Introduction
Mesenchymal tumor of the gallbladder is rare, and
the majority of cases present as sarcomas, which comprise
approximately 2% of all malignant tumors of the gallbladder
(1). Benign mesenchymal tumors of
the gallbladder are extremely rare, but granular cell tumor is the
most common type of benign mesenchymal tumor (2). Leiomyoma is one of the common
mesenchymal tumors of the gastrointestinal tract, particularly in
the esophagus and colon; however, only one case of leiomyoma of the
gallbladder has been reported in the English-language literature
(3). In this case report, we
describe a second case of leiomyoma of the gallbladder in a patient
with metastatic gastrointestinal stromal tumors (GISTs) in the
liver and discuss the differential diagnostic considerations. The
study was approved by the Ethics Committee of Shiga University of
Medical Science., Shiga, Japan. Informed consent was obtained from
the patient.
Case report
A 55-year-old female with a metastatic GIST in the
liver was identified, using computed tomography (CT), to also
possess a tumorous lesion of the gallbladder. The patient had
received a partial gastrectomy for submucosal tumor of the stomach
4 years previously, and a CT scan revealed multiple metastatic
lesions in the liver prior to surgery. The histopathological and
immunohistochmical analyses of the resected stomach specimen
identified a moderate risk GIST, according to the classification by
Miettinen et al (4). The
tumor size was 2.5 cm, mitotic figures were >5/50 high-power
fields, and immunohistochemical analysis revealed that the tumor
cells were positive for CD117 and CD34, but negative for desmin and
S-100 protein. Following surgery, imatinib was administered and
subsequently, follow-up CT revealed that the number and size of the
metastatic liver lesions were stable. A total of 4 years after the
surgery, a tumorous lesion, measuring 8 mm in diameter, was
identified in the neck of the gallbladder via follow-up CT.
Metastatic GIST in the gallbladder was clinically suspected, thus,
a laparoscopic cholecystectomy was conducted. The postoperative
course was uneventful.
Formalin-fixed, paraffin-embedded tissue blocks of
