Introduction
Haemangioblastoma is a slowly growing, highly
vascular solid mass of uncertain histogenesis, also known as
capillary haemangioblastoma (1). It
typically occurs within the central nervous system (CNS),
predominantly in the cerebellum (2). Renal haemangioblastoma is an extremely
uncommon disease with a poorly established diagnosis due to a lack
of descriptions of typical symptoms. To the best of our knowledge,
there are 6 cases reported previously (Table I) (3,4). In
the present study, we report the case of a patient with
haemangioblastoma involving the kidney, which may be mistaken for
other renal tumours, in particular renal cell carcinoma (RCC). The
study was approved by the ethics committee of Peking University
Shenzhen Hospital, Shenzhen, China. Written informed patient
consent was obtained from the patient.
 | Table IReported cases of renal
haemangioblastoma. |
Table I
Reported cases of renal
haemangioblastoma.
| Case | Author | Year | Age
(years)/gender | Chief complaint | Size (cm) | Clinical
features | VHL (yes/no) | Immunohistochemical
staining | Follow-up (months)
prognosis |
|---|
| 1 | Nonaka | 2007 | 71/female | Asymptomatic | 6.8 | Right renal upper
pole | No | S100+,
SMA+, MSA+, calponin+,
vimentin+ | 108, without
disease |
| 2 | Ip | 2010 | 58/male | Haematuria and
polycythaemia | 5.5 | Right renal upper
pole | No | S100+,
NSE+, α-inhibin+ | 24, alive |
| 3 | Ip | 2010 | 55/female | Low back pain | 3.5 | Right renal upper
pole | No | S100+,
NSE+, α-inhibin+ | 48, alive |
| 4 | Verine | 2011 | 64/male | Other disease | 3.2 | Left renal upper
pole | No | CA-IX+,
S100+, NSE+, α-inhibin+ | 12, no
recurrence |
| 5 | Wang | 2012 | 29/male | Other disease | 2.7 | Right renal | No | S100+,
NSE+, α-inhibin+ | 20, without
disease |
| 6 | Liu | 2012 | 16/female | Haematuria | 1.2 | Left renal upper
pole | No | AE1/AE3−,
S100+, NSE+, α-inhibin+ | 6, no recurrence |
| 7 | Present | 2012 | 61/male | Checkup | 6.5 | Right renal upper
pole | No | S100+,
NSE+, α-inhibin+ | 12, no
recurrence |
Case report
A 61-year-old male, who was found to have a right
renal tumour during a routine examination, was admitted to our
department for further examination on April 20, 2011. The patient
was asymptomatic with a normal appetite, no abdominal pain and no
weight changes. The patient had no urinary, respiratory or
cardiovascular symptoms, no constitutional symptoms and had not
previously undergone surgery. His family history was unremarkable.
Physical examination revealed a well-developed and well-nourished
male. The patient was afebrile and had a pulse of 66 beats per min,
temperature 36.7°C, blood pressure 120/60 mmHg and respiration 20
per min. The chest was clear to percussion and auscultation and no
masses were palpable on abdominal examination.
Laboratory examination revealed that haemoglobin was
12.3 g/dl, white blood cell count was 7.21×109/l, with
61.4% granulocytes. Glucose was 5.88 mmol/l, blood urea nitrogen
was 8.25 mmol/l and serum creatinine was 82.2 μmol/l. Liver
function tests and serum electrolytes were within normal limits.
