapy. Int J Gynecol Cancer. 13 (Suppl 2):S192–S195. 2003.
View Article : Google Scholar
|
|
194
|
Pang L and Guo Z: Differences in
characteristics and outcomes between large-cell neuroendocrine
carcinoma of the ovary and high-grade serous ovarian cancer: A
retrospective observational cohort study. Front Oncol.
12:8916992022. View Article : Google Scholar : PubMed/NCBI
|
|
195
|
Patel SC, Frandsen J, Bhatia S and Gaffney
D: Impact on survival with adjuvant radiotherapy for clear cell,
mucinous, and endometriod ovarian cancer: The SEER experience from
2004 to 2011. J Gynecol Oncol. 27:e452016. View Article : Google Scholar : PubMed/NCBI
|
|
196
|
Pestell KE, Medlow CJ, Titley JC, Kelland
LR and Walton MI: Characterisation Of The P53 Status, Bcl-2
expression and radiation and platinum drug sensitivity of a panel
of human ovarian cancer cell lines. Int J Cancer. 77:913–918. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
197
|
Zielske SP: Epigenetic DNA methylation in
radiation biology: On the field or on the sidelines? J Cell
Biochem. 116:212–217. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
198
|
Kurrey NK, Jalgaonkar SP, Joglekar AV,
Ghanate AD, Chaskar PD, Doiphode RY and Bapat SA: Snail and slug
mediate radioresistance and chemoresistance by antagonizing
p53-Mediated apoptosis and acquiring a stem-like phenotype in
ovarian cancer cells. Stem Cells. 27:2059–2068. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
199
|
Liu WJ, Huang YX, Wang W, Zhang Y, Liu BJ,
Qiu JG, Jiang BH and Liu LZ: NOX4 signaling mediates cancer
development and therapeutic resistance through HER3 in ovarian
cancer cells. Cells. 10:16472021. View Article : Google Scholar : PubMed/NCBI
|
|
200
|
Chen J, Jia Y, Jia ZH, Zhu Y and Jin YM:
Silencing the expression of MTDH increases the radiation
sensitivity of SKOV3 ovarian cancer cells and reduces their
proliferation and metastasis. Int J Oncol. 53:2180–2190.
2018.PubMed/NCBI
|
|
201
|
Zhao Y, Liu S, Wen Y and Zhong L: Effect
of MicroRNA-210 on the growth of ovarian cancer cells and the
efficacy of radiotherapy. Gynecol Obstet Invest. 86:71–80. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
202
|
Xing Y, Cui D, Wang S, Wang P, Xing X and
Li H: Oleuropein represses the radiation resistance of ovarian
cancer by inhibiting hypoxia and microRNA-299-targetted heparanase
expression. Food Funct. 8:2857–2864. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
203
|
Marques C, Ferreira da Silva F, Sousa I
and Nave M: Chemotherapy-free treatment of recurrent advanced
ovarian cancer: Myth or reality? Int J Gynecol Cancer. 33:607–618.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
204
|
Marchetti C, De Felice F, Romito A,
Iacobelli V, Sassu CM, Corrado G, Ricci C, Scambia G and Fagotti A:
Chemotherapy resistance in epithelial ovarian cancer: Mechanisms
and emerging treatments. Semin Cancer Biol. 77:144–166. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
205
|
Falzone L, Bordonaro R and Libra M:
SnapShot: Cancer chemotherapy. Cell. 186:1816–1816.e1. 2023.
View Article : Google Scholar
|
|
206
|
Raab M, Sanhaji M, Zhou S, Rödel F,
El-Balat A, Becker S and Strebhardt K: Blocking mitotic exit of
ovarian cancer cells by pharmaceutical inhibition of the
anaphase-promoting complex reduces chromosomal instability.
Neoplasia. 21:363–375. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
207
|
Swanton C, Nicke B, Schuett M, Eklund AC,
Ng C, Li Q, Hardcastle T, Lee A, Roy R, East P and Kschischo M:
Chromosomal instability determines taxane response. Proc Natl Acad
Sci USA. 106:8671–8676. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
208
|
Pradhan M, Risberg BÅ, Tropé CG, van de
Rijn M, Gilks CB and Lee CH: Gross genomic alterations and gene
expression profiles of high-grade serous carcinoma of the ovary
with and without BRCA1 inactivation. BMC Cancer. 10:4932010.
View Article : Google Scholar : PubMed/NCBI
|
|
209
|
Tang Z, Yang J, Wang X, Zeng M, Wang J,
Wang A, Zhao M, Guo L, Liu C, Li D and Chen J: Active DNA end
processing in micronuclei of ovarian cancer cells. BMC Cancer.