the resected gallbladder specimens were cut into 3-μm
sections, deparaffinized and rehydrated. Each section was stained
with hematoxylin and eosin, and then used for immunostaining and
in situ hybridization. Immunohistochemical and in
situ hybridization analyses were conducted using an autostainer
(XT system Benchmark; Ventana Medical Systems, Tucson, AZ, USA)
according to the manufacturer’s instructions. The following primary
antibodies were used: a mouse monoclonal antibody against
alpha-smooth muscle actin (alphasm-1; Novocastra Laboratories,
Ltd., Newcastle upon Tyne, UK), a mouse monoclonal antibody against
CD34 (QBEnd/10; Novocastra Laboratories, Ltd.), a rabbit polyclonal
antibody against CD117 (c-kit; DakoCytomation, Glostrup, Denmark),
a mouse monoclonal antibody against desmin (D33; DakoCytomation), a
mouse monoclonal antibody against h-caldesmon (h-CD;
DakoCytomation), a mouse monoclonal antibody against Ki-67 (MM1;
Novocastra Laboratories, Ltd.), and a rabbit polyclonal antibody
against S-100 protein (Nichirei Bioscience, Tokyo, Japan). For
in situ hybridization, an INFORM EBER (EBV-encoded early
RNA) 1 probe (Ventana Medical Systems) was used.
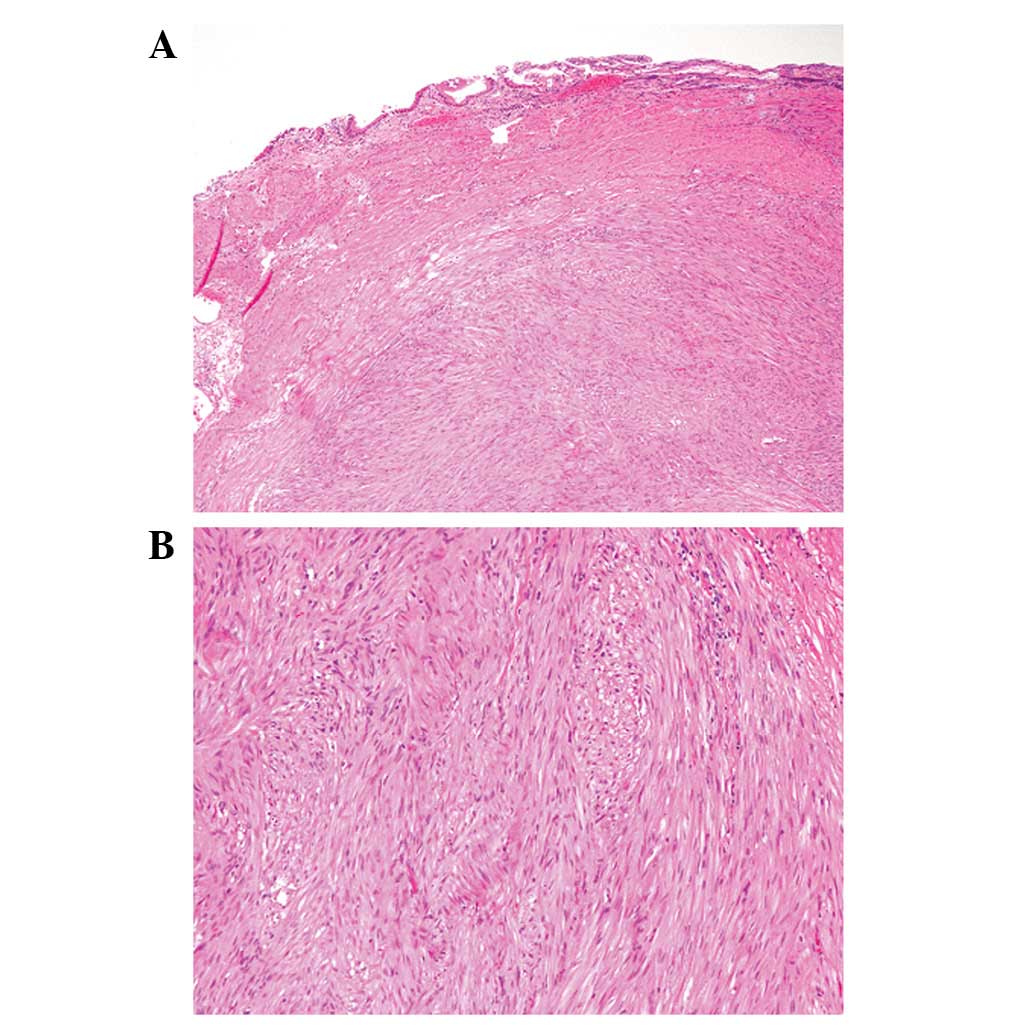
Gross examination revealed a sharply demarcated
intramural whitish nodule, measuring 8×7 mm in diameter, in the
neck of the gallbladder. Microscopically, the nodule was
well-circumscribed and appeared to have arisen from the muscular
layer of the gallbladder with pendulation into the mucosa. The
nodule was composed of a proliferation of spindle cells arranged in
intersecting fascicles, which contained eosinophilic cytoplasm and
bland cigar-shaped nuclei with blunt edges (Fig. 1). Mitotic figures were rarely noted
(<1/50 high-power fields), and necrosis was not observed.
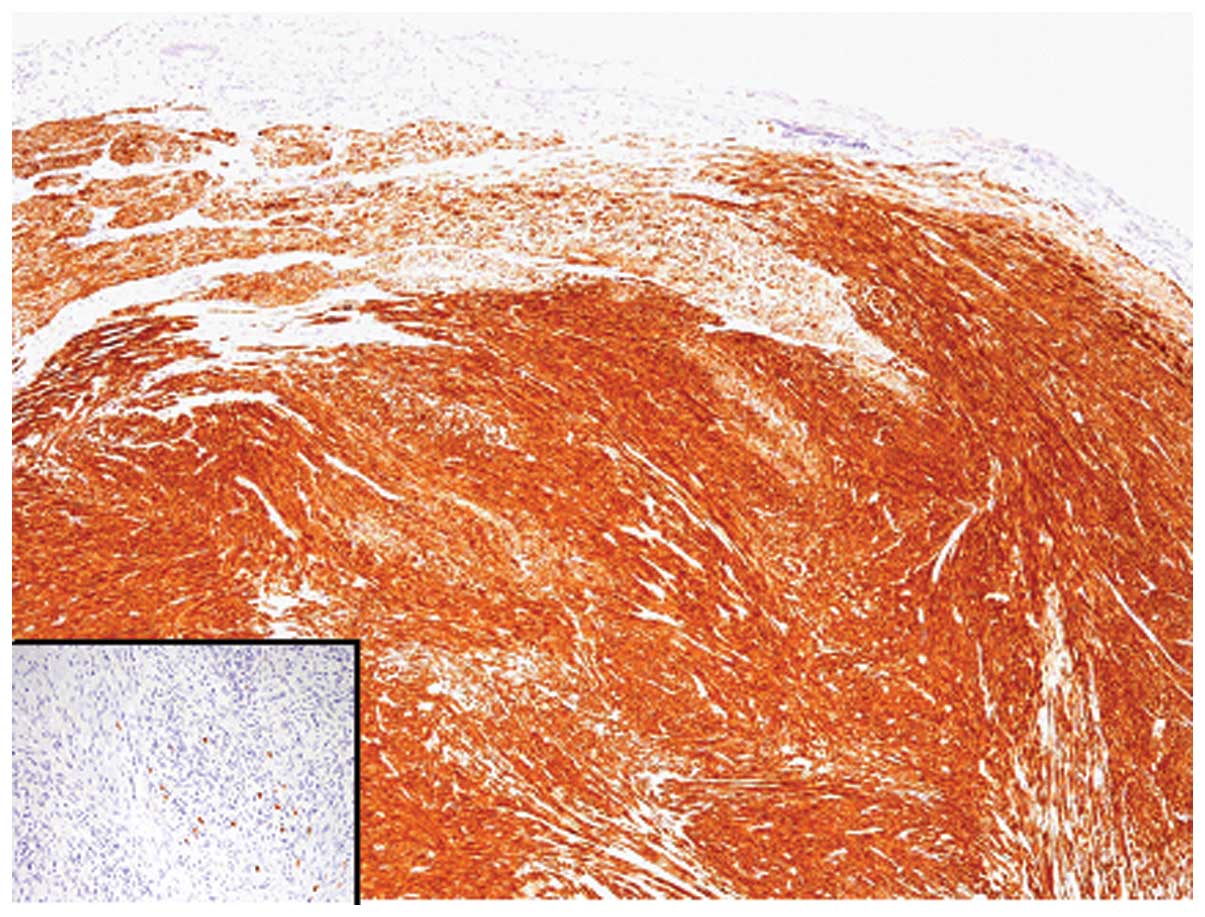
Immunohistochemical analyses revealed that tumor cells were
strongly and diffusely positive for desmin, alpha-smooth muscle
actin and h-caldesmon, and negative for CD34, CD117 and S-100
protein (Fig. 2). The Ki-67
labeling index was 0.4%. No EBER 1-positive cells were identified
using in situ hybridization.
