Introduction
Papillary thyroid carcinoma is a common carcinoma.
During the past several decades, an increasing incidence of thyroid
cancer has been observed in several countries, including China.
However, papillary thyroid carcinoma with fibromatosis-like stroma
(PTC-FLS) is rare and was first reported in 1832 (1,2). A
discerning characteristic of PTC-FLS is the formation of fibroma
(nodular tumor composed of stromal cells) without large growth of
papillary carcinoma. The histogenesis and clinicopathological
features of PTC-FLS have not yet been fully clarified, due to the
rarity of the disease (3,4). Further investigation into PTC-FLS is
necessary. In the present study. one particular PTC-FLS case was
reported, and the diagnosis and management of this tumor was
reviewed through assessment of the literature.
Case report
A 42-year-old female patient was admitted to
Shaoxing Hospital (Shaoxing, China), due to a mass on the right
side of her neck. This mass had gradually enlarged over the
previous 7 months. Upon physical examination, a 3-cm firm nodular
mass was revealed in the right lobe of her thyroid gland. Serum
free tetra- and tri-iodothyronine (fT4 and fT3) and thyroid
stimulating hormone (TSH) tests, in addition to routine laboratory
examinations (including thyroid function tests) all exhibited
normal results. Additionally, thyroid peroxidase antibody (TPOAb),
thyroglobulin antibody (TgAb) and thyroid stimulating hormone
receptor antibody (TRAb) were at the normal level. A right
hemithyroidectomy with a central compartment lymphadenectomy was
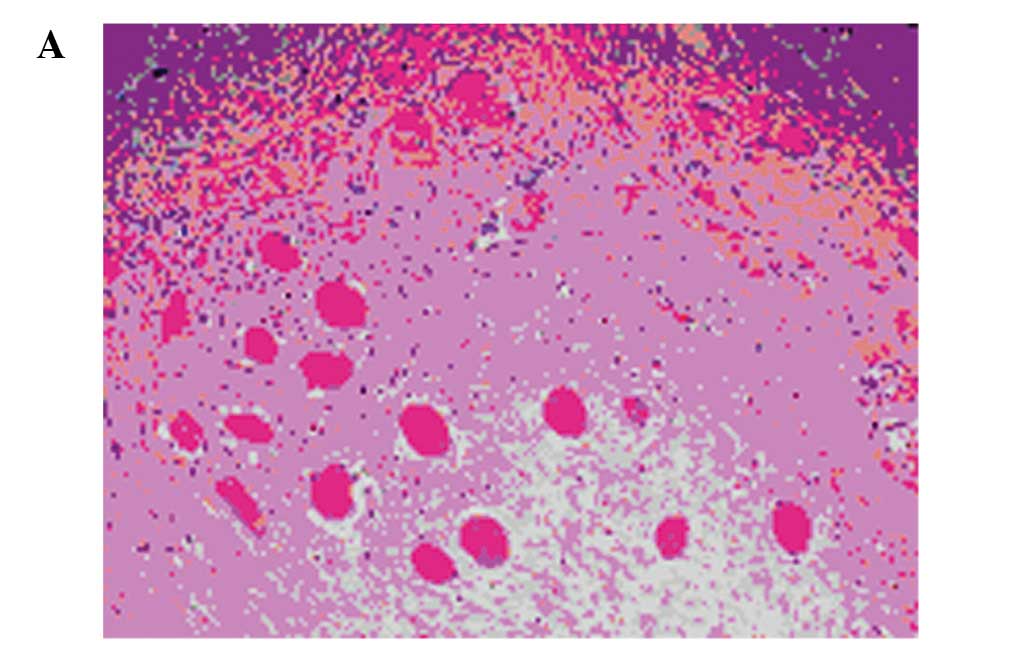
performed. Post-operative histologic examination revealed a
fibroma-like tumor (Fig. 1).
Histological examination identified a complex neoplasm in which a
minor component of typical papillary carcinoma was intermingled
with a dominant and exuberant stromal proliferation.
Immunohistology results revealed that the proliferated stromal
cells were positive for vimentin and smooth muscle actin (SMA), but
negative for thyroglobulin, S-100 and CK. Post-operative follow-up
was scheduled at 3-month intervals for 2 years and then at 6-month
intervals for the next 3 years. There were no signs of tumor
recurrence at the 5-year follow-up.
The study was approved by the Ethics Committee of
Shaoxing Hospital, China Medical University, Shaoxing, China.
Written informed consent was obtained from the patient prior to the
study.
Discussion
Here, we presented a case of PTC with
fibromatosis-like stroma. Papillary thyroid carcinomas typically
contain fibrous stroma of varying degrees and are occasionally
almost completely replaced by hyalinized fibrous tissues with
multiple or sole microcalcification. However, an extremely large
stromal component in PTC is rarely found, which is a typical
feature of PTC-FLS (5).
Fibromatosis is a tumor-like lesion that develops from fascia or
aponeurosis of fibrous tissue. It occurs mainly in the shoulder,
chest and back, but rarely in the thyroid. The etiology of PTC-FLS
is unknown; in 63% of cases there is a history of surgical trauma
(6). Studies have demonstrated that
one possible mechanism is that the stromal component is an
exaggerated mesenchymal reaction to injuries resulting from tumor
invasion into the stroma. Another possibility is that the stromal
component is hormone dependented tumorigenesis in nature (7). Notably, it has been revealed that
estrogen receptors are involved in 30% of PTC-FLS cases (8). Proliferating fibroblasts that had
formed lumps lined with carcinomatous epithelial components were
observed, which were similar to the leaf-like structures identified
in breast phyllodes tumors. PTC-FLS is considered to be at
high-risk of misdiagnosis, due to its rarity and fast-growing
biological behavior, in the same way as other malignant tumors.