18:4262018. View Article : Google Scholar : PubMed/NCBI
|
|
210
|
Morden CR, Farrell AC, Sliwowski M,
Lichtensztejn Z, Altman AD, Nachtigal MW and McManus KJ: Chromosome
instability is prevalent and dynamic in high-grade serous ovarian
cancer patient samples. Gynecol Oncol. 161:769–778. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
211
|
Gorringe KL, Chin SF, Pharoah P, Staines
JM, Oliveira C, Edwards PA and Caldas C: Evidence that both genetic
instability and selection contribute to the accumulation of
chromosome alterations in cancer. Carcinogenesis. 26:923–930. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
212
|
Bayani J, Paderova J, Murphy J, Rosen B,
Zielenska M and Squire JA: Distinct patterns of structural and
numerical chromosomal instability characterize sporadic ovarian
cancer. Neoplasia. 10:1057–1065. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
213
|
Birkbak NJ, Eklund AC, Li Q, McClelland
SE, Endesfelder D, Tan P, Tan IB, Richardson AL, Szallasi Z and
Swanton C: Paradoxical relationship between chromosomal instability
and survival outcome in cancer. Cancer Res. 71:3447–3452. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
214
|
Hille S, Rein DT, Riffelmann M, Neumann R,
Sartorius J, Pfützner A, Kurbacher CM, Schöndorf T and Breidenbach
M: Anticancer drugs induce mdr1 gene expression in recurrent
ovarian cancer. Anticancer Drugs. 17:1041–1044. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
215
|
Zhang C, Wang M, Shi C, Shi F and Pei C:
Long non-coding RNA Linc00312 modulates the sensitivity of ovarian
cancer to cisplatin via the Bcl-2/Caspase-3 signaling pathway.
Biosci Trends. 12:309–316. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
216
|
Cui Y, Qin L, Tian D, Wang T, Fan L, Zhang
P and Wang Z: ZEB1 Promotes chemoresistance to cisplatin in ovarian
cancer cells by suppressing SLC3A2. Chemotherapy. 63:262–271. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
217
|
Sen T, Sen N, Brait M, Begum S, Chatterjee
A, Hoque MO, Ratovitski E and Sidransky D: Np63 confers tumor cell
resistance to cisplatin through the AKT1 transcriptional
regulation. Cancer Res. 71:1167–1176. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
218
|
Kumar S, Kumar A, Shah PP, Rai SN,
Panguluri SK and Kakar SS: MicroRNA signature of cis-platin
resistant vs. cis-platin sensitive ovarian cancer cell lines. J
Ovarian Res. 4:172011. View Article : Google Scholar : PubMed/NCBI
|
|
219
|
Leung AWY, Veinotte CJ, Melong N, Melong
N, Oh MH, Chen K, Enfield KSS, Backstrom I, Warburton C, Yapp D, et
al: In vivo validation of PAPSS1 (3′-phosphoadenosine
5′-phosphosulfate synthase 1) as a cisplatin-sensitizing
therapeutic target. Clin Cancer Res. 23:6555–6566. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
220
|
Kritsch D, Hoffmann F, Steinbach D, Jansen
L, Mary Photini S, Gajda M, Mosig AS, Sonnemann J, Peters S,
Melnikova M, et al: Tribbles 2 mediates cisplatin sensitivity and
DNA damage response in epithelial ovarian cancer. Int J Cancer.
141:1600–1614. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
221
|
Nam EJ, Kim S, Lee TS, Kim HJ, Lee JY, Kim
SW, Kim JH and Kim YT: Primary and recurrent ovarian high-grade
serous carcinomas display similar microRNA expression patterns
relative to those of normal ovarian tissue. Oncotarget.
7:70524–70534. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
222
|
Chong GO, Jeon HS, Han HS, Son JW, Lee YH,
Hong DG, Lee YS and Cho Y: Differential MicroRNA expression
profiles in primary and recurrent epithelial ovarian cancer.
Anticancer Res. 7:2611–2617. 2015.
|
|
223
|
Chong GO, Jeon HS, Han HS, Son JW, Lee YH,
Hong DG, Park HJ, Lee YS and Cho YL: Overexpression of
microRNA-196b accelerates invasiveness of cancer cells in recurrent
epithelial ovarian cancer through regulation of homeobox A9. Cancer
Genomics Proteomics. 14:137–142. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
224
|
Zhou Y, Wang M, Wu J, Jie Z, Chang S and
Shuang T: The clinicopathological significance of miR-1307 in
chemotherapy resistant epithelial ovarian cancer. J Ovarian Res.
8:232015. View Article : Google Scholar : PubMed/NCBI
|
|
225
|
Chen C, Hu Y and Li L: NRP1 is targeted by
miR-130a and miR-130b, and is associated with multidrug resistance
in epithelial ovarian cancer based on integrated gene network
analysis. Mol Med Rep. 13:188–196. 2016. View Article : Google Scholar : PubMed/NCBI
|