Urinalysis was unremarkable. Chest X-ray was normal. A non-contrast
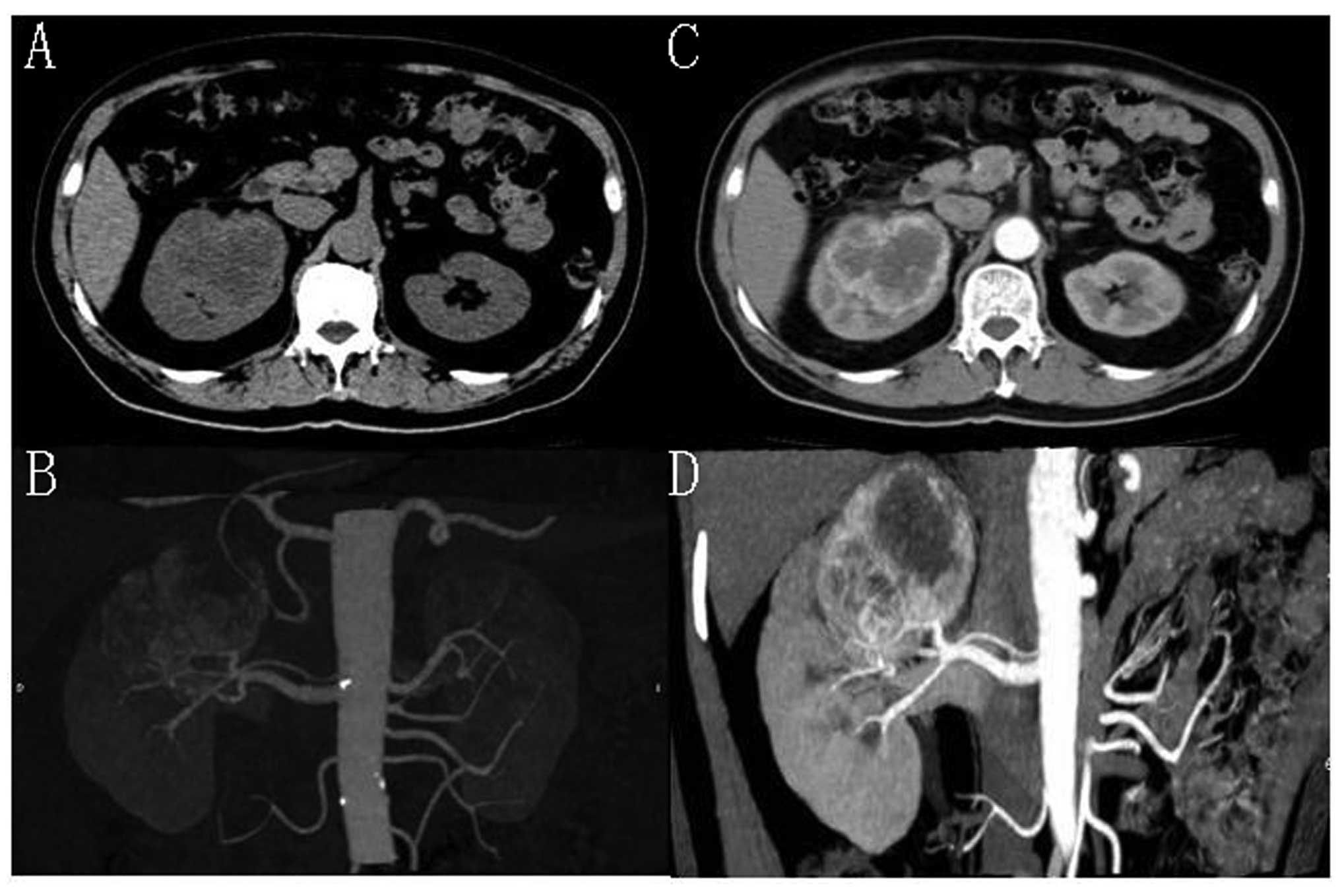
computed tomography (CT) scan of the kidneys revealed a 6.5×6.2-cm
round hypodense mass [48.2–54.2 Hounsfield units (HU)] in the upper
pole of the right kidney (Fig. 1A and
B). A contrast-enhanced CT revealed a heterogeneously enhanced
mass with a non-enhanced hypodense region in the centre (Fig. 1C and D).
A right radical nephrectomy was performed on April
25, 2011. Tumour invasion to the adjacent tissue was not observed.
Grossly, the tumour was a solid and well-encapsulated mass 6.5 cm
in diameter. Microscopic examination revealed polygonal cells
diffusely positive for α-inhibin, neuron-specific enolase (NSE) and
S100 and confirmed renal haemangioblastoma. There was no clinical
evidence of von Hippel-Lindau (VHL) disease. Magnetic resonance
imaging (MRI) revealed no other tumours.
The patient was discharged on the fifth
postoperative day after an uncomplicated post-surgical recovery. No
evidence of recurrence or residual disease appeared on CT scans at
follow-up (1 year).