According to these histopathological and
immunohistochemical findings, a final diagnosis of leiomyoma of the
gallbladder was made.
Discussion
Here, we describe the second reported case of
leiomyoma of the gallbladder in a patient with metastatic GIST in
the liver. Wachter et al first reported a case of leiomyoma
of the gall-bladder in 2010 (3).
The present case is unique since the patient had multiple
metastatic GISTs in the liver, and the gallbladder nodule was
preoperatively suspected to be metastatic GIST. Immunohistochemical
results of the present case (CD117 negativity and desmin
positivity) confirmed a diagnosis of leiomyoma.
Differential diagnosis of gallbladder leiomyoma
includes leiomyosarcoma and GIST (3). Leiomyosarcoma is the second most
common type of sarcoma in the gallbladder (6). In contrast to leiomyosarcoma,
leiomyoma lacks nuclear atypia, pleomorphism, increased mitotic
activity and necrosis, therefore, differentiation from
leiomyosarcoma is not difficult. Epstein-Barr virus
(EBV)-associated leiomyosarcoma/smooth muscle tumor occasionally
involves the gallbladder in a setting of immunosuppression, either
acquired or iatrogenic (2,5). This type of tumor is characterized by
the proliferation of oval to spindle-shaped mesenchymal cells, as
well as positive and negative immunoreactivity for alpha-smooth
muscle actin and desmin, respectively (5). EBER 1-positivity by in situ
hybridization is also a characteristic feature (5). In addition, GIST of the gallbladder is
rarely reported (6), and metastatic
GIST should be also included in the differential diagnostic
considerations, as in the present case. Although both leiomyoma and
leiomyosarcoma may occasionally mimic GIST in morphology, the
immunohistochemical characteristics of GIST can easily
differentiate leiomyoma (CD117 negativity and desmin positivity)
from GIST (CD117 positivity and desmin negativity) (5).
In conclusion, we report a case of leiomyoma of the
gallbladder. Leiomyoma of the gallbladder is extremely rare;
however, it may be an underrecognized entity. It is important to
differentiate leiomyoma from GIST to avoid unnecessary long-term
clinical follow-up and treatment.
References
|
1.
|
A DuffyM CapanuGK Abou-AlfaGallbladder
cancer (GBC): 10-year experience at Memorial Sloan-Kettering Cancer
Centre (MSKCC)J Surg Oncol98485489200818802958
|
|
2.
|
M MiettinenCDM FletcherLG
KindblomMesenchymal tumours of the gallbladder and extrahepatic
bile ductsWHO Classification of Tumours of the Digestive SystemFT
BosmanF CarneiroRH HrubanND TheiseIARCLyon2772010
|
|
3.
|
DL WachterMJ BüttnerK GrimmA HartmannA
AgaimyLeiomyoma of the gallbladder: a case report with review of
the literature and discussion of the differential diagnosisJ Clin
Pathol63177179201010.1136/jcp.2009.07064920154041
|
|
4.
|
M MiettinenJ LasotaGastrointestinal
stromal tumors: pathology and prognosis at different sitesSemin
Diagn Pathol237083200610.1053/j.semdp.2006.09.00117193820
|
|
5.
|
WI Al-DarajiHR MakhloufM MiettinenPrimary
gallbladder sarcoma: a clinicopathologic study of 15 cases,
heterogeneous sarcomas with poor outcome, except pediatric botryoid
rhabdomyosarcomaAm J Surg
Pathol33826834200910.1097/PAS.0b013e3181937bb3
|
|
6.
|
ID PeerlinckTT IrvinPT SarsfieldJM
HaringtonGIST (gastro-intestinal stromal tumour) of the
gallbladder: a case reportActa Chir Belg104107109200415053476
|