On palpation, thyroid fibromatosis may be confused
with thyroid cancer; computerized tomography imaging revealed the
fibromatosis to be a large, irregular mass with a lobulated edge
and no capsule, exhibiting invasive growth into soft tissues and
surrounding muscles. Therefore, this mass may be easily
misdiagnosed as a malignant tumor (7). Although contrast-enhanced CT scans
reveal the rich blood supply in thyroid fibromatosis, this is
ineffective in differentiating thyroid fibromatosis from thyroid
cancer. The definitive diagnosis of PTC-FLS may be determined by
examining an intra-operative frozen section and a post-operative
paraffin section. PTC-FLS must be treated surgically as a low-grade
malignant tumor. As the recurrence rate for local excision is
20–45%, complete excision needs to be performed (9). In certain cases, when tumors invade
nerves and significant organs, it is difficult to perform this
procedure. Invaded organs have a greater impact on the patient’s
quality of life, rendering complete surgery a contradictory
solution. However, we suggest that complete surgery should be
performed if possible.
For patients who do not wish to undergo surgery or
cannot afford the operation, local excision in addition to
radiation therapy may be an effective treatment. Radiation therapy
is more suitable, as the recurrence rate is reduced with a
radiation dose of 50–60 Gy (10).
However, there are also numerous studies demonstrating the
ineffectiveness of radiotherapy (10). A number of systemic therapies have
been studied for inoperable cases of fibromatosis, such as
antiestrogens; nonsteroidal anti-inflammatory drugs (NSAIDs),
including indomethacin, sulindac and cyclo-oxygenase-2 (COX-2)
inhibitors; interferons and various other drugs, including
methotrexate in combination with doxorubicin, ifosfamide and
vinblastine or vinorelbine. In addition, more recently, target
therapy with imatinib has been applied in platelet-derived growth
factor receptor-beta (PDGFR-β)-positive tumors. Chemotherapy with a
low-dose of methotrexate and vinblastine (or its less neurotoxic
analog, vinorelbine) on a weekly basis has been demonstrated to
achieve a 70% relapse-free survival rate at 10 years (11). Likewise, indomethacin has been
demonstrated to be effective in certain cases of fibromatosis
(12). Traditional Chinese medicine
may also be effective in this disease.
The prognosis of this tumor depends on its size and
location. Typically, the 10-year survival rate is 94% and the
20-year survival rate is 86% (11).
However, for patients with aggressive fibromatosis involving vital
organs or large blood vessels, the survival rate is lower.
References
|
1
|
Mizukami Y, Nonomura A, Matsubara F,
Michigishi T, Ohmura K and Hashimoto T: Papillary carcinoma of the
thyroid gland with fibromatosis-like stroma. Histopathology.
20:355–357. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mizukami Y, Kurumaya H, Kitagawa T, Minato
H, Nonomura A, Michigishi T and Noguchi M: Papillary carcinoma of
the thyroid gland with fibromatosis-like stroma: a case report and
review of the literature. Mod Pathol. 8:366–370. 1995.PubMed/NCBI
|
|
3
|
Arena S, Salamone S, Cianci R, Scollo C,
Masucci R, Giannone G, Manusia M, Vigneri R and La Rosa GL:
Aggressive fibromatosis of the neck initiated after thyroidectomy.
J Endocrinol Invest. 29:78–81. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Schwarzlmüller B and Hofstädter F:
Fibromatosis of the thyroid gland region. An electron-microscopic
and enzyme-histochemical study. Virchows Arch A Pathol Anat Histol.
377:145–155. 1978.(In German).
|
|
5
|
Shields CJ, Winter DC, Kirwan WO and
Redmond HP: Desmoid tumours. Eur J Surg Oncol. 27:701–706. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pepe P, Panella P, Pennisi M and Aragona
F: Does color Doppler sonography improve the clinical assessment of
patients with acute scrotum? Eur J Radiol. 60:120–124. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Russ G, Bigorgne C, Royer B, Rouxel A and
Bienvenu Perrard M: The thyroid imaging reporting and data system
(TIRADS) for ultrasound of the thyroid. J Radiol. 92:701–713.
2011.(In French).
|
|
8
|
Mizukami Y, Nonomura A, Matsubara F,
Michigishi T, Ohmura K and Hashimoto T: Papillary carcinoma of the
thyroid gland with fibromatosis-like stroma. Histopathology.
20:355–357. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Clark SK and Phillips RK: Desmoids in
familial adenomatous polyposis. Br J Surg. 83:1494–1504. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kiel KD and Suit HD: Radiation therapy in
the treatment of aggressive fibromatoses (desmoid tumors). Cancer.
54:2051–2055. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ballo MT, Zagars GK, Pollack A, et al:
Desmoid tumor: prognostic factors and outcome after surgery,
radiation therapy, or combined surgery and radiation therapy. J
Clin Oncol. 7:158–167. 1999.PubMed/NCBI
|
|
12
|
Easter DW and Halasz NA: Recent trends in
the management of desmoid tumors. Ann Surg. 210:765–769. 1989.
View Article : Google Scholar : PubMed/NCBI
|