Discussion
Capillary haemangioblastoma is a benign tumour of
uncertain histogenesis that generally occurs in a relatively
restricted area of the CNS (2). In
microscopic views, the tumours may exhibit significant nuclear
pleomorphism, mimicking carcinoma or other malignancies (1,2). A
majority of cases arise sporadically, whereas 25% are a
manifestation of VHL disease (5).
This tumour typically occurs within the CNS, predominantly in the
cerebellum (2). Haemangioblastoma
has also been rarely reported in sites outside of the CNS,
including peripheral nerves, liver, lung, pancreas,
retroperitoneum, kidney, pancreas, bladder, soft tissues of the
ankle and popliteal fossa and nasal skin, usually in the setting of
known VHL disease (6).
There are only a few studies concerning sporadic
haemangioblastoma occurring outside the central nervous system.
Sporadic renal haemangioblastoma are extremely rare, with only 6
cases reported previously (3,4). We
describe the 7th sporadic renal haemangioblastoma. The diagnosis in
the present case was based on the presence of typical morphology
and immunophenotype (S100+, NSE+,
α-inhibin+) (5).
CT scanning, with and without the administration of
contrast material, is necessary to take full advantage of the
contrast enhancement characteristics of highly vascular renal
parenchymal tumours. In general, any renal mass that enhances with
intravenous administration of contrast material on CT scanning by
more than 15 HU should be considered an RCC until proven otherwise
(7). In this patient, a
contrast-enhanced CT revealed a heterogeneously enhanced mass (more
than 20 HU; Fig. 1). The mass was
thus highly suggestive of RCC. Until now, characteristic imaging
features of renal haemangioblastoma remained unknown (3,5).
Haemangioblastoma is likely to be an underrecognised
tumour of the kidney as it mimics numerous tumour types
morphologically and is usually not considered in the differential
diagnosis (8). A correct diagnosis
is important for patients as haemangioblastoma is a benign disease,
unlike malignant RCC (3). It is not
necessary for patients with sporadic renal haemangioblastoma to
receive further treatment (e.g., molecular targeted therapy) and
their follow-up is different from that of patients with RCC
(3).
We report a solid lesion of the kidney found to be a
sporadic renal haemangioblastoma. Our review of published studies
revealed only 6 cases reported previously. Haemangioblastoma is
likely to be an underrecognised tumour of the kidney, as it mimics
a number of tumour types morphologically and is usually not
considered in the differential diagnosis. A correct diagnosis is
important to avoid overdiagnosis and unnecessary clinical
treatment.
Acknowledgements
This study was supported by the
National Natural Science Foundation of China (No. 81101922).
References
|
1
|
Karabagli H, Karabagli P, Alpman A and
Durmaz B: Congenital supratentorial cystic hemangioblastoma. Case
report and review of the literature. J Neurosurg. 107(Suppl 6):
515–518. 2007.PubMed/NCBI
|
|
2
|
Hussein MR: Central nervous system
capillary haemangioblastoma: the pathologist's viewpoint. Int J Exp
Pathol. 88:311–324. 2007.PubMed/NCBI
|
|
3
|
Wang CC, Wang SM and Liau JY: Sporadic
hemangioblastoma of the kidney in a 29-year-old man. Int J Surg
Pathol. Jan 23–2012.(Epub ahead of print).
|
|
4
|
Liu Y, Qiu XS and Wang EH: Sporadic
hemangioblastoma of the kidney: a rare renal tumor. Diagn Pathol.
May 1–2012.(Epub ahead of print).
|
|
5
|
Ip YT, Yuan JQ, Cheung H and Chan JK:
Sporadic hemangioblastoma of the kidney: an underrecognized
pseudomalignant tumor? Am J Surg Pathol. 34:1695–1700.
2010.PubMed/NCBI
|
|
6
|
Verine J, Sandid W, Miquel C, Vignaud JM
and Mongiat-Artus P: Sporadic hemangioblastoma of the kidney: an
underrecognized pseudomalignant tumor? Am J Surg Pathol.
35:623–624. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zagoria RJ and Dyer RB: The small renal
mass: detection, characterization, and management. Abdom Imaging.
23:256–265. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Nonaka D, Rodriguez J and Rosai J:
Extraneural hemangioblastoma: a report of 5 cases. Am J Surg
Pathol. 31:1545–1551. 2007. View Article : Google Scholar : PubMed/NCBI
|